Abstract
Objective:
To establish a telerobotic surgical service between a teaching hospital and a rural hospital for provision of telerobotic surgery and assistance to aid rural surgeons in providing a variety of advanced laparoscopic surgery to their community patients.
Summary Background Data:
The above service was established between St. Joseph's Hospital in Hamilton and North Bay General Hospital 400 km north of Hamilton on February 28, 2003. The service uses an IP-VPN (15 Mbps of bandwidth) commercially available network to connect the robotic console in Hamilton with 3 arms of the Zeus-TS surgical system in North Bay.
Results:
To date, 21 telerobotic laparoscopic surgeries have taken place between North Bay and Hamilton, including 13 fundoplications, 3 sigmoid resections, 2 right hemicolectomies, 1 anterior resection, and 2 inguinal hernia repairs. The 2 surgeons were able to operate together using the same surgical footprint and interchange roles seamlessly when desired. There have been no serious intraoperative complications and no cases have had to be converted to open surgeries. The mean hospital stays were equivalent to mean laparoscopic LOS in the tertiary institution.
Conclusions:
Telerobotic remote surgery is now in routine use, providing high-quality laparoscopic surgical services to patients in a rural community and providing a superior degree of collaboration between surgeons in teaching hospitals and rural hospitals. Further refinement of the robotic and telecommunication technology should ensure its wider application in the near future.
We report the establishment of the world's first clinical telerobotic remote surgical service between a teaching hospital in Hamilton, Ontario and a rural community hospital in North Bay, Ontario, how the service was established, and a brief report of our experience with the first 21 telerobotic remote advanced laparoscopic procedures performed.
The first telerobotic surgery was a laparoscopic cholecystectomy performed on a patient in Strasbourg, France by a surgeon from New York City on September 7, 2001.1 Although the “Lindbergh operation” was successful, many questioned the feasibility of routine use of this technology. Questions were raised about the application of telerobotic remote surgery for advanced laparoscopic procedures, its use in rural and remote corners of the world where a dedicated ATM (asynchronous transfer mode) band (as used during the “Lindbergh operation”) is not available, and the ease by which the robotic arms can be assembled by those not expert in robotics present at the bedside of a remote patient.
We report the establishment of the world's first telerobotic surgical service between a teaching hospital and a community hospital more than 400 km away for the purpose of providing advanced laparoscopic surgical care more effectively to patients in this rural community.
METHODS
Telesurgical Robotic System
A Zeus TS microjoint system (Computer Motion Inc, Santa Barbara, CA) is used to provide telepresence for the telerobotic surgeon in Hamilton Ontario, experienced in advanced laparoscopic procedures (Fig. 1a). The 3 arms of the robot in North Bay, Ontario are set up during each case by the local laparoscopic surgeon (Fig. 1b) with training in laparoscopic surgery through short training courses and 5 mentoring and telementoring sessions. A digital camera (Stryker 988, Stryker Canada, Waterdown, Ontario) is used to provide the laparoscopic view for both surgeons.
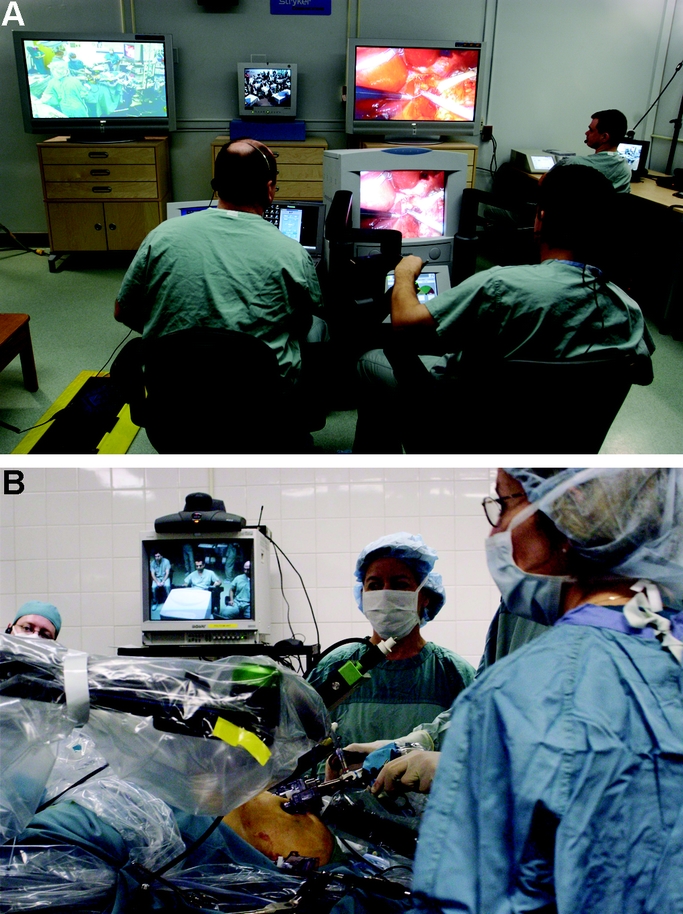
FIGURE 1. (a) Telerobotic Room at St. Joseph's Hospital in Hamilton. (b) Setup of the Zeus TS Robotic Arms in the operating room of North Bay General Hospital.
Telecommunication Link
A commercially available IP/VPN (Internet Protocol-Virtual Private Network) network with QOS (Quality of Service) is used to link the 2 hospitals at a bandwidth of 15 Mbps (Fig. 2). This system runs the local Internet as well as secure communication between banks, government offices, and other similar institutions. This service includes an active line and a fully redundant (active backup) line enabling the telerobotic surgeon to use the second line immediately if there is failure of the first line. The telerobotic surgeries are performed at the highest priority QOS, which is a function of the network, thus ensuring signal transmission at the most rapid rate possible between the 2 sites. The surgical signals take priority over any other traffic on the network at the time.
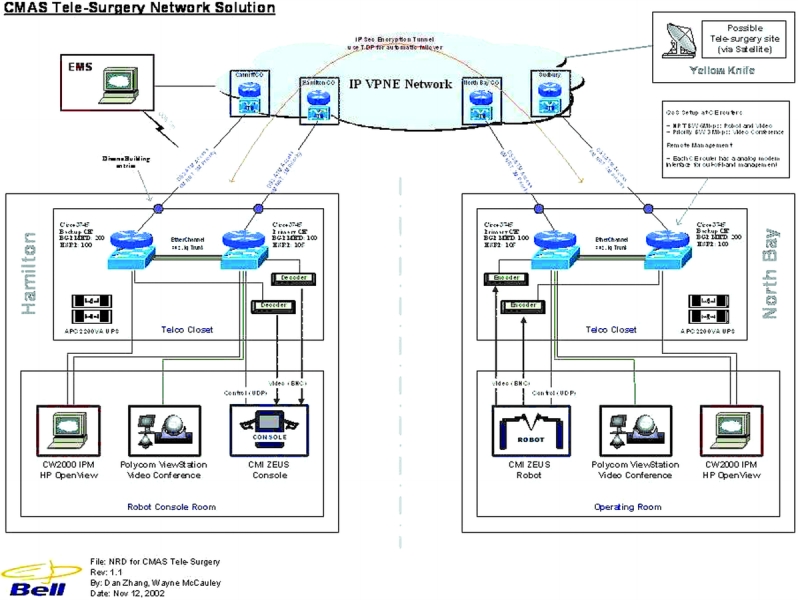
FIGURE 2. The IP/VPN network used to provide the telecommunication connection between the St. Joseph's telerobotic room and North Bay General Hospital.
Support Staff
The local laparoscopic surgeon as well as the nursing team in North Bay were trained with the use of the robotic arms and instrumentation prior to the start of the service. An experienced technician was also present during each case to ensure smooth setup of the robotic arms.
Telerobotic Room in Hamilton
The telerobotic room is equipped with 2 large-screen televisions bringing images of the operating room in North Bay as well as the laparoscopic scope view (Fig. 1a). The sound from the North Bay operating room as well as the voices of the laparoscopic surgeon and staff are heard over speakers. The environment is created such as to allow the telerobotic surgeon to be immersed in the atmosphere of the North Bay operating room. The 2 surgeons are also in constant communication using wireless headsets.
Ethical and Medicolegal Issues
The service was put into place only after obtaining full ethical approval by the Ethics Boards of both hospitals (St. Joseph's Healthcare Hamilton and North Bay General Hospital). A special consent form and patient information sheet were developed with the assistance of the Ethics Boards. Both surgeons are medically insured by the Canadian Medical Protection Association and have privileges at the local hospital to perform advanced laparoscopic procedures. A legal agreement between the 2 surgeons and 5 partners (St. Joseph's Healthcare Hamilton, North Bay General Hospital, Bell Canada, Stryker Canada, and Computer Motion Inc.) was signed prior to the establishment of the service delineating the scope of each party's responsibility during telerobotic surgery cases.
RESULTS
The service commenced on February 28, 2003. For the inaugural day, 2 telerobotic laparoscopic Nissen fundoplications (TR-LNF) were performed. Six days later a telerobotic laparoscopic right hemicolectomy (TR-LRH) was performed. To date, 21 telerobotic surgeries have been performed, including: 13 laparoscopic Nissen fundoplications, 2 laparoscopic right hemicolectomies, 1 laparoscopic anterior resection, 3 laparoscopic sigmoid resections, and 2 laparoscopic hernia repairs.
Technical Aspects of Telerobotic Surgery
The overall latency experienced by the telerobotic surgeon was 135–140 ms. Of this, 14 ms was due to network delay between Hamilton and North Bay and the rest was due to compression and decompression of the video signals by the MPEG CODECs. This latency was noticeable for the telerobotic surgeon, but he was able to adapt to it without difficulty. At this latency, the telerobotic surgeon was able to safely and effectively use the 3 robotic arms to view the anatomic area of interest and complete complex surgical tasks that included fine dissection and identification of key structures (vagi, ureter, duodenum, etc), as well as suturing.
Intraoperative Collaboration
During each surgery, the telerobotic surgeon in Hamilton and the laparoscopic surgeon in North Bay collaborated to perform the surgeries. In half of the Nissen fundoplications, most of the paraesophageal dissection and suturing was performed by the telerobotic surgeon with the assistance of the laparoscopic surgeon, whereas in the other half, most of the paraesophageal dissection and suturing was done by the laparoscopic surgeon with assistance from the telerobotic surgeon. The telerobotic laparoscopic colectomies were also performed with the collaboration of the 2 surgeons. The mobilization of the colon and identification of all key structures (ureter, duodenum, and mesenteric vessels) was performed telerobotically and the resection was done by the laparoscopic surgeon through a small periumbilical incision. In one right hemicolectomy case (case 15), the robotic arms were positioned on the right side of the patient in an attempt to see whether the telerobotic surgeon could assist the local surgeon more efficiently, but we found that this setup led to the telerobotic surgeon experiencing paradoxical movements constantly and prevented him from assisting effectively. The case was completed laparoscopically by the local surgeon with telementoring from the distant (telerobotic) surgeon.
Setup Time
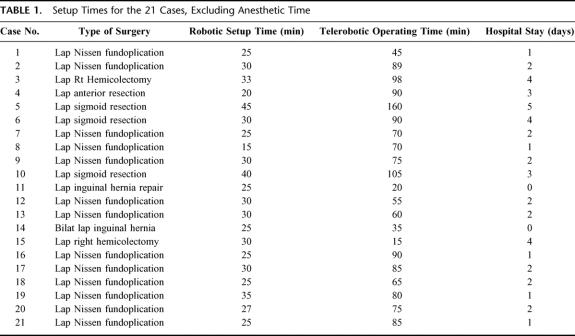
The setup times for the 21 cases excluding anesthetic time are given in Table 1. The setup time for the third case was longer than usual because of minor technical difficulty with instrumentation, which was dealt with prior to the start of the surgery.
TABLE 1. Setup Times for the 21 Cases, Excluding Anesthetic Time
Intraoperative Complications
There have been no major intraoperative complications during any of the 21 surgeries. The hospital stays are provided in Table 1.
There was a temporary disturbance in signal transmission during the first colectomy, but the telerobotic surgeon was able to switch immediately to the second telecommunication line with a delay of less that 1 second and continue. The disruption was so short in duration that there was no impact on the course of surgery and did not result in any complications. There has been a serosal tear of the colon by the robotic grasper in 2 cases, but both were in the segment that was eventually removed and had no clinical significance.
Postoperative Recovery
The recovery of all patients has been uneventful. Two of 13 patients who underwent laparoscopic Nissen fundoplication complained of some dysphagia at the 2 weeks’ postoperative visit, whereas a third had atypical chest pain at that time.
Future Surgeries
The 2 surgeons aim to collaborate to perform a number of other laparoscopic cases including Heller's myotomy, adrenalectomy, and nephrectomy. Cases have already been booked for the upcoming months on a weekly basis. There are also plans to expand the telerobotic surgical service between Hamilton, Ontario and Chicoutimi in northern Quebec by the end of the year.
DISCUSSION
After the first successful demonstration of telerobotic surgery by Professor Marescaux and colleagues in September 2001,1 many skeptics suggested that it would take another decade before this technology would be put into clinical use.2 Less than a year and a half later, we have now established a clinical hospital-to-hospital service to provide high-quality advanced laparoscopic surgical care for patients in a rural community. Although the robotic technology used is similar to the one used in the “Lindbergh operation,”1 the main difference is our ability to use a commercial fiberoptic network already in existence between the rural and teaching hospitals in Canada. The ability to use such a network means that this service can easily be extended to other rural sites with relatively little expense. There are plans to extend this service to Chicoutimi in northern Quebec and to Yellowknife NWT in the Arctic Circle in the near future.
The primary advantage of this technology to the healthcare system is that it enables local surgeons, who wish to offer a wider array of laparoscopic procedures to their patients, to gain experience and expertise with the assistance of an expert surgeon. The local surgeon involved in these cases had been partially trained in advanced laparoscopic techniques through short training courses, mentoring, and telementoring but not through a formal fellowship in laparoscopic surgery. The expert assistance of the telerobotic surgeon allows the local surgeon to perform these surgeries with a greater degree of confidence and ease and with excellent outcome. The alternative at this time is for either the patient to be transported to a tertiary center or for the expert surgeon to travel to remote local hospitals to perform these surgeries, both options involving considerable expense and obstacles in a country as large as Canada.
Prior to the commencement of the service, a great deal of work went into the reduction of the risk of communication failure and robotic failure. Although both possibilities do exist, it is believed that the chance of either event is approximately 1 in 1000. Local patients have had no hesitation to request telerobotic procedures and in fact the demand has increased for this type of collaboration.
Our center intends to develop a Surgical Support Network for provision of telementoring3 and telerobotic surgery between 8 teaching hospitals and 32 rural communities in Canada over the next 3 years. The ease with which the 2 surgeons have already been able to collaborate during the surgeries and interchange operating tasks in spite of latency4,5 has validated the notion that clinical use of telerobotic surgery is not only possible but is safe and effective in improving access to advance surgical care for rural and remote patients.
ACKNOWLEDGMENTS
The authors would like to acknowledge the assistance of the following persons, without whom this project would not have succeeded: the technical support staff from Bell Canada, Stryker Canada, and Computer Motion Inc.; Trevor Chapman, Cheryl Little, and Tammy Troy-Hempey from Centre for Minimal Access Surgery; the operating room staff at North Bay General Hospital; Catherine Gill Pottruff for assistance in preparation of the manuscript; and 21 courageous patients and their families.
Footnotes
Supported by a grant from the Canada Health Infostructure Partnership Program.
Reprints: Dr. M. Anvari, St. Joseph's Healthcare, 50 Charlton Avenue E., Hamilton, Ontario, Canada, L8N 4A6. E-mail: anvari@mcmaster.ca.
REFERENCES
- 1.Marescaux J, Leroy J, Rubino F, Smith M, Vix M, Simone M, Mutter Transcontinental robot-assisted remote telesurgery: Feasibility and potential applications. Ann Surg. 2002;235:300–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ballantyne GH. Robotic surgery, telerobotic surgery, telepresence and telementoring. Review of early clinical results. Surg Endosc. 2002;16:1389–1402. [DOI] [PubMed] [Google Scholar]
- 3.Link RE, Schulam PG, Kavoussi LR. Telesurgery. Remote monitoring and assistance during laparoscopy. Urol Clin North Am. 2001;28:177–188. [DOI] [PubMed] [Google Scholar]
- 4.Fabrizio MD, Lee BR, Chan DY, et al. Effect of time delay on surgical performance during telesurgical manipulation. J Endourol. 2000;14:133–138. [DOI] [PubMed] [Google Scholar]
- 5.Thompson JM, Ottensmeyer MP, Sheridan TB. Human factors in telesurgery: effects of time delay and asynchrony in video and control feedback with local manipulative assistance. Telemed J. 1999;5:129–137. [DOI] [PubMed] [Google Scholar]