Abstract
Objective:
This review addresses the historical evolution of hiatal hernia (HH) repair and reports in a chronological fashion the major milestones in HH surgery before the laparoscopic era.
Methods:
The medical literature and the collections of the History of Medicine Division of the National Library of Medicine were searched. Secondary references from all sources were studied. The senior author's experience and personal communications are also reported.
Results:
The first report of HH was published in 1853 by Bowditch. Rokitansky in 1855 demonstrated that esophagitis was due to gastroesophageal reflux, and Hirsch in 1900 diagnosed an HH using x-rays. Eppinger diagnosed an HH in a live patient, and Friedenwald and Feldman related the symptoms to the presence of an HH. In 1926, Akerlund proposed the term hiatus hernia and classified HH into the 3 types that we use today. The first elective surgical repair was reported in 1919 by Soresi. The physiologic link between HH and gastroesophageal reflux was made at the second half of the 20th century by Allison and Barrett. In the midst of a physiologic revolution, Nissen and Belsey developed their famous operations. In 1957, Collis published his innovative operation. Thal described his technique in 1965, and in 1967, Hill published his procedure. Many modifications of these procedures were published by Pearson and Henderson, Orringer and Sloan, Rossetti, Dor, and Toupet. Donahue and Demeester significantly improved Nissen's operation, and they were the first to truly understand its physiologic mechanism.
Conclusion:
Hiatal hernia surgery has evolved from anatomic repair to physiological restoration.
The treatment of hiatal hernia, a major component of today's surgical practice, was not recognized as a significant clinical entity until the first half of the 20th century, and its relationship with gastroesophageal reflux remained unnoticed until the 1950s. This review addresses the evolution of hiatal hernia surgery and reports the major milestones before the laparoscopic era.
Although congenital and posttraumatic diaphragmatic hernias were described as far back as the 16th century, hiatal hernia was not recognized as a significant clinical entity until the first half of the 20th century. Surprising as it seems to modern surgeons, the relationship between hiatal hernia and gastroesophageal reflux remained unnoticed until the 1950s. In the second half of the 20th century, an appreciation of the pathophysiology of gastroesophageal reflux changed hiatal hernia surgery from simple restoration of anatomy to more physiologic operations. At the dawn of the new millennium, technological advances in both diagnosis and therapy have made treatment of hiatal hernia and gastroesophageal reflux a major component of surgical practice. This review addresses the historical evolution of hiatal hernia repair and reports in a chronological fashion the major milestones in hiatal hernia surgery before the laparoscopic era.
Hiatal Hernia Before the 20th Century
Ambrose Pare (1579), Rivierius Lazari (1689), Giovanni Batista Morgagni (1761), Vincent Alexander Bochdalek (1848), and many other distinguished physicians make up an impressive list of pioneers whose names have been associated with the first descriptions of posttraumatic and congenital diaphragmatic hernias.1 Acquired herniation through the esophageal hiatus (ie, what is now referred to as hiatal hernia) had been described only in passing before the x-ray era. This is probably attributable to the classic autopsy techniques of the time in which the esophagus was usually cut just above the diaphragm and taken out with the heart and lungs, losing all connections with its intra-abdominal segment and stomach.2
In 1819, Rene Theophile Hyacinthe Laennec described posttraumatic and congenital diaphragmatic hernias in his treatise on auscultation, “De l’ auscultation mediate.”3 He stated: “it even appears that the stomach and intestines have at times been known to pass into the chest by the openings which afford a passage of the esophagus, aorta and even to the great sympathetic nerve.” Sir Astley Cooper4 in 1824 also mentioned that protrusion of the viscera through the diaphragm could take place at the natural apertures formed for the passage of esophagus, vena cava, aorta, or through unnatural openings. Cooper considered herniation the result of malformation or injury. In 1853, Henry Ingersoll Bowditch5 reviewed all cases of diaphragmatic hernia published between 1610 and 1846. The collected series of 88 cases, all postmortem findings, contained 3 cases of “dilatation of the esophageal opening,” which Bowditch characterized as “very curious.” In these 3 cases, Bowditch noted that “esophagus presented a very abrupt change of its course. In all, it descended through the diaphragm as usual but turned back toward the left to enter the abnormal aperture caused by the hernia and to join the stomach in the chest.” This was perhaps the first report of what is now classified as a type II or paraesophageal hernia (Fig. 1).
FIGURE 1. Henry Ingersoll Bowditch reviewed the early series of hiatal hernias described at postmortem examination in 1846 and probably should be credited with the first description of what is now referred to as a paraesophageal hernia. (Courtesy of the National Library of Medicine.)
While the recognition of hiatal hernia as a common anatomic abnormality would have to wait for the widespread adoption of x-rays, the damage done to the esophagus by gastroesophageal reflux was postulated in medical literature as early as 1800. Charles Michel Billard6 in Paris published the first case of esophagitis in a child in 1828. Carl Rokitansky,7 a pathologist in Vienna in 1855, demonstrated that esophagitis of the lower esophagus was due to gastroesophageal reflux. His report, however, had little impact on clinical medicine at that time. Many clinicians such as Friedrich Albert von Zenker8 and Sir Morrel Mackenzie9 felt reflux of gastric juice into the esophagus to be only an agonal occurrence with no clinical significance. When Heinrich Quincke10 in Germany attributed 3 cases of esophageal ulceration to the regurgitation of gastric juice in 1879, a heated controversy developed. This controversy persisted for over half a century! Wilder Tileston11 clearly described the typical symptoms of esophagitis in 1906. In his study, he reviewed 41 cases and he added 3 of his own. Although many of these patients had esophageal ulceration, as well as frequent vomiting and pyloric stenosis, the importance of his contribution lies in that Tileston gave a description of the typical symptomatology of esophagitis, and he felt that these symptoms were caused by insufficiency of the cardia. Joseph Sheehan12 described the esophagoscopic findings of esophagitis in 1920, and Porter Vinson13 was the first to note the association between esophagitis and stricture 1 year later. The term peptic esophagitis was introduced in 1934 by Hamperl14 on the basis of his pathologic studies almost 80 years after Rokitansky's work. One year later, Asher Winklestein15 introduced the term in the English literature.
Hiatal Hernia in the First Half of the 20th Century
The advent of radiography was the first important step in the diagnosis and management of hiatal hernia. Around the turn of the century, a first-year medical student at Harvard Medical School (later to become a professor) named Walter Cannon begun a research project with a fellow second-year medical student, Albert Moser, studying deglutition with x-rays using bismuth capsules. The project had been suggested by the professor of physiology Henry Pickering Bowditch. They presented their work before the American Physiologic Society in 1898. Theirs was the first study of the anatomy and physiology of the cardia by means of contrast material.16 One year later, Moriz Benedikt repeated the experiments with a mercury-filled bougie, and in 1900, Hirsch diagnosed a hiatal hernia by means of x-rays and a mercury-filled balloon prior to autopsy. An increasing number of cases began to appear and at the turn of the century; it seemed like a new disease entity had emerged. Four years later, Eppinger diagnosed a hiatal hernia in a live patient.17 He made his diagnosis primarily on the basis of auscultation and then used x-rays to support his clinical judgment. In 1911, Eppinger summarized the literature of diaphragmatic hernia identifying 635 cases, of which only 11 involved the esophageal hiatus.18 In 1925, 33 cases were added by Carl Hedblom19 in an extensive review. In that same year, Julius Friedenwald and Maurice Feldman20 described the typical symptoms for the first time (ie, heartburn) and related these to the presence of a hiatal hernia. They believed that the cause of the hernia was the failure of the muscle surrounding the diaphragm to closely encircle the esophagus. In 1926, Ake Akerlund21 in Stockholm reported 30 more cases, proposed the term hiatus hernia, and classified hiatal hernias into 3 types. Akerlund stated, “Diaphragmatic hernia through the esophageal hiatus may properly be termed hiatus hernia. They are most often true nontraumatic hernias and can be classified in 3 groups: a) hiatus hernias with congenitally shortened esophagus (thoracic stomach), b) paraesophageal hernias, c) hernias not included in a and b.” He also noted that patients with hiatal hernia complained of pain immediately after ingestion of food, frequently associated with heartburn, and sometimes complained of dysphagia. Despite the prevailing opinion at the time, he concluded that hiatal hernia must be a common affliction. In the same year, Robins and Jankelson22 demonstrated radiographically that gastroesophageal reflux was associated with epigastric and substernal discomfort in 90% of their patients with hiatal hernia. In 1930, Max Ritvo,23 a Boston radiologist, published a series of 60 cases drawn from 8000 barium studies he had performed. Ritvo stated that the cause of the “acquired esophageal orifice hernia” is the increased intraabdominal tension, which can be caused by conditions such as constipation, pregnancy and obesity. He also reported epigastric pain, heartburn, nausea, vomiting, and regurgitation as clinical correlates of hiatal hernia in the majority of his patients but concluded that “the complaints are mild and operative measures are only rarely necessary.” Later that year, Moore and Kirklin24 detailed the appropriate radiologic methods for demonstrating the presence of hiatal hernias: the employment of recumbent postures and the manual pressure over the abdomen. The acceptance of hiatal hernia as a distinct entity was not universal. Kirklin pointed out that “the clinical significance of small hernias demonstrable only under more or less artificial conditions has not been fully determined” and Sauerbruch et al25 in 1932 reported that “the radiologic appearance of hiatal hernia occurs in the absence of any symptoms” and considered hiatal hernia an artifact.
The First Operative Trials
In 1919, Angelo Soresi26 published the first treatise describing elective surgical repair of hiatus hernia entitled “Diaphragmatic Hernia. Its Unsuspected Frequency: Its Diagnosis: Technique for Radical Cure.” The aim of his paper was “to call the attention of interns and of surgeons to the frequency of diaphragmatic hernias especially small ones, because patients suffering from this condition are not properly treated.... This lack of interest is not easily explained, because diaphragmatic hernias give rise to so many complicated and serious symptoms, which if not properly attended to, will lead the patient to an unfortunate life and premature death.” Soresi's paper proceeds with almost messianic zeal to attribute a wide variety of abdominal symptoms to the presence of even the smallest hiatal hernias. In spite of being melodramatic, Soresi's report details the original abdominal approach to the hiatus. His operation consisted of reduction of the hernia and closure of the opening of the diaphragm. He described his operative technique such that “the suture has to close in the most perfect manner the opening of the diaphragm especially around the organs that pass through it, esophagus, vena cava, aorta, but without compressing the important organs just mentioned. If the esophagus or the aorta are found in the gap the stitch is somewhat modified: The needle goes through the most superficial layer of the organ that is included in the gap, but the surgeon must be exceedingly careful not to enter the lumen of the organ.”
Following Soresi's report, interest in the surgical treatment of hiatal hernia grew. Stuart Harrington27,28 and his colleagues at The Mayo Clinic published their experience treating 27 patients in 1928. The Mayo clinic group refined the criteria for patient selection, choosing to observe patients whose hiatal hernias were discovered radiographically during the course of a general examination. Patients felt to have symptomatic diaphragmatic hernias were usually approached transabdominally. The operation was basically the one that Soresi had used 10 years earlier. Harrington emphasized that: “closure of the hernia opening is essential for the relief of symptoms.” When he was not able to close the diaphragm, he sutured the herniated viscera to the abdominal wall, a procedure that he called “palliative.” He also introduced phrenic neurectomy via a cervical incision as an adjunct in cases of large hiatal hernias where the hiatus was difficult to close. He reported zero mortality, and his recurrence rate was 12.5%. The correction of hiatus hernia by paralyzing the left hemidiaphragm was tried by other surgeons over the next 2 decades. The results were unpredictable and the method was finally abandoned.
In 1950, Richard Sweet29 from Massachusetts General Hospital published his transthoracic technique. Sweet, using many of the principles developed in the treatment of inguinal hernias, reduced the hernia, crushed the phrenic nerve, and plicated the hernia sac. He then narrowed the hiatus with heavy silk sutures until he could get his index finger between the esophagus and the rim of the hiatus. Sweet suggested that in some cases an additional suture of fascia lata obtained from the left thigh should be used to reinforce the repair. This technique may be the predecessor of the current use of pledgeted sutures. Sweet also reported that in some cases the esophagus was congenitally short, preventing reduction of the stomach into the abdomen. In these cases, he suggested that no attempt to alter the location of the cardia and stomach needed to be made. Two years later, he reported a series of 111 consecutive cases of hiatal herniorrhaphies with good short-term results.30
Hiatal Hernia in the Second Half of the 20th Century
Although it seems surprising to today's surgeons, a physiologic link between hiatal hernia and gastroesophageal reflux had yet to be made as the second half of the 20th century began. Surgical procedures were based solely on anatomic observations. Many surgeons believed that symptoms in patients with hiatal hernias emanated from pinching of the stomach as it traversed the hiatus. The surgeons of the first half of the 20th century had focused on correcting an anatomic defect. To their dismay, many patients had successful restoration of anatomy but persisting symptoms. Surgeons were inclined to focus on the degree of hiatal closure as responsible for persisting symptoms, and some, such as Saeurbruch in Berlin, went so far as to enlarge the hiatal orifice to relieve the presumed constricting effect of the hiatal fibers on the herniated stomach¡
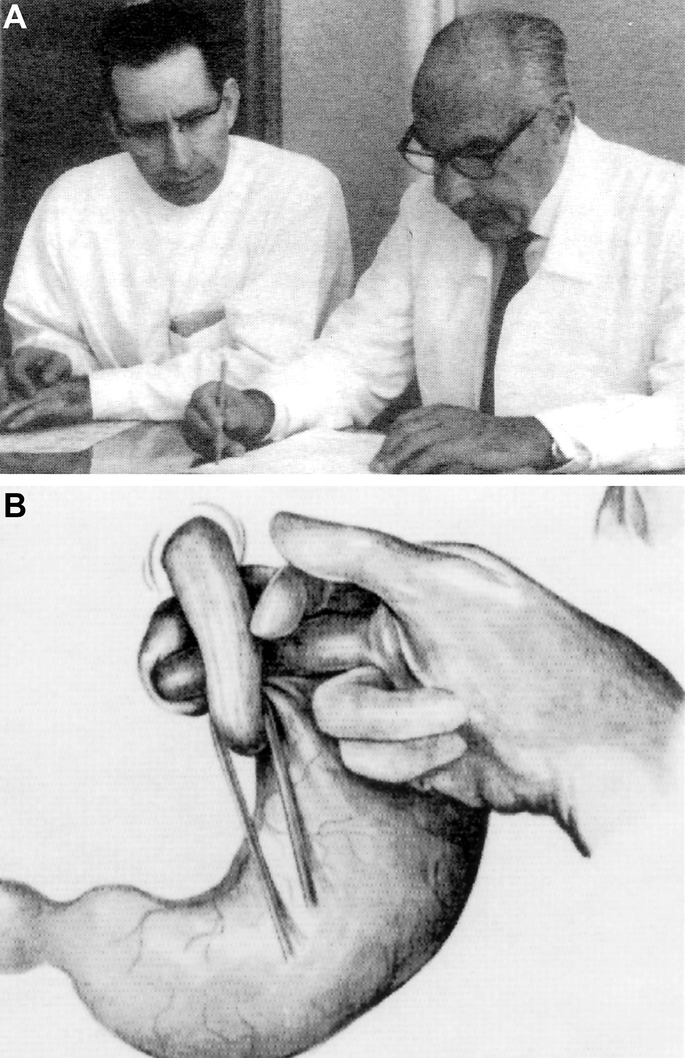
Philip Allison in Leeds and Norman Barrett in London played a major role in changing the established perception of the sliding hernia from that of an anatomic mechanical condition to a functional physiologically based disorder and established that reflux esophagitis and its complications were the physiologic consequences of anatomic abnormalities. Allison should be credited for initiating the modern era of antireflux surgery. In his classic paper published in 1951,31 he aimed to “emphasize the relation between the altered physiology at the cardia, and a common form of indigestion consisting mainly of heartburn, gastric flatulence and postural regurgitation” (Fig. 2A). He attributed the occurrence of these symptoms to reflux esophagitis due to incompetence of the gastroesophageal junction and he stated that “the cause of the incompetence is a sliding hernia of the stomach through the esophageal hiatus of the diaphragm into the posterior mediastinum.” Allison focused on the crural sling as the key factor in preventing reflux. He believed these crural fibers functioned as a pinchcock to prevent reflux. His transthoracic surgical technique consisted of (1) reduction of the herniated cardia back into the abdomen; (2) retention of the cardia to that position by suturing the phrenoesophageal ligament and peritoneum to the abdominal aspect of the diaphragm; and (3) approximation and light suture of the crural fibers behind the esophagus. Allison emphasized the importance of light suture so that the muscle fibers of the hiatus could continue to function. Allison classified hiatal hernia into 2 types: the sliding hernia and the paraesophageal or rolling, now more commonly designated as the type I and type II, and he observed that these 2 types give rise to different symptoms and had a different prognosis.
Allison supported the surgical treatment of sliding hernias for 2 reasons. Primarily, because the symptoms from reflux esophagitis were distressing to the patient and also because he had noticed that “persistent superficial inflammation is liable to be complicated by ulceration or fibrosis with stricture formation, when the surgical treatment may become unavoidable and much more formidable.” Over a 5-year period, Allison saw 204 patients with hiatal hernias, and he had operated on 33 patients with hiatal hernias and esophagitis but no stenosis. There was 1 death, and 30 of 32 surviving patients had excellent short-term results. Twenty-two years later, he reviewed 421 of his own cases and reported a recurrence of the hernia or gastroesophageal reflux in 49% of his sliding hiatal hernia repairs. He was courageous enough to report this to the American Surgical Association meeting in 1973.32
Whereas Allison focused on reduction of the hiatal hernia and proper closure of the diaphragmatic sling, Norman Barrett33 focused on restoration of the cardioesophageal angle as the critical element in the prevention of reflux (Fig. 2B). Long before fiberoptic endoscopies could confirm it, he postulated the presence of a fold of mucosa at the gastroesophageal junction that functioned as a flap valve. Restoration of the cardiophrenic angle was therefore the key objective of an antireflux operations, a concept that became central to subsequent operations developed by Belsey and Hill. Apart from his classic report on the columnar lined esophagus and its ulcerative complications, Barrett also emphasized the frequency of sliding hiatus hernia, the occurrence of paraesophageal hernia, and he discussed the way in which acid reflux is prevented. He reported, “To summarize my views about the rationale of operations to cure reflux esophagitis, I believe that the hernia should be reduced because its presence permits reflux; the esophageal hiatus may sometimes require diminishing in size in the hopes that this maneuver will help to prevent a recurrence of the hernia; the esophagogastric angle should be reconstituted by fixing the cardia below the diaphragm and so allowing the fundus of the stomach to ballon up under the dome.” Barrett considered the phrenoesophageal ligament of no importance, and he believed that the left gastric artery and its mesentery were the anatomic structures that maintained the stomach under the diaphragm in normal people. Barrett's contributions stimulated surgeons to design procedures aimed at improving the function of the cardia rather than simply focusing on hernia reduction.
The confluence of 2 streams of thought, the anatomic focusing on herniation and the physiologic focusing on acid reflux, were critical to the development of modern hiatal hernia surgery. The identification of the lower esophageal sphincter and use of manometry were reported in 1956.34,35 Esophageal pH monitoring would come 2 decades later.36 These tools linked anatomy and physiology to permit accurate diagnosis of reflux disease and provided an objective standard for evaluation of surgery. In the midst of this physiologic revolution, Rudolph Nissen and Ronald Belsey developed the operations used by most surgeons in the 21st century.
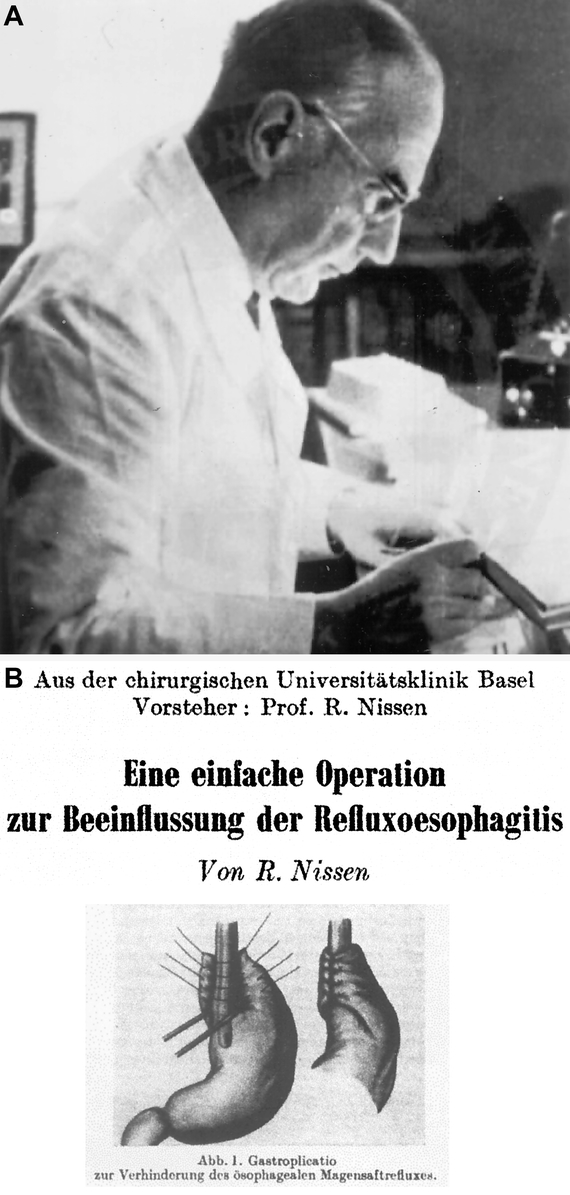
The development of the Nissen fundoplication has been falsely described as an example of progress in surgery by accident. In fact, Rudolf Nissen was a man of great power of observation, and his pioneering contribution was the result of 30 years of surgical trials (Fig. 3). Nissen, the son of a Prussian physician, began his career in Munich as an associate to Professor Sauerbruch. Although Nissen was to be remembered for the development of his antireflux operation, he began his career performing surgery for victims of tuberculosis. He was the first Western surgeon to perform a successful pneumonectomy, reporting this in 1931, 2 years before Evarts Graham did so in the United States.37 When Hitler enacted the Jewish Boycott in 1933, Nissen fled from Berlin and became chief of surgery in Istanbul. In 1936, he treated a 28-year-old man with a distal esophageal ulcer penetrating into the pericardium. The procedure performed was a transpleural mobilization and resection of the distal esophagus and cardia with insertion of the esophageal stump into the gastric fundus. In an effort to prevent leakage of the esophagogastric anastomosis, he implanted the distal segment of the esophagus into the anterior wall of the gastric body using the Witzel technique used for gastrostomies. The patient survived, and Nissen noted in follow-up that the patient's reflux symptoms had been abolished.38 In spite of this success, Nissen used the techniques of Harrington and Allison during the 1940s and early 1950s for treatment of hiatal hernias, but he was disappointed by the high incidence of relapses. In 1946, while chief of surgery at Maimonides Hospital in New York, the famous American radiologist Gustav Bucky came to see Nissen, desperately ill from an incarcerated paraesophageal hernia. Nissen reluctantly agreed to operate on Bucky but judged that Bucky was too frail to tolerate a thoracotomy. In spite of the fact that nearly all hiatal hernia repairs had been performed transthoracically, Nissen performed a laparotomy, reduced the hernia, and performed an anterior gastropexy. The patient recovered completely and remained free of symptoms throughout a follow-up of more than 15 years. At that time, Nissen felt that this procedure might prove effective in high-risk elderly patients, and he considered accentuation of the angle of His as the mechanism of action of gastropexy.39 It is unknown if Nissen was aware that Boerema had published the first description of anterior gastropexy (ie, the fixation of the lesser curvature of the stomach to the anterior abdominal wall) as the sole necessary procedure in the surgical repair of hiatus hernia 1 year previously.40 Though transabdominal hernia reduction and gastropexy remain useful adjuncts in the surgical management of paraesophageal hernias, the benefits of anterior gastropexy proved to be short lived for the management of sliding hernias and reflux symptoms. In 1955, disillusioned with the results of gastropexy, Nissen recalled the success of his procedure in Istanbul and opted to create a similar Witzel tube around the esophagus, though this time without esophageal resection. Furthermore, given the large experience with gastroplasty, he decided to perform this procedure transabdominally. Now in Basel, Switzerland, he operated upon a 49-year-old woman with a 3-year history of reflux esophagitis without a hiatal hernia. The phrenoesophageal ligament was divided and the esophagus mobilized, while the short gastric arteries were not divided. Using his right hand, he then passed the gastric fundus behind the stomach through an opening provided by the divided gastrohepatic ligament. A fundoplication was performed wrapping both anterior and posterior walls of the stomach around the lower 6 cm of the esophagus. He used 4 or 5 interrupted sutures, 1 or more of which also incorporated part of the anterior wall of the esophagus. The wrap was performed around a large-bore indwelling intraesophageal stent. The clinical outcome was excellent and was reproduced in a subsequent patient. These 2 cases were published in 1956, and Nissen named the operation gastroplication.41–43
Whereas Nissen relied on his keen sense of memory and intuition, the Belsey Mark IV operation was the culmination of years of observations in the Frenchay endoscopy unit in Bristol, England. Since late 1940s, Ronald Belsey had embarked upon a program of surgical trials based on his endoscopic observations. Using a rigid endoscope and examining the sedated but awake patient in the sitting position, Belsey came to appreciate that reflux was the result of a patulous cardia. Reduction of the cardia below the diaphragm was felt to be a key to maintaining the cardiophrenic angle and hence competence of the lower esophageal sphincter. These observations prompted him to design a new procedure based on the assumption that the restoration and maintenance of an intraabdominal segment of esophagus could play a role in the control of reflux. Belsey assumed that a transthoracic approach was mandatory because extensive mobilization of the esophagus would be routinely necessary to restore the intraabdominal esophageal segment without tension. He focused his efforts on the design of a procedure taking into account 2 main issues: (1) the necessary length of intraabdominal esophagus to be restored; (2) the simplest means of maintaining this segment intraabdominally. Belsey believed that the application of surgical techniques evolved in animal models was unrewarding and consequently these 2 main issues would have to be solved by surgical trial and error. Additionally, he considered long-term follow-up to be the only means for the assessment of a new surgical technique.
Belsey followed his own principles rigorously, and perhaps the most salient lesson derived from his work is his remarkable restraint in deferring publication until the long-term success of his operation was assessed in a large number of patients. He called his final procedure Mark IV to serve notice that this was not his first thought (and possibly not his last) on the subject but the result of a series of surgical trials designated as Marks I, II and III. Mark I was essentially Allison's procedure, while Marks II and III represented various degrees of fundoplication. These initial 3 techniques were tested during the period 1949 to 1955, and the results were unsatisfactory in about a third of the patients. There were also 7 postoperative deaths. The final Mark IV operation was adopted in 1952; Belsey published his findings only after he became sufficiently satisfied with the durability of the technique he had developed. Thus, in 1961, Hiebert44 reported the results of 71 surgically treated patients with symptomatic reflux but no demonstrable hernia, and 6 years later in a classic and extremely influential paper, Skinner and Belsey45 reviewed the long-term follow-up of 1030 patients, most with hiatal hernia. With a minimum follow-up of 5 years, 85% of patients had no reflux symptoms (Fig. 4A).
Another significant development occurred in 1957, when J. Leigh Collis in Birmingham, England, published his innovative operation for treating the difficult problem of the irreducible hiatal hernia, esophagitis and stricture.46 Collis believed that “the acute angle of implantation of the esophagus into the stomach which in turn is produced by the normally functioning crural muscle can be effective alone in controlling gastroesophageal competence.” His goal was to design a procedure to avoid the complicated resectional operations and the endless esophageal dilatations, especially “in the frail and aged.” Collis gastroplasty created controversy and did not prove to fully control reflux esophagitis. Many surgeons reported significant early and late complications, some resulting from the creation of an iatrogenic Barrett's esophagus. The technique, however, was not without significant merit. Robert Henderson and Griffith Pearson47 in Toronto in 1976 combined Collis gastroplasty with the Belsey procedure in a group of difficult patients (previously failed antireflux operation and a shortened esophagus, stricture, transmural ulcerative esophagitis, large combined sliding, and paraesophageal hernia difficult to be reduced without tension) and reported outstanding results. Mark Orringer and Herbert Sloan48 in Ann Arbor combined Collis gastroplasty with the Nissen 360-degree antireflux gastric wrap. The Ann Arbor group also published excellent results. The problem of the firm, fixed, fibrous strictures occurring as a result of peptic esophagitis was also addressed by Alan Thal, who described his technique using a gastric patch in 1965.49
While Nissen was performing his initial fundoplications, Lucius Hill carefully studied the physiology and anatomy of the gastroesophageal junction and esophageal hiatus (Fig. 4B). He further elucidated the mechanism of gastroesophageal reflux using manometry to demonstrate the existence of a high-pressure zone in the terminal esophagus. He also was a pioneer in the use of pH sensing to confirm the diagnosis of gastroesophageal reflux preoperatively and then confirm the physiologic success of his operations. Hill's extensive studies of the anatomy of the esophageal hiatus in cadavers led him to conclude that the strongest portion of the phrenoesophageal membrane lay posteriorly both as direct attachments to the esophagus and the median arcuate ligament. Combining his understanding of lower esophageal sphincter function and anatomy, Hill demonstrated that maintenance of the cardiophrenic angle was the essential element in the control of gastroesophageal reflux. Hill then designed an operation that restored the angle of His by reapproximating the phrenoesophageal bundles and anchoring them to the median arcuate ligament. Hill was as passionate as his rivals, Nissen and Belsey, in proclaiming the superiority of his technique. His original report, “Newer Concepts of the Pathophysiology of Hiatal Hernia and Esophagitis,” lambasted many of his predecessors for poor follow-up and lack of objective determination of reherniation or reflux. He wrote that “these points indicate that current repair of hiatal hernia is in about the same state as repair of inguinal hernia at the time of Bassini and Halsted in 1888. Their recurrence rates for inguinal hernia were lower in 1888 than they are for hiatal hernia in current documented reports.”50 In 1967, Hill published his 8-year experience with the technique he had developed.51 He designated his operation as posterior gastropexy, and this operation became the only gastropexy procedure that has withstood the test of time. In Hill's initial experience, there was a high incidence of postoperative dysphagia, so Hill subsequently performed the procedure using intraoperative manometry. This unique approach allowed tailoring of the anchoring sutures to achieve a lower esophageal sphincteric pressure of 35 mm Hg or less. In the subsequent 30 years, Hill continued to study the anatomic and physiologic aspects of gastroesophageal reflux. In the mid-1990s, he described the flap valve mechanism of the cardia, an anatomic feature so important it is now incorporated into anatomic textbooks. Additionally, he proposed a grading system of the flap valve mechanism that correlated with the patient's reflux status better than the measurement of the lower esophageal sphincter pressure alone.52,53
In the 1970s, Nissen's fundoplication was rapidly adopted worldwide and became the most popular antireflux operation. The original operation underwent modifications by Nissen himself, as well as by other surgeons. Closure of the hiatus was recognized as an essential part of all antireflux procedures to avoid herniation of the fundoplication. An important modification was described by Rudolf Nissen's favorite pupil, Mario Rossetti (Fig. 5). 43 This was the creation of the fundoplication using only the anterior wall of the gastric fundus. As Hill was fond of pointing out, dysphagia was extremely common following a Nissen fundoplication. In Europe, construction of a partial wrap (less than 360 degrees) was proposed by Dor et al54 and Andre Toupet55 in an effort to minimize the postoperative symptoms plaguing patients who underwent Nissen fundoplication. When Toupet introduced this concept in the early 1960s, he was harshly criticized, and his procedure received little attention until the laparoscopic era. In the United States, Donahue et al56 and Demeester and Johnson57 also worked to improve on Nissen's operation. They were the first to truly understand the physiologic mechanism of Nissen's fundoplication and modified it by division of short gastric vessels and the creation of a loose floppy wrap. Demeester and Johnson evaluated the optimal length of the wrap and convincingly showed that a loose wrap of just 2 cm was sufficient for reflux suppression and reduced the incidence of troublesome postoperative bloating and dysphagia.58 It is this modification of the original Nissen fundoplication that is most commonly performed in the laparoscopic era.
The development of minimally invasive surgical techniques has led to a dramatic increase in the number of antireflux operations being performed. The widespread availability of physiologic testing with esophageal motility studies and 24-hour pH probe studies has greatly improved the identification of those patients likely to benefit from surgery. A description of the many significant developments in the laparoscopic era is beyond the scope of this review. Modern surgeons working in an era of animal rights, privacy protection, and public wariness of clinical trials will be hard pressed to duplicate the feats of the pioneers in hiatal hernia surgery. The lessons learned about the physiologic basis of gastroesophageal reflux and the need for long-term follow-up will need to be applied as new techniques are introduced and marketed. It will be interesting to see how the 21st-century surgeons adjust to the current environment to achieve the high standards set by their predecessors.
ACKNOWLEDGMENTS
The authors would like to thank Dr. Earl Wilkins and Dr. Clem Hiebert for their advice, invaluable support, and help in finding original source materials.
Footnotes
Correspondence: David W. Rattner, MD, Chief, Division of General and Gastrointestinal Surgery, Massachusetts General Hospital, Boston, MA 02114. E-mail: drattner@partners.org.
REFERENCES
- 1.Hochberg LA. Thoracic Surgery before the 20th Century. New York: Vantage Press; 1960. [Google Scholar]
- 2.Bettex M, Oesch I. The hiatus hernia saga: ups and downs in gastroesophageal reflux: past, present, and future perspectives. J Pediatr Surg. 1983;18:670–680. [DOI] [PubMed] [Google Scholar]
- 3.Laennec RTH. De l'Auscaltation Mediate, ou Traite du Diagnostic des Maladies des Poulmons et du Coeur, Fonde Principalement sur ce Nouveau Moyen d'Exploration. Paris: Chez J.-A. Brosson et J.-S. Chaude; 1819. [Google Scholar]
- 4.Cooper A. The Lectures of Sir Astley Cooper, Bart. F.R.S. Surgeon to the King, on the Principles and Practice of Surgery, with Additional Notes and Cases by Frederick Tyrrell. London: Thomas and George Underwood; 1824–1827.
- 5.Bowditch HI. A Treatise on Diaphragmatic Hernia. Buffalo: Jewett Thomas; 1853.
- 6.Billard CM. Traite des Maladies des Enfans Nouveaux-Nes et a la Mamelle: Fonde sur de Nouvelles Observations Cliniques et d'Anatomie Pathologique, Faites a l'Hopital des Enfans-Trouves de Paris, dans le Service de M. Baron. Paris: J.B. Bailliere; 1828. [PMC free article] [PubMed]
- 7.Rokitansky C. Quoted by Nissen R. In Fundoplication und Gastropexie Bei Refiuxkrankheit und Hiatushernie. New York: G Thieme Verlag Stuggart; 1981. [Google Scholar]
- 8.Zenker FA, von Ziemsen H. Diseases of the esophagus. In: Cyclopedia of the Practice of Medicine. Vol 8. New York: William Wood; 1878:1–214. [Google Scholar]
- 9.Mackenzie M. A Manual of Diseases of the Throat and Nose: Including the Pharynx, Larynx, Trachea, Oesophagus, Nose and Naso-Pharynx. Vol 2. London: J. & A. Churchill; 1884.
- 10.Quincke H. Esophageal ulcers from digestive juice (ulcus oesophagi ex digestione). Dtsch Arch Klin Med. 1879;24:72. [Google Scholar]
- 11.Tileston W. Peptic ulcer of the oesophagus. Am J Med Sci. 1906;132:240–265. [Google Scholar]
- 12.Sheehan JE. Ulcer of the esophagus from the standpoint of an endoscopist. Med Rec. 1920;97:319. [Google Scholar]
- 13.Vinson PP. Oesophageal stricture following the vomiting of pregnancy. Surg Gynecol Obstet. 1921;33:412. [Google Scholar]
- 14.Hamperl H. Peptische oesophagins [Peptic esophagitis]. Verh Dtsch Pathol. 1934;27:208. [Google Scholar]
- 15.Winklestein A. Peptic esophagitis: a new clinical entity. JAMA. 1935;104:906. [Google Scholar]
- 16.Cannon WB, Moser A. The movements of the food in the esophagus. Am J Physiol. 1898;1:435–444. [Google Scholar]
- 17.Schwarz GS. Historical aspects of the anatomy of the cardia with special reference to hiatus hernia. Bull N Y Acad Med. 1967;43:112–125. [PMC free article] [PubMed] [Google Scholar]
- 18.Eppinger H. Allgemeine und spezielle Pathologie des Zwerchfells. In: Frankl-Hochwart L, ed. Supplemente zu H. Nothnagel, Spezielle Pathologie und Therapie. Wien: Holder; 1911. [Google Scholar]
- 19.Hedblom CA. Diaphragmatic hernia: a study of three hundred and seventy eight cases in which operation was performed. JAMA. 1925;85:947. [Google Scholar]
- 20.Friedenwald J, Feldman M. Report of an interesting type of diaphragmatic hernia of the cardia of the stomach through the esophageal orifice. Am Med Sci. 1925;170:263. [Google Scholar]
- 21.Akerlund A, Onnell H, Key E. Hernia diaphragmatica hiatus oesophagei vom anastomischen und roentgenologischen gesichtspunkt. Acta Radiol. 1926;6:3–22. [Google Scholar]
- 22.Robins SA, Jankelson IR. Cardio-esophageal relaxation. JAMA. 1926;87:1961–1964. [Google Scholar]
- 23.Ritvo M. Hernia of the stomach through the esophageal orifice of the diaphragm. JAMA. 1930;94:15–21. [Google Scholar]
- 24.Moore AB, Kirklin BR. Progress in the roentgenological diagnosis of diaphragmatic hernia. JAMA. 1930;95:1966–1969. [Google Scholar]
- 25.Sauerbruch F, Chaoul H, Adam A. Hiatus hernia. Dis Med Wochenschr. 1932;82:1709–1712. [Google Scholar]
- 26.Soresi AL. Diaphragmatic hernia: its unsuspected frequency: diagnosis and technique for radical cure. Ann Surg. 1919;69:254–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Harrington SW. Diaphragmatic hernia. Arch Surg. 1928;16:386–415. [Google Scholar]
- 28.Harrington SW. The surgical treatment of the more common types of diaphragmatic hernia: esophageal hiatus, traumatic, pleuroperitoneal hiatus, congenital absence and foramen of Morgagni: report of 404 cases. Ann Surg. 1945;122:546–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sweet RH. Diaphragmatic hernia. In: Sweet RH, ed. Thoracic Surgery. Philadelphia: WB Saunders; 1950:316–334. [Google Scholar]
- 30.Sweet RH. Esophageal hiatus hernia of the diaphragm: anatomical characteristics, technique of repair, results of treatment in 111 consecutive cases. Ann Surg. 1952;135:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Allison PR. Reflux esophagitis, sliding hiatal hernia and anatomy of repair. Surg Gynecol Obstet. 1951;92:419–431. [PubMed] [Google Scholar]
- 32.Allison PR. Hiatus hernia (a 20 year retrospective survey). Ann Surg. 1973;178:273–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Barrett NR. Hiatus hernia. Br J Surg. 1954;42:231–243. [DOI] [PubMed] [Google Scholar]
- 34.Fyke FE, Code CF, Schiegel JF. The gastroesophageal sphincter in healthy beings. Gastroenterologia. 1956;86:135–150. [DOI] [PubMed] [Google Scholar]
- 35.Kramer P, Ingelfinger FJ, Atkinson M. The motility and pharmacology of the oesophagus in cardiospasm. Gastroenterologia. 1956;86:174–178. [DOI] [PubMed] [Google Scholar]
- 36.Habibulla KS, Collis JL. Intraluminal pressure, transmucosal potential difference and pH studies in the oesophagus of patients before and after Collis repair of a hiatal hernia. Thorax. 1973;28:342–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nissen R. Exstirpation eines ganzen Lungenflugels. Dtsch Zbl Chir. 1931;58:3003–3006. [Google Scholar]
- 38.Nissen R. Die transpleurale Resection der Kardia. Dtsch Z Chir. 1937;249:311–316. [Google Scholar]
- 39.Nissen R. Gastropexy as the lone procedure in the surgical repair of hiatus hernia. Am J Surg. 1956;92:389–392. [DOI] [PubMed] [Google Scholar]
- 40.Boerema I, Germs R. Fixation of the lesser curve of the stomach to the anterior abdominal wall after reposition of the hernia through the esophageal hiatus. Archivum Chirurgical Neerlandicum. 1955;7:351–359. [PubMed] [Google Scholar]
- 41.Nissen R. Eine einfache Operation zur Beeinflussung der Refluxeosophagitis. Schweiz Med Wochenschr. 1956;86:590–592. [PubMed] [Google Scholar]
- 42.Nissen R. Reminiscences: reflux esophagitis and hiatal hernia. Rev Surg. 1970;27:307–314. [PubMed] [Google Scholar]
- 43.Liebermann-Meffer, Stein H. Rudolf Nissen and the World Revolution of Fundoplication. St Louis, MI: Quality Medical Publishing Inc; 1999.
- 44.Hiebert CA. Surgical management of esophageal reflux and hiatal hernia. Ann Thorac Surg. 1961;52:159–160. [DOI] [PubMed] [Google Scholar]
- 45.Skinner DB, Belsey RH. Surgical management of esophageal reflux and hiatus hernia: long-term results with 1,030 patients. J Thorac Cardiovasc Surg. 1967;53:33–54. [PubMed] [Google Scholar]
- 46.Collis JL. An operation for hiatus hernia with short esophagus. J Thorac Surg. 1957;34:768–788. [PubMed] [Google Scholar]
- 47.Pearson FG, Henderson RD. Long-term follow-up of peptic strictures managed by dilatation, modified Collis gastroplasty and Belsey hiatus hernia repair. Surgery. 1976;80:396–404. [PubMed] [Google Scholar]
- 48.Orringer MB, Sloan H. An improved technique for the combined Collis-Belsey approach to dilatable esophageal strictures. J Thorac Cardiovasc Surg. 1974;68:298–302. [PubMed] [Google Scholar]
- 49.Thal AP. A unified approach to surgical problems of the esophagogastric junction. Ann Surg. 1968;168:542–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hill LD, Tobias J, Morgan EH. Newer concepts of the pathophysiology of hiatal hernia and esophagitis. Am J Surg. 1966;111:70–79. [DOI] [PubMed] [Google Scholar]
- 51.Hill LD. An effective operation for hiatal hernia: an eight-year appraisal. Ann Surg. 1967;166:681–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hill LD, Kozarek RA. The gastroesophageal flap valve. J Clin Gastroenterol. 1999;28:194–197. [DOI] [PubMed] [Google Scholar]
- 53.Hill LD, Kozarek RA, Kraemer SJ, et al. The gastroesophageal flap valve: in vitro and in vivo observations. Gastrointest Endosc. 1996;44:541–547. [DOI] [PubMed] [Google Scholar]
- 54.Dor J, Humbert P, Dor V, et al. The role of the modified Nissen procedure in the prevention of reflux following Heller's extramucosal cardiomyotomy. Mem Acad Chir. 1962;88:877–882. [Google Scholar]
- 55.Toupet A. Technique d'eosophago-gastroplastie avec phreno-gastropexie dans la cure radicales des hernies hiatales et comme complement de l'operation de Heller dans les cardiospasmes. Mem Acad Chir. 1963;89:394–399. [Google Scholar]
- 56.Donahue PE, Larson GM, Stewardson RH, et al. Floppy Nissen fundoplication. Rev Surg. 1977;34:223–224. [PubMed] [Google Scholar]
- 57.Demeester TR, Johnson LF. Evaluation of the Nissen antireflux procedure by esophageal manometry and 24 hour pH monitoring. Am J Surg. 1975;129:94–100. [DOI] [PubMed] [Google Scholar]
- 58.DeMeester TR, Bonavina L, Albertucci M. Nissen fundoplication for gastroesophageal reflux disease: evaluation of primary repair in 100 consecutive patients. Ann Surg. 1986;204:9–20. [DOI] [PMC free article] [PubMed] [Google Scholar]


