Abstract
Objective:
To summarize the currently published scientific evidence for the venous flow effects of mechanical devices, particularly intermittent pneumatic compression, and the relation to prevention of deep vein thrombosis (DVT).
Summary Background Data:
While intermittent pneumatic compression is an established method of DVT prophylaxis, the variety of systems that are available can use very different compression techniques and sequences. In order for appropriate choices to be made to provide the optimum protection for patients, the general performance of systems, and physiological effects of particular properties, must be analyzed objectively.
Methods:
Medline was searched from 1970 to 2002, and all relevant papers were searched for further appropriate references. Papers were selected for inclusion when they addressed specifically the questions posed in this review.
Results:
All the major types of intermittent compression systems are successful in emptying deep veins of the lower limb and preventing stasis in a variety of subject groups. Compression stockings appear to function more by preventing distension of veins. Rapid inflation, high pressures, and graded sequential intermittent compression systems will have particular augmentation profiles, but there is no evidence that such features improve the prophylactic ability of the system.
Conclusions:
The most important factors in selecting a mechanical prophylactic system, particularly during and after surgery, are patient compliance and the appropriateness of the site of compression. There is no evidence that the peak venous velocity produced by a system is a valid measure of medical performance.
Intermittent pneumatic systems for prevention of deep vein thrombosis will have different hemodynamic effects depending on their design. While all systems have been shown to be effective prophylaxis, there is no evidence that a particular compression sequence or construction is more effective than any other in preventing thrombosis.
Mechanical methods of deep vein thrombosis (DVT) prophylaxis have, over the last 30 years, gained widespread acceptance for surgical patients and are beginning to become popular in long-distance travel. However, intermittent compression devices, in particular, have developed into a great variety of forms, with little general understanding of the relative efficacy of specific systems. Although in essence all systems rely on a pump periodically inflating and deflating air bladders within cuffs that are wrapped around the limb, the cuffs can cover the calf, or a whole leg, or just the feet, can inflate uniformly, or sequentially with graded pressures, and can have rapid or moderate inflation rates. These different attributes naturally have cost implications, and, more importantly, possible influences on patient compliance, which is critical with these methods of prophylaxis; the longer they are used, the better the protection. Therefore, it is important, when choosing a system for patient care, to understand the hemodynamic reasoning behind its attributes, the validity of those claims, and any medical implications, before cost and compliance are considered. There is no doubt that intermittent compression prevents DVT, but does it require anything more than squeezing the leg once a minute?
The origins of the innovations in pump and cuff design are rooted in analysis of blood flow effects. The link between blood flow velocity and DVT is over a century-and-a-half old, since Rudolf Virchow not only first described DVT and the subsequent risk of pulmonary embolism, but afterward also deduced the causal factors.1–3 The so-called “triad” (stasis, vessel damage, and hypercoagulability) are still accepted influences on thrombogenesis, but it was prevention of stasis alone that drove the development of intermittent compression for prophylaxis of DVT. Electrical stimulation had been used to produce muscle contraction, to stimulate the natural muscle pump,4–6 but the intermittent compression methodology that already existed for treatment of lymphedema was soon adapted as an alternative that was more suitable for postsurgical application, since it was painless.7–9
All intermittent compression systems have a simple main objective, and that is to squeeze blood from the underlying deep veins, which, assuming that the valves are competent, will be displaced proximally. On deflation of the cuff, the veins will refill, and due to the intermittent nature of the system will ensure periodic flow of blood through the deep veins, so long as there is a supply. Properties of that pulse of flow, such as its peak velocity, duration, and percentage augmentation, can easily be assessed with Doppler ultrasound and have always been a source of competition between compression devices.
The aim of this review is to use the assessments of systems that have been made and published since the first systems were tested in the early 1970s to answer some common questions on flow properties, principally in relation to intermittent compression, and to determine the relevance of those data in preventing DVT.
MATERIALS AND METHODS
A Medline search was performed for 1970–2002 to identify all publication relating to mechanical prophylaxis of DVT, and those papers analyzing flow effects of the systems were selected. There was thorough follow-up of references quoted in the selected papers for publications not identified through Medline. The objective of this review was not to provide meta-analysis, or a systematic review, but rather to answer specific questions that have been posed to the authors during several years of research into the topic; therefore, references are given to those papers that specifically address the questions. In the case of typical flow velocities, or particular garment types (foot/calf/calf and thigh), references are prominent examples of publications from major journals that give sufficient data, and not every study that, for instance, has ever used foot compression. This article does not seek to endorse the product of any particular manufacturer, and all the types of compression discussed are available from several different manufacturers.
RESULTS
What Effect Do Intermittent Compression Systems Have on Venous Blood Flow Velocity?
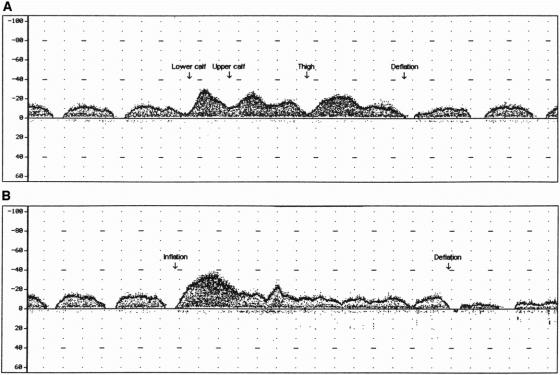
Intermittent compression systems augment blood flow in proximal veins for a short time, while they compress. The size, duration, and profile of that augmentation will be dependent on the particular compression system that is used. Changes have been observed in the femoral vein, as a result of calf and thigh compression,10–17 and of foot compression;14–19 in the popliteal vein due to calf compression,13,15,16 and foot compression;13,15,16,18,19 and in the posterior tibial vein after foot compression.13,19 It is, of course, difficult to measure changes in the popliteal vein with most thigh-length cuffs, just as measurements in the posterior tibial vein would not describe outflow effects when thigh or calf-length garments are used. Examples of velocity measurements in the femoral and posterior tibial veins are given in Figure 1, in this case due to foot compression. In the posterior tibial vein, there is a sharp augmentation, against a background of resting flow too slow to be detected, whereas the femoral augmentation is smoother, and greater in duration, with resting flow easily detectable.
FIGURE 1. A: Venous blood flow velocity in the posterior tibial vein during compression by a foot cuff (velocity [cm/s] vs. time [1 second per vertical dotted line]). B: Venous blood flow velocity in the femoral vein during compression by a foot cuff (velocity [cm/s] vs. time [1 second per vertical dotted line]).
The site of velocity measurement is important since the blood flow velocity in a vein is dependent on the diameter of that vein.20 Under normal circumstances, the greatest diameter of the common femoral vein is approximately 16 mm,21 the popliteal vein is 8 mm,21 and the posterior tibial vein 4 mm.22 Therefore, for a given amount of blood being ejected from, for instance, the foot, the velocities achieved would be expected to be higher in the posterior tibial vein than the femoral. However, the velocity must also depend on the part of the limb compressed, since the plantar venous plexus within the foot holds a smaller volume of blood than the calf and thigh. Different volumes of blood accelerated through the same blood vessel would be expected to have different velocity properties.
Reports have consistently shown that all intermittent compression systems produce changes in femoral vein velocity. At pressures around 40 mm Hg, the typical maximum velocities achieved with calf and/or thigh compression would be 35–60 cm/s11–13,17 with augmentations (maximum velocity during compression compared with maximum velocity resting) at around 50–250%.10,12,14,17 Corresponding popliteal velocities are around 55 cm/s.13 Pressures of 120 mm Hg have produced peak velocities of >100 cm/s in both popliteal and femoral veins,16 as has a system that inflates rapidly to 80 mm Hg before reducing to “normal” levels.17 Foot compression has produced more modest results, typically 20–40 cm/s in the femoral vein,13,17–19 with figures for the popliteal vein slightly higher (30–55 cm/s), as expected. Posterior tibial vein velocity in one example was over twice that in the popliteal vein.19
It should always be noted, however, that venous blood flow is variable. Not only will resting blood flow in the femoral vein change from person to person,23 but will change in a single subject over time, due to natural fluctuations in the inflow to the limb.24 The pattern of flow will change according to the particular physiology and body position at the time, with breathing and the cardiac cycle modulating the flow to differing extents.25 Moreover, venous blood pressure will change; therefore, the reproducibility of the velocity results from a particular pump in a particular individual over time will not be perfect.
Is Thigh Compression Important in DVT Prophylaxis?
Lower limb compression cuffs for DVT prophylaxis come in at least five varieties, foot compression, foot and calf compression, calf compression, calf and thigh compression, and whole limb compression, irrespective of how the compression is applied (ie, uniform/graded sequential). The choice of cuff is sometimes dictated by the circumstance – whole leg compression would not be appropriate during or after knee surgery – however, in other cases, the choice might not be obvious and would be left to the preference of the surgeon.
There have been few studies that have included the velocity effects of thigh and calf versus calf compression.11,12,17 Comparisons have been made between the pumps of different manufacturers, but the differences between the systems were greater than simply the garment length; therefore, the data are of questionable use to assess the thigh contribution. In a direct comparison of the thigh and calf garment of a single manufacturer, one study appeared to show higher peak velocities and augmentation for the thigh length garment, although there was no direct statistical evaluation of the difference.17 Assuming that graded sequential devices were not designed to produce higher peak velocities than uniform systems (and are therefore comparable for this measure, if not any other), then in 2 studies where uniform calf compression was compared with graded sequential thigh-length compression, 1 found no statistically significant difference in peak velocities,11 and the other showed calf compression to be preferable (peak 39.5 cm/s vs. 34.2 cm/s, augmentation 107.0% vs. 77.3%, P < 0.002).12
Clearly, sufficient direct evidence for a difference is lacking. Although it might seem logical that the more of the limb that you compress, the greater the effect, since the major deep veins of the thigh are supplied by the calf, it could be argued that calf compression is all that is necessary, as it will prevent stasis in the thigh. The DVT outcome studies comparing thigh and calf-length systems are similarly scarce. The research comparing calf-length uniform compression with thigh-length graded sequential compression reported no significant difference in the calf DVT outcomes, but a significant difference in the number of proximal DVT (7.2% calf-length, 2.4% thigh-length, P < 0.05).10 Again, due to the difference in the systems, it would be impossible to know which property of the particular system produced the difference, particularly since the uniform system inflated very slowly, and compressed in a 1 minute ‘on,’ 1 minute ‘off’ cycle, and that DVT was only detected some time after intermittent compression has ceased. Another study by Fedullo et al has been quoted by Vanek,26 which showed no significant difference, again between uniform calf compression, and graded sequential thigh-length compression.
If there is a difference in performance between calf, and thigh and calf compression, it is not yet clear, but it is clear that both types are effective.
Is Foot Compression as Effective as Calf Compression?
Foot compression has become a popular alternative to calf compression in recent years, especially during surgery on the lower limbs where calf compression might restrict access. Indeed, the “out of the way” nature of the cuffs has encouraged their use in all types of surgery. Foot compression, however, needs significantly higher pressures than calf compression, typically 130 mm Hg or more, compared with 40 mm Hg in the calf, there being a small amount of blood in the plantar venous plexus: about 20–30 mL,27 compared with 100–150 mL in the calf,28 and the muscles are less readily compressible. This inevitably means that patient compliance can be more of a problem with foot compression,29 although the proper use of intermittent compression in a hospital situation will depend on many other factors, such as staff training.30,31
There is good recent evidence that foot compression is hemodynamically effective,13–19,32–34 typically showing doubling of peak velocities on compression compared with resting, with some small differences between systems.13 Comparison with calf and/or thigh compression depends, as previously discussed, on the definition of a “good” response. In at least 2 such comparative studies, the performance of the foot compression devices was poorer than for other systems, and indeed worse than in noncomparative studies of foot compression.14,17 It would certainly appear, from limited information, that foot compression is less hemodynamically effective than calf compression (peak velocity, duration, etc.).16 The venous volume ejected by foot compression will always be lower16; therefore, even when systems are set to reduce high peak velocities, the augmentation would not be expected to last as long as from other compression systems.
DVT outcome studies on foot compression have also been generally positive, and it would appear from one study to be as effective as graded-sequential calf compression.35 Other investigations have compared foot compression to the use of heparin, aspirin, and compression stockings. The outcomes of those trials cannot be used to compare with those from calf compression, as there would be so many confounding factors, but in general it would appear that foot compression is more effective than certain types of heparin and aspirin,36,37 and stockings, but perhaps not as effective,38 or at least no more effective,29 than low molecular weight heparin. The combination of stockings and foot compression has proved more effective than stockings alone in both DVT and pulmonary embolism incidence.39,40
Is Graded Sequential Compression “Better” Than Uniform Compression?
Graduated or graded sequential compression uses multiple bladders to compress the limb in a “milking” action. The cuffs are sequential because the most distal bladder inflates first and the most proximal bladder last and are graded because the most distal bladder will inflate to the highest pressure, and the most proximal to the lowest. The cuffs were devised after rigorous laboratory work on fluid flow,41–43 which indicated that they would be more efficient at emptying a limb.
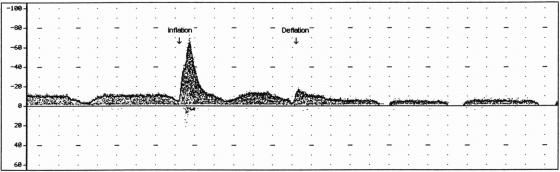
A typical velocity profile from such a system is shown in Figure 2a, where it can be seen that the individual bladders (their inflations labeled in the figure) produce individual peaks in the augmentation, effectively spreading out the augmentation over a long period. The peak velocities produced by such systems are however generally no higher than simpler uniform compression, an example of which is the response in Figure 2b.
FIGURE 2. A: Venous blood flow velocity in the femoral vein during compression by a three-bladder graduated sequential thigh-length cuff (velocity [cm/s] vs. time [1 second per vertical dotted line]). B: Venous blood flow velocity in the femoral vein during compression by a two-bladder uniform thigh-length cuff (velocity [cm/s] vs. time [1 second per vertical dotted line]).
Whether graded sequential is “better” than uniform depends on how you define the success of intermittent compression. If the aim is to extend the augmentation period by a second or 2 over that produced otherwise, then they are “better.” However, intermittent compression for DVT prophylaxis aims to prevent thrombosis. In that regard, there is no evidence that they are significantly better, as concluded early on in a paper by Salzman et al,44 among whose authors were Kamm and Shapiro who were instrumental in designing a graded sequential system. The conclusion has been confirmed by others more recently.45 To quote Salzman et al: “These results suggest either that uniform compression offers all that can be expected of external pneumatic calf compression in prevention of venous thrombosis, or that even if a study with greater statistical power showed graded-sequential filling to be superior, the benefit/cost ratio of the more complex latter system is not likely to be large.” Fifteen years later, complexity in an intermittent compression system has still not been shown to equate with efficacy.
Is “Distal Venous Trapping” Important?
Graduated compression was devised, partly due to the concerns about the phenomenon termed “distal venous trapping.” The idea was first documented by Kamm and Shapiro in 1976,46 and was promoted again by Nicolaides et al in 1980.10 Simply expressed, distal venous trapping is when a cuff system compresses both the calf and thigh simultaneously, and the blood ejected from the calf is prevented from returning to the heart by the compressed thigh. The other manifestation would be a single bladder where a proximal section of vein is caused to collapse before the rest, trapping blood in the distal segment. Kamm and Shapiro used models of veins to show that collapse during compression could occur in only a very small proximal part of the vein, producing outflow characteristics that they had measured from their hydraulic models.
The implication of that research was that trapping was a property of uniform compression systems and would prevent proper emptying of the deep veins by the cuffs. However, if this were true, there would surely be evidence either that uniform systems had poorer velocity properties, or worse DVT incidence, and as has been noted, DVT incidence has never been shown to be poorer with uniform systems.
Nicolaides et al10 produced illustrations of apparent distal venous tapping with uniform compression. When a cuff inflates, it empties the deep veins; when it deflates, those deep veins must refill. When observations are made on deflation, for instance in the femoral vein, the flow velocity will decline, sometimes to zero, as the inflow is taken up refilling the deep veins (a notable reduction can be seen in Fig. 2b from a uniform compression system). Nicolaides et al showed examples where there was no reduction in velocity on deflation, and assumed that there was no emptying, and therefore, distal venous trapping. However, if there had been no emptying, there would have been no augmentation of flow, which there clearly was in the illustration. Indeed, experimentally, with the variability of venous flow, it is quite easy to select examples where there is comparably little reduction postcompression, with whatever system. Figure 3 is an example from a type of graded sequential system where there is not only no decrease but a notable increase in flow on deflation, indicating blood trapped in the knee and/or foot region.
FIGURE 3. Venous blood flow velocity in the femoral vein during compression by a two-bladder graduated sequential thigh-length cuff (velocity [cm/s] vs. time [1 second per vertical dotted line]).
Distal venous trapping happens, but there is no evidence that it happens consistently, or with a particular system. Indeed, if it does happen sporadically, it is probably of little consequence as the time the blood is “trapped” is only short. A variety of perfectly natural activities, such as yawning, laughing, and coughing, will restrict outflow for short times. Some blood will have been emptied from the veins beneath the cuff if flow is augmented proximally, and that should be enough to prevent stasis. Until there is firm evidence of distal venous trapping reducing the effectiveness of DVT prophylaxis, it cannot be considered an important feature of intermittent compression generally, and only when uniform compression is shown to have worse DVT outcomes than graded sequential compression can distal venous trapping be considered a negative aspect of uniform compression in particular.
Is “Asymmetric” Compression Different to Circumferential Compression?
Aside from the site of compression and the graded sequential/uniform difference, there is another way to differentiate compression systems, and that is in the extent of the air bladders. Some particularly older systems have bladders that extend over the whole limb (circumferential), either as boots that zip up or wrap-around garments rather like extended sphygmomanometer cuffs. The total volume of the bladder is then quite large, and powerful pumps are required for inflation unless extremely long inflation times are used. The noncircumferential (“asymmetric”)-type garments typically have a smaller bladder in the part of the garment that is placed at the back of the limb. The bladder will extend along the length of the garment, but not to its entire circumference. The idea is that the inflation of the bladder will act against the nonstretching material around the rest of the limb, and compression will be applied along the whole surface.
There remains little research into the relative physiological and medical merits of these different cuff formats, except to say that both circumferential (boot or cylinder type,47,48 and wrap-around49,50) and noncircumferential51,52 have been used with success in DVT prophylaxis, and both have been shown to prevent stasis.12,14,17 One study53 has used finite-element analysis to model the deformation of a limb under those different compression cuffs. It concluded that so-called “asymmetric” (ie, noncircumferential) calf compression had advantages in emptying veins over circumferential calf compression. However, it should be noted that their model was quite simple and assumed compression at points at the front and back of the limb. In a real cuff, the bladder is only at the back, although it is assumed that the material over the rest of the limb has an effect. Foot compression can also be “asymmetric” (compressing the sole of the foot) or “circumferential” (compressing the whole foot), but there is no specific comparative research in this area.
Is Intermittent Compression Effective in the Upper Limb?
Intermittent compression of the arms for prevention of DVT at that site is a relatively new area of interest, but upper limb DVT is being reported, particularly associated with central venous catheters.54 There are patents for upper-limb cuffs for possible prophylactic devices, but not published experimental data. Some experimentation has looked at systemic effects of intermittent compression (on fibrinolysis) by compressing the arms, and measuring lower limb DVT outcomes.55 Most upper limb intermittent compression is to treat lymphedema.56
What Effect Do Compression Stockings Have on Venous Blood Flow Velocity?
Compression stockings are cheaper and simpler than intermittent compression devices and, for that reason, remain the most popular physical method of DVT prophylaxis. Their method of action, however, remains unclear. There is growing consensus that they are effective DVT prophylaxis,57–60 although perhaps not as effective as anticoagulants or intermittent compression.26 There has been suggestion that they are not as useful in certain types of orthopedic surgery as in other procedures61,62 but may, in combination with other prophylactic methods, be more effective than it or the other method alone.60
Much of the initial enthusiasm for compression stockings was supported by physiological evidence from radiopharmaceutical clearance,63–65 invasive electromagnetic flowmeters,7 and early Doppler ultrasound,66,67 that intermittent compression increased resting venous blood flow velocities. The method of action that is often quoted, and has been suggested for some time,68 is that the stockings compress the veins and reduce their diameter. The velocity of a given amount of blood flowing through a vessel is dependent on its cross-sectional diameter, as previously stated; therefore, the stockings would be expected to increase the velocity in the vein.
Some later studies using modern duplex ultrasound techniques have found no increases in resting flow velocity when stockings are worn.11,21,69 The diameter of veins under stockings has been found to reduce,70 and there have been measurements of changes in indices such as venous volume, and ejection fraction after tiptoe exercise,71,72 and venous capacitance after cuff compression.73 The evidence, when grouped together, suggests that a significant effect of stockings may be to reduce pooling of blood in deep veins by mechanically preventing distension of the vessels. Operative venodilatation has been recorded,74 and it would be logical for the risk of stasis to be higher during surgery where there is excessive venous distension. Improvements in venous pump function would perhaps be of more relevance in preventing travel DVT, and to aid those with chronic venous insufficiency, than those immobile during surgery.
The major drawback with stockings is their fitting. Thigh-length stockings, in particular, appear to be difficult to apply and wear in some circumstances, and some have preferred calf-length stockings for that reason.75–77 More worrying are studies of thigh-length,78 and calf-length79 stockings in clinical settings where the large majority of the stockings did not produce the pressure profile intended by the manufacturers (98% for calf-length), and the majority (70% for thigh-length, 54% for calf-length) produced “reverse gradients,” where the pressure was higher at the proximal end of the cuff. The danger is that poorly fitted stockings, or those of an incorrect shape and size, could produce “tourniquets” at the proximal end, causing ischemia,80 and an increased risk of thrombosis.79
The hemodynamic effects of stockings remain uncertain, although prevention of pooling is a plausible mechanism for their undoubted efficacy in preventing DVT. While not necessarily as effective as other prophylactic methods, their ready availability would recommend their use in the absence of other options, or in combination with other methods. However, it is vitally important that stockings are correctly fitted, and do not wrinkle, slip, or otherwise produce a compressive band at the proximal end.
Should Compression Stockings Be Used in Combination With Intermittent Compression?
Some manufacturers of intermittent compression systems, particularly those who also produce stockings, recommend that the two types of compression should be worn together: the stockings underneath the cuff. If the proposed mechanisms of action are true (stockings preventing distension, intermittent compression emptying veins), then there is no reason why both should not be worn together, as they are separate effects. However, there is relatively little research into either the hemodynamic effects (whether stockings improve the velocity augmentation of intermittent compression) or into the DVT outcomes. The first major study, which is often quoted, found that there was a reduction in rates of DVT in general surgical patients when graduated compression stockings were worn with graded sequential intermittent compression, as opposed to the intermittent compression alone.81 Velocity studies, however, have not been as positive, with the combination of the same stockings and the same intermittent compression device producing augmentation equal to intermittent compression alone,11 and stockings in combination with foot compression even appear to have reduced the expected velocities.82
There is not enough research into this area of combined treatments to come to definite conclusions. Although the potential for intermittent compression and compression stockings for DVT prophylaxis emerged at around the same time, compression stockings have gained acceptance more rapidly, despite slightly inferior levels of scientific evidence. Therefore, it is not surprising that in comparisons of efficacy so few have used stockings as the variable against a background of intermittent compression. If combined use could provide even greater protection, then it would be necessary to research the fitting of the stockings, and the potential of intermittent compression to exacerbate the wrinkling of stockings beneath.
What Effect Do Exercise Devices Have on Venous Blood Flow Velocity?
While physical methods of DVT prophylaxis have been used in the surgical environment because the risk of bleeding is lessened, they would appear to be ideally suited to use in long-haul travel. Although the possible risk of DVT during flights has been suggested for more than 60 years,83 it has only recently occupied the public mind. Intermittent compression devices have not yet been developed into forms that would be used easily during long-haul travel. Exercise devices (air cushions, primarily) have therefore been recommended, along with compression stockings.84
Most of the exercise devices encourage limb exercise by the user, who pushes air from the bladder under one foot to the bladder under their other foot, or alternatively to a second bladder under the same foot (front to back, and vice versa) in a similar action to the treddle devices, which are also available. The cushions do not provide any prophylaxis by themselves, they simply, at best, allow plantar and dorsiflexion, which is known to effectively empty the deep veins by activating the calf muscle pump14,17 and, therefore, is a perfectly good way of preventing stasis. “Stamping” on the cushion with no flexion would be unlikely to be as efficient, as the calf muscles are not as actively employed. The drawback of exercise devices is obvious; they are not effective when not used, especially not when sleeping on the plane.
DISCUSSION
The first conclusion that is obvious from the publications that have been quoted here is that intermittent compression works. Even relatively simple, gentle systems prevent venous stasis efficiently, and the many clinical papers on intermittent compression26 show that the method is effective in preventing thrombosis, and compares favorably with pharmacological prophylaxis. There are clearly flow implications to the particular type of compression used, but evidence for the clinical influences of those differences in flow patterns (peak velocity, duration, etc.) are poor or nonexistent. There is no reason to believe that any particular compression is more or less effective in preventing DVT than any other system. This is particularly true when peak velocities are considered, which are a very popular measure among some manufacturers of the “efficacy” of their systems. There is no evidence that intermittent compression systems that produce higher velocities on compression yield lower DVT rates. High peak velocity does not equal better DVT protection. Indeed, one recent study by Proctor et al would suggest the opposite.45 A rapidly inflating device (‘V’ in the paper), designed to produce high velocities, produced higher DVT incidences than slower systems, although one paper alone would not be sufficient to caution against using rapidly inflating cuffs.
The scope of this review has been limited to the flow velocity effects of the mechanical prophylaxis systems. There is no doubt that they prevent DVT, but what is clear from the published papers is that there is considerable uncertainty as to how intermittently compressing veins prevents DVT. The general assumption that prevention of stasis is the key has not been proved, though seems likely. There has been some conjecture about how compression might promote flow disturbance in valve pockets, thereby stripping away forming thrombi,43,85 but again there is no convincing scientific evidence. However, since 1976 when Knight and Dawson suggested that applying leg cuffs to the arm prevented DVT in legs,55 there has been good research into possible systemic hematological effects, particularly changes in fibrinolysis.86–92 Hypercoagulability is another of Virchow's triad, and its prevention, without having necessarily to compress the site where a DVT might form, would greatly enhance the usefulness of intermittent compression. The results of the research have been mixed, but it should be remembered that hematological tests for fibrinolysis have evolved and are continuing to evolve over the 30 years of work. This area has probably not attracted the volume of research that is deserves, and current work may yet yield exciting results. If a definite change could be shown, then there remains the question of how the compression effects hematological changes, and what is the connection with the well-described hemodynamic changes.
Whatever the mechanism of the effects of mechanical systems, they offer a simple, and generally complication-free prophylactic method for most surgical patients. There have been a few reports of compartment syndrome when intermittent compression is used with surgery in the lithotomy position,93–95 although another report96 demonstrated that it was the lithotomy position itself that was to blame for the syndrome, and that intermittent compression even prevented the increase in intracompartment pressure. There have been 4 cases of peroneal nerve palsy reported in association with use of intermittent compression, (plus stockings in 2 cases).93,97,98 The suggestion has been made that the cuff might compress the nerve against the fibular head, although for this to be likely a calf or calf and thigh garment must be worn quite high up on the limb. While the issue must be kept under review, the current evidence is only from case reports where there is great uncertainty as to the etiology of the condition.
The popularity of mechanical methods of prophylaxis has spread steadily since initial development, although awareness of intermittent compression, particularly outside the United States, is not as widespread as stockings or pharmacological products. The only disadvantages of intermittent compression over pharmacological prophylaxis are principally those of application and compliance; intermittent compression can only be certain to be preventing stasis when applied to the limb, although there may be longer-term hematological changes after application. However, these issues can be resolved with training and education, particularly in the correct application of the devices,31,99 and use before, during, and after surgery. It is perhaps less important, in a clinical setting, to spend extra money on systems that produce particularly high velocities, than to ensure that whichever system is used is applied with an appropriate protocol, and patient use and compliance are monitored correctly.
CONCLUSION
Intermittent compression prevents DVT and prevents venous stasis. The precise way in which that stasis is prevented appears to be of much less relevance than ensuring that systems are applied properly.
ACKNOWLEDGMENTS
Huntleigh Technology PLC provided financial support to Dr. Morris, in the form of a Research Fellowship.
Footnotes
Reprints: Rhys Morris, PhD, Department of Medical Physics and Bioengineering, University of Wales College of Medicine, Heath Park, Cardiff, CF14 4XN, Wales, UK. E-mail: morrisrj@cf.ac.uk.
REFERENCES
- 1.Virchow RLK. Die Verstopfung den Lungenarterie und ihre Flogen. Beitr Exper Path Physiol. 1846;2:1. [Google Scholar]
- 2.Virchow RLK. Phlogose und Thrombose im Gefäßsystem. Gesammelte Abhandlungen Zur Wißenschaftlischen Medizin. Frankfurt-am-Main: Von Meidinger Sohn & Comp; 1856:458–636. [Google Scholar]
- 3.Virchow RLK. Neuer Fall von t”dtlicher Embolie der Lungenarterien. Arch Pathol Anat. 1856;10:225–228. [Google Scholar]
- 4.Doran FSA, Drury M, Sivyer A. A simple way to combat the venous stasis which occurs in the lower limbs during surgical operations. Br J Surg. 1964;51:486–492. [DOI] [PubMed] [Google Scholar]
- 5.Browse NL, Negus D. Prevention of postoperative leg vein thrombosis by electrical muscle stimulation: an evaluation with 125I-labelled fibrinogen. Br Med J. 1970;3:615–618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nicolaides AN, Kakkar VV, Field ES, et al. Optimal electrical stimulus for prevention of deep vein thrombosis. Br Med J. 1972;3:756–758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sabri S, Roberts VC, Cotton LT. Prevention of early postoperative deep vein thrombosis by intermittent compression of the leg during surgery. Br Med J. 1971;4:394–396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hills NH, Pflug JJ, Jeyasingh K, et al. Prevention of deep vein thrombosis by intermittent pneumatic compression of calf. Br Med J. 1972;1:131–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Roberts VC, Sabri S, Beeley AH, et al. The effect of intermittently applied external pressure on the haemodynamics of the lower limb in man. Br J Surg. 1972;59:223–226. [DOI] [PubMed] [Google Scholar]
- 10.Nicolaides AN, Fernandes é Fernandes J, Pollock AV. Intermittent sequential pneumatic compression of the legs in the prevention of venous stasis and postoperative deep venous thrombosis. Surgery. 1980;87:69–76. [PubMed] [Google Scholar]
- 11.Keith SL, McLaughlin DJ, Anderson FA Jr, et al. Do graduated compression stockings and pneumatic boots have an additive effect on the peak velocity of venous blood flow? Arch Surg. 1992;127:727–730. [DOI] [PubMed] [Google Scholar]
- 12.Flam E, Berry S, Coyle A, et al. Blood-flow augmentation of intermittent pneumatic compression systems used for prevention of deep vein thrombosis prior to surgery. Am J Surg. 1996;171:312–315. [DOI] [PubMed] [Google Scholar]
- 13.Ricci MA, Fisk P, Knight S, et al. Hemodynamic evaluation of foot venous compression devices. J Vasc Surg. 1997;26:803–808. [DOI] [PubMed] [Google Scholar]
- 14.Westrich GH, Specht LM, Sharrock NE, et al. Venous haemodynamics after total knee arthroplasty: evaluation of active dorsal to plantar flexion and several mechanical compression devices. J Bone Joint Surg Br. 1998;80:1057–1066. [DOI] [PubMed] [Google Scholar]
- 15.Malone MD, Cisek PL, Comerota AJ Jr, et al. High-pressure, rapid-inflation pneumatic compression improves venous hemodynamics in healthy volunteers and patients who are post-thrombotic. J Vasc Surg. 1999;29:593–599. [DOI] [PubMed] [Google Scholar]
- 16.Delis KT, Slimani G, Hafez HM, et al. Enhancing venous outflow in the lower limb with intermittent pneumatic compression: a comparative haemodynamic analysis on the effect of foot vs. calf vs. foot and calf compression. Eur J Vasc Endovasc Surg. 2000;19:250–260. [DOI] [PubMed] [Google Scholar]
- 17.Whitelaw GP, Oladipo OJ, Shah BP, et al. Evaluation of intermittent pneumatic compression devices. Orthopedics. 2001;24:257–261. [DOI] [PubMed] [Google Scholar]
- 18.Andrews B, Sommerville K, Austin S, et al. Effect of foot compression on the velocity and volume of blood flow in the deep veins. Br J Surg. 1993;80:198–200. [DOI] [PubMed] [Google Scholar]
- 19.Johnson BF, Manzo R, Bergelin R, et al. Flow characteristics in the deep veins of the leg during quiet respiration and with compression of the plantar veins. J Vasc Invest. 1997;3:80–86. [Google Scholar]
- 20.Burton AC. Physiology and Biophysics of the Circulation: An Introductory Text. Chicago: Year Book, 1965. [Google Scholar]
- 21.Mayberry JC, Moneta GL, de Frang RD, et al. The influence of elastic stockings on deep venous hemodynamics. J Vasc Surg. 1991;13:91–99. [DOI] [PubMed] [Google Scholar]
- 22.Buhs CL, Bendick PJ, Glover JL. The effect of graded compression elastic stockings on the lower leg venous system during daily activity. J Vasc Surg. 1999;30:830–834. [DOI] [PubMed] [Google Scholar]
- 23.Fronek A, Criqui MH, Denenberg J, et al. Common femoral vein dimensions and hemodynamics including Valsalva response as a function of sex, age, and ethnicity in a population study. J Vasc Surg. 2001;33:1050–1056. [DOI] [PubMed] [Google Scholar]
- 24.Lewis P, Psaila JV, Davies WT, et al. Measurement of volume flow in the human common femoral artery using a duplex ultrasound system. Ultrasound Med Biol. 1986;12:777–784. [DOI] [PubMed] [Google Scholar]
- 25.Abu-Yousef MM, Mufid M, Woods KT, et al. Normal lower limb venous Doppler flow phasicity: is it cardiac or respiratory? AJR Am J Roentgenol. 1997;169:1721–1725. [DOI] [PubMed] [Google Scholar]
- 26.Vanek VW. Meta-analysis of effectiveness of intermittent pneumatic compression devices with a comparison of thigh-high to knee-high sleeves. Am Surg. 1998;64:1050–1058. [PubMed] [Google Scholar]
- 27.Gardner AMN, Fox RH. The venous footpump: influence on tissue perfusion and prevention of venous thrombosis. Ann Rheum Dis. 1992;51:1173–1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Christopoulos DG, Nicolaides AN, Szendro G, et al. Air-plethysmography and the effect of elastic compression on venous hemodynamics of the leg. J Vasc Surg. 1987;5:148–159. [DOI] [PubMed] [Google Scholar]
- 29.Warwick D, Harrison J, Glew D, et al. Comparison of the use of a foot pump with the use of low-molecular-weight heparin for the prevention of deep-vein thrombosis after total hip replacement: a prospective, randomized trial. J Bone Joint Surg Am. 1998;80:1158–1166. [DOI] [PubMed] [Google Scholar]
- 30.Anglen JO, Goss K, Edwards J, et al. Foot pump prophylaxis for deep venous thrombosis: the rate of effective usage in trauma patients. Am J Orthop. 1998;27:580–582. [PubMed] [Google Scholar]
- 31.Cornwell EE III, Chang D, Velmahos G, et al. Compliance with sequential compression device prophylaxis in at-risk trauma patients: a prospective analysis. Am Surg. 2002;68:470–473. [PubMed] [Google Scholar]
- 32.Fleming P, Fitzgerald P, Devitt A, et al. The effect of the position of the limb on venous impulse foot pumps. J Bone Joint Surg Br. 2000;82:433–434. [DOI] [PubMed] [Google Scholar]
- 33.Killewich LA, Sandager GP, Nguyen AH, et al. Venous hemodynamics during impulse foot pumping. J Vasc Surg. 1995;22:598–605. [DOI] [PubMed] [Google Scholar]
- 34.Warwick D, Martin AG, Glew D, et al. Measurement of femoral vein blood flow during total hip replacement: duplex ultrasound imaging with and without the use of a foot pump. J Bone Joint Surg Br. 1994;76:918–921. [PubMed] [Google Scholar]
- 35.Spain DA, Bergamini TM, Hoffmann JF, et al. Comparison of sequential compression devices and foot pumps for prophylaxis of deep venous thrombosis in high-risk trauma patients. Am Surg. 1998;64:522–525. [PubMed] [Google Scholar]
- 36.Santori FS, Vitullo A, Stopponi M, et al. Prophylaxis against deep-vein thrombosis in total hip replacement: comparison of heparin and foot impulse pump. J Bone Joint Surg Br. 1994;76:579–583. [PubMed] [Google Scholar]
- 37.Stannard JP, Harris RM, Bucknell AL, et al. Prophylaxis of deep venous thrombosis after total hip arthroplasty by using intermittent compression of the plantar venous plexus. Am J Orthop. 1996;25:127–134. [PubMed] [Google Scholar]
- 38.Blanchard J, Meuwly JY, Leyvraz PF, et al. Prevention of deep-vein thrombosis after total knee replacement: randomised comparison between a low-molecular-weight heparin (nadroparin) and mechanical prophylaxis with a foot-pump system. J Bone Joint Surg Br. 1999;81:654–659. [DOI] [PubMed] [Google Scholar]
- 39.Fordyce MJ, Ling RS. A venous foot pump reduces thrombosis after total hip replacement. J Bone Joint Surg Br. 1992;74:45–49. [DOI] [PubMed] [Google Scholar]
- 40.Asano H, Matsubara M, Suzuki K, et al. Prevention of pulmonary embolism by a foot sole pump. J Bone Joint Surg Br. 2001;83:1130–1132. [DOI] [PubMed] [Google Scholar]
- 41.Kamm RD. Bioengineering studies of periodic external compression as prophylaxis against deep vein thrombosis: I. Numerical studies. J Biomech Eng. 1982;104:87–95. [DOI] [PubMed] [Google Scholar]
- 42.Olson DA, Kamm RD, Shapiro AH. Bioengineering studies of periodic external compression as prophylaxis against deep vein thrombosis: II. Experimental studies on a stimulated leg. J Biomech Eng. 1982;104:96–104. [DOI] [PubMed] [Google Scholar]
- 43.Kamm RD, Butcher R, Froelich J, et al. Optimisation of indices of external pneumatic compression for prophylaxis against deep vein thrombosis: radionuclide gated imaging studies. Cardiovasc Res. 1986;20:588–596. [DOI] [PubMed] [Google Scholar]
- 44.Salzman EW, McManama GP, Shapiro AH, et al. Effect of optimization of hemodynamics on fibrinolytic activity and antithrombotic efficacy of external pneumatic calf compression. Ann Surg. 1987;206:636–641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Proctor MC, Greenfield LJ, Wakefield TW, et al. A clinical comparison of pneumatic compression devices: the basis for selection. J Vasc Surg. 2001;34:459–464. [DOI] [PubMed] [Google Scholar]
- 46.Kamm RD, Shapiro AH. Hemodynamics of external pneumatic compression. In: Madden JL, Hume M, eds. Venous Thromboembolism: Prevention and Treatment. New York: Appleton-Century-Crofts, 1976:125–129. [Google Scholar]
- 47.Lee BY, Trainor FS, Kavner D, et al. Noninvasive prevention of thrombosis of deep veins of the thigh using intermittent pneumatic compression. Surg Gynecol Obstet. 1976;142:705–714. [PubMed] [Google Scholar]
- 48.Clarke-Pearson DL, Synan IS, Hinshaw WM, et al. Prevention of postoperative venous thromboembolism by external pneumatic calf compression in patients with gynecologic malignancy. Obstet Gynecol. 1984;63:92–98. [PubMed] [Google Scholar]
- 49.Hartman JT, Yost RP, Robertson WW Jr, et al. Evaluation of thigh length sequential leg compression in the prevention of deep venous thrombosis. Thromb Haemost. 1981;46:400. [Google Scholar]
- 50.Bailey JP, Kruger MP, Solano FX, et al. Prospective randomized trial of sequential compression devices vs low-dose warfarin for deep venous thrombosis prophylaxis in total hip arthroplasty. J Arthroplasty 1991;6(suppl):29–35. [DOI] [PubMed] [Google Scholar]
- 51.Pidala MJ, Donovan DL, Kepley RF. A prospective study on intermittent pneumatic compression in the prevention of deep vein thrombosis in patients undergoing total hip or total knee replacement. Surg Gynecol Obstet. 1992;175:47–51. [PubMed] [Google Scholar]
- 52.Kamran SI, Downey D, Ruff RL. Pneumatic sequential compression reduces the risk of deep vein thrombosis in stroke patients. Neurology. 1998;50:1683–1688. [DOI] [PubMed] [Google Scholar]
- 53.Dai G, Gertler JP, Kamm RD. The effects of external compression on venous blood flow and tissue deformation in the lower leg. J Biomech Eng. 1999;121:557–564. [DOI] [PubMed] [Google Scholar]
- 54.Prandoni P, Polistena P, Bernardi E, et al. Upper-extremity deep vein thrombosis: risk factors, diagnosis, and complications. Arch Intern Med. 1997;157:57–62. [PubMed] [Google Scholar]
- 55.Knight MT, Dawson R. Effect of intermittent compression of the arms on deep venous thrombosis in the legs. Lancet 1976;2:1265–1268. [DOI] [PubMed] [Google Scholar]
- 56.Berlin E, Gjores JE, Ivarsson C, et al. Postmastectomy lymphoedema: treatment and a five-year follow-up study. Int Angiol. 1999;18:294–298. [PubMed] [Google Scholar]
- 57.Jeffery PC, Nicolaides AN. Graduated compression stockings in the prevention of postoperative deep vein thrombosis. Br J Surg. 1990;77:380–383. [DOI] [PubMed] [Google Scholar]
- 58.Wells PS, Lensing AW, Hirsh J. Graduated compression stockings in the prevention of postoperative venous thromboembolism: a meta-analysis. Arch Intern Med. 1994;154:67–72. [PubMed] [Google Scholar]
- 59.Agu O, Hamilton G, Baker D. Graduated compression stockings in the prevention of venous thromboembolism. Br J Surg. 1999;86:992–1004. [DOI] [PubMed] [Google Scholar]
- 60.Amarigiri SV, Lees TA. Elastic compression stockings for prevention of deep vein thrombosis. Cochrane Database Syst Rev. 2000;CD001484. [DOI] [PubMed]
- 61.Hui AC, Heras-Palou C, Dunn I, et al. Graded compression stockings for prevention of deep-vein thrombosis after hip and knee replacement. J Bone Joint Surg Br. 1996;78:550–554. [PubMed] [Google Scholar]
- 62.Levine MN, Gent M, Hirsh J, et al. Ardeparin (low-molecular-weight heparin) vs graduated compression stockings for the prevention of venous thromboembolism: a randomized trial in patients undergoing knee surgery. Arch Intern Med. 1996;156:851–856. [PubMed] [Google Scholar]
- 63.Meyerovitz BR, Nelson R. Measurement of the velocity of blood in lower limb veins with and without compression. Surgery. 1964;56:481–486. [PubMed] [Google Scholar]
- 64.Makin GS, Mayes FB, Holroyd AM. Studies on the effect of ‘Tubigrip’ on flow in the deep veins of the calf. Br J Surg. 1969;56:369–372. [DOI] [PubMed] [Google Scholar]
- 65.Lawrence D, Kakkar VV. Graduated, static, external compression of the lower limb: a physiological assessment. Br J Surg. 1980;67:119–121. [DOI] [PubMed] [Google Scholar]
- 66.Sigel B, Edelstein AL, Felix WR Jr, et al. Compression of the deep venous system of the lower leg during inactive recumbency. Arch Surg. 1973;106:38–43. [DOI] [PubMed] [Google Scholar]
- 67.Sigel B, Edelstein AL, Savitch L, et al. Type of compression for reducing venous stasis: a study of lower extremities during inactive recumbency. Arch Surg. 1975;110:171–175. [DOI] [PubMed] [Google Scholar]
- 68.Stanton JR, Freis ED, Wilkins RW. The acceleration of linear flow in the deep veins of the lower extremity of man by local compression. J Clin Invest. 1949;28:553–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Macklon NS, Greer IA. Technical note: compression stockings and posture: a comparative study of their effects on the proximal deep veins of the leg at rest. Br J Radiol. 1995;68:515–518. [DOI] [PubMed] [Google Scholar]
- 70.Coleridge-Smith PD, Hasty JH, Scurr JH. Deep vein thrombosis: effect of graduated compression stockings on distension of the deep veins of the calf. Br J Surg. 1991;78:724–726. [DOI] [PubMed] [Google Scholar]
- 71.Norgren L. Elastic compression stockings: an evaluation with foot volumetry, strain-gauge plethysmography and photoplethysmography. Acta Chir Scand. 1988;154:505–507. [PubMed] [Google Scholar]
- 72.Ibegbuna V, Delis K, Nicolaides AN. Effect of lightweight compression stockings on venous haemodynamics. Int Angiol. 1997;16:185–188. [PubMed] [Google Scholar]
- 73.Wilson YG, Allen PE, Skidmore R, et al. Influence of compression stockings on lower-limb venous haemodynamics during laparoscopic cholecystectomy. Br J Surg. 1994;81:841–844. [DOI] [PubMed] [Google Scholar]
- 74.Comerota AJ, Stewart GJ, Alburger PD, et al. Operative venodilation: a previously unsuspected factor in the cause of postoperative deep vein thrombosis. Surgery. 1989;106:301–308. [PubMed] [Google Scholar]
- 75.Benko T, Cooke EA, McNally MA, et al. Graduated compression stockings: knee length or thigh length. Clin Orthop. 2001;383:197–203. [PubMed] [Google Scholar]
- 76.Byrne B. Deep vein thrombosis prophylaxis: the effectiveness and implications of using below-knee or thigh-length graduated compression stockings. J Vasc Nurs. 2002;20:53–59. [DOI] [PubMed] [Google Scholar]
- 77.Hameed MF, Browse DJ, Immelman EJ, et al. Should knee-length replace thigh-length graduated compression stockings in the prevention of deep-vein thrombosis? S Afr J Surg. 2002;40:15–16. [PubMed] [Google Scholar]
- 78.Wildin CJ, Hui AC, Esler CN, et al. In vivo pressure profiles of thigh-length graduated compression stockings. Br J Surg. 1998;85:1228–1231. [DOI] [PubMed]
- 79.Best AJ, Williams S, Crozier A, et al. Graded compression stockings in elective orthopaedic surgery: an assessment of the in vivo performance of commercially available stockings in patients having hip and knee arthroplasty. J Bone Joint Surg Br. 2000;82:116–118. [DOI] [PubMed] [Google Scholar]
- 80.Merrett ND, Hanel KC. Ischaemic complications of graduated compression stockings in the treatment of deep venous thrombosis. Postgrad Med J. 1993;69:232–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Scurr JH, Coleridge-Smith PD, Hasty JH. Regimen for improved effectiveness of intermittent pneumatic compression in deep venous thrombosis prophylaxis. Surgery. 1987;102:816–820. [PubMed] [Google Scholar]
- 82.Warwick DJ, Pandit H, Shewale S, et al. Venous impulse foot pumps: should graduated compression stockings be used? J Arthroplasty. 2002;17:446–448. [DOI] [PubMed] [Google Scholar]
- 83.Shelter legs [editorial]. Lancet. 1940;2:722. [Google Scholar]
- 84.Scurr JH, Machin SJ, Bailey-King S, et al. Frequency and prevention of symptomless deep-vein thrombosis in long-haul flights: a randomised trial. Lancet. 2001;357:1485–1489. [DOI] [PubMed] [Google Scholar]
- 85.Mühe E. Intermittent sequential high-pressure compression of the leg: a new method of preventing deep vein thrombosis. Am J Surg. 1984;147:781–785. [DOI] [PubMed] [Google Scholar]
- 86.Allenby F, Boardman L, Pflug JJ, et al. Effects of external pneumatic intermittent compression on fibrinolysis in man. Lancet. 1973;2:1412–1414. [DOI] [PubMed] [Google Scholar]
- 87.O'Brien TE, Woodford M, Irving MH. The effect of intermittent compression of the calf on the fibrinolytic responses in the blood during a surgical operation. Surg Gynecol Obstet. 1979;149:380–384. [PubMed] [Google Scholar]
- 88.Tarnay TJ, Rohr PR, Davidson AG, et al. Pneumatic calf compression, fibrinolysis, and the prevention of deep venous thrombosis. Surgery. 1980;88:489–496. [PubMed] [Google Scholar]
- 89.Comerota AJ, Chouhan V, Harada RN, et al. The fibrinolytic effects of intermittent pneumatic compression: mechanism of enhanced fibrinolysis. Ann Surg. 1997;226:306–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kosir MA, Schmittinger L, Barno-Winarski L, et al. Prospective double-arm study of fibrinolysis in surgical patients. J Surg Res. 1998;74:96–101. [DOI] [PubMed] [Google Scholar]
- 91.Cahan MA, Hanna DJ, Wiley LA, et al. External pneumatic compression and fibrinolysis in abdominal surgery. J Vasc Surg. 2000;32:537–543. [DOI] [PubMed] [Google Scholar]
- 92.Macaulay W, Westrich G, Sharrock N, et al. Effect of pneumatic compression on fibrinolysis after total hip arthroplasty. Clin Orthop. 2002;399:168–176. [DOI] [PubMed] [Google Scholar]
- 93.Lachmann EA, Rook JL, Tunkel R, et al. Complications associated with intermittent pneumatic compression. Arch Phys Med Rehabil. 1992;73:482–485. [PubMed] [Google Scholar]
- 94.Verdolin MH, Toth AS, Schroeder R. Bilateral lower extremity compartment syndromes following prolonged surgery in the low lithotomy position with serial compression stockings. Anesthesiology. 2000;92:1189–1191. [DOI] [PubMed] [Google Scholar]
- 95.Cohen SA, Hurt WG. Compartment syndrome associated with lithotomy position and intermittent compression stockings. Obstet Gynecol. 2001;97:832–833. [DOI] [PubMed] [Google Scholar]
- 96.Pfeffer SD, Halliwill JR, Warner MA. Effects of lithotomy position and external compression on lower leg muscle compartment pressure. Anesthesiology. 2001;95:632–636. [DOI] [PubMed] [Google Scholar]
- 97.Pittman GR. Peroneal nerve palsy following sequential pneumatic compression. JAMA. 1989;261:2201–2202. [DOI] [PubMed] [Google Scholar]
- 98.McGrory BJ, Burke DW. Peroneal nerve palsy following intermittent sequential pneumatic compression. Orthopedics. 2000;23:1103–1105. [DOI] [PubMed] [Google Scholar]
- 99.Haddad FS, Kerry RM, McEwen JA, et al. Unanticipated variations between expected and delivered pneumatic compression therapy after elective hip surgery: a possible source of variation in reported patient outcomes. J Arthroplasty. 2001;16:37–46. [DOI] [PubMed] [Google Scholar]