Abstract
Objective:
We sought to examine the effect of subspecialty training on operative mortality following lung resection.
Summary Background Data:
While several different surgical subspecialists perform lung resection for cancer, many believe that this procedure is best performed by board-certified thoracic surgeons.
Methods:
Using the national Medicare database 1998 to 1999, we identified patients undergoing lung resection (lobectomy or pneumonectomy) for lung cancer. Operating surgeons were identified by unique physician identifier codes contained in the discharge abstract. We used the American Board of Thoracic Surgery database, as well as physician practice patterns, to designate surgeons as general surgeons, cardiothoracic surgeons, or noncardiac thoracic surgeons. Using logistic regression models, we compared operative mortality across surgeon subspecialties, adjusting for patient, surgeon, and hospital characteristics.
Results:
Overall, 25,545 Medicare patients underwent lung resection, 36% by general surgeons, 39% by cardiothoracic surgeons, and 25% by noncardiac thoracic surgeons. Patient characteristics did not differ substantially by surgeon specialty. Adjusted operative mortality rates were lowest for cardiothoracic and noncardiac thoracic surgeons (7.6% general surgeons, 5.6% cardiothoracic surgeons, 5.8% noncardiac thoracic surgeons, P = 0.001). In analyses restricted to high-volume surgeons (>20 lung resections/y), mortality rates were lowest for noncardiac thoracic surgeons (5.1% noncardiac thoracic, 5.2% cardiothoracic, and 6.1% general surgeons) (P < 0.01 for difference between general surgeons and thoracic surgeons). In analyses restricted to high-volume hospitals (>45 lung resections/y), mortality rates were again lowest for noncardiac thoracic surgeons (5.0% noncardiac thoracic, 5.3% cardiothoracic, and 6.1% general surgeons) (P < 0.01 for differences between all 3 groups).
Conclusions:
Operative mortality with lung resection varies by surgeon specialty. Some, but not all, of this variation in operative mortality is attributable to hospital and surgeon volume.
To examine the effect of surgeon specialty on operative mortality with lung resection, we studied operative mortality rates across general, cardiothoracic, and noncardiac thoracic surgeons using the national Medicare database during the years 1998 to 1999. Overall, adjusted operative mortality rates were lowest for cardiothoracic and noncardiac thoracic surgeons. Some, but not all, of this variation in operative mortality is attributable to hospital and surgeon volume.
Many believe that subspecialty training may improve surgical outcomes in high-risk surgery. Examples of this finding have been published across a wide range of surgical subspecialties. For example, in carotid endarterectomy, vascular surgeons were found to have lower in-hospital mortality and stroke rates than neurosurgeons or general surgeons.1 In colorectal cancer, several studies have found that colorectal surgeons have lower local and overall recurrence rates.2–5 While many believe that additional subspecialty training can result in improved outcomes in complex procedures, it is important to note that not all studies examining this effect6 have found a significant differences across surgeon specialty.
However, the impact of surgeon specialty on outcomes with lung cancer surgery is uncertain. Surgeons that are board-certified in thoracic surgery have greater training in thoracic procedures than general surgeons. Moreover, some thoracic surgeons eschew cardiac procedures, focusing primarily on lung procedures. Although 1 study7has compared outcomes by specialty, this study was relatively small, restricted to 1 state, and was limited in examination of potentially confounding variables, such as hospital setting and hospital volume in lung resection.
Although many believe lung resection is best performed by board-certified thoracic surgeons, the empiric basis for this assumption has not been established. For this reason, we performed a national study comparing operative mortality rates with lung resection between noncardiac thoracic, cardiothoracic, and general surgeons.
METHODS
Patients and Databases
Using data from the national Medicare database in this retrospective cohort study, we obtained 100% national samples from the Health Care Financing Administration's MEDPAR and denominator files for the years 1998 to 1999. This file contains hospital discharge abstracts for acute care hospitalizations of all US Medicare recipients under the hospital (Part A) insurance program. Only patients in fee-for-service arrangements are included in the MEDPAR file. Thus, our sample excludes Medicare patients enrolled in risk-bearing health maintenance organizations (less than 10%) during this time period. We excluded patients under age 65 or over age 99. Further details on the database are available elsewhere.8
We linked patients and surgeons using the unique provider identifier number in each patient record in the Medicare database. We then categorized surgeons into 3 distinct, mutually exclusive subspecialty categories: general surgeons, noncardiac thoracic surgeons, and cardiothoracic surgeons (see Fig. 1). To ensure that we accurately designated thoracic surgeons, we obtained a list of board-certified thoracic surgeons from the American Board of Thoracic Surgery (ABTS), the certifying body for thoracic surgeons. This list was merged with our Medicare file to identify thoracic surgeons. We further characterized thoracic surgeons as cardiothoracic surgeons or noncardiac thoracic surgeons. The former were defined as those performing at least 1 coronary artery bypass graft (CABG) procedure on any Medicare patient during the study period. Thoracic surgeons that did not perform any CABG procedures during the study period were designated as noncardiac thoracic surgeons. Noncardiac thoracic and cardiothoracic surgeons were analyzed separately in the analysis.
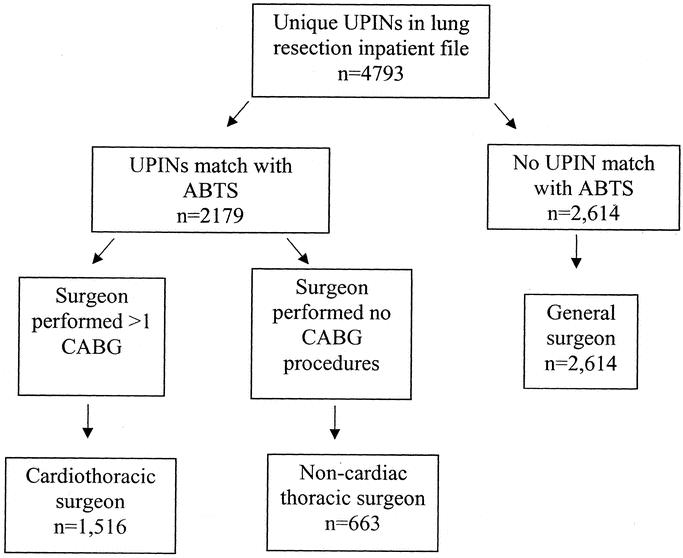
FIGURE 1. Determination of surgeon subspecialty. ABTS, American Board of Thoracic Surgery; N, number of providers; UPIN, Unique Provider Identifier Number.
Analysis
We used the patient as the unit of analysis. Our exposure variable was surgeon specialty (general, cardiothoracic, or noncardiac thoracic), and our main outcome measure was operative mortality, defined as death before discharge or within 30 days of the operative procedure. Deaths occurring after discharge but within 30 days of the operative procedure were captured by using the National Death Index.9
Utilizing methods previously described,8,10 we used multiple logistic regression to study relationships between patient level variables and our main outcome measures. We adjusted for the following variables: age, sex, race (African American, non–African American), and patient comorbidities. Patient comorbidities were identified using information from both the index admission and admission occurring within the preceding 6 months. Comorbidities were compiled into a Charlson score11 for each patient, a commonly used measure of comorbidity status. The Charlson score weights patients based on the number and type of comorbidities recorded in the discharge abstract. Comorbidities typically include diagnoses such as chronic obstructive pulmonary disease, coronary artery disease, or hypertension. We also adjusted for the extent of resection (lobectomy versus pneumonectomy).
We also adjusted for characteristics of the hospital in which each surgeon practiced. For surgeons who operated in more than 1 hospital, we used the hospital in which he or she performed the most cases. Using the 1998 American Hospital Association file, we adjusted for the following variables: teaching status, medical school affiliation, and the presence or absence of a cancer program approved by the American College of Surgeons.
Given the well-documented association between operative mortality and hospital volume,8,12,13 we also adjusted for hospital volume in lung resection. To eliminate any bias introduced by assignment of high- and low-volume cut points, hospital volume was considered as a continuous variable. Given evidence1,7,12,14 that operative mortality varies with surgeon experience, we adjusted for surgeon volume in lung resection, also considered as a continuous variable. In measuring hospital and surgeon volume, we defined volume as the total number of lung resections (both Medicare and non-Medicare patients) treated by the individual hospital or surgeon. Additionally, we adjusted for the effect of clustering15 of patients within surgeons and within hospitals. Results from these regression models were used to generate adjusted mortality rates using predicted risk estimates.
All analyses were performed using STATA (STATA Corporation, College Station, TX). All tests of significance are at the 5% level, and all P values are 2 tailed. The institutional review board at Dartmouth Medical School approved our study protocol.
RESULTS
Patient and Surgeon Characteristics
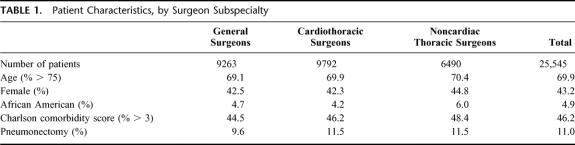
Overall, 25,545 patients were included in our analysis. Of these, 36% underwent lung resection by general surgeons, 39% by cardiothoracic surgeons, and 25% by noncardiac thoracic surgeons. There were no substantial differences in mean age, sex, race, or comorbidity score or between groups (Table 1). Approximately 89% of patients in all groups underwent lobe resection, and approximately 11% underwent pneumonectomy.
TABLE 1. Patient Characteristics, by Surgeon Subspecialty
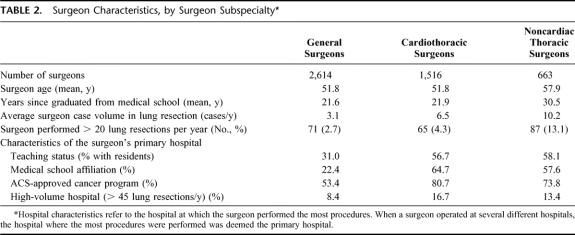
Overall, 2614 general surgeons, 1516 cardiothoracic surgeons, and 663 noncardiac thoracic surgeons were included in our analysis (Table 2). Surgeon characteristics varied by specialty. Thoracic surgeons, on average, were slightly older, had higher procedure volumes in lung resection, and were more likely to practice in high-volume hospitals than general surgeons. Hospitals serving as the primary hospitals for cardiothoracic and noncardiac thoracic surgeons were more likely to be teaching institutions, employ residents, be affiliated with a medical school, and be a part of an American College of Surgeons cancer program than the primary hospitals for general surgeons.
TABLE 2. Surgeon Characteristics, by Surgeon Subspecialty
Operative Mortality by Surgeon Specialty
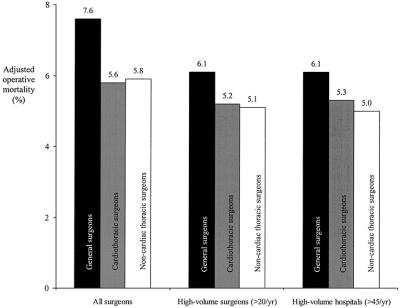
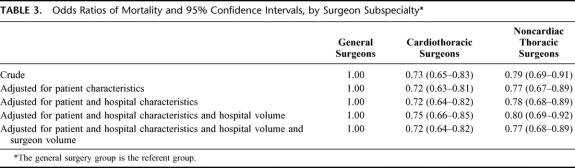
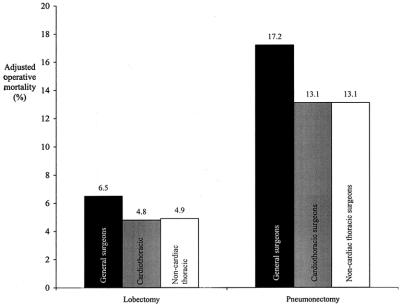
Adjusted operative mortality rates varied by surgeon specialty (Fig. 2). The lowest mortality rates were seen in patients undergoing surgery by thoracic surgeons. Adjusted operative mortality rates ranged from 5.6% with cardiothoracic surgeons to 5.8% with noncardiac thoracic surgeons to 7.6% with general surgeons (P < 0.001 for difference general and thoracic surgeons). Odds ratios of operative mortality are shown in Table 3, using the general surgery group as the referent group. Crude odds ratios are shown in the first row, while odds ratios adjusted for patient, hospital, and surgeon characteristics are shown in the latter rows. The crude odds ratios show a relative reduction in the odds of operative mortality across surgeon specialties of greater than 20%. This effect changes little when adjusting for patient and hospital characteristics. When we adjust for continuous measures of surgeon and hospital volume, the effect is only slightly attenuated for both cardiothoracic surgeons and noncardiac thoracic surgeons.
FIGURE 2. Adjusted operative mortality with lung resection, by surgeon specialty, stratified by surgeon and hospital volume, at the patient level.
TABLE 3. Odds Ratios of Mortality and 95% Confidence Intervals, by Surgeon Subspecialty
We then examined whether specialty-related differences persisted in analysis restricted to high-volume surgeons and high-volume hospitals. First, we restricted our analysis to only high-volume surgeons (>20 lung resections/y, the highest 25th percentile of surgeon volume). Only a small percentage of general and cardiothoracic surgeons were high-volume surgeons (2.7% and 4.3%, respectively), while over 13% of noncardiac thoracic surgeons were high-volume surgeons. Within the group of high-volume surgeons, adjusted operative mortality rates were lowest for noncardiac thoracic (5.1%) and cardiothoracic surgeons (5.2%), and slightly higher for general surgeons (6.1%) (P < 0.01 for difference between general surgeons and thoracic surgeons).
Second, we limited our analysis to high-volume hospitals (>45 lung resections/y, the highest 25th percentile of hospital volume). Within high-volume hospitals, a trend similar to the subgroup analysis of surgeon volume was noted. Adjusted operative mortality rates were lowest for noncardiac thoracic surgeons (5.0%) and cardiothoracic surgeons (5.3%), and slightly higher for general surgeons (6.1%) (P < 0.01 for differences between all 3 groups).
Last, we examined if the extent of resection affected the effect of surgeon specialty. While baseline risks were more than twice as high in pneumonectomy, adjusted operative mortality continued to be highest among general surgeons and lowest among thoracic surgeons (Fig. 3), irrespective of the extend of resection.
FIGURE 3. Adjusted operative mortality with lung resection, by procedure type (pneumonectomy or lobectomy). NCTS, noncardiac thoracic surgeons.
DISCUSSION
Our study of lung resection compared operative mortality in lung resection across surgical subspecialties. While we found that overall, board-certified thoracic surgeons have lower rates of operative mortality in lung resection than general surgeons. However, when we restricted our analysis to high-volume surgeons or high-volume hospitals, the differences in operative mortality between general and thoracic surgeons were less pronounced. Therefore, while operative volume explains some of the difference between general and thoracic surgeons, other patient, surgeon, and hospital factors are likely to influence a patient's operative risk with lung resection.
Our study has several limitations. First, our study is based on administrative data from Medicare. As the limits of administrative data for risk adjustment have been well documented,16,17 we may not have adequately accounted for differences in case mix across surgical specialties. However, it is important to note that observed differences in patient characteristics were quite small, and what small trends there were tended to suggest increased operative risk in the patients of thoracic surgeons. Second, our study may not have classified every surgeon's specialty correctly in every case. Despite using a registry of thoracic surgeons taken directly from the ABTS, some thoracic surgeons, because of the time required for licensure, may have been incorrectly identified as general surgeons. However, misclassifications such as this would tend to bias our results toward the null. Additionally, we did not account for lung cancer stage in our analysis. However, while long-term survival is clearly stage dependent,18 there is little evidence that operative mortality varies significantly by stage. And last, while preoperative chronic obstructive pulmonary disease is captured as a comorbidity in our dataset, data from patient-level pulmonary function tests to quantify the overall severity of the patient's chronic lung disease are not available in our dataset. Future work in this area should aim to incorporate data using patient-level pulmonary function testing, using clinical databases such as the Society of Thoracic Surgeons General Thoracic Surgery Database.19
Despite these limitations, our study has important strengths. First, our study uses a large, national cohort of patients to obtain what may be the most precise estimates published to date of operative mortality rates of lung resection across different surgical subspecialties. Second, our study explores what may be different about thoracic surgeons, in terms of practice patterns and case volume. To our review, there is only 1 previously published study comparing the outcomes of general and thoracic surgeons. This study examined lung resection in South Carolina between 1991 and 1995,7 reporting slightly lower mortality rates for thoracic surgeons. However, this study was limited to 1 state, was relatively small in sample size (1583 cases), and used data that are nearly a decade old. Additionally, this study did not differentiate between those surgeons who focus specifically on noncardiac thoracic surgery and cardiothoracic surgeons, who perform both heart and lung surgery.
Our study demonstrated significant differences in performance in lung resection across surgical subspecialties. However, these differences may not be singularly attributable to the additional training undertaken by ABTS-certified thoracic surgeons. There were also structural differences between thoracic and general surgeons in practice settings. First, thoracic surgeons, both cardiothoracic and noncardiac thoracic, were more likely to practice in larger hospitals than general surgeons. Second, hospitals where thoracic surgeons practice were also more likely to have medical school affiliations and American College of Surgeons–approved oncology programs. Third, thoracic surgeons, especially noncardiac thoracic surgeons, on average had larger case volumes than general surgeons. While our results have adjusted for several of these factors, there are likely several other unmeasured structural differences between the practices of general and thoracic surgeons that translate into improved outcomes.
Similarly, given that structural aspects of care differed between thoracic and general surgeons, one may suspect that processes of care may differ by surgeon specialty as well. Several examples of possible processes of care that may differ across specialty are easily imaginable. First, improvements in preoperative patient selection, such as the use of modalities such as PET scans,20 might help high-performing surgeons identify patients who are unlikely to benefit from resection. Second, the use of epidural catheters to aid in intraoperative and postoperative pain management might help lower risks of postoperative pulmonary complications.21 Third, certain surgeons and hospital systems may be more likely to provide postoperative care for their patients in ICU staffed by full-time intensivist, a process of care shown to decrease mortality and length of stay.22 However, measuring differences in the implementation and results of these process remains difficult, as many of these potentially important processes are not evaluated, even within organized quality improvement initiatives such as the Society of Thoracic Surgery General Thoracic Surgery Database.19
In conclusion, our study demonstrated that operative mortality with lung resection varies by surgeon specialty. Thoracic surgeons, on average, had the lowest operative mortality rates. However, the relationship of operative mortality and surgeon specialty was sensitive to surgeon and hospital characteristics, most notably volume. High-volume surgeons, regardless of specialty, had excellent outcomes. Future quality-improvement efforts in thoracic surgery should study what it is that high-volume providers do differently to achieve better outcomes in lung resection. Then, by identifying and disseminating structural variables and processes of care associated with better outcomes, there is potential to improve patient care at all hospitals performing thoracic surgery.
Footnotes
Dr. Birkmeyer was supported by a grant from the Agency for Healthcare Research and Quality (R01 HS10141-01).
The views expressed herein do not necessarily represent the views of the Department of Veterans Affairs or the United States Government.
Reprints: Philip P. Goodney, MD, Department of Surgery, Dartmouth-Hitchcock Medical Center, Lebanon NH 03765. E-mail: philip.goodney@hitchcock.org.
REFERENCES
- 1.Hannan EL, Popp AJ, Feustel P, et al. Association of surgical specialty and processes of care with patient outcomes for carotid endarterectomy. Stroke. 2001;32:2890–2897. [DOI] [PubMed] [Google Scholar]
- 2.Reinbach DH, McGregor JR, Murray GD, et al. Effect of the surgeon's specialty interest on the type of resection performed for colorectal cancer. Dis Colon Rectum. 1994;37:1020–1023. [DOI] [PubMed] [Google Scholar]
- 3.Read TE, Myerson RJ, Fleshman JW, et al. Surgeon specialty is associated with outcome in rectal cancer treatment. Dis Colon Rectum. 2002;45:904–914. [DOI] [PubMed] [Google Scholar]
- 4.Dorrance HR, Docherty GM, O'Dwyer PJ. Effect of surgeon specialty interest on patient outcome after potentially curative colorectal cancer surgery. Dis Colon Rectum. 2000;43:492–498. [DOI] [PubMed] [Google Scholar]
- 5.Wigmore SJ, Madhavan K, Currie EJ, et al. Does the subspecialty of the surgeon performing primary colonic resection influence the outcome of patients with hepatic metastases referred for resection? Ann Surg. 1999;230:759–765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cowan JA Jr, Dimick JB, Thompson BG, et al. Surgeon volume as an indicator of outcomes after carotid endarterectomy: an effect independent of specialty practice and hospital volume. J Am Coll Surg. 2002;195:814–821. [DOI] [PubMed] [Google Scholar]
- 7.Silvestri GA, Handy J, Lackland D, et al. Specialists achieve better outcomes than generalists for lung cancer surgery. Chest. 1998;114:675–680. [DOI] [PubMed] [Google Scholar]
- 8.Birkmeyer JD, Siewers AE, Finlayson EV, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346:1128–1137. [DOI] [PubMed] [Google Scholar]
- 9.National Death Index home page. Available at: http://www.cdc.gov/nchs/r&d/ndi/ndi.htm. Accessed October 16, 2003.
- 10.Goodney PP, Siewers AE, Stukel TA, et al. Is surgery getting safer? national trends in operative mortality. J Am Coll Surg. 2002;195:219–227. [DOI] [PubMed] [Google Scholar]
- 11.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis. 1987;40:373–383. [DOI] [PubMed] [Google Scholar]
- 12.Halm EA, Lee C, Chassin MR. Is volume related to outcome in health care? a systematic review and methodologic critique of the literature. Ann Intern Med. 2002;137:511–520. [DOI] [PubMed] [Google Scholar]
- 13.Hannan EL, Kilburn HJ, Bernard H, et al. Coronary artery bypass surgery: the relationship between inhospital mortality rate and surgical volume after controlling for clinical risk factors. Med Care. 1991;29:1094–1107. [PubMed] [Google Scholar]
- 14.Hannan EL, Siu AL, Kumar D, et al. The decline in coronary artery bypass graft surgery mortality in New York State: the role of surgeon volume. JAMA. 1995;273:209–213. [PubMed] [Google Scholar]
- 15.Localio AR, Berlin JA, Ten Have TR, et al. Adjustments for center in multicenter studies: an overview. Ann Intern Med. 2001;135:112–123. [DOI] [PubMed] [Google Scholar]
- 16.Fisher ES, Whaley FS, Krushat WM, et al. The accuracy of Medicare's hospital claims data: progress, but problems remain. Am J Public Health. 1992;82:243–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Iezzoni LI. The risks of risk adjustment. JAMA. 1997;278:1600–1607. [DOI] [PubMed] [Google Scholar]
- 18.Ries L, Eisner M, Kosary C, et al. SEER Cancer Statistics Review 1975–2000. Bethesda, MD: National Cancer Institute; 2003. [Google Scholar]
- 19.Society of Thoracic Surgery General Thoracic Surgery Database Collection Form. Available at: http://www.ctsnet.org/file/GTSDBCollectionToolv1-3.pdf. Accessed February 1, 2003.
- 20.Gupta NC, Graeber GM, Rogers JS 2nd, et al. Comparative efficacy of positron emission tomography with FDG and computed tomographic scanning in preoperative staging of non-small cell lung cancer. Ann Surg. 1999;229:286–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ballantyne JC, Carr DB, deFerranti S, et al. The comparative effects of postoperative analgesic therapies on pulmonary outcome: cumulative meta-analyses of randomized, controlled trials. Anesth Analg. 1998;86:598–612. [DOI] [PubMed] [Google Scholar]
- 22.Pronovost PJ, Angus DC, Dorman T, et al. Physician staffing patterns and clinical outcomes in critically ill patients: a systematic review. JAMA. 2002;288:2151–2162. [DOI] [PubMed] [Google Scholar]