Abstract
Objective:
To determine the efficacy of CT scan in mapping the superior and inferior epigastric vessels, relative to landmarks apparent at laparoscopy.
Summary Background Data:
Trauma to abdominal wall blood vessels occurs in 0.2% to 2% of laparoscopic procedures. Both superficial and deep abdominal wall vessels are at risk. The superficial vessels may be located by transillumination; however, the deep epigastric vessels cannot be effectively located by transillumination and, thus, other techniques should be used to minimize the risk of injury to these vessels.
Methods:
Abdominal and pelvic CT images of 100 patients were studied. The location of the superior and inferior epigastric vessels from the midline were determined at five levels, correlated with each other and with the patient age, body mass index, and history of midline laparotomy using Pearson's correlation coefficient and multivariate analysis.
Results:
CT scan was successful in mapping the epigastric vessels in 95% of patients. At the xiphoid process level, the superior epigastric vessels (SEA) were 4.41 ± 0.13 cm from the midline on the right and 4.53 ± 0.14 cm on the left. Midway between xiphoid and umbilicus, the SEA were 5.50 ± 0.16 cm on the right of the midline and 5.36 ± 0.16 cm on the left. At the umbilicus, the epigastric vessels were 5.88 ± 0.14 cm on the right and 5.55 ± 0.13 on the left of the midline. Midway between the umbilicus and symphysis pubis, the inferior epigastric (IEA) were 5.32 ± 0.12 cm on right and 5.25 ± 0.11 cm on the left. At the symphysis pubis, the IEA were 7.47 ± 0.10 cm on the right and 7.49 ± 0.09 cm away from the midline on the left side.
Conclusions:
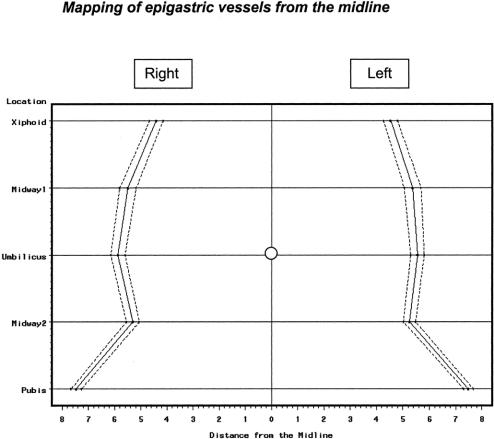
Epigastric vessels are usually located in the area between 4 and 8 cm from the midline. Staying away from this area will determine the safe zone of entry of the anterior abdominal wall.
Epigastric vessels are the most commonly injured vessels during laparoscopy. Review of 100 abdominal CT scans revealed that epigastric vessels are usually located in the area between 4 and 8 cm from the midline. Staying away from this area will determine the safe zone of entry of the anterior abdominal wall.
The widespread use of laparoscopy has led to the development of more advanced minimally invasive procedures that require placement of many trocars through the abdominal wall. Trocar injury is a potentially serious but preventable complication that occurs in 0.2% to 2% of laparoscopic surgery.1–4 Both superficial and deep epigastric vessels are at risk.5 The superficial abdominal wall vessels may be located by transillumination. However, the deep epigastric vessels cannot be effectively located by that method.6,7 Other techniques should be used to minimize injury to the deep epigastric vessels. The objective of this study is to map the deep epigastric vessels to determine a safety zone for anterior abdominal wall entry during laparoscopy.
MATERIALS AND METHODS
A total of 100 abdominal and pelvic computed tomography (CT) scans with intravenous contrast were randomly chosen at Michigan State University/Kalamazoo Center for Medical Studies. The following patients were excluded from the study: those younger than 15 years or older than 90 years, and those who had any condition that may alter the location of epigastric vessels, ie, gross skeletal deformities, large abdominal tumors, tense ascites, incisional hernia, or diathesis of recti. The location of the epigastric vessels were determined at five levels, namely, the xiphoid, midway between the xiphoid and umbilicus, the umbilicus, midway between the umbilicus and symphysis pubis, and at the level of the symphysis pubis. The distance between the epigastric vessels and midline were measured bilaterally at each level. Data consisted of 10 measurements (left/right at the above-described five levels). The locations of the superior and inferior epigastric vessels were compared with possible covariates (age, weight, height, body mass index [BMI]) with Pearson's correlation. Data are expressed as a mean ± sd followed by the 95% confidence interval.
RESULTS
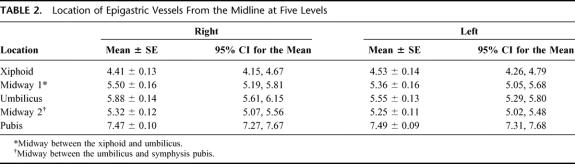
The demographic data of 100 patients considered for this study is presented in Table 1. The average age was 63.85 years, with a minimum age of 15 and maximum age of 90. There were 16 females and 84 males included in the study. The average weight was 79.03 kg and the average height was 68.02 inches. The average BMI was 26.45. Of these patients, 16% had undergone a previous midline surgery.
TABLE 1. Demographic Data
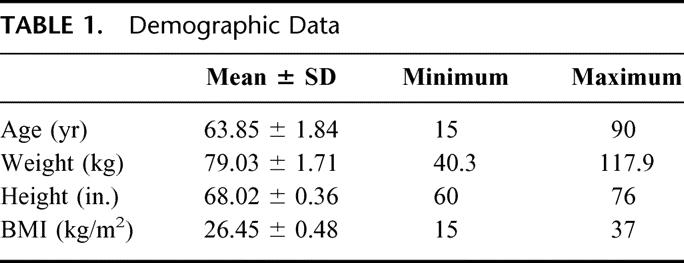
The locations of the superior and inferior epigastric vessels in relation to five different levels measured on both sides (left and right from the midline) are presented in Table 2. At the xiphoid level, the average distance of the epigastric vessels from the midline was 4.41cm on the right and 4.53 cm on the left side. At the level midway between the xiphoid and the umbilicus, the average distance of the epigastric vessel on the right was 5.50 cm and 5.36 cm on the left. At the umbilicus, the epigastric vessels on the right was 5.88 cm and 5.55 cm on the left from the midline. Midway between the umbilicus and the symphysis pubis, the right epigastric vessel was located 5.32 cm from the midline and 5.25 cm on the left. The epigastric vessels are farthest from the midline at the symphysis public level for both the right and left side. The epigastric vessels were 7.47 cm and 7.49 cm on the right side and left side, respectively, at the level of the symphysis pubis.
TABLE 2. Location of Epigastric Vessels From the Midline at Five Levels
The solid line in Figure 1 outlines these average distances of the epigastric vessels from the midline for each of the five locations. Also outlined in the graph are the upper and lower 95% confidence interval for each location (dashed line). It is safe to say that anywhere beyond that interval for each part, left and right, is a “safe zone.”
FIGURE 1. Mapping of epigastric vessels from the midline.
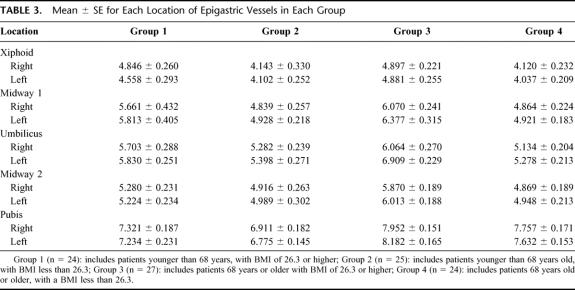
Correlation analysis between demographic variables (age, height, weight, BMI, and status of previous laparotomy) and the 10 measurements in Table 2 (left and right in five locations each) reveals that BMI and age are possible covariates, being significantly correlated with at least 9 of the 10 measurements. Considering the two covariates (BMI and age) in coming up with an estimate of area that identifies the location of superior and inferior epigastric arteries, data were categorized into four groups as follows: Group 1 includes patients younger than 68 years, with a BMI of 26.3 or higher (n = 24); Group 2 includes patients younger than 68 years, with a BMI less than 26.3 (n = 25); Group 3 includes patients 68 years of age or older, with a BMI of 26.3 or higher (n = 27); and Group 4 includes patients 68 years of age or older, with a BMI less than 26.3 (n = 24).
Table 3 shows the mean location of epigastric vessel with its corresponding standard error for the each of the five locations (left and right) under the four groups mentioned above. A Bonferroni pairwise test supports the following statements on setting safety zones to be considered for each group (taking into consideration that precise measurement will be done). Different safety zones must be considered for patients belonging to Group 2 and Group 3, when the patient is to be operated on the right side of the xiphoid area (P = 0.018) as well as on the left and right side of midway 1 area (left P = 0.023, right P = 0.042). The same is to be done for patients belonging to Group 3 and Group 4 if they are to be operated on the left side of midway 1 area (P = 0.024). If the patient is to be operated at the left side of the umbilical level and he/she belongs to Group 3, then the safety zone must be different from a person belonging to Group 1 (P = 0.030), Group 2 (P = 0.014), and Group 4 (P = 0.004). In the midway 2 area, only one safety zone can be considered for all patients. On the left side of the pubis are, safety zones for those in Groups 1 and 3 should be different (P = 0.004). For both left and right sides on this same area, different safety zones for patients in Groups 2 and 3 (left P < 0.001, right P = 0.002) and Groups 2 and 4 (left P = 0.007, right P = 0.010) must be considered.
TABLE 3. Mean ± se for Each Location of Epigastric Vessels in Each Group
The average distance of the epigastric vessels from the midline for both left and right sides is consistently higher for those with BMI more than or equal to 26.3 in all sections. Epigastric vessels of older patients with high BMI are further from the midline, on the average, as compared with the younger patients.
DISCUSSION
The complexity of advanced laparoscopic procedures necessitates placement of many large-bore trocars through the anterior abdominal wall. This can result in accidental injury to the abdominal wall vessels in 0.2% to 2.0% of cases.1–4 Undoubtedly, the most commonly injured vessel in laparoscopic procedures is the epigastric vessels.5,8
Injury to the epigastric vessels can result in different clinical presentations.5,7 During laparoscopy, bleeding may be manifested as oozing externally around the port site or dripping internally along the shaft of the cannula into the abdominal cavity. The injury may initially go unrecognized due to the temporary tamponade by both the cannula and pneumoperitoneum and present as hematoma or pseudoaneurysm later.9
Injury to inferior epigastric artery may cause some problems itself. Necrosis of the rectus muscle is possible in case of absence of sufficient blood flow via the superior epigastric artery or collaterals.10 In case of aortoiliac occlusive disease, the inferior epigastric artery can become an important part of collateral blood supply to the leg by reversal of the blood flow; its occlusion or injury can lead to worsening of leg ischemia.11,12 Occlusion or injury of the superior or inferior epigastric artery also means that harvesting the transversus rectus abdominus muscle flap becomes impossible.9
Abdominal wall bleeding can be controlled with a variety of techniques.4,7,8 This includes application of direct pressure with the operating port, full-thickness abdominal wall suture ligation or tamponade with Foley catheter balloon inserted through the trocar site. If all these maneuvers fail to control the bleeding, exploration of the wound is mandatory. This may lead to unnecessary prolongation of the laparoscopic procedure or conversion to laparotomy with loss of all the advantages of minimally invasive surgery.
A review of the literature provided little detail about strategies to avoid such injuries.13 Utilizing computer tomography, we were able to visualize the path of the epigastric vessels in 95% of our patients. This should provide more structural information than that in standard anatomy textbooks. From our data it is clear that, regardless of the abdominal level, epigastric vessels (superior or inferior) are usually located in the area between 4 and 8 cm from the midline. Staying away from this area, either medially or laterally, will determine the safety zone of entry the abdominal wall without risk of injury to the epigastric vessels. To avoid accidental injury to the epigastric vessels, these anatomic landmarks should be considered whenever the anterior abdominal wall is to be violated, not only during laparoscopic or open surgical procedures but also during image-guided biopsy and paracentesis.
ACKNOWLEDGMENTS
We would like to express our appreciation to Nanette Townsend for her endeavors in the preparation of this manuscript.
Footnotes
This paper was presented at the Michigan Chapter of the American College of Surgeons on May 9, 2002 in Shanty Creek, Michigan.
Reprints: Alan A. Saber, MD, MS, Minimally Invasive Surgery, Michigan State University, Kalamazoo Center for Medical Studies, 1000 Oakland Drive, Kalamazoo, MI 49008. E-mail saber@kcms.msu.edu.
REFERENCES
- 1.Zaki H, Penketh R, Newton J. Gynaecological laparoscopy audit: Birmingham experience. Gynecol Endocrinol. 1995;4:251–257. [Google Scholar]
- 2.Aharoni A, Condea A, Leibovitz Z, et al. A comparative study of Foley catheter and suturing to control trocar-induced abdominal wall haemorrhage. Gynecol Endocrinol. 1997;6:31–32. [Google Scholar]
- 3.Vasquez JM. Vascular complications of laparoscopic surgery. J Am Assoc Gynecol Laparosc. 1994;1:163–167. [DOI] [PubMed] [Google Scholar]
- 4.Spitzer M, Golden P, Rehwaldt L, et al. Repair of laparoscopic injury to abdominal wall arteries complicated by cutaneous necrosis. J Am Assoc Gynecol Laparosc. 1996;3:449–452. [DOI] [PubMed] [Google Scholar]
- 5.Hurd WW, Pearl ML, DeLancey JO, et al. Laparoscopic injury of abdominal wall blood vessels: a report of three cases. Obstet Gynecol. 1993;82(4 Pt 2 suppl):673–676. [PubMed] [Google Scholar]
- 6.Quint EH, Wang FL, Hurd WW. Laparoscopic transillumination for the location of anterior abdominal wall blood vessels. J Laparoendosc Surg. 1996;6:167–169. [DOI] [PubMed] [Google Scholar]
- 7.Tomacruz RS, Bristow RE, Montz FJ. Management of pelvic hemorrhage. Surg Clin North Am. 2001;81:925–948. [DOI] [PubMed] [Google Scholar]
- 8.Lin P. Complications of laparoscopy: strategies for prevention and cure. Obstet Gynecol Clin North Am. 1999;26:23–38. [DOI] [PubMed] [Google Scholar]
- 9.Verbist J. Pseudoaneurysm of the inferior epigastric artery. Acta Chir Belg. 1997;97:196–198. [PubMed] [Google Scholar]
- 10.Heppert V, Holz F, Winkler H, et al. Necrosis of the rectus abdominis muscle: complication after ilioinguinal approach. Unfallchirurg. 1995;98:98–101. [PubMed] [Google Scholar]
- 11.Krupski WC, Sumchai A, Efflney DJ, et al. The importance of abdominal wall collateral blood vessels. Arch Surg. 1984;119:854. [DOI] [PubMed] [Google Scholar]
- 12.Sistrom CL, Reiheld CT, Elliot H. Reversal of flow in the inferior epigastric arteries, Doppler ultrasonographic findings and significance. J Ultrasound Med. 1995;14:183–191. [DOI] [PubMed] [Google Scholar]
- 13.Whiteley MS. Use of a hand-held Doppler to avoid abdominal wall vessels in laparoscopic surgery. Ann R Coll Surg Engl. 1994;76:348–350. [PMC free article] [PubMed] [Google Scholar]