Abstract
Background:
Laparoscopic colonic surgery has been claimed to hasten recovery and reduce hospital stay compared with open operation. Recently, enforced multimodal rehabilitation (fast-track surgery) has improved recovery and reduced hospital stay in both laparoscopic and open colonic surgery. Since no comparative data between laparoscopic and open colonic resection with multimodal rehabilitation are available, the value of laparoscopy per se is unknown.
Methods:
In a randomized, observer-and-patient, blinded trial, 60 patients (median age 75 years) underwent elective laparoscopic or open colonic resection with fast-track rehabilitation and planned discharge after 48 hours. Functional recovery was assessed in detail during the first postoperative month.
Results:
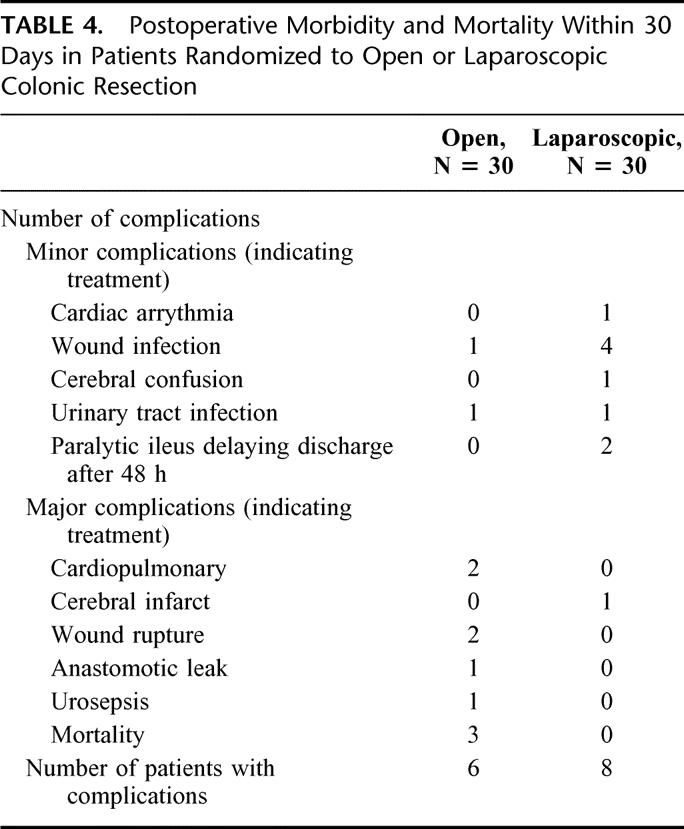
Median postoperative hospital stay was 2 days in both groups, with early and similar recovery to normal activities as assessed by hours of mobilization per day, computerized monitoring of motor activity assessed, pulmonary function, cardiovascular response to treadmill exercise, pain, sleep quality, fatigue, and return to normal gastrointestinal function. There were no significant differences in postoperative morbidity, mortality, or readmissions, although 3 patients died in the open versus nil in the laparoscopic group.
Conclusion:
Functional recovery after colonic resection is rapid with a multimodal rehabilitation regimen and without differences between open and laparoscopic operation. Further large-scale studies are required on potential differences in serious morbidity and mortality.
In a randomized, observer-and-patient, blinded trial in 60 patients undergoing fast-track elective laparoscopic or open colonic resection, recovery of gastrointestinal and cardiopulmonary function, ambulation, exercise capacity, pain, sleep, fatigue, and return to usual activities were similar. Mean hospital stay was 2.9 and 2.3 days, respectively.
Open colonic resection is usually associated with a hospital stay of about 6 to 11 days and a complication rate of 15% to 20%.1–6 Introduction of laparoscopic-assisted colonic resection has reduced the hospital stay to about 4 to 8 days, with the same or a slightly lower morbidity rate in randomized trials.1–6 Concomitant with these technical developments, an increased body of evidence has been developed to demonstrate that perioperative care regimens, including optimized pain relief, early oral feeding, and mobilization, have profound effects to improve postoperative recovery and outcome.7,8 These so-called multimodal rehabilitation programs or fast-track surgery7,8 have been applied after laparoscopic9,10 and open11 colonic resection, resulting in reduced hospital stay to about 2 to 3 days. Unfortunately, assessment of laparoscopic versus open colonic resection on early postoperative outcome in randomized studies1–6 has not included a revision of postoperative care principles adjusted to recent scientific data,7,8 and therefore the difference between laparoscopic and open colonic resection on early postoperative recovery remains to be determined. Such studies require an optimized regimen and observer-blinded regimen to minimize treatment bias due to expected benefits of minimal invasive surgery or other new surgical techniques.12
The aim of this study was therefore to assess the functional recovery after laparoscopic-assisted versus open colonic resection, where both groups received a multimodal rehabilitation program in a randomized observer and patient-blinded design, and with planned discharge after 48 hours.
PATIENTS AND METHODS
Patients
From February 1999 to September 2001, all patients over 55 years scheduled for elective right hemicolectomy or sigmoid resection were randomized to either open or laparoscopic operation. A well-defined multimodal rehabilitation program was followed in all patients, as described in detail previously,9,11 and includes continuous epidural analgesia for 48 hours, early oral feeding including protein drinks, active mobilization, and planned discharge on the second postoperative day.
Exclusion criteria were patients not able to take care of themselves at home or living in a nursing home and patients operated during summer and other holiday periods when the research team was not present. Patients were excluded after randomization if an epidural catheter could not be inserted, if an anastomosis was performed below 12 cm from the anus, or if a different operation than the scheduled was performed (stoma or no resection). Performance of additional resections, for instance, of small bowel or uterus, did not result in exclusion.
All patients were informed both orally and in writing about the 2 different surgical techniques, about the postoperative multimodal rehabilitation program including the scheduled pre- and postoperative assessments, and the expected discharge 2 days after operation.
The study was blinded both to the patient, the ward nurses, and the observer from the research team. An opaque dressing covering the whole abdomen was applied after surgery and was not removed until decision about discharge had been taken. Only the anesthetist, theater nurses, and the performing surgeons knew the type of surgical technique and the content of the epidural infusion. Ward rounds were performed by other surgeons, and if the dressing needed changing before discharge, a theater nurse was called (n = 2).
The patient's file contained a report of the performed operation and anesthesia, avoiding the precise description of the technique. A sealed envelope in the file contained the detailed complete information about the surgical procedure and the epidural infusion and could be opened, if necessary (not done).
The local ethical committee approved the study, and written patient acceptance was obtained.
Anesthesia and Postoperative Analgesia
All patients received a thoracic epidural catheter at T6-T7 for right hemicolectomy and at T9-T10 for sigmoid resection. Intraoperatively, all patients received 12 mL 0.5% bupivacaine followed by 4 mL per hour. In addition, the patients undergoing open operation received an epidural dose of morphine (2 mg ≤70 years and 1 mg >70 years). The epidural analgesia continued during surgery and for 48 hours with 0.25% bupivacaine and morphine 0.05 mg/mL, 4 mL hour, except in laparoscopic patients, who received only bupivacaine. General anesthesia was standardized in all patients with propofol and remifentanil as described before.11 Thirty minutes before termination of anesthesia, ketorolac 30 mg and ondansetron 4 to 8 mg were administered i.v., and at the end of surgery 20 mL 0.25% bupivacaine was injected in the incisions (subcutaneously and subfascially). Intraoperative fluid administration was standardized to 1500 mL isotonic saline and 500 mL hydroxyethyl starch (HAES), unless bleeding indicated otherwise. Normothermia was maintained with forced air warming (Bair-Hugger, Augustine Medical, Eden Prairie, MN).
Postoperatively, oral paracetamol 2 g was given every 12 hours. Rescue analgesia included oral ibuprofen 600 mg every 8 hours, additional epidural 0.125% bupivacaine 6 mL or, as a last choice, oral morphine 10 mg.
Surgical Procedures
Preoperative mechanical bowel preparation was performed with Phosphoral. A single preoperative dose of antibiotics (cefuroxime 3.0 g and metronidazole 1.5 g) was given. In the open group, right-sided hemicolectomy was performed through a right horizontal incision above the umbilicus and sigmoid resection through a curved incision in the left iliac fossa, extended toward the curvature if necessary,11 and laparoscopic resection as described before.9
Care Protocol and Investigations
Postoperative nasogastric tubes were not used. Cisapride 20 mg was given twice a day to the first 37 patients but omitted thereafter. Oral magnesia 1 g twice a day was given for a week, unless diarrhea occurred. Oral intake and mobilization followed a standardized care program,11 aiming at normal oral intake of fluid and solid food and mobilization (>8 hours) from 24 hours postoperatively. Discharge was planned to about 48 hours postoperatively, provided that oral intake was sufficient, that defecation had occurred, that pain could be managed by oral analgesics, and that the patients felt they could take care of themselves. At the time of discharge but before removal of the wound dressing, the ward nurses and patients assessed whether they thought the operation was performed open or laparoscopically. The patients were seen in the outpatient clinic on day 8 for removal of sutures and again on day 30 for a final assessment of convalescence and patient and relatives’ satisfaction.
A number of functional parameters were measured at predetermined intervals in the perioperative period. Pain at rest and during activity was scored every 4 hours (except during night) for the first 2 postoperative days. An overall pain score for one day at a time was assessed from postoperative days 3 to 7 and thereafter weekly for a total of 4 weeks on a scale from 0 to 3 (0 = no pain, 1 = slight pain, 2 = moderate pain, 3 = severe pain). Fatigue was scored on a similar scale. Pulmonary function—forced expired volume in first second (FEV1), forced vital capacity (FVC) and peak expiratory flow (PEF)—was measured with the patient in a sitting position.13 Oxygen saturation and heart rate were measured continuously during 1 night before surgery and the first 2 nights after surgery (11:00 pm to 7:00 am) by a pulse oxymeter (Nellcor N-3000, Nellcor Puritan Bennett Inc, Pleasanton, CA). Cardiovascular response to exercise was assessed on an electronic treadmill (Tunturi J 502 Piispanristi, Finland).13 Mental function was assessed by Hodkinson modification of the original Roth-Hopkins test.13 Quality of sleep was scored by the patient on a VAS-scale (0 = the best sleep and 10 = worst sleep/nightmare) 3 nights before and 7 nights after surgery. Mobilization was assessed as hours out of bed per day, recorded by the nurses and the patient during the first postoperative week.
Physical motor activity was monitored continuously by a hand wrist-worn Mini-Motion Logger Actigraph14 for 2 days preoperatively and 6 days postoperatively. The Mini-Logger was not used during showers, which was recorded in a log. Nausea and vomiting were recorded, as well as time to first defecation. Serum albumin and plasma CRP were analyzed preoperatively and on the second and eighth postoperative day. Convalescence and satisfaction were assessed by the patients and their closest relatives at day 30. All patients were encouraged to return to usual activities immediately after discharge.
Statistics
From a previous study,11 it was assessed that to show a mean difference in hospital stay of 1 day in the laparoscopic group with the same discharge criteria required 23 patients (2α = 0.05, β = 0.20). We therefore aimed at 60 evaluable patients with 30 in each group, allowing for predefined exclusion criteria after randomization. Data are presented as median and range. All data including patients converted from laparoscopic to open surgery were analyzed on intention-to-treat basis. Data for the 27 patients with a completed laparoscopic procedure were analyzed as well. Comparisons were done with Mann-Whitney for continuous data and χ2 test for categoric data between groups. Wilcoxon test was used to compare data within groups. Friedman 2-way analysis of variance was used to analyze change for repeated data within groups. P < 0.05 was considered statistically significant.
RESULTS
Patients
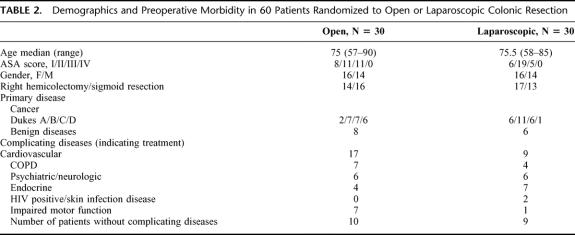
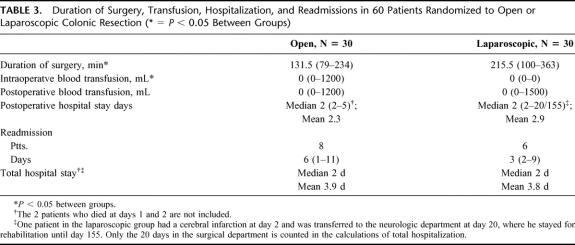
Seventy-five patients were eligible for the study. Fourteen patients were excluded after randomization (Table 1), leaving 30 patients in each group to be evaluated. Demographic data, ASA score, concomitant diseases, and preoperative morbidity were similar (P > 0.05) in the 2 groups (Table 2). Duration of surgery was significantly longer in the laparoscopic group: median 215 minutes versus 131 minutes (Table 3). Intraoperative blood transfusion was given more frequently in the open group (Table 3). Three patients in the laparoscopic group were converted to open surgery, 1 due to adhesions after earlier operation, 1 due to cancer growth into the duodenum, and 1 because hysterectomy had to be performed as well. Results from these patients were included in the laparoscopic group (intention to treat).
TABLE 1. Recruitment, Randomization, and Exclusions for the Study
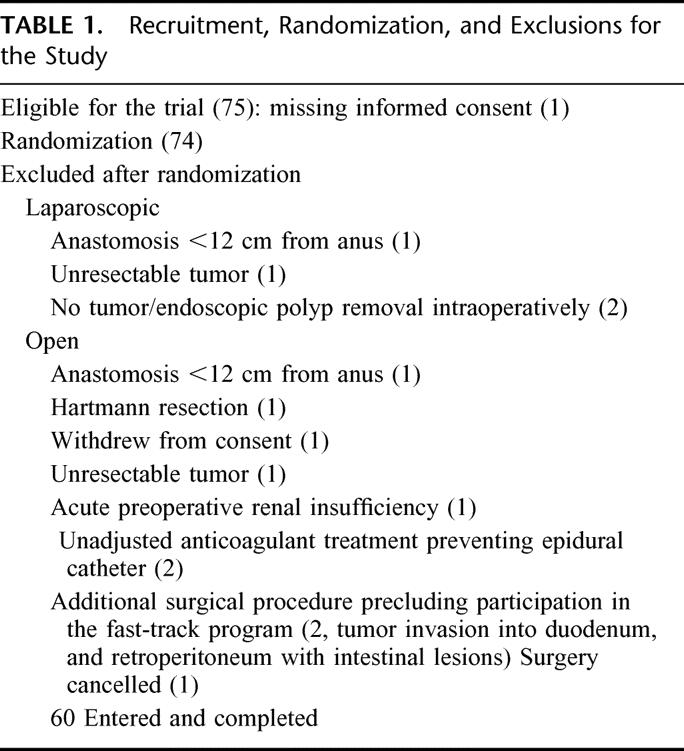
TABLE 2. Demographics and Preoperative Morbidity in 60 Patients Randomized to Open or Laparoscopic Colonic Resection
TABLE 3. Duration of Surgery, Transfusion, Hospitalization, and Readmissions in 60 Patients Randomized to Open or Laparoscopic Colonic Resection (* = P < 0.05 Between Groups)
Hospital Stay
Patients stayed median 2 days after surgery in both groups (range 2–5 days in the open group and 2–20 days in laparoscopic group; P > 0.05; Fig. 1). Eight patients in the open group and 6 patients in the laparoscopic group were readmitted after discharge. The reasons for readmission were wound infection (1), nausea and vomiting (1), bradycardia (1), gallbladder pain (1), and urinary tract infection (1) in the laparoscopic group and observation for wound infection (not found) (1), wound rupture (1), atrial fibrillation as before surgery, no further treatment (1), spinal headache (1), urosepsis (1), anastomotic leak (1), and social reasons (2), of which 1 was due to the husband's death, in the open group. Total hospital stay (primary plus readmission) was not different between groups (P > 0.05; Table 3).
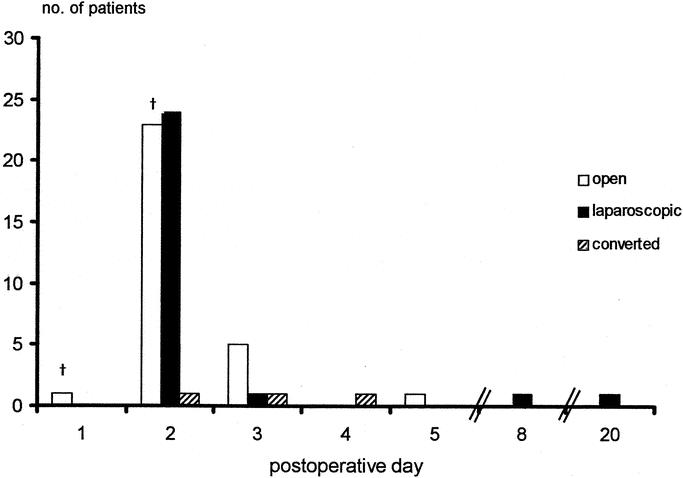
FIGURE 1. Primary hospital stay after open and laparoscopic colonic resection (P > 0.05 between groups). † indicates mortality.
Morbidity and Mortality
Postoperative complications were seen in 6 patients in the open group and 8 patients in the laparoscopic group (Table 4). Three patients died in the open group, 2 of cardiopulmonary causes on days 1 and 2, and 1 was reoperated for anastomotic leakage on day 8 and died at day 19 after a third operation for wound rupture on day 12.
TABLE 4. Postoperative Morbidity and Mortality Within 30 Days in Patients Randomized to Open or Laparoscopic Colonic Resection
Pain, Fatigue and Sleep Quality
At the day of operation and on day 1, patients in the laparoscopic group had a slightly higher (P < 0.05) pain score both at rest and during activity compared with the open group (data not shown). From days 2 to 30, there was no difference in pain score between groups (P > 0.05). The fatigue scores were similar in the 2 groups for the entire 4-week period at all assessments (Fig. 2). Sleep quality deteriorated slightly during the first postoperative night (P < 0.05) in the laparoscopic group. From the second night, there were no differences between groups (P > 0.05; Fig. 2).
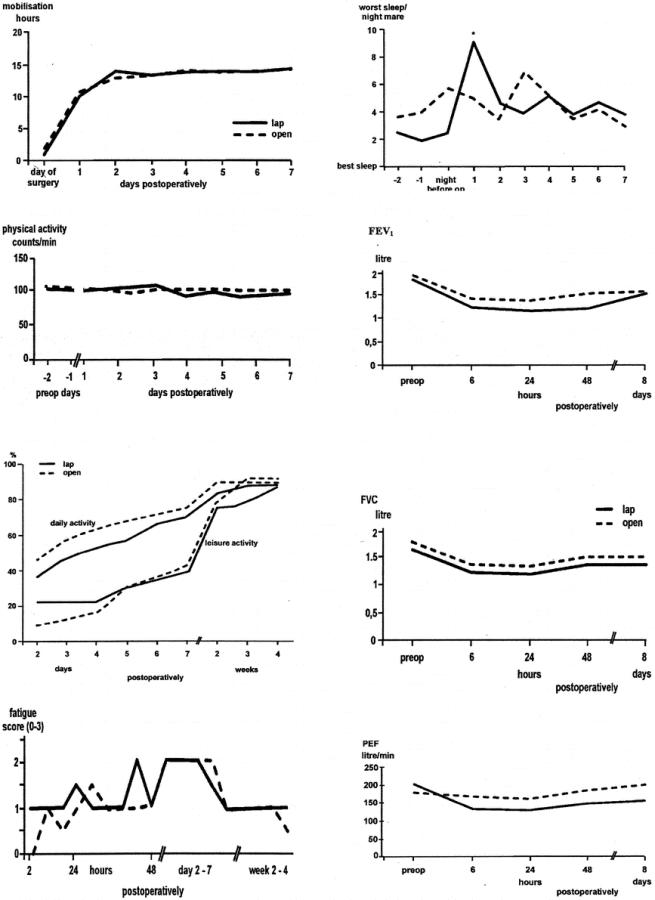
FIGURE 2. Mobilization, physical activity (Actigraph), fatigue and sleep quality, and daily and leisure activity after open or laparoscopic colonic resection (P > 0.05 between groups at all intervals, except for sleep quality; * = P < 0.05). Changes in pulmonary function (FEV1, FVC, and PEF) showed a statistical decrease in both groups (Friedman test). Wilcoxon test shows that FEV1 was back to preoperative values 48 hours postoperatively in the open group and FVC and PEF on day 8. In the laparoscopic group, FEV1 returned to be preoperative values 8 days postoperatively, but not FVC and PEF.
Motor Function
Patients were out of bed for median 10 hours on the first postoperative day in both groups, increasing to 14 hours from day 2 and thereafter, with no differences between the groups (P > 0.05; Fig. 2). Measurements of physical motor activity by the Actigraph confirmed a high degree of mobilization, and without differences between groups (P > 0.05; Fig. 2)
Gastrointestinal Function
There was no difference between the 2 groups in nausea or vomiting (data not shown). Median time to first defecation was 2 days in both groups (P > 0.05).
Cardiopulmonary Function
Pulmonary function (FEV1, FVC, and PEF) decreased significantly in the open group during the first postoperative week (P < 0.05), except for FEV1, which returned to preoperative values (P > 0.05) after 24 hours (Fig. 2). The 2 patients who died on days 1 and 2 are excluded from these calculations. Continuous measurements of oxygen saturation were successfully completed both pre- and postoperatively in 24 patients in the open group (excluding the 2 patients who died at days 1 and 2 and 4 patients due to technical error and in 30 patients in the laparoscopic group. Compared with preoperative values, there were no changes in mean saturation, time spent with saturation <90%, or number of episodes with hypoxemia in any of the groups (P > 0.05) Mean heart rate increased slightly (P < 0.05) on the first and second postoperative nights in both groups (data not shown). All patients completed the preoperative exercise test, and 24 patients in each group completed the postoperative treadmill exercise. In the open group, 5 patients preoperatively and 7 patients at day 8 were exhausted before reaching a heart rate of 120, corresponding figures being 8 and 5 in the laparoscopic group (P > 0.05). In the laparoscopic group, the amount of work performed until a heart rate of 120 or exhaustion decreased from 14.0 W preoperatively to 12.2 W on day 8 (P < 0.05) compared with no change from 18.1 W to 19.9 W, respectively, in the open group (P > 0.05). There was no difference (P > 0.05) between preoperative exercise performed between groups.
Mental Function
Median score in the open group (n = 27; 2 patients died and 1 would not participate on day 8) increased from 93% preoperatively to 100% on the first, second, and eighth postoperative day (P < 0.05). In the laparoscopic group (n = 29; the patient who had a cerebral infarct could not participate on day 8) no change was found from 100% preoperatively to 97% on postoperative day 1 and 97% on days 2 and 8 (P > 0.05).
P-CRP and S-Albumin
Changes in plasma CRP and serum albumin were similar in the 2 groups. In the open group, CRP increased from 9.5 mg/L preoperatively to 180.0 mg/L on the second postoperative day (P < 0.05) and returned to baseline on day 8 (15.0 mg/L, P > 0.05) and S-albumin decreased from 36.9 g/L preoperatively to 29.3 g/L on the second postoperative day (P < 0.05) and returned to baseline on the eighth postoperative day (35.6 g/L, P > 0.05). In the laparoscopic group, P-CRP increased from 10.0 mg/L preoperatively to 132.5 mg/L (P < 0.05) on day 2 and to 22.0 mg/L on day 8 (P < 0.05), while S-albumin decreased from 39.6 g/L preoperatively to 29.3 g/L on day 2 (P < 0.05) and 35.3 g/L on day 8 (P < 0.05).
Convalescence and Patient/Relatives’ Satisfaction
Return to normal daily activities is shown in Figure 2 and demonstrates an early recovery with a similar time course between open and laparoscopic patients (P > 0.05). Thirty percent of the patients and 41% of the relatives in the open group found the hospital stay to be too short, compared with 17% and 21%, respectively, in the laparoscopic group (P > 0.05). Four of the patients in the open group (pain, cancer diagnosis, feeling unwell, and suture removal) and 8 in the laparoscopic group (wound hematoma/infection, 3; urinary problems, 2; cancer diagnosis, pain, 2) had seen their general practitioner within 4 weeks.
At discharge, but before removing the wound dressing, the nurses correctly identified the type of surgery in 68% of patients in the open group compared with 79% in the laparoscopic group. The patients correctly identified the type of surgery in 62% of open operations and 59% of laparoscopic operations. Intention-to-treat results, including all patients randomized to the laparoscopic group, did not differ from the results compared with patients completing the laparoscopic procedure (P > 0.05).
DISCUSSION
Recent efforts to improve postoperative recovery and reduce hospital stay and morbidity include technical aspects such as minimal invasive (laparoscopic) surgery, anesthesiologic aspects (short-acting anesthetics and regional anesthesia), and optimized postoperative pain relief with continuous epidural analgesia in major procedures, together with adjustment of general postoperative care principles with avoidance of nasogastric tubes, drains, and with early institution of oral feeding and mobilization.7,8 This combined approach within the context of “fast-track” surgery has resulted in an improved surgical outcome in several procedures.7,8 Concomitantly with these developments, several randomized studies have been performed to compare single-modality intervention with laparoscopic-assisted colonic resection versus open surgery with conventional care but without documentation of definite advantages, except for a slightly shorter hospital stay, less pain and bleeding, and improved pulmonary function and oxygenation.1–6,15,16 Interestingly, the multimodal rehabilitation approach has in uncontrolled studies been demonstrated to lead to similar or better outcomes, with earlier recovery of organ functions in open procedures,11,13,17–19 compared with results from studies with single-intervention with laparoscopic surgery.1–6 However, in a recent nonrandomized comparative study, cost and hospital stay (3 versus 6 days) were lower with laparoscopic operation,20 but interpretation is hindered by lack of information on perioperative care regimens and limitations for early recovery.
To assess the potential benefit of minimal invasive (laparoscopic) surgery with expected less postoperative organ dysfunction,15 a better design of outcome studies is required12 where patients and the ward personnel are blinded to the type of surgical procedure and care is adjusted to the principles of fast-track surgery.21 The combination of “fast-track” care principles together with appropriate blinding is essential since outcomes otherwise merely may reflect traditions of care. This was clearly illustrated by a properly blinded randomized study in laparoscopic versus open cholecystectomy study,22 where hospital stay and convalescence were determined by traditions of care and not by the surgical technique investigated.21,22
The present study is the first randomized, blinded study to combine appropriate blinding with “fast-track” care in laparoscopic surgery, and it shows that functional recovery of a large variety of organ functions is fast but similar between laparoscopic and open procedures. These findings emphasize that postoperative outcome may merely depend on principles of postoperative care rather than single-modality intervention with minimal invasive surgery, at least in colonic resection where the patients with laparoscopic resection also receive an abdominal incision, although smaller than with open surgery. However, since minimal invasive surgery has definite advantages on various undesirable postoperative stress responses and organ dysfunctions,15 further studies are needed with laparoscopic colonic resection combined with an even more optimized “fast-track” care regimen than applied in our study.
One of the important results of this and earlier studies with fast-track colonic surgery9,11 is the very early normalization of gastrointestinal function within 2 days compared with usually 4 days.1–6 The instituted multimodal regimen leads to early normalization of the entire gastrointestinal motor function in the entire gastrointestinal tract, confirmed by Indium scintigraphy compared with nonoperated volunteers19 or between open and laparoscopic colonic resection.23 The early normalization of gastrointestinal function therefore allows early oral nutrition, which otherwise has been demonstrated to improve postoperative outcome.24 In addition, fast-track colonic resection leads to only minor reduction of pulmonary function and oxygen saturation in open procedures,13 and without differences between laparoscopic and open fast-track colonic surgery as demonstrated in the present study. The improved pulmonary function may be an important factor leading to the demonstrated smaller risk of pulmonary complications with fast-track versus conventional open colonic resection.17
The present study has focused on recovery of a variety of organ functions comparing open versus laparoscopic colonic surgery, but due to its relatively small size (n = 60), our study will not allow conclusions on other clinical outcomes such as cardiopulmonary, thromboembolic, wound or cerebral complications. Thus, the higher mortality (3 versus nil) in the open group may be related to the higher ASA scores in the open group. Therefore, further large-scale studies with fast-track laparoscopic versus open colonic resection are required to elucidate potential advantages of laparoscopic resection in high-risk patients to decrease serious morbidity and mortality. From our previous prospective, nonrandomized studies, no differences in mortality were observed between open groups17 (n = 130, mortality 4.8%) and laparoscopic groups9 (n = 50, mortality 4%). In these series and the present study, median age was between 75 and 80 years, which is about 10 to 20 years older than other series1,10,20,25,26
It has been assumed that laparoscopic colonic surgery was cost effective due to reduced hospital stay and nursing care despite higher operative costs,4,20,27 but in these studies optimized fast-track care principles were not applied in the open group, and cost issues between laparoscopic and open colonic surgery therefore require further assessment.
Insignificantly more patients and relatives found that discharge occurred too early in the open group (30 versus 17% and 41 versus 21%, respectively), calling for further studies on satisfaction with the 2 surgical methods.
In conclusion, based on the current results and other literature concerning fast-track laparoscopic or open colonic resection9–11,17,25–28 there may not be important differences in functional recovery between the 2 surgical techniques. However, the laparoscopic approach and its advantageous physiologic effects15 may result in reduced morbidity in high-risk patients,9,29 which should be explored in future studies.
Footnotes
The study was supported by Apotekerfonden 1991 and Danish Research Council (22-01-0160).
Reprints not available.
Correspondence: Henrik Kehlet, Section for Surgical Pathophysiology, The Juliane Marie Centre, 4074, Rigshospitalet, Copenhagen, DK-2100 Copenhagen, Denmark. E-mail: henrik.kehlet@rh.dk.
REFERENCES
- 1.Chapman AE, Levitt MD, Hewett P, et al. Laparoscopic-assisted resection of colorectal malignancies: a systematic review. Ann Surg. 2001;234:590–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Braga M, Gignali A, Gianotti L, et al. Laparoscopic versus open colorectal surgery: a randomized trial on short-term outcome. Ann Surg. 2002;236:759–767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lacy AM, Garcia-Valdecasas JC, Delgado S, et al. Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet. 2002;359:2224–2229. [DOI] [PubMed] [Google Scholar]
- 4.Jansson M, Bjöholt I, Carlsson CP, et al. Randomised clinical trial of the costs of open and laparoscopic surgery for colonic cancer. Br J Surg. 2004;91:409–417. [DOI] [PubMed] [Google Scholar]
- 5.Leung KL, Kwork SPY, Lam SCW, et al. Laparoscopic resection of rectosigmoid carcinoma: prospective randomised trial. Lancet. 2004;363:1187–1197. [DOI] [PubMed] [Google Scholar]
- 6.The Clinical Outcomes of Surgical Therapy Study Group. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med. 2004;350:2052–2059. [DOI] [PubMed] [Google Scholar]
- 7.Kehlet H, Dahl JB. Anaesthesia, surgery and challenges in postoperative recovery. Lancet. 2003;362:1921–1928. [DOI] [PubMed] [Google Scholar]
- 8.Kehlet H, Wilmore W. Multimodal strategies to improve surgical outcome. Am J Surg. 2002;183:630–641. [DOI] [PubMed] [Google Scholar]
- 9.Bardram L, Funch-Jensen P, Kehlet H. Rapid rehabilitation in elderly patients after laparoscopic colonic resection. Br J Surg. 2000;87:1540–1545. [DOI] [PubMed] [Google Scholar]
- 10.Senagore AJ, Duepree HJ, Delaney CP, et al. Results of a standardized technique and postoperative care plan for laparoscopic sigmoid colectomy: a 30-month experience. Dis Colon Rectum. 2003;46:503–509. [DOI] [PubMed] [Google Scholar]
- 11.Basse L, Jakobsen DH, Billesbølle P, et al. A clinical pathway to accelerate recovery after colonic resection. Ann Surg. 2000;232:51–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Horton R. Surgical research or comic opera: questions but few answers. Lancet. 1996;347:984. [DOI] [PubMed] [Google Scholar]
- 13.Basse L, Raskov HH, Jakobsen DH, et al. Accelerated postoperative recovery programme after colonic resection improves physical performance, pulmonary function and body composition. Br J Surg. 2002;89:446–453. [DOI] [PubMed] [Google Scholar]
- 14.Bisgaard T, Kjaersgaard M, Bernhard A, et al. Computerized monitoring of physical activity and sleep in postoperative abdominal surgery patients. J Clin Monit Comput. 1999;15:1–8. [DOI] [PubMed] [Google Scholar]
- 15.Kehlet H. Surgical stress response: does endoscopic surgery confer an advantage? World J Surg. 1999;23:801–807. [DOI] [PubMed] [Google Scholar]
- 16.Schwenck W, Böhm B, Witt C, et al. Pulmonary function following laparoscopic or conventional colorectal resection. Arch Surg. 1999;134:6–12. [DOI] [PubMed] [Google Scholar]
- 17.Basse L, Thorbøl JE, Løssl K, et al. Colonic surgery with accelerated rehabilitation or conventional care. Dis Colon Rectum. 2004;47:271–278. [DOI] [PubMed] [Google Scholar]
- 18.Henriksen MG, Jensen MB, Hansen HV, et al. Enforced mobilisation, early oral feeding and balanced analgesia improve convalescence after colorectal surgery. Nutrition. 2002;18:147–152. [DOI] [PubMed] [Google Scholar]
- 19.Basse L, Madsen JL, Kehlet H. Normal gastrointestinal transit after colonicresection using epidural analgesia, enforced oral nutrition and laxative. Br J Surg. 2001;88:1498–1500. [DOI] [PubMed] [Google Scholar]
- 20.Delaney CP, Kiran RP, Senagore AJ, et al. Case-matched comparison of clinical and financial outcome after laparoscopic or open colorectal surgery. Ann Surg. 2003;238:67–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kehlet H. Clinical trials in laparoscopic surgery: the second round will require a change in tactics. Surg Laparosc Endosc Percut Tech. 2002;12:137–138. [DOI] [PubMed] [Google Scholar]
- 22.Majeed AW, Troy G, Nicholl JP, et al. Randomized, prospective, single-blind comparison of laparoscopic versus small-incision cholecystectomy. Lancet. 1996;347:989–994. [DOI] [PubMed] [Google Scholar]
- 23.Basse L, Madsen JL, Billesbølle P, et al. Gastrointestinal transit after laparoscopic vs open colonic resection. Surg Endosc. 2003;17:1919–1922. [DOI] [PubMed] [Google Scholar]
- 24.Lewis SJ, Egger M, Sylvester PA, et al. Early enteral feeding versus “nil by mouth” after gastrointestinal surgery: systematic review and meta-analysis of controlled trials. BMJ. 2001;323:773–777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stephen AE, Berger DL. Shortened length of stay and hospital cost reduction with implementation of an accelerated clinical care pathway after elective colon resection. Surgery. 2003;133:277–282. [DOI] [PubMed] [Google Scholar]
- 26.Delaney CP, Zutshi M, Senagore AJ, et al. Prospective, randomized, controlled trial between a pathway of controlled rehabilitation with early ambulation and diet and traditional postoperative after laparotomy and intestinal resection. Dis Colon Rectum. 2003;46:851–859. [DOI] [PubMed] [Google Scholar]
- 27.Senagore AJ, Duepree HJ, Delaney CP, et al. Cost structure of laparoscopic and open sigmoid colectomy for diverticular disease: similarities and differences. Dis Colon Rectum. 2002;45:485–490. [DOI] [PubMed] [Google Scholar]
- 28.Anderson ADG, McNaught CE, MacFie J, et al. Randomised clinical trial of multimodal optimization and standard perioperative surgical care. Br J Surg. 2003;90:1497–1504. [DOI] [PubMed] [Google Scholar]
- 29.Senagore AJ, Madbouly KM, Fazio WV, et al. Advantages of laparoscopic colectomy in older patients. Arch Surg. 2003;138:252–256. [DOI] [PubMed] [Google Scholar]