Abstract
Objective:
To study findings at autopsy in patients with fatal acute thromboembolic occlusion of the superior mesenteric artery (SMA).
Summary Background Data:
Acute occlusion of the SMA is difficult to diagnose and mortality remains high. In Malmö, Sweden, the autopsy rate between 1970 and 1982 was 87%, creating possibilities for a population-based study.
Methods:
Among 23,496 clinical autopsies and 7569 forensic autopsies, 213 cases with acute thromboembolic occlusion of the SMA and intestinal infarction were identified.
Results:
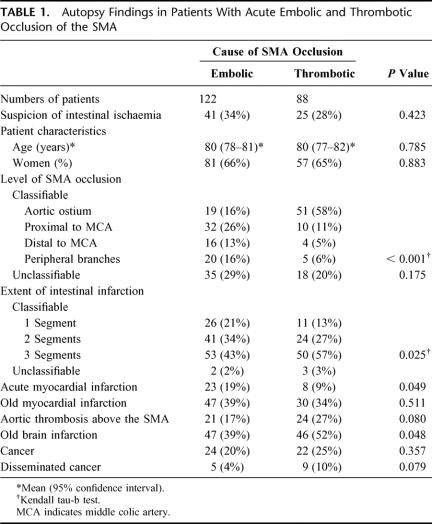
A clinical suspicion of intestinal infarction was documented in 32% of the patients, only 35% being in the care of surgeons. The embolus/thrombus ratio was 1.4 to 1. Thrombotic occlusions were located more proximally than embolic occlusions (P < 0.001), intestinal infarction was more extensive (P = 0.025) and thrombotic occlusions were associated with old brain infarction (P = 0.048), aortic wall thrombosis (P = 0.080), and disseminated cancer (P = 0.079). Patients with embolic occlusions (n = 122) had a higher frequency of acute myocardial infarction (AMI) than patients with thrombotic occlusions (P = 0.049). The embolic source was identified in 80%. In 115 (94%), synchronous embolism and/or source of embolus were present. There were findings of remaining cardiac thrombi in 58 (48%) and synchronous emboli affected 273 other arterial segments in 83 (68%).
Conclusions:
Early recognition and revascularization would have been a prerequisite for survival in at least half of the patients, since the jejunum, ileum, and colon were affected by infarction. A minority of all patients were under surgical care. AMI, cardiac thrombi, and synchronous emboli were common findings among patients with embolic occlusions.
Patients with autopsy-verified acute thromboembolic occlusion of the superior mesenteric artery were treated in nonsurgical departments in two thirds of the cases. Forty-nine percent had either concomitant AMI, ischemic stroke, or synchronous emboli. Embolus/thrombus ratio was 1.4 to 1. Thrombosis was associated with proximal occlusions and more extensive intestinal infarction.
Up to 1950, diagnosis of acute thromboembolic occlusion of the superior mesenteric artery (SMA) was considered to be early if it was made before the patient became moribund, allowing laparotomy, resection of the infarcted bowel, and possible survival.1 Progress in surgical2 and angiographic3 technique has followed, but outcome remains poor.4 Factors such as diagnostic difficulties at presentation and infrequent recognition prior to intestinal infarction5 have been held partly responsible for the continued poor prognosis. Even in a prospective study designed to identify cases with acute SMA occlusion, the diagnosis was often either established at a point of time when the intestinal infarction had reached an extension inaccessible for surgical therapy, or overlooked before death.6
Contemporary clinical series have stated that the disease is uncommon,7,8 despite the lack of supportive data. The impact of thorough autopsy studies on incidence has not been acknowledged. The paramount importance of a high autopsy rate in estimating the incidence of the disease was demonstrated in a population-based study, where we found that the diagnosis were suspected prior to death in only 39 out of 176 patients (22%) managed nonoperatively.9 In the studied population, the incidence was found to be even higher than that of ruptured abdominal aortic aneurysm10: 8.6 and 5.6 per 100,000 person years, respectively.
The Department of Pathology at Malmö General Hospital, Sweden, has a longstanding research commitment to vascular diseases and has been the central institute in epidemiologic studies of atherosclerosis supported by both WHO and by International Society of Federation of Cardiology.11–13 Between 1970 and 1982, 31,034 consecutive autopsies, composing an autopsy rate of 87%, were performed. Since then, changes in legislation and in public attitudes towards postmortem examinations have led to a decrease in autopsy rate, particularly among octogenarians and beyond to less than 10% in Sweden (www.sos.se/), which would make a contemporary study impossible to conduct.
The aims of the present autopsy study were to determine the nature of the thromboembolic occlusion, to elucidate the presence of concomitant thromboembolic disorders, and to identify determinants associated with severity of intestinal infarction in 213 patients with fatal acute thromboembolic occlusion of the SMA.
MATERIALS AND METHODS
Study Population
Between 1970 and 1982 the population of Malmö declined from 264,000 to 230,000 (Swedish Central Bureau of Statistics). During the study period, 35,784 deaths occurred among the Malmö population (Malmö Statistical Year Books, 1970–1982). In all, 23,446 clinical autopsies and 7588 forensic autopsies were performed, resulting in an 87% autopsy rate. Only patients where the acute thromboembolic occlusion of the SMA resulted in a transmural infarction of the intestine were included in this study.
Retrieval of Autopsy-Verified Cases
Clinical Autopsies
Among 23,496 clinical autopsies, 997 cases were either coded for (1) necrosis in the duodenum, small intestine, colon or rectum; and/or (2) thromboembolism in a visceral artery, and/or (3) mesenteric vessel occlusion/bowel infarction as the cause of death. The autopsy protocols from all these 997 cases were identified and analyzed.
All clinical autopsies were performed at the Department of Pathology, Malmö General Hospital, using a standardized detailed protocol. Findings were coded according to the Systematized Nomenclature of Pathology code, as defined by the College of American Pathologists in 1965. There was a standardized intraluminal exposure of all major arteries originating from the aorta, including the carotid and subclavian arteries and down to the division of the common femoral arteries. During the standardized examination of the SMA, the bowel package was divided from the great mesenteric vessels at the mesenteric root, leaving the greater part of the mesentery attached to the bowels. SMA was then cut open from its aortic origin and checked for intraluminal thrombus or embolus. Distal branches in the mesentery were also examined, especially if a short segment of the intestine showed signs of ischemia. The whole length of the intestines was cut open and checked for macroscopical necrosis. Microscopic examinations of the intestinal wall were performed liberally. Each site of embolic infarction of the cerebral hemispheres corresponded to embolism of a major artery, either anterior, middle, or posterior cerebral artery. Operation for embolism to the legs and arms within 1 week prior to death was registered as a synchronous embolic event.
Patients with intestinal infarction and nonocclusive mesenteric ischemia (n = 50) or mesenteric venous thrombosis (31) or indeterminate cause of arterial mesenteric ischemia (6) were excluded from the study.
Classification of Thrombosis and Embolism in the SMA
In the differentiation between thrombotic and embolic occlusions, the pathologist's description and conclusion were of utmost importance. The presence of synchronous embolism was a clear-cut finding of embolic occlusion. The findings of heart thrombi strongly supported an embolic occlusion. The characteristics of SMA, such as extension and location of atherosclerotic lesions, the appearance of single or multiple occluding clots, the level of occlusion, and the presence of clot adhesion to the intraluminal wall gave supportive information.
In the majority of cases, the extent and level of detail of information provided a clear picture whether thrombosis or embolism was the cause of occlusion. However, in 31 out of 213 patients (15%), the situation was less clear, and these autopsy protocols were validated separately by 2 experienced vascular surgeons (MB and DB) to reach a consensus. In 3 cases, it was not possible to elucidate the nature of the occluding lesion, and these cases were labeled as indeterminate.
Forensic Autopsies
According to the Swedish legislation, forensic autopsy was mandatory when death occurred outside of hospitals. During the years 1970 to 1982, 7588 cases from Malmö were referred to the Institution of Forensic Medicine in Lund. In all, 7569 (99.8%) case records were found and reviewed. Patients with intestinal infarction and nonocclusive mesenteric ischemia (n = 2), or mesenteric venous thrombosis (4) or indeterminate cause of arterial mesenteric ischemia (1) were excluded from the study.
Ethics
This study was approved by the Research Ethics Committee of the University of Lund.
Statistical Methods
Differences in proportions were evaluated using the χ2 test for nominal variables and Kendall tau-b test for ordinal variables. Distributions were expressed in terms of mean and standard deviation. Student t test was used to evaluate differences in mean age and the Mann-Whitney U test to evaluate differences in number of synchronous emboli between 2 groups of patients with cardiac thrombi.
RESULTS
Characteristics of the Patients
At clinical and forensic autopsies, 211 and 2 patients, respectively, were diagnosed with acute thromboembolic occlusion of the SMA and intestinal infarction. In the referral note for autopsy, a suspicion of intestinal ischemia was noted in 39 (22%) among the 176 patients managed nonoperatively and 30 (81%) among the 37 patients who underwent abdominal surgery and subsequent autopsy. Thus, in total, there was a documented suspicion of intestinal ischemia prior to death in 69 (32%) of the 213 cases. Apart from laparotomy, 10 limb embolectomies and 7 lower-limb amputations were undertaken within 1 week before death. The patients died in various ward units: geriatric (77/213; 36%), surgery (74; 35%), internal medicine (47; 22%), infectious diseases (6; 3%), oncology (5; 2%), and orthopedics (2; 1%). Two patients (1%) died outside of hospital. The patients at surgery wards had a mean age of 85 years, compared with 77 years in patients at both geriatric and internal medicine wards, respectively (P < 0.001), but there were no difference in distribution between men and women at these wards (P = 0.110).
Thrombosis Versus Embolism in the SMA
The cause of occlusion was embolism in 122 (57.3%), thrombosis in 88 (41.3%), and indeterminate in 3 (1.4%) (Table 1). Thrombotic occlusions were often located more proximal than embolic occlusions (P < 0.001). Synchronous emboli were found in 83 cases and were only found in those cases with embolic occlusion (68%). There were findings of cardiac thrombi in 58 patients with embolic occlusion (48%) compared with 10 patients with thrombotic occlusion (11%). Atrial fibrillation was documented in 49 patients with embolism (40%) and in 14 patients with thrombosis (16%). Adhesion of clot to the intraluminal wall was documented in 73 patients with thrombotic occlusion (83%) and in 47 patients with embolic occlusion (39%). The clots were “slightly” or “partially” adhesive to the intraluminal wall in 15 out of these 47 cases with embolic occlusion (32%). Microscopic examination of the occlusive lesion was undertaken in 14 patients with thrombotic occlusion (16%) and in 21 patients with embolic occlusion (17%). Chronic mesenteric ischemia was documented in 8 patients by disease history (n = 4) and arteriography (2) in the referral note and intestinal histology (2) in the autopsy protocol and was found in 7 patients with thrombotic (8%) and in 1 patient with indeterminate occlusion. In cases with thrombosis of the SMA, there were also thrombosis or severe atherosclerotic changes of the celiac trunk, right and left renal artery, in 33%, 11%, and 14%, respectively.
TABLE 1. Autopsy Findings in Patients With Acute Embolic and Thrombotic Occlusion of the SMA
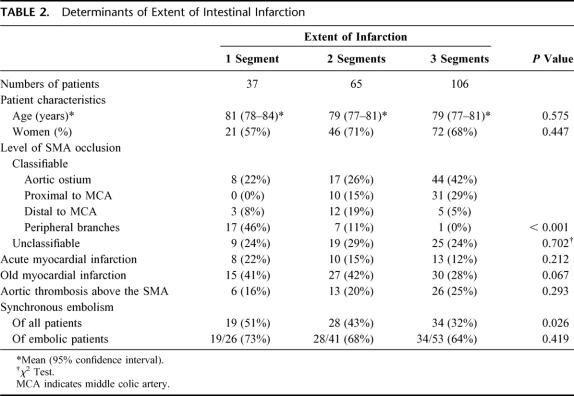
Determinants of Extent of Intestinal Infarction
The intestinal infarction affected jejunum, ileum, and colon in 158 (76%), 200 (96%), and 127 (61%) of the 208 classifiable cases, respectively (Fig. 1). At least 2 of these intestinal segments were infarcted in 82% of the cases. All 3 intestinal segments were infarcted in 50%. The intestinal infarction was more extensive in patients with thrombotic, compared with embolic, occlusions (P = 0.025) (Table 1). In patients with acute myocardial infarction (AMI), there was less extensive intestinal infarction than in patients without AMI. There was no association between age or synchronous emboli and extent of intestinal infarction (Table 2).
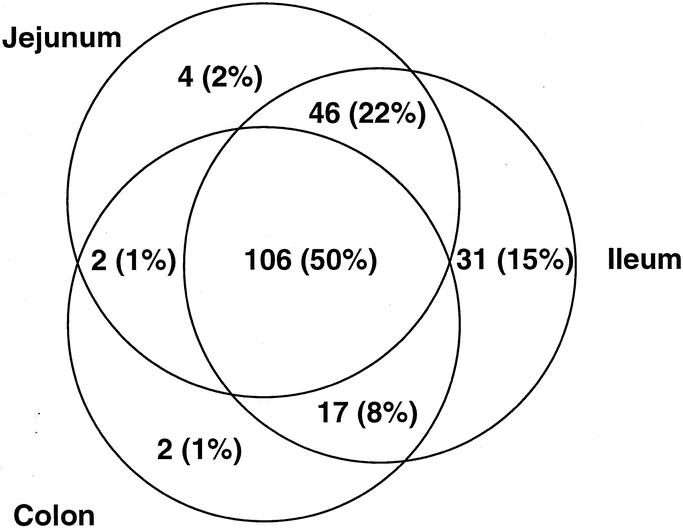
FIGURE 1. Extent of intestinal infarction in 208 patients with acute thromboembolic occlusion of the SMA.
TABLE 2. Determinants of Extent of Intestinal Infarction
Sources of Emboli
Among the 122 patients with embolus to the SMA, 86 (70%) had at least 1 of the following signs of a cardiac source: intracardiac thrombi (n = 58), AMI (23), or documented atrial fibrillation (49) in the referral note. The intracardiac thrombi were located in the auricle of the left atrium (n = 32), left atrium (9), foramen ovale (1), mitral valve (4), left ventricle (20), and aortic valve (1). In 6 patients, thrombi were found in at least 2 of these locations.
Paradoxic embolism was probable in 5 out of 8 cases with a patent foramen ovale, combined with venous thromboembolism and signs of pulmonary hypertension with a potential right-to-left intraatrial shunt.
Twenty-one (17%) of the 122 patients with embolus to the SMA had thrombosis of the aortic wall proximal to the origin of the SMA. In 6 of these patients, aortic thrombus was considered the probable source of embolus.
In all, it was possible to identify a probable source of the embolus in 80% of the patients with embolic occlusion.
Concurrent Acute Thromboembolic Diseases
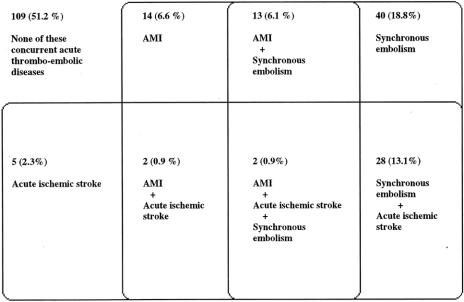
The concurrent presence of AMI, acute ischemic stroke, and synchronous embolism in the study patients is shown in Figure 2.
FIGURE 2. Concurrent acute thromboembolic disease. Occurrence of acute myocardial infarction (AMI), ischemic stroke, and synchronous embolism in 213 patients with acute thromboembolic occlusion of the SMA.
Apart from the SMA thromboembolism, there were 104 cases (49%) with at least 1 additional acute thromboembolic disease.
Synchronous Embolism
In 83 (68%) out of 122 patients, synchronous embolism was present, affecting a total of 273 other arterial segments than the SMA (Table 3). Up to 14 synchronous emboli were found, 29, 20, and 9 patients having synchronous emboli in 1, 2 and 3 arteries, respectively (Fig. 3). Hence, 2 or more synchronous emboli occurred in 54 patients (44%). No difference in the number of synchronous emboli was found between patients with atrial thrombi (n = 42) and the group with ventricular thrombi (n = 20) (P = 0.502).
TABLE 3. Anatomical Localization of 273 Synchronous Emboli in 83 Patients With Embolus to the SMA
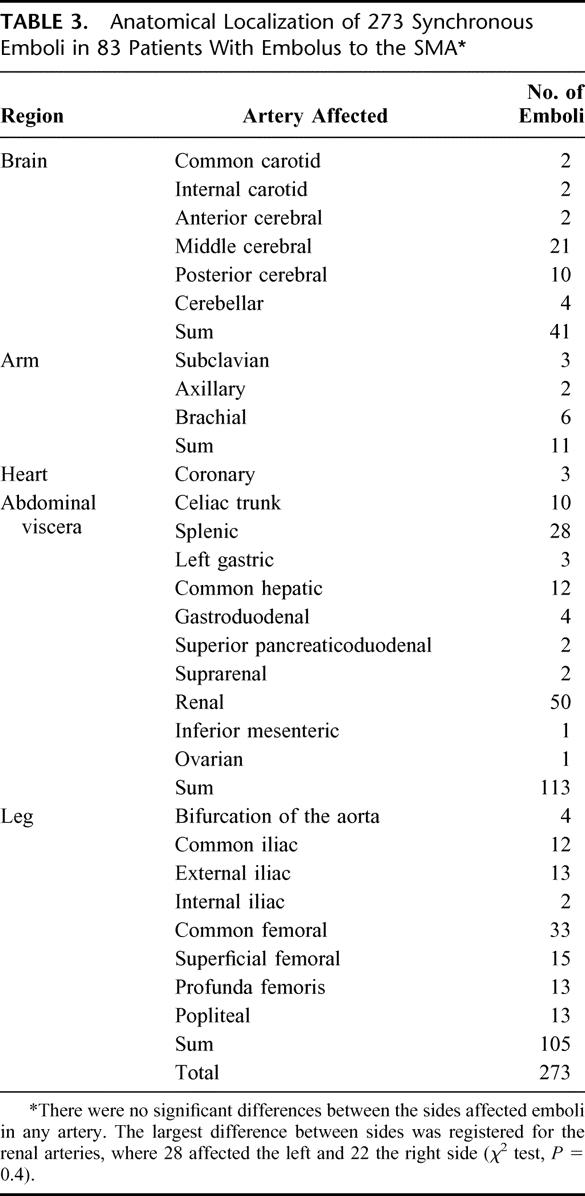
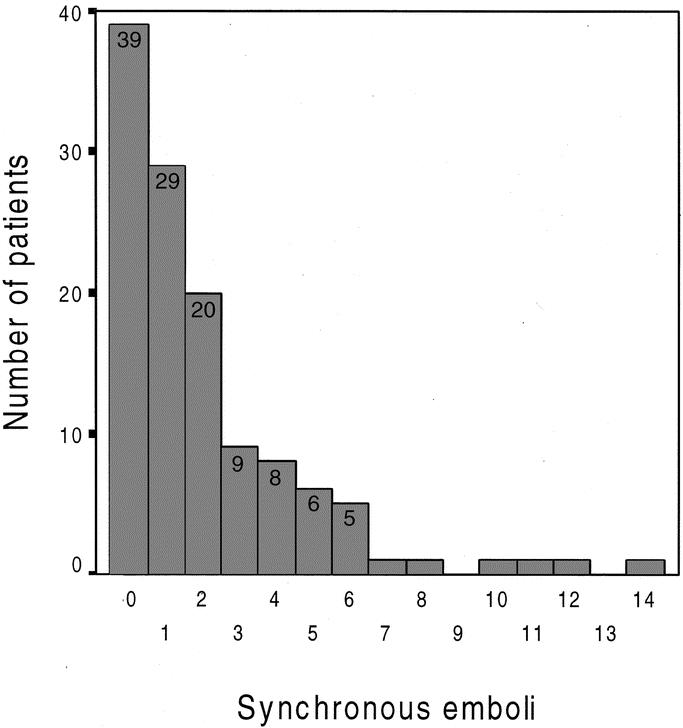
FIGURE 3. Number of synchronous emboli among 122 patients with an embolus to the SMA.
In all, there were objective signs of embolic disease, ie, source of emboli and/or synchronous embolism, in 115 (94%) of the 122 patients with embolic occlusion of the SMA.
DISCUSSION
It is well known that this disease often affects elderly patients with ischemic heart disease and atrial fibrillation. The present study has identified 3 other factors, however, that may contribute to a poor outcome. First, two thirds of the patients were managed in nonsurgery wards, where the probability of an early diagnosis is less likely.6,8,14 The patients were not selected to nonsurgical wards because of their age; on the contrary, patients treated in surgical wards were older. Second, the occlusion was often located proximally, even in embolic disease, resulting in extensive intestinal infarction. Early revascularization and collaboration with vascular surgeons then becomes a prerequisite of survival15 in the majority of these elderly patients. Third, the high frequency of multiple embolism is another important factor contributing to the poor outcome. This observation is not novel,3,4,6 but due to the study design of the present investigation, the extent of multiple embolism has never previously been demonstrated in such detail and extent. These identified factors may be responsible for the unchanged high mortality, 80% to 90%, reported in contemporary investigations, despite advances in radiologic and surgical technique, anesthesia, and intensive care.8,16
The etiology of occlusion, expressed as the embolus/thrombus ratio, varies in clinical series. In this study, embolic occlusions predominated, and the ratio was 1.4 to 1. Other investigators who reported a predominance of thrombotic occlusions had a high proportion of patients with chronic mesenteric ischemia.4,7,17 In contrast, embolic occlusions may dominate in series where chronic mesenteric ischemia is absent and/or where there is a high frequency of atrial fibrillation among the patients.6 The standardized procedure of intraluminal exposure of the SMA in this study ensured the verification of occlusive disease, and the meticulous autopsy technique made it possible to discriminate embolic from thrombotic occlusion in most cases. In spite of the presence of cardiac thrombi in 10 and atrial fibrillation in 14 cases, we found the occlusion to be thrombotic. Thus, this indicates that the classification of embolic occlusion based on atrial fibrillation or cardiac thrombi in clinical series will lead to an overestimation of cases with embolic occlusions. In 115 of the 122 cases with embolic occlusion, objective signs of embolic disease, such as synchronous embolism and/or source of embolus, were present. However, valid objective signs of thrombotic occlusion were more difficult to find: firm adhesion of clot to the intraluminal wall occurred more frequently in thrombotic than in embolic occlusions. Thus, we consider our finding that embolism dominated to be well founded. Obviously, populations may vary in this respect.
The extent of intestinal infarction was identified as a predictor of adverse outcome in previous studies,4,6,18–20 but neither age nor gender was a determinant for the extent of intestinal infarction in this study. Thus, old age should not solely deter the surgeon from surgery in a case with suspicion of intestinal ischemia. Acute thrombotic occlusions were often demonstrated to be localized proximally within the SMA, associated with a larger intestinal infarction, which also has been described in a paper mainly based on patients operated on.20 Clinical decision making in patients with AMI and suspicion of an acute embolic occlusion of the SMA may be difficult, but since there is a higher probability of a less-extensive intestinal infarction in these patients, curative surgical intent could be worthwhile.
The high frequency of remaining cardiac thrombi after embolic occlusion of the SMA emphasizes the importance of secondary prophylaxis with optimal antithrombotic treatment. Clinical implications are also attributed to the knowledge of the high proportion of proximal occlusions of the SMA. First, the occlusion may be detected by noninvasive imaging modalities with high resolution: contrast-enhanced 3-D magnetic resonance21 and multiple detector-row computed tomography (CT) angiography.22 Second, proximal occlusions are likely to be more accessible by vascular reconstructions than distal occlusions. It must be recognized, however, as was observed in a previous study on 60 patients undergoing acute SMA revascularization,15 that embolic occlusion cannot be excluded by examining only the proximal portion of the SMA with duplex or CT.
The fact that this study had to be conducted on patients who died 22 to 34 years ago raises relevant questions regarding the validity of our findings in a contemporary setting. We are only able to speculate whether changes in demography and pharmacology have altered the epidemiology, but the basic pathologic mechanisms are likely to be unchanged, which supports the validity of the main findings of our study. Moreover, there is no evidence that advances in radiologic imaging have resulted in earlier recognition and a different management of these patients.6
CONCLUSION
An interdisciplinary collaboration is important, since only a minority of the patients were in the care of surgeons. The thrombotic occlusions of the SMA were often located more proximally, and intestinal infarction was more extensive. AMI, cardiac thrombi, and synchronous emboli were common findings among patients with embolic occlusions, which have important clinical implications on diagnosis and management. Early recognition and revascularization would have been a prerequisite for survival in at least half of the patients, since the jejunum, ileum, and colon were affected by infarction.
Footnotes
Reprints: Stefan Acosta, MD, Department of Surgery, Blekinge County Hospital, Karlskrona SE 371 85, Karlskrona, Sweden. E-mail: stefan.acosta@telia.com.
REFERENCES
- 1.Boley SJ, Brandt LJ, Sammartano RJ. History of mesenteric ischemia. Surg Clin North Am. 1997;77:275–288. [DOI] [PubMed] [Google Scholar]
- 2.Klass AA. Embolectomy in acute mesenteric occlusion. Ann Surg. 1951;134:913–917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Batellier J, Kieny R. Superior mesenteric artery embolism: eighty-two cases. Ann Vasc Surg. 1990;4:112–116. [DOI] [PubMed] [Google Scholar]
- 4.Edwards M, Cherr G, Craven T, et al. Acute occlusive mesenteric ischaemia: surgical management and outcomes. Ann Vasc Surg. 2003;17:72–79. [DOI] [PubMed] [Google Scholar]
- 5.Eldrup-Jorgensen J, Hawkins R, Bredenberg C. Abdominal vascular catastrophes. Surg Clin North Am. 1997;77:1305–1320. [DOI] [PubMed] [Google Scholar]
- 6.Acosta S, Björck M. Acute thromboembolic occlusion of the superior mesenteric artery: a prospective study in a well defined population. Eur J Vasc Endovasc Surg. 2003;26:179–183. [DOI] [PubMed] [Google Scholar]
- 7.Park W, Glovicki P, Cherry K, et al. Contemporary management of acute mesenteric ischemia: factors associated with survival. J Vasc Surg. 2002;35:445–452. [DOI] [PubMed] [Google Scholar]
- 8.Mamode N, Pickford I, Leiberman P. Failure to improve outcome in acute mesenteric ischaemia: seven year review. Eur J Surg. 1999;165:203–208. [DOI] [PubMed] [Google Scholar]
- 9.Acosta S, Ögren M, Sternby N-H, et al. Incidence of acute thromboembolic occlusion of the superior mesenteric artery: a population-based study. Eur J Vasc Endovasc Surg. 2004;27:145–150. [DOI] [PubMed] [Google Scholar]
- 10.Bengtsson H, Bergqvist D. Ruptured abdominal aortic aneurysm: a population-based study. J Vasc Surg. 1993;18:74–80. [DOI] [PubMed] [Google Scholar]
- 11.Carlsson J, Sternby NH. Aortic aneurysms. Acta Chir Scand. 1964;127:466–473. [PubMed] [Google Scholar]
- 12.Kagan R, Sternby NH, Uemura K, et al. Atherosclerosis of the aorta and coronary arteries in five towns. Bull WHO. 1976;53:5–6. [PMC free article] [PubMed] [Google Scholar]
- 13.Sternby NH. Atherosclerosis in a defined population: an autopsy survey in Malmö, Sweden. Acta Pathol Microbiol Immunol Scand. 1968;suppl 194:5. [PubMed] [Google Scholar]
- 14.Finucane PM, Arunachalam T, O'Dowd J, et al. Acute mesenteric infarction in elderly patients. J Am Geriatr Soc. 1989;37:355–358. [DOI] [PubMed] [Google Scholar]
- 15.Björck M, Acosta S, Lindberg F, et al. Revascularization of the superior mesenteric artery after acute thromboembolic occlusion. Br J Surg. 2002;89:1–7. [DOI] [PubMed] [Google Scholar]
- 16.Wilson CW, Gupta R, Gilmour DG, et al. Acute superior mesenteric ischaemia. Br J Surg. 1987;74:279–281. [DOI] [PubMed] [Google Scholar]
- 17.Endean E, Barnes S, Kwolek C, et al. Surgical management of thrombotic acute intestinal ischaemia. Ann Surg. 2001;233:801–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Järvinen O, Laurikka J, Salenius J-P, et al. Acute intestinal ischaemia: a review of 214 cases. Ann Chir Gyn. 1994;83:22–25. [PubMed] [Google Scholar]
- 19.Kieny R. Surgical therapy of acute mesenteric artery occlusion. Langenbecks Arch Chir. 1990;(suppl II):303–309. [PubMed] [Google Scholar]
- 20.Ottinger L. The surgical management of acute occlusion of the superior mesenteric artery. Ann Surg. 1978;6:721–731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goyen M, Ruehrn S, Debatin J. MR angiography for assessment of peripheral vascular disease. Radiol Clin North Am. 2002;40:835–846. [DOI] [PubMed] [Google Scholar]
- 22.Fleischmann D. Multiple detector-row CT angiography of the renal and mesenteric vessels. Eur J Radiol. 2003;45:879–887. [DOI] [PubMed] [Google Scholar]