Abstract
Objective:
This study tested the hypothesis that weight-reduction (bariatric) surgery reduces long-term mortality in morbidly obese patients.
Background:
Obesity is a significant cause of morbidity and mortality. The impact of surgically induced, long-term weight loss on this mortality is unknown.
Methods:
We used an observational 2-cohort study. The treatment cohort (n = 1035) included patients having undergone bariatric surgery at the McGill University Health Centre between 1986 and 2002. The control group (n = 5746) included age- and gender-matched severely obese patients who had not undergone weight-reduction surgery identified from the Quebec provincial health insurance database. Subjects with medical conditions (other then morbid obesity) at cohort-inception into the study were excluded. The cohorts were followed for a maximum of 5 years from inception.
Results:
The cohorts were well matched for age, gender, and duration of follow-up. Bariatric surgery resulted in significant reduction in mean percent excess weight loss (67.1%, P < 0.001). Bariatric surgery patients had significant risk reductions for developing cardiovascular, cancer, endocrine, infectious, psychiatric, and mental disorders compared with controls, with the exception of hematologic (no difference) and digestive diseases (increased rates in the bariatric cohort). The mortality rate in the bariatric surgery cohort was 0.68% compared with 6.17% in controls (relative risk 0.11, 95% confidence interval 0.04–0.27), which translates to a reduction in the relative risk of death by 89%.
Conclusions:
This study shows that weight-loss surgery significantly decreases overall mortality as well as the development of new health-related conditions in morbidly obese patients.
We performed an observational 2-cohort study of morbidly obese patients who underwent weight loss surgery and nonoperated obese controls to show that a sustained 67% excess weight loss reduced the relative risk of death by 89% during the course of 5 years. In addition, there was a significant reduction in the risk of developing obesity-related conditions, such as cardiovascular, cancer, endocrine, infectious, psychiatric, and mental disorders, after the surgery. Weight-reduction surgery also decreased long-term direct health care costs.
In recent years, morbid obesity has emerged as a serious public health threat. After smoking, it is the second leading cause of preventable, premature death in the United States. It is estimated that there are 400,000 deaths attributable to obesity in the United States each year.1 The World Health Organization has recognized an epidemic of obesity throughout most of the developed and developing world.2 Canadian adult obesity trends have grown during a 13-year period from 5.6% in 1985 to 14.8% in 1998.
Obesity is associated with multiple complications and related comorbidities that lead to both physical and psychologic problems.3–6 Bariatric surgery has been shown to be an effective method for producing weight loss in obese patients in both the short and long term7–11 and to be more effective than dieting in producing sustained weight loss.12 To date, there has not been a population-based study demonstrating a significant impact of surgically induced permanent weight loss on mortality and the prevention of comorbidity in severe obesity. The current study addresses these issues by comparing the outcomes in 2 cohorts of morbidly obese patients.
METHODS
Study Design
This was an observational 2-cohort study that compared the morbidity and mortality of a cohort of morbidly obese patients treated with bariatric surgery at the McGill University Health Centre (MUHC) to that of matched morbidly obese controls who had not been treated surgically. The inception time of the bariatric cohort was the time of admission for surgery. The inception time for the control group was the date of surgery of their matched bariatric patients. A maximum of 6 controls were identified for each bariatric subject. The 2 cohorts were followed for a maximum of 5 years. The MUHC Research Institute ethics board approved the study.
Identification of Study Cohorts
A total of 1118 patients underwent bariatric surgery for the treatment of morbid obesity at the MUHC between January 7, 1986, and June 8, 2002. The unique health insurance numbers of these patients were used to retrieve their information from the provincial health insurance database of the Regie de l'assurance maladie du Quebec (RAMQ). The RAMQ database includes information regarding all health care utilization claims, including those for hospitalizations, physician visits, prescription medications, and other paramedical services. It is a single-payer system and captures all health expenditures and clinical outcomes. For example, if a patient dies in the province of Quebec, a physician must certify the death and submit an invoice to RAMQ, which is recorded in the database. This single-payer system ensures 100% clinical follow-up for both patient cohorts. Data concerning weight loss parameters for the surgically treated patients were extracted from the MUHC bariatric surgery patient registry. This registry is maintained in a prospective manner for all patients undergoing bariatric surgery.
Of the 1118 patients in the bariatric surgery cohort, 83 patients were excluded secondary to previous diagnosis and admission to hospital for 1 of the chronic conditions listed in Table 4 for the 6 months prior to surgery, identified in their RAMQ file. This does not imply that the disease condition was not present. We interpreted this to mean that the patient (for whatever reason, but not due to affordability) did not see a physician or visited a hospital for the condition. If a patient had repeat bariatric surgery, the index surgery was used as the inception date and the subsequent surgery was included in the morbidity assessment.
TABLE 4. Five-Year Morbidity and Mortality
The RAMQ database was queried to identify a maximum of 6 control subjects for each bariatric patient. The inclusion criteria for the controls were a diagnosis of morbid obesity according to the ICD9 codes (278.00, 278.01) for treatment in a hospital, treatment by a physician or as an indication for a prescription, as well as never having had surgery for the treatment of severe obesity (44.31, 44.39). Each bariatric patient was caliper matched to controls with respect to the date of the first diagnosis of morbid obesity within 2 years, age within 5 years and gender. There were a total of 6210 controls identified, of which 464 were excluded because they had been hospitalized for 1 of the chronic conditions listed in Table 4 within 6 months before the surgery date of their matched bariatric patient according to their RAMQ file. The final study sample included 1035 bariatric surgery patients and 5746 matched controls.
Surgical Procedures
The open Roux-Y (RY) Gastric bypass technique has been described previously.11,13 Since February 2002, we have been performing RY gastric bypass laparoscopically using 5 ports. We perform a hand-sewn gastrojejunostomy using a modification of Higa's technique.14 This ensures that the operation is very similar to the open RY gastric bypass, especially the creation of the very small vertically oriented gastric pouch. The time frame of this study captured the first 21 laparoscopic RY gastric bypass patients for this analysis. The technique for open vertical banded gastroplasty has been described previously.15
Determination of Outcomes
The RAMQ database was searched for all claims for health care services by subjects in both cohorts for the 5-year period after the date of inception. The ICD9 codes were used to classify the conditions leading to the use of health services.16 Morbidity was assessed using the incidence of new diagnoses during the follow-up period. Health care use during the follow-up period was measured by the number of hospitalizations, total hospital stay, and outpatient physician visits. The hospitalization and subsequent care required for the bariatric surgery was included in the total estimates of the bariatric cohort.
Weight loss for the bariatric surgery cohort was estimated using the percent change in body mass index (BMI) and percent excess weight loss. The percent change in BMI was calculated as: 100% × ([BMI0 –BMIi]/BMI0), where BMIi = the BMI at the last follow-up and BMI0 is the BMI at the time of surgery. The percent excess weight loss was calculated as: 100% × ([W0–Wi]/EW0), where W0 = the weight (kg) at the time of surgery, Wi = the weight (kg) at the last follow-up, and EW0 = the excess weight at the time of surgery. Excess weight was estimated according to the formula described by Deitel and Greenstein17 and are based on the Metropolitan Tables for middle frame individuals.
Estimation of Health Care Costs
Direct health care costs were expressed in 1996 Canadian dollars. For each subject, the total direct health care cost was estimated on the basis of the information in the RAMQ. This includes the total cost for each hospitalization, physician visit, and prescription medication. The costs for the surgery and subsequent care were included in the total cost estimates of the bariatric surgery cohort. The RAMQ costs reflect the value of the claim and are not necessarily equivalent to the costs for the services in the private sector.
Statistical Methods
The statistical significance of weight loss in the bariatric surgery cohort was assessed using the paired Student t test and was described using the mean change and 95% confidence intervals for the cohort. Differences between the bariatric surgery and control cohorts with respect to the mean number of hospitalizations, total hospital stay, and physician visits, as well as health care costs, were assessed for statistical significance with the Student t test. The incidence of chronic conditions was defined as the ratio of the number of new diagnoses during the 5-year follow up period over the total number of patients included in the cohort at inception. Relative risks with 95% confidence intervals and exact significance tests were used to assess the difference in morbidity rates between the 2 groups. Relative risks were calculated using the bariatric cohort as the exposed group and the control cohort as the reference. Therefore, relative risk estimates less than unity indicate a protective or beneficial association for the bariatric cohort. Incidence density rates for cause specific hospitalizations were calculated as events per 1000 person-years of follow-up. Rate ratios with 95% confidence intervals and exact significance tests were used to assess the between cohort differences with respect to the cause specific hospitalization rates. The between cohort difference with respect to mortality was assessed with the relative risk and the log-rank test for comparison of Kaplan–Meier survival curves.
RESULTS
Description of the Study Sample
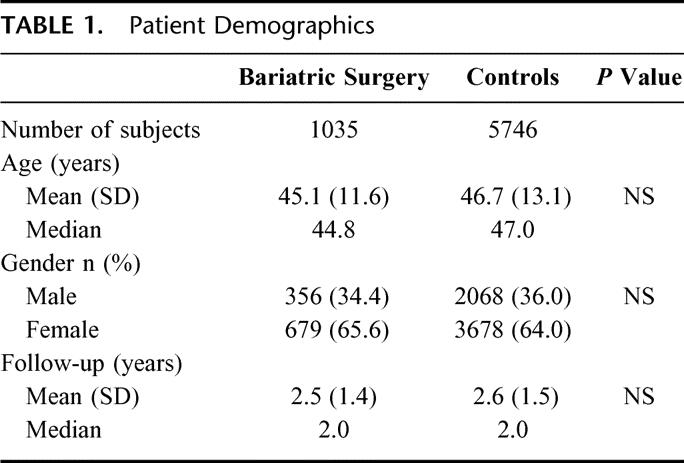
Seven different surgeons affiliated with the MUHC treated the 1035 bariatric patients during a period of 16.4 years. Four surgeons performed the majority (97%) of the procedures whereas 1 surgeon performed 48.5% of the bariatric procedures. The majority of the procedures were open RY isolated gastric bypasses (n = 820; 79.2%), followed by vertical banded gastroplasty (VBG; n = 194; 18.7%) and laparoscopic RY isolated gastric bypass (n = 21; 2.2%). Fifty-six percent were in the BMI range of 38–49, 32% in the BMI range of 50–59, 8% in the BMI range of 60–69, and the rest had a BMI > 70 (highest 98).
Thirty-five percent of the VBG patients were subsequently converted to open RY because of complications that included outlet obstruction (58%), failure to lose weight (33%), and miscellaneous reasons (9%). Table 1 describes the demographics of the 2 cohorts. There were no significant differences in age, gender, or follow-up.
TABLE 1. Patient Demographics
Weight Loss in Bariatric Surgery Patients
The data in Table 2 describe the weight loss achieved in the bariatric surgery cohort. There were significant reductions in mean percent initial excess weight loss (67.1%, P < 0.001) and in the percent change in BMI (34.6%, P < 0.001). The percent initial excess weight loss was significantly higher in patients who had undergone an open RY gastric bypass (68.7 ± 23.1) compared with VBG, especially those VBG patients who were not converted to RY gastric bypass (57.3 ± 24.8, P = 0.0000). VBG patients who were converted to RY gastric bypass achieved a percent excess weight loss of 66.3 ± 22.6, equivalent to de novo RY gastric bypass patients. Figure 1 shows the percent initial excess weight loss during the years in the surgery cohort. Our follow-up for determining the adequacy of the weight loss was good to 11 years but fell off dramatically during the next 6 years as patients relocated without leaving forwarding addresses or other contact information. Attempts to trace these patients (including the involvement of the local authorities) failed. Our patient followup is 72% complete during the 16 years of the study.
TABLE 2. Weight Loss, Bariatric Surgery Cohort
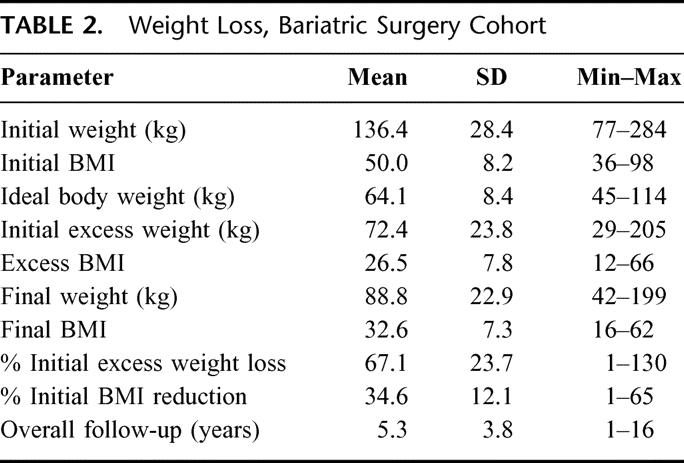
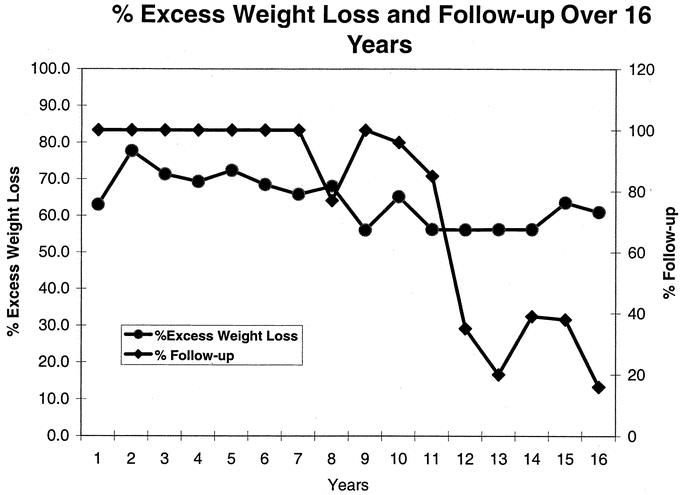
FIGURE 1. Percent initial excess weight loss by year in the surgery cohort.
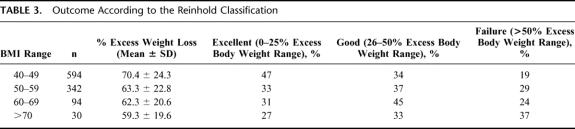
Table 3 shows the percent excess weight loss outcomes according to the modified Reinhold classification.18 Using the landmarks recently proposed by Biron et al19 for success, ie, a BMI < 35 for morbid obesity (BMI < 49) and a BMI < 40 for superobesity (BMI > 50), we achieved an 83% successful outcome in the morbidly obese patients and a 73% successful outcome in the superobese patients.
TABLE 3. Outcome According to the Reinhold Classification
Morbidity and Mortality
The data in Table 4 describe the morbidity and mortality during the 5-year follow-up period. In comparison with controls, bariatric surgery patients had significantly lower incidence rates for all the chronic conditions listed with the exception of those related to blood and blood forming organs. The most notable risk reduction was observed for the incidence of malignancies; cardiovascular and circulatory conditions, including hypertension; endocrinologic conditions, including type II diabetes; infectious diseases; and respiratory conditions. The bariatric surgery cohort patients were at increased risk for digestive disorders during the 5-year follow up when compared with controls.
The mortality rate in the bariatric surgery cohort was 0.68% compared with 6.17% for controls (relative risk 0.11; 95% CI 0.04–0.27). Mortality in the surgical group includes perioperative deaths (0.4%). Another way to describe the mortality data is a relative risk reduction of mortality of 89% by surgery that produced a sustained 67% excess weight loss, compared with no surgery controls. The Kaplan Meier survival analysis (Fig. 2) confirms that the mortality rate in the bariatric surgery cohort was significantly lower than that of controls (P < 0.001).
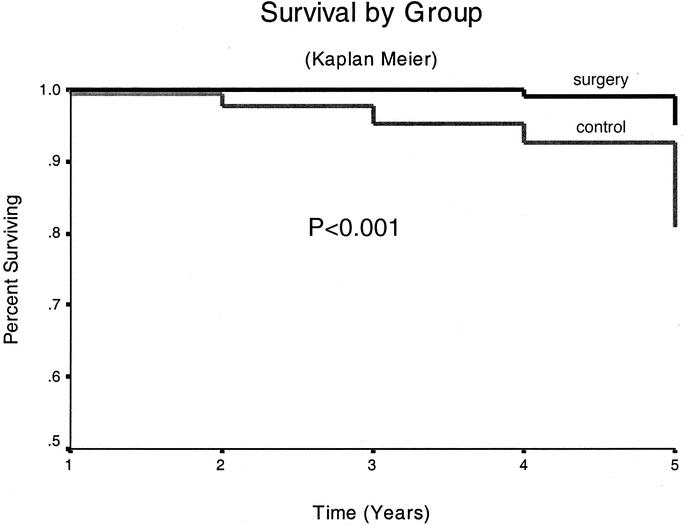
FIGURE 2. Survival by group (Kaplan Meier survival analysis).
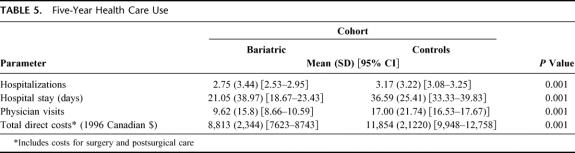
Health Care Use
The data in Table 5 show that the mean number of hospitalizations and the total in-hospital days were significantly lower in the bariatric surgery patients when compared with controls. Also, bariatric surgery patients made fewer physician visits in the 5-year follow-up period, including the planned yearly follow-up of the surgery group.
TABLE 5. Five-Year Health Care Use
The incidence rates of cause specific hospitalizations for the 2 cohorts are summarized in Table 6. The incidence rates of total hospitalizations for all individual causes were significantly lower for the bariatric surgery cohort when compared with controls. Patients in the bariatric surgery cohort had 50% fewer hospitalizations and highly significantly reduced hospitalization rates for cancers, cardiovascular, and circulatory conditions, including hypertension, infections, and respiratory conditions. The patients in the bariatric surgery cohort had significantly increased rates of hospitalizations for digestive conditions when compared with controls.
TABLE 6. Five-Year Hospitalization Rates
The mean total direct health care costs were significantly higher in the controls when compared with the bariatric surgery cohort for all specific diagnostic categories. The exceptions were the costs for digestive disorders for which the mean cost for the bariatric patients was 68% higher compared with controls. On average, the total direct health care cost for the controls was 45% higher compared with bariatric patients.
DISCUSSION
The impact of sustained weight loss in severely obese patients on mortality is unknown. The early results of the Swedish Obese Study20,21 showed that the excess health risks associated with obesity may not be fully appreciated. An interim analysis of the data reported in 200122 showed that compared with weight stability, large intentional weight loss resulted in substantial reductions in the 2-year incidence of several cardiovascular risk factors. After 8 years, there was still a reduced risk of developing diabetes in the surgical group, whereas the incidence of hypertension was equal in the 2 treatment groups. They were not able to show an effect on mortality with intentional weight loss that averaged 25.6% initial excess weight lost in their study.
We report an observational study using a combination of hospital and provincial insurance administrative databases to assess the effectiveness of bariatric surgery and to compare the mortality, morbidity and health care use in morbidly obese patients treated with bariatric surgery to a cohort of matched morbidly obese patients who were not treated surgically. The selection of patients on the basis of their exposure or treatment, without knowledge of the outcome, the inclusion only of patients who were at risk for the ascertained morbidity indicators, ie, excluding those with a history of the outcomes, and matching the controls with respect to the duration of disease and age are key elements of the study's design. These elements make the current study an excellent simulation of a prospective cohort study and a valid representation of a “real-life” situation.
The results of the current study show that for up to 16 years after bariatric surgery, patients experience significant and sustained weight loss. This result is expected and compatible with those reported in other studies. The results showing reduced mortality, reduction in the development of new comorbid conditions, and reduced health care use after surgery in combination with the demonstrated effectiveness in weight loss are unique findings of the current study.
The effects of morbid obesity on the risk for hypertension, coronary artery disease, and vascular disorders23,24; diabetes25,26; cancer27; and respiratory conditions28,29 have been well documented. In the current study, patients having undergone bariatric surgery had significantly reduced risk of developing cancer, cardiovascular disease, endocrinological disorders, infectious diseases, musculoskeletal disorders, and respiratory conditions.
The increased risk for gastrointestinal disorders in the surgery cohort was expected, and one that we feel serves as an internal consistency check of the analysis. After surgery, some patients experience stenosis of the vertical banded outlet, stenosis of the gastrojejunostomy, stomal ulcers, gastro-gastric fistula, small bowel obstructions, incisional hernias, dumping syndrome, and diarrhea.30 Thus, one expects to see increased physician visits and hospitalizations for treatment of these conditions.
Morbid obesity increases the risk for mortality.31,32 The current study demonstrates that in patients being treated with bariatric surgery, the risk of 5-year mortality is reduced by 89%. This is a significant observation because it not only suggests the role of morbidity as a risk factor for early mortality but also provides evidence that surgical treatment of obesity produces a significant reduction in mortality. We feel that the improved weight loss due to the efficacy of the RY gastric bypass and the conversion of the failed vertical banded gastroplasty patients to RY gastric bypass, which resulted in sustained initial excess weight loss of at least 67% compared with 25% initial excess weight loss in the Swedish Obese Study accounts for the observed significant reduction in mortality in our study. The majority of the surgical procedures in the Swedish Obese Study are vertical banded gastroplasty and adjustable gastric banding. Both procedures are associated with less initial excess weight loss compared with the RY gastric bypass. Benotti et al33 reported on 5178 patients with morbid obesity that underwent surgical treatment in 12 different centers and stated that “operative and late mortality rates were quite similar to observed death rates for nonobese men and women between 25–64 years of age.” MacDonald et al24 studied 232 morbidly obese patients with noninsulin-dependent diabetes and followed 154 patients who underwent a gastric bypass and 78 patients who did not have surgery (personal preference or insurance issues). The operated group mean follow-up was 9 years and the nonoperated group mean follow-up was 6.2 years. Mortality in the nonoperated group was 28% compared with 9% for the surgical group (including perioperative deaths, P < 0.0003).
Flum and Dellinger (personal communication, 2004) conducted a retrospective cohort study using the Washington State Comprehensive Hospital Abstract Reporting System database and the Vital Statistics database. They concluded from their study that a modest overall survival benefit is associated with weight loss surgery.
When compared with matched controls, the patients in our study who underwent bariatric surgery also had significantly reduced health care use rates and total direct health care costs. This finding is significant from a societal and health-economic point of view because the health care services and costs associated with surgery were included in the total costs for the bariatric surgery patients. These results have shown that on the average, the total direct health care costs for managing a morbidly obese patient may be reduced by 45% within 5 years after surgery. The total benefit would be greater if indirect costs were examined.
A potential weakness of the current study is the lack of data regarding weight loss in the controls. Severely obese patients are not likely to lose weight during a 5-year period without surgery. If they did lose weight during the 5-year period, similar to the operated patients, then the hypothesis would have to be modified, specifically that weight loss surgery exerts its therapeutic effects by a mechanisms other then weight loss. The evaluation of effectiveness for weight loss was essential in developing a comprehensive benefit profile. If the procedure did not produce significant and sustained weight loss, any other benefits with respect to the other outcomes listed would be of no consequence.
The strengths of the current study are related to the design and the selection of the cohorts. The exclusion of patients with a history of the ascertained outcomes allows the estimation of true incidence and removes potential selection bias and confounding. Matching the cases and controls with respect to age, gender, and duration of disease further reduces the possibility of confounding from these factors because both are potentially associated with the morbidity indices studied and with increased risk for mortality. The random selection of controls from an administrative database reduces selection bias and bias by indication that would have been introduced if hospital based controls were used. Despite the marked reduction in our ability to follow our patients in the Bariatric Surgery Clinic of the MUHC after 11 years, visits to other health care institutions and professionals were captured 100% in the RAMQ database (single-payer system). Although more extensive risk-benefit assessments may be useful in providing more detailed data regarding the impact of bariatric surgery, the current study has produced evidence supporting the implementation of bariatric surgery in the management of the morbidly obese patient.
ACKNOWLEDGMENTS
The authors thank M. Bouldadakis, D. Vincelli, J. L. Sylvestre, and B. Rode for their help with patient follow-up. Special thanks to the Judicial Identification Section of the Montreal Urban Community Police Department for their help in tracing patients lost to follow-up.
Discussions
Dr. Walter J. Pories (Greenville, South Carolina): As expected, the McGill group scores again with another valuable contribution to our understanding of bariatric surgery. We are delighted of course that the Canadian statistics confirm our findings at East Carolina, published in 1997, that demonstrated a mortality rate of 1% per year in diabetic patients who underwent the gastric bypass compared to a mortality of 4.5% per year in a group who were scheduled for surgery but who were canceled at the last minute for personal or insurance reasons. In the straight language of the rural South, that means the gastric bypass reduced the mortality in morbidly obese diabetics by 78%.
Before we feel too good about these statistics, however, let me remind you that we have over 8 million Americans who have a BMI >40. If they were all in 1 state, it would be the 12th largest state in the Union, larger than Virginia.
The only effective treatment for these unfortunate individuals is surgery. Even so, only 120,000 bariatric operations were done in the U.S. last year—only enough to treat one half of 1% of the individuals who need it. And most of these only after a fight with the carrier.
What if we had a pill that could provide full remission of diabetes and durable weight loss? Would it be acceptable if only half a percent of the eligible patients were treated?
There are many reasons for that failure to provide the treatment our citizens need. And we bear much of that fault. We have not always delivered the operations in a consistent, efficient, and safe manner. We have not trained enough surgeons; we have not developed the facilities to provide this complex care. We have not collected the data needed to identify which operation is best for whom. We have not exploited the great opportunities for research.
Of course, there are other reasons. Our medical colleagues are still not convinced of the merit of the surgery and insurance carriers are threatened by visions of unforeseen costs. A lot of reasons. They all add up to the same thing: Our patients are not getting the treatment they need.
Dr. Christou's demonstration that bariatric surgery reduces mortality and morbidity of our most rapidly spreading epidemic is an important lesson. Which leads to my question: How can we meet this new challenge? How can we provide bariatric surgery to more of those 8 million suffering Americans and all of those Canadians as well?
Dr. Nicolas V. Christou (Montreal, Quebec, Canada): Thank you very much, Dr. Pories, for those kind remarks.
To answer your question, we need to convince ourselves as a surgical community, as well as our primary care colleagues, as well as the administrators and others who control the purse strings, as to the value of weight loss surgery. It should be on an equal footing with cancer surgery and cardiac surgery.
We have to provide high quality care, especially bariatric peri-operative surgical care, to these patients with acceptable mortalities. More importantly, I think we need to have high quality outcome studies that demonstrate the efficacy and the cost savings to be had by this procedure, and I thank the Association for allowing us to present this particular trial. We must reduce the waiting lists not only by surgery but also by prevention. I think similar techniques that have been used to reduce mortality from tobacco use perhaps should be applied to the epidemic of the obesity as well. With all these initiatives taken together, I think we will be able to provide the care needed by these desperate patients.
Dr. Bruce M. Wolfe (Sacramento, California): The recent identification of obesity as a leading cause of death, if not the leading cause of death, in the U.S. has accentuated interest in the question: Does bariatric surgical intervention improve survival?
The importance of the present study is accentuated by the fact that a prospective, randomized trial of surgical candidates to include a “no surgery” control group has not been feasible and continues to not be feasible. It is appropriate to look at any potential differences that might exist between the 2 cohorts that have been compared in the present study.
The surgical patients are for the most part highly motivated to lose weight and improve their health. They participate in a comprehensive pre- and postoperative care program which might, for example, also stimulate diminished smoking, increased physical activity or exercise, both of which are known to enhance survival independent of body mass index. Do you have any comment on whether there might be differences between these 2 populations?
Dr. Nicolas V. Christou (Montreal, Quebec, Canada): Thank you, Dr. Wolfe, for your kind comments.
I really cannot provide that information because the database is returned to us in a blinded fashion. Also any deviation outside of the study parameters has to be pre-approved and the study redone. I think your comments are such that perhaps we can go back and reexamine the data by obtaining additional information pertaining to your question, but I do not have that data at hand presently.
Dr. Hans Jeekel (Rotterdam, The Netherlands): In Holland we have less experience because we have less obese patients, and we would like to learn from your experience.
Your conclusion is that weight loss surgery reduces mortality. Shouldn't your conclusion be that gastric bypass surgery is reduced? That is one question.
A second question, you had reduction in cancer occurrence. What kind of cancer occurrence is it? Is the follow-up low enough to evaluate the primary cancer occurrence? Or is it the occurrence of metastases, a slower recurrence of metastases at that time, or a slower growth of existing primary tumor?
And the last question, what is your next study? Will the control group be treated in some way?
Dr. Nicolas V. Christou (Montreal, Quebec, Canada): Thank you very much, Dr. Jeekel, for your kind comments. I think if we were to be purists, you are correct, most of our procedures were RY gastric bypasses; therefore, weight loss through gastric bypass surgery should be our conclusion.
As far as the types of cancers are concerned, again I cannot answer that question. Because of the way that the data is received in a highly confidential manner, et cetera, we have to go back for a subsequent analysis. We intend to do this, because the mortality differences between the two cohorts were so overwhelming. We expected to see differences in endocrinological, musculoskeletal, etc, but the cancer rates surprised us. We intend to go back and look at the specific reasons. We have the same problem with cause of death. We do not know why subjects died because of the encryption of the data.
As far as your third question in terms of the control group, we do not know their actual weights. We assume that they were morbidly obese because of the ICD9 coding. The coding is very rigorous. We also do not have any data as to weight loss in the control cohort. If the control cohort also lost weight during the observation period, we would have to modify our hypothesis at least that the benefit derived by gastric bypass may not be due to weight loss but perhaps due to other reasons.
Dr. Richard C. Thirlby (Seattle, Washington): My question was addressed just a second ago. Many databases have shown a direct correlation between body mass index and mortality. I don't believe you know the body mass index of your nonoperative control cohort. Thus, the key question in this study is, “Are they comparable BMI's?” My hunch is that the operated group has a higher mean BMI than your control arm. It would be very nice to know. Another way to address this is, do you have any information on a correlation between excess body weight loss in your surgical group and cost of care, mortality, or co-morbidities?
Dr. Nicolas V. Christou (Montreal, Quebec, Canada): Thank you, Dr. Thirlby. Very pertinent questions.
I think we have already answered the first question. As far as the excess weight loss correlations, we are continuing to do post hoc analysis of the data. As far as mortality is concerned, we will not be able to answer the question as to the minimum excess weight that will impact on mortality. We do not have enough deaths, fortunately, in the surgical cohort to do this. However, on the other co-morbidities, I think we will attempt to determine a relationship, if any, between the 2, and we hope to report this in subsequent publications.
Footnotes
Reprints: Nicolas V. Christou, MD, PhD, Room s9.30, 687 Pine Ave. W., Montreal, Quebec, Canada H3A1A1. E-mail: nicolas.christou@MUHC.McGill.ca.
REFERENCES
- 1.Mokdad AH, Marks JS, Stroup DF, et al. Actual causes of death in the United States, 2000. JAMA. 2004;291:1238–1264. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:1–253. [PubMed] [Google Scholar]
- 3.Kral JG. Morbidity of severe obesity. Surg Clin North Am. 2001;81:1039–1061. [DOI] [PubMed] [Google Scholar]
- 4.Sherwood NE, Story M. Obesity: a public health perspective. Clin Fam Pract. 2002;4:469. [Google Scholar]
- 5.Barofsky I, Fontaine KR, Cheskin LJ. Pain in the obese: impact on health-related quality-of-life. Ann Behav Med. 1998;19:408–410. [DOI] [PubMed] [Google Scholar]
- 6.Han TS, Tijhuis MA, Lean ME, et al. Quality of life in relation to overweight and body fat distribution. Am J Public Health. 1998;88:1814–1820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.O'Brien PB, Brown W, Smith A. The lap band provides effective control of morbid obesity: a prospective study of 350 patients followed up to 4 years. Obes Surg. 2000;10:233–239.10929154 [Google Scholar]
- 8.MacDonlad KG, Long SD, Swenson MS, et al. The gastric bypass: 16 year follow up. Obes Surg. 1999;9:124–129. [Google Scholar]
- 9.Linner JH. Comparative effectiveness of gastric bypass and gastroplasty. A clinical study. Arch Surg. 1982;117:695–700. [DOI] [PubMed] [Google Scholar]
- 10.Albert M, Spanos C, Shikora S. Morbid obesity: the value of surgical intervention. Clin Fam Pract. 2002;4:447. [Google Scholar]
- 11.MacLean LD, Rhode BM, Sampalis J, et al. Results of the surgical treatment of obesity. Am J Surg. 1993;165:155–162. [DOI] [PubMed] [Google Scholar]
- 12.National Institutes of Health. Very low-calorie diets. National Task Force on the prevention and treatment of obesity. JAMA. 1993;270:967–974. [PubMed] [Google Scholar]
- 13.MacLean LD, Rhode BM, Nohr CN. Late outcomes of isolated gastric bypass. Ann Surg. 2000;231:524–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Higa KD, Boone KB, Ho T, et al. Laparoscopic Roux-en-Y gastric bypass for morbid obesity: technique and preliminary results of our first 400 patients. Arch Surg. 2000;135:1029–1033. [DOI] [PubMed] [Google Scholar]
- 15.MacLean LD, Rhode BM, Forse RA. Late results of vertical banded gastroplasty for morbid obesity and superobesity. Surgery. 1990;107:20–27. [PubMed] [Google Scholar]
- 16.ICD-9-CM Official Guidelines for Coding and Reporting. Coding Clinic for ICD-9-CM 2002;19:21–71.
- 17.Deitel M, Greenstein RJ. Recommendations for reporting weight loss. Obes Surg. 2003;13:159–160. [DOI] [PubMed] [Google Scholar]
- 18.Reinhold RB. Critical analysis of long-term weight loss following gastric bypass. Surg Gynecol Obstet. 1982;155:385–394. [PubMed] [Google Scholar]
- 19.Biron S, Hould FS, Lebel S, Marceau S, et al. Twenty years of biliopancreatic diversion: what is the goal of the surgery? Obes Surg. 2004;14:160–164. [DOI] [PubMed] [Google Scholar]
- 20.Sjostrom L. Swedish Obese Subjects—an intervention study on obesity. Lakartidningen. 1988;85(8):636–9. [PubMed] [Google Scholar]
- 21.Sjostrom L, Larsson B, Backman L, et al. Swedish obese subjects (SOS). Recruitment for an intervention study and a selected description of the obese state. Int J Obes Relat Metab Disord. 1992;16:465–479. [PubMed] [Google Scholar]
- 22.Torgerson JS, Sjostrom L. The Swedish Obese Subjects (SOS) study—rationale and results. Int J Obes Relat Metab Disord. 2001;25(Suppl 1):S2–S4. [DOI] [PubMed] [Google Scholar]
- 23.Gleysteen JJ, Barboriak JJ, Sasse EA. Sustained coronary-risk factor reduction after gastric bypass for morbid obesity. Am J Clin Nutr. 1990;51:774–778. [DOI] [PubMed] [Google Scholar]
- 24.MacDonald KG, Long SD, Swenson MS, et al. The gastric bypass operation reduces the progression and mortality of NIDDM. J Gastrointest Surg. 1997;1:213–220. [DOI] [PubMed] [Google Scholar]
- 25.Pories WJ, Swanson MS, MacDonald KG, et al. Who would have thought it? An operation proves to be the most effective therapy for adult-onset diabetes mellitus. Ann Surg. 1995;222:339–350; discussion 350–352. [DOI] [PMC free article] [PubMed]
- 26.Herbst CA, Hughes TA, Gwynne JT, et al. Gastric bariatric operation in insulin-treated adults. Surgery. 1984;95:209–214. [PubMed] [Google Scholar]
- 27.Stevens J, Cai J, Pamuk ER, et al. The effect of age on the association between body-mass index and mortality. N Engl J Med. 1998;338:1–7. [DOI] [PubMed] [Google Scholar]
- 28.Sugerman HJ, Fairman RP, Baron PL, et al. Gastric surgery for respiratory insufficiency of obesity. Chest. 1986;90:81–86. [DOI] [PubMed] [Google Scholar]
- 29.Himes CL. Obesity, disease, and functional limitation in later life. Demography. 2000;37:73–82. [PubMed] [Google Scholar]
- 30.Byrne TK. Complications of surgery for obesity. Surg Clin North Am. 2001;81:1181–1193. [DOI] [PubMed] [Google Scholar]
- 31.Allison DB, Fontaine KR, Manson JE, et al. Annual deaths attributable to obesity in the United States. JAMA. 1999;282:1530–1538. [DOI] [PubMed] [Google Scholar]
- 32.Lew EA, Garfinkel L. Variations in mortality by weight among 750,000 men and women. J Chronic Dis. 1979;32:563–576. [DOI] [PubMed] [Google Scholar]
- 33.Benotti PN, Hollingshead J, Mascioli EA, et al. Gastric restrictive operations for morbid obesity. Am J Surg. 1989;157:150–155, 2065–2070. [DOI] [PubMed] [Google Scholar]