Abstract
Objective:
To characterize the injuries to children by acts against civilian populations (AACP).
Summary Background Data:
Only 2 articles have focused on the spectrum and severity of injuries to children by AACP.
Methods:
A retrospective case study of children 0 to 18 years old who were entered into the Israel National Trauma Registry as a result of AACP between September 29, 2000, and June 30, 2002.
Results:
A total of 158 children were hospitalized for injuries caused by AACP, accounting for 1.4% of all hospitalized injured children but for 10.9% of all in-hospital deaths for trauma. Explosions injured 114 (72.2%); shootings, 34 (21.5%); and other mechanisms such as stoning or stabbing, 10 (6.3%). Older children were injured by explosions more frequently than younger children (86.1% of 15- to 18-year-olds, 73.7% of 10- to 14-year-olds, 63.2% of 0- to 9-year-olds, P = 0.02). A higher percentage of children injured by explosions rather than by shootings were severely or critically injured (33.9% versus 18.8%, P = 0.10). The most frequently injured body regions were extremities (62.8%), head/face (47.3%), chest and abdomen (37.2%), and brain (18.2%). More than 1 body region was injured in 63.0%. Children injured by explosions as compared with shootings had a lower incidence of abdominal trauma (14.9% versus 20.6%), a similar incidence of chest trauma (16.7% versus 14.7%), but a higher incidence of extremity trauma (65.8% versus 53.0%). There were 7 in-hospital deaths, 6 due to severe head injury and 1 due to severe abdominal trauma; 6 of the 7 deaths were caused by explosions, and all but 1 occurred in children 15 to 18 years old.
Conclusions:
AACP cause significant morbidity and mortality in children, especially adolescents. Injury severity is significantly higher among children who are injured by explosions rather than by shootings.
Acts against civilian populations resulted in the hospitalization of 158 children during a 20-month period in Israel. Older children were more likely to be injured by explosions than by shooting and to be severely or critically injured. Multiple body regions were injured in 63%; although extremity, head/face, and torso injury predominated, death was usually due to massive brain injury.
There has been a sharp increase in acts against civilian populations (AACP) in Israel beginning September 29, 2000; during the period ending June 30, 2001, 64 children 0 to 18 years old were killed by AACP.1 During this same period, 89 children were killed in motor-vehicle collisions. Death due to AACP became the second leading cause of traumatic death for children in Israel during this time period.
The most common types of AACP use explosive devices and shooting. Explosive devices, usually detonated in public locations such as shopping centers, pubs, and restaurants, usually contain multiple types of foreign bodies, such as shell fragments, nails, bolts, and metal balls, resulting not only in blast injury but in penetration of multiple foreign bodies as well. Most gunshot wounds were inflicted by sniper shootings at high velocity into passing cars or at pedestrians. Additionally, there were a few incidents of gunshots from automatic weapons into crowds of people. Other mechanisms include stabbing, stone throwing at motor vehicles or directly at the victim, and deliberate running over of the victim with a motor vehicle.
The pattern of injuries resulting from explosions and shootings during AACP has been well described in adults.2 Only 1 previous report on the Oklahoma City bombing described the spectrum of injuries due to explosions in children.3 A recent paper compared injuries due to AACP to other types of trauma in Israeli children.4 Only 1 description of shooting during AACP was identified, but children were not specifically addressed.5
This study characterizes the spectrum and severity of injury in children from AACP and explores possible explanations for the resulting clinical picture.
MATERIALS AND METHODS
The study population consisted of patients less than 18 years old who were injured during AACP. Cases of injury from AACP were identified though the use of the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes for external cause of injury (e-codes) E990–E998.
The study period extended from September 29, 2000, to June 30, 2002. Data on patient characteristics, nature of the injury, and outcome were obtained from the Israel National Trauma Registry, which records all hospitalizations for physical trauma at 9 trauma centers (including all 6 level I trauma centers) in the country. In-hospital deaths and transfers to acute care hospitals are recorded as well. Patients who were declared dead in the field or immediately upon arrival to the emergency department were not included in the data set. All 9 centers are designated tertiary-care and referral hospitals that receive the majority of severe or complicated cases of physical injury.
Medical diagnoses derived from the registry were coded according to the ICD-9-CM and included up to 10 diagnoses per patient. The Barell Injury Diagnosis Matrix6,7 was used to classify the diagnostic data: type of injury (fracture, dislocation, etc) was distributed along the matrix columns and cross-matched with bodily region affected (brain, head, torso, upper extremity, lower extremity, other), distributed in the matrix rows. The severity of injury was estimated using the Injury Severity Score (ISS),8 an anatomic scoring system that grades overall injury on a scale of mild (score of 1–8), moderate (score of 9–14), and severe (16 or greater).
Injury distribution and pattern analysis was done according to 6 body regions: (1) severe anatomic brain injury such as epidural and subdural hematomas, subarachnoid bleeding, cerebral lacerations, etc (TBI); (2) head/face/neck, including skull fractures without intracranial injury and concussion but excluding cervical spine injury (HEAD); (3) spinal cord and vertebral column injury (SCI/VCI); (4) chest, abdomen, pelvis, buttocks, and urogenital injuries (TORSO); (5) upper and lower extremities (EXTR); and (6) and other/unspecified region (OTHER).
SAS statistical software was used for the statistical analysis. Pearson χ2 test was used for categorical data, t test for continuous variables, and Wilcoxon nonparametric test for continuous variables with a nonnormal distribution. A value of P < 0.05 was considered statistically significant.
RESULTS
During the study period, September 29, 2000, to June 30, 2001, 11,654 children ages 0 to 18 years were entered into the Israel Trauma Registry. One hundred fifty-eight (1.4%) were injured by AACP, 2462 (21.1%) in motor vehicle collisions (MVC) and 9034 (77.5%) by other mechanism such as falls and burns. The in-hospital mortality rate for AACP trauma was 4.4%, over 3 times that for MVC (1.4%) and almost 20 times that for other mechanisms of injury (0.3%). Even though AACP accounted for only 1.4% of all injured children during the study period, it was responsible for 10.9% of all in-hospital deaths from trauma.
The most common mechanism of injury in AACP was explosion (N = 114, 72.2%) followed by shooting (N = 34, 21.5%); 10 children (6.3%) were injured by other means including stone throwing, stabbing, and deliberate running over by a motor vehicle. Due to their small number and the variety of mechanisms, these children are not included in further analysis, leaving 148 children in the study group. As seen in Figure 1, the proportion of children with minor injury (ISS 1-8) was greater for children injured by shooting, and a greater proportion of children injured by explosion had a ISS greater than or equal to 16, indicating severe or critical injury (33.9% versus 18.8%, P = 0.10).

FIGURE 1. Severity of injury.
As seen in Figure 2, children who were injured by explosions were significantly older than children injured by shooting. Less age variability is noted for shooting. Figure 3 demonstrates that a larger percentage of children 15 to 18 years old had ISSs 16 or greater as compared with other age groups due to explosion being the most common mechanism of injury in this age group.

FIGURE 2. Age distribution by mechanism.

FIGURE 3. Injury severity by age group.
The data suggest that females suffered greater morbidity and mortality than males, although this did not reach statistical significance. Females and males were equally represented in the data set, and there was no statistically significant difference between females and males injured by explosions (78.4% versus 75.7%, P = 0.7). However, 5 of the 7 children killed were female. A higher percentage of females had an ISS greater than 16 (36.1% versus 25.0%, P = 0.3); this difference remained for children injured by explosions (38.6% versus 29.1%, P = 0.6). There was no difference in the distribution of injuries by sex in children who were injured by explosions (data not presented).
Multiple procedures were performed as part of the initial stabilization of the injured children upon arrival to the emergency department. These procedures included medication and fluid administration (51.3% and 38.5% of injured children), insertion of nasogastric tube (11.5%), and tracheal intubation (10.1%). Diagnostic radiology procedures included plain x-rays (55.4%), CT scan (35.5%), and ultrasound (23.6%).
There were no invasive surgical procedures such as emergency thoracotomy performed in the emergency department.
The most frequently injured body regions were the extremities, with 62.8% of children sustaining injuries, followed by head (47.3%), torso (37.2%), TBI (18.2%), other (8.1%), and SCI/VCI (2.7%). An ISS greater than 16 occurred more frequently in children having TBI (66.7%), SCI/VCI (75.0%), and torso (58.2%) injuries. Children who died had a higher frequency of TBI, torso, and extremity injuries.
The majority of children sustained injury to multiple body regions. Children sustained injuries to 1 or 2 body regions 79.1% of the time, to 3 body regions 16.5% of the time, and to 4 body regions 4.3% of the time. No child injured by shooting sustained injury to more than 2 body regions. As expected, increasing number of body regions injured was associated with a greater proportion of children with ISS greater than 16. The percent of children with ISS greater than 16 and injury to 1 body region was 9.6%, with injury to 2 body regions 40.4%, and with injury to 3 or 4 body regions 47.8% and 83.3%. No pattern could be detected in which anatomically adjacent body regions were injured (eg, head and torso, torso and extremities). The high frequency of extremity injury resulted in this association with every other body region. In addition, no association could be found between ISS greater than 16 and a particular clustering of body-region injuries. The small number of deaths in the study population was too small to determine whether mortality rates increased with injury to increasing number of body regions.
A different injury pattern was observed for explosions and shootings as seen in Figure 4. Head, torso, and extremity injuries commonly resulted from both mechanisms of injury. Head injuries were almost twice as common among children injured by explosions as by shooting; when injuries to the “head” region are detailed, the difference is even more striking. Children injured by explosions had 2.5 times as many facial injuries (29.8% versus 11.8%) and 4.4 times as many eye injuries (13.2% versus 3.0%) as children injured by shooting. The higher incidence of torso injury in children injured by shooting is due to a higher incidence of abdominal trauma (20.6% versus 14.9%); the incidence of chest trauma is similar (14.7% versus 16.7%) for shootings and explosions. Injuries to upper extremities (26.5% versus 40.4%) and lower extremities (38.2% versus 49.1%) were more frequent in children injured by explosions rather than by shooting. There was a statistically significant difference in injury to “other” body region between children injured by explosions rather than by shootings (10.5% versus 0%, P = 0.05) but no difference in injuries to the spinal cord/vertebral column (2.6% versus 2.9%).
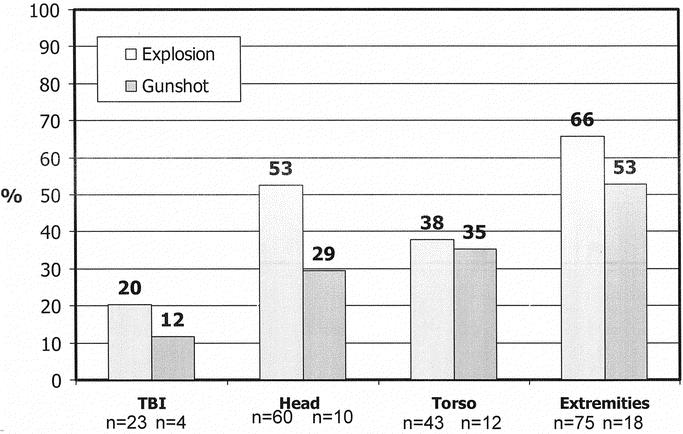
FIGURE 4. Injury distribution by mechanism.
Seven children died after hospital admission, 6 of whom were injured by explosion and 1 by other mechanism; no child died as a result of shooting. All of the children who died as a result of explosion were aged 15 to 18 years, whereas the child killed by other mechanism (stoning) was less than 1 year old. All these children had ISSs of 16 or more, and 6 of the 7 had ISSs greater than 25; no child with ISS greater than 50 survived. Two patients died prior to ICU admission and 5 patients died in the ICU; there were no deaths in the hospital wards. One child died on the second hospital day, 2 children died on the sixth hospital day, 1 child on the 12th hospital day, and 1 on the 17th. All but 1 of the children had multiple, severe head injuries, including subarachnoid hemorrhage (2), severe cerebral edema (3), penetrating cerebral injury (3), laceration of a cerebral sinus (1), and cerebral hematoma (3). The final child suffered massive isolated abdominal trauma due to an explosion, including injury to the abdominal aorta and lacerations of the kidney, liver, and small bowel.
DISCUSSION
Our results show that AACP cause significant injury in children. A previous study demonstrated that morbidity and mortality were significantly higher in Israeli children injured by AACP as compared with usual trauma mechanisms such as MVCs or falls.4 Injuries due to AACP may involve any region of the body and tend to involve multiple regions. Children injured by explosions had a greater number of body regions injured and therefore higher ISS scores. Although the small number of deaths precluded analysis of the association between the number of body regions injured and incidence of death, the data suggest that the location (TBI and torso) and type of injury are the major determiners of mortality.
A clear interrelationship exists between mechanism of injury, age, and severity of injury. Explosions were responsible for the substantial morbidity and mortality in children 15 to 18 years old. These explosions most commonly occurred in public venues such as restaurants, discos, and pubs that are frequented by older adolescents and young adults. A typical example is the explosion at the Dolphinarium on the evening of Friday, December 1, 2001, at 11:45 pm, a dance club visited almost exclusively by Russian immigrants in their late teens and early twenties. The explosion among persons waiting to enter the club killed 21 people, 16 of them under 18 years old.
There are several possible explanations for the suggestion of increased morbidity and mortality among females as compared with males. Hadden et al9 suggested that clothing played a protective role in explosions; women's heads were protected against lacerations by hats and hair, while men's extremities were protected against lacerations, burns, and abrasions by pants. This was not found in our population, probably due to changes in dress norms since Hadden's article was published in 1978. The difference between sexes may be due to chance alone due to the small study population; this will be clarified as more data are accrued.
Our in-hospital mortality rate of 5.3% for explosions is similar to what has been reported in the literature for adults.9–12 The only article dealing with explosive injury to children, by Quintana et al,3 noted an immediate mortality rate of 28.8% from the bombing in Oklahoma City but no in-hospital deaths. Only 7 of the 47 surviving children were admitted and all to the ICU. This population differs from our study population by the distribution of injury severity and the mechanism of injury. The magnitude of the bomb in Oklahoma City was significantly larger than the bombs detonated in proximity to our study population, and fire and crush injury played a significant role in morbidity and mortality in Oklahoma City.
Since all the explosions in this study contained metallic foreign bodies, it is difficult to separate the effects of blast injury from the effects of the projectiles contained within the bombs. Primary blast injury consists of perforated eardrum(s), blast lung (pulmonary contusions, hemopneumothorax, emphysema, alveolar-venous fistulas), and blast abdomen (hemorrhage and perforation of closed viscus, pneumoperitoneum).13 Data recorded by ICD-9 codes do not allow clear differentiation between injuries due to blast effect and injuries due to penetrating foreign bodies contained in the explosives. Preliminary analysis of our data was unable to separate the effects of primary blast injury from projectile injury. Further analysis is planned to determine the specific contributions of primary blast injury and projectile injury to morbidity and mortality, reflecting recent research, which has defined these injuries as multidimensional.14–16
A number of studies have noted the highest injury specific mortality rate in explosions is due to truncal injury. Our injury specific mortality rate (proportion of children with this injury who died) for chest trauma was 10.5%; and for abdominal trauma, 17.7%. The chest-injury-specific mortality rate is similar to the report of 8.2% for one bus bombing involving adults,17 although lower than 18.3% reported for a different bus bombing10 in which multiple significant other injuries contributed to the higher mortality rate. These injury-specific mortality rates are similar to those reported by Frykburg and Tepas11 for chest (11%) and abdominal (19%) injury, but exact comparisons are difficult. Figures were reported for immediate survivors, of which 30% were eventually admitted. Since some of these patients may have died prior to hospital admission, the actual injury-specific mortality rate for only admitted patients may be lower. Three studies, however, did not report any deaths in patients with abdominal trauma due to explosions,9,10,17 suggesting that the presence of metallic foreign bodies in the explosives may have contributed to mortality in abdominal trauma, further supporting the literature on multidimensional injuries.14–16
Our severe-head-injury rate of 16.8% falls within the range of 2%9 to 57%3 reported in studies describing explosion injuries in which metallic foreign bodies were not present; exact comparisons are difficult due to varying definitions of severe head injury. The severe-head-injury–specific mortality rate in our population was 21.7%, which is similar to the 20% and 25% described by Hadden et al9 and Katz et al.10 This suggests that the presence of metallic foreign bodies in the explosion did not substantially contribute to morbidity and mortality from severe head injury.
Only 1 article could be located that addressed shooting injury due to AACP; this article is contemporary to the period of this paper and included both children and adults.5 The closest analogy to the shooting mechanism in our population is a drive-by shooting. Although multiple descriptions of gunshot injuries to children exist,18–20 the specific mortality and morbidity associated with this mechanism have not been reported, making comparisons to our population difficult.
All hospitalized children who were injured by AACP were admitted to one of the trauma-registry-participating hospitals, so no cases of seriously injured, hospitalized children were missed in data collection. However, one limitation of this study is the absence of nonhospitalized children in the data set, such that only data on the more severe spectrum of injury are available for analysis. Due to overtriaging and overadmitting in mass-casualty events, it is expected that some mildly injured children would have been admitted as well.21,22 A second limitation is the relatively small study population and the small number of in-hospital deaths, which precluded using mortality as an outcome measure. Data on prehospital management are not included in the database and are beyond the scope of this paper.
Injury and death due to AACP has become a worldwide medical-management and public-health issue. Injury severity is significantly higher among children injured by explosions than by shootings. Our findings suggest that the presence of metallic foreign bodies significantly increases the morbidity and mortality associated with abdominal trauma, but additional analysis is necessary to determine changes in injury pattern. Additional research will also help to differentiate between penetrating injury due to foreign bodies and primary blast injury. As AACP continue to be a problem worldwide, this information can help improve medical management of these victims.
ACKNOWLEDGMENTS
Thanks to Prof. Yehuda Hiss, National Institute of Forensic Pathology, for mortality figures.
Footnotes
The Israel Trauma Group is a study group composed of the heads of trauma units of all hospitals belonging to the Israel National Trauma Registry: Drs R. Alfici, E. Ishtov, J. Jeroukhimov, Y Klein, Y. Kluger, M. Michaelson, A. Rivkind, G. Shaked, D. Simon, and M. Stein.
Reprints: Dr. Lisa Amir, Unit of Emergency Medicine, Schneider Children's Medical Center of Israel, Kaplan 14, Petach Tikva, Israel 49202. E-mail: lamir@clalit.org.il.
REFERENCES
- 1.Personal communication, Dr. Y Hiss, Head of National Institute of Forensic Pathology, June 19, 2003.
- 2.Peleg K, Aharonson-Daniel L, Stein M, et al. Patterns of injury in hospitalized terrorist victims. Am J Emerg Med. 2002;21:258–262. [DOI] [PubMed] [Google Scholar]
- 3.Quintana DA, Jordan FB, Tuggle DW, et al. The spectrum of pediatric injuries after a bomb blast. J Pediatr Surg. 1997;32:307–311. [DOI] [PubMed] [Google Scholar]
- 4.Aharonson-Daniel L, Waisman Y, Dannon YL, et al. Epidemiology of terror-related versus non-terror-related traumatic injury in children. Pediatrics. 2003;112:e280. [DOI] [PubMed] [Google Scholar]
- 5.Mintz Y, Shapira SC, Pikarsky AJ, et al. The experience of one institution dealing with terror: the El Aqsa riots. Isr Med Assoc J. 2002;4:554–556. [PubMed] [Google Scholar]
- 6.Barell V, Aharonson-Daniel L, Fingerhut LA, et al. An introduction to the Barell body region by nature of injury diagnosis matrix. Injury Prev. 2002;8:91–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.http://www.cdc.gov/nchs/about/otheract/ice/barellmatrix.htm.
- 8.Baker SP, O'Neill B, Haddon W, et al. The Injury Severity Score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187–196. [PubMed] [Google Scholar]
- 9.Hadden WA, Rutherford WH, Merrett JD. The injuries of terrorist bombing: a study of 1532 consecutive patients. Br J Surg. 1978;65:525–531. [DOI] [PubMed] [Google Scholar]
- 10.Katz E, Ofek B, Adler J, et al. Primary blast injury after a bomb explosion in a civilian bus. Ann Surg. 1989;209:484–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Frykberg ER, Tepas JJ. Terrorist bombings: lessons learned from Belfast to Beirut. Ann Surg. 1988;208:569–576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mellor SG. The relationship of blast loading to death and injury from explosion. World J Surg. 1992;16:893–898. [DOI] [PubMed] [Google Scholar]
- 13.Wightman JM, Gladish SL. Explosions and blast injuries. Ann Emerg Med. 2001;37:664–678. [DOI] [PubMed] [Google Scholar]
- 14.Peleg K, Aharonson-Daniel L, Stein M, et al. Gunshot and explosion injuries: characteristics, outcomes and implications for care of terror related injuries in Israel. Ann Surg. 2004;239:311–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sorkin P, Nimrod A, Biderman P, et al. The quinary (V th) injury pattern of blast. J Trauma, in press. [PubMed]
- 16.Kluger Y. Bomb explosions in acts of terrorism-detonation, wound ballistics, triage and medical concerns. Isr Med Assoc J. 2003;5:1–6. [PubMed] [Google Scholar]
- 17.Leibovici D, Gofrit ON, Shapira SC. Eardrum perforation in explosion survivors: is it a marker of pulmonary blast injury? Ann Emerg Med. 1999;34:168–172. [DOI] [PubMed] [Google Scholar]
- 18.Nance ML, Stafford PW, Schwab CW. Firearm injury among urban youth during the last decade: an escalation in violence. J Pediatr Surg. 1997;32:949–952. [DOI] [PubMed] [Google Scholar]
- 19.Laraque D, Barlow B, Durkin M, et al. Children who are shot: a 30-year experience. J Pediatr Surg. 1995;30:1072–1075. [DOI] [PubMed] [Google Scholar]
- 20.Snyder AK, Chen LE, Foglia RP, et al. An analysis of pediatric gunshot wounds treated at a level I pediatric trauma center. J Trauma. 2003;54:1102–1106. [DOI] [PubMed] [Google Scholar]
- 21.American College of Surgeons Committee on Trauma. Field categorization of trauma victims. Bull Am Coll Surg. 1986;71:17–21. [Google Scholar]
- 22.Mor M, Waisman Y. Triage principles in multiple casualty situations involving children: the Israeli experience. Pediatric Emergency Medicine Database (serial online). August 2002. Available from PERC-Pediatric Emergency Research Canada. Accessed November 20, 2003.


