Abstract
Objective:
The goal of this report is to examine the success of vacuum-assisted fascial closure (VAFC) under a carefully applied protocol in abdominal closure after open abdomen.
Summary Background Data:
With the development of damage control techniques and the understanding of abdominal compartment syndrome, the open abdomen has become commonplace in trauma patients. If the abdomen is not closed in the early postoperative period, the combination of adhesions and fascial retraction frequently make primary fascial closure impossible and creation of a planned ventral hernia is required. We have previously reported our experience with the development of a technique for VAFC that allowed for closure of the fascia in many such patients long after initial operation. During this previous study, during which the technique was being developed, VAFC was successful in 69% of patients in whom it was applied, and 22 patients were successfully closed at ≥ 9 days after initial surgery (range, 9 to 49 days). A protocol for the use of VAFC in patients with open abdomen was developed on the basis of these data and has been employed since October 2001. The outcome of this protocol's use is examined.
Methods:
This is a prospective evaluation of all trauma patients admitted to Wake Forest University Baptist Medical Center over a 19-month period who required management with an open abdomen. VAFC employs suction applied to a large polyurethane sponge under an occlusive dressing in the wound and allows for constant medial traction of the abdominal fascia. It is attempted in all patients in whom the rectus muscles and fascia are intact. Studied variables include fascial closure rate, time to closure, incidence of wound dehiscence, and hernia development after closure.
Results:
From November 1, 2001, through May 31, 2003, 212 laparotomies were performed in injured patients; 53 (25%) of these patients required open abdomen management. Mean injury severity score for the group was 34, with an average abdominal abbreviated injury score of 2.9. Forty-five (78%) survived until abdominal closure. Vacuum dressings were used in all 45 but VAFC was not attempted in 2 patients (1 due to development of enterocutaneous fistula, 1 because a rectus flap was used for another wound). Closure rate in those undergoing VAFC was 88% (38), with mean time to closure being 9.5 days. This is significantly higher than the 69% rate of fascial closure during the time in which the technique was developed (P = 0.03). Twenty-one patients (48%) were closed at ≥ 9 days (range, 9 to 21 days). Two patients (4.6%) developed wound dehiscence and underwent successful reclosure. One patient (2.3%) developed a ventral hernia on follow-up, which has since been repaired
Conclusions:
The use of VAFC under a carefully defined protocol has resulted in significantly higher fascial closure rates, obviating the need for subsequent hernia repair in most patients. The utility of this technique is not limited to the early postoperative period, but it can be successful as much as 3 to 4 weeks after initial operation.
A method of vacuum-assisted fascial closure (VAFC) applied to all trauma patients with open abdomen under a carefully defined protocol is examined. This method resulted in an 88% fascial closure rate, with some closures as much as 21 days after initial operation. This is an improvement over our previous closure rate with this technique and has significantly reduced the need for planned ventral hernia creation with later repair in this population.
Twenty years ago, the idea of electively leaving the abdomen of a surgical patient open after laparotomy was an abhorrent one to most surgeons. In the intervening years, the development of the concept of the damage control laparotomy and the understanding of the abdominal compartment syndrome has markedly changed this idea. It is now recognized that the combination of acidosis, coagulopathy, and hypothermia represent a potentially lethal combination in the injured patient, and prolonged operation in such a case will only worsen the problem. In this situation, abbreviated laparotomy aimed at stopping surgical bleeding and limiting contamination is usually preformed. This frequently leaves the abdomen in such a state that the patient requires at least one if not several reoperations to restore intestinal and/or vascular continuity.
We also now know that visceral or retroperitoneal edema due to shock and reperfusion may increase intraabdominal pressure to dangerous levels, leading to organ dysfunction. Patients with this constellation of symptoms must have their abdomens left open temporarily to allow for visceral and renal perfusion as well as adequate pulmonary function.
With recognition of optimal management of these 2 patient populations, the care of the injured patient has been greatly improved. With the solution to one problem, however, another has been created. A method for temporary coverage of the open abdomen is now required. Surgeons have responded with several alternatives, many of which are effective in protecting the viscera and allowing serial access to the peritoneum.1–5 The reported eventual fascial closure rate varies from 50% to 70%, depending on the technique. All of these methods have in common the problem of the inability to obtain primary fascial closure beyond 7 to 10 days. After this, the viscera have adhered to the anterior abdominal wall and the fascia has retracted. This situation requires the creation of a planned ventral hernia and eventual abdominal wall reconstruction in the ensuing months.5
A recent report from our institution outlined the development of a technique of vacuum-assisted fascial closure (VAFC) in which a primary fascial closure rate of 69% was reported with the technique.6 More importantly, VAFC allowed for the fascial closure of 22 of these patients at large intervals after the original laparotomy (mean, 21 days; range, 9 to 49 days). The ability to close the abdomen at such an interval was felt to be a significant improvement over earlier techniques, and a protocol for management of the open abdomen incorporating this technique was implemented. The authors speculated on the basis of these results that more aggressive employment of VAFC under such a protocol would lead to higher rates of abdominal closure overall and further decrease need for future abdominal wall reconstruction.
The aim of this study is to examine the use of VAFC under this protocol and its effect on abdominal outcome.
METHODS
Patient Population
This is a prospective evaluation of all patients admitted to the trauma service at Wake Forest University Baptist Medical Center who required open abdomen after damage control laparotomy or due to abdominal compartment syndrome over a 19-month period. Comparison is made to patients managed with an open abdomen in the previous 5-year period who were identified in the previously published work.6
Open Abdomen Management
Before 1996, many patients requiring open abdomen management at our institution were managed with a standard vacuum pack dressing as described by Barker et al.1 Beginning in 1996, a polyurethane sponge (V.A.C.; KCI International, San Antonio, TX) was substituted for the surgical towel described by the Chattanooga group in some patients. It was observed that this appeared to result in more frequent fascial closure than the previous method. It was felt that the reason for this is that the vacuum, when applied to the sponge in contact with the fascia, allowed for constant medial traction, thus preventing loss of domain. This method was eventually adopted as the standard method of open abdomen dressing, and a 5-year experience with the development of this technique was reported in 2002.
A protocol for the management of the open abdomen with VAFC was instituted on the trauma service on the basis of this report, and the outcomes were tracked. The protocol is outlined in Figure 1. Initially, a standard vacuum dressing with a surgical towel is usually applied. After the edema has resolved to the point that a sponge will fit into the wound, the process of VAFC begins. One of the most important steps is shown in Figure 2; a perforated polyethylene sheet is placed over the bowel and under the fascial edges. This prevents the viscera from adhering to the abdominal wall during the days or weeks to follow, preserving exposure for subsequent fascial suture placement. Over this is placed the sponge (Fig. 3), which is stabilized by a running suture on the skin edges. This pushes the viscera down into the abdomen so that the sponge will eventually be in contact with the majority of the cross-section of the abdominal wall. Suction tubing and an occlusive dressing are then applied as in Figure 4. As suction is applied, the sponge shrinks, pulling the edges of the wound toward the midline uniformly (Fig. 5.) The sutures serve only to hold the sponge and the abdominal wall in place before application of suction, but place little to no tension on the wound edges after suction is applied. This is shown in Figure 6; the sutures, initially under some tension, are now lax, and all of the traction on the edges of the abdominal wall is provided by the suction applied to the dressing. The dressing is changed every 3 to 5 days; this may be done in the intensive care unit if necessary. As the wound is pulled together and edema resolves, the upper and lower ends of the wound may be closed as shown in Figure 7. Finally, the fascia is completely closed and the skin left open (Fig. 8).
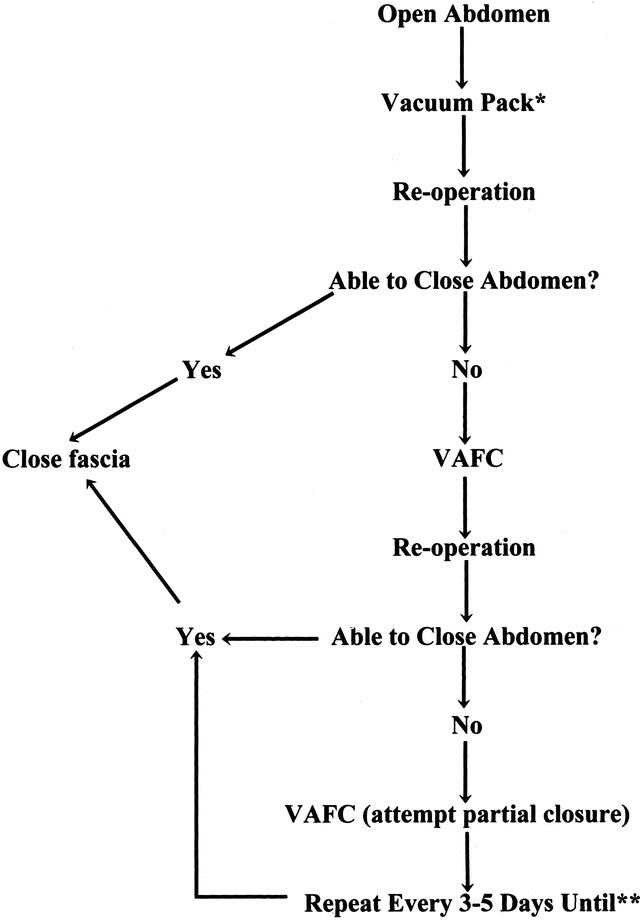
FIGURE 1. Algorithm for VAFC applied to patients requiring open abdomen. *Standard vacuum pack dressing as described by Barker et al3 using surgical towel. Sponge is usually placed at second look when edema has improved. **Or until repeated dressing changes interfere with patient recovery.

FIGURE 2. A polyethylene sheet is tucked under the fascia to prevent adherence of the viscera to the abdominal wall.
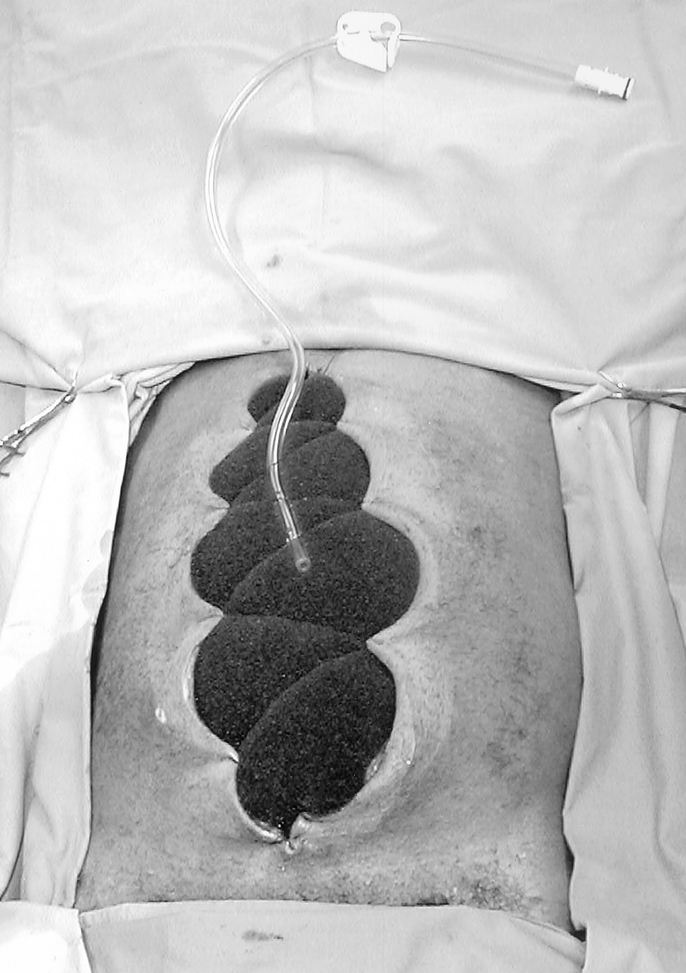
FIGURE 3. The sponge is stabilized with suture and suction tubing applied.

FIGURE 4. An occlusive dressing is placed before the application of suction.

FIGURE 5. Suction is applied, resulting in contraction of the wound and medial traction on the fascia.

FIGURE 6. Note the laxity in the suture after suction application. All tension on the wound edges is now produced by the suction on the sponge.

FIGURE 7. The abdomen may be partially closed.

FIGURE 8. The abdomen is finally completely closed 21 days after initial operation.
Data Analysis and Statistics
Studied end points included fascial closure rate, time to closure, abdominal complications, including fistula, abscess, and dehiscence, as well as postoperative incidence of ventral hernia. In our previous experience, we were unable to close any patient after 9 days without the use of VAFC, so we have identified any patient closed beyond 9 days as a late closure.
Statistical analyses were performed using Statview 5.0 (SAS Institute Inc., Cary, NC). Dichotomous variables were compared using χ2 or Fisher exact test where appropriate. Continuous variables were compared using Student t test. Significance is defined as P ≤ 0.05.
RESULTS
General Population
From November 1, 2001, through May 31, 2003, 212 patients admitted to the trauma service at Wake Forest University Baptist Medical Center underwent laparotomy. Of these, 53 (25%) required management with an open abdomen (13% from penetrating injury, 87% from blunt injury). The abdomen was left open after damage control laparotomy in 45 patients and after decompressive laparotomy for abdominal compartment syndrome in 8 patients. Of these patients, 45 (78%) survived until eventual abdominal closure. The mean age of this group was 36 ± 15 years, mean injury severity score (ISS) and abdominal abbreviated injury scores (abd AIS) were 34 ± 12 and 2.9 ± 2.3, respectively, and admission base deficit was −10 ± 5 mEq/L. Thirteen intestinal repairs were preformed in 12 of these patients; these comprised 2 stomach repairs, 4 colon repairs, 6 small bowel resections with reanastomosis, and 1 colon resection with reanastomosis. Vacuum dressings were used in all 45 patients, but VAFC was attempted in only 43. The other 2 had planned ventral hernia creation without attempt at fascial closure. Of these, 1 patient was left open due to development of an enterocutaneous fistula at the site of an enterotomy repair, and the other had required a rectus flap for another site.
Abdominal Closure
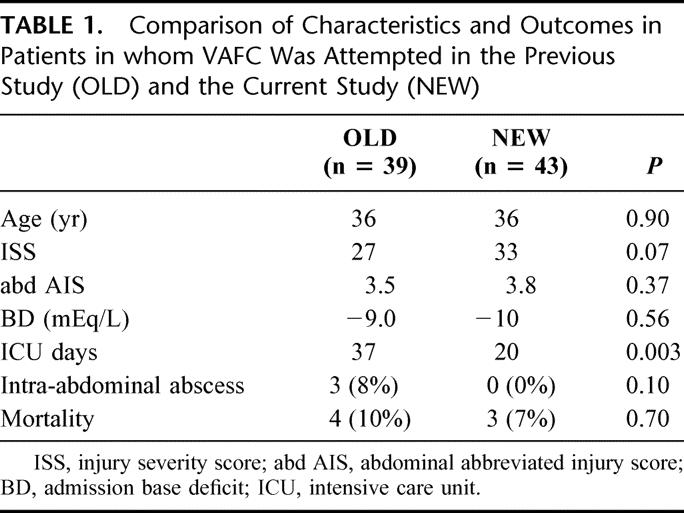
The remaining 43 patients underwent attempted VAFC under protocol, and the technique was successful in 38 (88%). This is significantly higher than the 69% closure rate (P = 0.03) that was seen in the previous study done during technique development. Mean time until abdominal closure was 9.6 days (range, 1 to 21 days). Mean number of dressing changes in the closed group was 3.4 (range, 1 to 9). The groups in which VAFC was attempted in the previous study and the current study are compared in Table 1 to determine if there are group characteristics that would account for this difference in closure rate. The age, severity of injury, and admission shock was similar between the 2 groups. Thus it appears likely that the reason for the improved closure rate is a consistent application of the VAFC protocol.
TABLE 1. Comparison of Characteristics and Outcomes in Patients in whom VAFC Was Attempted in the Previous Study (OLD) and the Current Study (NEW)
Late Closure
An important benefit of VAFC in addition to improving abdominal closure rate is that it allows for fascial closure weeks after initial laparotomy, with 21 patients (48%) undergoing late (>9 days) closure. The range of closure times in this group was 9 to 21 days.
Closure Failure
The group in whom VAFC failed was compared with those who were successfully closed to determine if there were group characteristics that might predict difficulty or inability to close. The groups did not differ, however, with the mean age (37 vs. 36 years; P = 0.89), mean ISS (35 vs. 33; P = 0.84), mean abd AIS (3.7 vs. 3.8; P = 0.90), and mean admission base deficit (−11 vs. −10 mEq/L; P = 0.71) being similar. All failures occurred in those with an open abdomen secondary to damage control laparotomy (5 of 31), with none occurring in the abdominal compartment syndrome population (0 of 7); however, this did not reach statistical significance (P = 0.57). Therefore, it is not clear why the technique fails in some.
Abdominal Complications and Hernia Rate
One patient with a vacuum dressing developed an enterocutaneous fistula at the site of an intestinal repair. VAFC was not attempted in this patient, but it is possible that the fistula was related to vacuum therapy. No other fistulae were seen. No patient developed intraabdominal abscess. While in the hospital, 2 patients (4.6%) with successful fascial closure developed wound dehiscence and were successfully reclosed. Mean follow-up on the closed patients is currently 185 days (range, 14 to 708 days), and 1 patient has been found to have a ventral hernia that has subsequently been repaired (2.3%).
DISCUSSION
The concept of leaving the abdomen open intentionally after laparotomy has gone from surgical heresy to an accepted method of management in certain circumstances. Along with this transition have come several methods of managing the open abdomen that afford protection to the viscera and allow for a simple return to the abdomen at the time of reoperation. While the eventual goal in all cases is to close the abdominal fascia when safe, this proves difficult to impossible after 7 to 10 days. In this case, a skin graft is placed and the resulting hernia is repaired some months later. This method works well, but it does require a second major operation with the potential for attendant morbidity. Other series have documented a fascial closure rate of 50 to 70% in abdomens left open due to edema.1–5 The current data demonstrate a fascial closure rate of 88%, with almost half of these closures occurring at 9 to 21 days after initial operation. Thus the technique of VAFC allows for the large majority of abdomens to be closed with fewer hernia repairs required. In addition, the technique allows for successful closure at a significant interval after laparotomy.
The advent of the concept of damage control laparotomy in severely injured patients has been largely responsible for advances in care of the open abdomen patient. It is now clear that in a subgroup of patients undergoing laparotomy for trauma, the metabolic derangements of acidosis, hypothermia, and coagulopathy are more likely to be immediately life-threatening than lack of definitive surgical repair of injuries.7–9 Techniques such as packing of bleeding sites, intestinal discontinuity, and temporary intravascular shunts make return to the operating room at a more opportune time necessary, and abdomens of such patients have been managed with a number of temporary closure devices.1,10–13 Visceral or retroperitoneal edema after definitive repair may continue to make safe fascial closure impossible.
The second common situation in which open abdomens are seen in trauma patients is after decompressive laparotomy in the face of abdominal compartment syndrome. Abdominal compartment syndrome may be seen due to intraabdominal injury14 as well as secondary to edema in the face of shock and resuscitation despite the absence of intraabdominal injury.15 The syndrome produces significant cardiopulmonary and renal derangements,16–18 and decompressive laparotomy leads to improvement in these conditions.19 Fifteen percent of the current population required decompressive laparotomy. This is frequently followed by prolonged edema, making subsequent abdominal closure difficult.
In situations such as the damage control laparotomy and the patient with abdominal compartment syndrome, several methods have been developed for temporary abdominal closure. Initially, simple plastic coverings such as the Bogata bag were employed.10 The goal of these temporary abdominal dressings was to prevent evisceration, and protect the underlying viscera while allowing for easy peritoneal access.
Perhaps the 2 methods that have become most widely used are the placement of temporary mesh and the vacuum pack dressing as described by Barker et al.1 The issue of temporary abdominal closure was examined by the Memphis group in 1994.5 Among other issues, they commented on the various prostheses available, including polytetrafluoroethylene patch, polypropylene mesh, and polyglactin 910 mesh. Because of the favorable combination of visceral protection, ease of use, low fistula rate, and low cost, they concluded that absorbable polyglactin 910 was the best suited for this management technique. Other institutions have echoed this, and temporary absorbable mesh placement has become a workhorse in the management of the open abdomen. It allows for sequential closure when possible, provides protection to the underlying bowel as well as a method for fluid egress, and it allows for easy abdominal re-entry when necessary.
The vacuum pack dressing has been well studied by Barker et al and has also proven to be a safe and effective method of temporary abdominal closure. In addition to providing protection and ease of application, it also allows for the control and measurement of abdominal fluid drainage. While these and other methods all provide a satisfactory system of temporary closure, the downside of all of these techniques may be best summed up by Dr. Barker in the discussion of their paper in 2000: “If a patient goes over 6 days, the probability of being able to do a primary fascial closure is markedly decreased.”1
The combination of fascial retraction and adherence of the viscera to the overlying abdominal wall soon make the creation of a planned ventral hernia necessary. While these techniques are well described and remain an important piece of the open abdomen management armamentarium, they do necessitate a future major abdominal operation if the fascia is not closed early.
VAFC differs from these and other techniques in that it prevents both fascial retraction and visceral adherence, allowing for continuing attempts at abdominal closure several weeks after laparotomy. This is an extension of the standard vacuum pack technique and has 2 important components allowing for later closure. The first is the perforated polyethylene sheet placed over the bowel. This must be tucked under the fascial edges, and prevents adherence. The second is the thick polyurethane sponge as opposed to the surgical towel used in the original technique. This provides suction to the cross-section of the abdominal wall, preventing fascial retraction by creating constant medial tension on the fascia without injuring it as some similar techniques using suture might. It is these 2 features that likely account for the higher closure rate seen with this technique and reduce the need for future hernia repair. This technique has also been examined by Garner et al, and their results reinforce this concept.20
While the technique is useful, it is not applicable in all settings; depending on the scenario, it is best employed in combination with other methods. The dressing itself is not distensible; for this reason, it should not be used in those at risk for redevelopment of compartment syndrome. The dressing also does not lend itself to the dramatic visceral edema with bulging bowel sometimes seen in the critically ill patients. A standard vacuum pack or absorbable mesh may be required in these patients until edema has resolved enough to allow for VAFC.
In summary, several useful methods for open abdominal management have been developed in recent years. VAFC should now be placed in this arsenal of techniques and may represent an improvement over previous techniques in that it allows for a higher rate of abdominal closure than those reported for other methods. When carefully applied under a protocol for open abdomen management, it allowed for an 88% fascial closure rate, and almost half of these closures occurred later in the patient's hospital course. This represents a significant improvement in the closure rate over our previous data, and it has substantially reduced the need for the creation of a controlled ventral hernia at our institution.
Discussions
Dr. Timothy C. Fabian (Memphis, Tennessee): I would like to compliment the authors on another important contribution to the management of the open abdomen with this technique of vacuum-assisted fascial closure. They had only 1 intestinal fistula in 53 patients and while the follow-up is relatively short, a mean of 6 months, they have observed only 1 ventral hernia. My concerns with comparison of these results with other reported techniques, however, revolve around patient selection for open abdomen management. It is not always clear that similar populations are being compared.
We recently reported our experience with the use of absorbable mesh for open abdomen management in 274 patients over an 8-year period (Ann Surg, Vol 238, 349–355, 2003). Those 274 cases represented 10% of the population requiring emergency laparotomy in our series. The series reported today, the 53 laparotomies over one and a half years treated by the vacuum-assisted fascial closure technique, represented 25% of your laparotomies over that time period. I think we are not comparing the same populations. We were only able to obtain secondary fascial enclosure in 22% compared with 88% in this study. Since you appear to be using the open abdomen technique more than twice as frequently, is it possible the difference in our results is at least partially explained by more of our patients having primary fascial closure, avoiding open abdomen management?
Along a similar vein, you report today significantly better results (88% vs. 69%) compared to your initial experience with vacuum closure. I am not convinced those 2 populations are exactly the same. First, in the old study there were 39 cases over 5 years compared to 43 cases over one and a half years in the new study, essentially the same number of cases in one third the time. Are you sure there were that many more laparotomies in the 2 time periods to account for the difference?
Second, while there were similarities in the 2 groups as stratified in Table 1 of the manuscript according to age, injury severity, and base deficit as presented today, there were also differences. The ICU stay in the old study was nearly twice that of the present study, 37 days versus 20 days. The abdominal abscess rate was 8% versus none at this time. I would speculate the present study was overall less severely ill because of liberalization of application of open management. Please respond.
Another question I would have is your fistula rate is quite admirable. How many of these patients had intestinal suture lines that might have increased the risk associated with constant suction being applied? Regardless of these criticisms, you have made an important and novel contribution to open abdomen management. The only way to completely resolve some of the questions raised today would be via a prospective randomized trial. Do you have any interest in such a trial?
Dr. Robert Maxwell (Chattanooga, Tennessee): I would like to thank you for the privilege of the podium this morning to discuss yet another exciting paper from the Division of Trauma at Wake Forest by Dr. Meredith and colleagues. The manuscript is well written and provided in a timely fashion, as is the custom of the department. The work serves as a sequel to a previously published technique of open abdominal management after ascending the learning curve with the first paper. This somewhat radical modification of the negative pressure dressing pioneered in Chattanooga exceeds previous techniques developed simply to protect the viscera and is designed proactively to achieve primary fascial closure during periods of extensive visceral edema. This modification consists of a running skin closure over a commercially available polyurethane sponge. The negative pressure is intended to off-load stress along the suture line and reclaim abdominal domain. This technique is widely applicable to a variety of conditions which can result in open abdominal wounds, as is commonplace in many surgical ICUs. However, in this series it was performed exclusively in blunt and penetrating trauma patients. Over a 19-month period, 43 patients were prospectively evaluated under the guidelines of a strict protocol, 38 successfully achieving primary fascia closure, for a closure rate of 88%. One patient was excluded from the analysis secondary to the development of an entero-cutaneous fistula. Two patients subsequently dehisced but were successfully reclosed. Five patients failed to achieve closure, although the authors were unable to determine any factors that might predict this outcome. One patient presented in follow-up with a delayed incisional hernia.
In summary, this technique appears to be a clever improvement over existing methods and appears to improve closure rates without added morbidity. Patients successfully closed obviously avoid delayed abdominal wall reconstruction at a later date, often after they have convalesced from other injuries. Since your first publication we have begun the selective application of your technique in our own practice and have realized similar promising results. However, if you include the 2 dehiscences and the hernia as well as the fistula as failures, the success rate drops to 77%, which is not much better than reported rates of 70% to 75% now seen in the literature. It should come as no surprise, I might add parenthetically, that your 2 dehiscences are at increased risk for long-term hernia development. We therefore have several questions and 1 final comment.
First, could you elaborate on how you determine when to convert from the standard VAC after the initial damage control laparotomy to the present technique with respect to visceral edema? The manuscript alludes to the fact that you may use several “towel VACs” before proceeding with the sponge. We were concerned that the running closure could cut through the edematous bowel and lead to increased fistula rates if inappropriately performed.
Secondly, how many patients in this series had enterotomies repaired, bowel resections, or stoma formations, and are there any contra-indications to the application of this technique?
Third, have you considered analyzing body mass index as a factor in predicting failure of the technique? Our experience has shown us that the bigger they are, the harder they fall and the harder they are to put back together again.
Finally, the reported follow-up is short and should be observed for longer periods for delayed hernia formation in the entire population of both papers.
Dr. J. David Richardson (Louisville, Kentucky): We put a VAC on almost everything now. Because the patients are so complicated, trying to compare them we have certainly found difficult. I need clarification about your protocol. If you have an exposed suture line do you do the VAC or does that stay your hand?
Dr. Preston Miller (Winston-Salem, North Carolina): As Dr. Meredith said, there was a time in general surgery that leaving the abdomen open intentionally was considered surgical heresy, it just wasn't done. Fortunately this is no longer the case, and through the years we have begun to understand that with the need for damage control laparotomy and the need for treatment of abdominal compartment syndrome, the abdomen is and should be left open more and more commonly. Our aim here was to try to describe a technique that we have used that we believe leads to a higher rate of abdominal closure and also preserves the ability to close the fascia far into the hospital stay of these patients. I think these data do demonstrate that, because we had an 88% closure rate, some of which were closed at 21 days after their initial operation.
Dr. Fabian's and Dr. Richardson's points are very important, though. And that is, if you are not comparing apples to apples, you don't know how these results may be generalizable to other institutions and other situations.
Dr. Fabian, you first asked about the population difference in Memphis and Wake Forest and the difference between the 10% open abdomen rate versus the 25% open abdomen rate. Having had the good fortune to train in Memphis I have seen that population, and having been at Wake Forest for 2 years I have seen that also, and they are vastly different populations, I think. We have 60% of our patients transferred in from other institutions. They come down out of the mountains of Virginia and North Carolina. Sometimes they are unable to fly, they have long ambulance rides. These people have prolonged compensated or sometimes uncompensated shock and are not being resuscitated. And as a result, we see a lot of visceral edema that I think other programs may not see as much of. I think that is a difference in the 2 populations.
You also asked about our comparison to our earlier work and the rate of open abdomen with our laparotomies. First of all, remember that was a retrospective work and the data gathering may have reflected that, as opposed to this, which is prospective. But you asked, is it possible that this group was actually a little less sick than the last group and that is why we were able to close more abdomens? Or asked another way, have we liberalized our indications for use of the open abdomen? I think the answer to that is yes, and I think it has been to the benefit of the patient. We more and more realize that leaving the abdomen open is safe, it is effective in preventing abdominal compartment syndrome, and I think we do use it more than we used to.
That being said, I think it is important to understand that these patients were severely injured. Their base deficit when they got there was 10, their ISS was 34. I think it would be a mistake to assume that a large number of these patients could have been easily closed. As a matter of fact, half of them were unable to be closed until 9 to 21 days afterwards. So I don't think simply liberalization of our criteria explains our results.
Dr. Maxwell, you asked about how do we decide when to use a VAC sponge. We use basically when it is technically possible, and that is when the visceral edema is resolved enough to be able to piece together the dressing. You asked about the sutures. The sutures go over the sponge, so they don't lay across the bowel. So there is really no risk to the bowel from that. As far as intestinal repairs or ostomies—Dr. Fabian mentioned this, too—I don't know the exact numbers of that. We don't avoid a VAC if there has been a repair. Now, had there been a fistula or suture line sitting in the middle of the open abdomen, I would be pretty anxious about using a VAC without trying some other type of coverage with that.
In conclusion, I think this is a useful technique and hopefully it can be added to the armamentarium of the management of the open abdomen.
Footnotes
Reprints: Preston R. Miller, MD, Assistant Professor, Department of Surgery, Wake Forest University School of Medicine, Medical Center Blvd., Winston-Salem, NC 27157. E-mail: pmiller@wfubmc.edu.
REFERENCES
- 1.Barker DE, Kaufman HJ, Smith LA, et al. Vacuum pack technique of temporary abdominal closure: a seven year experience with 112 patients. J Trauma. 2000;48:201–207. [DOI] [PubMed] [Google Scholar]
- 2.Aprahamian C, Wittman DH, Bergstein JM, et al. Temporary abdominal closure (TAC) for planned relaparotomy in trauma. J Trauma. 1990;30:719–723. [DOI] [PubMed] [Google Scholar]
- 3.Smith PC, Tweddell JS, Bessey PQ. Alternative approaches to abdominal wound closure in severely injured patients with massive visceral edema. J Trauma. 1992;32:16–20. [DOI] [PubMed] [Google Scholar]
- 4.Mayberry JC, Mullins RJ, Crass RA, et al. Prevention of abdominal compartment syndrome by absorbable mesh prosthesis closure. Arch Surg. 1997;132:957–961. [DOI] [PubMed] [Google Scholar]
- 5.Fabian TC, Croce MA, Pritchard FE, et al. Planned ventral hernia: Staged management for acute abdominal wall defects. Ann Surg. 1994;219:643–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Miller PR, Thompson JT, Faler BJ, et al. Late fascial closure in lieu of ventral hernia: the next step in open abdomen management. J Trauma. 2002;53:843–849. [DOI] [PubMed] [Google Scholar]
- 7.Rotondo MF, Schwab CW, McGonigal MD, et al. “Damage control”: an approach for improved survival in exsanguinating penetrating abdominal injury. J Trauma. 1993;35:375–382. [PubMed] [Google Scholar]
- 8.Burch JM, Oritz VB, Richardson RJ. Abbreviated laparotomy and planned reoperation for critically injured patients. Ann Surg. 1992;215:476–484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Morris JA Jr, Eddy VA, Blinman TA, et al. The staged celiotomy for trauma: issues in unpacking and reconstruction. Ann Surg. 1993;217:576–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fernandez L, Norwood S, Roettger R, et al. Temporary intravenous bag silo closure in severe abdominal trauma. J Trauma. 1996;40:258. [DOI] [PubMed] [Google Scholar]
- 11.Bender JS, Bailey CE, Saxe JM, et al. The technique of visceral packing: recommended management of difficult fascial closure in trauma patients. J Trauma. 1994;36:182–185. [PubMed] [Google Scholar]
- 12.Tremblay LN, Feliciano DV, Schmidt J, et al. Skin only or silo closure in the patient with open abdomen. Am J Surg. 2001;182:670–675. [DOI] [PubMed] [Google Scholar]
- 13.Cuesta MA, Doblas M, Casteneda L, et al. Sequential abdominal re-exploration with the zipper technique. World J Surg. 1991;15:74–80. [DOI] [PubMed] [Google Scholar]
- 14.Meldrum DR, Moore FA, Moore EE, et al. Cardiopulmonary hazards of perihepatic packing for major liver injuries. Am J Surg. 1995;170:537. [DOI] [PubMed] [Google Scholar]
- 15.Maxwell RA, Fabian TC, Croce MA, et al. Secondary abdominal compartment syndrome: an under-appreciated manifestation of severe hemorrhagic shock. J Trauma. 1999;47:995–999. [DOI] [PubMed] [Google Scholar]
- 16.Kron IL, Harman PK, Nolan SP. The measurement of intra-abdominal pressure as a criterion for abdominal re-exploration. Ann Surg. 1994;33:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Doty JM, Saggi BH, Sugerman HJ, et al. Effect of increased renal venous pressure on renal function. 1999;47:1000–1003. [DOI] [PubMed] [Google Scholar]
- 18.Diebel LN, Wilson RF, Dulchavsky SA, et al. Effect of increased intra-abdominal pressure on hepatic arterial portal venous and hepatic microcirculatory blood flow. J Trauma. 1992;33:279–283. [DOI] [PubMed] [Google Scholar]
- 19.Chang MC, Miller PR, D'Agostino R, et al. Effects of abdominal decompression on cardiopulmonary function and visceral perfusion in patients with intra-abdominal hypertension. J Trauma. 1998;44:440–445. [DOI] [PubMed] [Google Scholar]
- 20.Garner GB, Ware DN, Cocanour CS, et al. Vacuum assisted wound provides early fascial reapproximation in trauma patients with open abdomens. Am J Surg. 2001;182:630–638. [DOI] [PubMed] [Google Scholar]


