Abstract
Objective:
To evaluate in what manner ageing affects functional outcome and quality of life (QoL) in patients with chronic ulcerative colitis (CUC) after ileal pouch-anal anastomosis (IPAA).
Summary Background Data:
Short-term function and QoL after IPAA is good. However, patients are usually young, and little is known about the influence of time and ageing on long-term outcomes after IPAA.
Methods:
Using a standardized questionnaire, functional outcome, QoL, and complications were assessed prospectively in a cohort of 409 patients followed annually for 15 years after IPAA.
Results:
Follow-up was complete in the single cohort of 409 patients and functional and QoL outcomes summarized at 5, 10, and 15 years. Daytime stool frequency changed little (mean 6), while nighttime frequency increased from 1 stool to 2 stools. Incontinence for gas and stool increased from 1% to 10% during the day and from 2% to 24% at night over 15 years. The cumulative probability of pouchitis increased from 28% at 5 years to 38% at 10 years and to 47% at 15 years. Bowel obstruction and stricture were other principal long-term complications. At 15 years, 91% of patients had kept the same job. Work was not affected by the surgery in 83%, while social activities, sports, traveling, and sexual life all improved after surgery and did not deteriorate over time.
Conclusions:
These long-term results in a single cohort of 409 IPAA patients are unique and are likely a more accurate reflection of long-term outcome than has been previously reported. These data support the conclusion that IPAA is a durable operation for patients requiring proctocolectomy for CUC; functional and QoL outcomes are good, predictable, and stable for 15 years after operation.
In a single cohort of 409 ileo pouch-anal anastomosis (IPAA) patients followed for 15 years, functional outcome remained stable with a mean of 6 stools a day and 2 at night. Fecal continence was largely preserved and quality of life was excellent. IPAA is a durable operation for chronic ulcerative colitis patients requiring proctocolectomy.
Ileal pouch-anal anastomosis (IPAA) is the surgical treatment of choice for patients requiring proctocolectomy for chronic ulcerative colitis (CUC), because the goals of eliminating disease and preserving fecal continence are achieved in the great majority of patients. Over the past 2 decades, several analyses from this1–4 and other institutions5–8 have shown that IPAA is a safe and effective operation for patients with CUC; bowel functional generally is acceptable, and quality of life (QoL) is good and comparable to that of the general population.9 However, these observations are based for the most part on the results of gathered within 5 to 8 years of operation among groups of patients followed for variable lengths of time. Whether these outcomes remain durable is unknown. Furthermore, follow-up in IPAA patients must still be considered short term, as most of the patients undergoing pouch surgery are young and have life expectancies of another 40 to 50 years.
Our aim, therefore, was to evaluate functional outcome and QoL in a single cohort of patients with CUC followed annually for 15 years after IPAA. Such a longitudinal study of outcomes, in which the same patients are followed sequentially over time, provides a unique set of data which should provide a clear picture of the effect of time and ageing on the function of ileal pouches.
PATIENTS AND METHODS
During the 20-year period between January 1981 and December 2001, 1885 patients underwent IPAA for CUC at the Mayo Clinic. For 409 of the 1885 patients, annual follow-up was complete for 15 years. By definition, this cohort of IPAA patients all had intact functioning pouches throughout the period of follow-up. Success of the operation, measured by rate of pouch retention, was thus 100%. A conventional outcome report from this institution documented that among all patients operated upon for CUC, approximately 92% of patients retained a functioning pouch for up to 15 years.1
Data files were created for each patient in which all preoperative, postoperative, and follow-up information was recorded prospectively. Preoperative data recorded included stools per day and sexual function, while the follow-up data recorded stool frequency, degree of continence, ability to discriminate stool from gas, use of medications and pads, and sexual and urinary abnormalities. Follow-up began 1 year after closure of the ileostomy and was conducted yearly by questionnaire. Follow-up was conducted by a data clerk and statisticians; surgeons did not participate.
QoL data were recorded using techniques established by us several years ago.10 Patients were asked to enumerate in what manner the operation affected several “activity” or “performance” categories. The categories were sports, sexual, social activities, recreation, work around the house, family relationships, and travel.
Although it remains difficult to quantify and to define precisely, fecal incontinence during the day and night was recorded as never, occasional (1–2 episodes per week) or frequent (more than 2 episodes per week). Pouchitis is a poorly understood syndrome characterized clinically by increased frequency of loose, watery, and sometimes bloody stools; fecal urgency; incontinence; lower abdominal cramping; malaise; and fever. In our practice, although it is preferable to endoscope and biopsy patients suspected of having pouchitis, we continue to determine that a patient has pouchitis if symptoms are present for 2 to 3 days and those symptoms are alleviated promptly (less than 24 hours) by administration of metronidazole or ciprofloxacin.1,4
Nearly all patients underwent a 2-stage operation. The first stage consisted of abdominal colectomy, complete mobilization of the small bowel mesentery, and complete rectal mobilization using a close rectal resection technique.4,11 The terminal 24 to 30 cm of ileum was used to construct a stapled ileal reservoir. The IPAA was then completed either by excision of the anal transition zone (ATZ) and hand sewing the pouch to the anal canal or by preserving the ATZ and double-stapling the pouch to the anal canal. A diverting ileostomy was performed in 98% of patients. Details of both hand-sewn and double-stapled IPAA as performed at our institution is provided in Reilly et al.12 The second stage of the operation, that is, closure of the diverting stoma, was accomplished 2 to 3 months later (10 patients had a 1-stage procedure).
Statistics
Summary data are presented as mean (range) for continuous variables and percentages for discrete variables. The endpoints of primary interest were compared among the 1-, 5-, 10-, and 15-year follow-up time points. Outcomes composed of binary variables were compared using Cochran's Q statistic. Endpoints that were ordinal or continuous in nature were compared among the 4 time points using Friedman's procedure. Specific complications were analyzed as time-to-event outcomes. Specifically, the cumulative probability of remaining free of specific complications was estimated using the method of Kaplan and Meier. All statistical tests were 2-sided, and P values less than 0.05 were considered significant. The analysis was performed using SAS version 8.2 (SAS Institute Inc., Cary, NC) and Splus (Insightful Corporation, Seattle, WA).
RESULTS
Follow-up was completed at yearly intervals for 15 years in all 409 patients. The mean age of the patients was 33 years (range 14–62) at the time of ileoanal anastomosis. There were 218 men and 191 women. The mean number of stools per day before ileoanal anastomosis was 9 (1–30). Sexual activity before the operation was graded as normal in only 62% of patients, as reduced because of the disease in 20%, and as absent in 18%. Among the 409 patients, 16 had a diagnosis of indeterminate colitis made intraoperatively, and 11 had a diagnosis of Crohn's disease made at some point subsequent to IPAA.
Functional Outcome
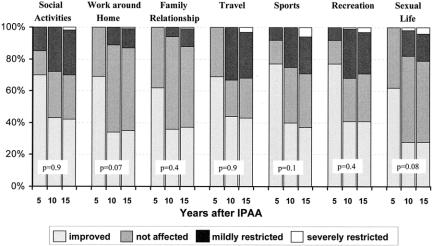
Table 1 summarizes functional outcomes in 409 patients at 1, 5, 10, and 15 years after IPAA. Stool frequency during the day increased from a mean of 5.5 at 1 year to 6.2 at 15 years. Although this was a statistically significant increase, the biologic or clinical significance was likely minimal. The clinical significance of the increase in nighttime stool frequency from 1.1 to 2.0 may be more substantial, however.
TABLE 1. Functional Outcome in 409 Patients at 1, 5, 10, and 15 Years of Follow-up
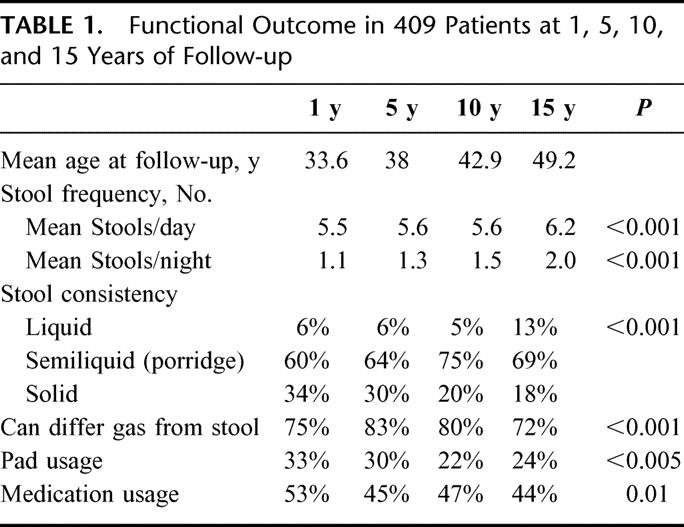
More important, perhaps, is the incontinence data; whereas at 1 year 81% of patients never experienced any daytime fecal incontinence, by 10 years that percentage had dropped to 55% and remained at 55% until 15 years (Fig. 1). This decrease in perfect continence was accompanied by an increase in only occasional and not frequent episodes of daytime fecal incontinence. Fecal incontinence at night also worsened over time; whereas 47% of patients never had incontinence at 1 year, this decreased to only 24% by 15 years (Fig. 1). Unlike daytime incontinence, however, this decrease in perfect continence was accompanied by an increase in frequent fecal incontinence. Interestingly, the percentage of patients recording their stools as being liquid doubled over the 15-year period (6% to 13%), while the percentage who described their stool as solid decreased from 34% to 18%.
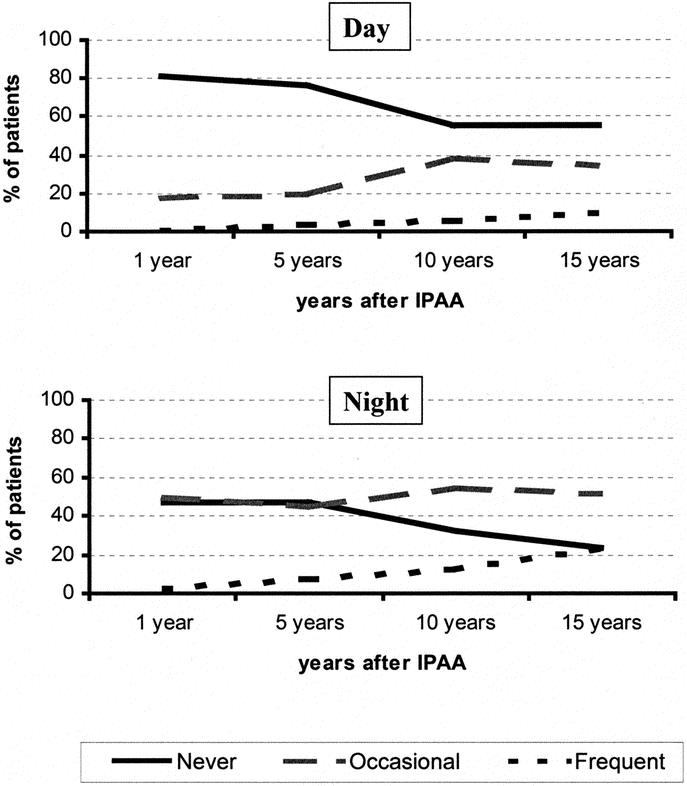
FIGURE 1. Daytime and nighttime fecal incontinence by years after IPAA. Never, perfect fecal continence; occasional, fecal spotting on underclothes, 1–2 episodes per week; frequent, more than 2 episodes per week. Data points are connected for illustration purposes.
Despite these changes, the use of medications to alter transit (stool bulking agents, Loperamide Lomotil and Questran) remained stable at about 50% of patients throughout the follow-up. Importantly, the ability of the patients to discriminate stool from gas remained constant as well (Table 1).
Complications
The principal ongoing complication after IPAA was pouchitis. Among these 409 patients, 47% had at least 1 episode of pouchitis by 15 years after operation (Fig. 2). The probability of other pouch-related complications is shown in Figures 3 and 4. Stricturing of the anastomosis occurred in 21% of the patients at some point in their follow-up. Usually, these occur early and are dealt with easily by simple dilatation. Chronic stricture is a continuing problem in about 8% of patients. Pelvic sepsis occurs in 1 of 2 settings: (i) early in the postoperative course, which is likely secondary to an operative complication; or (ii) at some point removed in time from the operation, the cause likely being related to Crohn disease. Small bowel obstruction is a common and continuing complication in patients after ileoanal anastomosis and, indeed, after any operation which removes the colon. Episodes of obstruction occurred in 25% of this patient cohort.
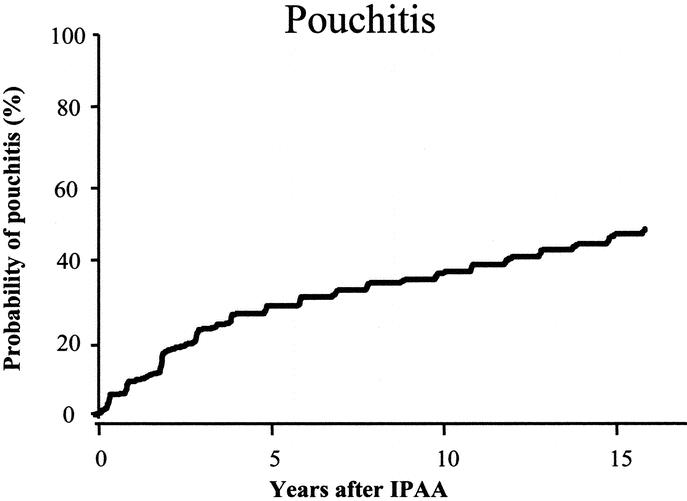
FIGURE 2. Kaplan-Meier curve depicting the probabilities of developing pouchitis by years after IPAA.
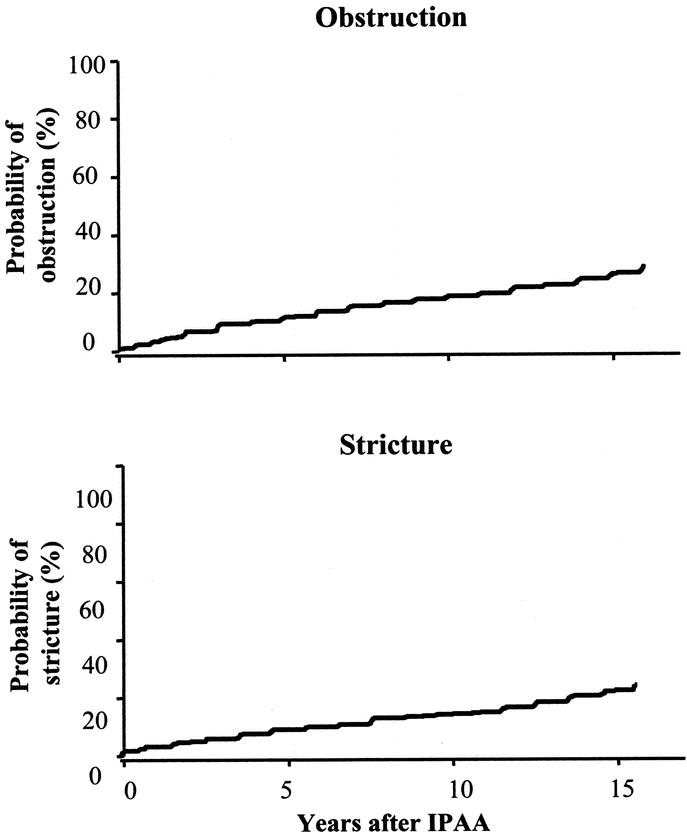
FIGURE 3. Kaplan-Meier curves depicting the probabilities of obstruction and stricture by years after IPAA.
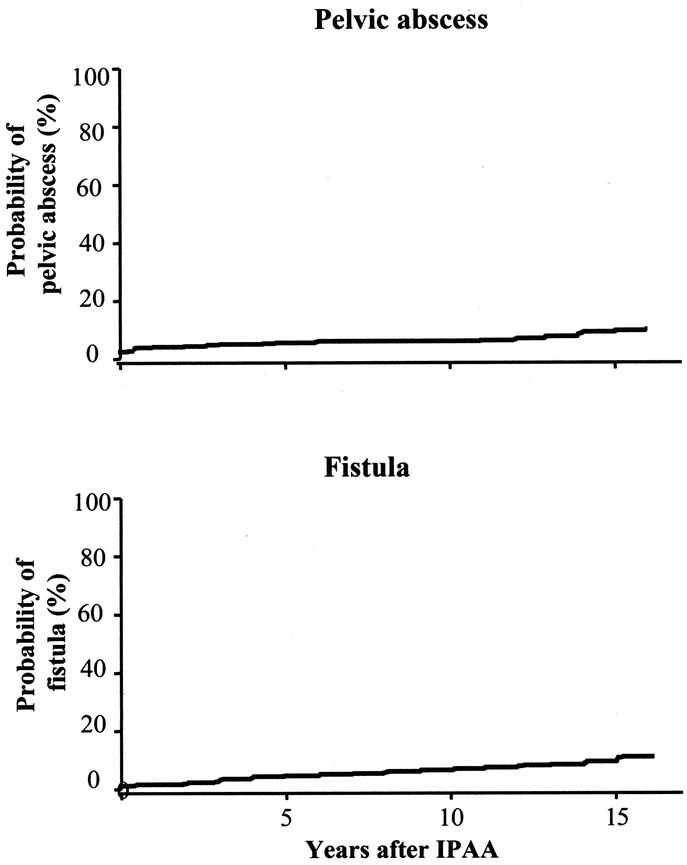
FIGURE 4. Kaplan-Meier curves depicting the probabilities of developing pelvic abscess and fistula by years after IPAA.
QoL and Satisfaction
Social activities, sports, traveling, recreational activities, family relationship, work around home, and other activities did not deteriorate over time (Fig. 5). Sexual activities were not restricted at 5 years, but by 10 and 15 years after IPAA, mild restriction were reported by 16% and 17% and severe restriction by 2% and 4%, respectively. Grouped by gender, no difference was noted at 5 and 10 years, but at 15 years of follow-up, more men than women reported severe sexual restriction (6% men versus 2% women), whereas more women were only mildly restricted (14% men versus 20% women, P = 0.03). At 5, 10, and 15 years, 100%, 95%, and 91%, respectively, of patients had kept the same job, and work was not affected by the surgery in 85%, 91%, and 83%, respectively. Diet was unchanged in 61% of patients or slightly more restricted in 39% at 15 years of follow-up.
FIGURE 5. Comparison of QoL results in several areas of daily activities at 5,10, and 15 years after IPAA.
DISCUSSION
The influence of age on pouch function has been evaluated in several studies comparing patients of different ages at the time of surgery. Outcomes were equivalent in younger (<45 years) and older patients (>65 years).1,5,13,14 Furthermore, subanalysis of patients over 70 years of age at surgery showed IPAA may be an acceptable surgical option for selected, healthy, motivated septuagenarians who are eager to preserve fecal continence.15 However, the small number of older patients in these various series has prevented an accurate assessment of the functional outcome and QoL after IPAA, particularly with ageing, as evaluations have been made at 1 time point only after IPAA and length of follow-up between younger and older patients differ. Most studies only report mean follow-ups of 4 to 6 years, with few patients followed for long periods of time. Tulchinsky et al16 reported upon 183 patients (29% of total) who had been followed for 10 years, while Michelassi et al,7 in another recently published study, followed only 7 of 263 patients for 10 years. Finally, 2 studies from the Cleveland Clinic5,17 included a small number of patients who had been followed 8 years after IPAA (17% of total patients); indeed, the mean follow-up was only 4 to 5 years in various age groups.
In an attempt to more clearly define patient specific outcomes, we earlier reported on a small single cohort of 75 patients which had been assessed at 1 and 10 years following IPAA and found little change in functional outcome over time.2 In the present study, we have expanded upon this earlier report by prospectively and annually following each of 409 patients for 15 years after operation for CUC, thus providing a unique longitudinal perspective on clinical and functional outcomes after IPAA.
We found that time had no adverse clinical impact on the number of bowel movements during the day (mean 6) and only little during the night (mean 2 at 15 years). However, episodes of fecal incontinence did increase after 10 and 15 years compared with the first 5 years after IPAA. The number of patients with perfect continence declined both during the day and night. The daytime decline was accompanied only by increased occasional incontinence, but the nighttime decline was accompanied by increased frequent incontinence. This change in continence might be due to a decline in sphincter strength known to occur with age.18,19 Occult obstetric sphincter injuries in women likely play an important role as well.20 Most of the patients in this study were still younger than 55 years at the time of last follow-up, and thus, it will be important to follow these patients as they age past 65 years. Interestingly, several community-based studies have documented an age-related increase in IBS21 and fecal incontinence in women.22 Whether the increase in problems with fecal incontinence reported in our study is related to the operation, as a sequel of ageing, or both is unknown.
Although we found a statistical significant change in functional outcome at 5, 10, and 15 years after IPAA, this change may not be clinically challenging as continence was achieved in over 85% of patients at 15 years after the IPAA. Moreover, QoL did not seem to be influenced adversely. The changes documented in Table 1, while statistically significant, are not likely clinically relevant. The statistical differences are largely driven by the large sample size and longitudinal analysis, resulting in high statistical power to detect small differences. Although functional outcomes and QoL are associated statistically9 and these changes perceived as worsening outcomes, the patients themselves do not appear to be disappointed.
QoL has become an important measure of operative outcome, perhaps because more conventional measures of quality such as morbidity and mortality have declined steadily. Many attempts have been made to define and assess QoL.23,24 Because no generally accepted QoL measurements after surgery for CUC exists in general, or after IPAA in particular, most studies use a combination of validated general QoL scores and simple well-being questions.5,8,9,25 QoL is not only related to functional status but also to ideas about what constitutes well-being.
Over the past 20 years, we have measured the performance status of patients after IPAA in several areas of daily activities: sports, housework, recreation, social activity, family relationship, sexual activity, and travel.10 We realize that these categories do not describe all aspects of QoL, but because the same questions have been asked in the same way, every year, they would be expected to show a trend toward improvement or deterioration if a significant change appeared. In spite of altered bowel function, very little change occurred, and at 15 years, all IPAA patients enjoyed an excellent QoL and good health and good performance scores in all categories. Although functional results after IPAA are better than after Brooke ileostomy or a Kock pouch,26 they are not perfect; patients, however, appear to adapt to these challenges and learn to handle them without being restricted in their daily living.
A criticism of this study might be that the group of 409 patients represented a special selection of IPAA patients because, by definition, all had a functioning pouch in place 15 years after IPAA and thus do not represent the overall long-term results of pouch surgery. Indeed, this is a special group of IPAA, and the data set is unique. Such longitudinal studies of large numbers of patients, all of whom were followed 15 years, do not exist. It was not a goal of the study to detail conventional outcomes data in terms of failure. These data are well known. Farouk et al1 documented the long-term failure rate to be 8% at 15 years at our institution. Tulchsky et al16 reported a cumulative failure of 9% at 5 years and of 13% at 10 years at St. Marks. Seventy-five percent of those failures occurred late (after 1 year) and were caused in 80% of patients by pelvic sepsis and by poor function. In a multivariate analysis of 494 CUC patients after IPAA, the risk of pouch-related septic complications was significantly dependent on the presence and on the dose of long-term corticoid medication at the time of IPAA but was not higher in patients older than 50 years at time of surgery.27 However, median follow-up was only 57 months. In another study, the cumulative probability of pouch failure was 7% at 10 years and strongly correlated with fistula formation but not with other parameters like gender and pouchitis.28
Whether the patients in this study 15 years after surgery are still at risk for pouch failure is unknown, but failure did not occur after 10 years.1 However, even after having a normally functioning pouch for extended periods of time, patients are still at risk for typical pouch-related complications, pouchitis being the most frequent. Typical episodes of pouchitis are quite short and did appear not to alter overall QoL and functional results. Small bowel obstruction is another frequent complication, occurring in 25% of our patients at 15 years. This rate is actually slightly lower than that estimated by others (31% cumulative risk at 10 years), but generally the need for surgery only is 7.5% at 10 years.29 Adhesions seem to be the major cause of obstruction. Such adhesions may be reduced with instillation of adhesion-prevention gels into the abdominal cavity30,31 or by a laparoscopic approaches.32 Whether laparoscopy reduces formation of adhesions in the pelvis and therefore reduces the rate of small bowel obstruction and mitigates the lowered fecundity ratio experienced by women after IPAA for CUC is the subject of ongoing studies.33 When pregnancy does occur, we have recently documented that successful pregnancy and vaginal delivery occur routinely in women after IPAA and that pouch function and the incidence of complications appear unaffected over time.34
Among the 409 patients operated for CUC in this study, the diagnosis was changed intraoperatively or during follow-up to indeterminate colitis in 16 patients and to Crohn disease in another 11 patients. No difference in functional outcome or QoL was seen. The numbers certainly are too small to draw definitive conclusions, but we35 and others36,37 have previously shown that patients with indeterminate colitis and CUC have equivalent function, QoL, and pouch survival rates after IPAA. The 11 patients with a change of diagnosis to Crohn disease with a normally functioning pouch after 15 years are most likely the exception, as most studies agree that Crohn disease, whether it develops after surgery for CUC or indeterminate colitis, is associated with unpredictable long-term outcomes.35 Only 1 study describes good 10-year functional outcomes, but the number of patients was small (n = 20), and Crohn-related complications occurred in 35% of patients.38 With improved medical therapies, including Imuran and Remicade, patients with Crohn disease and an ileal pouch may experience reasonably good long-term outcomes.39
CONCLUSIONS
The goals of surgery for CUC are to eradicate the disease, protect the patient from future malignant disease, and, most important because patients are young, to preserve reliable control of stool function and thus a good QoL. The long-term results in this large single cohort of IPAA patients are unique and are likely quite accurate reflections of individual patient outcomes over time. These data support the conclusion that IPAA is a durable operation for patients requiring proctocolectomy for CUC; functional and QoL outcomes are good, predictable, and stable for 15 years after operation.
Discussions
Dr. Robert D. Fry (Philadelphia, Pennysylvania): Dr. Hahnloser, I congratulate you. That was a nice presentation. And I commend you and your colleagues for this study that contributes significantly to our understanding of long-term results of restorative proctocolectomy for ulcerative colitis.
You indicated that all of these patients were operated on for chronic ulcerative colitis. Is this really true? Does this mean that none of these patients were treated for acute fulminant ulcerative colitis but only for disease that had become chronic? If so, might it be possible that patients with ulcerative colitis that was fulminant and not chronic would have different long-term outcome?
You note that the principal ongoing complication after this operation is pouchitis. But is seems to me that your definition of pouchitis is really very liberal. The patient that had a bout of gastroenteritis, took some metronidazole, got over it in a couple of days, would, by your criteria, have pouchitis. Such incidents increased as the number of years passed, as you would expect this to. Do you really mean to imply that pouchitis becomes a more significant problem with the passage of time?
Incontinence was noted to become more significant over the years. Was there a difference in this problem between men and women? Could this be related to obstetrical injuries which would occur only in women or did men also experience this mild but significant deterioration incontinence?
Finally, I wonder if you could elaborate a little more on these 11 patients that turned out to have Crohn’s disease, but in whom you maintained a functioning pouch. How was the diagnosis of Crohn’s disease established? What steps did you then take that were obviously successful in controlling the disease and preserving the pouch?
Again I congratulate the authors on an excellent paper. I appreciate the opportunity to have received the manuscript ahead of time.
Dr. Dieter Hahnloser (Zurich, Switzerland): Thank you, Dr. Fry, for your comments and insightful questions.
In relation to the indication for surgery, all patients were operated on electively for chronic ulcerative colitis, with the exception of three patients who underwent an emergency operation for fulminant disease. Although we did not see any difference in functional outcome in these three patients compared to patients with chronic disease, the number of patients was too small to allow any definitive conclusions. Because the entire colon and rectum are removed and we routinely divert patients for 2 to 3 months, we do not expect to find differences in functional outcome or quality of life between an emergency operation for acute inflammation and elective surgery for chronic ulcerative colitis. Only ten out of the 409 patients did not receive a temporary loop ileostomy and none of them were operated upon because of acute inflammation. Function outcome and QoL were comparable.
In relation to pouchitis, our definition might be considered liberal, but we applied it consistently over the 15 years of study. Although it is preferable to endoscope and biopsy patients suspected of having pouchitis, we continue to determine that a patient has pouchitis if symptoms are present for 2–3 days, and those symptoms are alleviated promptly (less than 24 hours) by administration of Metronidazole or Ciprofloxacin. About 50 patients out of 100 will develop at least 1 episode of pouchitis at 15 years of follow-up. Out of those 50 patients half of them, or 25 out of the total of 100, will have more than 1 episode of pouchitis and 7 out of the 100 patients will have a chronic problem. Finally, less than 1 of 100 patients will actually lose the pouch due to chronic pouchitis. Although the definition of chronic pouchitis is difficult to make, very few patients seem to have an ongoing problem. The use of probiotics in such patients might be helpful.
Regarding your question if there is a difference between men and women, we have looked at this in detail and did not find any significant changes in functional outcome or QoL between men and women. We know however that in women after vaginal delivery, occult sphincter injuries can occur in about one-third of the patients, and patients can become symptomatically incontinent at the age of 60 years or older. In this study, at 15 years of follow-up the mean age of patients was still only 50 years. Therefore, we still have to wait another 10 to 15 years before we can answer that question.
In relation to the patients with Crohn's disease, 11 of the 409 patients had the diagnosis changed from chronic ulcerative colitis to Crohn's disease. For 8 out of the 11, this change of diagnosis was done immediately perioperatively after pathologic examination of the resected specimen, and for 3 of them the diagnosis was changed during follow-up. All 3 patients developed perianal complications or perianal Crohn's disease; 1 patient with a pouch-vaginal fistula which was successfully reoperated, and 2 patients with abscesses which were incised and drained. One patient developed a fistula and was treated with a Seton. We currently do not recommend IPAA for patients with known Crohn's colitis, because the long-term outcome is unpredictable and pouch failure at 10 years can be as high as 60%. The 11 patients with a change of diagnosis to Crohn's disease with a normally functioning pouch after 15 years are most likely the exceptions.
Dr. Fabrizio Michelassi (Chicago, Illinois): I would like to congratulate Dr. Hahnloser and colleagues from the Mayo Clinic for yet another contribution to our understanding of long-term functional results after restorative proctocolectomy and ileo-anal anastomosis for ulcerative colitis. Having presented the long-term results on 400 patients with this very procedure last year at this meeting, I know how difficult it is to follow these patients year after year and have a rigorous and complete follow-up. I have 2 questions.
You have demonstrated that the functional results are excellent and stable at 15 years in the whole group. Are there subgroups where that is not true and where indeed you have observed a deterioration over time? I am specifically thinking of patients who underwent the initial operation at age 55 or older, or patients who developed chronic pouchitis, which fortunately occurs in a minority of patients but affects their functional results and quality of life.
You have shown some deterioration in the night continence of these patients over 15 years: was there a difference in the degree of deterioration whether the initial procedure was done as a stapled or a hand-sewn anastomosis?
Dr. Dieter Hahnloser (Zurich, Switzerland): Dr. Michelassi, thank you very much for your questions.
We have looked at the influence of age on pouch function. At last follow-up, only 23 out of the 409 patients were older than 65 years. Among these older patients, the number of stools per day was 6 and per night was and this was different from the group as a whole. Also, incontinence data was comparable in those patients. However, patients older than 65 years at last follow-up showed a slightly higher percentage of frequent incontinence at night (33%) compared to 22% in the whole group. We know from community based studies that with age, irritable bowel syndrome becomes more frequent and might influence continence, especially at night. Clearly, patients need to be followed up longer to answer this question.
In relation to chronic pouchitis, in this study, we have only asked if patients had an episode of pouchitis during the last year. It is difficult to define chronic pouchitis. Do patients requiring antibiotics every 2 to 3 months on a regular basis have chronic pouchitis? Or patients with 1 episode per year for 3 or 4 years in a row? Or patients with chronic histological changes on biopsies? Unfortunately, we cannot answer this question.
Also, with this study, we cannot comment on the long-term functional outcomes comparing hand-sewn versus double-stapled ileo-anal anastomosis, because all anastomoses in this population with 15 years of follow-up were done during a time where we did not staple. Therefore, all anastomoses were hand-sewn. However, from our prospective trial, we know that there is no difference in short-term function between stapled and hand-sewn patients.
Dr. Merril T. Dayton (Buffalo, New York): The modern version of this operation has now been available to us for about 25 years, and I think your study nicely documents its durability over much of that time period.
I was a little surprised, however, that you did not look a little more carefully at pouch loss and pouch failure. Pouch loss is arguably the ultimate measure of failure of this operation.
So I would like to ask you, what have you observed with regards to the patterns of pouch loss? Do most pouches fail within the first 2 years? Or do failures still occur 10–15 years out? I think it is a very important parameter to look at when we are looking at the impact of aging on this operation.
Dr. Dieter Hahnloser (Zurich, Switzerland): Thank you, Dr. Dayton, for your question.
As I hoped I mentioned initially, the study population was chosen because they had a functioning ileal pouch in place for 15 years. Therefore, pouch success was 100%. To try to answer your question, we know from our other studies that pouch failure approximates 8% at 15 years and 9% at 20 years of follow-up. From our previous analysis of pouch failure, and also in a recent review of the St. Marks experience, we know that about 75% of pouch loss occurs after the first year, and are mainly caused by pelvic sepsis. In the early postoperative course, sepsis is mainly due to operative complications while, later the cause is likely related to Crohn's disease. Pouch failure is also slightly more frequent in patients with indeterminate colitis compared to patients with chronic ulcerative colitis.
Dr. Eric W. Fonkalsrud (Los Angeles, California): I would like to congratulate Dr. Hahnloser and associates at the Mayo Clinic, including our moderator, Dr. Kelly, for their many pioneering efforts in developing the ileoanal pouch and for this excellent long-term follow-up.
Rectal stricture was one of your major long-term complications occasionally associated with infection in the pelvis. Rectal stricture often causes obstruction to pouch outflow, which then commonly results in stasis in the pouch with increased bacterial growth, which may then lead to a cascade of events resulting in repeated episodes of pouchitis. Could you tell us how you manage these rectal strictures if in fact you do encounter them frequently, and then how you manage the episodes of chronic pouchitis?
Have you had an opportunity to study pouch enlargement over the years associated with rectal strictures, and, if so, have you found it necessary to revise any of your pouches because of progressive enlargement causing stasis?
Dr. Dieter Hahnloser (Zurich, Switzerland): Thank you, Dr. Fonkalsrud.
It is interesting that you mentioned this cascade that can occur in a patient with stricture, because one of the patients I have described with Crohn's disease had a stricture, which was dilated on several occasions, then formed an abscess and developed a fistula that needed surgical treatment. However, the pouch is still in place and therefore, he was included in our study. Most of the strictures we see are treated conservatively by dilatation. Either we tell the patients to digitalize or to use dilators of different diameters.
In relation to pouch enlargement with time, we acknowledge your significant contribution in this area. Patients coming for follow-up visits to Rochester are not routinely studied for pouch enlargement with barium studies, and therefore, I cannot answer your question.
I wish to express my thanks to the Association for the privilege of presenting our paper.
Footnotes
Reprints: John H. Pemberton, MD, Mayo Clinic, Gonda 9-S, 200 First Street SW, Rochester, MN 55905. E-mail: riehle.jolyn@mayo.edu.
REFERENCES
- 1.Farouk R, Pemberton JH, Wolff BG, et al. Functional outcomes after ileal pouch-anal anastomosis for chronic ulcerative colitis. Ann Surg. 2000;231:919–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McIntyre PB, Pemberton JH, Wolff BG, et al. Comparing functional results one year and ten years after ileal pouch-anal anastomosis for chronic ulcerative colitis. Dis Colon Rectum. 1994;37:303–307. [DOI] [PubMed] [Google Scholar]
- 3.Meagher AP, Farouk R, Dozois RR, et al. J ileal pouch-anal anastomosis for chronic ulcerative colitis: complications and long-term outcome in 1310 patients. Br J Surg. 1998;85:800–803. [DOI] [PubMed] [Google Scholar]
- 4.Pemberton JH, Kelly KA, Beart RW Jr, et al. Ileal pouch-anal anastomosis for chronic ulcerative colitis: long-term results. Ann Surg. 1987;206:504–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Delaney CP, Fazio VW, Remzi FH, et al. Prospective, age-related analysis of surgical results, functional outcome, and quality of life after ileal pouch-anal anastomosis. Ann Surg. 2003;238:221–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ko CY, Rusin LC, Schoetz DJ Jr, et al. Long-term outcomes of the ileal pouch anal anastomosis: the association of bowel function and quality of life 5 years after surgery. J Surg Res. 2001;98:102–107. [DOI] [PubMed] [Google Scholar]
- 7.Michelassi F, Lee J, Rubin M, et al. Long-term functional results after ileal pouch anal restorative proctocolectomy for ulcerative colitis: a prospective observational study. Ann Surg. 2003;238:433–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Weinryb RM, Liljeqvist L, Poppen B, et al. A longitudinal study of long-term quality of life after ileal pouch-anal anastomosis. Am J Surg. 2003;185:333–338. [DOI] [PubMed] [Google Scholar]
- 9.Carmon E, Keidar A, Ravid A, et al. The correlation between quality of life and functional outcome in ulcerative colitis patients after proctocolectomy ileal pouch anal anastomosis. Colorectal Dis. 2003;5:228–232. [DOI] [PubMed] [Google Scholar]
- 10.Pemberton JH, Phillips SF, Ready RR, et al. Quality of life after Brooke ileostomy and ileal pouch-anal anastomosis: comparison of performance status. Ann Surg. 1989;209:620–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kelly KA, Pemberton JH, Wolff BG, et al. Ileal pouch-anal anastomosis. Curr Probl Surg. 1992;29:57–131. [DOI] [PubMed] [Google Scholar]
- 12.Reilly WT, Pemberton JH, Wolff BG, et al. Randomized prospective trial comparing ileal pouch-anal anastomosis performed by excising the anal mucosa to ileal pouch-anal anastomosis performed by preserving the anal mucosa. Ann Surg. 1997;225:666–676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Takao Y, Gilliland R, Nogueras JJ, et al. Is age relevant to functional outcome after restorative proctocolectomy for ulcerative colitis? prospective assessment of 122 cases. Ann Surg. 1998;227:187–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tan HT, Connolly AB, Morton D, et al. Results of restorative proctocolectomy in the elderly. Int J Colorectal Dis. 1997;12:319–322. [DOI] [PubMed] [Google Scholar]
- 15.Delaney CP, Dadvand B, Remzi FH, et al. Functional outcome, quality of life, and complications after ileal pouch-anal anastomosis in selected septuagenarians. Dis Colon Rectum. 2002;45:890–894. [DOI] [PubMed] [Google Scholar]
- 16.Tulchinsky H, Hawley PR, Nicholls J. Long-term failure after restorative proctocolectomy for ulcerative colitis. Ann Surg. 2003;238:229–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fazio VW, O'Riordain MG, Lavery IC, et al. Long-term functional outcome and quality of life after stapled restorative proctocolectomy. Ann Surg. 1999;230:575–584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McHugh SM, Diamant NE. Effect of age, gender, and parity on anal canal pressures: contribution of impaired anal sphincter function to fecal incontinence. Dig Dis Sci. 1987;32:726–736. [DOI] [PubMed] [Google Scholar]
- 19.Ryhammer AM, Laurberg S, Sorensen FH. Effects of age on anal function in normal women. Int J Colorectal Dis. 1997;12:225–229. [DOI] [PubMed] [Google Scholar]
- 20.Sultan AH, Kamm MA, Hudson CN, et al. Anal-sphincter disruption during vaginal delivery. N Engl J Med. 1993;329:1905–1911. [DOI] [PubMed] [Google Scholar]
- 21.Locke G, Yawn B, Wollan B. The incidence of clinically diagnosed irritable bowel syndrome in the community. Gastroenterology. 1999;116:G032. [Google Scholar]
- 22.Bharucha AE, Locke GR, McKeon K, et al. Prevalence and impact of fecal incontinence in women. Gastroenterology. 2004, in press.
- 23.Garrett JW, Drossman DA. Health status in inflammatory bowel disease: biological and behavioral considerations. Gastroenterology. 1990;99:90–96. [DOI] [PubMed] [Google Scholar]
- 24.Guyatt GH, Feeny DH, Patrick DL. Measuring health-related quality of life. Ann Intern Med. 1993;118:622–629. [DOI] [PubMed] [Google Scholar]
- 25.Robb BW, Gang GI, Hershko DD, et al. Restorative proctocolectomy with ileal pouch-anal anastomosis in very young patients with refractory ulcerative colitis. J Pediatr Surg. 2003;38:863–867. [DOI] [PubMed] [Google Scholar]
- 26.Kohler LW, Pemberton JH, Zinsmeister AR, et al. Quality of life after proctocolectomy: a comparison of Brooke ileostomy, Kock pouch, and ileal pouch-anal anastomosis. Gastroenterology. 1991;101:679–684. [PubMed] [Google Scholar]
- 27.Heuschen UA, Hinz U, Allemeyer EH, et al. Risk factors for ileoanal J pouch-related septic complications in ulcerative colitis and familial adenomatous polyposis. Ann Surg. 2002;235:207–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lepisto A, Luukkonen P, Jarvinen HJ. Cumulative failure rate of ileal pouch-anal anastomosis and quality of life after failure. Dis Colon Rectum. 2002;45:1289–1294. [DOI] [PubMed] [Google Scholar]
- 29.MacLean AR, Cohen Z, MacRae HM, et al. Risk of small bowel obstruction after the ileal pouch-anal anastomosis. Ann Surg. 2002;235:200–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Thornton MH, Johns DB, Campeau JD, et al. Clinical evaluation of 0.5% ferric hyaluronate adhesion prevention gel for the reduction of adhesions following peritoneal cavity surgery: open-label pilot study. Hum Reprod. 1998;13:1480–1485. [DOI] [PubMed] [Google Scholar]
- 31.Oncel M, Remzi FH, Senagore AJ, et al. Comparison of a novel liquid (Adcon-P) and a sodium hyaluronate and carboxymethylcellulose membrane (Seprafilm) in postsurgical adhesion formation in a murine model. Dis Colon Rectum. 2003;46:187–191. [DOI] [PubMed] [Google Scholar]
- 32.Hahnloser D, Young-Fadok TM. Earlier postoperative spontaneous diuresis in laparoscopic versus open total proctocolectomy and ileo pouch-anal anastomosis. Surg Endosc. 2003;17:S238. [Google Scholar]
- 33.Olsen KO, Joelsson M, Laurberg S, et al. Fertility after ileal pouch-anal anastomosis in women with ulcerative colitis. Br J Surg. 1999;86:493–495. [DOI] [PubMed] [Google Scholar]
- 34.Hahnloser D, Pemberton JH, Wolff BG, et al. Pregnancy and delivery before and after ileal pouch-anal anastomosis (IPAA) for inflammatory bowel disease: immediate and long-term consequences and outcomes. Dis Colon Rectum. 2004;47:1127–1135. [DOI] [PubMed] [Google Scholar]
- 35.Yu CS, Pemberton JH, Larson D. Ileal pouch-anal anastomosis in patients with indeterminate colitis: long-term results. Dis Colon Rectum. 2000;43:1487–1496. [DOI] [PubMed] [Google Scholar]
- 36.Delaney CP, Remzi FH, Gramlich T, et al. Equivalent function, quality of life and pouch survival rates after ileal pouch-anal anastomosis for indeterminate and ulcerative colitis. Ann Surg. 2002;236:43–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dayton MT, Larsen KR, Christiansen DD. Similar functional results and complications after ileal pouch-anal anastomosis in patients with indeterminate vs ulcerative colitis. Arch Surg. 2002;137:690–694. [DOI] [PubMed] [Google Scholar]
- 38.Regimbeau JM, Panis Y, Pocard M, et al. Long-term results of ileal pouch-anal anastomosis for colorectal Crohn's disease. Dis Colon Rectum. 2001;44:769–778. [DOI] [PubMed] [Google Scholar]
- 39.Colombel JF, Ricart E, Loftus EV Jr, et al. Management of Crohn's disease of the ileoanal pouch with infliximab. Am J Gastroenterol. 2003;98:2239–2244. [DOI] [PubMed] [Google Scholar]