Abstract
Aim of Study:
The objective of this study was to determine the pattern of recurrence after one or more episodes of adhesive small bowel obstruction (ASBO) during a follow-up period of up to 40 years. Furthermore, we wanted to analyze possible factors with an influence on the recurrence rate and to study the magnitude of “everyday” abdominal pain among these patients.
Patients and Methods:
Hospital records of 500 patients operated on for adhesive obstruction at Haukeland University Hospital from 1961 to 1995 were studied. The patients were followed until death, loss to follow-up, or end of study (February 2002), with a median follow-up of 10 years and a maximum follow-up time of 40 years. A questionnaire was sent to all living patients to obtain information on recurrences and abdominal complaints.
Results:
The cumulative recurrence rate for patients operated once for ASBO was 18% after 10 years and 29% at 30 years. For patients admitted several times for ASBO, the relative risk of recurrent ASBO increased with increasing number of prior ASBO episodes. The cumulative recurrence rate reached 81% for patients with 4 or more ASBO admissions. Other factors influencing the recurrence rate were the method of treatment of the last previous ASBO episode (conservative versus surgical) and the number of abdominal operations prior to the initial ASBO operation. Compared to results from the general populations, more ASBO patients suffer from abdominal pain at home. Women and patients having matted adhesions have significantly more complaints about abdominal pain than men and patients with band adhesions.
Conclusion:
The risk of recurrence increased with increasing number of ASBO episodes. Most recurrent ASBO episodes occur within 5 years after the previous one, but a considerable risk is still present 10 to 20 years after an ASBO episode. Surgical treatment decreased the risk of future admissions for ASBO, but the risk of new surgically treated ASBO episodes was the same regardless of the method of treatment. People treated for ASBO seem to be more prone to experiencing abdominal pain than the normal population, especially those having matted adhesions.
Five hundred patients operated on for adhesive small bowel obstruction were followed retrospectively for up to 41 years. The pattern of recurrent obstructions relative to number of previous adhesive obstructions, and other explanatory factors, was investigated using Kaplan-Meier survival analyses. Cox regression analyses were utilized to obtain the relative risks of recurrence related to various cofactors.
The recurrent nature of adhesive small bowel obstruction (ASBO) represents a major clinical problem. Because adhesive obstruction commonly follows previous abdominal surgery,1–4 surgical treatment may seem like a paradox. However, in many patients, the obstruction will not resolve without surgery, and in others, the risk of strangulation offers the surgeon no other alternative.
The recurrence rate after an ASBO admission given in previous studies varies from 19% to 53%.5–8 Recurrence rates varies according to whether the patients were operated on or not, how the recurrence rates were calculated (ie, whether or not the length of follow-up for each patient was considered), the selection of patients for each study, and the treatment policy of the institution (early operation versus “watchful waiting”).
In a study by Miller et al,4 the number of previous ASBO episodes was a significant factor influencing the risk of having a recurrent ASBO admission. Others have found that the method of treatment (surgical or conservative) significantly influenced the risk of recurrence, with patients treated conservatively having the highest recurrence rate.7
The focus of this study was to investigate the pattern of recurrence in patients operated for ASBO. By presenting the course of disease for 500 patients followed for up to 40 years, the risk of recurrence after 1 or several ASBO episodes was studied as well as the time to recurrence. Potential factors having an impact on the risk of recurrence were studied, as were abdominal discomfort and pain among these patients.
PATIENTS AND METHODS
Five hundred patients admitted to Haukeland University Hospital for ASBO every second year from 1961 to 1995 form the basis of this study. Medical records were investigated retrospectively for 500 patients with 686 episodes of ASBO. The maximum follow-up period was 41 years. A manual recording system was used to identify patients operated on before 1972. Later, a computerized system was used.
Only patients having had at least 1 operation for small bowel obstruction caused by adhesions (ASBO) were included. Patients with other causes of SBO (irradiation injury, cancer, incarcerated abdominal wall hernia, etc.) were excluded. The study population consisted of patients in whom the index ASBO episode was surgically treated, thus ensuring the diagnosis of ASBO. All subsequent recurrent episodes of ASBO, conservatively as well as surgically treated, were included.
The diagnosis of ASBO was confirmed during surgery for those operated on. In nonsurgically treated patients, an ASBO episode was defined as an admission to hospital for a patient already treated surgically for ASBO in the past, and in whom the plain abdominal film showed obstruction. In patients for whom no description of the x-ray was found in the patients’ files, 3 of the following diagnostic criteria had to be fulfilled: presence of abdominal pain, vomiting, complete constipation (gas and feces), or the surgeon in charge giving the diagnosis of ASBO.
There are 2 hospitals in the well-defined catchment area. Our study population consisted of patients primarily operated at the Haukeland University Hospital, which admits most of abdominal emergencies. Some of these patients had recurrent ASBO episodes that were treated at the other hospital (the Deaconess Hospital Haraldsplass). For these patients, the hospital record from that hospital was also studied and the ASBO episode included. Information on death and addresses of patients was obtained from the National Peoples Registry of Norway. Every individual can be followed based on a unique 11-digit birth identification number.
The phrase “initial operation” is used for the first ASBO operation in a patient's medical history (Fig. 1). We define an “index operation” as the operation for ASBO by which the patient was selected for the study and from which we followed each patient. This operation is called the “index operation” whether or not the patient had any prior operations for ASBO. In the majority of patients, the “index operation” was the initial operation (Example I, Fig. 1). If the “index operation” was not the “initial operation” (ie, if the initial ASBO operation occurred before 1961), it was registered as episode 2 or 3 according to the number of previous ASBO episodes each patient had had (Example II, Fig. 1). A recurrence is defined as a new hospital admission for ASBO for a patient already treated for ASBO at least once. A recurrence is thus a second or later ASBO episode (Fig. 1) and is called so irrespective of treatment (surgery or conservative).
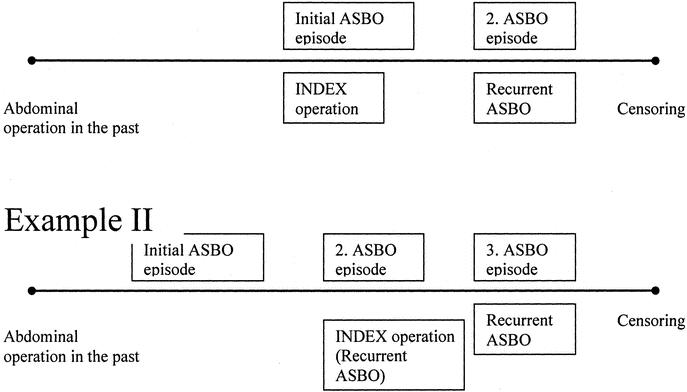
FIGURE 1. Relevant events and the terms used to describe them during a follow-up period for 2 different patient categories. Example I, Patients in whom the index operation is the initial one for ABSO (444 patients; 89% of the patients). Example II, Patients in whom the initial ABSO operation occurred during a year not included in the study (i.e., before 1961). (The index operation was not the initial operation in 56 patients; 11%).
The types of adhesions found during surgery were described as “matted” or “band” in the operation notes in 477 out of 574 episodes of ASBO (initial and recurrent) for which the patient was surgically treated. For the remaining episodes, the types of adhesions were incompletely described, although the presence of adhesions as the cause of obstruction was stated in the operation notes. The obstruction was located in the upper 1 meter of the small bowel in 6% of the cases, in the middle part in 31%, and in the lower 1 meter in 34%. The point of obstruction in the small bowel was uncertain in 29% of the cases.
When strangulated (ischemic) bowel was found and the surgeon decided that resection was required, the strangulation was referred to as “nonviable.” If the bowel was described as strangulated, but resection was not needed, the strangulation was considered to be viable. “Complications” are defined as postoperative complications and included pulmonary, cardiac, or urinary complications, thrombosis/embolism, major hemorrhage, wound infection, or rupture, abdominal abscess, and/or fistula.
“Censoring date” is defined as the date on which the follow-up was ended; death, end of study, or loss to follow-up. By the end of the follow-up period, (February 2002), 239 patients were dead and 261 were still alive. For patients who died, the end point of follow-up was the date of death.
Of the 261 patients still alive, a questionnaire was sent to 243 patients during the winter of 2001/2002 (4 patients were visitors from foreign countries and for 14 patients we were unable to obtain a correct address). Two hundred eight patients (86%) returned the questionnaires. Information about admissions to hospital for ASBO, operations for ASBO, and complaints potentially connected to the ASBO history of the patients was obtained for these patients. For all patients who returned the questionnaire, the end of follow-up was the receiving date for each letter.
For patients still alive who did not return the questionnaire, the end of follow-up was the date of the investigation of the medical record for patients living in Bergen. For those not living in Bergen (12 patients), the last admission to hospital from which we had information from the medical records, represented the censoring date.
Statistical Methods
The length of follow-up time was calculated from the index operation until censoring date. The cumulative recurrence rate for several subgroups of patients (patients with matted or band adhesions, patients having 1, 2, 3, 4, or more previous ASBO episodes, etc) was calculated using the Kaplan-Meier method (1 minus the “survival rate”).
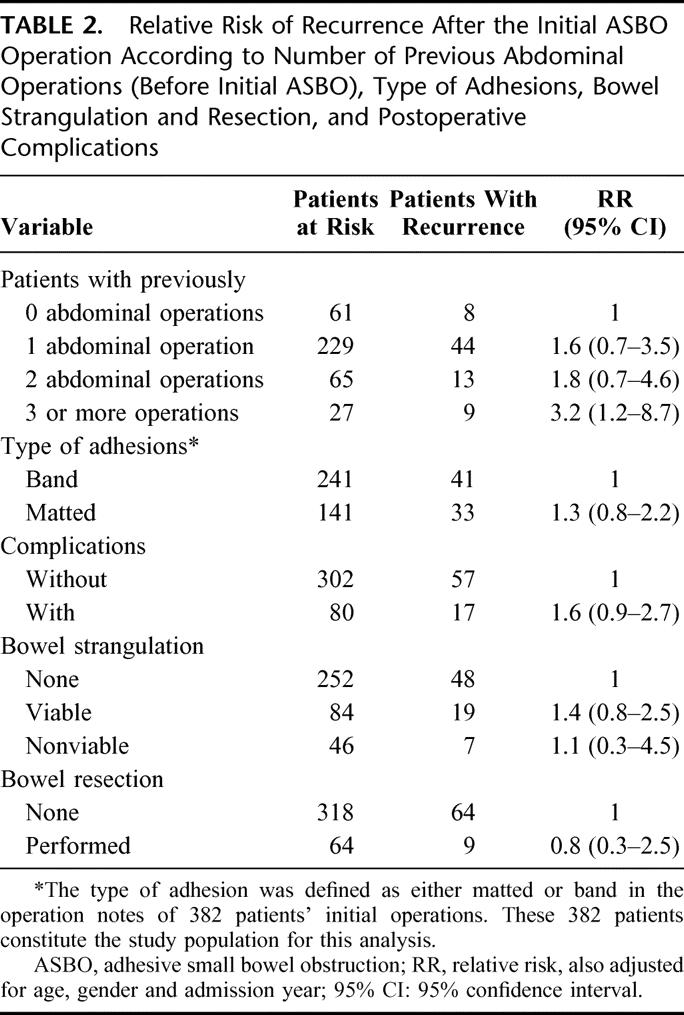
Risk factors for recurrence were analyzed using a Cox regression model. By including all ASBO incidents, we could estimate the relative risk (RR) of recurrence after 2, 3, 4, or more ASBO episodes compared with after one ASBO episode (Table 1). A separate analysis was made to study the relative risks of recurrence after the initial ASBO operation for explanatory factors connected to the ASBO operation (type of adhesions found during surgery, complications etc) (Table 2). For this purpose, only initial episodes were included in the analysis (all were treated surgically).
TABLE 1. Relative Risks of Recurrence After 1 or More ASBO Admissions (All ASBO Episodes Included)
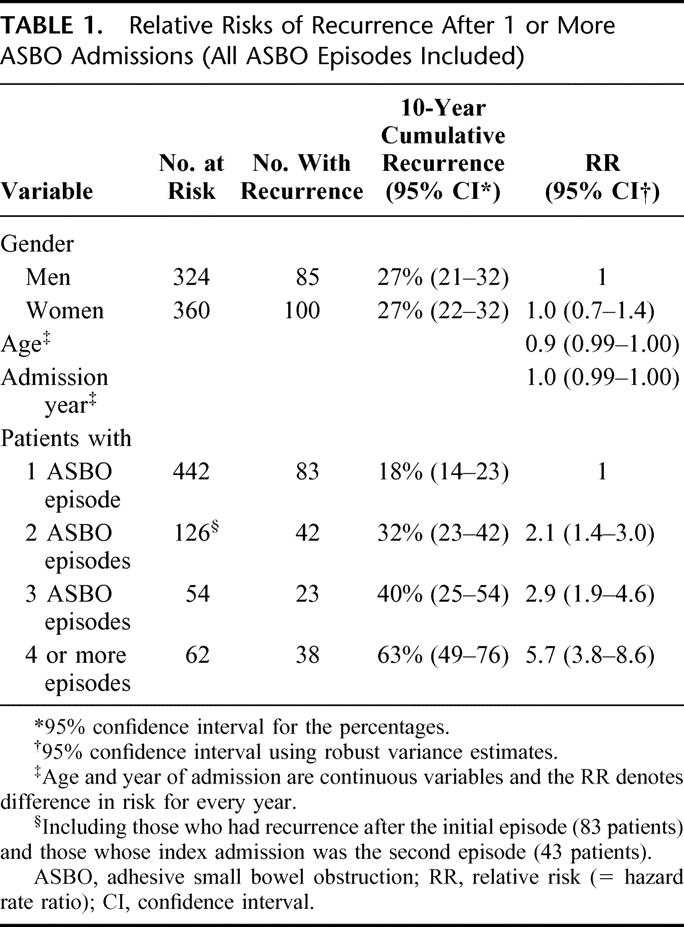
TABLE 2. Relative Risk of Recurrence After the Initial ASBO Operation According to Number of Previous Abdominal Operations (Before Initial ASBO), Type of Adhesions, Bowel Strangulation and Resection, and Postoperative Complications
To account for multiple events per patient (recurrent ASBO episodes), a marginal Cox-regression model9 was used to calculate robust variance estimates (given in Tables 1 and 3). In Table 2, only the initial operation in each patient was included, and a standard Cox regression analysis was sufficient. Checking of proportionality in the Cox regression model was done using time-dependent covariates calculated from Schoenfeld residuals9 in the S plus statistical package.
TABLE 3. Relative Risks of Recurrence According to Method of Treatment for the ASBO Episode (Surgical vs. Conservative) Adjusted for Age, Gender and Admission Year
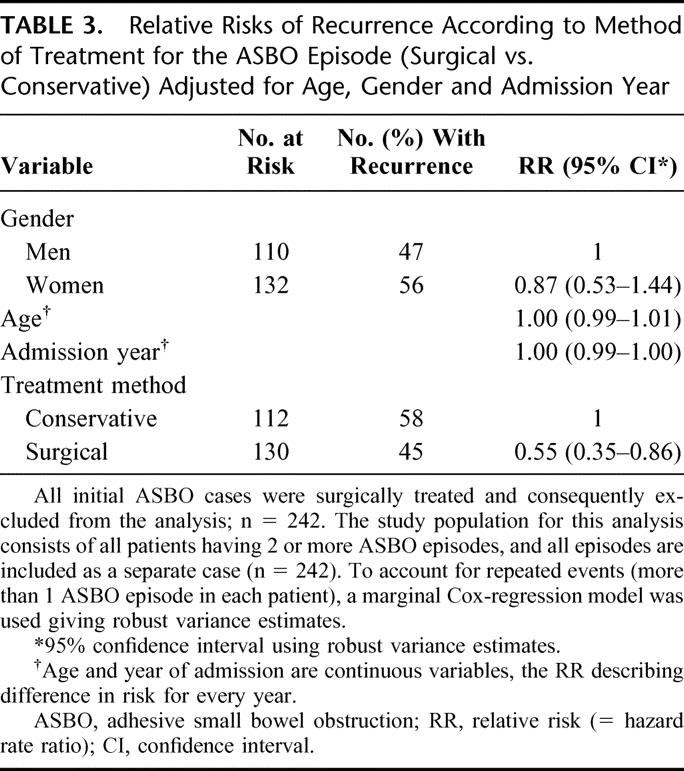
In the marginal regression analysis given in Table 3, all patients having 2 or more episodes of ASBO were included, and all these patients’ ASBO episodes were included as separate cases.
Age and admission year were included as continuous variables because categorization and the functional form of both variables showed linear behavior.9 For gender, male was used as reference in the regression analyses. The variable “previous abdominal operations” was included as a categorical variable, with “no operations” as reference category. Similarly, the variable “ASBO episodes” was included as a categorical variable with one ASBO episode as the reference category. For the variable “treatment method,” conservative treatment was used as reference and for “type of adhesion,” band adhesion was the reference category.
Analysis of the data for abdominal pain in the patient group was performed using a logistic regression analysis with abdominal pain as the dependent variable.
RESULTS
There were 240 men and 260 women, median age 56 and 55 years, respectively. The maximum follow-up time was 41 years and the median follow-up time was 11 years (mean 14). Twenty-eight percent of the patients were followed for 20 years or longer. The total number of admissions for ASBO during the study period (1961 until February 2002) was 686.
Previous Abdominal Operations
The number of previous abdominal operations occurring before the initial ASBO operation is given in Table 4. Also shown is the time interval between the last abdominal operation and the initial ASBO operation.
TABLE 4. Number of Previous Abdominal Operations Before Initial ASBO Operation and Time From Last Abdominal Operation Until Initial ASBO Operation
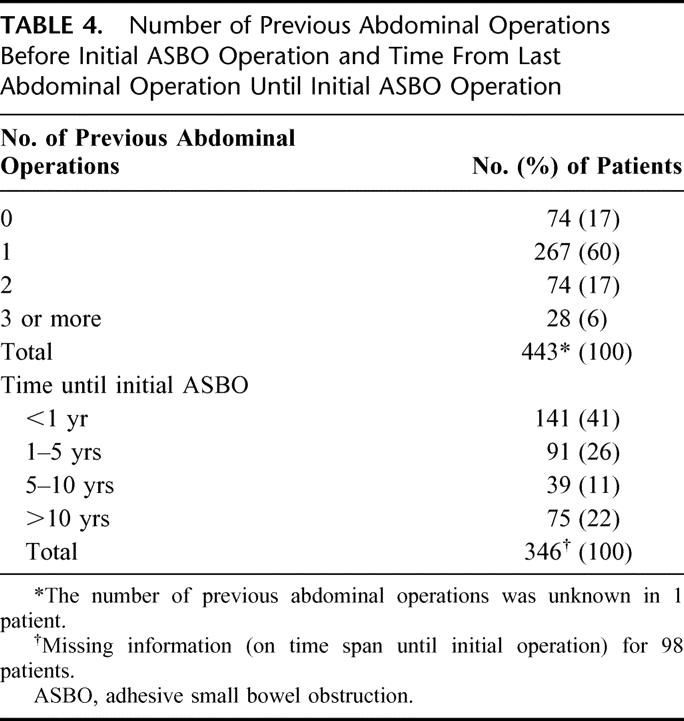
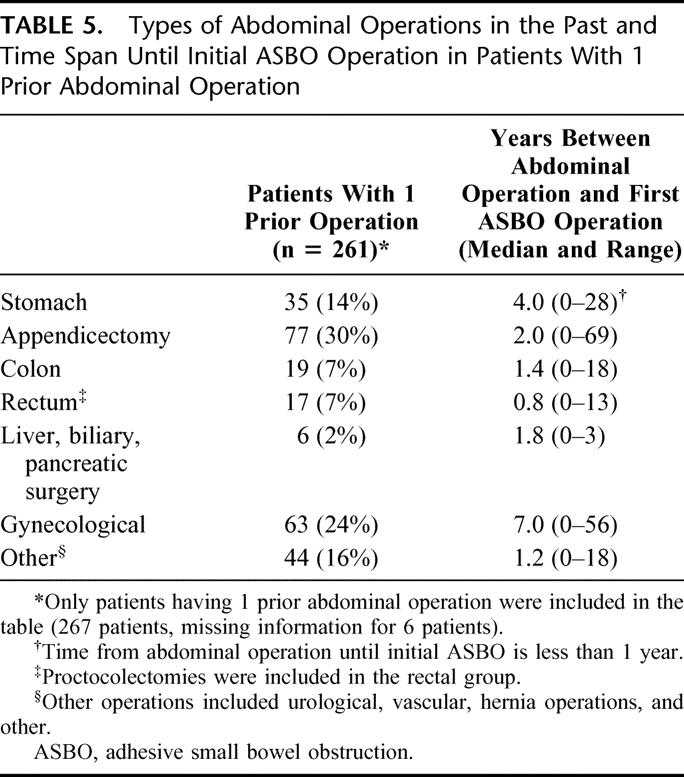
Type of previous abdominal operations and the time between such operation and the initial ASBO operation are listed in Table 5. The difference in the median time interval between the various types of operations was statistically significant (P = 0.01, Kruskal-Wallis test).
TABLE 5. Types of Abdominal Operations in the Past and Time Span Until Initial ASBO Operation in Patients With 1 Prior Abdominal Operation
Recurrence of Adhesive Small Bowel Obstruction
In Figure 2, cumulative recurrence rates are given for patients admitted once or several times for ASBO (surgically and nonsurgically treated recurrences were included). One year after an initial ASBO operation, 7% had had a second ASBO episode (surgically or nonsurgically treated) and within 10 years, 18% had had a second episode. The recurrence rate continued to increase until 29% at 25 years after the initial operation. After this point, no patient had recurrent episodes of ASBO.
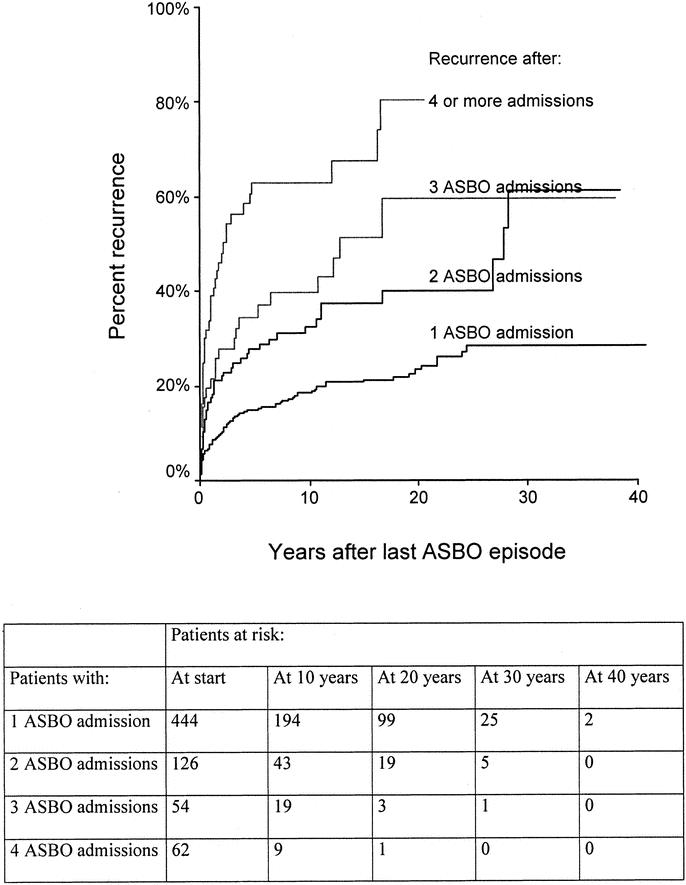
FIGURE 2. Cumulative recurrence rate after 1 or more episodes of ASBO.
Of patients with 2 admissions for ASBO (those who had recurrence after the initial episode and those whose index admission was the second episode), 17% had a third admission within the first year, 32% within 10 years, and 40% at 20 years. Of patients with 3 admissions and those with 4 or more admissions for ASBO, 19% and 33%, respectively, had a repeat ASBO within the first year and 40% and 63%, respectively, within 10 years.
Fifty percent of recurrences (occurring within our study period) appeared within the first 5 years after the initial ASBO admission (Fig. 2). The median time interval between the first and second admission for ASBO was 2 years and between second and third admission, 1.2 years. For patients having had 4 or more ASBO episodes, the median time until recurrence was 0.7 years.
In Table 1, the relative risk of ASBO recurrence according to number of previous ASBO episodes is given. The relative risk increased with the number of previous ASBO episodes. Separate analyses for ASBO operations alone, excluding the conservatively treated recurrences, also revealed a statistically significant correlation between the number of previous ASBO operations and the risk of recurrence (results not given).
The association between type of treatment (surgical versus conservative) and the risk of recurrence after 2 or more ASBO episodes is given in Table 3. We found that the risk of recurrence was significantly lower in patients when the last ASBO episode was surgically treated than when it was nonsurgically treated (RR 0.55). Subanalyses showed that the relative risk of being reoperated was the same regardless of treatment method for the last episode (RR 0.79, 95% confidence interval [CI]: 0.39–1.59). However, the relative risk of being readmitted for ASBO without being operated was significantly lower for patients treated surgically for their last ASBO episode (RR 0.42, 95% CI 0.25–0.69). Thus, surgical treatment of a recurrent ASBO episode was associated with a significantly decreased risk of having conservatively treated ASBO episodes in the future, but the need for subsequent surgery for ASBO was similar regardless of the method of treatment.
Influence of the Number of Prior Abdominal Operations, the Type of Adhesions, Bowel Strangulation and Resection, and Postoperative Complications
Table 2 shows the influence of other factors on the risk of recurrence after the initial ASBO operation. Surgically as well as nonsurgically treated recurrences were included. Patients with 3 or more prior abdominal operations before their initial ASBO operation had an increased risk of recurrence compared with those with no prior abdominal operations.
Figure 3 shows cumulative recurrence rates after the index ASBO operation, stratified for the nature of adhesions found at surgery (band or matted). Patients with matted adhesions appeared to have recurrences earlier and more often than patients only having a band adhesion (P = 0.07, log-rank test).
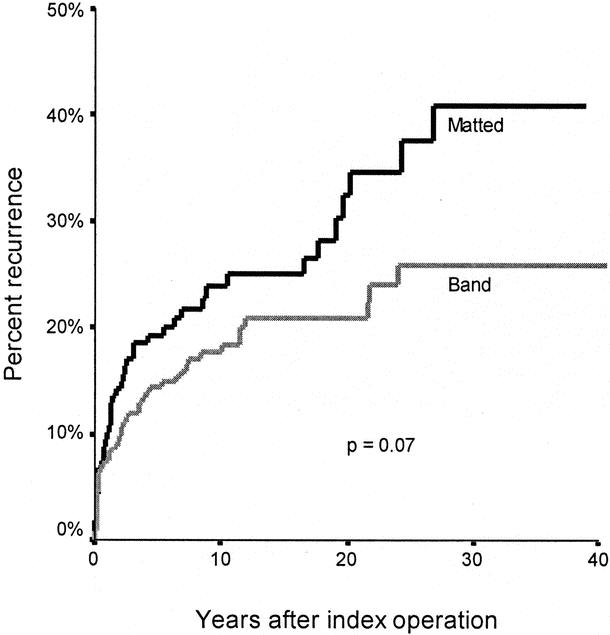
FIGURE 3. Recurrence after index operation for ASBO according to type of adhesion found during surgery.
Of all patients operated on for ASBO, 22% experienced postoperative complications. Whether or not a patient had complications did not significantly influence the risk of recurrence (Table 2). The rate of postoperative complications did, however, increase with increasing number of previous ASBO episodes; 44% of patients operated on for their third episode experienced complications versus 20% of those operated for the first ASBO episode (Table 6). Table 7 shows the crude recurrence rates after surgery for ASBO according to some important postoperative complications (wound infections, wound dehiscence, abdominal abscesses, and intestinal fistulas). The number of patients who had these complications was small, but the results suggest that the risk of recurrence is high among these patients.
TABLE 6. Bowel Resection, Bowel Strangulation, and Postoperative Complications Associated With Initial or Later Operations for ASBO
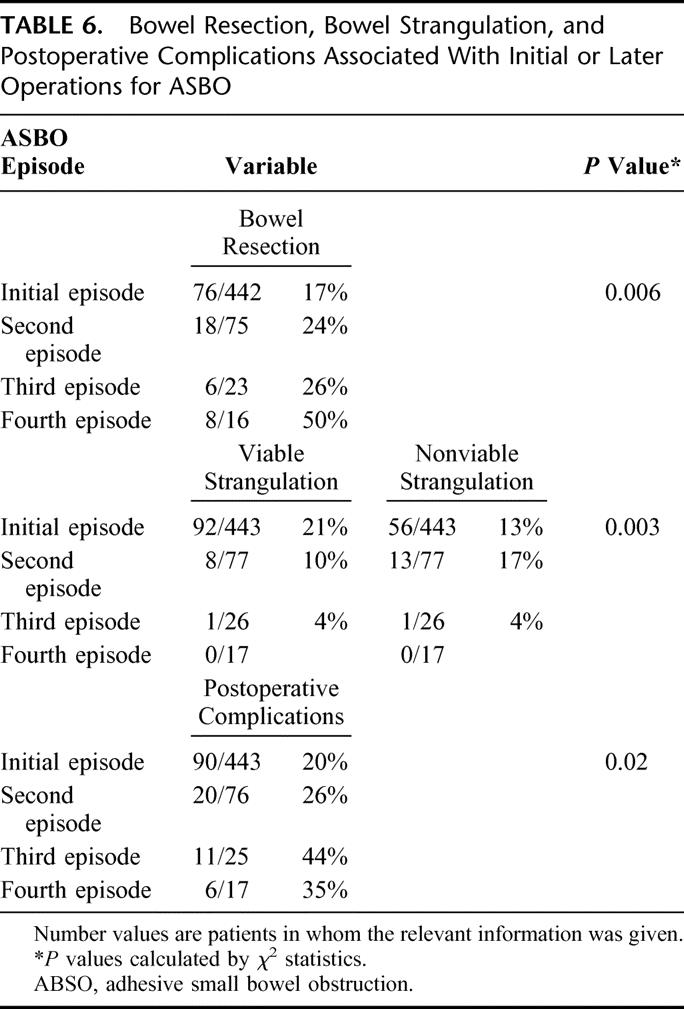
TABLE 7. Crude Recurrence Rates for Patients With Selected Postoperative Complications After Surgery for ASBO
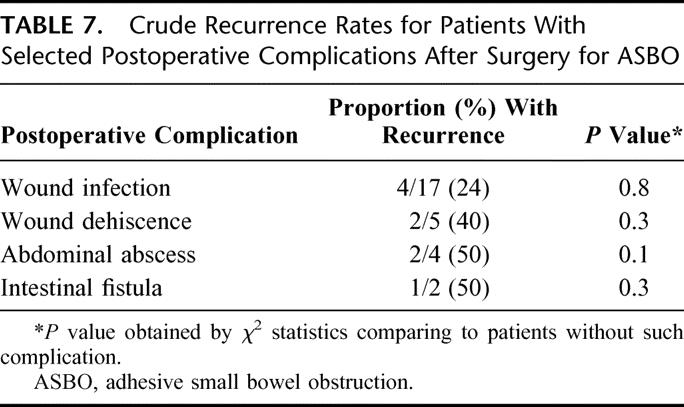
The frequency of viable and nonviable bowel strangulation was 12% and 18%, respectively, in 563 operations for ASBO for which information on this item was given in the operational notes. Bowel resection was carried out in 19% of the operations. Neither bowel strangulation nor resection influenced the risk of recurrent ASBO significantly (Table 2). The frequency of bowel resection, however, increased according to the number of previous ASBO episodes (Table 7). A patient being operated on for a third ASBO episode was thus more likely to need bowel resection than a patient operated on for his initial ASBO episode. This was not associated with more patients having bowel strangulation (Table 7). On the contrary, Table 7 shows that the frequency of bowel strangulation decreased at later episodes of ASBO.
An accidental enterotomy requiring repair occurred in 6% of the operations. Enterostomy was made in 0.8% and a colostomy in 0.2% of the operations. These variables were not included in the analysis.
Type of Prior Abdominal Operation
Recurrence rates for patients having undergone one of 4 major groups of abdominal operations are shown in Figure 4. In the analysis including all 4 groups, we found no difference in recurrence rate. However, when comparing patients having undergone appendectomy with those having had gynecologic surgery, it was revealed that patients having undergone appendectomies had a higher risk of recurrence after their index ASBO episode than patients undergoing laparotomies for gynecologic disorders (P = 0.05, log-rank test). Patients having had colonic and rectal surgery were included in the same group because Kaplan-Meier survival analyses disclosed no difference in recurrence rates between the groups (P = 0.98, log-rank test).
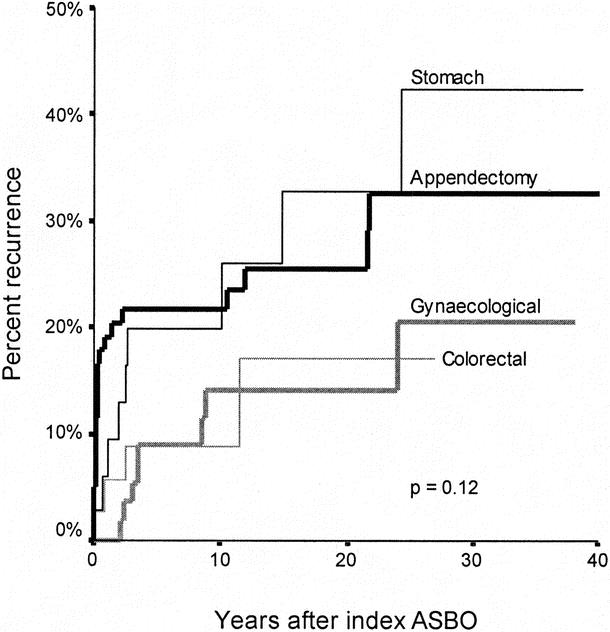
FIGURE 4. Recurrence after index ASBO operation among patients having had 1 previous abdominal operation, according to the type of operation.
Abdominal Pain Observed at Home Among Patients Treated for Adhesive Small Bowel Obstruction
Of the 208 patients who returned the questionnaire, 198 answered the part describing complaints at home (the other 10 patients only gave information on hospital admissions). Among these, 119 patients (60%) had no abdominal pain or not more than they considered normal, 66 patients (33%) had some degree of abdominal pain, and 14 patients (7%) had considerable abdominal pain. Of the 80 patients (66+14) experiencing more abdominal pain than normal, 38 described the pain as moderate, 41 as fairly strong, and 1 as very strong. Nine patients suffered from abdominal pain every day, 34 about once a week, 21 once every month, and 15 more seldom (1 did not answer that question).
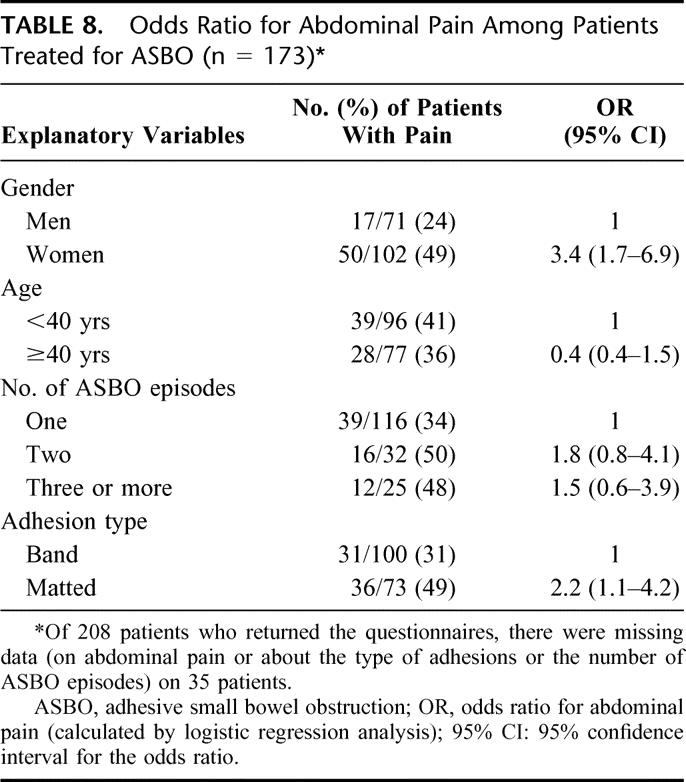
Forty-nine percent of women versus 24% of men reported abdominal pain, (odds ratio [OR] 3.4, Table 8). We found no influence of age or number of ASBO episodes on the occurrence of abdominal pain. The type of adhesion found during surgery was related to abdominal pain, the OR for abdominal pain being 2.2 (95% CI: 1.1–4.2) in patients having matted adhesions when compared with those with a band (Table 8).
TABLE 8. Odds Ratio for Abdominal Pain Among Patients Treated for ASBO (n = 173)
DISCUSSION
Abdominal surgery is known to cause formation of adhesions, which in turn may cause bowel obstruction.3,4,10,11 Surgical treatment of ASBO may lead to additional formation of adhesions, possibly contributing to recurrent episodes of ASBO.2,12
Only patients having their initial ASBO episode treated surgically were included in our study, thus ensuring a homogenous group of patient in whom the diagnosis of ASBO was reliable. In other papers addressing the same issue, both surgically and conservatively treated initial episodes of ASBO were included.4,5,7,8
In our population, the initial ASBO episode occurred within 1 year after the last previous abdominal operation in 41% of the patients and between 1 and 5 years after the last abdominal operation in 26% of the patients. This corresponds well with the study by Miller et al in which 28% of the patients presented with ASBO within 1 year and 30% between 1 and 5 years postlaparotomy.4
In a study of 309 patients with mechanical SBO, Landercasper et al7 had a maximum follow-up period of 10 years (average 4.4 years). Barkan et al8 investigated a rather small study population (90 patients) with a follow-up of up to 45 years, but the results presented concerned the first 13 years. Miller et al reported recurrence of ASBO during a 10-year period.4
In the present study, the maximum follow-up time was 41 years, and the median follow-up time was 11 years (mean 14). To our knowledge, such a long study period has not been reported before. Our results demonstrate that although the risk of recurrence is greatest during the first 5 years after an initial ASBO operation, it reaches 18% after 10 years, 23% after 20 years, and 29% at 25 years. A similar pattern was found when analyzing recurrence after 2, 3, 4, or more ASBO episodes. In our opinion, extending the follow-up period added valuable information about the rate and timing of recurrence after ASBO.
Published series report recurrence rates of 19 to 53%.5,6,8 Recurrent obstruction developed in 34% within 4 years and in 42% within 10 years in the study by Landercasper et al.7 This recurrence rate is higher than that found among our patients with one ASBO admission (19% within 10 years). Possible reasons for the discrepancy are that no differentiation between initial or later SBO episodes was made in their study, only about half the patients were surgically treated, and their study group also included patients having SBO caused by radiation injury, neoplasm, hernias, and others. Miller et al, investigating 410 patients having 675 admissions for ASBO from 1986 to 1996,4 found that 33% of the patients were readmitted for ASBO after the initial ASBO episode. The result corresponds well with that of our study, in which 29% of patients had a recurrence after their initial ASBO episode during the follow-up period.
In our study, the number of previous ASBO admissions greatly influenced the risk of readmission for ASBO. The more ASBO admissions, the higher the risk of recurrence and the shorter time until recurrence (Fig. 2, Table 1). For patients with more than 4 admissions, 63% had a recurrence within 10 years (33% within 1 year). The results correspond well with those of other studies.4,8 Landercasper et al,7 however, found no significant association between the number of previous laparotomies and obstructions and the risk of recurrence. The inclusion of patients having many different causes of SBO makes a comparison with our results difficult. The present results and those of Miller et al strongly suggest that a high number of antecedent ASBO admissions is a major risk factor for recurrence.
In the group of patients having undergone 2 or more ASBO admissions, we found that the risk of recurrence was lower after a surgically treated obstruction than after a conservatively treated one (Table 3). This finding is supported by results of other studies.5,7,8 Landercasper et al found recurrence rates of 29% and 53% for patients that did and did not undergo surgery.7 Miller et al found no difference in total recurrence rate between patients treated conservatively and those treated by operation. They did, however, demonstrate that patients treated conservatively were readmitted more rapidly than those treated surgically.4
Interestingly, we found that the difference in risk of recurrence between patients managed surgically and nonsurgically disappeared when analyzing the risk of experiencing surgically managed recurrences. Operating a patient for his ASBO did indeed reduce the risk of future hospital admissions for ASBO, but not the risk of undergoing a new ASBO operation.
Miller et al found that patients having multiple matted adhesions were more prone to be readmitted for ASBO than those having a single band were.4 In our study, the type of adhesions had no effect on the risk of recurrence (Table 2), whereas the number of prior abdominal operations did. Given a relationship between number of laparotomies and the presence of matted adhesions (shown in the study by Miller et al4 and present in our own study), it seems reasonable to believe that the finding of matted adhesions in a patient indeed increases the risk of recurrence (as suggested in Fig. 3).
Postoperative complications after ASBO surgery did not significantly influence the risk of recurrence in the present study. Another interesting finding was that bowel strangulation or the performance of bowel resection did not influence the risk of subsequent ASBO. However, the percentage of patients in need of bowel resection and the percentage experiencing postoperative complications increased according to the number of previous ASBO episodes. Thus, the results of repeated surgery for ASBO was not only an increased risk of readmission for ASBO, but also an increased risk of needing bowel resection and having complications if operation is required.
Abdominal Pain
Among the patients who returned the questionnaire, 40% experienced more abdominal pain than they considered “normal.” Of these patients, 38 judged the pain as moderate and 41 as fairly strong. The rate of reported abdominal pain differs in published series of “normal” populations. In a study of 6199 randomly selected persons, 27% reported abdominal pain in the past year,13 and 21.8% of 2510 individuals in another study reported abdominal pain or discomfort within the last month.14
In the present study, we did not ask whether or not the patients experienced abdominal pain at all, but if they had more abdominal pain than they considered normal or common. For this reason, when as much as 60% of our patients reported to have no more pain than they considered normal, we have reason to believe that some of them think that some degree of abdominal pain is normal. Thus, the 40% estimate of patients enduring abdominal pain may be too low when comparing it to “normal” population studies.13–16 Therefore, our results strongly suggest that this patient group, in addition to their high risk of being readmitted to hospital for ASBO, also suffers from more abdominal pain than the background population.
The type of adhesions influenced the rate of patients experiencing abdominal pain, the odds for abdominal pain being 2.2 for patients with matted adhesions compared with those with a band. We also found that abdominal pain was reported twice as often in women as in men. In the studies on normal populations, women similarly experienced abdominal pain significantly more often than men did.13–16 This indicates that the gender difference is associated with factors other than the ASBO operations.
In conclusion, we found that the risk of recurrence increased with increasing number of ASBO episodes. About 50% of recurrent ASBO episodes within our study period occur within 5 years of the previous one. Still, a considerable risk of recurrence was present 20 years after an ASBO episode.
Surgical treatment decreased the risk of future admissions for ASBO, but the risk of new surgically treated ASBO episode was the same regardless of the method of treatment. In addition to the pain related to hospital admissions for ASBO, these patients seem to be more prone to experiencing abdominal pain than the normal population, especially those having matted adhesions.
Footnotes
This study was supported by The Research Council of Norway.
Reprints: Dr. Bjørg-Tilde Fevang, Institute of Surgery, Haukeland University Hospital, Bergen 5021, Norway. E-mail: Bjorg.Fevang@kir.uib.no.
REFERENCES
- 1.Mucha P Jr. Small intestinal obstruction. Surg Clin North Am. 1987;67:597–620. [DOI] [PubMed] [Google Scholar]
- 2.Ellis H. The causes and prevention of intestinal adhesions. Br J Surg. 1982;69:241–243. [DOI] [PubMed] [Google Scholar]
- 3.Ræf LE. Causes of abdominal adhesions in cases of intestinal obstruction. Acta Chir Scand. 1969;135:73–76. [PubMed] [Google Scholar]
- 4.Miller G, Boman J, Shrier I, et al. Natural history of patients with adhesive small bowel obstruction. Br J Surg. 2000;87:1240–1247. [DOI] [PubMed] [Google Scholar]
- 5.Akgur FM, Tanyel FC, Buyukpamukcu N, et al. Adhesive small bowel obstruction in children: the place and predictors of success for conservative treatment. J Pediatr Surg. 1991;26:37–41. [DOI] [PubMed] [Google Scholar]
- 6.Ulvik NM, Quigstad E. Mechanical small bowel obstruction due to adhesions. Ann Chir Gynaechol. 1978;67:13–6. [PubMed] [Google Scholar]
- 7.Landercasper J, Cogbill TH, Merry WH, et al. Long-term outcome after hospitalization for small-bowel obstruction. Arch Surg. 1993;128:765–770; discussion 770–771. [DOI] [PubMed]
- 8.Barkan H, Webster S, Ozeran S. Factors predicting the recurrence of adhesive small- bowel obstruction. Am J Surg. 1995;170:361–365. [DOI] [PubMed] [Google Scholar]
- 9.Therneau TM, Grambsch PM. Modeling Survival Data: Extending the Cox Model. New York, NY: Springer; 2000. [Google Scholar]
- 10.Ellis H. The clinical significance of adhesions: focus on intestinal obstruction. Eur J Surg. 1997;(suppl 577):5–9. [PubMed] [Google Scholar]
- 11.Ellis H, Moran BJ, Thompson JN, et al. Adhesion-related hospital readmissions after abdominal and pelvic surgery: a retrospective cohort study. Lancet. 1999;353:1456–1457. [DOI] [PubMed] [Google Scholar]
- 12.Jones PF, Munro A. Recurrent adhesive small bowel obstruction. World J Surg. 1985;9:868–875. [DOI] [PubMed] [Google Scholar]
- 13.Adelman AM, Revicki DA, Magaziner J, et al. Abdominal pain in an HMO. Fam Med. 1995;27:321–325. [PubMed] [Google Scholar]
- 14.Sandler RA, Stewart WF, Liberman JN, et al. Abdominal pain, bloating, and diarrhea in the United States: prevalence and impact. Dig Dis Sci. 2000;45:1166–1171. [DOI] [PubMed] [Google Scholar]
- 15.Kay L, Jorgensen T, Jensen KH. Epidemiology of abdominal symptoms in a random population: prevalence, incidence, and natural history. Eur J Epidemiol. 1994;10:559–566. [DOI] [PubMed] [Google Scholar]
- 16.Agreus L, Svardsudd K, Nyren O, et al. The epidemiology of abdominal symptoms: prevalence and demographic characteristics in a Swedish adult population: a report from the Abdominal Symptom Study. Scand J Gastroenterol. 1994;29:102–109. [DOI] [PubMed] [Google Scholar]


