Abstract
T-cell-mediated immune effector mechanisms play an important role in the containment of human immunodeficiency virus/simian immunodeficiency virus (HIV/SIV) replication after infection. Both vaccination- and infection-induced T-cell responses are dependent on the host major histocompatibility complex classes I and II (MHC-I and MHC-II) antigens. Here we report that both inherent, host-dependent immune responses to SIVmac251 infection and vaccination-induced immune responses to viral antigens were able to reduce virus replication and/or CD4+ T-cell loss. Both the presence of the MHC-I Mamu-A*01 genotype and vaccination of rhesus macaques with ALVAC-SIV-gag-pol-env (ALVAC-SIV-gpe) contributed to the restriction of SIVmac251 replication during primary infection, preservation of CD4+ T cells, and delayed disease progression following intrarectal challenge exposure of the animals to SIVmac251 (561). ALVAC-SIV-gpe immunization induced cytotoxic T-lymphocyte (CTL) responses cumulatively in 67% of the immunized animals. Following viral challenge, a significant secondary virus-specific CD8+ T-cell response was observed in the vaccinated macaques. In the same immunized macaques, a decrease in virus load during primary infection (P = 0.0078) and protection from CD4 loss during both acute and chronic phases of infection (P = 0.0099 and P = 0.03, respectively) were observed. A trend for enhanced survival of the vaccinated macaques was also observed. Neither boosting the ALVAC-SIV-gpe with gp120 immunizations nor administering the vaccine by the combination of mucosal and systemic immunization routes increased significantly the protective effect of the ALVAC-SIV-gpe vaccine. While assessing the role of MHC-I Mamu-A*01 alone in the restriction of viremia following challenge of nonvaccinated animals with other SIV isolates, we observed that the virus load was not significantly lower in Mamu-A*01-positive macaques following intravenous challenge with either SIVmac251 (561) or SIVSME660. However, a significant delay in CD4+ T-cell loss was observed in Mamu-A*01-positive macaques in each group. Of interest, in the case of intravenous or intrarectal challenge with the chimeric SIV/HIV strains SHIV89.6P or SHIVKU2, respectively, MHC-I Mamu-A*01-positive macaques did not significantly restrict primary viremia. The finding of the protective effect of the Mamu-A*01 molecule parallels the protective effect of the B*5701 HLA allele in HIV-1-infected humans and needs to be accounted for in the evaluation of vaccine efficacy against SIV challenge models.
The rate of human immunodeficiency virus type 1 (HIV-1) infection in developing countries has significantly increased in the last few years, and there is therefore an urgent need for the development of an effective vaccine. Studies in animal models have demonstrated the potential role of HIV-based neutralizing antibodies (Ab) in protecting against HIV infection (4, 34). The induction of neutralizing Ab against primary isolates by various vaccine modalities, however, has proven to be difficult, and restriction of viral replication by cell-mediated immune effector mechanisms appears to be a more realistic goal at present. The contribution of cell-mediated immune responses in controlling HIV-1 replication has been inferred in both acute and chronic HIV-1 infections (8, 27, 40, 42, 47) and clearly demonstrated in the simian immunodeficiency virus macaque (SIVmac) model (22, 35, 52).
Poxvirus-based vaccine candidates with various degrees of attenuation are known to induce cell-mediated immune responses and have been shown to prevent infection following challenge exposure to viruses with low virulence, such as some strains of HIV-2 (1, 3, 15) or SIVmac (21). They were also found to reduce viral burden following challenge exposure to highly pathogenic SIVmac isolates (7, 17, 41, 53). In addition, among the poxvirus vaccine candidates, NYVAC and ALVAC have also been demonstrated to be able to induce virus-specific CD4+ and CD8+ T-cell responses in SIV-infected macaques treated with antiretroviral therapy (18; our unpublished results).
ALVAC (canarypox virus)-based immunogens have been extensively evaluated as veterinary and human vaccine candidates (44) (unpublished results) with three such vaccines being registered with regulatory agencies. These are ALVAC-rabies and ALVAC-feline leukemia virus vaccines for cats and ALVAC-canine distemper virus vaccine for dogs. ALVAC-based HIV-1 vaccine candidates have been tested in more than 1,200 human volunteers and have been shown to be safe and immunogenic (11, 45). Preventive immunization of macaques with a canarypox vector-based HIV-2 immunogen was found to protect macaques from a nonpathogenic HIV-2 challenge (15). The relative efficacy of this vaccine modality, however, has not been assessed previously in the highly pathogenic SIVmac251 macaque model, in which disease progression and survival can be evaluated.
The usefulness of the SIVmac251 model in the evaluation of vaccine immunogenicity has been further enhanced by knowledge of macaque major histocompatibility complex (MHC) Mamu-A*01 status and SIV-specific epitopes restricted by this allelic form (2, 28–30). A study was therefore designed to assess whether immunization with an ALVAC-based vaccine candidate expressing the SIVmac251 Gag, Pol, and Env components and subsequent boosting with subunit gp120 boost could confer immunity and prevent or contain SIVmac251 replication following a mucosal exposure to SIVmac251. The results indicate that vaccination with ALVAC-SIV-gpe modified significantly the natural course of SIVmac251 (561) infection in Mamu-A*01-negative macaques (i.e., delayed the CD4+ T-cell loss) and that some Mamu-A*01-positive macaques naturally controlled viral replication. The MHC class I (MHC-I) Mamu-A*01 effect was also investigated following intravenous challenge with SIVmac251 (561) and SIVSME660 as well as with two simian/human immunodeficiency virus (SHIV) strains. The results indicate that the route of challenge exposure to SIV isolates influences the natural restriction of viremia in Mamu-A*01-positive animals regardless of the strain used and that in macaques infected with two independent SHIV isolates viremia restriction does not occur regardless of the challenge route.
MATERIALS AND METHODS
Vaccines, immunization protocol, and challenge virus stock.
Sixty-four macaques were used in this study. The ALVAC-SIV-gpe (vcp180) was engineered to express the gag, pol, and env genes of SIVmac251(K6W) (14) from the I3L and the H6 promoters (43). The H6 env and the I3L gag and pol cassettes were inserted in the ALVAC C3 locus in a head-to-head (5′-to-5′) configuration. Prior to amplification and purification of the vcp180 virus, the expression of the SIVmac251 genes was assessed in chicken embryo fibroblasts (data not shown). Groups A and B received 108 PFU of the ALVAC-SIV-gpe vaccine candidate by the intramuscular route at weeks 0, 4, 26, 52, and 113 or 143, and only animals in group B were inoculated intramuscularly with gp120 at weeks 26, 52, and 113 or 143 (Fig. 1). Groups C and D received 108 PFU of ALVAC-SIV-gpe gp160 at the same intervals as groups A and B by the intramuscular and, in addition, the intrarectal and intranasal routes (Fig. 1). Group D also received SIV gp120 (300 μg) adjuvanted in QS-21 (100 μg) at the same time intervals as group B (Fig. 1). The first control group received 108 PFU of ALVAC parental virus by the intramuscular route (group E), and the second was constituted of naive animals (group F). Group G received inoculations of gp120 (300 μg) in QS-21 adjuvant (100 μg) at weeks 0, 8, and 55. The SIV gp120 used for immunization was purified from the serum-free culture supernatant of SIVmac251 chronically infected Hut 78 cells by immunoaffinity column chromatography using anti-gp120 Ab as described previously (25). The macaques were challenged at week 117 of 147; animals were challenged intrarectally with 30 mucosal infectious doses of the SIVmac251 (561) isolate. The SIVmac251 challenge stock was prepared by culturing phytohemagglutinin (PHA)-activated peripheral blood mononuclear cells (PBMC) from a Mamu-A*01-positive infected macaque (561L) exposed to SIVmac251 by the vaginal route. The SIV challenge stock [SIVmac251 (561)] was titered in vivo in rhesus macaques by inoculating six animals with different dilutions of virus stock via the rectal route. Since six of six animals inoculated with the virus (0.5 ml diluted to 1.5 ml with RPMI medium) became infected, as evidenced by high plasma viremia and a drop in CD4 counts, this dose of virus was selected for all challenge studies.
FIG. 1.
Schematic representation of the immunization regimen. IM, intramuscular route; IR, intrarectal route; IN, intranasal route; V, vcp180 (ALVAC-SIV-gpe), 108 PFU; vcp, empty vector control (ALVAC), 108 PFU; •, gp120 (300 μg) in QS-21 (100 μg). The numbers on the right indicate the number of Mamu-A*01-positive and Mamu-A*01-negative macaques in each group. The long black arrow signifies the time (week 117 or 147) of intrarectal challenge with SIVmac251 stock 561.
SHIVKU2 challenge virus stock.
The SHIVKU2 challenge stock (23) was prepared by culturing PHA-activated PBMC from an infected macaque that was inoculated intravenously with SHIVKU2. The SHIVKU2 challenge stock was titered in vivo in rhesus macaques by rectal inoculation of animals with different dilutions of virus stock. Since six of six animals inoculated with the virus (0.5 ml diluted to 1 ml with RPMI medium) became infected, as evidenced by high plasma viremia, this dose of virus was selected for all challenge studies.
Immunological assays.
Serum samples were tested for SIV-specific Ab responses using an enzyme-linked immunosorbent assay (ELISA) described elsewhere (7). Serum titers were determined as the highest dilutions of immune serum producing ELISA values (A450) greater than or equal to two times the binding detected with a corresponding dilution of preimmune serum.
To assess SIV-specific serum-neutralizing activity, two types of assays were conducted with sera from the vaccinated animals. In the first assay, sera were tested for their ability to neutralize a T-cell-line-adapted stock of SIVmac251 grown in H9 cells and assayed in CEMx174 cells as described previously (38). In the second assay, neutralization of the challenge stock of SIVmac251 (561) was examined in PHA-activated human PBMC by measuring a reduction in viral p27 Gag antigen synthesis (31). CD4+ T-cell count in the PBMC of challenged animals was determined by standard flow-cytometric analyses (FAST Systems, Inc., Gaithersburg, Md.).
CTL assay and tetramer staining.
PBMC (8 × 106) from macaques were cultivated in vitro with paraformaldehyde-fixed, autologous B-lymphoblastoid cell lines (B-LCL) infected with vaccinia virus encoding SIV Env and SIV Gag components. On day 3 of culture, 20 U of recombinant human interleukin-2 per ml was added to the cultures. On day 12 of culture, the lymphocytes were centrifuged over a Ficoll-diatrizoate gradient and assessed as effector cells in a standard 51Cr-release cytolytic assay. Target cells were B-LCL (106) cultured overnight with vaccinia virus encoding SIV Env, SIV Gag, or control antigen at a multiplicity of infection of 10 PFU/cell. B-LCL were then washed and labeled with 100 μCi of sodium 51chromate for 1.5 h. After being washed, 104 target cells were added per well in 96-well U-bottom plates in 100-μl volumes. Effector cells were added in another 100-μl volume at various concentrations to give effector-to-target ratios of 20:1, 10:1, 5:1, and 2.5:1. Plates were incubated at 37°C for 4 h. Fifty microliters of supernatant was transferred to counting plates and 200 μl of scintillation fluid was added and analyzed in a Wallac 1450 MicroBeta liquid scintillation counter. Specific release was calculated according to the following formula: (experimental release − spontaneous release)/(100% release − spontaneous release) × 100 (Table 1). The Mamu-A*01-positive rhesus monkeys were evaluated for p11C-specific cytotoxic T-lymphocytes (CTLs) using Mamu-A*01/p11C tetramer staining of unstimulated peripheral blood CD8+ T lymphocytes. Soluble tetrameric Mamu-A*01/peptide complexes were prepared, and 1 μg of phycoerythrin-labeled tetrameric Mamu-A*01/peptide complexes was used in conjunction with fluorescein isothiocyanate-labeled anti-human CD8α (Leu2a; Becton-Dickinson, San Diego, Calif.), energy-coupled dye-labeled anti-human CD8αβ (2ST8-5H7; Beckman Coulter, Fullerton, Calif.), and allophycocyanin-labeled anti-rhesus monkey CD3 (FN18) monoclonal Ab to stain p11C-specific CD8+ T cells. One hundred microliters of whole blood from the vaccinated monkeys was directly stained with these reagents, lysed, washed, and fixed.
TABLE 1.
Cytotoxic response to Gag and Env in the immunized animals
| ALVAC-SIV-gpe (vcp180) vacci-nation routea | gp120 boostb | Animal no.c | % percent CTL activityb at week:
|
|||||
|---|---|---|---|---|---|---|---|---|
| 28
|
54
|
115
|
||||||
| Env | Gag | Env | Gag | Env | Gag | |||
| IM | − | 428 | 10 | —e | 9 | — | 32 | — |
| IM | − | 398 | 12 | — | 16 | — | — | — |
| IM | − | 411 | 11 | — | — | — | 28 | — |
| IM | − | 412 | — | — | — | — | 25 | — |
| IM | − | 397 | — | — | — | — | — | — |
| IM | − | 423 | — | — | — | — | — | |
| IM | + | 402 | 22 | — | 40 | — | 42 | 26 |
| IM | + | 401 | 10 | — | 12 | — | 32 | — |
| IM | + | 416 | 12 | — | 23 | — | 14 | — |
| IM | + | 415 | 17 | — | 22 | — | — | — |
| IM | + | 429 | 13 | — | — | — | — | 26 |
| IM | + | 414 | 18 | — | — | — | — | — |
| IM, IR, IN | − | 400 | 17 | — | 47 | — | 28 | — |
| IM, IR, IN | − | 410 | 10 | — | — | — | — | — |
| IM, IR, IN | − | 399 | — | — | — | — | — | — |
| IM, IR, IN | − | 413 | — | — | — | — | — | — |
| IM, IR, IN | − | 424 | — | — | — | — | — | — |
| IM, IR, IN | − | 435 | — | — | — | — | — | — |
| IM, IR, IN | + | 409 | 22 | — | — | — | 33 | — |
| IM, IR, IN | + | 417 | 10 | — | — | — | — | — |
| IM, IR, IN | + | 418 | — | — | — | — | 19 | — |
| IM, IR, IN | + | 430 | NDf | ND | 11 | — | — | — |
| IM, IR, IN | + | 403 | — | — | — | — | — | — |
| IM, IR, IN | + | 404 | — | — | — | — | — | — |
IM, intramuscular; IR, intrarectal; IN, intranasal.
gp120 was given intramuscularly in QS-21 adjuvant.
Boldfaced numbers, Mamu-A*01-positive animals.
Percentage of cytolytic activity at an effector-to-target ratio of 20:1; cumulative CTL response: 16 of 24 (67%).
—, no cytotoxic activity.
ND, not determined.
Virological assay.
Animals were bled periodically following challenge, and viral load in plasma was assessed using a nucleic acid sequence-based amplification assay to quantify SIV RNA (48). In addition, PBMC collected from animals 21 days following virus challenge were subjected to quantitative virus isolation by coculturing with CEMx174 cells to confirm virus transmission.
RESULTS
Study design.
The experimental vaccination regimen included seven groups (A through G) of rhesus macaques (Fig. 1). The experimental groups A through D were immunized five times with ALVAC-SIV-gpe (108 PFU) and, at the time of the last three immunizations, animals enrolled in groups B and D were inoculated simultaneously with native SIVmac251 gp120. Control animals received either five immunizations with ALVAC vector (group E) or were left naive (group F). Lastly, group G animals received three inoculations with gp120. ALVAC-SIV-gpe was administered either by the intramuscular route (groups A and B) or by a combination of the intramuscular, intranasal, and intrarectal routes (groups C and D), whereas gp120 was administered by the intramuscular route, as described in Materials and Methods. A total of 19 Mamu-A*01-positive animals were included in the study and were distributed among the groups as summarized in Fig. 1.
Humoral immune response elicited by ALVAC-SIV-gpe.
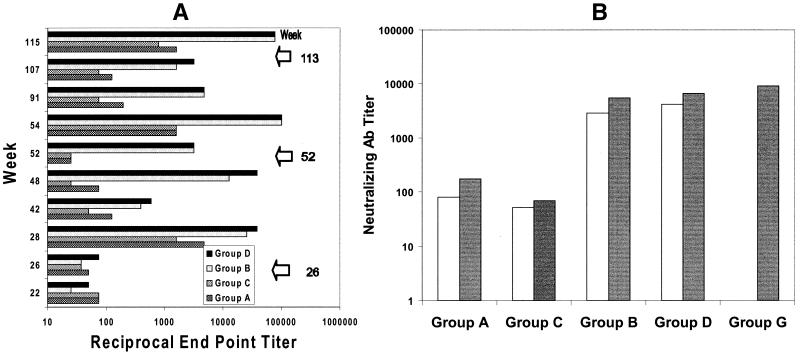
Serum Ab to SIVmac251 were measured in half of the animals from each group by ELISA using whole disrupted SIVmac251 virus spiked with purified gp120. Ab titers were negligible after two inoculations with ALVAC-SIV-gpe (data not shown). However, after the third immunization (week 26), the Ab titers increased and were highest in groups B and D, which also received the QS-21-adjuvanted gp120 (Fig. 2A). Although the Ab titers declined between immunizations, a steady level of Ab was present throughout the course of vaccination (Fig. 2A). A similar pattern was observed with the rest of the animals.
FIG. 2.
Humoral response in immunized animals. (A) Median titer values of Ab in prechallenge sera of the immunized macaques. ELISA Ab titers were obtained using a total lysate of SIVmac251 spiked with purified native gp120. (B) Neutralization Ab titers in sera of ALVAC-SIV-gpe-vaccinated macaques. The median neutralizing Ab titer of immunized animals from groups A through D to the laboratory-adapted SIVmac251 was assessed on CEMx174 cells using sera collected at month 12 (clear bar) and 2 weeks after the final boost (filled bar), whereas for group G animals the assay was conducted using sera collected at 2 weeks after the final boost (filled bar).
Both immunoglobulin G (IgG)- and IgA-specific Ab responses to SIV gp120 and p27 antigens were measured by ELISA in mucosal secretions such as rectal wash, saliva, and vaginal wash collected at week 115 in six animals from groups A through E. Neither IgG- nor IgA-specific Ab to SIV p27 were detected in animals from any of the vaccine groups (data not shown). In contrast, serum IgG-specific Ab response to gp120 was detected in most animals from groups B and D boosted with gp120 regardless of the route of administration of ALVAC-SIV-gpe. A low level of IgA-specific Ab to gp120 was detected in the saliva or vaginal secretions of two animals from group D only (data not shown).
Neutralizing Ab titers in sera from all ALVAC-vaccinated animals (groups A to D) collected at month 12 and 2 weeks following the final boost were measured against those of the laboratory-adapted SIVmac251 isolate in CEMx174 cells as well as the primary challenge stock of SIVmac251 (561) in human PBMC. For animals receiving the gp120 boost (group G), sera collected 2 weeks following the final boost were similarly assayed for neutralizing Ab titers. Neutralizing Ab titers to the laboratory-adapted SIVmac251 were detected in most animals receiving the vaccine candidate but were highest in animals boosted with the gp120 subunit preparation (Fig. 2B), whereas none of the serum samples neutralized the SIVmac251 (561) primary challenge stock in a human-PBMC-based assay (titers <1:5; 80% reduction in p27 synthesis was considered positive) (data not shown).
CTL activity induced by ALVAC-SIV-gpe.
T-cell-mediated cytolytic activity was assessed in the blood of six of the immunized animals in each group as well as in control animals from group E following the third, fourth, and last immunizations. Cumulatively, 16 of 24 (67%) animals demonstrated an Env-specific CTL activity at at least one time point analyzed. Thirteen animals recognized Env target cells after the third immunization and, of those, nine were also positive following either the fourth or the fifth immunization (Table 1). Overall, 22% of the vaccinees demonstrated CTL activity against either Env or Gag at all times, 42% were positive two times, and 67% were positive at any single point. Among the control animals in group E, only one animal scored positive at a single time point. There was a trend suggesting that the relative frequency of measurement of CTL responses in peripheral blood in animals vaccinated by the systemic route was higher than in animals vaccinated also by the mucosal route (10 of 12 versus 6 of 12, respectively) (Table 1).
A surprising finding was that only 2 of 24 animals had detectable cytolytic activity against the SIV Gag protein, whereas 16 of 24 animals had cytolytic activity against the SIV Env protein. A possible explanation is that CTLs specific for Gag may have existed at a frequency below the level of detection by the assay. In fact, staining with tetramer for the peptide p11C epitope following specific peptide stimulation in vitro demonstrated that most of the vaccinated Mamu-A*01-positive animals (Table 1) indeed had memory CTL response to the Gag-immunodominant p11C epitope prior to viral challenge exposure (data not shown).
Mock-vaccinated Mamu-A*01-positive macaques naturally restrict SIVmac251 (561) replication.
Following intrarectal challenge exposure to SIVmac251 stock 561, all 22 macaques from groups E, F, and G became viremic and seroconverted to viral antigens. Analysis of the plasma virus load during primary infection, set point, and chronic infection did not reveal significant differences among the groups, as summarized in Table 2. These data demonstrate that neither the gp120 subunit immunization nor the ALVAC mock vaccination influenced the virological outcome. Therefore, all these animals were gathered together to increase the statistical power of the subsequent analysis.
TABLE 2.
Comparison of virus load among animals from groups E, F, and G
| Immunizations |
P valuea for viremia at:
|
||
|---|---|---|---|
| Peak | Set point | 3–6 mo | |
| Mamu-A*01-negative macaques gp120-immunized (4) vs ALVAC-immunized (11) or naive | 0.10 | 0.49 | 0.75 |
| Mamu-A*01-positive macaques gp120-immunized (2) vs ALVAC-immunized (5) or naive | 0.57 | 1.0 | 0.95 |
| Mamu-A*01-positive macaques vs naive Mamu-A*01-negative control macaques gp120- or ALVAC-immunized (7) vs naive (5) | 0.76 | 0.69 | 0.064 |
Calculated from the exact Wilcoxon rank sum tests.
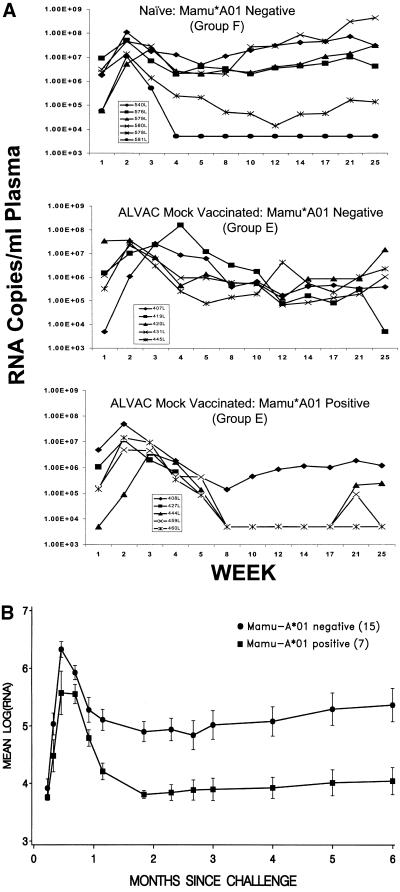
Interestingly, measurement of viral RNA in the Mamu-A*01-positive and -negative mock-vaccinated macaques revealed that among the Mamu-A*01-positive macaques four of five controlled viremia at set point up to week 17, as demonstrated for each animal in Fig. 3A. In fact, when the virus load in all the control animals (groups E, F, and G) was stratified according to the Mamu-A*01 status (15 were Mamu-A*01 negative and 7 were Mamu-A*01 positive), statistical analysis of the viral-load data demonstrated that in the seven mock-vaccinated Mamu-A*01-positive animals virus load was significantly lower than in the Mamu-A*01-negative macaques during primary viremia (0 to 28 days), at set point (2 to 3 months), and thereafter (for primary viremia, P = 0.0066 by the Wilcoxon rank sum test; for set point, P = 0.0007 by the Wilcoxon-Gehan test; for median viremia, P = 0.0068 by the Wilcoxon-Gehan test). In fact, most Mamu-A*01-positive animals had nondetectable viremia at set point and thereafter, as demonstrated for each animal in Fig. 3A and collectively in Fig. 3B. All together, these data indicate that the Mamu-A*01-positive macaques naturally restricted replication following intrarectal exposure to SIVmac251 (561).
FIG. 3.
Levels of viremia in control macaques following SIV251 challenge. (A) Viral RNA copies/milliliter of plasma over time in each animal from groups E, F, and G (Fig. 1). (B) Mean levels of viral load at each time point in Mamu-A*01-positive and -negative control macaques.
Effect of ALVAC-SIV-gpe vaccination in Mamu-A*01-positive animals.
Because of the natural ability of Mamu-A*01-positive macaques to control SIVmac251 (561) intrarectal infection, the statistical analysis of the relative efficacy of ALVAC-SIV-gpe vaccine was assessed independently in the Mamu-A*01-positive and the Mamu-A*01-negative animals. Genetic characterization of all animals enrolled in this study demonstrated the presence of 12 Mamu-A*01-positive animals among the 42 ALVAC-SIV-gpe-vaccinated macaques (Fig. 1). Unknown to us at the beginning of the study, the vaccinated Mamu-A*01-positive animals were interspersed unevenly in the experimental groups A through D (Fig. 1). Since in retrospect we observed a significant containment of viremia in the Mamu-A*01-positive animals (Fig. 3B), the overall evaluation of relative vaccine efficacy was assessed independently in Mamu-A*01-positive and -negative vaccinated and control macaques.
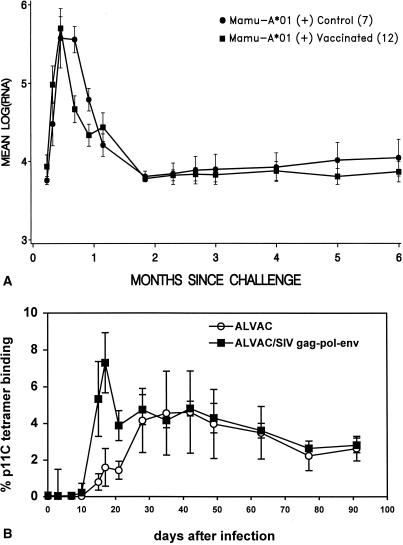
In Mamu-A*01-positive vaccinated and control macaques, the overall difference in viremia during primary infection (0 to 28 days) was not significant (Table 3), even though the vaccinated macaques appeared to control viremia faster than the nonvaccinated Mamu-A*01-positive animals (Fig. 4A). In fact, the quantitation of CD3+ CD8+ peptide p11C tetramer response in the blood of animals following challenge exposure demonstrated a faster appearance of this response in the vaccinated animals than in control animals (Fig. 4B), consistent with a secondary response. This difference was found to be significant in the interval from day 13 through day 28 postchallenge (P = 0.0075) by the application of repeated-measures analysis of variance to the arc-sine-transformed tetramer data (Fig. 4B). These data further support the importance of cell-mediated immunity in controlling SIV replication, as demonstrated by other studies (22, 29, 35, 52), and indicate that the ability of Mamu-A*01-positive animals to restrict viral replication may mask the relative efficacy of vaccines. No significant difference in the early CD4+ T-cell drop was observed between these two groups (data not shown). Accordingly, no deaths were observed in the Mamu-A*01-positive group regardless of the vaccination status (Fig. 5C).
TABLE 3.
Statistical analyses of plasma viral RNA load measured at different stages following virus challenge
| Groups compared |
P value for viral load at:
|
||
|---|---|---|---|
| Primary infection (0–28 days)a | Set pointb | 3–6 mo | |
| Mamu-A*01-positive macaques, vaccinated (12) vs mock vaccinated (7) | 0.54 | 0.79 | 0.49 |
| Mamu-A*01-negative macaques, vaccinated (30) vs mock vaccinated (15) | 0.0078 | 0.33 | 0.95 |
| Intramuscularly immunized macaques (16) vs intramuscularly, intrarectally, intranasally immunized macaques (14) | 0.16 | 0.96 | 0.94 |
| Mamu-A*01-negative macaques plus gp120 boost (17) vs no gp120 boost (13) | 0.8 | 0.95 | 0.53 |
Wilcoxon rank sum test (two-tailed).
Wilcoxon-Gehan test (two-tailed).
FIG. 4.
Viral load and anamnestic response in Mamu-A*01-positive control and ALVAC-SIV-gpe-vaccinated macaques. (A) Average viral load in the mock-vaccinated (•) and ALVAC-SIV-gpe-vaccinated (▪) Mamu-A*01-positive macaques. (B) Mean values of the frequency of SIV Gag p11C-tetramer-binding CD8+ lymphocytes in the whole blood of the control and ALVAC-SIV-gpe-immunized Mamu-A*01-positive rhesus monkeys after challenge with SIVmac251. The percent p11C tetramer represents p11C-tetramer-binding CD8αβ+ T cells in unstimulated whole blood at each time point tested. Open circles represent the means and standard errors of means (SEMs) of percent p11C-tetramer-binding CD8αβ+ T cells of five monkeys that received the control vaccine, and filled squares represent the means and SEMs of percentages of p11C-tetramer-binding CD8αβ+ T cells of six monkeys that received the ALVAC-SIV-gpe vaccine.
FIG. 5.
Virus load, CD4+ T cell counts, and survival in vaccinated and control Mamu-A*01-negative macaques. (A) Mean virus load in Mamu-A*01-negative vaccinated (•), control (•), and all vaccinated and nonvaccinated Mamu-A*01-positive animals (▪). In this analysis, only animals that were monitored for 1 year are included. Therefore, the group of Mamu-A*01-positive animals included 8 macaques (6 vaccinees and 2 controls), the group of Mamu-A*01-negative vaccinees included 18 macaques, and the group of Mamu-A*01-negative control animals included 6 macaques. Peak viral loads during primary infection differed significantly between vaccinated and mock-vaccinated Mamu-A*01-negative macaques (P = 0.011) when analyzed using the Wilcoxon rank sum test. Because of the frequency of left censoring, the Wilcoxon-Gehan test was applied to the median viral load over later intervals. However, in these intervals no significant difference in virus load was observed (P = 0.37 at set point and P = 0.97 thereafter). (B) Mean CD4+ T-cell count in the animal groups described in the legend to panel A. The same symbols are used as for panel A, and the same animals per group were analyzed. CD4+ T-cell counts were tested by repeated-measures analysis of variance of the square-root-transformed raw data, and during primary infection a significant difference was observed between vaccinated and control animals (P = 0.013). (C) Number of deaths for SIVmac251-related disease within 1 year of viral challenge. The animals per group are the same as for panel A. Survival probabilities were estimated by the Kaplan-Meier method and demonstrated a trend of higher survival in vaccinated macaques than in control macaques.
ALVAC-SIV-gpe vaccination decreases primary viremia and CD4+ T-cell loss in Mamu-A*01-negative macaques.
The effects of ALVAC-SIV-gpe vaccination on viral load and the natural course of SIVmac251 infection were evaluated separately in the Mamu-A*01-negative macaques. Of the 30 vaccinated and 15 mock-vaccinated Mamu-A*01-negative macaques, all became infected except 2 vaccinees. The 30 vaccinated animals experienced lower viremia in primary infection (first 28 days) than the 15 control macaques (P = 0.0078) (Table 3). When the peak viremia in the 30 vaccinated animals was compared to that in 11 control macaques (excluding 4 macaques that received gp120), this difference was even more significant (P = 0.0034) (Fig. 5A). The set-point viremias in the control and vaccinated macaques did not differ significantly (Table 3), but, remarkably, the analysis of the absolute CD4+ T-cell count (Fig. 5B) indicated that the 30 vaccinated animals were protected from acute loss of CD4+ T cells within the first 2 months of infection (P = 0.0099) and during the 1-year follow-up (P = 0.03). Among the vaccinated Mamu-A*01-negative macaques, fewer deaths occurred than among Mamu-A*01-negative control animals, but this difference did not reach statistical significance (Fig. 5C).
The contribution of boosting with the gp120 subunit preparation and the route of immunization of the ALVAC-SIV-gpe vaccine effect were also analyzed by comparing virus load and CD4+ T-cell count in Mamu-A*01-negative animals from groups A and C to those in animals from groups B and D. As demonstrated in Table 2, neither the monomeric gp120 subunit preparation nor the combination of the routes of immunization appeared to significantly contribute to the effect of ALVAC-SIV-gpe vaccination. Accordingly, no significant difference in the CD4+ T-cell counts was observed between the vaccinated groups of animals (data not shown).
Collectively, these data demonstrate that a decrease in virus load during primary and chronic infection and preservation of CD4+ T cells occurred in Mamu-A*01-positive animals regardless of their vaccination status. In Mamu-A*01-negative animals, however, a vaccine effect was also observed, and those macaques experienced a significantly lower level of viremia during primary infection than did control macaques. This effect was presumably associated with a better preservation of CD4+ T cells and was associated with fewer deaths in the vaccinated animals than in control animals within 1 year of SIVmac251 (561) infection.
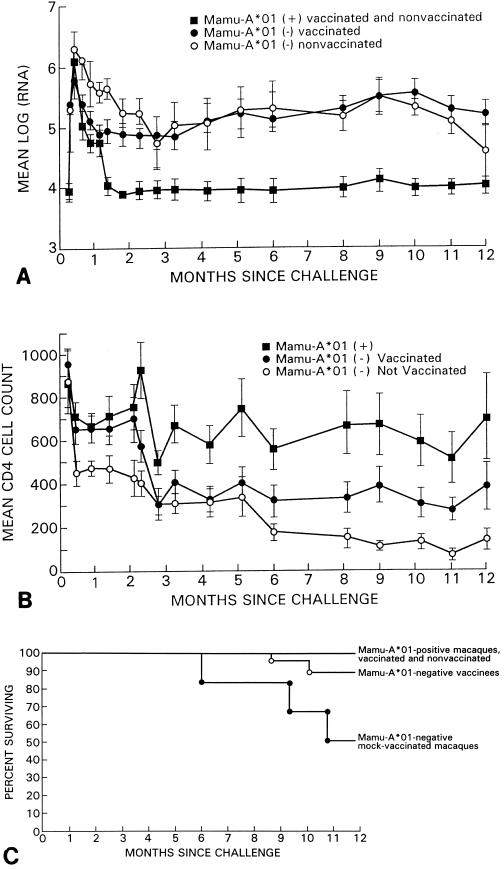
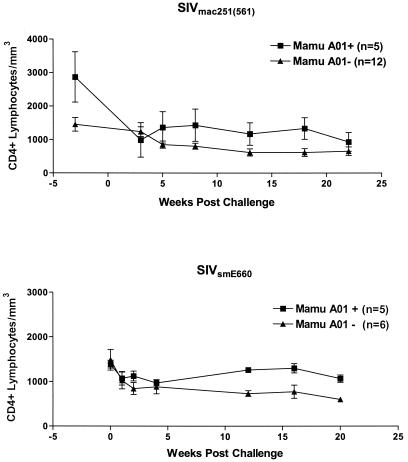
Preservation of CD4+ T cells in Mamu-A*01-positive macaques following intravenous challenge with either SIVmac251 (561) or SIVSME660.
We further investigated whether the inherent ability of Mamu-A*01-positive macaques to restrict viral replication observed in our study was dependent on the route of challenge. To do so, virus load and CD4+ T-cell counts were analyzed for up to 24 weeks postchallenge in 5 Mamu-A*01-positive and 12 Mamu-A*01-negative naive macaques previously infected intravenously with the same 561 stock of SIVmac251. In addition, to assess whether the Mamu-A*01 effect could also be extended to other SIV isolates, we retrospectively analyzed the virus load and CD4+ T-cell count in Mamu-A*01-positive and -negative control macaques infected previously with SIVSME660 (41, 53, 54). Analysis of the virus loads in the blood of macaques following intravenous exposure to SIVmac251 (561) or SIVSME660 did not reveal a significant reduction in virus load within the first 20 weeks of infection in animals from either group (data not shown). However, longitudinal analysis of the absolute CD4+ T-cell count during the same period indicated a better preservation of the absolute CD4+ T-cell count in Mamu-A*01-positive macaques infected with either virus (Fig. 6). In fact, in animals infected with the SIVmac251 (561) strain, repeated-measures analysis of variance on the square-root-transformed CD4+ T-cell count over a 6-month interval revealed that the differences in CD4+ T-cell counts were significant at the P level of <0.001 for each of the intervals analyzed (Fig. 6, top panel). Similarly, in macaques inoculated intravenously with SIVSME660, the loss in CD4+ T-cell counts differed significantly between Mamu-A*01-positive and -negative animals (Fig. 6, bottom panel) and was delayed in Mamu-A*01-positive macaques (weeks 8, 12, and 16; P < 0.052 for each by the Wilcoxon rank sum test and P < 0.0001 by the repeated-measures analysis of variance). All together, these results need to be accounted for in the evaluation of a vaccine effect when preservation of CD4+ T cells is included as a parameter of vaccine protection.
FIG. 6.
Analysis of the mean CD4+ T-cell value in Mamu-A*01-positive and Mamu-A*01-negative macaques after intravenous SIV challenge. (Top) Data from five Mamu-A*01-positive and 12 Mamu-A*01-negative macaques challenged intravenously with SIVmac251 (stock 561). (Bottom) Data from five Mamu-A*01-positive and six Mamu-A*01-negative macaques challenged intravenously with SIVSME660.
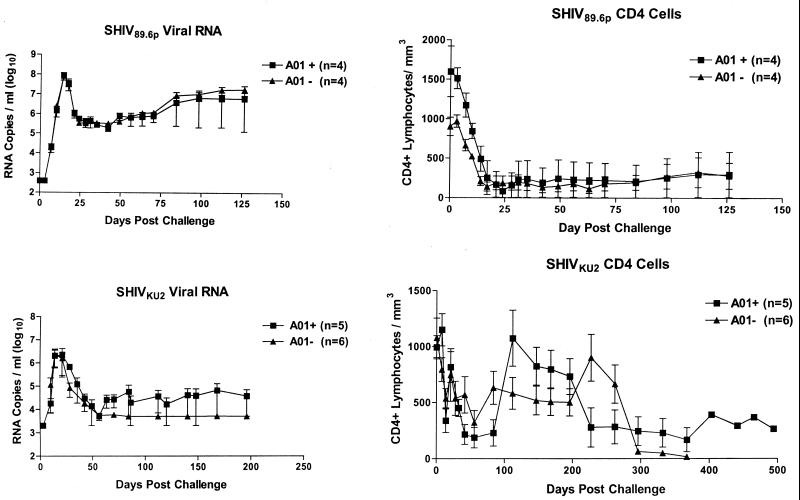
The Mamu-A*01 effect is not evident following infection with two chimeric SIV/HIV-1 strains.
Other macaque models used in the evaluation of HIV-1 vaccine candidates include the use of chimeric SHIVs. To investigate whether the Mamu-A*01 molecule could also have a protective effect following SHIV infection, the viremia and CD4+ T-cell counts of Mamu-A*01-positive and -negative macaques following challenge with either SHIV89.6P by the intravenous route or SHIVKU2 by the intrarectal route were compared. Viremia levels and CD4+ T-cell numbers did not differ among Mamu-A*01-positive and -negative animals following SHIV89.6P intravenous challenge (Fig. 7, upper panels) or SHIVKU2 intrarectal challenge (Fig. 7, lower panels).
FIG. 7.
Virus load and CD4+ T-cell counts in macaques infected with the SHIV89.6P and SHIVKU2 strains. Shown are viremia and CD4+ T-cell data obtained from four Mamu-A*01-positive and four Mamu-A*01-negative macaques infected intravenously with SHIV89.6P (top panels) and viremia and CD4+ T-cell counts obtained from five Mamu-A*01-positive and six Mamu-A*01-negative macaques infected intrarectally with SHIVKU2 (bottom panels).
DISCUSSION
In this study, we have demonstrated that prophylactic ALVAC-SIV-gpe vaccination of macaques followed by intrarectal challenge exposure with the highly pathogenic SIVmac251 strain was associated with lower primary viremia, better preservation of CD4+ T-cell counts during primary and chronic infection, and prolonged survival. The neutralizing Ab response induced by a monomeric gp120 subunit preparation did not contribute to the observed protection from disease, presumably because none of the animals developed an Ab response capable of neutralizing the primary-challenge stock virus. However, vaccination with the ALVAC-SIV-gpe induced SIV-specific CD8+ T-cell virus-specific cytolytic activity in 67% of the vaccinated animals and was associated with a significant secondary response to the Gag p11C peptide in the Mamu-A*01-positive macaque following virus challenge exposure. Similarly, the vaccinated Mamu-A*01-negative macaque did better than control nonvaccinated macaques.
It is to be noted that the viral challenge stock used in this study infected 100% of the control macaques (22 control animals and 6 animals in the titration study). It is quite likely that the infectivity of this stock as well as the size of virus inoculum used during challenge may far exceed that of HIV-1 transmission, as the recently estimated frequency of transmission of HIV-1 in humans appears to be relatively low (46, 50).
The immunogenicity of ALVAC-based HIV vaccine candidates has been extensively studied in human volunteers enrolled in clinical trials of phases I and II, and the immunogenicity of this vaccine in humans mirrors that observed in the macaques studied here (6, 10, 12, 13, 16, 24, 51). However, despite clear evidence of immunogenicity, enthusiasm to proceed to extended efficacy trials has been tempered by incomplete knowledge of vaccine-induced immune parameters and protection against lentivirus exposure. The study presented here indicates that although vaccinated macaques were not protected from infection they did demonstrate significant differences in the virological and clinical outcome following exposure to a pathogenic SIVmac251 challenge. It should be noted that despite such uncertainties as to whether results obtained in the macaque model can be extrapolated to humans, recent studies seem to indicate that it may be appropriate to do so. For instance, therapeutic intervention in SIVmac251 primary infection (18, 20, 32, 33, 39, 55) has paralleled closely results obtained in primary HIV-1 infection in humans (49), validating the SIV macaque model. Furthermore, the observation presented in this communication (that Mamu-A*01-positive macaques are better able to control viral replication than macaques carrying other MHC-I molecules) highlights additional similarities to HIV-1 infection of humans. In HIV-1 infection, the maximum heterogeneity of HLA class I molecules or the single HLA-B*5701 molecule has been associated with a more benign clinical course (9, 37) whereas HLA A1-B8-DR3, B27, CW7, and B*35-Cw*04 molecules are correlated with faster disease progression (9, 26, 36, 56). Mamu-A*01-positive rhesus macaques appear to develop early robust multiepitope virus-specific CD8+ T-cell responses (2) (B. R. Mothe et al., submitted for publication), which persist in various compartments (19) and may contribute to their ability to restrict viral replication, as observed in this study, and this further underscores the importance of the breadth of CD8+ T-cell immune response to the containment of viral replication. Finally, this study indicates that the genetic background of macaques used in preclinical studies of the relative efficacy of the SIVmac251 model needs to be accounted for in comparative studies. In this context, it is to be noted that upon intravenous challenge the Mamu-A*01-related protective effect was more evident on the loss of CD4+ T cells than on viremia. This effect did not appear to be restricted to our viral stock, since it was observed also with the SIVSME660 strain. Interestingly, however, in other studies in which intravenous transmission of SHIV89.6P viruses was assessed in naive Mamu-A*01-positive and -negative macaques (5) and in our studies following intrarectal challenge with SHIVKU2, the Mamu-A*01 effect was not evident, regardless of the route of challenge. These differences between SIV and SHIV strains are unclear but may be explained by a differential response of rhesus macaques to HIV-1 proteins (Env, Tat, Nef, Rev) present in the SHIV chimeric virus. In summary, our findings demonstrate that the ALVAC-based SIV-gpe vaccine protected macaques from disease induced by this highly pathogenic virus and warrant more testing of the efficacy of an ALVAC-based HIV vaccine candidate in humans.
Acknowledgments
We thank David I. Watkins for helpful discussion, Sharon Orndorff for technical coordination, and Steven Snodgrass for editorial assistance.
This work was supported in part by National Institutes of Health grant AI-85343 (N. L. Letvin and D. C. Montefiori), National Institute of Allergy and Infectious Diseases contracts N01-AI55271 and N01-AI55260 to Advanced BioScience Laboratories, Inc., and National Institute of Allergy and Infectious Diseases contract NIH-NIAID-AI-65312 (M. G. Lewis).
REFERENCES
- 1.Abimiku, A. G., G. Franchini, J. Tartaglia, K. Aldrich, M. Myagkikh, P. D. Markham, P. Chong, M. Klein, M. P. Kieny, E. Paoletti, R. C. Gallo, and M. Robert-Guroff. 1995. HIV-1 recombinant poxvirus vaccine induces cross-protection against HIV-2 challenge in rhesus macaques. Nat. Med. 1:321–329. [DOI] [PubMed] [Google Scholar]
- 2.Allen, T. M., B. R. Mothe, J. Sidney, P. Jing, J. L. Dzuris, M. E. Liebl, T. U. Vogel, D. H. O’Connor, X. Wang, M. C. Wussow, J. A. Thomson, J. D. Altman, D. I. Watkins, and A. Sette. 2001. CD8(+) lymphocytes from simian immunodeficiency virus-infected rhesus macaques recognize 14 different epitopes bound by the major histocompatibility complex class I molecule mamu-A*01: implications for vaccine design and testing. J. Virol. 75:738–749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Andersson, S., B. Makitalo, R. Thorstensson, G. Franchini, J. Tartaglia, K. Limbach, E. Paoletti, P. Putkonen, and G. Biberfeld. 1996. Immunogenicity and protective efficacy of a human immunodeficiency virus type 2 recombinant canarypox (ALVAC) vaccine candidate in cynomolgus monkeys. J. Infect. Dis. 174:977–985. [DOI] [PubMed] [Google Scholar]
- 4.Baba, T. W., V. Liska, R. Hofmann-Lehmann, J. Vlasak, W. Xu, S. Ayehunie, L. A. Cavacini, M. R. Posner, H. Katinger, G. Stiegler, B. J. Bernacky, T. A. Rizvi, R. Schmidt, L. R. Hill, M. E. Keeling, Y. Lu, J. E. Wright, T. C. Chou, and R. M. Ruprecht. 2000. Human neutralizing monoclonal antibodies of the IgG1 subtype protect against mucosal simian-human immunodeficiency virus infection. Nat. Med. 6:200–206. [DOI] [PubMed] [Google Scholar]
- 5.Barouch, D. H., S. Santra, J. E. Schmitz, M. J. Kuroda, T.-M. Fu, W. Wagner, M. Bilska, A. Craiu, X. X. Zheng, G. R. Krivulka, K. Beaudry, M. A. Lifton, C. E. Nickerson, W. L. Trigona, K. Punt, D. C. Freed, L. Guan, S. Dubey, D. Casimiro, A. Simon, M.-E. Davies, M. Chastain, T. B. Strom, R. S. Gelman, D. C. Montefiori, M. G. Lewis, E. A. Emini, J. W. Shiver, and N. L. Letvin. 2000. Control of viremia and prevention of clinical AIDS in rhesus monkeys by cytokine-augmented DNA vaccination. Science 290:486–492. [DOI] [PubMed] [Google Scholar]
- 6.Belshe, R. B., G. J. Gorse, M. J. Mulligan, T. G. Evans, M. C. Keefer, J. L. Excler, A. M. Duliege, J. Tartaglia, W. I. Cox, J. McNamara, K. L. Hwang, A. Bradney, D. Montefiori, and K. J. Weinhold. 1998. Induction of immune responses to HIV-1 by canarypox virus (ALVAC) HIV-1 and gp120 SF-2 recombinant vaccines in uninfected volunteers. NIAID AIDS Vaccine Evaluation Group. AIDS 12:2407–2415. [DOI] [PubMed] [Google Scholar]
- 7.Benson, J., C. Chougnet, M. Robert-Guroff, D. Montefiori, P. D. Markham, G. M. Shearer, R. C. Gallo, M. P. Cranage, E. Paoletti, K. Limbach, D. Venzon, J. Tartaglia, and G. Franchini. 1998. Recombinant vaccine-induced protection against the highly pathogenic SIVmac251: dependence on route of challenge exposure. J. Virol. 72:4170–4182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Borrow, P., H. Lewicki, B. H. Hahn, G. M. Shaw, and M. B. A. Oldstone. 1994. Virus-specific CD8+ cytotoxic T-lymphocyte activity associated with control of viremia in primary human immunodeficiency virus type 1 infection. J. Virol. 68:6103–6110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carrington, M., G. W. Nelson, M. P. Martin, T. Kissner, D. Vlahov, J. J. Goedert, R. Kaslow, S. Buchbinder, K. Hoots, and S. J. O’Brien. 1999. HLA and HIV-1: heterozygote advantage and B*35-Cw*04 disadvantage. Science 283:1748–1752. [DOI] [PubMed] [Google Scholar]
- 10.Clements-Mann, M. L., K. Weinhold, T. J. Matthews, B. S. Graham, G. J. Gorse, M. C. Keefer, M. J. McElrath, R.-H. Hsieh, J. Mestecky, S. Zolla-Pazner, J. Mascola, D. Schwartz, R. Siliciano, L. Corey, P. F. Wright, R. Belshe, R. Dolin, S. Jackson, S. Xu, P. Fast, M. C. Walker, D. Stablein, J.-L. Excler, J. Tartaglia, A.-M. Duliege, F. Sinangil, and E. Paoletti. 1998. Immune responses to human immunodeficiency virus (HIV) type 1 induced by canarypox expressing HIV-1MN gp120, HIV-1SF2 recombinant gp120, or both vaccines in seronegative adults. NIAID AIDS Vaccine Evaluation Group. J. Infect. Dis. 177:1230–1246. [DOI] [PubMed] [Google Scholar]
- 11.Egan, M. A., W. A. Pavlat, J. Tartaglia, E. Paoletti, K. J. Weinhold, M. L. Clements, and R. F. Siliciano. 1995. Induction of human immunodeficiency virus type 1 (HIV-1)-specific cytolytic T lymphocyte responses in seronegative adults by a nonreplicating, host-range-restricted canarypox vector (ALVAC) carrying the HIV-1MN env gene. J. Infect. Dis. 171:1623–1627. [DOI] [PubMed] [Google Scholar]
- 12.Evans, T. G., M. C. Keefer, K. J. Weinhold, M. Wolff, D. Montefiori, G. J. Gorse, B. S. Graham, M. J. McElrath, M. L. Clements-Mann, M. J. Mulligan, P. Fast, M. C. Walker, J. L. Excler, A. M. Duliege, and J. Tartaglia. 1999. A canarypox vaccine expressing multiple human immunodeficiency virus type 1 genes given alone or with rgp120 elicits broad and durable CD8+ cytotoxic T lymphocyte responses in seronegative volunteers. J. Infect. Dis. 180:290–298. [DOI] [PubMed] [Google Scholar]
- 13.Ferrari, G., W. Humphrey, M. J. McElrath, J. L. Excler, A. M. Duliege, M. L. Clements, L. C. Co, D. P. Bolognesi, and K. J. Weinhold. 1997. Clade B-based HIV-1 vaccines elicit cross-clade cytotoxic T lymphocyte reactivities in uninfected volunteers. Proc. Natl. Acad. Sci. USA 94:1396–1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Franchini, G., C. Gurgo, H. G. Guo, R. C. Gallo, E. Collalti, K. A. Fargnoli, L. F. Hall, F. Wong-Staal, and M. S. Reitz, Jr. 1987. Sequence of simian immunodeficiency virus and its relationship to the human immunodeficiency viruses. Nature 328:539–543. [DOI] [PubMed] [Google Scholar]
- 15.Franchini, G., M. Robert-Guroff, J. Tartaglia, A. Aggarwal, A. G. Abimiku, J. Benson, P. D. Markham, K. Limbach, G. Hurteau, J. Fullen, K. Aldrich, N. Miller, J. Sadoff, E. Paoletti, and R. C. Gallo. 1995. Highly attenuated HIV type 2 recombinant poxviruses, but not HIV-2 recombinant Salmonella vaccines, induce long-lasting protection in rhesus macaques. AIDS Res. Hum. Retrovir. 11:909–920. [DOI] [PubMed] [Google Scholar]
- 16.Fries, L. F., J. Tartaglia, J. Taylor, E. K. Kauffman, B. Meignier, E. Paoletti, and S. Plotkin. 1996. Human safety and immunogenicity of a canarypox-rabies glycoprotein recombinant vaccine: an alternative poxvirus vector system. Vaccine 14:428–434. [DOI] [PubMed] [Google Scholar]
- 17.Hanke, T., R. V. Samuel, T. J. Blanchard, V. C. Neumann, T. M. Allen, J. E. Boyson, S. A. Sharpe, N. Cook, G. L. Smith, D. I. Watkins, M. P. Cranage, and A. J. McMichael. 1999. Effective induction of simian immunodeficiency virus-specific cytotoxic T lymphocytes in macaques by using a multiepitope gene and DNA prime-modified vaccinia virus Ankara boost vaccination regimen. J. Virol. 73:7524–7532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hel, Z., D. Venzon, M. Poudyal, W.-P. Tsai, L. Giuliani, R. Woodward, C. Chougnet, G. M. Shearer, J. D. Altman, D. I. Watkins, N. Bischofberger, A. G. Abimiku, P. D. Markham, J. Tartaglia, and G. Franchini. 2000. Viremia control following antiretroviral treatment and therapeutic immunization during primary SIV251 infection of macaques. Nat. Med. 6:1140–1146. [DOI] [PubMed] [Google Scholar]
- 19.Hel, Z., J. Nacsa, B. Kelsall, W.-P. Tsai, N. Letvin, R. W. Parks, E. Tryniszewska, L. Picker, M. G. Lewis, Y. Edghill-Smith, M. Moniuszko, R. Pal, L. Stevceva, J. D. Altman, T. M. Allen, D. I. Watkins, J. V. Torres, J. A. Berzovsky, I. M. Belyakov, W. Strober, and G. Franchini. 2001. Impairment of Gag-specific CD8+ T-cell function in mucosal and systemic compartments of simian immunodeficiency virus mac251- and simian-human immunodeficiency virus KU2-infected macaques. J. Virol. 75:11483–11495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hodge, S., J. de Rosayro, A. Glenn, I. C. Ojukwu, S. Dewhurst, H. M. McClure, N. Bischofberger, D. C. Anderson, S. A. Klumpp, and F. J. Novembre. 1999. Postinoculation PMPA treatment, but not preinoculation immunomodulatory therapy, protects against development of acute disease induced by the unique simian immunodeficiency virus SIVsmmPBj. J. Virol. 73:8630–8639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hu, S. L., K. Abrams, G. N. Barber, P. Moran, J. M. Zarling, A. J. Langlois, L. Kuller, W. R. Morton, and R. E. Benveniste. 1992. Protection of macaques against SIV infection by subunit vaccines of SIV envelope glycoprotein gp160. Science 255:456–459. [DOI] [PubMed] [Google Scholar]
- 22.Jin, X., D. E. Bauer, S. E. Tuttleton, S. Lewin, A. Gettie, J. Blanchard, C. E. Irwin, J. T. Safrit, J. Mittler, L. Weinberger, L. G. Kostrikis, L. Zhang, A. S. Perelson, and D. D. Ho. 1999. Dramatic rise in plasma viremia after CD8+ T cell depletion in simian immunodeficiency virus-infected macaques. J. Exp. Med. 189:991–998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Joag, S. V., Z. Li, C. Wang, F. Jia, L. Foresman, I. Adany, D. M. Pinson, E. B. Stephens, and O. Narayan. 1998. Chimeric SHIV that causes CD4+ T cell loss and AIDS in rhesus macaques. J. Med. Primatol. 27:59–64. [DOI] [PubMed] [Google Scholar]
- 24.Kallas, E. G., D. C. Gibbons, H. Soucier, T. Fitzgerald, J. J. Treanor, and T. G. Evans. 1999. Detection of intracellular antigen-specific cytokines in human T cell populations. J. Infect. Dis. 179:1124–1131. [DOI] [PubMed] [Google Scholar]
- 25.Kalyanaraman, V. S., V. Rodriguez, F. Veronese, R. Rahman, P. Lusso, A. L. DeVico, T. Copeland, S. Oroszlan, R. C. Gallo, and M. G. Sarngadharan. 1990. Characterization of the secreted, native gp120 and gp160 of the human immunodeficiency virus type 1. AIDS Res. Hum. Retrovir. 6:371–380. [DOI] [PubMed] [Google Scholar]
- 26.Kaslow, R. A., R. Duquesnoy, M. VanRaden, L. Kingsley, M. Marrari, H. Friedman, S. Su, A. J. Saah, R. Detels, J. Phair, and C. Rinaldo. 1990. A1, Cw7, B8, DR3 HLA antigen combination associated with rapid decline of T-helper lymphocytes in HIV-1 infection. A report from the Multicenter AIDS Cohort Study. Lancet 335:927–930. [DOI] [PubMed] [Google Scholar]
- 27.Koup, R. A., J. T. Safrit, Y. Cao, C. A. Andrew, G. McLeod, W. Borkowsky, C. Farthing, and D. D. Ho. 1994. Temporal association of cellular immune responses with the initial control of viremia in primary human immunodeficiency virus type 1 syndrome. J. Virol. 68:4650–4655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kuroda, M. J., J. E. Schmitz, D. H. Barouch, A. Craiu, T. M. Allen, A. Sette, D. I. Watkins, M. A. Forman, and N. L. Letvin. 1998. Analysis of Gag-specific cytotoxic T lymphocytes in simian immunodeficiency virus-infected rhesus monkeys by cell staining with a tetrameric major histocompatibility complex class I-peptide complex. J. Exp. Med. 187:1373–1381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kuroda, M. J., J. E. Schmitz, W. A. Charini, C. E. Nickerson, M. A. Lifton, C. I. Lord, M. A. Forman, and N. L. Letvin. 1999. Emergence of CTL coincides with clearance of virus during primary simian immunodeficiency virus infection in rhesus monkeys. J. Immunol. 162:5127–5133. [PubMed] [Google Scholar]
- 30.Kuroda, M. J., J. E. Schmitz, W. A. Charini, C. E. Nickerson, C. I. Lord, M. A. Forman, and N. L. Letvin. 1999. Comparative analysis of cytotoxic T lymphocytes in lymph nodes and peripheral blood of simian immunodeficiency virus-infected rhesus monkeys. J. Virol. 73:1573–1579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Langlois, A. J., R. C. Desrosiers, M. G. Lewis, V. N. KewalRamani, D. R. Littman, J. Y. Zhou, K. Manson, M. S. Wyand, D. P. Bolognesi, and D. C. Montefiori. 1998. Neutralizing antibodies in sera from macaques immunized with attenuated simian immunodeficiency virus. J. Virol. 72:6950–6955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lifson, J. D., J. L. Rossio, R. Arnaout, L. Li, T. L. Parks, D. K. Schneider, R. F. Kiser, V. J. Coalter, G. Walsh, R. J. Imming, B. Fisher, B. M. Flynn, N. Bischofberger, M. J. Piatak, V. M. Hirsch, M. A. Nowak, and D. Wodarz. 2000. Containment of simian immunodeficiency virus infection: cellular immune responses and protection from rechallenge following transient postinoculation antiretroviral treatment. J. Virol. 74:2584–2593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lori, F., M. G. Lewis, J. Xu, G. Varga, D. E. J. Zinn, C. Crabbs, W. Wagner, J. Greenhouse, P. Silvera, J. Yalley-Ogunro, C. Tinelli, and J. Lisziewicz. 2000. Control of SIV rebound through structured treatment interruptions during early infection. Science 290:1591–1593. [DOI] [PubMed] [Google Scholar]
- 34.Mascola, J. R., G. Stiegler, T. C. Vancott, H. Katinger, C. B. Carpenter, C. E. Hanson, H. Beary, D. Hayes, S. S. Frankel, D. L. Birx, and M. G. Lewis. 2000. Protection of macaques against vaginal transmission of a pathogenic HIV-1/SIV chimeric virus by passive infusion of neutralizing antibodies. Nat. Med. 6:207–210. [DOI] [PubMed] [Google Scholar]
- 35.Matano, T., R. Shibata, C. Siemon, M. Connors, H. Lane, and M. A. Martin. 1998. Administration of an anti-CD8 monoclonal antibody interferes with the clearance of chimeric simian/human immunodeficiency virus during primary infections of rhesus macaques. J. Virol. 72:164–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McNeil, A. J., P. L. Yap, S. M. Gore, R. P. Brettle, M. McColl, R. Wyld, S. Davidson, R. Weightman, A. M. Richardson, and J. R. Robertson. 1996. Association of HLA types A1–B8-DR3 and B27 with rapid and slow progression of HIV disease. Q. J. Med. 89:177–185. [DOI] [PubMed] [Google Scholar]
- 37.Migueles, S. A., M. S. Sabbaghian, W. L. Shupert, M. P. Bettinotti, F. M. Marincola, L. Martino, C. W. Hallahan, S. M. Selig, D. Schwartz, J. Sullivan, and M. Connors. 2000. HLA B*5701 is highly associated with restriction of virus replication in a subgroup of HIV-infected long term nonprogressors. Proc. Natl. Acad. Sci. USA 97:2709–2714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Montefiori, D. C., T. W. Baba, A. Li, A. Bilska, and R. M. Ruprecht. 1996. Neutralizing and infection-enhancing antibody responses do not correlate with the differential pathogenicity of SIVmac239delta3 in adult and infant rhesus monkeys. J. Immunol. 157:5528–5535. [PubMed] [Google Scholar]
- 39.Mori, K., Y. Yasutomi, S. Sawada, F. Villinger, K. Sugama, B. Rosenwith, J. L. Heeney, K. Uberla, S. Yamazaki, A. A. Ansari, and H. Rubsamen-Waigmann. 2000. Suppression of acute viremia by short-term postexposure prophylaxis of simian/human immunodeficiency virus SHIV-RT-infected monkeys with a novel reverse transcriptase inhibitor (GW420867) allows for development of potent antiviral immune responses resulting in efficient containment of infection. J. Virol. 74:5747–5753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nixon, D. F., A. R. M. Townsend, J. G. Elvin, C. R. Rizza, J. Gallwey, and A. J. McMichael. 1988. HIV-1 Gag-specific cytotoxic T lymphocytes defined with recombinant vaccinia virus and synthetic peptides. Nature 336:484–487. [DOI] [PubMed] [Google Scholar]
- 41.Ourmanov, I., C. R. Brown, B. Moss, M. Carroll, L. Wyatt, L. Pletneva, S. Goldstein, D. Venzon, and V. M. Hirsch. 2000. Comparative efficacy of recombinant modified vaccinia virus Ankara expressing simian immunodeficiency virus (SIV) Gag-Pol and/or Env in macaques challenged with pathogenic SIV. J. Virol. 74:2740–2751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pantaleo, G., J. F. Demarest, H. Soudeyns, C. Graziosi, F. Denis, J. W. Adelsberger, P. Borrow, M. S. Saag, G. M. Shaw, and R. P. Sekaly. 1994. Major expansion of CD8+ T cells with a predominant V beta usage during the primary immune response to HIV. Nature 370:463–467. [DOI] [PubMed] [Google Scholar]
- 43.Perkus, M. E., E. B. Kauffman, J. Taylor, S. Mercer, D. Smith, J. VanderHoeven, and E. Paoletti. 1993. Methodology of using vaccinia virus to express foreign genes in tissue culture. J. Tissue Cult. Methods 15:72–81. [Google Scholar]
- 44.Perkus, M. E., J. Tartaglia, and E. Paoletti. 1995. Poxvirus-based vaccine candidates for cancer, AIDS, and other infectious diseases. J. Leukoc. Biol. 58:1–13. [DOI] [PubMed] [Google Scholar]
- 45.Pialoux, G., J. L. Excler, Y. Riviere, G. Gonzalez-Canali, V. Feuillie, P. Coulaud, J. C. Gluckman, T. J. Matthews, B. Meignier, and M. P. Kieny. 1995. A prime-boost approach to HIV preventive vaccine using a recombinant canarypox virus expressing glycoprotein 160 (MN) followed by a recombinant glycoprotein 160 (MN/LAI). The AGIS Group, and l’Agence Nationale de Recherche sur le SIDA. AIDS Res. Hum. Retrovir. 11:373–381. [DOI] [PubMed] [Google Scholar]
- 46.Quinn, T. C., M. J. Wawer, N. Sewankambo, D. Serwadda, C. Li, F. Wabwire-Mangen, M. O. Meehan, T. Lutalo, and R. H. Gray. 2000. Viral load and heterosexual transmission of human immunodeficiency virus type 1. Rakai Project Study Group. N. Engl. J. Med. 342:921–929. [DOI] [PubMed] [Google Scholar]
- 47.Rinaldo, C., X.-L. Huang, Z. Fan, M. Ding, L. Beltz, A. Logar, D. Panicali, G. Mazzarra, J. Liebmann, M. Cottrill, and P. Gupta. 1995. High levels of anti-human immunodeficiency virus type 1 (HIV-1) memory cytotoxic T-lymphocyte activity and low viral load are associated with lack of disease in HIV-1-infected long-term nonprogressors. J. Virol. 69:5838–5842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Romano, J. W., R. N. Shurtliff, E. Dobratz, A. Gibson, K. Hickman, P. Markham, and R. Pal. 2000. Quantitative evaluation of simian immunodeficiency virus infection using NASBA technology. J. Virol. Methods 86:61–70. [DOI] [PubMed] [Google Scholar]
- 49.Rosenberg, E. S., M. Altfeld, S. H. Poon, M. N. Phillips, B. M. Wilkes, R. L. Eldridge, G. K. Robbins, R.T. D’Aquila, P. J. Goulder, and B. D. Walker. 2000. Immune control of HIV-1 after early treatment of acute infection. Nature 407:523–526. [DOI] [PubMed] [Google Scholar]
- 50.Royce, R. A., A. Sena, W. Cates, Jr., and M. S. Cohen. 1997. Sexual transmission of HIV. N. Engl. J. Med. 336:1072–1078. [DOI] [PubMed] [Google Scholar]
- 51.Salmon-Ceron, D., J. L. Excler, L. Finkielsztejn, B. Autran, J. C. Gluckman, D. Sicard, T. J. Matthews, B. Meignier, C. Valentin, R. El Habib, C. Blondeau, M. Raux, C. Moog, J. Tartaglia, P. Chong, M. Klein, B. Milcamps, F. Heshmati, and S. Plotkin. 1999. Safety and immunogenicity of a live recombinant canarypox virus expressing HIV type 1 gp120 MN MN tm/gag/protease LAI (ALVAC-HIV, vCP205) followed by a p24E-V3 MN synthetic peptide (CLTB-36) administered in healthy volunteers at low risk for HIV infection. AGIS Group and L’Agence Nationale de Recherches sur le Sida. AIDS Res. Hum. Retrovir. 15:633–645. [DOI] [PubMed] [Google Scholar]
- 52.Schmitz, J. E., M. J. Kuroda, S. Santra, V. G. Sasseville, S. A. Simon, M. A. Lifton, P. Racz, K. Tenner-Racz, M. Dalesandro, B. J. Scallon, J. Ghrayeb, M. A. Forman, D. Montefiori, E. P. Rieber, N. L. Letvin, and K. A. Reimann. 1999. Control of viremia in simian immunodeficiency virus infection by CD8+ lymphocytes. Science 283:857–860. [DOI] [PubMed] [Google Scholar]
- 53.Seth, A., I. Ourmanov, M. J. Kuroda, J. E. Schmitz, M. W. Carroll, L. S. Wyatt, B. Moss, M. A. Forman, V. M. Hirsch, and N. L. Letvin. 1998. Recombinant modified vaccinia virus Ankara-simian immunodeficiency virus gag pol elicits cytotoxic T lymphocytes in rhesus monkeys detected by a major histocompatibility complex class I/peptide tetramer. Proc. Natl. Acad. Sci. USA 95:10112–10116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Seth, A., I. Ourmanov, J. E. Schmitz, M. J. Kuroda, M. A. Lifton, C. E. Nickerson, L. Wyatt, M. Carroll, B. Moss, D. Venzon, N. L. Letvin, and V. M. Hirsch. 2000. Immunization with a modified vaccinia virus expressing simian immunodeficiency virus (SIV) Gag-Pol primes for an anamnestic Gag-specific cytotoxic T-lymphocyte response and is associated with reduction of viremia after SIV challenge. J. Virol. 74:2502–2509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Spring, M., C. Stahl-Hennig, N. Stolte, N. Bischofberger, J. Heeney, P. ten Haaft, K. Tenner-Racz, P. Racz, D. Lorenzen, G. Hunsmann, and U. Dittmer. 2001. Enhanced cellular immune response and reduced CD8(+) lymphocyte apoptosis in acutely SIV-infected Rhesus macaques after short-term antiretroviral treatment. Virology 279:221–232. [DOI] [PubMed] [Google Scholar]
- 56.Steel, C. M., C. A. Ludlam, D. Beatson, J. F. Peutherer, R. J. Cuthbert, P. Simmonds, H. Morrison, and M. Jones. 1988. HLA haplotype A1 B8 DR3 as a risk factor for HIV-related disease. Lancet i:1185–1188 [DOI] [PubMed] [Google Scholar]