Abstract
Objective:
To establish the relation between vagus nerve dysfunction, gastric emptying, and antireflux surgery.
Summary Background Data:
Delayed gastric emptying occurs in up to 40% of reflux patients. After antireflux surgery, gastric emptying becomes normal or is even accelerated. Occasionally, severe gastric stasis is found and is associated with a negative outcome of the antireflux procedure. It has been suggested that injury to the vagus nerve could be the cause of this delayed emptying.
Methods:
We evaluated in a prospective study gastric emptying of solids and vagus nerve function (pancreatic polypeptide response to hypoglycemia) before and after surgery in 41 patients (22 women; age 43 ± 1.6 years) who underwent laparoscopic hemifundoplication.
Results:
All patients had relief of reflux symptoms varying from adequate (n = 8) to complete relief (n = 33). Gastric emptying of solids increased significantly (P < 0.001) after operation: lag phase from 19 ± 2 to 10 ± 1 minute, emptying rate (%/h) from 37 ± 2 to 48 ± 5 and half emptying time from 110 ± 8 to 81 ± 4 minutes. Gastric emptying improved to a similar extent in patients with delayed and normal preoperative gastric emptying. Postoperative signs of vagus nerve damage (PP peak < 47pmol/L) were present in 4 patients (10%). In these 4 patients gastric emptying both before and after operation did not differ from patients with normal vagus nerve function. In fact, none of the 41 patients had severely delayed emptying after laparoscopic hemifundoplication.
Conclusions:
Laparoscopic hemifundoplication affects vagus nerve integrity in 10% of patients, but this does not lead to a delay in gastric emptying. In fact, gastric emptying improved significantly after fundoplication.
Vagus nerve function and gastric emptying were prospectively studied in 41 patients undergoing laparoscopic hemifundoplication. Hemifundoplication affected vagus nerve function in 10% of patients but did not lead to a delay in gastric emptying. In fact, gastric emptying improved significantly after fundoplication.
Gastroesophageal reflux disease (GERD) is frequently associated with abnormal gastric motility. Delayed gastric emptying occurs in up to 40% to 50% of the patients.1–5 The cause of abnormal gastric motility in reflux disease is unknown, but evidence exists of neural dysfunction.6 The role of the vagus nerve has never been well established in previous studies. Some authors have observed that gastric secretory response to insulin-induced hypoglycemia, a vagal-cholinergic stimulus, is impaired in some patients7,8 and that approximately 40% of patients with reflux disease have abnormal parasympathetic cardiovascular reflexes.9 However, in other studies no significant correlation between autonomic nerve dysfunction and delayed gastric emptying has been found.
It has been reported that fundoplication may affect gastric emptying of solids and liquids. The observed acceleration of emptying may contribute to the success of fundoplication.10–12 However, in some cases gastric emptying is significantly delayed after fundoplication and is associated with a negative outcome of the antireflux procedure.9,13 A possible explanation for this delayed emptying could be injury to the vagus nerve.14 Because there is a close relationship between the distal part of the esophagus, the proximal stomach, and the vagus nerves, antireflux operations may jeopardize these nerves. The exact incidence of accidental vagotomy after antireflux surgery is not well known, but is thought to be approximately 2%.15,16 The effect of antireflux surgery on gastric emptying, and in relation to vagus nerve (dys)function has not been evaluated previously. Therefore, we have performed a prospective study on gastric emptying and vagus nerve function and their interrelation before and after antireflux surgery in a group of patients who underwent laparoscopic partial fundoplication.
MATERIALS AND METHODS
Patients
Laparoscopic partial fundoplication is the primary antireflux procedure of choice at our institution. Between 1994 and 1999, this procedure was performed in 65 patients with documented gastroesophageal reflux disease. Of these patients, 41 patients agreed to participate in this prospective study. The group of patients consisted of 22 women and 19 men with a mean age of 43 ± 2 years (range 22–66 years). All patients had reflux symptoms refractory to optimal medical therapy. GERD was diagnosed by a typical clinical history, endoscopic signs of esophagitis and/or abnormal esophageal acid exposure to the distal esophagus, measured by ambulatory 24-hour pH monitoring. All patients were evaluated pre- and postoperatively by standard symptom questionnaires, 24-hour ambulatory pH monitoring, gastric emptying tests, and measurements of plasma pancreatic polypeptide (PP) in response to insulin-induced hypoglycemia as an indirect test for vagus nerve integrity. Postoperative evaluation was performed 3 to 6 months after the operation.
Gastric Emptying
Gastric emptying of solids and liquids was measured by radionuclide scintigraphy with a dual-isotope method. The solid component of the meal consisted of a pancake (280 kCal) labeled with 15 MBq of technetium-99m colloid and the liquid component of 150 mL water labeled with 2 MBq indium-111 DTPA.17 All subjects ingested the pancake first, followed by water. Anterior images of gastric activity were acquired during 120 minutes starting from the onset of meal ingestion with 1 minute per frame. Data were analyzed to determine the lag phase, half-emptying time, and emptying rate for the solid component. The retention for liquids was calculated at 15, 30, 45, and 60 minutes after ingestion.
Gastric emptying for solids was considered normal if values for lag phase ranged from 13 to 31 minutes and for emptying rate from 36% to 79% per hour. Gastric emptying for solids was considered delayed if the emptying rate was ≤35% per hour.
Vagus Nerve Integrity
Vagus nerve integrity was measured indirectly by the response of plasma PP to insulin-induced hypoglycemia.14,18,19 The test was performed after an overnight fast. At time 0 minutes, 0.1 U/kg insulin (Actrapid, Novo Nordisk Farma BV, Bagsvaerd, Denmark) was administered intravenously by bolus infusion. At 10-minute intervals for 90 minutes, blood was drawn for measurement of PP and glucose. PP was measured by a sensitive and specific radioimmunoassay, as described previously.20 The nadir of blood glucose in response to insulin was <2.5 mmol/L in all subjects.
The response of the pancreas in secreting PP after hypoglycemia is mediated through efferent vagal activity. It has been demonstrated that after truncal vagotomy, but also during administration of atropine, the PP response to insulin-induced hypoglycemia is abolished.21,22 A peak increment in plasma PP <47 pmol/L is considered to be compatible with truncal vagotomy.19
Symptoms
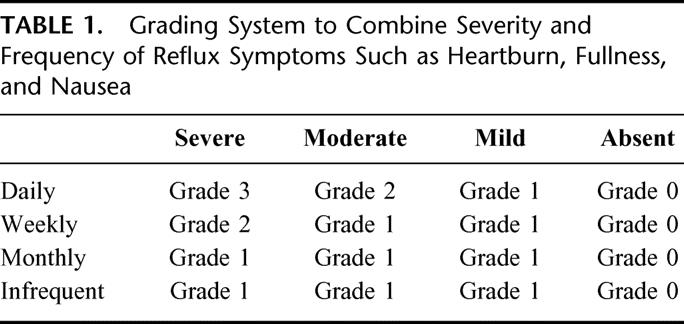
GERD symptoms were scored by a standardized symptom questionnaire before and at 3 and 6 months after operation. Symptoms included heartburn, retrosternal pain, sensation of fullness, and nausea. We combined severity and frequency of symptoms, according to a scoring system as shown in Table 1.
TABLE 1. Grading System to Combine Severity and Frequency of Reflux Symptoms Such as Heartburn, Fullness, and Nausea
Operation
Laparoscopic partial fundoplication was performed at 3 medical centers in the Leiden region by 3 senior surgeons (JR, PJJR, PN) experienced in laparoscopic antireflux surgery. The distal esophagus was mobilized, starting from the right side, for at least 7 cm above the gastroesophageal junction. No electrocautery was used. After mobilization, both the anterior and the posterior vagal nerve were identified. In all 62 patients, a posterior partial fundoplication (200 degrees) was performed by laparoscopy.
Statistical Analysis
Results of gastric emptying and vagus nerve function test are expressed as mean ± SEM. Results of the 24-hour pH metry are expressed as medians and ranges. Statistical analysis of gastric emptying data, reflux variables, symptom scores, and data from the vagus nerve function test obtained before and after operation was performed by using the Wilcoxon rank-sum test and the Mann-Whitney U test. The significance level was set at P < 0.05.
RESULTS
Symptoms
Before surgery, all 41 patients complained of reflux (Fig. 1). Surgery resulted in complete relief of reflux symptoms in 80% (33 patients). All patients improved after laparoscopic partial fundoplication. Mild complaints were present in 10 patients at 3 months and in 7 patients at 6 months after surgery.
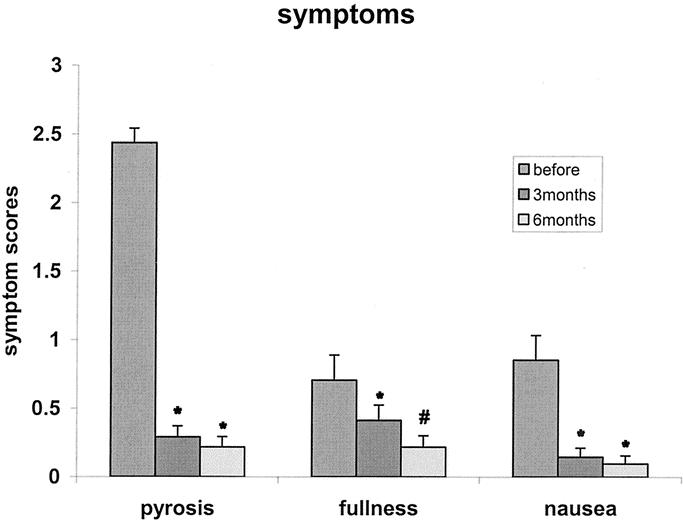
FIGURE 1. Symptom scores (mean ± SEM) for pyrosis, fullness, and nausea before, and at 3 and 6 months after laparoscopic partial fundoplication in 41 patients. *P < 0.01 compared with before surgery. #P < 0.05 compared with 3 months after surgery.
Before surgery, 12 patients had complaints of postprandial fullness, of whom 6 patients had severe complaints. Three months after surgery, 12 patients had postprandial fullness, of whom 6 had new-onset postprandial fullness. None of the patients had severe complaints. Six months after surgery, 7 patients had complaints of postprandial fullness (2 moderate, 5 mild). Scores for nausea had a similar pattern (Fig. 1).
24-Hour pH Metry
All 41 patients underwent 24-hour pH metry before and after surgery. After laparoscopic partial fundoplication, there was a significant decrease (P < 0.0001) in overall time with pH below 4 from 8.7% (2.5–20.2) to 1.1% (0–14.4). This was also true for acid exposure in upright position from 9.2% (0–29.5) to 1.8% (0–22.4) and in supine position from 5.1% (0–38.2) to 0% (0–21.6) postoperatively (P < 0.0001). In 33 patients (80%) there was a complete normalization of the 24-hour pH metry data (total time pH below 4:≤4.0%).23
Vagus Nerve Function
Preoperatively, none of the 41 patients had evidence of vagus nerve dysfunction. The plasma PP peak increment in response to insulin had a mean value of 146 ± 9 pmol/L. After operation, the plasma PP response was compatible with truncal vagotomy (PP peak increment ≤ 47pmol/L) in 4 patients. The mean value of the 37 patients without evidence of truncal vagotomy after fundoplication was 140 ± 13 pmol/L.
Gastric Emptying
Solids
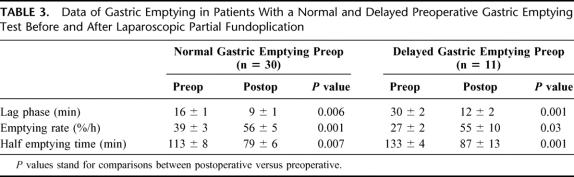
Gastric emptying increased significantly after laparoscopic partial fundoplication (Table 2). We divided the patient population into 2 groups: 1 with a normal and 1 with delayed preoperative gastric emptying. In both groups, gastric emptying increased significantly after laparoscopic partial fundoplication due to a decrease in lag phase, half emptying time, and an increase in emptying rate (Table 3). In 11 patients, gastric emptying was delayed before operation (gastric emptying rate ≤35%). After fundoplication, gastric emptying for solids normalized in 6 patients, improved in 4 patients, and remained delayed in only 1 patient. None of the patients with normal preoperative gastric emptying developed delayed gastric emptying rates after fundoplication (Fig. 2).
TABLE 2. Pre- and Postoperative Data of Gastric Emptying of Solids and Liquids (n = 41)
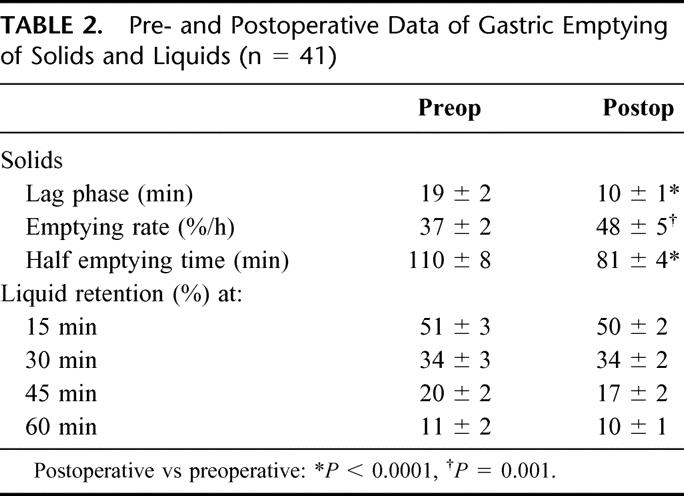
TABLE 3. Data of Gastric Emptying in Patients With a Normal and Delayed Preoperative Gastric Emptying Test Before and After Laparoscopic Partial Fundoplication
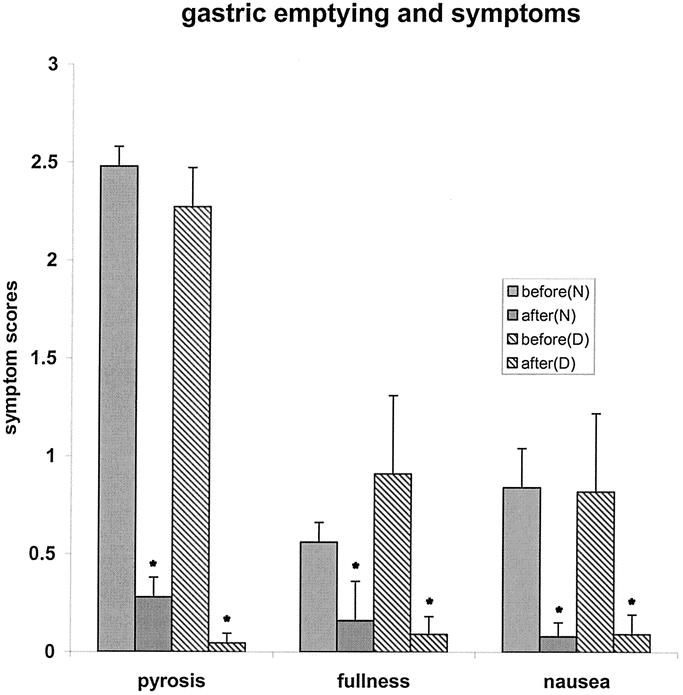
FIGURE 2. Symptom scores (mean ± SEM) for pyrosis, fullness, and nausea before and after laparoscopic partial fundoplication in 30 patients with normal (N) versus 11 patients with delayed (D) gastric emptying. *P < 0.05 compared with before operation.
Liquids
Gastric emptying of liquids was not delayed before or after surgery. No differences in pre- or postoperative gastric emptying data of liquids were observed (Table 2).
Relation Between Gastric Emptying, Vagus Nerve Function, and Gastrointestinal Symptoms
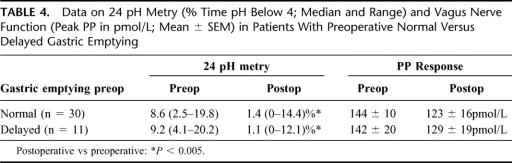
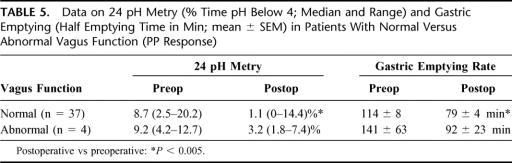
No significant correlation was found between dyspeptic symptoms and parameters of gastric emptying. Patients were divided into 1 group with normal and 1 group with delayed preoperative gastric emptying. A significant decrease in complaints of pyrosis, fullness, and nausea was seen in both groups (Table 4). Patients with a normal postoperative PP response had a significant decrease in gastrointestinal symptoms. The 4 patients with vagus nerve dysfunction (abnormal PP response) also showed a decrease in pyrosis and nausea but not in fullness (Table 5).
TABLE 4. Data on 24 pH Metry (% Time pH Below 4; Median and Range) and Vagus Nerve Function (Peak PP in pmol/L; Mean ± SEM) in Patients With Preoperative Normal Versus Delayed Gastric Emptying
TABLE 5. Data on 24 pH Metry (% Time pH Below 4; Median and Range) and Gastric Emptying (Half Emptying Time in Min; mean ± SEM) in Patients With Normal Versus Abnormal Vagus Function (PP Response)
The effect of fundoplication with respect to reflux control was not different between patients with normal and delayed preoperative gastric emptying. This was also true for PP secretion (Table 4).
The 4 patients with an abnormal PP response did not differ in reflux control (pH metry) or gastric emptying compared with patients with a normal PP response (Table 5).
After fundoplication, 4 patients were considered to be failures (ie, abnormal 24-hour pH metry and persistent reflux symptoms). Of these 4 patients, only 1 had evidence of vagus nerve dysfunction, whereas the remaining 3 patients had normal PP responses.
DISCUSSION
Gastric emptying is delayed in a substantial proportion of GERD patients.4–5 Severely delayed emptying may contribute to reflux or promote reflux and is considered as a relative contraindication for antireflux surgery. The results of our study are in line with previous studies: first, showing that delayed gastric emptying of solids is present in 28% of patients and second, that fundoplication significantly accelerates gastric emptying.10–12,24–27 Even in patients with a preoperative delayed gastric emptying test, gastric emptying became accelerated after fundoplication.
An explanation for the acceleration of gastric emptying after surgery is not apparent. Several factors may influence gastric emptying. The first factor is gastric compliance. In previous studies, we have shown that gastric wall properties are not significantly influenced by antireflux surgery. However, after fundoplication, postprandial accommodation of the proximal stomach is impaired.25,26 Decreased fundal capacity may result in more rapid transport of the meal to the distal part of the stomach, ie, the antrum, and thereby result in acceleration of gastric emptying.25,26,28 Wilbur et al showed that reduction of the radius of the proximal stomach by fundectomy accelerates gastric emptying of liquids.29
After laparoscopic partial fundoplication, we found that 10% of patients had signs of vagus nerve dysfunction as demonstrated by an impaired PP response to insulin hypoglycemia. Do changes in innervation negatively affect the results of fundoplication? Our group of 4 patients with signs of postoperative vagus nerve dysfunction was not different from the other group (normal PP response) with respect to control of gastroesophageal reflux symptoms, 24-hour pH metry, or gastric emptying (Fig. 3). It should be noted that the number of patients with an abnormal test (impaired PP response) was small. This is in line with the findings of a former study by Cunningham et al.6
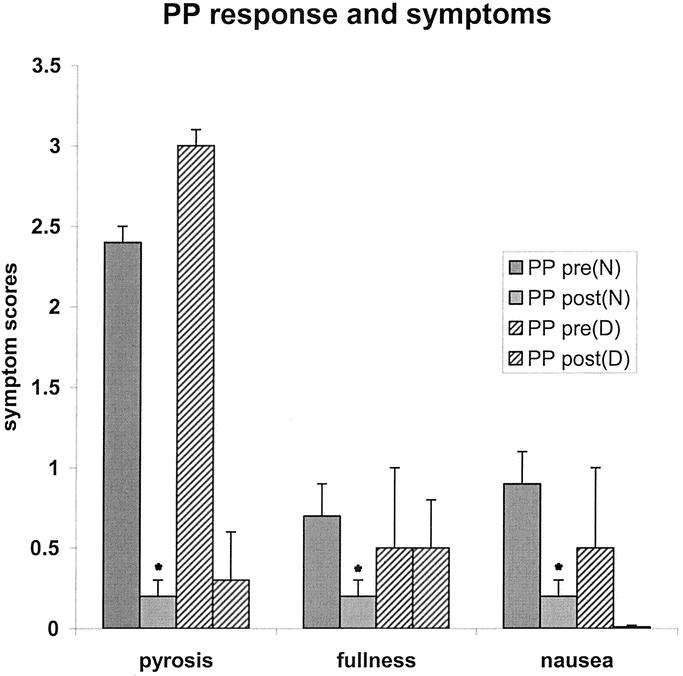
FIGURE 3. Symptom scores (mean ± SEM) for pyrosis, fullness, and nausea before and after laparoscopic partial fundoplication in 37 patients with normal PP response (N) versus 4 patients with vagus dysfunction (D). *P < 0.05 compared with before operation.
After dividing the patients into 1 group with normal versus 1 group with delayed preoperative gastric emptying, no significant differences in gastric emptying test data after operation were seen between both groups. In both groups, gastric emptying became significantly accelerated. Postoperative gastric emptying was similar in both groups. There were no differences present in results of the 24-hour pH metry between the 2 groups, nor in PP response to hypoglycemia. Therefore, we believe that a preoperative delayed gastric emptying test should not be considered a contraindication for antireflux surgery. This statement is in contrast with the results of other studies.11,13
Symptoms of fullness, nausea, and dyspepsia decreased after laparoscopic partial fundoplication. No correlation was found between dyspeptic symptoms and gastric emptying data. This is supported by the findings of Jamieson et al,27 but is in contrast with other studies.11,12,24 We compared patients with normal versus delayed preoperative gastric emptying, but our study showed no significant difference in the occurrence of dyspeptic symptoms before or after surgery.
The finding that gastric emptying of solids is accelerated after laparoscopic partial fundoplication may contribute to the success of the operation. There were no significant correlations between gastric emptying, dyspeptic symptoms, postoperative 24-hour pH metry, or the vagus nerve function test. Vagus nerve dysfunction, as demonstrated by the PP response to hypoglycemia, did not negatively influence the effect of laparoscopic partial fundoplication, nor did it correlate with gastric emptying.
We therefore believe that delayed gastric emptying should no longer be considered as a contraindication for antireflux surgery. Accidental vagus nerve dysfunction after laparoscopic partial fundoplication occurs in 10% of patients based on results of PP secretion in response to insulin hypoglycemia. Vagus nerve dysfunction does not adversely affect the success of antireflux surgery.
Footnotes
Reprints: Dr. A. A. M. Masclee, Department of Gastroenterology–Hepatology, Leiden University Medical Center, P.O. Box 9600, 2300 RC Leiden, The Netherlands. E-mail: a.a.m.masclee@lumc.nl.
REFERENCES
- 1.Holloway RH, Dent J. Pathophysiology of gastroesophageal reflux disease: lower esophageal dysfunction in gastroesophageal reflux disease. Gastroenterol Clin North Am. 1990;19:517–536. [PubMed] [Google Scholar]
- 2.Kahrilas PJ, Dodds WJ, Hogan WJ, et al. Esophageal peristaltic dysfunction in peptic esophagitis. Gastroenterology. 1986;91:897–904. [DOI] [PubMed] [Google Scholar]
- 3.King PM, Pryde A, Heading RC. Transpyloric fluid movements and antroduodenal motility in patients with gastroesophageal reflux. Gut. 1987;28:545–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maddern GJ, Chatterton BE, Collins PJ, et al. Solid and liquid gastric emptying in patients with gastro-oesophageal reflux. Br J Surg. 1985;72:344–347. [DOI] [PubMed] [Google Scholar]
- 5.Collins BJ, McFarland RJ, O'Hare MMT, et al. Gastric emptying of a solid-liquid meal and gastrointestinal hormone responses in patients with erosive oesophagitis. Digestion. 1986;33:61–68. [DOI] [PubMed] [Google Scholar]
- 6.Cunningham KM, Horowitz M, Riddell PS, et al. Relations among autonomic nerve dysfunction, oesophageal motility, and gastric emptying in gastro-oesophageal reflux disease. Gut. 1991;32:1436–1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Heatly RV, Collins RJ, James PD, et al. Vagal function in relation to gastro-esophageal reflux and associated motility changes. BMJ. 1980;280:755–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ogilvie AL, James PD. Impairment of vagal function in reflux oesophagitis. QJ Med. 1985;54:61–74. [PubMed] [Google Scholar]
- 9.Chakraborty TK, Ogilvie AL, Heading RC, et al. Abnormal cardiovascular reflexes in patients with gastro-oesophageal reflux. Gut. 1989;30:46–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Maddern GJ, Jamieson GG. Fundoplication enhances gastric emptying. Ann Surg. 1985;201:96–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hinder RA, Stein HJ, Bremner CG, et al. Relationship of a satisfactory outcome to normalization of delayed gastric emptying after Nissen fundoplication. Ann Surg. 1989;210:458–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bais JE, Samsom M, Boudesteijn EA, et al. Impact of delayed gastric emptying on the outcome of antireflux surgery. Ann Surg. 2001;234:139–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Maddern GJ, Jamieson GG, Chatterton BE, et al. Is there an association between failed antireflux procedures and delayed gastric emptying? Ann Surg. 1985;202:162–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gooszen HG, Horbach JMLM, Jansen EH, et al. Incidence of vagal nerve damage after antireflux surgery and the relation to symptoms. Gastroenterology. 1993;104:A90. [Google Scholar]
- 15.Belsey RHR. Transthoracic partial fundoplication (Belsey repair). In: Jamieson GG, ed. Surgery of the Oesophagus. London: Churchill Livingstone; 1988. [Google Scholar]
- 16.Low DE, Mercer CD, James EC, et al. Post Nissen syndrome. Surg Gynecol Obstet. 1988;167:1–5. [PubMed] [Google Scholar]
- 17.Jacobs F, Akkermans LMA, Oei HY, et al. A radioisotope method to quantify the function of the fundus, antrum and their contractile activity in gastric emptying of semi-solid and solid meal. In: Motility of the Digestive Tract. New York: Raven Press; 1982:233:–240. [Google Scholar]
- 18.Jansen EH, Horbach JMLM, Klamer M, et al. Plasma pancreatic polypeptide responses to insulin hypoglycemia after Nissen fundoplication. Scand J Gastroenterol. 1989;24:9–12.2467348 [Google Scholar]
- 19.Masclee AAM, Lamers CBHW. Effect of endoscopic sclerotherapy of esophageal varices on vagus nerve integrity. J Hepatol. 1994;21:724–729. [DOI] [PubMed] [Google Scholar]
- 20.Lamers CBHW, Diemel CM, Leer van E, et al. Mechanism of elevated serum pancreatic polypeptide concentrations in chronic renal failure. J Clin Endocrinol Metab. 1982;55:922–926. [DOI] [PubMed] [Google Scholar]
- 21.Schwartz TW. Pancreatic polypeptide: a hormone under vagal control. Gastroenterology. 1983;85:1411–1425. [PubMed] [Google Scholar]
- 22.Schwartz TW, Holst JJ, Fahrenkrug J, et al. Vagal, cholinergic regulation of pancreatic polypeptide secretion. J Clin Invest. 1978;61:781–789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Masclee AAM, de Best AC, de Graaf R, et al. Ambulatory 24-hour pH metry in the diagnosis of gastroesophageal reflux disease. Scand J Gastroenterol. 1990;25:225–230. [PubMed] [Google Scholar]
- 24.Lundell LR, Myers JC, Jamieson GG. Delayed gastric emptying and its relationship to symptoms of gas float after antireflux surgery. Eur J Surg. 1994;160:161–166. [PubMed] [Google Scholar]
- 25.Vu MK, Ringers J, Arndt JW, Lamers CBHW, et al. Prospective study of the effect of laparoscopic hemifundoplication on motor and sensory function of the proximal stomach. Br J Surg. 2000;87:338–343. [DOI] [PubMed] [Google Scholar]
- 26.Vu MK, Straathof JWA, vd Schaar PJ, et al. Motor and sensory function of the proximal stomach in reflux disease and after laparoscopic Nissen fundoplication. Am J Gastroenterol. 1999;94:1481–1489. [DOI] [PubMed] [Google Scholar]
- 27.Jamieson GG, Maddern GJ, Myers JC. Gastric emptying after fundoplication with and without proximal gastric vagotomy. Arch Surg. 1991;126:1414–1417. [DOI] [PubMed] [Google Scholar]
- 28.Lindeboom MYA, Vu MK, Ringers J, et al. Function of the proximal stomach after laparoscopic partial versus complete fundoplication. Am J Gastroenterol. 2003;98:284–290. [DOI] [PubMed] [Google Scholar]
- 29.Wilbur BG, Kelly KA, Code CF. Effect of gastric fundectomy on canine gastric electrical and motor activity. Am J Physiol. 1974;226:1445–1449. [DOI] [PubMed] [Google Scholar]