Abstract
Objective:
To examine the utility of magnetic resonance cholangiography (MRC) in the preoperative evaluation of patients with gallstone pancreatitis.
Summary Background Data:
Gallstone pancreatitis is often associated with the presence of common bile duct (CBD) stones that may require endoscopic removal prior to planned laparoscopic cholecystectomy. No reliable clinical criteria exist, however, that can accurately predict CBD stones and the need for preoperative endoscopic retrograde cholangiopancreatography (ERCP).
Methods:
Sixty-four patients were identified with gallstone pancreatitis based on clinical presentation and imaging studies over a three-and-a-half-year period. All patients underwent MRC, and the images were evaluated for gallstones, CBD stones, cholecystitis, and pancreatitis
Results:
Seventeen of the 64 patients (27%) with gallstone pancreatitis were found to have CBD stones confirmed by ERCP. MRC correctly predicted CBD stones in 16 of the 17 patients (sensitivity = 94%). In 1 additional patient, MRC demonstrated CBD stones not seen at ERCP, consistent with probable passage. By comparison, the sensitivities of other criteria for predicting CBD stones were (1) elevated bilirubin ≥2.0 mg/dL = 65%; (2) dilated duct on ultrasound = 55%; and (3) CBD stones on ultrasound = 27%. MRC was able to visualize gallbladder stones in 57 of 62 patients (94%) and correctly predicted acute cholecystitis in 6 of 8 patients. MRC also detected peripancreatic edema and inflammatory changes consistent with acute pancreatitis in 45 of 64 patients (70%).
Conclusions:
These results demonstrate that MRC can accurately identify CBD stones preoperatively in patients with gallstone pancreatitis and provide valuable information with respect to other biliary pathology, including cholelithiasis, acute cholecystitis, and pancreatitis. MRC is an effective noninvasive screening tool for CBD stones, appropriately selecting candidates for preoperative ERCP and sparing others the need for an endoscopic procedure with its associated complications.
Magnetic resonance cholangiography in patients presenting with gallstone pancreatitis is a safe and accurate screening tool for choledocholithiasis, identifying which patients may benefit from ERCP before cholecystectomy and sparing other patients the need for routine preoperative ERCP with its associated complications.
In 1901, Opie1 first described the association between obstruction of the distal bile duct due to migrating gallstones and the development of acute pancreatitis. Acosta and Ledesma2 later reported in 1974 that this biliary obstruction was often transient, with the majority of stones passing rapidly into the duodenum. The realization that migrating gallstones can precipitate an attack of acute pancreatitis has led to the recommendation that cholecystectomy be performed once the acute pancreatic inflammation has subsided. When possible, cholecystectomy is performed during the initial hospitalization to minimize the potential for further stone migration and recurrent pancreatitis.
Although the majority of common bile duct (CBD) stones pass spontaneously, 20% to 30% of patients with gallstone pancreatitis will have persistent CBD stones that fail to traverse the ampulla. The role of invasive imaging procedures such as ERCP in the early detection and management of these persistent stones is controversial. Several randomized, prospective studies suggest that early identification and removal of CBD stones results in decreased patient morbidity and may help prevent the progression of mild pancreatitis to severe disease.3,4 This has led to the general recommendation and common practice that all patients with gallstone pancreatitis undergo early ERCP to rule out the presence of CBD stones. Other investigators point out, however, that routine ERCP only benefits the small number of patients who actually have persistent CBD stones and that the majority of patients will have undergone an unnecessary invasive procedure,5–7 with its associated risks. Unfortunately, traditional noninvasive imaging modalities such as ultrasonography and computed tomography (CT) are limited in their ability to detect CBD stones. Clinical criteria such as the severity of pancreatitis or elevated serum bilirubin on admission have also proven unreliable in selecting those patients most likely to have persistent CBD stones and those most likely to benefit from early ERCP.
Magnetic resonance cholangiography (MRC) is a relatively new imaging modality that provides a noninvasive alternative to direct cholangiography. This imaging technique is able to create projectional images similar in detail and appearance to direct cholangiography, with high resolution of the bile duct and intraductal stones. MRC avoids the use of intravenous contrast or ionizing radiation and, unlike ultrasonography and ERCP, is less operator-dependent. MRC is also able to detect other biliary pathology such as gallbladder stones, as well as gallbladder and pancreatic inflammation, making it a useful initial imaging test for patients with suspected pancreatitis. There are no large studies, however, which address the utility of MRC in gallstone pancreatitis. Critics have argued that it is unclear if the presence of pancreatic inflammation diminishes the ability of MRC to visualize the distal CBD and identify ampullary stones. In addition, gallstone pancreatitis tends to be associated with relative small calculi, which MRC may not be able to identify.8 We performed MRC in a large, unselected group of patients with gallstone pancreatitis to evaluate its accuracy in detecting CBD stones and to determine the potential role of routine MRC in the initial evaluation of patients with gallstone pancreatitis.
PATIENTS AND METHODS
Sixty-four patients with gallstone pancreatitis who underwent MRC at the Johns Hopkins Bayview Medical Center from July 1995 through February 1999 were studied. A diagnosis of gallstone pancreatitis was based upon the presence of typical clinical features such as acute epigastric pain and nausea, with a serum amylase of at least twice the upper limits of normal (normal: <100 U/L). Pancreatitis was mild to moderate in all cases, and patients were included only if they had evidence of biliary calculi on conventional radiologic imaging (ultrasound, CT) or on direct cholangiography. Patients were excluded if other etiologies for pancreatitis were present such as alcohol use or trauma. MRC is used as a routine practice at our institution, and the data for this study were accrued prospectively. The cohort included 19 males and 45 females, with a median age of 56 years (range 19–89 years). The hospital course and clinical follow-up of each patient were reviewed, including the results of admission laboratory tests, imaging studies, and the findings at surgery or direct cholangiography. A diagnosis of CBD stones was made only if calculi were visualized in the bile duct on direct cholangiography or at surgical exploration. The diagnosis of acute cholecystitis was based on intraoperative findings and pathologic examination confirming acute gallbladder inflammation. Diagnostic studies such as ultrasound, CT, and ERCP were performed at the discretion of the attending surgeon. Forty-eight patients underwent abdominal ultrasonography and 36 patients underwent abdominal CT. ERCP was performed in 34 patients and intraoperative cholangiography (IOC) in 10 patients.
Fifty-five of the 64 patients underwent cholecystectomy, including 47 procedures performed laparoscopically, 4 planned open, and 4 requiring conversion from a laparoscopic to an open technique. Cholecystectomy was performed during the initial hospitalization in 48 patients, with a median length of stay of 4 days prior to surgery (range = 0 to 8 days). Seven patients underwent interval elective cholecystectomy (range = 18 to 42 days after initial discharge). Two patients had undergone prior cholecystectomy at other institutions but were included in the study due to acute pancreatitis secondary to retained CBD stones.
MRC
All patients underwent MRC imaging using a 1.5 T Siemens Magnetom Vision Scanner (Siemens Erlanger, Germany) using a circularly polarized body coil. The HASTE (Half Fourier acquisition single-shot turbo spin-echo) MR sequence was used and applied in axial, coronal, and sagittal planes, as previously described.9 A rapid image acquisition time of 13 seconds allowed for scanning during a single breath hold. Total room time was usually less than 10 minutes per patient. Source images were individually assessed and MRC performed by either maximal intensity projection or by thick-slab (20 mm) single-shot technique. No contrast agents, antiperistaltic drugs, or ionizing radiation was used.
All MRC examinations were performed early in each patient's hospitalization and prior to other procedures such as ERCP or surgery. Laboratory and initial imaging studies were performed on the day of admission. The median time interval between these studies and MRC was 1 day (range 0–4) and the median interval to ERCP was 2 days (range 0–6). The median interval between discovery of stones on MRC and surgery was 3 days (range 0–8). MRC images were assessed for the presence of CBD stones, gallbladder stones, acute cholecystitis, and acute pancreatitis. Biliary calculi were identified as round or faceted signal voids within the gallbladder or bile duct on at least 2 imaging planes. Acute cholecystitis was diagnosed by the findings of gallbladder wall thickening and pericholecystic edema fluid, as previously described.10 Evidence of acute pancreatitis included pancreatic enlargement and evidence of peripancreatic fluid.
RESULTS
CBD Stones
Seventeen of the 64 patients with gallstone pancreatitis were found to have CBD stones (27%), all documented at the time of subsequent ERCP. Endoscopic sphincterotomy with stone extraction was successful in all patients except 1 patient who required subsequent percutaneous transhepatic cholangiography and 1 patient who underwent surgical CBD exploration. CBD stones were not present in the remaining 47 patients, as confirmed by ERCP (n = 17), IOC (n = 8), or clinical course (n = 22). MRC correctly identified 16 of the 17 patients with CBD stones (Fig. 1). The one patient who was not identified was noted to have a small stone impacted at the ampulla and a minimally dilated bile duct (9 mm) at ERCP. MRC incorrectly predicted a CBD stone in 1 patient who subsequently had a normal ERCP. This patient was noted to have rapid resolution of symptoms, and it was felt that the stone may have passed in the 4-day interval between MRC and ERCP. The overall sensitivity and specificity of MRC for CBD stone detection was 94% and 98%, respectively.
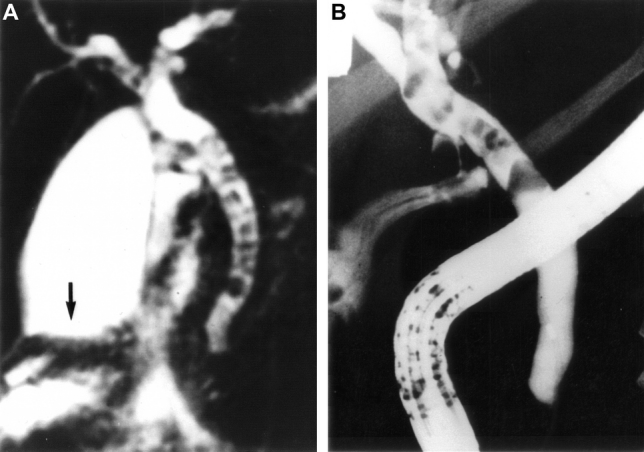
FIGURE 1. Twenty-seven-year-old woman with gallstone pancreatitis. A, MRC demonstrating the gallbladder with dependent gallstones (arrow). A dilated common bile duct is also seen with numerous filling defects consistent with CBD stones. B, ERCP in the same patient confirming CBD stones.
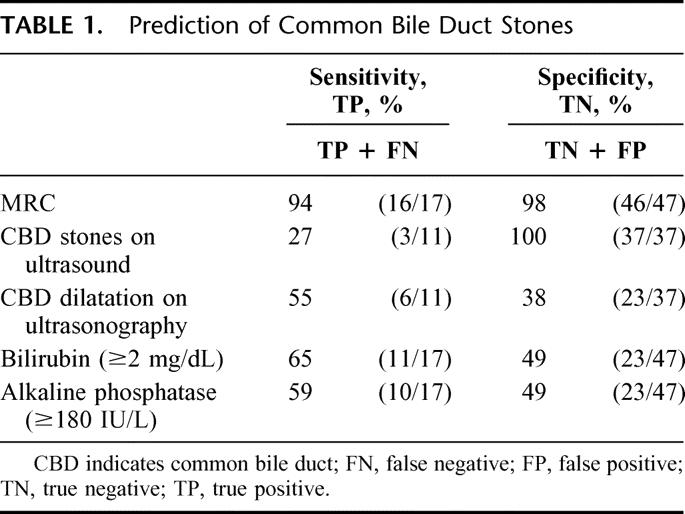
Traditional clinical criteria, including admission laboratory tests and ultrasound images, were also assessed for their ability to predict CBD stones (Table 1). An admission serum bilirubin ≥2 mg/dL was present in 11 of 17 patients with CBD stones and in 24 of the 47 patients without CBD stones, yielding a sensitivity of 65% and a specificity of 49%. An elevated serum alkaline phosphatase (≥180 IU/L) was present in 10 of 17 patients with CBD stones (sensitivity = 59%) and 24 of 47 patients without CBD stones (specificity = 49%). Abdominal ultrasound was performed in 11 patients with CBD stones and in 37 patients without CBD stones. Ultrasound correctly identified CBD stones in 3 of 11 patients (sensitivity = 27%). Ultrasound correctly predicted the absence of CBD stones in 37 patients (specificity = 100%). Bile duct dilatation (≥8 mm) on ultrasound has also been used to predict CBD stones and biliary obstruction. Twenty-nine of 48 patients were noted to have CBD dilatation on ultrasound examination. The sensitivity and specificity of CBD dilatation as a predictor of CBD stones was 55% (6/11 patients) and 38% (14/37 patients), respectively.
TABLE 1. Prediction of Common Bile Duct Stones
Acute Cholecystitis and Gallbladder Stones
Of the 62 patients with gallbladders containing gallstones, MRC correctly demonstrated gallbladder stones in 57 patients (sensitivity = 92%). Ultrasonography was performed in 46 patients, and gallstones were correctly identified in 42 patients (sensitivity = 91%). Acute cholecystitis was evident on gallbladder pathology and demonstrated intraoperatively in 8 of the 48 patients undergoing cholecystectomy during the initial admission. MRC demonstrated pericholecystic fluid consistent with acute gallbladder inflammation in 6 of the 8 patients (sensitivity = 75%) (Fig. 2). MRC correctly predicted the absence of acute gallbladder inflammation in 35 of 40 patients, for a specificity of 88%. The 2 patients with acute cholecystitis not predicted by MRC also had no evidence of acute cholecystitis on ultrasound. Overall, ultrasound data was used in 6 patients with acute cholecystitis and correctly predicted acute cholecystitis in 3 of these 6 patients.
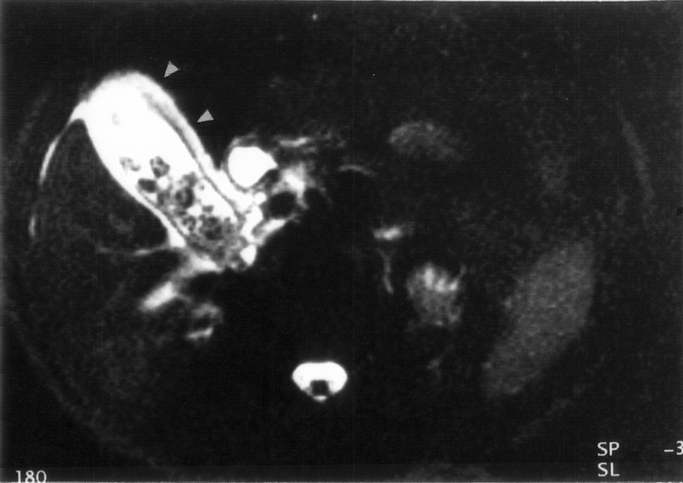
FIGURE 2. Cross-sectional MRC image of a patient with acute cholecystitis. Pericholecystic edema and inflammation appears as a white halo around the gallbladder (arrowheads).
Acute Pancreatitis
Pancreatic enlargement and peripancreatic fluid consistent with pancreatitis were evident on MRC in 45 of the 64 patients (70%) (Fig. 3). Abdominal CT imaging was available in 36 patients and demonstrated acute pancreatic inflammation in 27 patients (75%). One patient with a history of a previous episode of gallstone pancreatitis was noted to have a 6-cm pancreatic pseudocyst identified by both MRC and CT. Of the 36 patients undergoing both CT and MRC, the 2 studies agreed on the presence of acute pancreatitis in 24 patients and the absence of pancreatitis in 5 patients. MRC visualized changes consistent with pancreatitis in an additional 4 patients not seen by CT, whereas CT alone demonstrated acute pancreatitis in 3 patients not evident by MRC. All patients with evidence of pancreatitis on imaging studies had mild to moderate pancreatic inflammation without evidence of necrosis or abscess formation.
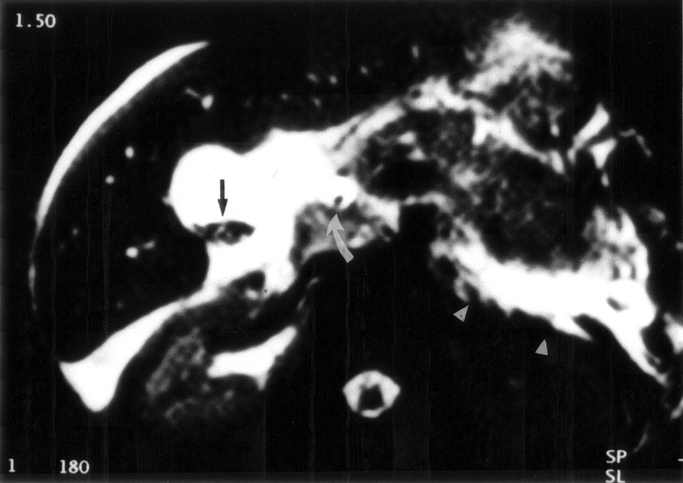
FIGURE 3. Cross-sectional MRC in a patient with biliary obstruction and acute pancreatitis. Pancreatic inflammation is present with an enlarged pancreas surrounded by acute fluid collections (appearing white on MRC) (arrowheads). Also seen is the gallbladder with stones (arrow) and a dilated common bile duct with an intraluminal stone (curved arrow).
DISCUSSION
MRC is a relatively new imaging modality that has been advocated as an alternative to direct cholangiography. In the present study, MRC was able to accurately identify persistent CBD stones in all but 1 patient with gallstone pancreatitis, and it also assisted in the diagnosis of cholelithiasis, acute cholecystitis, and pancreatitis. The main advantage of MRC is its noninvasiveness, excluding the need for intravenous contrast dye or ionizing radiation and the associated risks of renal failure and radiation exposure accordingly. It also has the benefit of being relatively operator independent, whereas the quality of other imaging modalities such as ultrasonography and ERCP may have significant variation related to operator expertise. Further, MRC has the advantage of accurately demonstrating both intraductal and extraductal biliary anatomy, as well as general regional anatomy and pathology. The main contraindications to MRC are severe obesity (exceeding the weight limit of the MR scanner), severe claustrophobia, and the presence of magnetic devices such as implanted cardiac pacemakers. Overall, MRC is a safe and standardized means of studying the hepaticopancreatic and biliary system.
The foremost clinical implication of MRC from this study is its ability to accurately detect CBD stones and, thus, noninvasively select those patients most likely to benefit from a preoperative intervention such as ERCP. The potential morbidity of ERCP including hemorrhage, perforation, and pancreatitis is as high as 10% and may be increased in the setting of preexistent acute pancreatitis.11,12 For this reason, the current use of ERCP as a routine screening tool for purely diagnostic purposes carries substantial risks. Unfortunately, traditional clinical and radiographic criteria used to predict CBD stones, such as elevated liver enzymes and ultrasonography, are nonspecific and unreliable, as seen in this study and others.13–15
This is the first study, to our knowledge, that specifically addresses the use of MRC to detect CBD stones in a large group of patients with gallstone pancreatitis. In a recent study, Hochwald et al16 reported on a subset of 10 patients with gallstone pancreatitis who underwent MRC. Only 1 of these patients had CBD stones, and these stones were missed by MRC. Other studies involving MRC and biliary obstruction without pancreatitis have shown similar results, with the sensitivities of CBD stone detection ranging from 81% to 100%.16–20 Small stone size8 and peripancreatic edema are factors encountered with gallstone pancreatitis that have been suggested to potentially impair the ability of MRC to visualize CBD stones. However, we found these factors to have little impact and that MRC correctly predicted CBD stones in 16 of 17 patients (94%).
The importance of identifying and removing persistent CBD stones early in the course of gallstone pancreatitis has been addressed in several randomized prospective studies. Neoptolemos and colleagues3 randomized patients with gallstone pancreatitis to receive either conventional conservative therapy or urgent ERCP within 72 hours of onset of symptoms. They found a reduction in morbidity and hospital stay in patients with predicted severe pancreatitis who underwent urgent ERCP. In a similar study, Fan et al4 noted a reduction in biliary sepsis, as well as reduced morbidity, in patients randomized to urgent ERCP. The authors concluded that all patients with gallstone pancreatitis should undergo urgent preoperative ERCP, and this recommendation has been affirmed by other authors.21,22 Conversely, some investigators argue that urgent ERCP and endoscopic sphincterotomy only benefit those few patients who actually have CBD stones.5–7 Although removal of obstructing stones may prevent the development of biliary sepsis and the progression of mild to severe pancreatitis, this may be outweighed by the cost and potential morbidity incurred by patients whose stones have already passed. MRC provides an attractive solution to this dilemma in its ability to accurately identify those patients with persistent CBD stones in the first 48 hours of admission, when therapeutic intervention can have its greatest impact.23
Another diagnostic option to detect possible persistent CBD stones is IOC at the time of cholecystectomy. CBD stones can then be managed by laparoscopic or open CBD exploration or postoperative ERCP.6 This has the theoretical advantage of postponing cholangiography for 4–5 days while awaiting surgery and allowing the maximal number of stones to pass on their own. Most stones that spontaneously pass, however, will have done so by admission or within the first 48 hours of the onset of symptoms.24 The duration of ampullary obstruction by CBD stones appears to be an important determinant of the severity of pancreatic injury.23 A potential therapeutic window for favorably impacting on disease progression may be lost if cholangiography is delayed until the time of cholecystectomy.
In addition to detecting choledocholithiasis, we also found MRC to be quite helpful in identifying other biliary pathology. Gallstones were imaged with a sensitivity similar to that of ultrasonography. MRC was also able to predict acute cholecystitis, as we have previously reported.10 Acute pancreatitis was seen by MRC in 75% of patients, and these images closely paralleled the findings of pancreatitis on CT. Complications of acute pancreatitis such as pseudocyst formation were also easily identified. Most patients in this study were noted to have mild to moderate pancreatitis, and we did not attempt to correlate the predicted severity of pancreatitis at admission with specific findings on MRC. In a recent study, however, noncontrast MRC was found to be as accurate as contrast-enhanced CT in predicting the severity of pancreatitis and identifying pancreatic necrosis.25
We recommend that MRC be performed as the initial diagnostic study in patients presenting with acute pancreatitis not attributable to alcohol abuse or other known etiologies. If gallstones are seen and the CBD is clear of stones on MRC, the patient can proceed to laparoscopic cholecystectomy once the acute pancreatic inflammation has subsided. Diagnostic ultrasound, CT, ERCP, and IOC can be avoided in the large majority of patients. If CBD stones are visualized on MRC, then urgent ERCP with stone extraction can be performed, followed by cholecystectomy later in the hospital stay. In the current study, the negative predictive value and positive predictive value of MRC for the presence of CBD stones was 98% and 94%, respectively. The decision to perform or not perform ERCP can, therefore, be made with a high degree of confidence, sparing many patients the morbidity and mortality associated with ERCP. Farrell et al26 constructed a theoretical model to predict the potential benefit of using MRC as a screening tool prior to ERCP in a variety of clinical settings. He found that MRC would have avoided ERCP in 197 patients (43%) over a 3-year period at his center. Moreover, he predicted that MRC would have avoided ERCP-related complications in 40 patients (3.5%) and ERCP-related mortality in 4 patients (0.35%).
In conclusion, MRC appears to be an ideal imaging modality in the initial evaluation of patients with gallstone pancreatitis. Gallstones and gallbladder inflammation can be detected by MRC with sensitivities similar to that obtained with ultrasonography. Cholangiograms can be generated that rival ERCP in their ability to predict CBD stones. MRC also appears to be as accurate as CT for depicting varying degrees of pancreatitis and may prove to have prognostic value with respect to predicting severity of disease. We believe that MRC is an excellent initial imaging modality and has the potential to replace other diagnostic studies in the evaluation of patients with suspected gallstone pancreatitis, selecting those patients most likely to benefit from therapeutic endoscopy or surgical intervention.
ACKNOWLEDGMENTS
The authors thank Dr. Julie A. Freischlag (Johns Hopkins Hospital) for her support with this research, and Dr. Julie Ritner (Brown University Hospital, Rhode Island) for her wisdom on applications of magnetic resonance imaging.
Footnotes
Reprints: Martin A. Makary MD, MPH, Assistant Chief of Service, Department of Surgery, Johns Hopkins Hospital, Blalock 658, 600 N Wolfe St, Baltimore, MD 21287-4658. E-mail: mmakary1@jhmi.edu.
REFERENCES
- 1.Opie EL. The etiology of acute hemorrhagic pancreatitis. Johns Hopkins Hosp Bull. 1901;121:182–188. [Google Scholar]
- 2.Acosta JM, Ledesma CL. Gallstone migration as a cause of acute pancreatitis. N Engl J Med. 1974;290:484–487. [DOI] [PubMed] [Google Scholar]
- 3.Neoptolemos JP, Carr-Locke DL, London NJ, et al. Controlled trial of urgent endoscopic retrograde cholangiopancreatography and endoscopic sphincterotomy versus conservative treatment for acute pancreatitis due to gallstones. Lancet. 1988;2:979–983. [DOI] [PubMed] [Google Scholar]
- 4.Fan S-T, Lai ECS, Mok FPT, et al. Early treatment of acute biliary pancreatitis by endoscopic papillotomy. N Engl J Med. 1993;328:228–232. [DOI] [PubMed] [Google Scholar]
- 5.Folsch U, Nitsche R, Ludtke R, et al. Early ERCP and papillotomy compared with conservative treatment for acute biliary pancreatitis. N Engl J Med. 1997;336:237–242. [DOI] [PubMed] [Google Scholar]
- 6.Chang L, Lo S, Stabile BE, et al. Preoperative versus postoperative endoscopic retrograde cholangiopancreatography in mild to moderate gallstone pancreatitis. Ann Surg. 2000;231:82–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hammarstrom L-E, Anderson R, Stridbeck H, et al. Influence of bile duct stones on patient features and effect of endoscopic sphincterotomy on early outcome of edematous gallstone pancreatitis. World J Surg. 1999;23:12–17. [DOI] [PubMed] [Google Scholar]
- 8.Diehl AK, Holleman DR, Chapman JB, et al. Gallstone size and risk of pancreatitis. Arch Intern Med. 1997;157:1674–1678. [PubMed] [Google Scholar]
- 9.Regan F, Smith D, Khazan R, et al. MR cholangiography in biliary obstruction using half-Fourier acquisition. J CAT. 1996;20:627–632. [DOI] [PubMed] [Google Scholar]
- 10.Regan F, Schaefer DC, Smith DP, et al. The diagnostic utility of HASTE MRI in the evaluation of acute cholecystitis. J CAT. 1998;22:638–642. [DOI] [PubMed] [Google Scholar]
- 11.Bilbao MK, Dotter CT, Lee TG, et al. Complications of endoscopic retrograde cholangiopancreatography (ERCP): a study of 10,000 cases. Gastroenterology. 1976;70:314–320. [PubMed] [Google Scholar]
- 12.Mehta SN, Pavone E, Barkun JS, et al. Predictors of post ERCP complications in patients with suspected choledocholithiasis. Endoscopy. 1998;30:457–463. [DOI] [PubMed] [Google Scholar]
- 13.Blackbourne LH, Earnhardt RC, Sistrom CL, et al. The sensitivity and role of ultrasound in the evaluation of biliary obstruction. Am Surg. 1994;60:683–690. [PubMed] [Google Scholar]
- 14.Koo KP, Traverso LW. Do preoperative indicators predict the presence of common bile duct stones during laparoscopic cholecystectomy? Am J Surg. 1996;171:495–499. [DOI] [PubMed] [Google Scholar]
- 15.Robertson GSM, Jagger C, Johnson PRV, et al. Selection criteria for preoperative endoscopic retrograde cholangiopancreatography in the laparoscopic era. Arch Surg. 1996;131:89–94. [DOI] [PubMed] [Google Scholar]
- 16.Hochwald SN, Dobryansky M, Rofsky NM, et al. Magnetic resonance cholangiopancreatography accurately predicts the presence or absence of choledocholithiasis. J Gastrointest Surg. 1998;2:573–579. [DOI] [PubMed] [Google Scholar]
- 17.Magnuson TH, Bender JS, Duncan MD, et al. Utility of magnetic resonance cholangiography in the evaluation of biliary obstruction. J Am Coll Surg. 1999;189:63–72. [DOI] [PubMed] [Google Scholar]
- 18.Guibaud L, Bret PM, Reinhold C, et al. Bile duct obstruction and choledocholithiasis: diagnosis with MR cholangiography. Radiology. 1995;197:109–115. [DOI] [PubMed] [Google Scholar]
- 19.Fulcher AS, Turner MA, Capps G, et al. Half-fourier RARE MR cholangiopancreatography: experience in 300 subjects. Radiology. 1998;207:21–32. [DOI] [PubMed] [Google Scholar]
- 20.Lomanto D, Pavone P, Laghi A, et al. Magnetic resonance cholangiopancreatography in the diagnosis of biliopancreatic disease. Am J Surg. 1997;174:33–38. [DOI] [PubMed] [Google Scholar]
- 21.Sharma VK, Howden CW. Meta-analysis of randomized controlled trials of endoscopic retrograde cholangiography and endoscopic sphincterotomy for the treatment of acute biliary pancreatitis. Am J Gastroenterol. 1999;94:3211–3214. [DOI] [PubMed] [Google Scholar]
- 22.Karjalainen J, Airo I, Nordback I. Routine early endoscopic cholangiography, sphincterotomy and removal of common duct stones in acute gallstone pancreatitis. Eur J Surg. 1992;158:549–553. [PubMed] [Google Scholar]
- 23.Acosta JM, Rubio Galli OM, Rossi R, et al. Effect of duration of ampullary gallstone obstruction on severity of lesions of acute pancreatitis. J Am Coll Surg. 1997;183:499–504. [PubMed] [Google Scholar]
- 24.Acosta JM, Ronzano GD, Pellegrini CA. Ampullary obstruction monitoring in acute gallstone pancreatitis: a safe, accurate and reliable method to detect pancreatic ductal obstruction. Am J Gastroenterol. 2000;95:122–127. [DOI] [PubMed] [Google Scholar]
- 25.Lecesne R, Taourel P, Bret PM, et al. Acute pancreatitis: interobserver agreement and correlation of CT and MR cholangiopancreatography with outcome. Radiology. 1999;211:727–735. [DOI] [PubMed] [Google Scholar]
- 26.Farrell RJ, Noonan N, Mahmud N, et al. Potential impact of magnetic resonance cholangiopancreatography workload and complication rate in patients referred because of abdominal pain. Endoscopy. 2001;33:668–675. [DOI] [PubMed] [Google Scholar]


