Abstract
Objective:
To determine the impact of the obesity epidemic on workload for general surgeons.
Summary Background Data:
In 2001, the prevalence of obesity in the United States reached 26%, more than double the rate in 1990. This study focuses on the impact of obesity on surgical practice and resource utilization.
Methods:
A retrospective analysis was done on patients undergoing cholecystectomy, unilateral mastectomy, and colectomy from January 2000 to December 2003 at a tertiary care center. The main outcome variables were operative time (OT), length of stay (LOS), and complications. The key independent variable was body mass index. We analyzed the association of obesity status with OT, LOS, and complications for each surgery, using multivariate regression models controlling for surgeon time-invariant characteristics.
Results:
There were 623 cholecystectomies, 322 unilateral mastectomies, and 430 colectomies suitable for analysis from 2000 to 2003. Multivariable regression analyses indicated that obese patients had statistically significantly longer OT (P < 0.01) but not longer LOS (P > 0.05) or more complications (P > 0.05). Compared with a normal-weight patient, an obese patient had an additional 5.19 (95% confidence interval [CI], 0.15–10.24), 23.67 (95% CI, 14.38–32.96), and 21.42 (95% CI, 9.54–33.30) minutes of OT with respect to cholecystectomy, unilateral mastectomy, and colectomy. These estimates were robust in sensitivity analyses.
Conclusions:
Obesity significantly increased OT for each procedure studied. These data have implications for health policy and surgical resource utilization. We suggest that a CPT modifier to appropriately reimburse surgeons caring for obese patients be considered.
We merged administrative and clinical data to estimate the impact of obesity on general surgical resources. Obesity significantly increased operative time for all 3 surgical procedures (cholecystectomy, unilateral mastectomy, and colectomy) studied. There was no effect of obesity on length of stay or in-hospital complications. The obesity epidemic will increase the workload for general surgeons.
According to the 2002 Behavioral Risk Factor Surveillance System Survey collected by the Centers for Disease Control and Prevention, the prevalence of obesity among US adults has doubled since 1990.1 The rate of increase in obese individuals has reached epidemic proportions in the United States. Concurrent with the increase in obesity, obesity-related diseases have also increased. In fact, obesity and obesity-related diseases have almost surpassed tobacco as the most significant etiology of preventable death.2
Annual healthcare expenditures for an obese individual are $732 more than for a nonobese individual.3 In fact, healthcare expenditures attributable to obesity accounted for 9.1% of the total US healthcare expenditures for fiscal year 1998.3 The burden of the obesity epidemic on healthcare resource utilization has been demonstrated for multiple aspects of the healthcare delivery system. Increases in physician office visits, hospital admissions and hospital length of stay (LOS), nursing home admission, and prescription drug usage have been described for obese patients.4–6
The obesity epidemic has several implications for the field of general surgery. Much attention has been given to the increased demand for bariatric surgical services; however, the impact of obesity on surgeons’ workload extends well beyond this. Increases in obesity-related diseases such as gallstones, breast cancer, and colon cancer will increase the demand for general surgical services. Obesity has been implicated as a risk factor for postoperative complications. Obesity does not appear to be an independent predictor of severe postoperative complications but does increase the risk for wound complications.7–9 Furthermore, poor long-term functional outcomes following hernia and antireflux surgery have been associated with obesity.10,11
The purpose of this study is to focus on the impact of the obesity epidemic on general surgery workload. Prior studies on surgeon workload, particularly regarding the impact of the aging population, have concluded that there will be an increased demand for surgical services in the future.12,13 There are no studies that specifically address how the increase in the prevalence of obesity will affect surgeon workload. We undertook this study to describe the impact of obesity on acute-care services for 3 surgical procedures; cholecystectomy, unilateral mastectomy, and colectomy. These procedures, which account for approximately 15% of a general surgeon's workload, were chosen because of the fairly uniform nature of the procedure and their use in the treatment of obesity-related diseases.14 We have included procedures done by multiple surgeons over multiple years in our analysis. We specifically focused on the association of obesity on operative time (OT), LOS, and in-hospital complications.
Data and Methods
Data used for this study were from the University of Alabama at Birmingham Hospital from January 1, 2000, to December 31, 2003. The study was approved by the institutional review board under a waiver of informed consent. We used current procedural terminology, 4 codes to select all instances of 3 surgeries (cholecystectomy, unilateral mastectomy, and colectomy) from claims data. Variables of interest in the claims data included LOS and demographics. These claims data were merged with the anesthesia clinical database to collect additional information on OT, weight/height, American Society of Anesthesiologists (ASA) class, and identification of attending surgeon. We conducted targeted chart reviews to verify the procedures, diagnosis, identification of attending surgeon, and to retrieve additional surgery-specific information on previous abdominal surgery, laparoscopic versus open cholecystectomy, emergent versus elective colectomy, in-hospital complications, and death. We excluded patients who were trauma patients or underwent a concomitant surgery. We excluded males in the mastectomy group and those who underwent immediate breast-reconstruction procedures.
Outcome Variables
The dependent variables measured were OT, LOS, and in-hospital complications and death. OT was measured in minutes and defined as procedure start time to procedure end time. LOS was measured in days from the admission date to the discharge date. Complications and death that occurred in the same admission as the operative procedure were recorded. Complications were defined as any event that deviated from the normal postoperative course. All infectious and cardiac complications were included. Bleeding was defined as requiring greater than 2 units of packed red blood cells postprocedure or a return to the operating room to evacuate a hematoma. We did not include prolonged ileus as a complication unless it required a return to the operating room.
Independent Variables
The independent variable of key interest was obesity status, measured by body mass index (BMI; weight in kilograms divided by height in meters squared). We categorized BMI into 3 levels, according to the World Health Organization classifications for normal weight (BMI = 18–24.9), overweight (BMI = 25–29.9) and obese (BMI >30).15 We performed sensitivity analysis by using the continuous measure of BMI as an alternative, and the estimates of obesity impact remained robust. Thus, we chose to report the estimates using the categorized BMI.
Other covariates were age categories (under 45, 45–64, and 65+), race (African American versus non–African American), and gender (the cholecystectomy and colectomy samples only). We used ASA class as a proxy for case mix. In addition, we constructed a set of binary indicators for prior abdominal surgery (cholecystectomy and colectomy only), laparoscopic cholecystectomy, elective colectomy, and subtype of colectomy (ie, right colectomy including ileocecectomy, left colectomy including left and sigmoid, and total abdominal colectomy).
Statistical Models
One of the key concerns of statistical analysis was potential biases caused by unobserved surgeon characteristics that could correlate with the outcome variable (ie, OT, LOS, or complications) and obesity status. Evidence suggests that health care providers might withhold certain treatments to obese patients because the treatments could be perceived by providers to be less effective on obese patients than normal-weight patients.16 Furthermore, some surgeon-specific characteristics (attending surgeon's teaching style, surgeon's experience) could explain a large amount of variation in operation time and discharge decisions. Many of these factors are unobservable or difficult to measure and might lead to biased estimates of the impact of obesity on OT or LOS if not accounted for in the analysis. To minimize potential confounding biases induced by surgeon characteristics, we used a set of surgeon dummy indicators to control for any time-invariant surgeon heterogeneity in the regression analyses. There were 8 individual surgeons who performed cholecystectomy, 12 who performed colectomy, and 5 who performed mastectomy during the study period.
To examine the association of obesity status with OT, LOS and complications, we first used Pearson correlation coefficients to examine strength of association of obesity status with the outcome variables for each of the 3 surgeries. We then used the ordinary least squares technique to regress the 3 outcome variables on patient obesity status. Other covariates included surgeon dummy, patient-level demographics, ASA class, and additional surgery-specific characteristics to control for patient case mix, as well as year dummy to control for secular trends. Concerned about the skewness of OT and LOS, we also explored the use of log-transformation on the 2 variables, but the estimated impact of obesity status on OT or LOS remained virtually unchanged (we do not report the log-transformed results in this study). Standard errors were adjusted via Huber standard errors correction.17 We used the Stata statistical software for all statistical analyses.18
RESULTS
Characteristics of the Samples
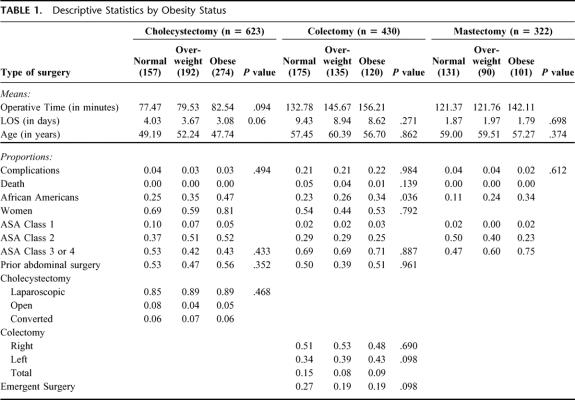
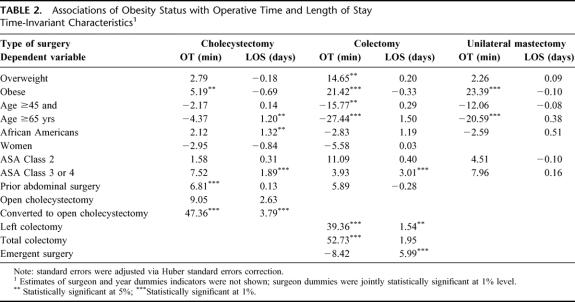
The 3 surgery samples contained 623, 322, and 430 patients for cholecystectomy, unilateral mastectomy, and colectomy, respectively. The proportion of obese patients was 44% in the cholecystectomy sample, 31% in the unilateral mastectomy sample, and 28% in the colectomy sample (Fig. 1). The descriptive statistics of each of the 3 samples were summarized in Table 1.
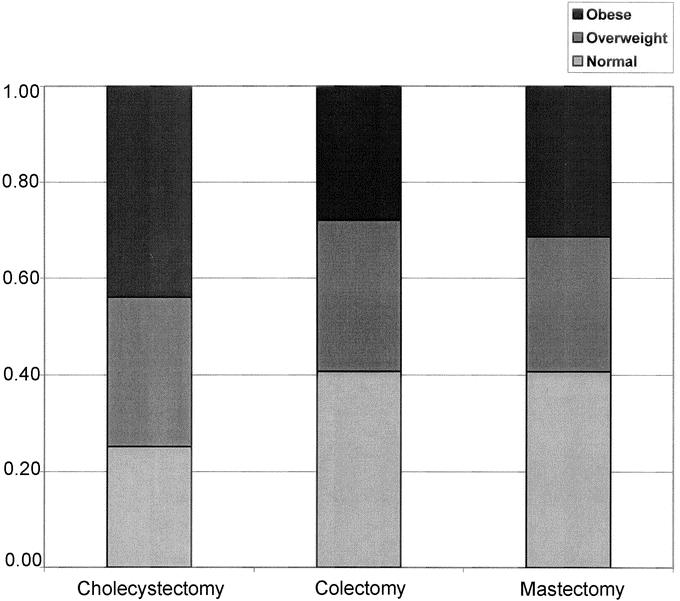
FIGURE 1. Proportion of subjects by obesity status for each surgical procedure.
TABLE 1. Descriptive Statistics by Obesity Status
Demographic covariates showed that obese patients were younger than normal or overweight patients, and the proportion of African Americans was the highest in the obese category in each of the 3 surgeries (Table 1). For example, among patients receiving cholecystectomy, the proportion of African Americans was 25% in the normal-weight category, 35% in the overweight category, and 47% in the obese category. There were no significant correlations between obesity status and ASA class, although the proportion of patients classified as ASA class 3 or 4 increased in each category of obesity status.
Unadjusted OT of obese patients was consistently longer than that of normal-weight patients for mastectomy and colectomy procedures (Fig. 2). Unadjusted associations of obesity status with LOS were not significant for any procedure (Fig. 3). There were no deaths in the mastectomy or cholecystectomy groups and 15 (3.5%) deaths in the colectomy group. Of these 15 deaths, 9 (60%) were patients in the normal BMI category, 5 (33.3%) in the overweight, and 1 (6.7%) in the obese categories. Complications occurred in 15 (or 3.5%) of those undergoing mastectomy, 11 (or 3.4%) of those undergoing cholecystectomy, and 93 (22%) of those undergoing colectomy. The unadjusted analysis of in-hospital complications and deaths did not demonstrate an association with obesity status for any of the 3 procedures. Due to the low rate of occurrences of morbidity and mortality, regression analysis was not performed for these variables.
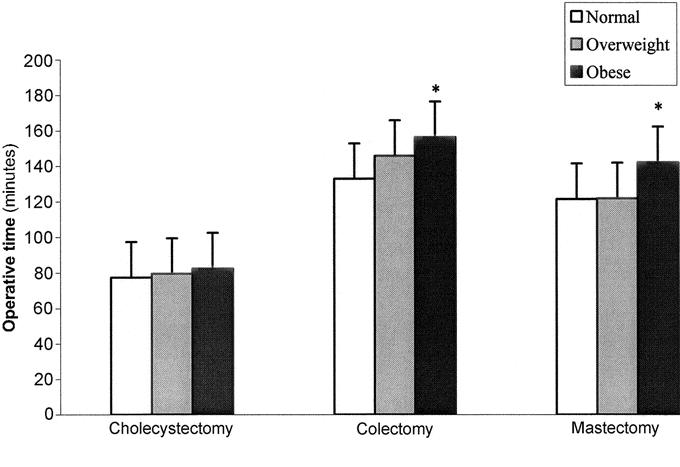
FIGURE 2. Unadjusted operative time by obesity status.
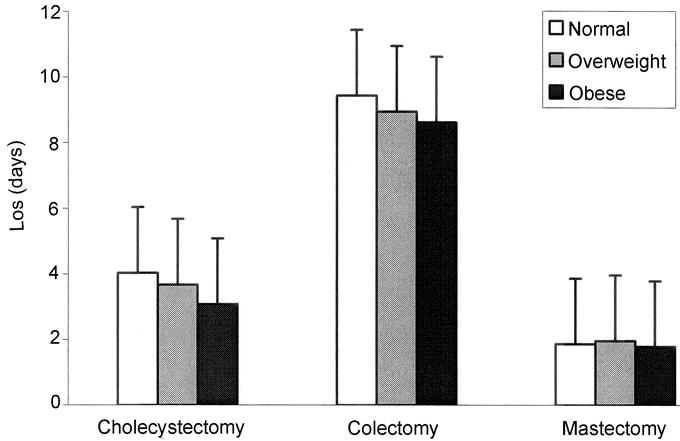
FIGURE 3. Unadjusted LOS by obesity status.
Multivariable Regression Analysis
The main regression estimates of the impact of obesity status on OT and LOS are summarized by procedure in Table 2. OT of obese patients was significantly longer than that of normal-weight patients (P < 0.01) for each of the 3 procedures, but differences in OT between normal and overweight patients were not statistically significant except for colectomy (P < 0.05). After adjustment for the covariates displayed in Table 2 and including dummy variables for each surgeon, obese patients had a mean additional 5.19 (95% confidence interval [CI], 0.15–10.24), 23.67 (95% CI, 14.38–32.96), and 21.42 (95% CI, 9.54–33.30) minutes of OT with respect to cholecystectomy, unilateral mastectomy, and colectomy. These numbers represented a 7% (ie, 5.19/77.47. =7%), 16%, or 20% increase in average OT compared with a normal-weight patient undergoing a respective surgery. LOS, adjusted for covariates, did not differ significantly by obesity status (P > 0.05) for each of the 3 surgeries.
TABLE 2. Associations of Obesity Status with Operative Time and Length of Stay Time-Invariant Characteristics
The estimated associations of age with OT and LOS showed that patients in more advanced age categories had shorter OT and somewhat longer LOS in comparison to patients under age 45 years old. In particular, patients at least 65 years of age required 27 minutes less OT (P < 0.01) to complete a colectomy. We further controlled for ICD-9 diagnoses (eg, colon cancer, diverticulitis, colitis, or Crohn), but the estimate of age persisted. ASA class was not associated with OT but was statistically significantly associated with LOS for cholecystectomy and colectomy (P < 0.01). The estimates of surgery-specific characteristics showed that conversion from a laparoscopic to an open cholecystectomy significantly increased OT and LOS in comparison to a laparoscopic cholecystectomy (P < 0.01), and an emergent colectomy did not affect OT but significantly increased LOS in comparison to an elective case (P < 0.01).
DISCUSSION
Our study found that patient BMI has a direct relationship with OT for all procedures studied (7% mean increase in time for cholecystectomy, 16% for colectomy, and 20% for unilateral mastectomy). We did not find any association of BMI with hospital LOS, major complications or mortality. Our data most likely underestimate the wound complications following surgical procedures because we did not capture complications that occurred after discharge. Most wound infections are not apparent for 5 to 10 days post surgery. Our median LOS was 3.5 days for cholecystectomy, 1.9 days for mastectomy, and 9 days for colectomy; therefore, our ability to capture wound infections was quite limited. Other studies have demonstrated increased wound complications in obese patients.7 Our data, however, concur with other studies demonstrating no increase in major complications or LOS for obese patients undergoing elective general surgery.7–9 These data are the first to focus on the impact of obesity on OT for multiple general surgical procedures. Previous studies have shown that obesity is associated with an increase in OT, but there were not adjusted for surgeon fixed effects.7,19–21
There are 3 main limitations of our study. First, this is a retrospective single institution study from a tertiary care center. These results may not be generalizable to other surgeons or institutions. Second, this study only analyzed 3 common surgical procedures. These procedures account for approximately 15% to 30% of a general surgeon's workload.13,14 Our results may not be generalizable to other operations. The third limitation is that our estimates of association between obesity and OT may be biased by other unobservable confounders. However, our findings were quite consistent for all 3 procedures and for all attending surgeons studied. The direct relationship between BMI and OT, as well as the consistent impact of BMI on all 3 procedures, suggests that this relationship is valid.
These data have significant implications for surgeons and healthcare delivery systems. We chose to study 3 common general surgical procedures used to treat obesity-related diseases: gallstones, breast cancer, and colon cancer. Increases in OT associated with these procedures affect the workload not only for surgeons but also personnel in anesthesia and nursing. Increases in costs related to OT increase the economic burden to hospitals and society.
Because obese patients spend more time in the operating room, this translates into an increased workload for anesthesiologists and perioperative nursing personnel. In an era where there is a nursing shortage, particularly with acute-care nurses, hospitals will have to increase salaries to attract and retain nurses.22,23 A shortage of anesthesiologists and certified registered nurse anesthetists has also been described.24 Our data demonstrate that at least for general surgery procedures, there will be an increased demand for their services due to an increase in time patients will spend in the operating room. Shortages of nursing and anesthesia personnel and increased demand for operating room time may lead to increased waiting times for surgery. A study done in Canada, where the resources are more fixed, demonstrated that lack of OR time did lead to significant delays in surgical treatment of cancer.25
Surgeon workload will increase substantially with the obesity epidemic. Not only will cases take longer but, based on the literature, there will be more cases. The obesity epidemic has already resulted in substantial increases in admissions related to gallstones, breast and colon cancer.26–28 If the current trend in obesity continues, more than 50% of Americans will be obese by 2020, leading to an increase in the prevalence of obesity-related diseases that will require surgical treatment.
Finally, the specific issue of prolonged OT is important for surgical reimbursement. Current reimbursement, based on relative value units (RVU), compensates surgeons a flat fee for the global period as defined by the third-party payer. When adjusted for inflation, the 2002 Medicare reimbursement for colectomy and mastectomy had decreased by 50% from the 1989 reimbursement rates.29 During the same time period, the prevalence of obesity doubled.1 Taken together, the impact of the obesity epidemic and decreasing reimbursement by third-party payers on surgeon salary is significant. Surgeons, in essence, are getting paid less to do more.
Other providers of healthcare are less financially impacted by the obesity epidemic. Obese patients have more clinic visits and, in general, have higher complexity of disease.30 Primary-care providers are compensated by visit and may be compensated at a higher level due to the complexity of the visit. In a survey of primary-care physicians, more than 50% of those who responded viewed obese patients negatively.31 Surgeons’ attitudes toward obese patients are not well characterized; however, anecdotal observations are that surgeons view obese patients as requiring more work. We propose that a CPT modifier for obesity be developed. BMI is a readily available, objective measure. Alternatively, the RVU assigned to surgical cases should be modified to account for the changing demographics and clinical characteristics, including obesity, of the surgical population. Recognizing and reimbursing surgeons for the additional time and effort necessary to care for obese patients would fairly compensate this group of healthcare providers for the additional burden caused by the obesity epidemic.
Obesity is an economic burden to hospitals, society, and, specifically, to surgeons. Our study found that obesity increased OT for each procedure studied. Further studies need to be done to determine if these effects are found for other procedures. Hospitals and surgeons need to be prepared for the increased surgery time necessary to care for obese patients.
Discussions
Dr. Edward E. Cornwell, III (Baltimore, Maryland): The authors have studied the surgical outcome in nearly 1400 patients undergoing 3 common surgical procedures.
The first observation that impressed me in this manuscript, which I was appreciative to receive well in advance for review, was that 36% of the patients in this study were obese and another 30% were overweight, reflecting an emerging epidemic as described by Dr. Vickers. The authors also an increased operative time of between 5 and 23 minutes for the various surgical procedures studied, but no differences in complications, length of stay, or mortality. Taken in the context of yesterday's presentation by Dr. Mabry and colleagues that defined surgical work as time times intensity, the case is made for the prediction of an increased workload for the general surgeon.
When one considers that reimbursements for surgical procedures over the last 2 decades have markedly decreased as patients’ weights have increased, the increased operative times have prompted the authors to point out that surgeons are getting “paid less to do more.”
First, in the largest group studied, that is the group undergoing cholecystectomy, obese patients were significantly younger than their skinnier counterparts. Is it possible that the lack of differences in length of stay or complications among the 3 different weight classifications is a result of the competing influences of heavier weight on the one hand and younger age on the other? The obese patients were younger, yet they have similar lengths of stay and complication rates. It would also be interesting to assess quality of surgery, for example, in obese patients undergoing colectomy for cancer in terms of numbers of mesenteric lymph nodes.
Secondly, isn't it possible in this era of outpatient care that a prospective analysis extending perhaps a couple of weeks beyond discharge might turn up different findings for the rates of complications such as deep venous thrombosis and wound infections? Complications such as these that are managed on an outpatient basis could potentially add to the burden of health care without increasing length of stay.
So far, the authors have nicely made the case that the epidemic of obesity is likely to extend the operative time for cholecystectomies, colectomies, and mastectomies by 5 to 23 minutes. It is entirely possible that a prospective study of the magnitude of common postoperative complications up to 2 to 3 weeks postdischarge may identify other differences that presently only weigh heavily on our minds.
Dr. Lazar J. Greenfield (Ann Arbor, Michigan): To me, the most impressive finding of this review is not the impact of obesity on operative time which most of us would have predicted, but the negative findings of no increase in complications or length of hospital stay. So the first question is whether this is a justifiable conclusion, in terms of complication incidence, without further information, as mentioned previously, on the postdischarge development of problems such as wound infection or venous thrombosis. Do you have any information on readmission rates for these late complications?
In addition to the challenges posed to surgeons by obese patients, anesthesiologists have to deal with difficult venous access and intubation. Do you know whether total OR time was further compromised by induction or extubation times? You have emphasized costs, but not included your own institutional costs. Since hospitals can charge based on OR time used, what additional costs are actually involved for the hospital and how much can be reimbursed?
Subsequent care of these patients requires more nurses for mobilization and possibly more attention from other caregivers such as respiratory therapists. Some of these costs can also be recovered by the hospital, and I wonder if total hospital charges differed by weight category.
Some of the findings seem unusual, such as shorter operative times for older patients and what appeared to be shorter length of stay for obese cholecystectomy patients, allowing the potential of other admissions for hospital cost recovery. What is your explanation for these differences? And was the relationship between ASA class 3 or 4 and longer length of stay for both colectomy and mastectomy patients, but not cholecystectomy patients, a function of age? And if you control for both age and ASA status, do you still have a difference in operative times?
The bottom line as characterized in the study is that this is probably an example of unreimbursed additional burden for surgeons, and payors certainly need to recognize the discrepancy and reward surgeons for their increasing ability to manage this growing problem.
Dr. J. Patrick O'Leary (New Orleans, Louisiana): It is sort of counterintuitive to think that obese Americans operated upon by surgeons don't have a higher complication rate. Certainly, wound complications are sometimes delayed in these patients and may not be diagnosed before discharge. Therefore, I was surprised by the duration. Could you expand on this observation?
Dr. Vickers, you also said that you were going to compare these by surgeons. Some surgeons do have a tendency to take care of folks who are a little bit heavier; therefore, did you look at your results with respect to the surgeons involved?
Dr. John O. Gage (Pensacola, Florida): As the authors very amply demonstrated, there is more work of the physician in operating on obese patients. However, I think when we are looking for modifiers, we are dealing with a government and an insurance industry that plays a budget-neutral game, and until obese patients make up a majority of those patients operated on for these disease processes, that if we do get a modifier, they will subtract that money paid for the obese patient from the normal patient. And while that remains the majority of those that we operate on, I think a majority of the audience may have a little difficulty in accepting that decrease for the increases granted those in the obese group.
Dr. Paul R.G. Cunningham (Syracuse, New York): I rise also to recognize that this is a critical issue for obese patients and the surgeons that take care of them across the nation. But I would also like to mention that perhaps we as a nation are on a learning curve in terms of treating obese patients. In the bariatric population that are undergoing obesity surgery, our lengths of stay have fallen from approximately 5 days 2 years ago to 2 or 2 and a half days. And I am wondering if Dr. Vickers has a comment about the experience at the university in terms of the falling length of stay with this challenging population of patients.
Dr. Mary T. Hawn (Birmingham, Alabama): I'd like to thank all the participants for their interesting discussion. First, I would like to address Dr. Cornwell's questions regarding our study.
In terms of what was the relationship between obesity and age with regard to length of stay and complications, given that obese people were younger than nonobese people in our study, we specifically tested for an impact of age with obesity in our multivariable regression models and did not find an interaction between age and obesity for length of stay or complication. But looking forward, as this young obese population ages, the impact operative time and therefore surgical workload are going to increase.
In terms of looking at stage of disease, we did not specifically look at number of lymph nodes in order to determine what the quality of the surgery was in our study. We did look at stage of disease and did not find any difference in stage of disease for the mastectomy or colectomy groups. It would be interesting to go back and look at lymph-node numbers because there have been reports in other procedures such as cystectomies that obesity does decrease the number of lymph nodes obtained in a surgical resection.
We did not find an association between BMI and complications. This result was surprising to us and it is surprising to many members of the Association. We definitely underestimated complications in this study because the length of stay for our mastectomy and cholecystectomy group was 3 days and our colectomy group was 9 days, and most wound complications will occur after that.
The problem with going back to the outpatient chart to estimate complications retrospectively is that it will not be an accurate estimate. We do need a prospective analysis to further understand this. The best way to do this analysis would be to use the National Surgical Quality Improvement Program (NSQIP) Database, which is a prospectively collected database in the VA and now in the private sector.
Unfortunately, BMI is not one of the variables collected in that database. We would put forth that BMI should be a variable that is collected by the NSQIP both in the VA and the private sector so that we could further understand the impact of obesity on postoperative complications.
Dr. Greenfield also had several additional questions regarding costs and charges. We specifically did look at costs and charges. Charges for operative time paralleled operative time for obese patients, and they were increased statistically in the obese population. However, overall, hospital charges were not different between the 2 groups.
Length of stay in the cholecystectomy group is somewhat biased because we could not include our outpatient cholecystectomies in this analysis; we were only looking at cholecystectomies that were done on the hospital side. The reason for that is we didn't have access: the records in the outpatient facility were not electronic during the study period. Due to this sample bias, we most likely underestimate the impact of obesity on operative time and length of stay in the cholecystectomy group.
I would just like to show you a slide of our cholecystectomy data broken down by procedure type. If you look at open cholecystectomy you can see that there is a significant effect of obesity on operative time, and, interestingly enough, as shown in blue, the laparoscopic cholecystectomy, there is a trend that obesity affects the time of a laparoscopic cholecystectomy as well.
To answer Dr. O'Leary's questions about the surgeon effect, these data were adjusted by surgeons in the multivariable model. The surgeon variable was statistically significant. We felt that this variable controlled for many immeasurable variables both in terms of teaching style and operative technique, as well as patient management style for length of stay.
To address Dr. Gage's comment that a CPT modifier will decrease overall reimbursement, there is a precedent set for reimbursing for extra time. Two examples are the CPT modifier for splenic flexure mobilization for colectomy and for mesh implantation at incisional hernia repair, and we suggest that there be consideration given to the CPT modifier for obesity. I just want to again emphasize as shown on this slide from Dr. Russell's, and I believe he is here, testimony to Congress in 2002 about the problems of decreasing reimbursement for surgical procedures over the last 14 years. And you can see for some of our procedures studies, colectomies and mastectomies, reimbursements have gone down by over 50% and at the same time obesity has doubled. This further magnifies the disparity in surgical reimbursement over the past 10 to 15 years.
Footnotes
Reprints: Mary T. Hawn, MD, MPH, KB 417, 1530 3rd Ave South, Birmingham, AL 35294. E-mail: mhawn@uab.edu.
REFERENCES
- 1.Mokdad AH, et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA. 2003;289:76–79. [DOI] [PubMed] [Google Scholar]
- 2.Mokdad AH, et al. Actual causes of death in the United States, 2000. JAMA. 2004;291:1238–1245. [DOI] [PubMed] [Google Scholar]
- 3.Finkelstein EA, Fiebelkorn IC, Wang G. National medical spending attributable to overweight and obesity: how much, and who's paying? Health Aff (Millwood). 2003;suppl:W3-219–226. [DOI] [PubMed] [Google Scholar]
- 4.Trakas K, Lawrence K, Shear NH. Utilization of health care resources by obese Canadians. CMAJ. 1999;160:1457–1462. [PMC free article] [PubMed] [Google Scholar]
- 5.Zizza CA, et al. Obesity affects nursing-care facility admission among whites but not blacks. Obes Res. 2002;10:816–823. [DOI] [PubMed] [Google Scholar]
- 6.Zizza C, et al. Length of hospital stays among obese individuals. Am J Public Health. 2004;94:1587–1591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dindo D, et al. Obesity in general elective surgery. Lancet. 2003;361:2032–2035. [DOI] [PubMed] [Google Scholar]
- 8.Thomas EJ, et al. Body mass index as a correlate of postoperative complications and resource utilization. Am J Med. 1997;102:277–283. [DOI] [PubMed] [Google Scholar]
- 9.Klasen J, et al. Increased body mass index and peri-operative risk in patients undergoing non-cardiac surgery. Obes Surg. 2004;14:275–281. [DOI] [PubMed] [Google Scholar]
- 10.Perez AR, Moncure AC, Rattner DW. Obesity adversely affects the outcome of antireflux operations. Surg Endosc. 2001;15:986–989. [DOI] [PubMed] [Google Scholar]
- 11.Langer C, et al. Prognosis factors in incisional hernia surgery: 25 years of experience. Hernia. 2004:EPub ahead of print. [DOI] [PubMed]
- 12.Etzioni DA, et al. The aging population and its impact on the surgery workforce. Ann Surg. 2003;238:170–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu JH, et al. The increasing workload of general surgery. Arch Surg. 2004;139:423–428. [DOI] [PubMed] [Google Scholar]
- 14.Ritchie WP Jr, Rhodes RS, Biester TW. Work loads and practice patterns of general surgeons in the United States, 1995–1997: a report from the American Board of Surgery. Ann Surg. 1999;230:533–542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Seidell JC, Flegal KM. Assessing obesity: classification and epidemiology. Br Med Bull. 1997;53:238–252. [DOI] [PubMed] [Google Scholar]
- 16.Evans JS, Dennis I, Dean J. General practitioner's tacit and stated policies in the prescription of lipid-lowering agents. Br J Gen Pract. 1995;45:15–18. [PMC free article] [PubMed] [Google Scholar]
- 17.White H. A heteroskedasticity-consistent covariate matrix estimator and a direct test for heteroskedasticity. Econometrica. 1980;48:814–838. [Google Scholar]
- 18.Stata Statistical Software. College Station, TX: StataCorp; 2003. [Google Scholar]
- 19.Gatsoulis N, et al. Laparoscopic cholecystectomy in obese and nonobese patients. Obes Surg. 1999;9:459–461. [DOI] [PubMed] [Google Scholar]
- 20.Efron JE, et al. Restorative proctocolectomy with ileal pouch anal anastomosis in obese patients. Obes Surg. 2001;11:246–251. [DOI] [PubMed] [Google Scholar]
- 21.Perka C, et al. The influence of obesity on perioperative morbidity and mortality in revision total hip arthroplasty. Arch Orthop Trauma Surg. 2000;120:267–271. [DOI] [PubMed] [Google Scholar]
- 22.Spetz J. Hospital nurse wages and staffing, 1977 to 2002: cycles of shortage and surplus. J Nurs Adm. 2004;34:415–422. [DOI] [PubMed] [Google Scholar]
- 23.Spetz J, Given R. The future of the nurse shortage: will wage increases close the gap? Health Aff (Millwood). 2003;22:199–206. [DOI] [PubMed] [Google Scholar]
- 24.Rowland RG, Wofford DA. Are you prepared for a shortage of anesthesia providers? Healthc Financ Manage. 2003;57:66–70. [PubMed] [Google Scholar]
- 25.Simunovic M, et al. A snapshot of waiting times for cancer surgery provided by surgeons affiliated with regional cancer centres in Ontario. CMAJ. 2001;165:421–425. [PMC free article] [PubMed] [Google Scholar]
- 26.Brown WJ, Dobson AJ, Mishra G. What is a healthy weight for middle aged women? Int J Obes Relat Metab Disord. 1998;22:520–528. [DOI] [PubMed] [Google Scholar]
- 27.Pi-Sunyer FX. Medical hazards of obesity. Ann Intern Med. 1993;119(7 pt 2):655–660. [DOI] [PubMed] [Google Scholar]
- 28.Calle EE, Thun MJ. Obesity and cancer. Oncogene. 2004;23:6365–6378. [DOI] [PubMed] [Google Scholar]
- 29.Russell T. Statement of the American College of Surgeons to the Subcommittee on Health Committee on Energy and Commerce, U.S. House of Representatives. 2002.
- 30.Wee CC, et al. Influence of body weight on patients’ satisfaction with ambulatory care. J Gen Intern Med. 2002;17:155–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Foster GD, et al. Primary care physicians’ attitudes about obesity and its treatment. Obes Res. 2003;11:1168–1177. [DOI] [PubMed] [Google Scholar]