To the Editor:
In the February issue of Annals of Surgery, Cillo et al reported on the use of orthotopic liver transplantation (OLT) for the treatment of moderately or well-differentiated hepatocellular carcinoma (HCC). As noted by the authors, most transplant centers and the United Network for Organ Sharing have adopted the “Milan criteria” as initially proposed by Mazzaferro et al1; however, the authors suggest that preoperative tumor grade may be a more accurate criterion for selecting HCC patients for OLT. Using a selection protocol based on grade, Cillo et al reported that G1 and G2 HCC had an extremely low rate of tumor recurrence after OLT, comparable with that of incidentally detected HCC. Although we agree that tumor grade bears strongly on prognosis, we believe that the relative importance of tumor grade may have been overstated in the Cillo et al article. In the article, patients were highly selected not only with regard to tumor grade but also tumor size (median tumor size, 2.5 cm). Although the authors attribute their low incidence of microscopic vascular invasion (MVI) (4%) to the fact that only G1-G2 HCC were considered for OLT, small tumor size and perhaps other factors (selection of better biology based on waiting time on transplant list) could also explain the unexpectedly low incidence of MVI.2
The interaction of tumor size, nuclear grade, and MVI is complex and these factors are known to compete in multivariate models with regard to prognosis.3–5 Hemming et al have reported that although vascular invasion, tumor size greater than 5 cm, and poor tumor grade were significant predictors of tumor recurrence by univariate analysis, only vascular invasion remained significant on multivariate analysis.3 Jonas et al reported that tumor diameter in correlation with histopathologic grading was predictive of vascular invasion but only in HCCs larger than 5 cm.4 Because of the exceedingly low incidence of both MVI and large tumors in the report by Cillo et al, it is impossible to assess the impact of each of these factors on tumor grade in this study.
Based on our own experience with HCC patients in the International Cooperative Study Group on Hepatocellular Carcinoma,6 we would have expected a significantly higher incidence of MVI than the 4% reported by Cillo et al. Of the 591 HCC patients in our multicenter database, 23.9% and 50.8% of G1 and G2 patients, respectively, had MVI well over the rate reported by Cillo et al. Patients with G1 and G2 tumors < 5 cm had a 16.7% and 30.0% rate of MVI, respectively. As expected, G1 and G2 patients with tumors ≥ 5 cm had even higher rates of MVI (32.3% and 67.9%, respectively) (Fig. 1). The relative high incidence of MVI in G1 and G2 patients in our experience makes us question the general applicability of the Cillo et al findings. Although their work corroborates earlier findings that low tumor grade leads to a good prognosis in patients with small tumors and no MVI, it fails to answer the more difficult question of how patients with low-grade, larger tumors with or without MVI fare after OLT.
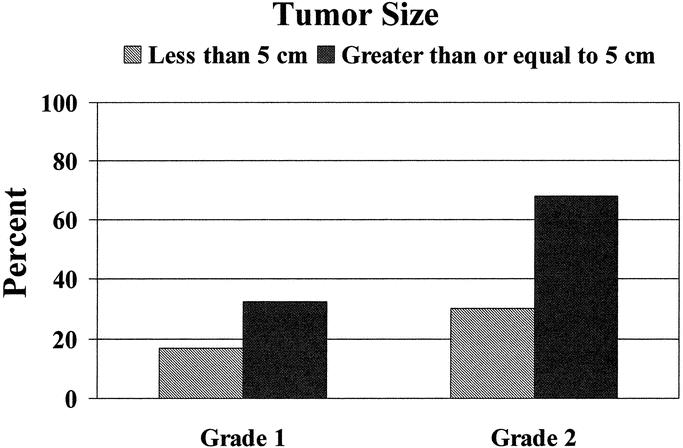
FIGURE 1. Of the 591 HCC patients in the International Cooperative Study Group multicenter database, 23.9% and 50.8% of GJ and G2 patients, respectively, had microvascular invasion on final surgical pathology. Patients with smaller tumors (< 5 cm) were less likely to have microvascular invasion (G1, 16.7%; G2, 30.0%) than patients with larger tumors (≥ 5 cm) (G1, 32.3%; G2, 67.9%).
We agree with the authors that fine needle aspiration biopsy may in the future be helpful in preoperatively stratifying patients with regard to biology of HCC,7 but we believe it is premature to state that grade is the main factor that influences prognosis after OLT. Future investigations will need to include patients with a broader range of tumor sizes, degree of vascular invasion, as well as grade to clarify which factor, or combination of factors, has the most prognostic power in predicting outcome after OLT for HCC.
Timothy M. Pawlik, MD, MPH
Eddie K. Abdalla, MD
Jean-Nicolas Vauthey, MD
University of Texas
M. D. Anderson Cancer Center
Department of Surgical Oncology
Houston, TX
REFERENCES
- 1.Mazzaferro V, Regalia E, Doci R, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996;334:693–699. [DOI] [PubMed] [Google Scholar]
- 2.Tsai TJ, Chau GY, Lui WY, et al. Clinical I significance of microscopic tumor venous invasion in patients with resectable hepatocellular carcinoma. Surgery. 2000;127:603–608. [DOI] [PubMed] [Google Scholar]
- 3.Hemming AW, Cattral MS, Reed AI, et al. Liver transplantation for hepatocellular carcinoma. Ann Surg. 2001;233:652–659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jonas S, Bechstein WO, Steinmuller T, et al. Vascular invasion and histopathologic grading determine outcome after liver transplantation for hepatocellular carcinoma in cirrhosis. Hepatology. 2001;33:1080–1086. [DOI] [PubMed] [Google Scholar]
- 5.Esnaola NF, Lauwers GY, Mirza NQ, et al. Predictors of microvascular invasion in patients with hepatocellular carcinoma who are candidates for orthotopic liver transplantation. J Gastrointest Surg. 2002;6:224–232. [DOI] [PubMed] [Google Scholar]
- 6.Vauthey IN, Lauwers GY, Esnaola NF, et al. Simplified staging for hepatocellular carcinoma. J Clin Oncol. 2002;20:1527–1536. [DOI] [PubMed] [Google Scholar]
- 7.Vauthey IN, Ajani JA. Liver transplantation and hepatocellular carcinoma biology: beginning of the end of the era of educated guesses. J Clin Oncol. 2003;21:4265–4267. [DOI] [PubMed] [Google Scholar]


