Abstract
Context:
An increase of terror-related activities may necessitate treatment of mass casualty incidents, requiring a broadening of existing skills and knowledge of various injury mechanisms.
Objective:
To characterize and compare injuries from gunshot and explosion caused by terrorist acts.
Methods:
A retrospective cohort study of patients recorded in the Israeli National Trauma Registry (ITR), all due to terror-related injuries, between October 1, 2000, to June 30, 2002. The ITR records all casualty admissions to hospitals, in-hospital deaths, and transfers at 9 of the 23 trauma centers in Israel. All 6 level I trauma centers and 3 of the largest regional trauma centers in the country are included. The registry includes the majority of severe terror-related injuries. Injury diagnoses, severity scores, hospital resource utilization parameters, length of stay (LOS), survival, and disposition.
Results:
A total of 1155 terror-related injuries: 54% by explosion, 36% gunshot wounds (GSW), and 10% by other means. This paper focused on the 2 larger patient subsets: 1033 patients injured by terror-related explosion or GSW. Seventy-one percent of the patients were male, 84% in the GSW group and 63% in the explosion group. More than half (53%) of the patients were 15 to 29 years old, 59% in the GSW group and 48% in the explosion group. GSW patients suffered higher proportions of open wounds (63% versus 53%) and fractures (42% versus 31%). Multiple body-regions injured in a single patient occurred in 62% of explosion victims versus 47% in GSW patients. GSW patients had double the proportion of moderate injuries than explosion victims. Explosion victims have a larger proportion of minor injuries on one hand and critical to fatal injuries on the other. LOS was longer than 2 weeks for 20% (22% in explosion, 18% in GSW). Fifty-one percent of the patients underwent a surgical procedure, 58% in the GSW group and 46% in explosion group. Inpatient death rate was 6.3% (65 patients), 7.8% in the GSW group compared with 5.3% in the explosion group. A larger proportion of gunshot victims died during the first day (97% versus 58%).
Conclusions:
GSW and injuries from explosions differ in the body region of injury, distribution of severity, LOS, intensive care unit (ICU) stay, and time of inpatient death. These findings have implications for treatment and for preparedness of hospital resources to treat patients after a terrorist attack in any region of the world. Tailored protocol for patient evaluation and initial treatment should differ between GSW and explosion victims. Hospital organization toward treating and admitting these patients should take into account the different arrival and injury patterns.
Terror related injuries were characterized through retrospective analysis of trauma registry data: 1155 patients, 71% male, 53% aged 15 to 29 years. Gunshot wounds and explosion injuries differed in injured body regions, severity distribution, length of stay, intensive care unit stay, and time of inpatient death. The implications for treatment and for preparedness of hospital resources following a terrorist attack are discussed.
Terror-related injuries have become a threat for populations all over the world. With the increase of terror-related activities, physicians will be increasingly required to treat victims of mass casualty incidents, requiring a broadening of their existing skills and itemed knowledge of various mechanism of injuries.1–3
In Israel, terrorist acts have been an unfortunate reality for many years. The most recent uprising has been particularly devastating, causing extensive loss of life and injuries to young civilians.
Medical care for victims of earlier periods of terror was predominantly for stabbings,4 being hit by objects such as rocks and stones and explosions due to explosives concealed and detonated by remote control. The recent eruption of terror activity comprises of 2 major forms – suicide bomber explosions and gunshots. These attacks resulted in victims sustaining injuries that are more complex and severe than earlier periods of terror activity.5,6 The need to understand the effects and implications of these 2 terror mechanisms led to this study. Gunshot and explosion wounds, which vary in injury profile, hospital services utilization, patient characteristics, and outcome are described and compared. The comparison serves to stress the differences in injury patterns and help produce specific protocols for each of the 2 injury mechanisms. The purpose of this study is: (1) to characterize and compare the effects of gunshot and explosion injuries caused by terrorist acts; and (2) to see how these findings contribute to the severity and outcome of terror-related injuries and the implications for care.
METHODS
This study was a retrospective cohort study of all patients recorded in the Israeli National Trauma Registry (ITR) between October 1, 2000, and June 30, 2002, due to terror-related injuries. The definition of terror-related injury was based on ICD-9-CM external cause of injury E990-E998.
The ITR records all casualty admissions to hospitals, in-hospital deaths, and hospital transfers at 9 of the 23 trauma centers in Israel. The 9 hospitals include all 6 level I trauma centers in Israel and 3 of the largest regional trauma centers in the country. The remaining 14 hospitals include smaller hospitals, not included in the registry. Patients seen there were not recorded unless they were transferred to higher levels of care. However, on the basis of reports by the Ministry of Health, 7 in the year 2002, hospitals in the trauma registry included nearly 80% of hospitalizations due to terror.
The registry includes the majority of severe terror-related injuries. Patient demographic details and data on the nature of injuries, treatment, and outcome were obtained from the registry. Medical diagnoses were classified on the basis of both ICD-9-CM7 coding and AIS8 coding. Severity measures such as AIS8 and ISS9 were used to rank severity. Indicators on hospital resource utilization included length of stay (LOS), intensive care treatment (ICU), and surgical procedures. Inpatient survival and disposition were also noted. The framework for injury diagnoses analysis was based on the Barell body region by nature of injury diagnosis matrix.10,11 The matrix was modified to include 5 injury types: fractures; internal injuries; open wounds; burns; and others. This matrix describes 9 body regions as follows: traumatic brain injury (TBI); other head; spinal cord and column; chest; abdomen; pelvis, trunk, back, and buttock; upper extremities; lower extremities; and other.
These categories enable a broad epidemiologic analysis of injury distribution and also provide for specific anatomic characteristics of injury.
The data set includes up to 10 diagnostic codes per patient. ICD-9-CM diagnosis codes were substituted with corresponding matrix units for the analysis of injury. Using matrix terminology, multiple injury profiles12 were defined.
Internal injuries were defined as injuries in the range of ICD-9-CM codes 850–854, 860–868, subdivided into 3 body regions: head, torso, and abdomen.
SAS statistical software was used for data analysis. Parameters were described and compared between GSW patients and patients injured by explosion. Statistical tests included Pearson χ2 for categorical data, t-tests for continuous variables, and Wilcoxon nonparametric tests where continuous variables did not distribute normally. A value of P < 0.05 was considered statistically significant.
RESULTS
Study Population
During the study period, a total of 1155 patients were recorded in the ITR as sustaining injuries caused by terrorist acts. The majority of patients were injured by explosion (n = 623, 54%). Thirty-six percent (410 patients) had gunshot wounds (GSW), and the remaining 10% (122 patients) were injured by other means. These other injuries were sustained from a variety of violent acts, including stabbings, rocks and other propelled objects, and vehicular assaults. Due to the small number of patients and the diversity of injury mechanisms represented by the “other” cohort, this paper will focus on the 2 larger patient subsets: GSW patients and patients injured in explosions, a total of 1033 patients.
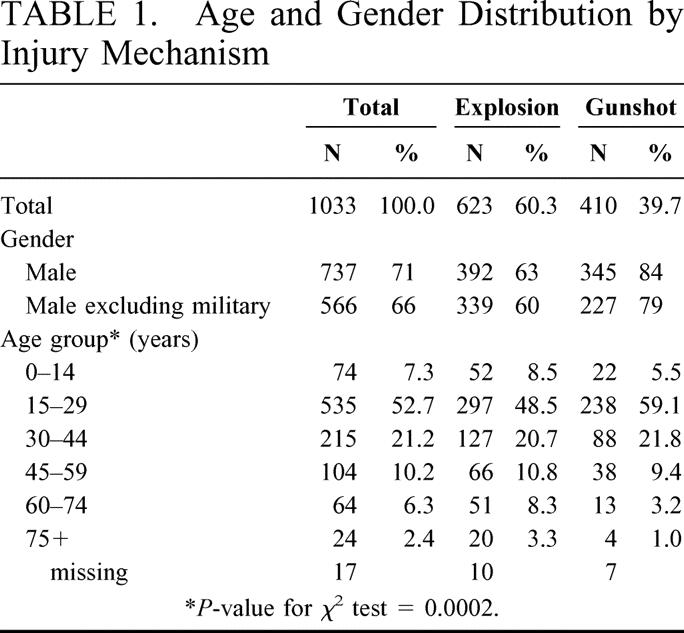
Most patients (n = 737, 71%) were male. GSW casualties included a significantly larger proportion of males compared with explosion injuries as demonstrated in Table 1. Male predominance persisted when injuries during military duty were excluded, though the rate declined. More than half (n = 535, 53%) of the patients were between 15 and 29 years of age, 59% in the GSW group and 48% in the explosion group (Table 1). Patients injured in explosion had a higher proportion of children and elderly than GSW patients.
TABLE 1. Age and Gender Distribution by Injury Mechanism
Injury Characteristics
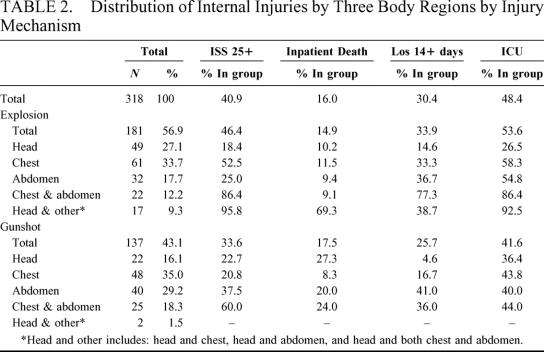
Approximately one third of the patients (n = 318) suffered internal injuries, 181 in explosion and 137 in GSW (30% in both groups).
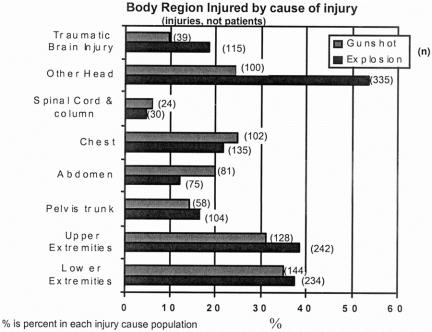
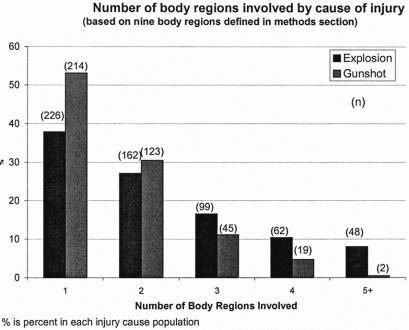
Overall, apart from chest, spine, and abdominal injuries, which are more frequent in GSW victims, all other body regions are injured more frequently in explosion (Fig. 1). Most notable is the excess number of head and brain injuries in patients injured by explosion. The involvement of multiple body regions in a single patient is significantly more common in explosion victims at 62% as compared with 47% in GSW patients (χ2 P < 0.001), thus the total number of injuries in this population is larger. Figure 2 shows the number of body regions involved in the injury for GSW and explosion victims. The proportion of patients with 1 or 2 body regions injured in gunshot terrorist attacks is significantly higher than the proportion in victims of explosion. Patients injured in explosions have higher rates of involvement of 3 or more body regions involved in an injury. Only 2 patients with GSW had 5 or more body regions affected.
FIGURE 1. Body region injured by cause of injury (injuries, not patients). % is percent in each cause population.
FIGURE 2. Number of body regions involved by cause of injury (based on nine body regions defined in Methods section. % is percent in each cause population.
GSW patients suffered significantly higher proportions of open wounds (63% versus 53%, χ2 P = 0.0009) and fractures (42% versus 31%, χ2 P = 0.0005). Burns were present in 91 patients (8.8%), all were victims of explosion. The severity of injury of burn patients was high (30% with ISS of 25 or higher); however, 68% of the patients with burn injuries had also sustained penetrating or blunt injuries or both, contributing to the high severity and injury complexity.
More than 40% of the patients sustaining internal injuries had a critical or fatal injury: an injury with an ISS of 25+ (Table 2). For purpose of analysis, internal injuries were divided into 3 body regions (head, chest, and abdomen) and their combinations. The most frequent injury for both gunshot and those injured by explosion was the chest (n = 171). Single injuries to the abdomen were more frequent in GSW patients. Injuries to the head only were more common in explosions. Injuries affecting both chest and abdomen occurred in 18% of GSW and 12% of explosion victims. Other multiple region injuries to patients with internal injuries were more common in patients injured by explosion (9% in explosion versus 1.5% in GSW patients). The severity, LOS, ICU stay, and inpatient death rates by body region injured are summarized in Table 2.
TABLE 2. Distribution of Internal Injuries by Three Body Regions by Injury Mechanism
Injury Severity
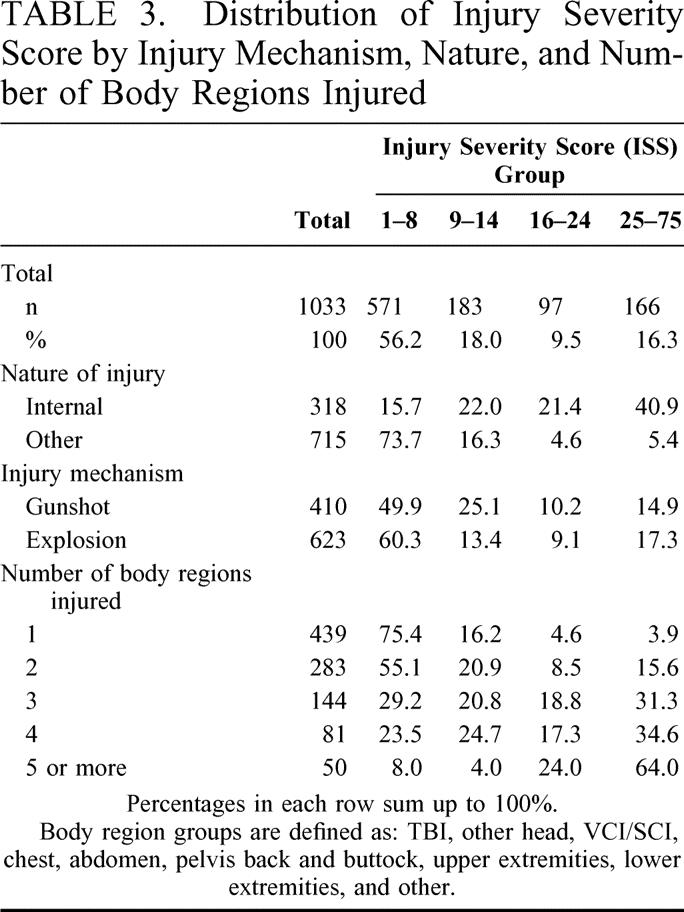
A total of 263 patients (26%) suffered severe, ISS ≥ 16, injuries. Table 3 details the distribution of severity groups for both injury mechanisms. Patients injured by explosion have a larger proportion of minor injuries and a larger proportion of critical to fatal injuries. The proportion of moderate (ISS 9–14) injuries in GSW patients is almost 2-fold higher than in patients injured by explosion (χ2 P < 0.001). Severity of injury for patients with internal injuries was higher with 62% of the patients suffering a severe (ISS 16+) injury (61% in the GSW group, and 63% in the the explosion group). Multidimensional injuries such as burns and penetrating injuries were also associated with high severity, and nearly half had an ISS of 16+. The most severe injuries however were noted in patients with internal injuries, described in Table 2. Ninety-six percent of explosion victims with head and other injuries and 86% of patients with chest and abdominal injuries from explosion had an ISS of 25 or higher.
TABLE 3. Distribution of Injury Severity Score by Injury Mechanism, Nature, and Number of Body Regions Injured
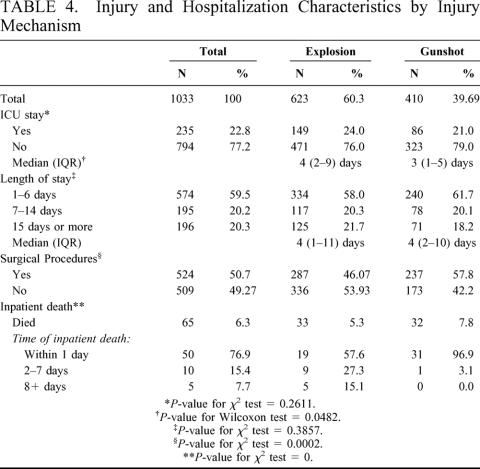
Utilization of Hospital Services
A total of 235 patients (23%) were hospitalized in the intensive care unit (ICU) (Table 4). While the proportion requiring ICU treatment did not differ between GSW and explosion victims, the duration of stay was significantly longer for patients injured by explosion (P = 0.048). Patients with multiple body regions injured had higher rates of ICU stay, increasing from 9% in patients with 1 body region through 23% for those with 2 body regions and up to 71% of patients with more than 2 body regions. Fifty-five percent of the patients with burns and penetrating injuries had been to the ICU. Internal injury patients, particularly those with multiple injuries had the highest rates of ICU admissions (Table 2).
TABLE 4. Injury and Hospitalization Characteristics by Injury Mechanism
Total length of stay (LOS) was longer than 2 weeks for 196 patients (20%) (Table 4). Patients with internal injuries had increased LOS, and the number of body regions involved in the injury also correlated with LOS. The longest hospitalizations were of patients with multidimensional injuries including a combination of burns and penetrating injuries in 1 patient.
Slightly more than half (51%) of the patients underwent a surgical procedure, 58% in GSW group and 46% in the explosion group (Table 4).
Inpatient Mortality
Inpatient death rate was 6.3% (65 patients). There was no statistically significant difference between the groups in death rate (χ2 P = 0.11); however, a significantly larger proportion of GSW victims died during the first day (Fig. 3, P < 0.0001). No patients injured by gunshot who survived longer than 7 days died. The outcomes for internal injury patients were significantly worse, with a death rate of 16%. Multiple internal injury patients had death rates ranging from 17% in chest & abdomen patients to 80% in patients with head, chest, and abdomen internal injuries. Overall, patients with multidimensional injuries to multiple body regions had higher inpatient mortality rates. Of the patients with 5 or more body regions injured, 18% died, compared with 4% in patients with only 1 body region injured.
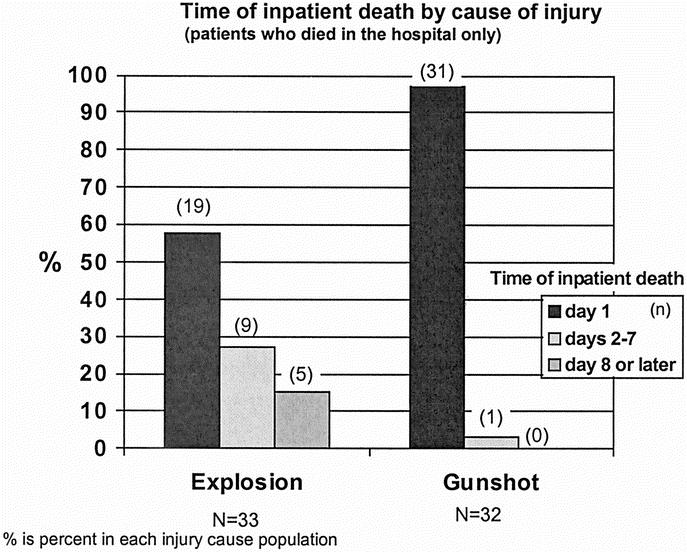
FIGURE 3. Time of inpatient death by cause of injury (patients who died in the hospital only. % is percent in each cause population.
DISCUSSION
This study focused on patients injured and hospitalized after a terrorist attack during 21 months of increased terrorist activities in Israel, from October 2000 to June 2002. The differences between GSW and explosion victims were explored.
The first difference is in the arrival fashion; explosion victims are usually part of a mass casualty event and arrive at the hospital as part of a group while GSW patients are more often injured in sporadic events and arrive as individuals. This point has important implications for hospital organization and may affect patient care. The treatment of severe patients that arrive as an isolated event can be handled within the resources of the trauma center based on physicians from general surgery and other surgical subspecialties, as well as nursing staff. Handling a multiple or mass casualty event demands a different organization of the hospital setting. The sudden influx of patients creates a simultaneous demand on resources that may cause bottlenecks, for example in operation rooms, diagnostic imaging, ICU and specialist staff, particularly in subspecialties.
In a mass casualty scenario, “minimal acceptable care”1 is provided. Minimal acceptable care refers to concentrating efforts on a maximal number of salvageable patients. Although this may seem alien to the usual strive for excellence, the conservation of critical hospital resources is a key consideration. In the initial phase, during which there is an ongoing flow of casualties and the eventual number of victims is still unknown, minimal acceptable care is applied on a temporary basis only until the mass casualty situation subsides. The definitive phase begins when no new casualties are arriving, things are under control, and optimal care can be provided.1
The literature reports that the patterns of injury in patients injured by explosion vary. The initial blast can cause tissue damage, and propelled fragments can cause penetrating injuries. Falling objects or impact from blast displacing the victim's body against a stationary object usually cause blunt injuries but could also cause penetrating injuries. Additionally, victims often suffer burns from the heat discharged by the explosive device or by fire ignited by the blast.1,13,14 The recent uprising in Israel introduced a previously unknown form of injury created by new types of projectiles such as nails, bolts, and other sharp metal objects included in the explosives. These projectiles are propelled in all directions, causing penetrating injuries that are often difficult to detect. As a result, even victims who arrive at the hospital with apparently minimal injuries may require close observation and diagnostic screenings. The critical patients who are transferred to the operating theater immediately after injury should have total body fluoroscopy to find metal foreign bodies that may complicate their course if not detected. Other patients who can wait for further investigation in a delayed fashion, should have total body computed tomographic scan.
The combination of multiple injuries from various mechanisms has been described recently.15,16 Complex injuries of such nature are demonstrated here by the relatively large proportion of burn patients who had also sustained penetrating injuries. Such multidimensional injury pattern16 deserves special attention and indicates special investigatory protocols and management strategies. For example, a patientwho suffers blast lung injury will need fluid restriction. A patient who suffers burns will need liberal fluid administration. The combination of blast lung with burn injury will require sophisticated invasive monitoring for fluid management.
The large proportion of internal injuries in this population (30%), both penetrating and blunt, is a further cause for the high rate of severe injury in terror-related trauma as compared with other forms of trauma.5,17 The most common injured body regions in this study were the head and the extremities, similar to results reported from Ireland.18 Internal injuries were mostly to the chest (54%). This is potentially explained by the majority of explosions occurring in confined spaces such as busses and shops. Furthermore, the victims were mainly civilians who are unprotected, and the use of nails and bolts as part of the bomb, not previously experienced in Ireland, increased the extent of the wound. A study comparing injuries of casualties of terror during military activity, while wearing protective vests and helmets confirms this assumption as the distribution of injuries among patients injured during military activity were mostly to the head and extremities, with a relatively lower proportion of internal injuries to the abdomen, chest, and head, resulting in less severe outcomes (K. Peleg and L. Aharonson-Daniel; unpublished study).
The involvement of multiple body regions was found to be more common in explosion victims. Multiple body region injuries are a significant cause for increased overall injury severity. The proportion of severe (ISS 16+) injuries in patients with 5 or more injuries is almost 90%, more than 10 times higher than in patients with 1 body region injured. By definition, ISS is likely to increase with multiple body regions injured. However, the distribution of severity of injury is worthy of note as patients injured in explosions have a larger proportion of minor injuries and a larger proportion of critical to fatal injuries. The proportion of moderate (ISS 9–14) injuries in patients injured by gunshot is almost 2-fold higher than in patients injured by explosion (χ2 P < 0.001). This could possibly be explained by the high proportion of fractures (42%) in patients injured by gunshot, as limb fractures are usually assigned a moderate severity score.
As explosion injuries include a large proportion of multiple injuries to the same body region and injuries to more than 3 body regions (Table 3), ISS may underestimate the injury severity due to the fact that it scores only the most severe injury in each body region.6,19 This finding suggests a need to create a new ISS that would take into account multidimensional injuries.
The average duration of stay of explosion victims in the ICU was longer than that of GSW patients. As ICU beds are a limited resource and require heavy staffing and expensive care, this finding has important implications on hospital resource use.
When discussing patient mortality, it is important to remember that the data used in this study exclude patients who died at the scene as well as those who arrived dead to the hospital. Comparisons of death rate with other studies is therefore limited to studies of similar inclusion criteria.20 Inpatient death rate was 6.3% (65 patients). This rate was double the inpatient death from road traffic casualties (2.8%) and 3-fold higher than other trauma (1.8%) in the ITR.17
Time of death was significantly different between the groups; patients injured from GSW died mostly on the first day and never after day 7, while inpatient death in patients injured by explosion was more likely to occur later during the hospitalization. This could be due to the fact that patients with GSW die more often from exsanguinations or brain injury rather than organ failure and complications seen in patients injured in explosions.
CONCLUSION
Gunshot and explosion injuries comprise the majority of terror-related trauma in Israel during the most recent uprising. These mechanisms differ in injury severity distribution, in the proportion of patients suffering multiple injuries, in the duration of stay in ICU, and in the body region of injury. While the inpatient death rate is not significantly different between the 2 injury modalities, the time of death is different with GSW patients expiring within 24 hours. These findings have implications for treatment and for the preparedness of hospital resources and training to treat patients after a terrorist attack in any region of the world. Tailored protocol for patient evaluation and initial treatment should differ between GSW and explosion victims. Disaster management plans should include the possibility of terrorist bombing, and medical preparedness should anticipate that a large proportion of the injuries will be nonfatal.
Footnotes
Reprints: Kobi Peleg, PhD, MPH, Center for Trauma and Emergency Medicine Research, Gertner Institute, Sheba Medical Center, Tel Hashomer, Israel 52621. E-mail: kobip@gertner.health.gov.il.
REFERENCES
- 1.Stein M, Hirshberg A. Limited mass casualties due to conventional weapons: a daily reality of a level 1 trauma center. In: Terror and Medicine, Shemer J, Shoenfeld Y, eds. Berlin: Pabst Science Publishers, 2003;385. [Google Scholar]
- 2.Frykberg ER, Tepas JJ III, Alexander RH. The 1983 Beirut Airport terrorist bombing. Injury patterns and implications for disaster management. Am Surg. 1989 Mar;55:134–141. [PubMed]
- 3.Mallonee S, Shariat S, Stennies G, et al. Physical injuries and fatalities resulting from the Oklahoma City bombing. JAMA. 1996;276:382–387. [PubMed] [Google Scholar]
- 4.Hanoch J, Feigin E, Pikarsky A, et al. Stab wounds associated with terrorist activities in Israel. JAMA. 1996;276:388–390. [PubMed] [Google Scholar]
- 5.Peleg K, Aharonson-Daniel L, Stein M, et al. Patterns of injury in hospitalized terrorist victims. Am J Emerg Med 2003;21:258–262. [DOI] [PubMed] [Google Scholar]
- 6.Mintz Y, Shapira SC, Pikarsky AJ, et al. The experience of one institution dealing with terror: the El Aqsa Intifada riots. Isr Med Assoc J. 2002;4:554–556. [PubMed] [Google Scholar]
- 7.Practice Management Information Corporation (PMIC). International Classification of Diseases, 9th revision, clinical modification 5th edition (ICD-9CM). Los Angeles: Practice Management Information Corporation, 1998. [Google Scholar]
- 8.Association for the Advancement of Automotive Medicine (AAAM). Committee on Injury Scaling. The Abbreviated Injury Scale-1990 Revision (AIS-90). Des Plaines IL: Association for the Advancement of Automotive Medicine, 1990. [Google Scholar]
- 9.Baker SP, et al. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187–196. [PubMed] [Google Scholar]
- 10.Barell V, Aharonson-Daniel L, Fingerhut LA, et al. An introduction to the Barell body region by nature of injury diagnosis matrix. Inj Prev. 2002;8:91–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.The Barell body region by nature of injury diagnosis matrix, accessed on January 16, 2004. http://www.cdc.gov/nchs/about/otheract/ice/barellmatrix.htm. [DOI] [PMC free article] [PubMed]
- 12.Aharonson-Daniel L, Boyko V, Ziv A, et al. A new approach to the analysis of multiple injuries using data from a National Trauma Registry. Injury Prev. 2003;9:156–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mellor SG. The relationship of blast loading to death and injury from explosion. World J Surg. 1992;16:893–898. [DOI] [PubMed] [Google Scholar]
- 14.Stapczynski JS. Blast injuries. Ann Emerg Med. 1982 Dec;11:687–694. [DOI] [PubMed]
- 15.Sorkin P, Nimrod A, Biderman P, et al. The quinary (V th) injury pattern of blast. J Trauma. 2003; (in press). [PubMed]
- 16.Kluger Y. Bomb explosions in acts of terrorism – detonation, wound ballistics, triage and Medical Concerns. IMAJ. 2003. [PubMed]
- 17.Peleg K, Aharonson-Daniel L, Stein M, et al. The Epidemiology of Terror – Data from the Israeli National Trauma Registry in Terror And Medicine, Shemer J, Shoenfeld Y, eds. Berlin: Pabst Science Publishers, 2003;360–365. [Google Scholar]
- 18.Hadden WA, Rutherford WH, Merrett JD. The injuries of terrorist bombing: a study of 1532 consecutive patients. Br J Surg. 1978;65:525–531. [DOI] [PubMed] [Google Scholar]
- 19.Osler T, Baker SP, Long W. A modification of the injury severity score that both improves accuracy and simplifies scoring. J Trauma. 1997;43:922–925; discussion 925–926. [DOI] [PubMed]
- 20.Shapira SC. Beware of comparing international health systems, including trauma units. IMAJ. 2002;4:117–118. [PubMed] [Google Scholar]