Abstract
Objective:
To report on the long-term follow-up of a randomized clinical trial comparing pancreatic head resection according to Beger and limited pancreatic head excision combined with longitudinal pancreatico-jejunostomy according to Frey for surgical treatment of chronic pancreatitis.
Summary Background Data:
Resection and drainage are the 2 basic surgical principles in surgical treatment of chronic pancreatitis. They are combined to various degrees by the classic duodenum preserving pancreatic head resection (Beger) and limited pancreatic head excision combined with longitudinal pancreatico-jejunostomy (Frey). These procedures have been evaluated in a randomized controlled trial by our group. Long-term follow up has not been reported so far.
Methods:
Seventy-four patients suffering from chronic pancreatitis were initially allocated to DPHR (n = 38) or LE (n = 36). This postoperative follow-up included the following parameters: mortality, quality of life (QL), pain (validated pain score), and exocrine and endocrine function.
Results:
Median follow-up was 104 months (72-144). Seven patients were not available for follow-up (Beger = 4; Frey = 3). There was no significant difference in late mortality (31% [8/26] versus 32% [8/25]). No significant differences were found regarding QL (global QL 66.7 [0–100] versus 58.35 [0–100]), pain score (11.25 [0–75] versus 11.25 [0–99.75]), exocrine (88% versus 78%) or endocrine insufficiency (56% versus 60%).
Conclusions:
After almost 9 years’ long-term follow-up, there was no difference regarding mortality, quality of life, pain, or exocrine or endocrine insufficiency within the 2 groups. The decision which procedure to choose should be based on the surgeon's experience.
We report on the long-term results (104 months) of 74 patients who underwent organ-sparing pancreatic head resection (Beger vs. Frey) for chronic pancreatitis. In essence, no differences regarding mortality, quality of life, pain, or exocrine or endocrine insufficiency could have been detected within the 2 groups.
Patients with chronic pancreatitis suffering from severe pain pose a therapeutic challenge.1 Currently employed therapeutic options in conservative and operative treatment of chronic pancreatitis mainly address the symptoms and eventually evolving complications of the disease. Based on the hypotheses of pain origin in chronic pancreatitis—perineural inflammation2 and ductal hypertension3—2 principles have been introduced to surgery for chronic pancreatitis: drainage and resection.
A variety of different procedures has been proposed emphasizing one or the other.4–6 Both options are combined in the principle of duodenum preserving pancreatic head resection. Various modifications of the original method, described by Beger et al,7 have been suggested,8 but only the modification proposed by Frey and Smith9 received considerable attention.
Chronic pancreatitis with an inflammatory mass in the head of the pancreas has been considered the classic indication for a resective procedure (ie, partial pancreatoduodenectomy).10 This mass will frequently generate complications of adjacent organs (eg, common bile duct stenosis and duodenal stenosis).11 The sacrifice of otherwise-not-diseased organs (ie, duodenum, distal bile duct, and papilla) and occasionally distal stomach is the major disadvantage of this procedure.
Duodenum-preserving resection of the head of the pancreas also tackles the problem. This procedure includes subtotal resection of the pancreatic head, sparing the stomach, duodenum, and common bile duct while it reliably provides pain relief. As a possible alternative, a modification of the Partington-Rochelle procedure has been promoted by Frey and Smith.9 It basically consists of a limited excision of the pancreatic head in combination with a longitudinal pancreaticojejunostomy (extended Partington-Rochelle procedure).
To compare both techniques of duodenum-preserving resection of the head of the pancreas, a prospective randomized study was devised, and the operative results, including a 30-month follow-up, have been published previously.12
Long-term results after treatment of chronic pancreatitis will define, however, what procedure should be recommended to these patients since late mortality and morbidity is a significant factor in patients undergoing surgery for chronic pancreatitis.13 The following study consequently focuses on the late follow-up (median, 104 months) of this randomized controlled trial with regard to morbidity, mortality, quality of life, and late outcome of pancreatic exocrine and endocrine function, as well as definitive control of organ complications arising from adjacent organs.
METHODS
Patients
The presented data are results of a long-term follow-up of a closed randomized trial. The design of the randomized trial, inclusion and exclusion criteria, as well as patient assessment, treatment assignment, technical aspects of the operative procedures, in-hospital morbidity, and mortality and early postoperative results (follow-up at 30 months), are reported elsewhere.12
In essence, inclusion criteria were an inflammatory mass in the head of the pancreas (>35 mm in diameter), severe recurrent pain attacks (at least 1 per month requiring opiates), history of pain attacks for at least 1 year, or coexisting complications from adjacent organs (eg, common bile duct stenosis, duodenal stenosis). Disease-related exclusion criteria were chronic pancreatitis without involvement of the pancreatic head, pseudocysts without duct pathology, and portal vein thrombosis. Patient-related exclusion criteria were myocardial infarction within 6 months, detection of a malignant pancreatic tumor, and coexisting malignancy of other organs.
All patients were preoperatively seen by a panel of gastroenterologists and surgeons who decided on the indication for surgery. An inflammatory mass in the head of the pancreas was visualized in all patients.
Surgical intervention was indicated if endoscopic interventional therapy was not effective or not indicated. Patients were randomly allocated to undergo either Beger or Frey procedure. Of the originally 80 randomized patients, 6 were secondarily excluded after intraoperative finding of pancreatic carcinoma at frozen section.
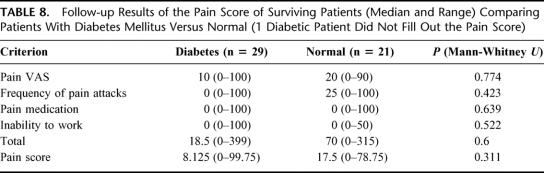
The primary endpoints of the study were pain assessed by a recently published pain score (Table 1) 14 and improvement of quality of life. Quality of life was measured by the European Organisation for Research and Treatment of Cancer's quality-of-life questionnaire15 and an additional module of 20 specific items incorporating a disease-specific symptom scale, a treatment-strain scale, and an overall hope and confidence scale. This scoring system has previously been validated for patients with chronic pancreatitis.14 Further criteria were definitive control of complications arising from adjacent organs, mortality and morbidity rates, exocrine and endocrine pancreatic function, and occupational rehabilitation.16
TABLE 1. The Pain Score (Total Score = Sum of Single Median Values, Pain Score = Total Score Divided by 4)
The study population consisted of 74 patients (n = 38 Beger, n = 36 Frey). These patients were reassessed after a median of approximately 8.5 years postoperatively (range, 72–144 months) by investigators who were unaware of group allocation. Patients were contacted by mail to fill out the quality-of-life questionnaire and pain-score forms. In addition, patients were asked to report to our outpatient clinic to sample stool for the assessment of exocrine pancreatic function (fecal pancreatic elastase, normal value: >200 μg/g feces). In all patients who were not on oral antidiabetic agents or insulin, an oral glucose tolerance test (OGTT) was performed and the results were classified as normal or diabetes mellitus according to the criteria set forth by the German Diabetes Society in 200217 (in accordance with WHO criteria of 1997). Diabetes mellitus was defined as blood glucose level of >200 mg/dL (11.1 mmol/L) 2 hours after OGTT. Continuous alcohol consumption was defined as average daily consumption of >12 g alcohol.18,19
The family practitioner and the local administration were contacted for all patients that did not answer by mail to assess if the patient had died. Patients that were not retrieved by these methods were declared as “lost to follow-up.”
Surgical Procedures
The procedures have been described elsewhere.12 Basically, the Beger operation included subtotal resection of the pancreatic head following transection of the pancreas above the portal vein. The body of the pancreas was drained by an end-to-end or end-to-side pancreatojejunostomy using a Roux-en-Y loop. The same jejunal loop drained the resection cavity by a side-to-side anastomosis to the rim of the resection cavity of the pancreatic head and uncinate process.
Limited pancreatic head excision combined with longitudinal pancreaticojejunostomy (Frey procedure) refrained from pancreatic transection above the portal vein. For reconstruction, 1 longitudinal pancreatojejunostomy was employed, draining the resection cavity of the head, uncinate process, body, and tail of the pancreas. Identification of the intrapancreatic course of the distal bile duct was facilitated by insertion of a metal probe into the choledochal duct through a proximal choledochotomy.20
In essence, the main difference between the 2 procedures was a much lesser extent of resection in the Frey procedure, leaving the uncinate process intact and refraining from transection above the portal vein, in contrast to Beger variant.
Statistical Analysis
SPSS 11.0 (SPSS Inc., Chicago, IL) was used for statistical analysis. Quality-of-life scores (functional and symptom scales) and pain scores were evaluated using the Mann-Whitney U test, and all other data were compared using the χ2 test. Statistical analysis was made on an intention-to-treat basis.
RESULTS
Hospital course and early postoperative results (median follow-up, 30 months) are reported elsewhere12
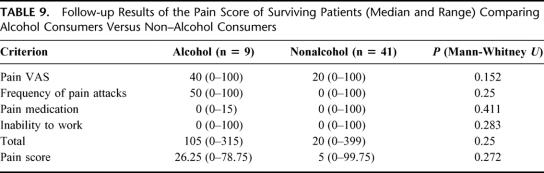
Follow-up and Mortality (Table 2)
TABLE 2. Death During Follow-up, Cause
Seven patients were lost to follow-up (Beger: 4; Frey: 3). Of the remaining 67 patients, 16 had died (Beger: 8; Frey: 8), leaving 51 patients (Beger: 26; Frey: 25) available for long-term follow-up. All patients entered the analysis.
The majority of patients died of chronic pancreatitis-unrelated causes,21,22 although in 6 patients the reason remained unclear.
Pain and Quality of Life
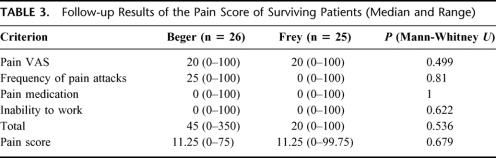
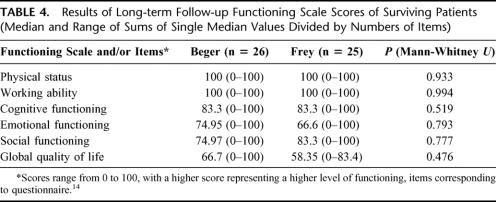
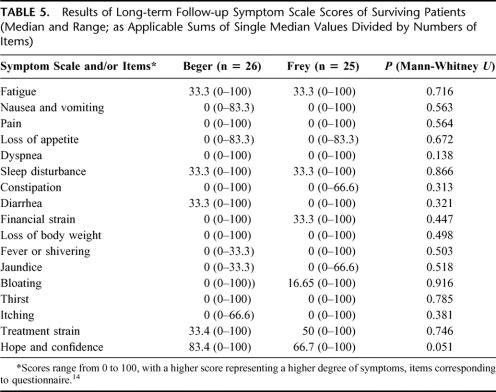
All 51 patients filled out the respective questionnaires. In surviving patients, there was no difference between the 2 groups regarding quality of life and pain score (Tables 3, 4, 5).
TABLE 3. Follow-up Results of the Pain Score of Surviving Patients (Median and Range)
TABLE 4. Results of Long-term Follow-up Functioning Scale Scores of Surviving Patients (Median and Range of Sums of Single Median Values Divided by Numbers of Items)
TABLE 5. Results of Long-term Follow-up Symptom Scale Scores of Surviving Patients (Median and Range; as Applicable Sums of Single Median Values Divided by Numbers of Items)
Comparing the quality-of-life and pain scores regarding the distribution of ranks using cross tables (χ2 test), there were no significant differences between the groups.
Control of Complications From Adjacent Organs (Table 6)
TABLE 6. Results of Long-term Follow-up of Surviving Patients
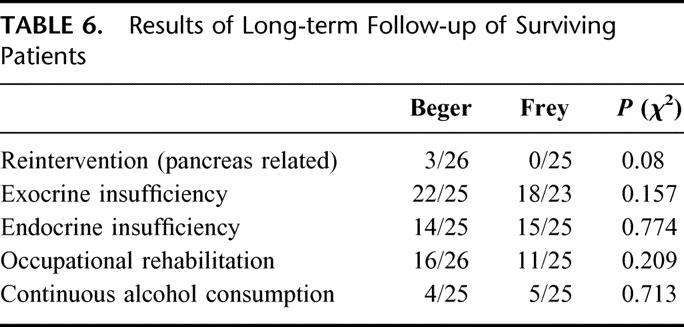
In 3 patients (all in the Beger group), a reintervention was necessary. One patient suffered from distal common bile duct stenosis due to recurrent chronic pancreatitis in the pancreatic head remnant after 84 months. He underwent a redo resection of the pancreatic head and a reinsertion of the distal bile duct into the resection cavity.23 The other 2 patient also suffered from recurrent chronic pancreatitis with enlargement of the pancreatic head remnant. One patient had additional pathology of the pancreatic duct in the tail. He underwent a Frey procedure 98 months postoperatively. The other patient underwent a pylorus-preserving partial pancreatoduodenectomy (PPPD) 74 months postoperatively because of a lesion which was highly suspicious of pancreatic carcinoma. The histopathology, however, only revealed recurrent severe chronic pancreatitis.
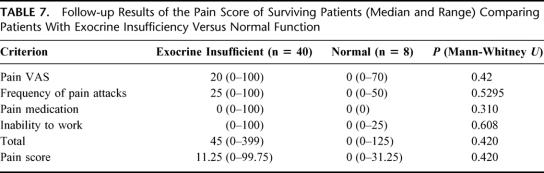
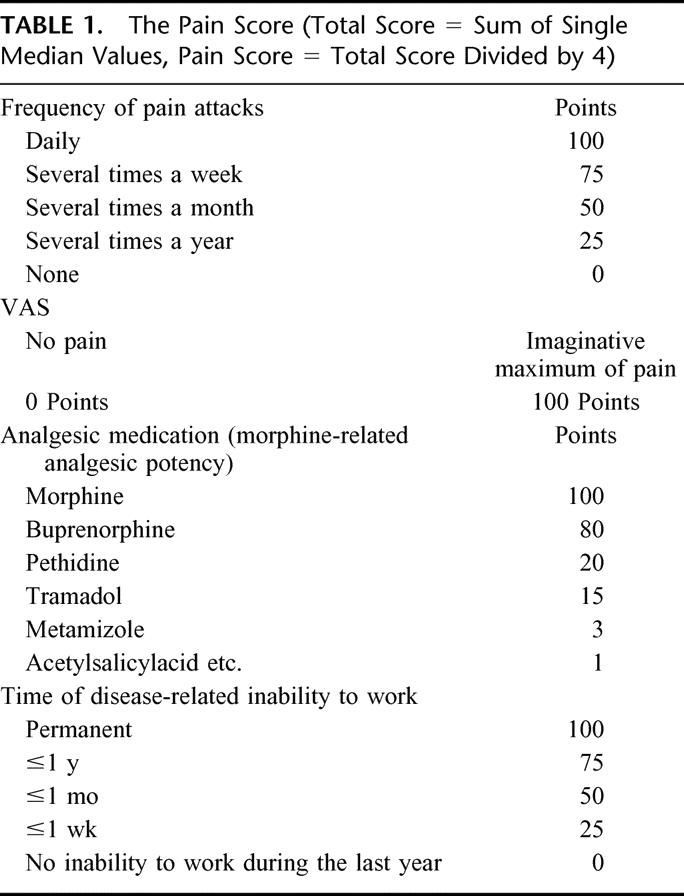
Exocrine and Endocrine Insufficiency (Tables 6–8)
TABLE 7. Follow-up Results of the Pain Score of Surviving Patients (Median and Range) Comparing Patients With Exocrine Insufficiency Versus Normal Function
TABLE 8. Follow-up Results of the Pain Score of Surviving Patients (Median and Range) Comparing Patients With Diabetes Mellitus Versus Normal (1 Diabetic Patient Did Not Fill Out the Pain Score)
Three patients (Beger: 1; Frey: 2) refused to be seen in the outpatient clinic and did not send stool samples for evaluation of exocrine insufficiency; therefore, results of 48 patients (Beger: 25; Frey: 23) were available regarding exocrine insufficiency. Of these 3 patients, 2 were known to be diabetic (Beger: 1; Frey: 1), so endocrine data were available in 50 patients (Beger: 25; Frey: 25).
Almost all patients were exocrine insufficient in both groups (Beger: 88%, 22/25; Frey: 78%, 18/23; ns). The rate of diabetic patients was slightly lower, with no significant difference between the 2 groups (Beger: 56%, 14/25; Frey: 60%, 15/25; ns).
Regarding pain score, there was no difference between patients with normal resp. abnormal exocrine or endocrine function (Tables 7, 8).
Occupational Rehabilitation (Table 6)
Twenty-six patients were professionally rehabilitated (Beger: 16/26; Frey: 11/25; n.s.). Of the nonprofessionally rehabilitated patients, 5 were unemployed (Beger: 4; Frey: 1; ns). The other patients were retired (Beger: 3; Frey: 6) (early retirement in all patients; before age 65 in males and 62 in females) or worked at home (household) voluntarily (Beger: 1; Frey: 2).
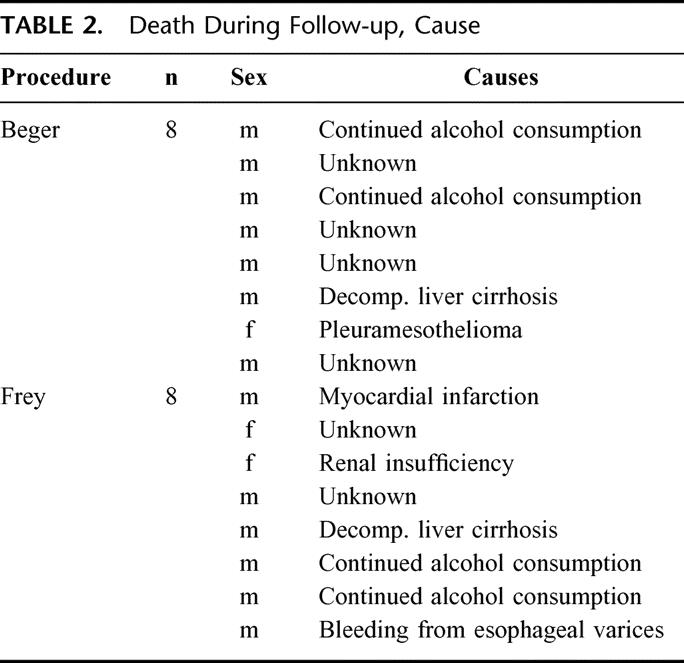
Continuous Alcohol Consumption (Tables 6, 9)
TABLE 9. Follow-up Results of the Pain Score of Surviving Patients (Median and Range) Comparing Alcohol Consumers Versus Non–Alcohol Consumers
One patient refused to give information about his alcohol consumption (Beger); therefore, 50 patients were available for evaluation (Beger: 25; Frey: 25). Nine patients admitted continuous alcohol consumption (Beger: 4, Frey: 5; ns).
If the pain score is compared between alcohol consumers and non–alcohol consumers, no difference is found in subgroups, total score, or pain score (Table 9). The same holds true for comparison between the 2 groups regarding functional and symptom scales (data not shown). There was no correlation between alcohol consumers and pain score (Table 9). Alcohol consumption did not make a difference between exocrine and endocrine insufficiency or the necessity for a reintervention due to pancreas-related problems (alcohol consumer: 1; non–alcohol consumer: 1; the other patient refused to give information about his drinking habits).
DISCUSSION
Surgical therapy for patients with chronic pancreatitis has become an accepted treatment modality that is most effective in relieving pain.24 In particular, resection of the head of the pancreas (pacemaker of the disease25) that harbors ductal and/or parenchymal pathologies in 95% of patients with chronic pancreatitis26 effectively relieves pain. Realizing this, the surgeon is faced with the decision to choose an optimal procedure for the patient. It should deliver pain control and quality of life while being safe and free of side effects. Prior to the introduction of the duodenum-preserving principle,7 extensive resective procedures, like partial pancreatoduodenectomy, have been the operative standard when aiming at the pancreatic head. Later, this procedure was modified to always incorporate additional drainage of the main pancreatic duct and at the same time leave the pancreas intact on top of the mesentericoportal axis.9 All these procedures provided adequate pain relief, controlled complications arising from adjacent organs, and identified pancreatic cancer during surgery that had been missed despite a broad diagnostic workup.27–30 To compare the efficacy of these procedures, 4 randomized trials have been initiated and early results have been reported.12,25,31–33
In one study, partial pancreatoduodenectomy (Whipple procedure) was compared with duodenum-preserving resection of the head of the pancreas.31 Pain and quality of life were assessed by descriptional, nonvalidated techniques. It was concluded that duodenum-preserving resection of the head of the pancreas provided quicker recuperation and better preservation of exocrine and endocrine pancreatic function while being equally effective in terms of pain control. In another study, better preservation of pancreatic function and superior pain control after duodenum-preserving resection of the head of the pancreas was found compared with PPPD after a very limited follow-up of 6 months. Quality of life was not assessed in that study.25 Our group was not able to demonstrate any significant differences between duodenum-preserving resection of the head of the pancreas and the combined drainage and local excision (Frey) regarding quality of life, pain control, exocrine and endocrine pancreatic function, and control of complications arising from adjacent organs in a short-term study.12 In another trial, we, however, found superior results regarding morbidity and quality of life for patients undergoing LE when compared with PPPD.33
There has been 1 recent report about results of a nonrandomized trial comparing classic Whipple (n = 30) versus duodenum-preserving resection of the pancreatic head according to Beger (n = 35), with a follow-up of 18 to 24 months postoperatively.34 The authors described better quality-of-life scores and less incidence of diabetes mellitus after the duodenum-preserving resection of the pancreatic head. This study, however, has a major drawback (nonrandomized; therefore susceptible to bias), and the follow-up is not long enough to draw any final conclusion.
After completing the long-term follow-up of our patients after pancreatic-head resection measured with reliable and valid scores, this is the first report on quality of life and pain after a meaningful time interval of 8.5 years, based on a randomized trial following surgical treatment of chronic pancreatitis.
Interestingly, no significant differences were detected in surviving patients over 8 years postoperatively. The initial impression that lesser resection and therefore sparing of undiseased organ would be of some benefit for the patient was not confirmed in this long-term follow-up. However, and maybe most important, both the functional scale and the symptom scale reflected improved quality of life in both groups compared with early postoperative levels. The same holds true for the pain score, with almost identical low values, as reported previously.33
In previous studies, continued alcohol abuse correlated with persisting pain after surgery.35–38 Other groups presented data about the relation of pain and continuous alcohol consumption in the natural course of pancreatitis.22,39 In our study population, no relation between continuous drinking and pain course was established (Table 9). The differing results might be explained by the fact that in the studies mentioned, the operative procedures were primarily drainage procedures. In addition, continuous alcohol consumption and “pain relief” were not precisely defined.
Both procedures were equally effective in controlling symptoms arising from adjacent organs, even though the only 3 patients who underwent a reintervention were patients in the Beger group. Whether this is a true difference can only be speculated since the study population might have been too small to detect a significant difference.
This is the longest available follow-up of a randomized trial comparing 2 organ-preserving procedures in patients suffering from chronic pancreatitis. The results show no difference between both surgical alternatives regarding quality of life and pain relief. Although one might speculate that a larger multi-institutional study could eventually demonstrate significant differences, we believe that these potential differences are too marginal to gain clinical impact.
The reported results after duodenum-preserving resection of the pancreatic head according to Beger can almost be superimposed on the results of the largest series of long-term followed patients after DPHR. Beger et al,40 in a nonrandomized study, reported on 303 patients undergoing duodenum-preserving pancreatic-head resection for chronic pancreatitis, with a mean follow-up of 5.7 years. Late mortality was 12.6%, redo operations related to pancreatic problems were necessary in 3.3%, and 61% of patients were found to have either pathologic glucose tolerance testing or manifested diabetes mellitus. Seventy-two percent were put on enzyme supplementation, but no data were given regarding pancreatic exocrine functional tests.
In our study population, there was no relation between pain and exocrine or endocrine insufficiency (Tables 7 and 8). Although we found a considerable amount of exocrine and endocrine insufficiency in our patients, the reported quality of life was good, irrespective of pancreatic insufficiency. This underlines the impact of chronic pain on the patients’ quality of life. It also hints towards the effectiveness of both procedures in addressing the pancreatic head as the main factor in the development of pain. It also underlines the fact that the development of pancreatic insufficiency probably develops independent of the surgical procedure41 and seems to be related to the chronic feature of the disease.
It is not legitimate to statistically compare our study populations with study populations that have been reported elsewhere. We can, therefore, only assume an overall late mortality rate of around 30% (28.8%-35%) and a pancreatitis-related death rate of around 15% (12.8%-19.8%) in patients with chronic pancreatitis without surgical intervention during a similar follow-up period.21,22,39,42 This leaves around 15% of patients dying of pancreatitis-unrelated causes, which parallels the mortality rate in our study population. Even though we do not have information about the cause of death in 6 patients, all other patients died of causes that were unrelated to chronic pancreatitis. Therefore, one might conclude that either complete resection of the pancreatic head (Beger) or limited excision (Frey) results in a very low pancreas-related death rate since it controls the disease effectively after long-term follow-up.
In conclusion, both the standard duodenum-preserving resection of the pancreatic head (Beger) and the limited pancreatic-head excision with extended drainage (Frey) ensure comparable quality of life and pain control after long-term follow-up. These surgical procedures were equally effective in controlling symptoms arising from adjacent organs and have an acceptably low mortality rate. Since both procedures are equally effective, future operations will be tailored to the patient's individual needs using a combination and or modification of the 2 procedures, only as long as the pancreatic head is addressed.43,44
With the available data and precise instruments allowing the measurement of quality of life and pain, a comparison between patients undergoing effective surgical treatment and conservative and endoscopic alternatives will become possible and necessary.
ACKNOWLEDGMENTS
The authors would like to thank Volker Schoder, MSc, Department of Mathematics and Computer Sciences in Medicine, University Hospital Eppendorf, for his support in statistical calculation.
Footnotes
Reprints: J. R. Izbicki, MD, FACS, Department of General Surgery, University Hospital Hamburg Eppendorf, Martinistrasse 52, D-20246 Hamburg, Germany. E-mail: izbicki@uke.uni-hamburg.de.
REFERENCES
- 1.Warshaw AL. Pain in chronic pancreatitis: patients, patience, and the impatient surgeon. Gastroenterology. 1984;86:987–989. [PubMed] [Google Scholar]
- 2.Bockmann DE, Buechler M, Malfertheimer P, et al. Analysis of nerves in chronic pancreatitis. Gastroenterology. 1988;94:1459–1469. [DOI] [PubMed] [Google Scholar]
- 3.Ebbehoj N, Svendsen LB, Madsen P. Pancreatic tissue pressure in chronic obstructive pancreatitis. Scand J Gastroenterol. 1984;19:1066–1068. [PubMed] [Google Scholar]
- 4.Puestow CB, Gillesby WJ. Petrograde surgical drainage of pancreas for chronic pancreatitis. Arch Surg. 1958;76:898–906. [DOI] [PubMed] [Google Scholar]
- 5.Partington PF, Rochelle REL. Modified Puestow procedure for retrograde drainage of the pancreatic duct. Ann Surg. 1960;152:1037–1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Whipple AO. Radical surgery for certain cases of pancreatic fibrosis associated with calcareous deposits. Ann Surg. 1946;124:991–1006. [PMC free article] [PubMed] [Google Scholar]
- 7.Beger HG, Witte C, Krautzberger W, et al. [Experiences with duodenum-sparing pancreas head resection in chronic pancreatitis]. Chirurg. 1980;51:303–307. [PubMed] [Google Scholar]
- 8.Strate T, Bloechle C, Busch C, et al. Modifications of the duodenum-preserving pancreatic head resection. Ann Ital Chir. 2000;71:71–79. [PubMed] [Google Scholar]
- 9.Frey CF, Smith GJ. Description and rationale of a new operation for chronic pancreatitis. Pancreas. 1987;2:701–707. [DOI] [PubMed] [Google Scholar]
- 10.Jimenez RE, Fernandez-del Castillo C, Rattner DW, et al. Pylorus-preserving pancreaticoduodenectomy in the treatment of chronic pancreatitis. World J Surg. 2003;27:1211–1216. [DOI] [PubMed] [Google Scholar]
- 11.Beger HG, Buechler M. Duodenum preserving resection of the head of the pancreas in chronic pancreatitis with inflammatory mass in the head. World J Surg. 1990;14:83–87. [DOI] [PubMed] [Google Scholar]
- 12.Izbicki JR, Bloechle C, Knoefel WT, et al. Drainage versus Resektion in der chirurgischen Therapie der chronischen Kopfpankreatitis: eine randomisierte Studie. Chirurg. 1997;68:369–377. [DOI] [PubMed] [Google Scholar]
- 13.Sakorafas GH, Farnell MB, Nagorney DM, et al. Pancreatoduodenectomy for chronic pancreatitis: long-term results in 105 patients. Arch Surg. 2000;135:517–523. [DOI] [PubMed] [Google Scholar]
- 14.Bloechle C, Izbicki JR, Knoefel WT, et al. Quality of life in chronic pancreatitis: results after duodenum-preserving resection of the head of the pancreas. Pancreas. 1995;11:77–85. [DOI] [PubMed] [Google Scholar]
- 15.Aaronson NK, Ahmedzai S, Bergman B, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85:365–376. [DOI] [PubMed] [Google Scholar]
- 16.Frey CF, Pitt HA, Yeo CJ, et al. A plea for uniform reporting of patient outcome in chronic pancreatitis. Arch Surg. 1996;131:233–224. [DOI] [PubMed] [Google Scholar]
- 17.Brueckel J, Koebberling J. Definition, Klassifikation und Diagnostik des Diabetes mellitus. Diabetes Stoffwechsel. 2002;11(suppl. 2):6–39. [Google Scholar]
- 18.Mukamal KJ, Rimm EB. Alcohol's effect on the risk for coronary heart disease. Alcohol Res Health. 2001;25:255–261. [PMC free article] [PubMed] [Google Scholar]
- 19.Klatsky AL. Moderate drinking and reduced risk of heart disease. Alcohol Res Health. 1999;23:15–22. [PMC free article] [PubMed] [Google Scholar]
- 20.Izbicki JR, Bloechle C, Knoefel WT, et al. Complications of adjacent organs in chronic pancreatitis managed by duodenum-preserving resection of the head of the pancreas. Br J Surg. 1994;81:1351–1355. [DOI] [PubMed] [Google Scholar]
- 21.Ammann RW, Akovbiantz A, Largiader F, et al. Course and outcome of chronic pancreatitis. Gastroenterology. 1984;86:820–828. [PubMed] [Google Scholar]
- 22.Lankisch PG, Happe-Loehr A, Otto J, et al. Natural course in chronic pancreatitis: pain, exocrine and endocrine pancreatic insufficiency and prognosis of the disease. Digest. 1993;54:148–155. [DOI] [PubMed] [Google Scholar]
- 23.Izbicki JR, Bloechle C, Broering DC, et al. Reinsertion of the distal common bile duct into the resection cavity during duodenum preserving resection of the head of the pancreas for chronic pancreatitis. Br J Surg. 1997;84:791–792. [DOI] [PubMed] [Google Scholar]
- 24.Warshaw AL, Banks PA, Fernandez-del Castillo C. AGA technical review: treatment of pain in chronic pancreatitis. Gastroenterology. 1998;115:765–776. [DOI] [PubMed] [Google Scholar]
- 25.Buechler M, Friess H, Mueller MW, et al. Randomized trial of duodenum preserving pancreatic head resection versus pylorus preserving Whipple in chronic pancreatitis. Am J Surg. 1995;169:65–70. [DOI] [PubMed] [Google Scholar]
- 26.Izbicki JR, Bloechle C, Knoefel WT, et al. Surgical treatment of chronic pancreatitis and quality of life after operation. Surg Clin North Am. 1999;79:913–944. [DOI] [PubMed] [Google Scholar]
- 27.Frey CF, Amikura K. Local resection of the head of the pancreas combined with longitudinal pancreaticojejunostomy in the management of patients with chronic pancreatitis. Ann Surg. 1994;220:492–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Buechler MW, Friess H, Bittner R, et al. Duodenum-preserving pancreatic head resection: long-term results. J Gastrointest Surg. 1997;1:13–19. [DOI] [PubMed] [Google Scholar]
- 29.Stapleton GN, Williamson RCN. Proximal pancreatoduodenectomy for chronic pancreatitis. Br J Surg. 1996;83:1433–1440. [DOI] [PubMed] [Google Scholar]
- 30.Saeger HD, Schwall G, Trede M. Standard Whipple in chronic pancreatitis. In: Beger HG, Buechler M, Malfertheimer P, eds. Standards in Pancreatic Surgery. Berlin: Springer; 1993:385–391. [Google Scholar]
- 31.Klempa I, Spatny M, Menzel J, et al. Pankreasfunktion und Lebensqualität nach Pankreaskopfresektion bei der chronischen Pankreatitis. Chirurg. 1995;66:350–359. [PubMed] [Google Scholar]
- 32.Izbicki JR, Bloechle C, Knoefel WT, et al. Duodenum preserving resections of the head of the pancreas in chronic pancreatitis: a prospective randomized trial. Ann Surg. 1995;221:350–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Izbicki JR, Bloechle C, Broering DC, et al. Extended drainage versus resection in surgery for chronic pancreatitis: prospective randomized trial comparing the longitudinal pancreaticojejunostomy combined with local pancreatic head excision with the pylorus preserving pancreatoduodenectomy. Ann Surg. 1998;228:771–779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Witzigmann H, Max D, Uhlmann D, et al. Quality of life in chronic pancreatitis: a prospective trial comparing classical Whipple procedure and duodenum-preserving pancreatic head resection. J Gastrointest Surg. 2002;6:173–179. [DOI] [PubMed] [Google Scholar]
- 35.Leger L, Lenriot JP, Lemaigre G. Five to twenty year follow-up after surgery for chronic pancreatitis in 148 patients. Ann Surg. 1974;180:185–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Trapnell JE. Chronic relapsing pancreatitis: a review of 64 cases. Br J Surg. 1979;66:471–475. [DOI] [PubMed] [Google Scholar]
- 37.Ammann RW, Largiader F, Akovbiantz A. Pain relief by surgery in chronic pancreatitis? relationship between pain relief, pancreatic dysfunction, and alcohol withdrawal. Scand J Gastroenterol. 1979;14:209–215. [DOI] [PubMed] [Google Scholar]
- 38.Holmberg JT, Isaksson G, Ihse I. Long term results of pancreaticojejunostomy in chronic pancreatitis. Surg Gynecol Obstet. 1985;160:339–446. [PubMed] [Google Scholar]
- 39.Miyake H, Harada H, Kunichika K, et al. Clinical course and prognosis of chronic pancreatitis. Pancreas. 1987;2:378–385. [DOI] [PubMed] [Google Scholar]
- 40.Beger HG, Schlosser W, Friess HM, et al. Duodenum-preserving head resection in chronic pancreatitis changes the natural course of the disease: a single-center 26-year experience. Ann Surg. 1999;230:512–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Malka D, Hammel P, Sauvanet A, et al. Risk factors for diabetes mellitus in chronic pancreatitis. Gastroenterology. 2000;119:1324–1332. [DOI] [PubMed] [Google Scholar]
- 42.Lankisch PG. Natural course of chronic pancreatitis. Pancreatology. 2001;1:3–14. [DOI] [PubMed] [Google Scholar]
- 43.Gloor B, Friess H, Uhl W, et al. A modified technique of the Beger and Frey procedure in patients with chronic pancreatitis. Dig Surg. 2001;18:21–25. [DOI] [PubMed] [Google Scholar]
- 44.Knoefel WT, Eisenberger CF, Strate T, et al. Optimizing surgical therapy for chronic pancreatitis. Pancreatology. 2002;2:379–385. [DOI] [PubMed] [Google Scholar]