Abstract
Objective:
To assess evacuation priorities during terror-related mass casualty incidents (MCIs) and their implications for hospital organization/contingency planning.
Summary Background Data:
Trauma guidelines recommend evacuation of critically injured patients to Level I trauma centers. The recent MCIs in Israel offered an opportunity to study the impositions placed on a prehospital emergency medical service (EMS) regarding evacuation priorities in these circumstances.
Methods:
A retrospective analysis of medical evacuations from MCIs (29.9.2000–31.9.2002) performed by the Israeli National EMS rescue teams.
Results:
Thirty-three MCIs yielded data on 1156 casualties. Only 57% (506) of the 1123 available and mobilized ambulances were needed to provide 612 evacuations. Rescue teams arrived on scene within <5 minutes and evacuated the last urgent casualty within 15–20 minutes. The majority of non-urgent and urgent patients were transported to medical centers close to the event. Less than half of the urgent casualties were evacuated to more distant trauma centers. Independent variables predicting evacuation to a trauma center were its being the hospital closest to the event (OR 249.2, P < 0.001), evacuation within <10 minutes of the event (OR 9.3, P = 0.003), and having an urgent patient on the ambulance (OR 5.6, P < 0.001).
Conclusions:
Hospitals nearby terror-induced MCIs play a major role in trauma patient care. Thus, all hospitals should be included in contingency plans for MCIs. Further research into the implications of evacuation of the most severely injured casualties to the nearest hospital while evacuating all other casualties to various hospitals in the area is needed. The challenges posed by terror-induced MCIs require consideration of a paradigm shift in trauma care.
The majority of 1156 urgent and non-urgent casualties from 33 mass casualty incidents in Israel were evacuated to the nearest hospital rather than to a trauma center. The causes of this phenomenon are analyzed. Implications of these findings for hospital contingency planning and applicability of trauma guidelines under these circumstances are discussed.
Civilian mass casualty events are becoming an increasingly important security issue all over the world1–3 since terrorism is not an endemic phenomenon, but an epidemic.
Prehospital Trauma Life Support (PHTLS) guidelines state that critically injured, but salvageable patients, should be promptly evacuated and transferred, preferably to a Level I trauma center, immediately following primary triage and resuscitation.4 This approach has been practiced by the rescue teams of the Magen David Adom Israeli National Emergency Medical Services (MDA) since Advanced Trauma Life Support (ATLS) courses were initiated in Israel in 1990.
Thus, PHTLS and ATLS guidelines have been strictly followed in Israel, resulting in admission of most major civilian trauma victims to trauma centers. However, the recent onslaught of terror related mass casualty incidents in this country has forced a change in practice in such circumstances, resulting in a paradigm shift. Both PHTLS and ATLS deal primarily with the treatment of a single patient. In the situation of a mass casualty incorporating multiple and severe civilian injuries, evacuating all critically injured patients to a Level I trauma center may not be applicable, as treatment of a patient population must take priority over treatment of individuals.5 In a mass casualty event, the impositions placed upon prehospital rescue services in regards to evacuation priorities become the most dominant consideration. This phenomenon has been observed during the recent events in Israel.
We undertook to perform a retrospective analysis of medical evacuations carried out by the MDA rescue teams from the scenes of terror related mass casualty incidents to examine whether PHTLS evacuation guidelines remain valid in these circumstances. Our study offers a unique insight into real-life evacuation priorities in such real-time events. This experience has led us to realize that a paradigm change may be necessary in contingency planning for such circumstances, with a shift from the trauma center concept to medical centers in general.
METHODS
A retrospective analysis was performed of emergency medical evacuations from terror related mass casualty incidents by the rescue teams of the Israeli MDA organization during the 2-year period from September 29th 2000 to September 31st 2002. Mass casualty incidents were defined as terrorist attacks of a large enough scale to recruit most of the rescue teams and security force resources within a defined region, regardless of the actual number of casualties. Some of these incidents were ongoing during the actual mobilization of the rescue teams and throughout the process of medical evacuations; therefore the potential for casualties rather than the actual number of casualties was often the deciding factor.
The Israeli MDA emergency medical service has the advantage of being a nationwide network with a central command allowing for centralized on-scene organization and later data collection with post hoc analysis. All ambulance mobilization and movement is coordinated by the regional dispatch center. The decision-making process regarding the choice of hospital at the time of evacuation is as follows: the most senior medical person intended to accompany the individual ambulance reports the patients’ injuries to the senior coordinator on location and together they choose a destination. Upon leaving the location of the event, the ambulance driver notifies the dispatch center of the intended destination. The dispatcher may suggest that the ambulance be directed elsewhere based on their knowledge of previous evacuations to this location (e.g.; inundation). The senior medical person in the ambulance is, however, entitled to insist on continuing to the specified location. This person is also entitled to change the destination of the ambulance if reassessment of the patients’ injuries/condition justifies such a decision to their estimation. When a patient is in extremis, evacuation will be to the hospital most proximal to the event.
Each mass casualty incident incurs a series of routine debriefings. Data were obtained from real time recordings of dispatch and vehicle personnel and from the protocols of the MDA debriefings that immediately followed each and every incident.
For the purposes of this study, the locations of the mass casualty incidents were divided into 3 types of regions according to hospital accessibility. An event was categorized as occurring within a large urban region if it took place within the metropolitan area of 1 of the 3 largest cities in Israel. In these cities evacuation options included a trauma center as well as other medical centers. Events that occurred within smaller cities with a relatively large population but with only medical centers in close proximity were categorized as urban events. Events were categorized as occurring within a rural region if they transpired either in a sparsely populated area or in a town with a small population, provided the evacuation time from this location to both trauma centers and all other medical centers was greater than 20 minutes.
Mass casualty incidents were included in the study only if the MDA debriefings contained sufficiently detailed information and the location of the incident fell clearly within one of the 3 region categories.
During evacuations patients are categorized by MDA personnel as urgent or non urgent. An urgent patient is always considered and treated upon arrival to hospital as though they were critically injured. However, only two thirds of urgent patients are found to be critically injured while one third is found to be moderately injured. This initial overtriage minimizes undertriaging of potentially life threatening injuries.5
We looked at the evacuation pattern of the entire patient population and of patients defined as urgent in relation to the types of hospitals and various other factors affecting decision-making, such as: times to arrival of ambulances and times to evacuation, the number of available ambulances, the distance to the various hospitals, and the breakdown of the severity of injuries according to the admitting hospital.
To achieve a reproducible estimate of the relative distances of each hospital from each incident site, an assessment of the following considerations was made: the actual distance in kilometers by vehicle, the topography (hilly or flat, straight or tortuous), the quality of the roads, and the density of the traffic at the particular time of the event. Each factor was given a score of either 0 (no impact) or 1 (negative impact) and hospitals participating in the incident by admitting injured patients were then graded accordingly. The hospital or hospitals receiving the lowest score (either 0 or 1) were defined as close. The hospitals that received the highest scores (3–4) were defined as distant. Those receiving an intermediate score (2) were defined as intermediate.
Statistical Analysis
Data was collected and analyzed using Access 2002 (© Microsoft Co. Redmont WA). A database was designed for the purposes of this study, allowing linkage of appropriate details. Statistical analysis was performed using SPSS 10 (SPSS Inc. Chicago, Illinois). Descriptive statistics used included counts, means, ranges, SDs, and proportions. Logistic regression was used to seek for the independent factors predicting evacuation to a Level I trauma center. Univariate analysis was used initially, followed by multivariate analysis (stepwise backward) to adjust for covariates and possible interactions. The time from the beginning of the event to evacuation was examined as both a continuous and a categorical variable (stratified into 5-minute periods).
RESULTS
From September 29th 2000 to September 31st 2002, 1116 terror related incidents occurred in Israel. Of these events, 45 were mass casualty incidents in the sense that most of the rescue services and security force resources in a certain region were mobilized. The MDA records of all of these incidents were screened for the purpose of this study. Seven incidents were excluded from the study because of poor quality or inadequate data. Five events occurred in regions that did not clearly fall within our definition of the region categories. Thus the full data from 33 mass casualty incidents form the basis of this study.
Twelve of these incidents occurred within a large urban region. Of these, 4 were explosions in a closed space, 5 explosion in an open space, and 3 automatic weapon shootings. Twelve incidents occurred in urban regions: 4 explosions in a closed space, 4 explosions in an open space, 3 automatic weapon shootings, and 1 combined explosion with automatic weapon shooting. Only 9 events occurred in rural regions: 4 explosions in a closed space, 1 explosion in an open space, 3 automatic weapon shootings, and 1 combined incident of explosion and automatic weapon shooting.
In the 33 incidents, 230 died and a total of 1156 injured were evacuated to hospitals, yielding a dead to wounded ratio of 1:5 corresponding to the ratio typical of military combat in conventional wars.5
The upper portion of Table 1 details the total and per incident number of all and urgent casualties in the various regions. Urgent patients comprised 20.4% of the total. The lower portion of Table 1 depicts the choice of hospital made by the rescue teams for both the urgent and the non-urgent patients: trauma center or medical centers. In all 3 regions the overwhelming majority of patients were evacuated to medical centers: 69% in the large urban regions, 95% in the urban regions, and 77% in the rural regions. In the urban and rural regions the trauma centers received only small numbers of urgent patients: 9% and 34% respectively. Even in the large urban regions slightly less than half (48%) of the urgent casualties were evacuated to a trauma center despite much easier accessibility.
TABLE 1. Casualties by Type of Region and Choice of Hospital: Trauma Centers Versus Medical Centers
The time to arrival of rescue teams on scene, as judged by ambulance arrival times, was shorter in large urban and urban than in rural incidents (4 ± 2; 3 ± 2 and 8 ± 3 minutes, respectively). In these regions less time also elapsed from the arrival of the first ambulance to the first evacuation (large urban 5 ± 2, urban 6 ± 3, and rural 13 ± 4 minutes), the last urgent evacuation (large urban 16 ± 5, urban 17 ± 8, and rural 44 ± 26 minutes), and the last evacuation altogether (large urban 37 ± 17, urban 39 ± 24, and rural 90 ± 60 minutes).
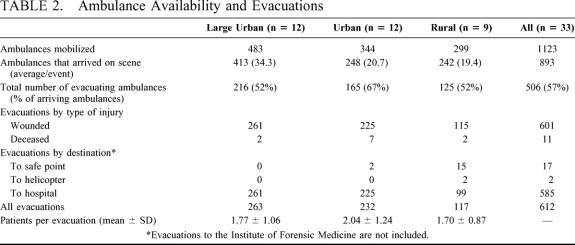
A total of 1123 ambulances were mobilized for the 33 mass-casualty incidents (Table 2). For organizational reasons (following initial traffic and on-scene reports to the dispatch center), only 893 ambulances (79%) were allowed to reach the location of the incidents, and only 506 ambulances (57%) actually provided 612 evacuations. Ninety-three ambulances performed more than 1 round of evacuations. Nineteen evacuations were performed from safe points to protect medical assets from a second hit.5 In these evacuations armored ambulances were used to transport the casualties under fire directly from the scene of the incident to a nonarmored ambulance or a helicopter waiting at a safe point (Table 2). Thus more than 1 vehicle was used to transport these patients, yielding an average of 0.93 evacuations per ambulance in the rural region, compared with 1.22 and 1.41 evacuations per ambulance in the large urban and urban regions (Table 2).
TABLE 2. Ambulance Availability and Evacuations
Table 3 demonstrates the choice of hospital made by the rescue teams by the distance of the hospital from the location of the incident in each region. In the urban and rural regions the overwhelming majority of patients in general, and urgent patients in particular, were transported to the nearest hospital. Even in the large urban regions, where trauma centers are more accessible, close to half of all patients and of the urgent patients were transported to the nearest and intermediately close medical centers. Trauma centers, often being the most remotely located, received only slightly more than half of the urgent patients. Due to the very early arrival of MDA teams and the rapidity of evacuation, a few urgent patients were dead upon arrival to hospital.
TABLE 3. Choice of Hospital by Distance From the Incident (Primary Triage Only)
Secondary transfer within 2 hours of injury occurred in 4 patients in the large urban regions, in 20 patients in urban regions, and in 3 patients in rural regions. For the majority of these patients, insufficient data exists regarding the urgency of their initial evacuation and the type and severity of their injuries. Twenty-four of these 27 patients were transferred from a medical center to a trauma center. We have no valid data regarding the extent and timing of the secondary wave of patient transfer occurring later.
The independent variables predicting evacuation to a Level I trauma center are presented in Table 4. The probability of an ambulance heading towards a Level I trauma center was 9.3 times higher if the evacuation occurred within 10 minutes of the beginning of the event (P = 0.003) and 5.6 times higher if there was an urgent patient on board (P < 0.001). If the trauma center happened to be the hospital closest to the event, the probability of a patient being evacuated to this location was extremely high (OR 249.2, P < 0.001), in events where the Level I trauma was only at an intermediate distance the probability of the patient being evacuated to the Level I trauma center dropped, and even more so when the trauma center was the most distant (OR 3.5, P = 0.043) (Table 4). The probability that an ambulance would head towards a trauma center also increased by almost 1.7 per each urgent patient already evacuated to this location.
TABLE 4. Factors Predicting the Choice of Hospital
DISCUSSION
Most interesting and important in our study is the fact that in the setting of terror related mass casualty events, the majority of all patients and the majority of urgent patients were evacuated to the nearest hospital and not necessarily to trauma centers. This was obviously most common in areas lacking a trauma center, but clearly occurred even in large urban regions, where the hospitals that happened to be in greater proximity to the event, rather than the trauma center, received a considerable number of both urgent and non urgent patients.
Compared with everyday civilian trauma, terror-related mass casualty events involve a relatively large proportion of severely injured casualties.6 In our experience there was a high incidence of multiple penetrating injuries (unpublished data) and a large number of complex multiorgan and multisystem injuries.6 The mechanisms of injury in this scenario are often multiple: blast, penetrating shrapnel, burn injury, and gunshot wounds. Unusual and often lethal shrapnel (screws, nails, bolts, metal scraps, and ball bearings) and dangerous chemical substances have been added to bombs. Additional considerations include the possibility of infective agents such as hepatitis, HIV, and other biological hazards being transmitted to the victim by penetration of foreign tissue (bone splinters and blood). The type of injuries sustained in these circumstances may easily lead to under-triage, as these aforementioned vectors may cause unpredictable and extensive tissue damage, often initially insidious, and may therefore lead to a sudden and unexpected deterioration in the condition of the patient.
The recent, 2-year Israeli experience with terror-related attacks has challenged our traditional trauma care system, raising the question of a paradigm shift. Prior to outlining the lessons gleaned from these civilian mass casualty incidences, it is important to briefly survey some of our previous concepts of military and civilian trauma care and management.
The evacuation hospital is one of the most important concepts that has emerged from the accumulated experience of the Israeli Defense Force medical corps during combat. The principle missions of this front-line medical facility are: performing primary triage and resuscitation, prompt life or limb saving surgery (only when absolutely necessary), and later evacuation to appropriate civilian medical centers. The evacuation hospital concept was successfully tested and practiced in the 1973 war in the Sinai Peninsula and in the 1982 conflict in Lebanon. Ultimately it was also suggested that civilian mass casualty events in this country should follow this concept.7
The initial civilian implementation of this strategy occurred in the early 1990s when Israel experienced a wave of terrorist bombings against public transportation buses. For the first time, the EMTs faced large-scale incidents within a civilian population, suffering unique and previously unknown, immediately life-threatening injuries.8–10 The dilemma faced was evacuating many urgent casualties to a more distant trauma center versus transporting them to a closer medical center for lifesaving resuscitation.
The current wave of terrorist attacks against civilians began in September 2000 and involved either suicide bombers or automatic weapon fire in crowded public locations. These incidents were much more frequent and on a larger scale than previously, demanding an immediate and full scale response of both rescue and security forces to isolate the danger zone, search for secondary bombs or gunmen, contain the ensuing public panic, and rapidly and efficiently evacuate the many severe casualties. At the same time, the high incidence of events also inflicted a significant burden of trauma patient admissions upon the various hospitals across the country, inundating limited civilian hospital facilities that are not normally geared towards admission of such large numbers of trauma patients within a short period of time.
In their contingency plan for mass casualties and war situations in Israel, Shemer et al assumed, based on the model of the evacuation hospital, that the most proximal hospital will receive the brunt of the casualties.11 This assumption has not been tested or proven in real-life civilian mass casualty incidents prior to September 2000. Our data demonstrate that on site, only minimal medical intervention with rapid evacuation to the nearest medical facility occurred. In this scenario, the nearest hospital therefore functioned as the civilian equivalent of the military evacuation hospital. Indeed the scoop and run principle was practiced in our current experience, not only for the individual patient, but also for the entire mass of casualties (en masse scoop and run).
The change of paradigm involves both on-scene management of mass casualty events, as well as hospital organization and contingency planning.
On-scene organization in civilian mass casualty events traditionally included 4 stages: a chaos phase followed by reorganization, site cleaning, and a late phase.3 Our recent experiences suggest that the sequence of on-scene management of mass casualty terrorist attacks against a civilian population should in fact include: (1) rapid primary on-scene triage within seconds to minutes of arrival by experienced emergency medical teams with only minimal medical intervention; (2) immediate evacuation of critically injured or premorbid casualties to the nearest hospital for primary resuscitation and stabilization (evacuation hospital concept); (3) and evacuation of all other casualties to all other medical centers to avoid over extending the capacity of any one hospital. Our analysis of on-scene events shows that during the evacuation process, time constraints allow for no organization or crowd control attempts. Proper execution of these measures, which require a high level of coordination and communication,12 may result in survival of casualties that may have been considered nonsalvageable in a military scenario. In the civilian scenario these casualties may stand a good chance of survival if rapid evacuation is provided to a nearby, well-prepared, and well-equipped hospital.
As a result of the evacuation priorities determined by the on-scene rescue teams, all hospitals should be prepared to act as the evacuation hospital in the case that a mass casualty event occurs in their vicinity. The evacuation of critically injured patients to the nearest hospital is clearly predicated on that facility possessing the means to deal with such a situation. This must be ensured by central governance that carries the responsibility of equipping hospitals and performing periodic drills for mass casualty events, as is the case in Israel. We recommend that all hospitals achieve an appropriate degree of surgical capability, be well disciplined in trauma care, and that all personnel (medical, nursing, and ancillary staff) participate in periodic training programs and hospital drills.
Based on simulation models, expansion of diagnostic imaging modalities and resuscitation beds should be given priority.13 Current contingency planning does not encompass all hospitals, and recommends periodic training for key disaster response personnel only.14
Even in the best of circumstances, mass casualty incidents carry the potential of overwhelming the capabilities of even the most organized of medical systems. A comprehensive and immediate demand is made upon resources, rendering even the initial in-hospital phase of minimal acceptable care extremely difficult to maintain.15 This situation may be exacerbated by the currently accepted practice of overtriage. Thus, coordination between hospitals for a bi-directional secondary wave of interhospital patient transfer may be required to alleviate disruption of routine work and provide relief for inundated trauma centers, as well as other medical centers.
Until further data is available regarding the correlation between the on-scene injury assessment and the in-hospital findings, and the implications of the current practice on patient outcome, our experience with terror induced civilian mass casualty events stresses the major role for each and every hospital in such an event. The constraints placed upon the rescue teams in such events necessitate evacuation of the most severely injured casualties to the nearest hospital, which should be appropriately equipped and staffed by personnel qualified to treat such injuries. All other casualties will need to be directed to all other medical facilities to avoid over-extending the capacity of any one hospital. Terror related mass casualty events pose a new challenge for trauma care and require consideration of a paradigm shift.
Footnotes
Reprints: Sharon Einav, MD, Department of Anesthesiology and Critical Care Medicine, Hadassah University Medical Center, Ein Kerem Campus, POB 12000, Jerusalem 91120, Israel. E-mail: bromi@md2.huji.ac.il.
REFERENCES
- 1.Louis J. Freeh, Director Federal Bureau of Investigation. Statement for the Record on the Threat of Terrorism to the United States before the United States Senate Committees on Appropriations, Armed Services, and Select Committee on Intelligence, May 10, 2001.
- 2.Slater MS, Trunkey DD. Terrorism in America. An evolving threat. Arch Surg. 1997;132:1059–1066. [DOI] [PubMed] [Google Scholar]
- 3.Stein M, Hirshberg A. Medical consequences of terrorism. The conventional weapon threat. Surg Clin North Am. 1999;79:1537–1552. [DOI] [PubMed] [Google Scholar]
- 4.The National Association of Emergency Medical Technicians and the American College of Surgeons Committee on Trauma. Introduction, In: PHTLS: Basic and Advanced Prehospital Trauma Life Support, 5th ed, McSwain N, Salomone J, eds. St Louis: Mosby; 2003. [Google Scholar]
- 5.Frykberg ER. Medical management of disasters and mass casualties from terrorist bombings: how can we cope? J Trauma. 2002;53:201–212. [DOI] [PubMed] [Google Scholar]
- 6.Trauma Injuries in Israel 2001. The Center for Trauma Research and Emergency Medicine Gertner Institute, ICDC, Trauma Division, Israel Ministry of Health, publication #6002, 2002.
- 7.Klausner JM, Rozin RR. The evacuation hospital in civilian disasters. Isr J Med Sci. 1986;22:365–369. [PubMed] [Google Scholar]
- 8.Pizov R, Oppenheim-Eden A, Matot I, et al. Blast lung injury from an explosion on a civilian bus. Chest. 1999;115:165–172. [DOI] [PubMed] [Google Scholar]
- 9.Katz E, Ofek B, Adler J, et al. Primary blast injury after a bomb explosion in a civilian bus. Ann Surg. 1989;209:484–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leibovici D, Gofrit ON, Stein M, et al. Blast injuries: bus versus open-air bombings–a comparative study of injuries in survivors of open-air versus confined-space explosions. J Trauma. 1996.;41:1030–1035. [DOI] [PubMed] [Google Scholar]
- 11.Shemer J, Heller O, Danon YL. Civilian-military health services contingency program for a mass casualty situation and wartime in Israel. Isr J Med Sci. 1991;27:613–615. [PubMed] [Google Scholar]
- 12.Klein JS, Weigelt JA. Disaster management: lessons learned. Surg Clin of North Am. 1991;71:257–266. [DOI] [PubMed] [Google Scholar]
- 13.Hirshberg A, Stein M, Walden R. Surgical resource utilization in urban terrorist bombing: a computer simulation. J Trauma. 1999;47:545–550. [DOI] [PubMed] [Google Scholar]
- 14.State of California Emergency Medical Authority. Proposed Disaster Medical Systems Standards and Guidelines. Available at: http://www.emsa.cahwnet.gov/dms2/draft_guidelines.doc
- 15.Hirshberg A, Holcomb JB, Mattox KL. Hospital trauma care in mass casualty incidents: a critical view. Ann Emerg Med. 2001;37:647–652. [DOI] [PubMed] [Google Scholar]