Abstract
Summary Background Data:
Our program has emphasized broad-based training that potentially allows residents to pursue a variety of career paths, with or without additional surgical training. Diverse experiences have emphasized a variety of rotations, including a university hospital with a large trauma service, several tertiary private institutions, and suburban and rural experiences with private practitioners. Our faculty includes surgeons with both broad-based and narrowly focused practices. In light of duty-hour restrictions and proposed changes in surgical training, we assessed the results of this model over an extended period.
Materials and Methods:
The case volume from the Residency Review Committee (RRC) operative logs, ABSITE scores, ABS performance, fellowship training, and subsequent career choices were examined for all graduating chief residents in general surgery from our program over the past 17 years. The impact of specialty faculty was assessed and data from 5 index (aortic, major esophagogastric, liver, pancreatic, and pelvic resections) cases were also abstracted from the logs. A survey was then sent to all 208 of the 212 surgeons who had completed the program since 1971.
Results:
Of the 115 residents who completed training in the last 17 years, 60 pursued fellowship training and 55 went directly into general surgical practice in 20 states. Fifteen of the 29 residents who had an elective laboratory experience were among the 23 who remained in academic careers. The operative experience has been excellent (1090 ± 42 total major; 240 ± 21 surgeon chief). Experience did not vary, even though the number of graduating chiefs ranged from 5 to 8 per year, and there have been no deficiencies in RRC index cases. The addition of specialty faculty (n = 5) at various intervals promptly increased the volume of complex cases in pelvic, liver, pancreas, and vascular surgery. Since all residents promptly passed the ABS examinations, it was not possible to discern factors associated with Board performances other than broad-based training. The survey demonstrated that most continued to practice broad-based general surgery and believed that such training was highly relevant to their current practice.
Conclusions:
The provision of broad-based training with generalists and specialty faculty has allowed for excellent breadth and depth in case volume. While many residents pursued fellowships, those who did not have indeed achieved successful careers. Most continue to practice general surgery, indicating the value of complete training in this field. It will be important to monitor these outcomes as changes in residency training occur.
The case volume from the Residency Review Committee operative logs for all graduating chief residents in general surgery from our program over the past 17 years showed a broad-based experience, which was further affected positively by specialty faculty. A survey distributed to 208 of the 212 surgeons who had completed our program since 1971 showed that most had a very satisfying general surgical practice, but many had deep concerns about the present climate in medicine. Broad-based general surgical training continues to be valuable and has direct utility in providing general surgeons with the skills to address societal needs for the future.
The methods of training general surgeons in the United States have been standardized over the last half century, the result of which has been the envy of the world and the highest standards of excellence realized.1 Specialization has been driven by technologic developments, increasing sophistication, and complexity of operations, and our ability to support older, ever more ill patients through the perioperative period. The training period of at least 5 years has been the most arduous in medicine, but it has produced the overall high standard of quality that presently exists broadly today. The core areas of general surgery have been defined by the American Board of Surgery, and required elements of the training program have been clearly spelled out by the Residency Review Committee (RRC) for surgery of the Accreditation Council on Graduate Medical Education (ACGME). Certificates of additional training in vascular and pediatric surgery and surgical critical care have only been available to those who have completed training in general surgery; however, the concept of early specialist training has surfaced and some applications for such programs are now being accepted by the RRC. The physician manpower prognostications of the last 3 decades have clearly been wrong in the fact that there is an enormous demand for general surgeons,2 particularly in less urban areas, and shortages have now been predicted for the upcoming decade.3,4 However, data on practice patterns following general surgery residency training from individual programs are inherently lacking, which would help answer the question of what portion of these residents eventually practice general surgery.
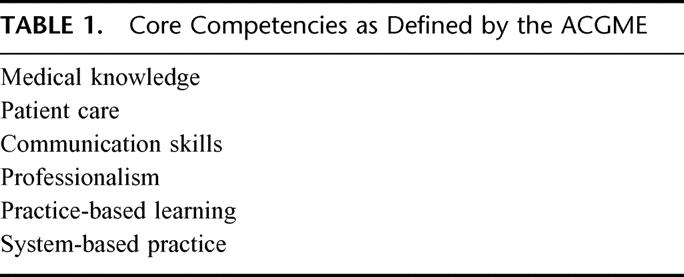
Challenges to the highly evolved modern general surgical residency training system seem to abound now, prompted by demands for increased medico-legal, political, and financial accountability and permeated by major changes in lifestyle preferences by medical graduates.1,2 Institution of the 6 core competencies by the ACGME (Table 1) for all residency programs5 has compelled program directors to alter curricular philosophy and search for appropriate evaluation tools. Restricted resident duty-hours will require increased training efficiency to accomplish the goal of training the competent general surgeon and will increase the cost of such training by the mandated hiring of physician extenders. This has been legislated in Europe by the European Economic Union to levels that seem absurd if training is to be accomplished in a meaningful time frame.6–8 To understand where we are now and how to continue to accomplish our ultimate goal of the well-trained general surgeon, we must examine the evolution of clinical training in surgery and the events that have resulted in resident work-hour limitations.
TABLE 1. Core Competencies as Defined by the ACGME
Graduate medical education has taken decades to approach uniformity across the country, particularly with regard to surgery and the surgical specialties. The American College of Surgeons was founded in 1913 with the idea of limiting performance of surgery to those properly trained and to eliminate itinerant practice.9 However, this took more than another half century and World War II to accomplish, with the founding of the American Board of Surgery in 1937 and the Residency Review Committee (RRC) for surgery in 1950. The RRCs, together with other member organizations, form the ACGME, which is responsible for the formal accreditation of individual residency programs and their sponsoring institutions. The pyramidal system essentially was phased out by applicants themselves, as these programs became less desirable. The current “rectangular system” with its built-in flexibility is well established, and although the American Board of Surgery requires only 5 clinical training years, many programs have a required laboratory year or 2 in addition to this time. Over the past decade, most hospitals have required at least completion of an accredited residency or timely certification for credentialing purposes in order for surgeons to be granted hospital privileges for particular procedures.
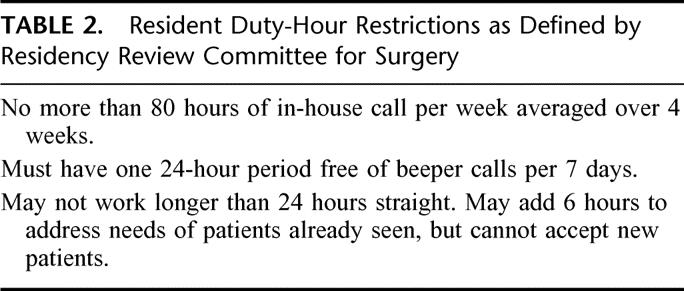
Following the death of Libby Zion,10 increased public awareness of resident working conditions, as well as political agendas, prompted the formation of a commission in New York to formally investigate this issue. Their findings resulted in the passage of legislation in New York that limits resident work hours. Subsequent institutional audits revealed violations, and penalties were levied against those institutions. The ACGME and RRC for surgery eventually adopted similar work-hour restrictions, which have been mandated as of July 1, 2003 (Table 2). We had adopted these guidelines a year earlier at the University of Louisville in an effort to more smoothly comply and study effects on our training program during this time.
TABLE 2. Resident Duty-Hour Restrictions as Defined by Residency Review Committee for Surgery
Operative case counting began in 1987, largely to measure potential competing fellowship effects on general surgery programs. This has now been standardized as a web-based program through the RRC site, but it has undergone significant refinement over this period. Boundary guidelines for number of total major operations and those performed during the chief year have been set by the RRC for surgery, and no deficiencies are allowed in any of the 15 major categories. We have strongly believed in broad-based training for general surgical residents, a philosophy melded to this program over 30 years ago. We believe that this sets the foundation for a successful lifetime of practice in general surgery, pursuit of additional fellowship training to augment this, or a focused practice in various specialty areas. In light of recent ideological changes toward general surgery residency training and reduced exposure time to its educational core, we have reviewed the operative experience of the graduating chief residents since the case-counting era began and surveyed attitudes among those who completed our program since 1971. The aim of this study, therefore, was to benchmark the operative experience of our chief residents over the last 17 years, determine the impact of new specialist faculty and fellows, and to survey the scope of and satisfaction with practice of our graduates over the past one third of a century. In particular, we were interested in what percentage practiced general surgery and the impact of fellowship training on practice pattern and development of a successful career.
MATERIALS AND METHODS
The case volume from the RRC operative logs, American Board of Surgery In-Training Examination (ABSITE) scores, ABS performance, subsequent fellowship training, and eventual career choices were examined for all graduating chief residents in general surgery from our program over the past 17 years. The impact of specialty focused faculty in general surgery was assessed by comparing the chief resident operative experience to the arrival of the faculty member, and data from 5 index (aortic, major esophagogastric, liver, pancreatic, pelvic resections) cases were also abstracted from the logs. An anonymous survey was then distributed to all surgeons who had completed the general surgery residency training program at the University of Louisville since 1971. The purpose of the survey was to determine the current scope of practice and addressed the following areas: practice affiliation and type, fellowship training, significant areas of practice, areas of Board Certification, years in practice, appropriateness of training to practice, and practice satisfaction.
RESULTS
Two hundred twelve residents completed the program from 1971 through 2003, of whom 115 completed training from June 1987 through June 2003 during the case-counting era. Of the 115 during the latter period, 60 pursued fellowship training and 55 went directly into general surgical practice in 20 states. Fifteen of the 29 residents who had an elective laboratory experience are among those who have remained in academic careers. Two thirds of these 115 trainees currently practice general surgery, and 23 have pursued academic surgical careers.
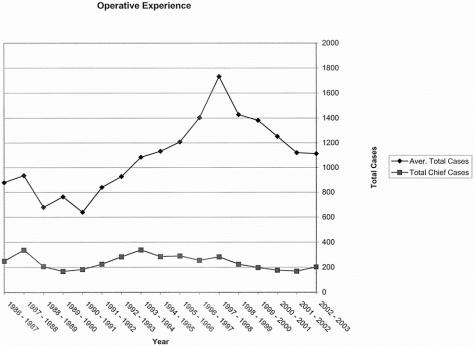
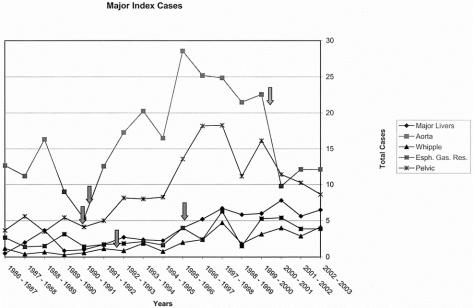
The operative experience (Fig. 1) has generally been excellent and has remained above the 90th percentile for total major cases (1090 ± 42 total major; 240 ± 21 surgeon chief). Experience did not vary, even though the number of graduating chiefs ranged from 5 to 8 per year, and there have been no deficiencies in RRC major case categories. The addition of specialty faculty in surgical oncology (1988 and 1996), colorectal (1990), vascular (1990), and hepatobiliary/ERCP surgery (1991) who developed major referral practices increased the volume of complex index cases for the residents in their several areas of expertise (Fig. 2). An example of this is the faculty person who completed an interventional biliary endoscopy fellowship overseas and returned to build up a high-volume practice of both interventional endoscopy and pancreatic surgery. The combined number of major pancreatic (distal resection, total resection, pancreaticoduodenectomy, Puestow, pseudocyst drainage) procedures from the chief resident operative logs in the 3-year period (1986 to 1989) before his fellowship was 107. In the period from 1997 to 2000, this number increased to 196. The addition of fellowships in trauma/critical care (1985), ERCP (1995), colorectal (1999), and minimal invasive (2000) did not markedly affect the operative experience of the general surgery chief residents. The departure of key faculty in vascular (1999) surgery was associated with a reduction in relevant index cases (Fig. 2).
FIGURE 1. Average total major cases and average total surgeon-chief cases per chief resident from 1986 through 2003 graduating years.
FIGURE 2. Total number of 5 major index cases (major hepatic resections, aortic procedures, major pancreatic resections, total gastrectomy and esophageal resections, major pelvic cases) per chief resident from 1986 through 2003 graduating years. Arrows indicate year in which specialty faculty began their appointment, except far right arrow denotes faculty departure.
The July 2002 introduction of the ACGME mandated resident duty-hour restrictions did not influence senior operative experience this past year. There was no correlation between operative volume/variety and scores on the ABSITE or on the qualifying examination itself. Since all residents promptly passed the ABS examinations, we could not discern positive or negative factors associated with Board performances other than broad-based training.
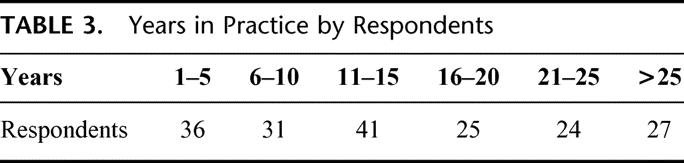
Of the 208 surveys distributed, 184 were returned. Ten surgeons had retired, and three were deceased. One hundred forty-eight were in group practice, and thirty-four had a solo practice. Two were in a missionary practice in Jamaica and Ecuador. One hundred thirty-four surgeons were in private practice, an additional ten were in a university-affiliated practice, and forty were full-time faculty in an academic setting. There was a relatively even distribution by 5-year segments of duration of practice (Table 3). Most believed that they were very well trained (161) or well trained (21), and the majority felt that they were extremely (62) or very (82) satisfied overall with their current practice. Although 26 felt only satisfied with their practice, 12 were discouraged and 2 disappointed; many others voiced unhappiness with the current state of the litigious environment, decreased reimbursement, and administrative hassles of managing all aspects of their practice.
TABLE 3. Years in Practice by Respondents
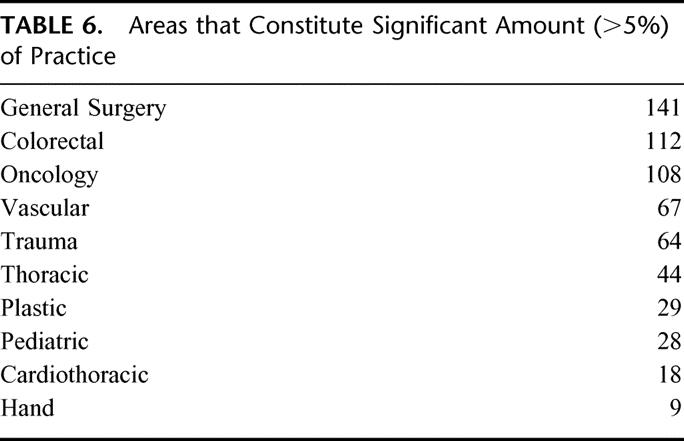
Although 104 undertook additional fellowship training (Table 4), most continued to have broad-based practices. In fact, all but 12 responders have maintained their ABS certificate in general surgery, regardless of whether their current practice included general surgery. The areas of current Board certification are listed in Table 5, and areas that constitute a significant (defined as >5%) portion of their practice are listed in Table 6. Comparison of the 2 tables demonstrates that practice patterns are, in fact, much broader than would be indicated by Board certification status alone, and that general surgical practice does indeed constitute a wide variety of areas. The top 3 areas were general, oncology, and colorectal, followed closely by vascular, trauma, and thoracic. In fact, of the 116 who considered themselves as practitioners of general surgery and responded to the question of scope of practice, 109 stated that they had either a broad-based or general practice of surgery.
TABLE 4. Surgical Fellowships Undertaken by University of Louisville Trainees (Total 104)
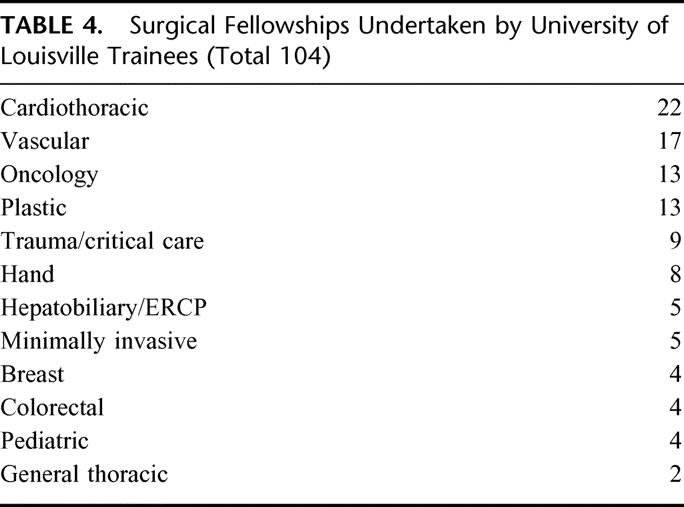
TABLE 5. Current Areas of Board Certification and Recertification
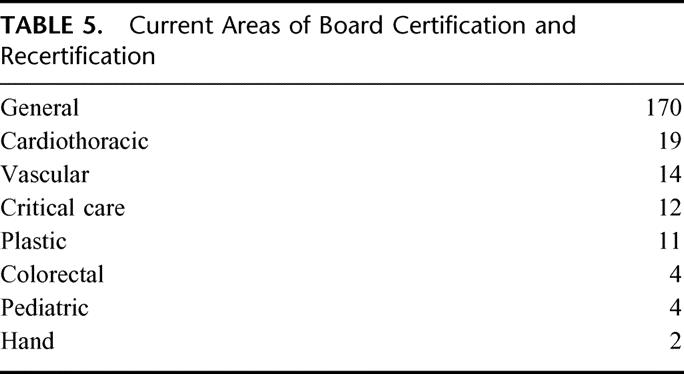
TABLE 6. Areas that Constitute Significant Amount (>5%) of Practice
DISCUSSION
Modern bedside clinical teaching had its origins during the Renaissance in Padua and then Leyden, where Hermann Boerhaave (1668 to 1738) trained many physicians during his 37-year career. Although efforts were made to standardize clinical teaching in the first 2 medical schools in the United States (University of Pennsylvania and Columbia College of Physicians and Surgeons), it remained for William Stewart Halstead to establish the first formal surgical training program at the Johns Hopkins. He had traveled to Europe and incorporated elements of the German training system, derived from Boerhaave, including its pyramidal nature, and essentially introduced the term residency in which the trainees literally resided in the hospital. The 1910 Flexner report documented the general disarray of medical education. Reform resulted in the closure of many proprietary medical schools, and major universities standardized curricula for medical students.11
Broad-based training over a defined period has been the hallmark of general surgery education in this country for a century. Numerous organizational bodies have sequentially refined such training during this time. This has resulted in preservation of most quality training programs, closing of many others, and exclusion of more of those who are not adequately trained from practicing surgery. Certification by the ABS and graduation from an RRC-accredited program in the appropriate areas of specialization is now required by most hospitals for privileges in the United States. The training is arduous and lengthy and requires an enormous time commitment by those who choose our profession. The achievement has been the high standard of quality care practiced by the overwhelming majority of surgeons in this country today, representing an enormous effort by few for the general public good of our citizens.12 However, declining medical student interest in surgical careers has continued,13,14 although the quality of this shrinking applicant pool has not allegedly deteriorated.15 Many useful suggestions to attract students into surgical careers have been recently promulgated16–18 and successful mentoring is certainly important.19
Public awareness of resident working conditions has led to increased scrutiny, resulting in the adoptions of restricted duty hours for the first time by the ACGME. Concerns over the adequate training of surgeons have been publicly debated, and many have believed that such restriction of exposure to complex disease processes over time will ultimately limit development of high quality clinical judgment.20 The duty-hours limitation has challenged residency programs to maximize educational related activity and minimize service, but, of course, the 2 are closely linked in nature. However, we must be cognitive of both student and resident perceptions about this issue, even though most are willing to work hard to achieve a meaningful clinical experience during residency,21,22 and attrition rate of surgical residents remains low at about one per residency every year.23 The consequences of these restrictions on patient care and operative experience remain to be seen. We wished to measure the operative experience of our program at this time, because this is “an end of an era,” in the fact that external regulatory forces will clearly reshape residency training.
This retrospective analysis provides a benchmark for our program in assessing future trends in our residency. The provision of broad-based training with generalists and specialty faculty has allowed for excellent breadth and depth in case volume. By extracting the 5 major index case categories from the operative logs, there is clear evidence that specialty faculty who develop referral practices lead to increased exposure to major operations for the general surgery residents. In fact, some of these cases are performed during the PGY-4 year, as these residents are chiefs on services in private integrated hospitals. Interestingly, the operative experience was similar, despite finishing differing numbers (5 to 8) of chief residents, which implies that cases are distributed throughout the final 3 years of training when the major operative experience is greatest.
One needs to recognize that there has been inherent variation over time in case-counting, as the method has evolved from a paper-based instrument into the present day web-based version. Software has also evolved over time so that portions of complex cases cannot be counted by multiple residents, and conversely certain cases are actually counted in 2 different areas. This may have led to artificial differences in year-to-year comparisons and may have accounted for some of the increases in numbers of cases seen over the past decade. The very steady baseline number of chief cases over the 17-year period would argue against this however. The addition of 4 fellowships over this time has not adversely affected the general surgical resident experience, and in fact may have augmented it, as additional cases are often scheduled because of a fellow. We have not yet seen a dramatic drop in surgeon-chief cases during the last year, despite institution of the restricted duty hours beginning July 2002, 1 year before the ACGME mandate. However, chief residents take call from home on all but the emergency general surgery/trauma/ burn service at University of Louisville Hospital, so continued monitoring of the operative experience will be required over the next decade to determine trends, as PGY-1, 2, and 3 residents routinely take in-house calls and would be most affected by the duty-hour requirements.
Changes in a residency over a third of a century may reflect many judgments, some of which proved to be clairvoyant and others less so. A conscious effort to correct a weakening of a key private hospital rotation led to a platform for innovation of very advanced surgical technologies, which now characterize an avant-garde approach to surgery in the 21st century.24
We have always believed that the breadth of general surgical training is the keystone of quality in all surgical practice.25 Individually, we doubt that shortening training under any guise, before the full impact of the duty hours reduction is assessed, is a serious mistake. Furthermore, we ask whether the general surgical residency that has a marked minority of its trainees choose to practice general surgery is indeed fulfilling its core calling adequately.
It is reassuring to have as high a response rate as we did from the survey, and even more so to find that the overwhelming majority believed their training prepared them for practice. Despite the current climate in medicine, most were very satisfied with their current practice and many have broad-based practices consistent with their general surgery training. We believe that such training best prepares one to face the clinical realities of the disease spectrum seen by surgeons; in fact, one surgeon responded that he continued to be amazed by the number of new clinical problems seen on a regular basis. While many residents pursued fellowships, those who did not have achieved innately successful careers. Most continue to practice general surgery, indicating the value of complete training in this field. Clearly, for these surgeons, the personal and professional gratification of their chosen profession and practice outweigh the challenge of contemporary medicine.
ACKNOWLEDGMENTS
We would like to thank Molly Poole, Residency Coordinator for Division of General Surgery, and other Departmental staff for their assistance in compilation of data and distribution of the survey instrument.
Discussions
Dr. Lewis M. Flint, Jr. (Tampa, Florida): I am pleased and really proud to be able to comment on this paper. This kind of academic outcomes research is clearly needed. My estimate is that fewer than 3% of the surgery training programs in the United States have clear data on the location of the practices of their graduates and the demographics and characteristics of those practices. We also need to be concerned about the long-term outcomes, particularly with regard to the imposition of work hours. I really worry that we haven't had a chance to look at that yet and we don't know what the outcome is going to be.
In informal conversations with colleagues from Europe, particularly Germany and the United Kingdom, there has been a lot of concern expressed over the competence of current graduates of training programs in those countries where there has been strict enforcement of work hours limitations.
My first question, Dr. Cheadle, has to do with the role of specialty units within the broad-based training environment. For example, you probably have read, as I did, the report from Sweden that recently appeared in the journal Surgery about the work hours limitations. Their conclusion was that to preserve clinical outcomes at a high level they have been stimulated to develop highly specialized units to which are referred, in a sort of mandatory way, patients with certain diseases. What implication do you think this has for the future practice satisfaction of these people that we are training to do very difficult, complex operations, when they may find out that in their practice environment they aren't able to do these operations?
I have some specific questions about the caseload experience and the practice profiles of the graduates. Did the practice, that is the broad-based general surgery practice of the graduates, have any relationship to the size of the community they practice in? A lot of us have heard that in order to support specialty units and specialty practices, you have to have a population of some say over 50,000, others say over 100,000. It probably varies according to the area of specialty. But was there any relationship between the ability to practice a broad-based form of general surgery and the size of the community?
Finally, was there any relationship between the broad-based surgical practice and the type of practice the person was in? We all know that people tend to practice like the group they join. So if the group placed a high value on being broad-based general surgeons, we might expect that the graduate joining that group would emulate that behavior. And I wonder if you have any data on that.
Dr. Galen V. Poole (Jackson, Mississippi): Thank you very much for the opportunity to discuss this paper. I would also like to thank Dr. Cheadle for getting me a copy of the manuscript to read several weeks ago, and then an updated copy a few days ago, which really made it very easy to prepare this presentation. Although this was presented as one paper, there are really 2 messages here and 3 independent studies. The first of those was of a review of surgery residency training at a watershed mark in our history as surgical educators. Another is the impact of specialist-trained surgical faculty on the training of what would be generalist surgeons. The third component is the practice patterns and the satisfaction of their practice of a group of surgeons, all of whom have trained at a single institution.
I think we have heard an excellent summary of the results. Basically if you have a high quality residency program with excellent leadership, faculty have been recruited and have enriched that program, you have selected good residents and have a case-rich environment, you are going to have good surgeons come out of it. Specialist-trained faculty clearly do enrich the case numbers and provide a higher complexity of cases for surgical residents. And despite socioeconomic forces that we have all have heard about, and are regarded as negative influences on the practice of surgery, most surgeons are clearly happy with what they do, at least in large measure.
Now although these issues may appear somewhat disjointed, they clearly follow a common thread. And that thread is the education of surgeons. I do have several questions for Dr. Cheadle and his group. You clearly have a very broad-based residency program. You have given your residents a very rich operative experience. And despite that, one half of them do fellowships, although a substantial proportion of those go on to practice a broad-based general surgical practice. If they have had such a good training program, then why, after 5 years, why do they have to obtain more training?
Although you have stated that the chief resident case numbers are fairly stable, if you look at that graph, there were over 300 chief resident cases per year in the 1993 cohort, whereas in the 2003 cohort it was down to 200 cases per chief resident, a rather substantial decline. I wonder if you have any concerns about that or if you feel that needs to be addressed in some way? This could also be reflected in the total case numbers, although I think that you have addressed that adequately in your presentation.
Thirdly, although work hours restrictions may not have had an early impact on resident case numbers, do you have any way to assess how they might have affected the residents’ ability to develop judgment, to provide continuity of patient care, and to develop a mature clinical decision-making process, either positively or negatively? Fourth, and this is something that I think was addressed by President Richardson's presentation this morning, if 29 of your residents went on to do an extra 1 or more years of research training, why did only 15 remain in academic surgery? What are the disincentives, and what can we do to make the practice of an academic career better for young, bright, inquisitive young men and women? With regard to physician satisfaction, did this vary by specialty training? Did it vary by years in practice? Who was the most unhappy? And why was that?
Finally—and you know this—what you have done is to have established a benchmark. The Program Committee for 2013 is going to have to have you come back with a decade follow-up to let us know if these trends are going to continue, and whether resident work hour limitations have had any positive, negative, or no ascertainable effect on residency training.
Dr. Michael J. Edwards (Little Rock, Arkansas): We stand here on the eve of the 100th anniversary of Halsted's lecture to the Yale Medical School regarding the training of a surgeon. I suggest that the principles that he espoused in that seminal paper have not changed. I was heartened as a resident interviewee, in the early 1980s, to read something Dr. Hiram Polk had written in the 1970s which said quality surgical training required, 1) appropriate patient contacts of an adequate depth and breadth; 2) committed teachers; and 3) motivated students. For more than 30 years his program has been able to attract all 3. I think you cannot analyze any of those 3 factors in isolation of the other 2. I think that sometimes we lose our way in talking about broad-based surgery, when we should, rather, talk about principle-based surgery. And frankly, principle-based surgery is what this paper is about. It is about what it takes to progressively transform a young woman or man to unwaveringly embrace a certain set of principles for a lifetime. The denominator of “time” that we have used (and it may now be, or not be, appropriate) has been 5 years. I ask you to consider, however, that we now stand at a crossroads with confounding variables such as residency work hours. I find it incredulous that we would try to manipulate too many variables at one time. Would you please elaborate in regard to the wisdom, or lack thereof in this regard?
In fact, as I serve as a new chair, having been on the job now just over 365 days, and I am impressed that those most interested in truncating general surgery residency are just those individuals that need so much more of it. They tend to be that sort of individual who wavers in principle; for example they, more often than others, fail to follow through and make sure that their patients get an adequate bowel prep and the proper prophylactic antibiotic for an elective colon resection. They tend to be those who gravitate to a specialty, not so much to be a leader, a commitment so vital to academic and private communities alike, but rather for competitive advantage. If for no other reason, maybe we ought to make their training 5 years to make sure that they specialize for the right reasons. This is perhaps not politically correct, but as you know, I am not.
Dr. Polk, Dr. Richardson, and the others found that the sub-specialists who came on board in an academic program had a profound impact on residence training. I just wonder, though, Dr. Cheadle, what do you think about the situation when you are attending a future cardiac surgeon, with a pancreatic resection, when you know that same case would perhaps be much better invested in another individual's experience? What should we do in those situations? Should we persist with the status quo?
I want to compliment Dr. Cheadle, Dr. Richardson, and Dr. Polk for personally being great leaders and teachers. I am confident that they have implemented in others, to the degree that I know they have in me, sound principles that are not only broad-based but principle-based; with specialized and committed teachers they have defined a strong foundation for the future of surgery.
Dr. John R. Potts, iii (Houston, Texas): I am going to play off a bit of what Dr. Poole said. Regardless of what the Program Committee does in 2013, I think the 2003 Program Committee should be congratulated on including this surgical education outcomes paper in our program this year.
We hear paper after paper about surgical outcomes. And yet we have all been through surgical education. Many of us participate in it on a daily basis. And I think it is high time that we have surgical education outcomes papers presented to this organization and every surgical organization on a regular basis.
I am going to talk about what I consider to be paper 2 of Dr. Cheadle's paper. Dr. Poole categorized it as paper 3. But it is the outcomes study on which I want to focus.
The authors have ably demonstrated that their broad-based general surgery training program produces individuals who practice broad-based general surgery. Of course, this is influenced to a large degree, I think, by the location of their training program, the history of their training program, and the philosophy of their program. In addition, I think it is influenced by the way in which the survey itself was constructed and worded. Nevertheless, the outcome seems quite apparent.
Perhaps as a result of that outcome, and in my opinion equally important to if not more important than that outcome, is the fact that their graduates are highly satisfied in their professional practice. Not every specialty can say that. If you survey pediatricians, internists and so forth, you will not find that degree of satisfaction. And I think their program and surgery in general are to be congratulated for keeping our graduates happy.
Now, there are many forces at work in surgical education today—Dr. Richardson talked about some of those this morning, Dr. Cheadle talked about some of them in his paper—that individually and collectively could have a devastating effect on general surgery training. We talked about the ACGME Outcomes Project. We talked about the duty hours regulation, life-style choices amongst the medical students, the decreased reimbursement and increased litigation against the faculty members, and what outcome that has on education. To those concerns I think should be added the declining financial status of the academic health centers and the fact that many of them actually are threatened with their survival, the future of federally financed medical education, which is likewise on the rocks in this country, and, of course, those calls from the derivative subspecialties of surgery who want to separate their trainees at an earlier time.
These forces are changing and will further change surgical education as we know it. I don't frankly know what surgical education will look like in America 10, 20, or 30 years from now. If I had to guess, I would guess that that education model would be one that is much more highly structured; one that is objectively oriented and competency based; one that is a graduate student model that is financially self-supporting. I think that is an important consideration—and one that is done more in the skills lab and through self-study than it is on the wards, in the clinics and in the operating rooms. In that particular model, I think it will be difficult to maintain this very broad-based surgical training. I would like to know Dr. Polk's thoughts about that.
I would also like to ask another couple of questions. First is, one of the most commonly cited shortcomings of graduate medical education in this country is a lack of preparation of our trainees for the business of surgery and the business of medicine. Now, your survey tool did not address that specific question, but I am curious whether any of the respondents addressed that with you.
Secondly, many of us in this audience are program directors. We are now challenged to produce our own outcomes research tool on our residency programs. So I would ask what advice you would give us in terms of your experience with this particular survey. What questions should we include? What questions should we add? How should we go about doing it?
Dr. Spence M. Taylor (Greenville, South Carolina): Dr. Cheadle, I enjoyed your paper very much. I am struck sitting here that this is the total opposite of what is going on in Greenville, South Carolina. It is a city of about 400,000 people where the general surgical community has basically relinquished all of their willingness to do trauma call or any other aspect of broad-based general surgery that they deem as inconvenient. The trend is to go more towards breast surgery or bariatric surgery or some other type of elective practice exclusively. We can't get them to take trauma calls, even if we pay them. It is the total opposite in your community. I wonder why?
I think we as general surgeons are our own worst enemies sometimes. We have purposely allowed ourselves to fall away from broad-based general surgery. I would just like your comments.
Dr. Hiram C. Polk, Jr. (Louisville, Kentucky): Ladies and gentlemen, we appreciate the interest in this subject and the chance to share this material with you. First of all I want to recognize that Drs. Richardson, Glen Franklin, and Bill Cheadle have contributed enormously to this. This is truly a joint effort.
First of all, this was a lifetime effort to consciously do what we thought was right for contemporary surgical residents. There is no theory about this. There is no educational grand scheme. It is what we thought was best at the time. I think Dr. Edwards made some very gracious comments that put some of this into perspective. But doing the right thing for the right reason at the right time is something that serves us all pretty well as teachers.
Secondly, I would like to speak to Dr. Flint's point about relationships with your alumni. Not only does this permit you do to do longitudinal studies like this, it provides a wonderful opportunity for ongoing fund-raising by a department. Several people in this audience are the backbone of that effort. It is not just a chance to find out who is happy and who is living where and print their grandchildren's picture in our alumni newsletter. The point is building a relationship where they seem to care about the viability of their surgical alma mater.
Dr. Flint asked about continuity of care and the duty hours issue, and that is the subject for another paper in 4 or 5 years. The theme you must recognize though from the Swedish and British studies is if you are so dumb as to complicate reducing duty hours by reducing duration of training, you are going to produce an inferior product. The Brits did that 10 years ago. The Swedes did it 5 years ago. If you want to reproduce it by shortening the duty hours and then follow that up with shortening training, we will all find out how to convert a really good product into a much less good one.
Dr. Flint asked about the size of the town and whether it influences what general surgeons do. I think you can see that to some degree is true. Our people tend to be the same whether they work in larger cities or not. Similarly, we couldn't make much comment on the nature of the group practices in which they work. There is some self-selection from groups that do broad-based general surgery and looking for more of the same.
I think Dr. Poole was correct in mentioning there are 3 messages in this. We do think that our specialist surgeons have enriched our case mix, and you can see that. Similarly, the loss of faculty in such an area can hurt education as well.
If you want to talk about the half that chose to do specialty training, realize that half chose not to. And that could be a high water mark for most of the training programs in America today. We still think that is a prideful thing to do and that our best residents are very comfortable with that plan. The same question was directed about careers in academic surgery, ie why people didn't do more? I submit to you that there are not very many residency programs that have 15% of their total graduates who have remained in academic surgery for a career. That is something of which we are proud, rather than concerned about.
Dr. Edwards made a point about principle-based training and surgery. That is a new definition, but it is a definition that ought to be studied over a long period of time.
Dr. Spence Taylor asked about local problems and local solutions. And I thought Dr. Richardson in his presidential address among many things this morning showed us how important it has been to us to build a relationship with the surgeons who practice in Louisville and in Kentucky and Indiana. They have been our principle referring doctors over time. We compete with them in some areas and we carefully don't compete with them in others. We do some things that are special and they do some things that are special. They continue to be our biggest supporters politically and financially. I actually think that is an important part of my job on an ongoing basis.
John Potts made a nice comment about the long follow-up in this. As many of you know, surgical education papers often report 12- to 18-month follow-ups for a lot of things, and that has become the norm for some educators. I think this kind of 25- or 30-year follow-up is meaningful and we are even more proud of what these surgeons have done.
Now, the history and philosophy of our faculty has been the same over a long time. We try to stay contemporary. We made modifications in the early ’90s. I am sure we will make more. The business issue was brought up. We try to teach our residents with coding and paying attention to compliance. I think nobody until their last year is really interested in the basics of surgical practice. I think the outcomes research issue was documented by Dr. Shively's presentation this morning.
The closing line in Dr. Cheadle's talk is very important. Our graduates have ongoing respect for themselves, for their teachers, and for the specialty they practice. And that is what we need in surgery in America now more than anything. I think that rather than being carried away with philosophical changes, we need to continue to let the times dictate what we want to be. We need to keep an eye on the goal of training the best possible broad-based surgeon who understands that the moral commitment to continuity of care doesn't change with duty hours and it doesn't change with fashion. Thank you.
Footnotes
Reprints: William G. Cheadle, MD, Department of Surgery, University of Louisville, Louisville, KY 40292. E-mail: wg.cheadle@louisville.edu.
Supported in part by the Center for Advanced Surgical Technologies and the Mary and Mason Rudd Surgical Teaching Endowment, Louisville, KY.
REFERENCES
- 1.Polk HC Jr. Challenges in surgical education, competencies, work hours, and workforce. Assessment and adaption. Am J Surg. 2002;184:225–253. [DOI] [PubMed] [Google Scholar]
- 2.Richardson JD. Workforce and lifestyle issues in general surgery training and practice. Arch Surg. 2002;137:515–520. [DOI] [PubMed] [Google Scholar]
- 3.Knapp R. Financing graduate medical education and limiting resident work hours: a political assessment. Am J Surg. 2002;184:187–195. [DOI] [PubMed] [Google Scholar]
- 4.Bland KI, Isaacs G. Contemporary trends in student selection of medical specialties. Arch Surg. 2002;137:259–267. [DOI] [PubMed] [Google Scholar]
- 5.Itani K. A positive approach to core competencies and benchmarks for graduate medical education. Am J Surg. 2002;184:196–203. [DOI] [PubMed] [Google Scholar]
- 6.Wallack MK, Chao L. Resident work hours: the evolution of a revolution. Arch Surg. 2001;136:1436–1432. [DOI] [PubMed] [Google Scholar]
- 7.Ihse I, Haglund U. The Swedish 40-hour workweek: How does it affect surgical care? Surgery. 2003;134:17–18. [DOI] [PubMed] [Google Scholar]
- 8.Buchler P, Kraus TW, Friess H, et al. Labor legislation in the European Union has impact on workforce management in surgical centers. Surgery. 2003;134:3–11. [DOI] [PubMed] [Google Scholar]
- 9.Davis L. Fellowship of Surgeons: A History of the American College of Surgeons. Chicago: American College of Surgeons; 1988. [Google Scholar]
- 10.Brensilver JM, Smith L, Lyttle CS. Impact of the Libby Zion case on graduate medical education in internal medicine. Mt Sinai J Med. 1998;65:296–300. [PubMed] [Google Scholar]
- 11.Bartlett RH. Teaching from patients. In: Bartlett RH, Zelenock GB, Strodel WE, et al., eds. Medical Education. A Surgical Perspective. Chelsea, MI: Lewis Publishers; 1986:133–147. [Google Scholar]
- 12.Polk HC Jr. Surgery and the ultimate public good. Ann Surg. 1989;209:505–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Polk HC Jr. The declining interest in surgical careers, the primary care mirage, and concerns about the contemporary undergraduate surgical education. Am J Surg. 1999;178:177–179. [DOI] [PubMed] [Google Scholar]
- 14.Newton DA, Grayson MS. Trends in career choice by US medical school graduates. JAMA. 2003;290:1179–1182. [DOI] [PubMed] [Google Scholar]
- 15.Cofer JB, Biderman MD, Lewis PL, et al. Is the quality of surgical residency applicants deteriorating? Am J Surg. 2001;181:44–49. [DOI] [PubMed] [Google Scholar]
- 16.O'Herrin JK, Becker YT, Lewis B, et al. Why do students choose careers in surgery? J Surg Res. 2003;114:260. [DOI] [PubMed] [Google Scholar]
- 17.Kozar RA, Lucci A, Miller CC, et al. Brief intervention by surgeons can influence students toward a career in surgery. J Surg Res. 2003;111:166–169. [DOI] [PubMed] [Google Scholar]
- 18.O'Herrin JK, Lewis BJ, Rikkers LF, et al. Medical student operative experience correlates with a match to a categorical surgical program. Am J Surg. 2003;186:125–128. [DOI] [PubMed] [Google Scholar]
- 19.Richardson JD. Surgical reminiscences: on mentoring. Arch Surg. 2000;135:1369–1370. [DOI] [PubMed] [Google Scholar]
- 20.Polk HC Jr. The fate and growth of general surgery in the United States. Langenbecks Arch Surg. 2002;387:63–66. [DOI] [PubMed] [Google Scholar]
- 21.Whang EE, Perez A, Ito H, et al. Work hours reform: perceptions and desires of contemporary surgical residents. J Am Coll Surg. 2003;197:624–630. [DOI] [PubMed] [Google Scholar]
- 22.Miller G, Bamboat ZM, Allen F, et al. Attitudes of applicants for surgical residency toward work hour limitations. J Surg Res. 2003;114:295–296. [DOI] [PubMed] [Google Scholar]
- 23.Morris JB, Leibrandt TJ, Rhodes RS. Voluntary changes in surgery career paths: a survey of the program directors in surgery. J Am Coll Surg. 2003;196:611–616. [DOI] [PubMed] [Google Scholar]
- 24.Klodell CT, Martin RCG II, Allen JW, Polk HC Jr. Advanced surgical technology experience valuable to the basic education of general surgery residents. Bull Am Coll Surg. 2001;86:11–15. [PubMed] [Google Scholar]
- 25.Richardson JD. The role of general surgery in the age of surgical specialization. Am Surg. 1999;65:1103–1107. [PubMed] [Google Scholar]