Abstract
Objective:
We will review the contribution to the Medicare Fee Schedule (MFS) by the techniques of intensity of work per unit of time (IWPUT), the building block methodology (BBM), and the work accomplished by the American College of Surgeons General Surgery Coding & Reimbursement Committee (GSCRC) in using IWPUT/BBM to detect undervalued surgical procedures and recommend payment increases.
Summary Background Data:
The MFS has had a major impact on surgeons’ income since its introduction in 1992 by the Centers for Medicare and Medicaid (CMS) and additionally has been adopted for use by many commercial insurers. A major component of MFS is physician work, measured as the relative value of work (RVW), which has 2 components: time and intensity. These components are incorporated by: RVW = time × intensity.
Methods:
This work formula can be rearranged to give the IWPUT, which has become a powerful tool to calculate the amount of RVW performed by physicians. Most procedures are valued by the total RVW in the global surgical package, which includes pre-, intra-, and postoperative care for a time after surgery. Summing these perioperative components into RVW is called the building block methodology (BBM).
Results:
Using these techniques, the GSCRC increased the values for 314 surgery procedures during a recent CMS 5-year review, resulting in an increase to general surgeons of roughly $76 million annually.
Conclusions:
The use of IWPUT/BBM has been instrumental to correct payment for undervalued surgical procedures. They are powerful methods to measure RVW across specialties and to solve reimbursement, compensation, and practice management problems facing surgeons.
This paper will review the contribution to the Medicare Fee Schedule by the techniques of intensity of work per unit of time (IWPUT), building block methodology (BBM), and the work accomplished by the American College of Surgeons in using IWPUT/BBM to detect undervalued surgical procedures and to correct payment for undervalued surgical procedures.
The Medicare Fee Schedule (MFS), which was first implemented in 1992, has had a broad impact upon all practicing physicians in America. It is the basis for fees that are paid for services provided to Medicare beneficiaries and is also used for payment by many third party-insurers as well. Despite its importance to surgical reimbursement, most surgeons know very little about the MFS, its history of development, or how fees are calculated for their most common procedures. This paper will review the development and evolution of the methodology used to construct the physician work component of the MFS, with special attention to 2 powerful tools: the measurement of intensity of work per unit time (IWPUT) and the building block methodology (BBM), which can be used with IWPUT to calculate physician work. The process has been refined by many groups, including the Centers for Medicare and Medicaid Services (CMS), the AMA/Specialty Society Relative Value Update Committee (RUC), the American College of Surgeons General Surgery Coding & Reimbursement Committee (GSCRC), and other national specialty societies. A robust methodology has been developed over this time period to combine the measurement of IWPUT with the BBM to calculate physician work during the global surgical period. This methodology allows us to measure and compare the resource-based work effort of physicians across a wide spectrum of specialties and allows us to more easily derive a value for work for a given global procedure or a single encounter. These 2 concepts (IWPUT and BBM) have been applied to a wide range of endeavors, including production of compensation packages for surgeons, calculation of relative reimbursement for newly developed procedures, improved practice management, and exploration of work estimation for nonglobal procedures and services.
What's in a Name? Intensity by Any Name Is an Important Metric
The measurement of work performed by physicians has evolved over the last 2 decades, and as that analytic work has progressed, the terminology for the metric of intensity of work has also changed. IWPUT has variously been used as the acronym for: 1) intraoperative work per unit time, 2) intraservice work per unit time, and 3) intensity of work per unit time. Generally, these terms are all interchangeable, provided that the work and time being measured is in the intraservice (intraoperative) portion of a CPT code. To avoid confusion with other published texts and articles, we will use IWPUT to stand for the IWPUT for either the intraoperative or the intraservice component of a given CPT code. We will conversely use work per unit time (WPUT) to describe the intensity of work per unit of time for the preoperative and postoperative time periods for procedural CPT codes and for the preservice and postservice periods of nonprocedural codes.
History of the Development of the MFS by CMS and Harvard
Prior to 1992, physician payment in America was based upon the concept of usual and customary reimbursement, in which payment was roughly proportional to the average charge submitted by providers in a given area.
In 1992, CMS implemented the MFS, which is a fixed payment system. The MFS contains a relative value unit (RVU) for every code that describes physician and provider services and procedures and is administered by CMS. Development of the concepts and methodology underlying implementation of the MFS was an immense undertaking with many facets, and the work of a research team at the Harvard School of Public Health (Harvard) was particularly important. This research team, in a cooperative agreement with CMS, spent many years in the mid- to late 1980s developing a resource-based relative value scale (RBRVS) for physician services that would become the basis of the MFS.1–3 The MFS includes Current Procedural Terminology (CPT) codes, alphanumeric HCPCS codes, and G codes. (Current Procedural Terminology code, American Medical Association. Health Care Procedure Coding System code. The level II HCPCS codes, which are established by CMS's Alpha-Numeric Editorial Panel, primarily represent items and supplies and nonphysician services not covered by the American Medical Association's Current Procedural Terminology-4 (CPT-4) codes; Medicare, Medicaid, and private health insurers use HCPCS procedure and modifier codes for claims processing. Level II alphanumeric procedure and modifier codes comprise the A to V range. “G” codes are temporary codes assigned by CMS, generally for new procedures or services.) There are 3 separate components to each RVU, which are assigned by CMS: the relative value for physician work (RVW), the relative value for practice expense (RVPE), and the relative value for malpractice insurance expense (RVMP). For each component, the assigned units are not absolute but are arranged in rank order relative to one another; thus, the phrase relative value units and relative value scale.
The formula for total RVU for each physician service or procedure is:
where RVU = total relative value, RVW = relative value of work, RVPE = relative value of practice expense, and RVMP = relative value of malpractice insurance expense. (The relative value for malpractice insurance expense (RVMP) is additionally adjusted by CMS-assigned geographic factors that take into account the differences in specialty malpractice insurance between different areas of the country.) It is the physician work component (RVW) that became the focus of investigation over this last decade by the various groups mentioned above.
Based on Harvard research, the following 4 dimensions of physician work are described by:
time
technical skill and physical effort
mental effort and judgment
psychologic stress
The Harvard team found that although the strongest predictor of physician work is time, the other 3 nontemporal dimensions of physician work, collectively called intensity, are critically important in determining the “relative” value of work across the spectrum of all physician services. Simply stated, work is equal to the time of service multiplied by the intensity of that service, or conversely, work divided by time equals intensity.
Global Period Concept
Physician work (RVW) can be further divided into 3 phases: preservice work, intraservice work, and postservice work (vide infra). The Harvard team also determined that the intraservice work proved to be the most variable as far as intensity of physician work. These components can each be divided by the time that it takes to perform that work component to yield another metric, which is a measure of the intensity of work per unit of time, and this number can be quite useful for many purposes. Definitions for each component of the global period are important to understand and are the following.
Preservice Period
For surgical services, the preservice period includes all usual physician services provided from the day before surgery until the operative procedure begins. For nonsurgical services, such as evaluation and management (E/M) services, preservice work includes preparing to see the patient, reviewing records, and communicating with other professionals.
Intraservice Period
For surgical services, the intraservice or intraoperative period includes all “skin-to-skin” (start of the skin incision until the incision is closed) physician work that is a necessary part of the procedure. For nonsurgical services, such as E/M services, the intraservice work includes the work provided while the physician is with the patient and/or family, or “face-to-face” time.
Postservice Period
For surgical services with a global period of zero days, the postservice period includes all postoperative care following skin closure, on the day of surgery. For surgical services with global periods of 10 or 90 days, the postservice work includes the same work as a surgical service with a global period of zero days, and, in addition, includes postoperative hospital and office visits within the assigned global period of 10 or 90 days. For nonsurgical services such as E/M services, the postservice work includes arranging for further services, reviewing results of studies, and communicating further with the patient, family, and other professionals, which may include written and telephone reports, as well as calls to the patient.
Calculation of Work
The Harvard researchers constructed the initial RBRVS by first investigating the resource inputs of physicians’ services and developing methods to measure them. In the first phase of their study, vignettes or descriptions of physicians’ services were developed for 372 services performed by 1 or more of 18 specialties. For intraservice work, a process of magnitude estimation was used to obtain relative value measurements by means of a survey. Magnitude estimation is a technique that ranks work in relation to a reference using a ratio scale. (For example, if the work of reference procedure A is given an arbitrary value of 100 on a scale of 0 to infinity, using magnitude estimation, surveyees would be asked to place procedures B through Z on this scale, relative to procedure A.) Pre- and postservice work values were then calculated from survey data of selected codes, using the survey's time (geographic mean) multiplied by an assigned intensity factor. These pre- and postservice data were then extrapolated to all codes.
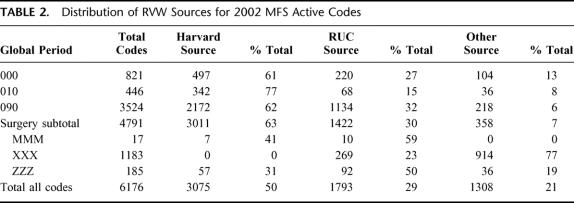
Although only 200 CPT codes were investigated through surveys in phase I of the study, by algorithms and extrapolation, the Harvard team developed a relative value scale for about 1400 codes. This combination of magnitude estimation for intrawork and extrapolation of pre- and postwork was the basis for recommendations for the initial RBRVS submitted to CMS as part of the phase I study. After phase I was complete, phase II focused on further review and development of values for global surgical services, using a newly adopted broader global-fee policy (that is, including postsurgery visits within 90 days after surgery). Work performed during phase II also determined that a well-organized, structured panel consisting of 11 to 14 physicians in a specialty can produce estimates of work that are quite similar to survey estimates from a larger sample. Phase III of the Harvard study focused primarily on using the small group process tested in phase II to generate RBRVS values for the remaining codes, for the revised E/M visit codes, and for other new code descriptors that had been developed by the CPT editorial panel after phase II was complete. Thus, by phase II of the Harvard study, emphasis was shifted to refinement of values by the small group process in contrast to the use of surveys of representative physicians used in phase I. This small group process is still in use today as a major tool to help evaluate RVW. Harvard Study Phase III report assigned intensities for pre- and postservice.4 Table 1 below includes this information, along with the intensity values (WPUT) rescaled to the current MFS (shown in parentheses).
TABLE 1. Intensity (W/T) of Pre- and Postsurgical Services, by Component, for Phase II and Phase III of the Harvard RBRVS Study
These intensity values are still important today as they are frequently used by the RUC, CMS, and specialty organizations to compare work between procedures and services. The intensity values are also used in the formula for the BBM, which will be presented and discussed below.
CMS Utilization of Work and Intensity Measures During the Refinement of the MFS
Intensity measures became a key issue for CMS following publication of the 1992 MFS because conflicting comments were received for RVWs assigned to E/M services. When the 1993 MFS was published, CMS announced its decision that the RVWs for E/M services should increase in a linear fashion so that the IWPUT would be the same for every code within a given family of E/M services, regardless of the duration of the visit.5 This conclusion is generally consistent with the findings of the Harvard study. The E/M RVWs were adjusted by multiplying the IWPUT for each family of E/M codes by the typical (face-to-face) time for each code to determine an intraservice work value (RVW-intra). The values for pre- and postservice work, determined to be a percentage of the intraservice work, were added to the RVW-intra to calculate a total RVW for each E/M service.
In the 1997 MFS Proposed Rule, the importance of IWPUT in the implementation and refinement of RVWs by CMS was again highlighted and reinforced by the agency's decisions.6 CMS rejected specific RVW recommendations for E/M services but agreed that the intensities of E/M services should be increased to bring them closer to the intensities of procedural services on the physician fee schedule. CMS also agreed that postservice work had increased over time and proposed to increase its fixed percentage of intraservice work. CMS followed a straightforward methodology in revising the RVWs for the E/M services. They assigned a revised IWPUT for each family of services by increasing the IWPUT developed in 1992 by 10%. Preservice and postservice work, as a percentage of the intraservice work, was increased by 25%. The net effect of this use of IWPUT during the first 5-year review was a redistribution of more than $2 billion, primarily to E/M services from all other services on the fee schedule.
In addition to the use of IWPUT to determine the RVW for E/M services, CMS has explicitly applied this methodology over the years to other services, including anesthesia, neurosurgery, hand surgery, reconstructive microsurgery, otolaryngology, pediatric surgery, vascular surgery, and ophthalmology. Based on a review of all MFS Proposed and Final Rules between June 1991 and November 2001, it is estimated that the RVWs for 576 codes are based on IWPUT calculations made by CMS. In addition, payments for 273 anesthesia codes under the anesthesia fee schedule are now based on the use of IWPUT. Together, the E/M and anesthesia services represented less than 5% of all codes but accounted for almost one third of the $53.5 billion in total Medicare Part B allowed charges in 2003. However, the RBRVS values established in phase III of the Harvard study remain an important part of the MFS. In 2001, the RVWs for more than 60% of surgical services were based on the Harvard RBRVS.
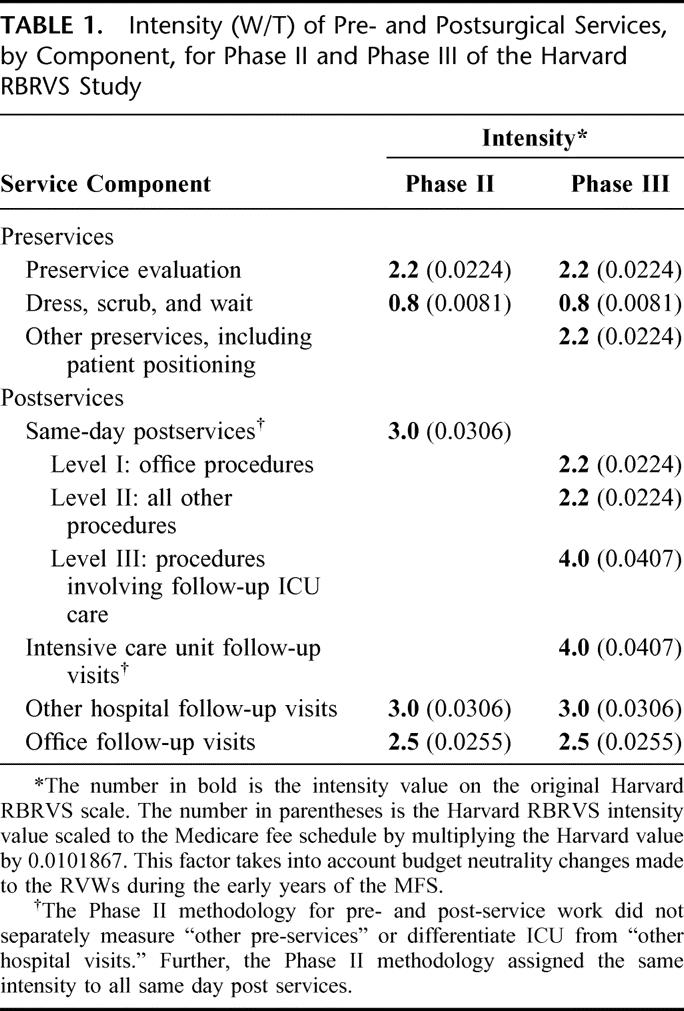
To gain a better perspective on the basis for valuation of work, Table 2 summarizes the source of RVWs for 6176 codes on the 2002 MFS. The RVWs for the codes in the column “Other Source” were developed primarily by CMS, generally as crosswalks from established codes, many of which are radiology services with relative values based on ranking from the American College of Radiology relative value scale.
TABLE 2. Distribution of RVW Sources for 2002 MFS Active Codes
Summary of the Development of the MFS by CMS and Harvard
It is clear that the MFS began with a study of magnitude estimation of physician work for a very limited number of services. However, to increase precision, the Harvard research team and CMS additionally used intensity, the BBM, and a predictive algorithm to calculate, extrapolate, and produce a fee schedule for all services.
RUC History and Process: How CPT Codes Have Been Valued by the RUC and CMS
The RUC was formed in November 1991 after a series of discussions between the AMA and the major national medical specialty societies regarding the planned implementation of the MFS. Currently, the RUC is composed of 29 members representing national physician/provider specialty societies, including the AMA, and 1 representative from the CPT Editorial Panel. The work of the RUC is supported by an advisory committee composed of representatives from more than 100 national specialty societies that have a seat in the AMA House of Delegates. The RUC meets 3 times each year to provide peer review of specialty society RVW recommendations for new and revised codes, prior to submitting recommendations to CMS. Additionally, the RUC assists CMS in the periodic review of RVWs for all CPT codes as required by law, every 5 years.
Specialty societies follow a well-defined process when developing RVW recommendations for new or revised codes prior to presentation to the RUC. After the CPT Editorial Panel accepts a new or revised code, all specialty societies are given the opportunity to conduct a survey to develop a recommendation for an RVW for the CPT code. Societies who choose to conduct a survey develop a list of services to be used as reference points or relative comparisons. The reference services are included in a customized survey that states the new procedure or service; describes a typical patient requiring this code or service; and asks for details of pre-, intra-, and postservice time, number of hospital/office visits, and complexity/intensity rating, all relative to a code chosen from the reference list. The survey statistical data (from at least 30 responses) are then reviewed by the specialty society's internal consensus committee to develop a specialty-recommended RVW. Two or more specialty societies may jointly survey and develop a recommendation for a code used by multiple specialties. The survey results and recommendations are then presented to the RUC, along with rationales for the recommended value. After deliberation and discussion, the RUC then votes on a value for a given CPT code, and these recommendations are then submitted to CMS. Upon receipt of the recommendations, CMS medical staff reviews them with the assistance of Medicare carrier medical directors, as needed. CMS publishes its decision on RVWs for new and revised codes in the Federal Register near the end of each year. These values take effect January 1 the following year as “interim” values. After a public comment period, and any necessary adjustments, they become final values.
MFS 5-Year Review Process: Use of Intensity to Value CPT Codes
In addition to annual updates reflecting changes in CPT coding, CMS is mandated by law to conduct a review of all RVWs at least every 5 years and make any needed adjustments to maintain relativity in the schedule. The success of the RUC's role in the annual updates has led CMS to seek assistance from the RUC in these 5-year review processes.
The RUC survey process for the first 2 5-year reviews (CY1995 and CY2000) has included the same basic methodology as the annual update process for new and revised codes, with some important innovations. First, a modified survey instrument was necessary because the 5-year review involved evaluating the work of established codes with established RVWs instead of new codes with no RVWs. In attempting to change the RVW for a given CPT code, specialties had to offer evidence/rationales that were judged compelling; for example, incorrect assumptions made in the initial valuation of the service, failure to include appropriate specialties in the initial valuation process, or large variations among codes in a code family caused by flawed methodologies used for initial valuation.
The RUC's first major use of intensity as a mechanism to value work came with the first 5-year review. The American Association of Neurologic Surgeons (AANS) conducted 2 major surveys: The first was a survey of high-volume neurosurgical key reference services to establish relative values for codes to be used as benchmarks or anchors within families of codes, and the second was a survey of key misvalued codes scattered among the neurosurgery codes that were then compared with the anchor codes. Operative log data were used for the intraservice time of many of the procedures surveyed, and the values for IWPUT were calculated using an algorithm based on the actual survey responses for estimates of intensity for each category of service (pre-, intra-, and postservice). The RUC accepted the entire AANS proposal to correct the alignment of all neurologic services. CMS accepted the RUC recommendation and made the recommended increases and decreases to the RVWs for neurosurgical services. Thus, the MFS RVWs for the majority of neurosurgical services is based upon use of both intensity measures, as well as operative log times.
The RUC also used IWPUT in the development of its recommendations for anesthesia services during the first 5-year review. The American Society of Anesthesiologists submitted a study that evaluated anesthesia work in relation to other services by partitioning an anesthesia service into 5 distinct components, assigning intensity values to these components based on the intensity values of benchmark procedures and multiplying anesthesia time per component by its corresponding intensity. The 5 defined components included preanesthesia, induction, procedure, emergence, and postanesthesia. CMS reviewed and accepted the RUC recommendations and increased the work for anesthesia services by 22.76%. Similar to the neurosurgery codes discussed above, the entire anesthesia fee schedule is based upon assigned intensity values.
In addition to these applications of an IWPUT methodology for revising the RVWs, there are more than 100 additional examples of services in orthopedics, cardiac surgery, general surgery, vascular surgery, urology, and cardiology where the RUC has made RVW recommendations based on the explicit use of IWPUT.7
After the First 5-Year Review: Adoption of Standard Intensity Measures for Preservice and Postservice Work for Global Services
Intensity has primarily been used to describe the work of the intraservice portion of a procedure. However, for global surgical procedures, a significant percentage of work may be included in the preservice or postservice periods. After the first 5-year review, attention was directed to refinement of the preservice and postservice periods and the WPUT intensity for each of those periods.
Preservice and Immediate Same-Day Postservice Work
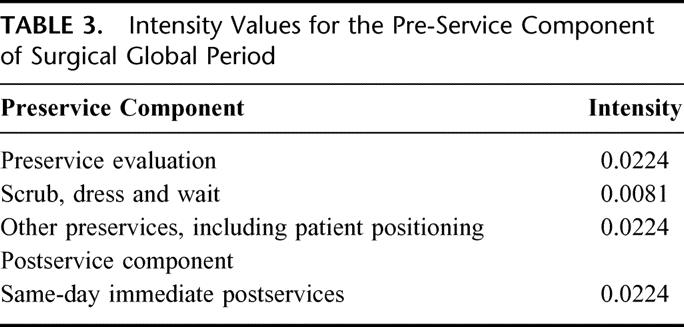
The current formula used by the RUC when calculating work in the preservice and immediate same day postoperative period is based on the findings of the Harvard RBRVS Phase III study8 utilizing the following intensities listed in Table 3.
TABLE 3. Intensity Values for the Pre-Service Component of Surgical Global Period
Postservice Work After the Day of Surgery
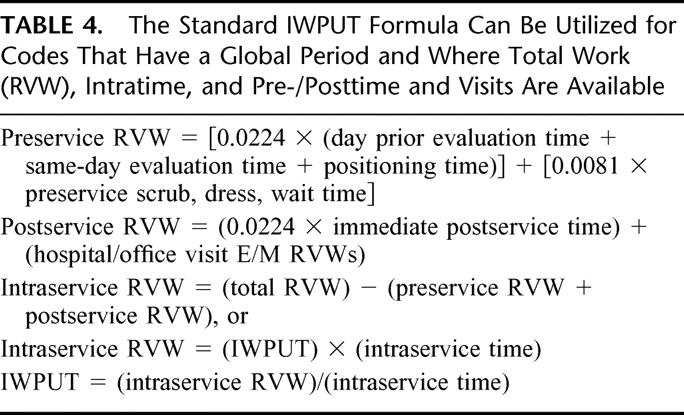
As noted earlier in this paper, E/M services were increased starting in 1997 as a result of the first 5-year review, based on an assigned intraservice intensity and an increase in pre- and postservice work (as a percentage of intraservice work for those services). CMS initially made no changes in the RVWs for global procedures that include E/M services in the preservice and postservice periods. However, the American College of Surgeons and many surgical specialty societies argued that the decision not to raise the RVWs for global surgical services unfairly penalized them. The College sponsored a more comprehensive survey to identify the number and level of E&M services provided as part of the global surgical package and won RUC and CMS endorsement that discrete E&M codes comprise the postoperative portion of the global package.9 In 2000, the American College of Surgeons presented a proposal to the RUC for a BBM developed by the ACS GSCRC. This methodology to “build” an RVW was based on the principles used by Harvard and CMS and included standard intensities for pre- and immediate postservice work and E/M RVWs for the postprocedure visits within a global period. The formula used for BBM is detailed in Table 4; however, the prime elements of the BBM are summarized by:
TABLE 4. The Standard IWPUT Formula Can Be Utilized for Codes That Have a Global Period and Where Total Work (RVW), Intratime, and Pre-/Posttime and Visits Are Available
The RUC agreed with this concept and adopted an important provision that formalized the process of utilizing the BBM to calculate an RVW. This decision is noteworthy because it acknowledged one of the important findings of the Harvard RBRVS study: that E/M services provided by surgeons during the postoperative period are comparable to other E/M services. Further, the BBM provides a means for calculating intraservice work and serves as a basis for identifying and correcting the RVWs for procedures where the postservice work is significantly undervalued. The following year, because of the changes to the E/M services and the evidence that the RVWs for global surgical services were developed using a BBM, the RVWs for all codes with a global period were increased to account for the E/M component within each. This 2001 increase in surgical fees corrected the inequity created in 1997 when CMS increased discrete E/M services, without increasing the E/M services in the global surgical period.10
Second MFS 5-Year Review: Use of IWPUT and BBM to Improve the Review Process
In preparation for the second MFS 5-year review, the ACS GSCRC used a Harvard-based BBM to review and calculate revised RVWs for global surgical services. The GSCRC used the BBM and an estimate of IWPUT in a large-scale review of general surgery codes that appeared to be misvalued from the time of the Harvard project. The GSCRC first divided the large number of codes into groups or families of related services and then identified a benchmark service (usually the highest volume code) within each family to serve as a reference (or anchor) point. Next, by consensus of a panel of surgeons familiar with the procedures, an IWPUT was assigned to each anchor service that was within the existing range of IWPUTs for all Medicare services. The IWPUTs of the anchor codes were aligned relative to each other (on a scale), and then the remaining codes were assigned IWPUTs within the range appropriate within and between families.
This consensus panel assignment and ranking of IWPUT was independently validated using a paired-comparison survey and analysis developed by statisticians at the University of Chicago.11 This validation further confirmed the early findings of the Harvard Study that a well-organized, structured panel consisting of 11 to 14 physicians in a specialty can produce estimates of work that are quite similar to survey estimates from a larger sample. The IWPUTs and Harvard time and visit data were analyzed to determine which general surgery services were misvalued and in need of refinement during the second 5-year review.
To expedite review of over 300 general surgery global services, 1 or 2 anchor codes in each family were surveyed using the standard RUC survey instrument and only time and visit information (a mini survey) were surveyed for the remaining codes in each family. Then, based on the results of the full RUC surveys for the anchor codes, and utilizing time and visit data and the IWPUT ranking developed for all general surgery services, the BBM was applied and revised RVWs for the non-RUC surveyed services were calculated.
Although the final proposal to the RUC included considerable discussion and statistical analysis that supported the use of survey and BBM in combination to address over 300 codes, the RUC determined that it would extrapolate recommended changes to the RVWs for the anchor codes to other codes in each family to retain the relativity in the existing MFS. A ratio of the recommended RVW for the anchor code to the then current MFS RVW for the anchor code was multiplied by the existing RVWs for the other codes in each family (where the RUC determined that the underlying rationale for changing the anchor code should apply to the entire family of services). This resulted in “family” RVW increases and decreases for many general surgery procedures. However, by ignoring the IWPUT ranking within families developed by small panel consensus and applying fixed percentage increases and decreases to entire families, the RUC perpetuated anomalies within and between families of codes. Despite these drawbacks, using the techniques of IWPUT and BBM, the GSCRC increased the RVWs for 314 general surgery procedures, resulting in an annual increase to general surgeons’ Medicare-allowed charges of approximately $76 million.
A similar approach to revising RVWs for families of codes was used by vascular and cardiac surgery for codes submitted for the second MFS 5-year review.12 After the second MFS 5-year review, the RUC submitted revised RVW recommendations for 870 services to CMS, who agreed with 93% of those recommendations.13
The Evolution of Work Measurement: Defining a Standard Intensity Formula and Approval of Other Alternate Work Measurement Methods
After the second MFS 5-year review, the RUC recognized the importance of intensity as a method for measuring work and ranking physician global services within and between specialties by formally adopting a proposal by the GSCRC to use the following formula to assist in review of the recommended RVWs for new and revised codes14 (Table 4).
As discussed above, the standard RUC method for developing RVW recommendations is to conduct surveys using a standard survey instrument. However, the RUC has also approved alternative ways to develop RVW recommendations. Valuing the incremental increase in work and application of payment rules are 2 additional approved methods for nonsurvey valuation of physician work.
Previously, the use of IWPUT and BBM had not been formally recognized as an alternative way to develop RVW recommendations, but instead was used “as a measure of relativity between codes or in families of codes.” As noted above, a review of the rationale for the 2000 RVWs included in the MFS shows that measures of intensity, such as IWPUT, have been used many times.15 At its September 2002 meeting, the RUC made an important advance: recognizing and approving the GSCRC's proposal for the use of intensity and IWPUT analysis as a third alternative method for developing RVW recommendations.
Going Into the Future With New Technology: Using IWPUT and BBM to Either Compare, Measure, or Generate RVW
Can IWPUT be Used to Detect Misvalued Services?
Over time, it has become clear that magnitude estimation for total work is not precise and that the most accurate comparison of physician work between specialties occurs when the comparison is divided into pre-, intra-, and postservice intervals.16
As shown with the BBM, calculating preservice and postservice RVWs is very straightforward. In contrast to the straightforward calculations for preservice and postservice RVWs, the calculation for the intraservice RVW is somewhat more complicated because the IWPUT of physician work between services within specialties and between specialties can vary widely. However, that same difference in IWPUT for seemingly similar services can become a marker or clue that a particular service is not valued correctly. Thus, a very useful tool to detect misvalued services within a family of services or between specialties is an aberrant IWPUT value. Because the preservice and postservice RVWs are generally standardized, the primary analysis to detect misvalued codes would involve detecting the variations of IWPUT between similar services or CPT families of codes.
In fact, in preparation for the second MFS 5-year review, CMS contracted with Health Economics Research (HER) to provide technical assistance, and their report supported the BBM approach. In their report, HER states: “The building block approach has several advantages, including simplifying the rating task for physicians by allowing them to focus on the work of a specific service component and comparing it to that of another service for the same component .... In addition to simplifying the rating of work, the building block approach has other advantages, including allowing greater flexibility in bundling and unbundling services for payment and providing opportunities for validating the components of work as a means of validating total work.”17
Can a RVW be Generated by the Use of IWPUT and the BBM?
In general, IWPUT values are either (1) estimated, (2) assigned, or (3) calculated. Estimation and assignment has traditionally been used to generate de novo values, while calculation of IWPUT has been used to check and validate the appropriateness of IWPUT values within and between families of codes.
Harvard, CMS, and the RUC have all assigned intensities at one time or another to calculate RVWs. Two important IWPUTs have been assigned, first by Harvard during their research, and later confirmed by CMS: (1) E/M services have an IWPUT of 0.031, and (2) intensive care management services have an IWPUT of 0.067.18 As an example of the BBM, if the intraservice time is known and the pre- and postservice work is known, then the total RVW can be quickly calculated by using the BBM formula if an IWPUT can be estimated or assigned.
There are 3 established methods for estimating and assigning the IWPUT for intraservice work: (1) survey, (2) consensus panel, or (3) paired-comparison study.19 All 3 methods are based on magnitude estimation, and anchor IWPUTs are usually established to check for validity. In 2002, the mean IWPUT for 4606 codes with a global period was calculated as 0.053, with a standard deviation of 0.032, which from a practical standpoint gives a range of IWPUT for most CPT codes of 0.021 to 0.085 (1 standard deviation).
How Can an IWPUT Be Calculated?
A variation of the BBM equation can also be used to calculate the IWPUT for a code. This calculation is accomplished by subtracting the pre- and postservice RVWs from the total RVW and then dividing the intraservice RVW by the intraservice time. This methodology is useful when developing a recommendation for a new service that must be compared with existing services or for reviewing the RVWs of existing codes. This calculation is particularly helpful to assess whether the RVW for a service is relatively and appropriately aligned with other services and their IWPUTs.
Other Future Applications of Intensity Measurement
We feel that incorporation of these various methods of measuring and calculating IWPUT will become commonplace in the coming years and may even replace the survey-based magnitude estimation method, in some cases. Based upon the evolution and refinement of physician work measurement that has occurred over the last 15 years, we foresee the following applications:
Increased used of the BBM to detect and correct anomalies existing in families of similar services.
Improved and simplified survey techniques, where new codes with similar preservice and postservice work compared with existing codes are surveyed only for intensity and time of the intraservice component.
Improved cross-specialty comparisons of intensity and work, utilizing comparisons of IWPUT to assure work equivalency.
Use of IWPUT and BBM in concert with large national databases that provide procedure time, hospital length of stay, and postoperative visits to generate more accurate RVWs.
Use of IWPUT and the BBM as a method to calculate physician compensation, resource allocation, and to help solve practice management problems for multispecialty organizations and clinics.
CONCLUSIONS
Summary of the History of the MFS and the Use of IWPUT and BBM
Based upon an extensive review of the Harvard study and actions of CMS and the RUC, we conclude the following regarding the measurement and use of work, intensity, and IWPUT:
Surveys of total physician work are not the only valid method for determining RVWs. The empirical findings from the original RBRVS research, as well as CMS refinement, have shown that structured comparisons of work per unit of time (intensity) have value in assessing the appropriateness of RVWs obtained from physicians’ judgments of work. This is particularly true when these comparisons are made within groups of clinically similar services and for comparable periods of the total service (eg, interservice versus intraservice). The work of the ACS GSCRC has emphasized and confirmed these findings.
Fixed-intensity values were assigned by the Harvard researchers to the pre- and postoperative components of surgical services, which were then multiplied by time to calculate pre- and postwork (time × intensity). The pre- and postwork were then summed and added to the intraservice work to obtain the total work estimate (ie, BBM). These values represent Harvard Study assigned intensity values which are still in use today by CMS and the RUC.
There is a common misperception that all surgical procedures on the MFS have gone through a formal RUC survey process. The RVWs for surgical services on the current MFS that are still based on the Harvard study (63% of total surgical services; see Table 2) are therefore not based on surveys of total physician work, because Harvard used a BBM that included work, time, and intensity.
CMS has explicitly used IWPUT as an integral part of the implementation and refinement of RVWs dating back to the first year of the fee schedule, when the RVWs for E/M services were established on the basis of IWPUT. Additionally, physician payments for E/M services, anesthesia, and many surgical services are based on the use of IWPUT. These services represented less than 5% of all codes, but accounted for almost one third of the $53.5 billion in total Medicare Part B–allowed charges in 2003. The net effect of this use of IWPUT during the first 5-year review was a redistribution of more than $2 billion, primarily to E/M services from all other services on the fee schedule.
The RUC has used intensity and IWPUT to develop RVW recommendations. Based on a review of codes that have gone through the RUC process through 2001, it is estimated that the RUC RVW recommendations to CMS for approximately 400 codes are based largely on IWPUT calculations. The value of these codes in 2001 represented $2 billion in allowed charges and $13 million in allowed claims.
The RUC has approved methods to develop RVW recommendations other than surveys, including the use of a standardized formula to calculate IWPUT and intraservice RVW.
After 15 years of research and experience regarding the development and refinement of the physician work component of the RBRVS, it may be possible to determine new RVWs for new procedures by surveying for time and visit information and applying the established standards for intensity for preservice and postservice work and assigning an IWPUT for the calculation of intraservice work. This use of the BBM would result in more precise RVWs than by a survey of magnitude estimation alone.
Using the techniques of IWPUT and the BBM, the GSCRC increased the values for 314 surgical procedures during a recent CMS 5-year review, resulting in an annual increase to general surgeons of roughly $76 million.
Discussions
Dr. Edward M. Copeland III (Gainesville, Florida): This paper catalogs the historical contributions made by the American College of Surgeons Coding and Reimbursement Committee and describes in detail the method by which surgical fees were initially derived and have recently been revised. Three authors have been awarded the Distinguished Service Award from the American College of Surgeons: Drs. John O. Gage, Josef E. Fischer, and LaMar McGinnis, Jr. The majority of the authors are now or have been regents or officers of the College and are actually sitting on the fourth row in this room right here today.
The Medical Fee Schedule was implemented in 1992, and general surgeons were late in challenging them. Several of the specialty societies, including the American Association of Neurological Surgeons and the American Society of Anesthesiologists, reviewed and revised their fee schedules, which were accepted and implemented. Prior to 1992, there was no organization to assume the responsibility for review of general surgery codes and fee schedules implemented by the Medical Fee Schedule. Certainly neither the General Surgery RRC nor the American Board of Surgery could do it, and prior to this time, the American College of Surgeons maintained that it was an educational organization that represented the interest of all of its members (an ideal that the ACS maintains to this date and will continue to maintain into the future). Therefore, the general surgeons were left with no representative body, and fee schedules for us reflected, in the minds of most general surgeons, this lack of representation. Other organizations such as the American Society of General Surgeons were formed and had as their platform the representation of general surgeons in an attempt to mimic the association and societal representation of our surgical specialty colleagues.
In 1992, the General Surgery Coding and Reimbursement Committee of the ACS took on the challenge of representing general surgeons in the coding and reimbursement arena. You have just heard some of the successes of this committee. The College has not been criticized by our specialty colleagues for this representation, and reimbursement by these specialties has not been negatively affected. Some may say it is “too little, too late.” We all know that it is never too late, and too little is now being appropriately addressed by the College. With the proper representation, general surgeons should receive a fair break from reimbursement organizations.
All of us owe a debt of gratitude to the authors and to others such as Dr. George Block for the hard work to accomplish these tasks. We must do our best to assure that general surgeons will not be fragmented by multiple organizations that deliver mixed messages to the government that either dilute or negate our growing influence.
Dr. Mabry, do other organizations that report to represent general surgeons in this arena help or hinder the work that the ACS Coding and Reimbursement Committee is doing?
Dr. William W. Turner, Jr. (Jackson, Mississippi): The authors of this paper are, as we all know, “household names” in the arcane world of physician payment policy. This is complex stuff, and its complexity matches directly the degree to which it is valuable to surgeons. This manuscript has to be read several times. The authors have reported the detailed and painstaking work that has gone into the succeeding iterations of the original work from the Harvard School of Public Health that gave us the RBRVS. The work of the General Surgery Coding and Reimbursement Committee of the American College of Surgeons has brought great value to surgeons, and we are grateful. I have 2 questions concerning the “cognitive” part of perioperative services and 1 question concerning the valuation of intraoperative work intensity.
The authors report the successes that have been achieved in defining the postoperative “cognitive” services that are imbedded in the global surgical package through a methodology that equates those services to the familiar E&M RVWs. The authors point out that CMS has assigned an IWPUT of 0.031 for E&M services that are of a non–critical-care nature. The imputed value of that portion of the global surgical package RVW related to postoperative care is determined by the time that it takes to render that aspect of care. Are the authors satisfied that postoperative care is now adequately relatively valued in comparison to the free-standing E&M codes in terms of work intensity and time components for preservice, intraservice, and postservice activities?
A decision for surgery, even that made the day prior to or the day of operation (billable under the 57 modifier) is billable as a separate E&M service. Is there “discounting” of such service in the imbedded preservice component of operative care?
Finally, we are approaching the third CMS-mandated 5-year review. With the second 5-year review, the AMA/Specialty Society RUC determined that they would extrapolate RVWs for anchor codes to other codes in families, retaining the relative value scale in the existing Medicare fee schedule. The authors point out that this resulted in an annual increase to general surgeons in Medicare-allowed charges of $76 million. Was there more money to be had in the original recommendations of the General Surgery Coding and Reimbursement Committee? Are there net gains in Medicare-allowed charges still to be had by a strategy for the upcoming 5-year review that includes a further attempt to use the IWPUT and the building block methodology to correct remaining inequities and those created by the RUC extrapolation process carried on in the second 5-year review?
Dr. Thomas R. Russell (Chicago, Illinois): I come up to also mention that this is an unusual paper to be accepted at the Southern Surgical. But yet this is critically important. And there is nobody in this audience today that isn't concerned about reimbursement. And as was pointed out yesterday by Dr. McDonald, the A.C.S. Governor, it is the number 1 issue affecting surgeons in this country.
You cannot carry on a safe, effective practice and do safe care running your offices or your department on a financial shoestring. We need to be appropriately compensated for what we do. We shouldn't be embarrassed about doing this kind of work.
As Ted Copeland pointed out, we were late in the game. This is not something that the College was used to doing. But we were thrust into this by the Omnibus Budget Reconciliation Act of ’88 which then led into the RBRVS of ’92.
Let me say a few things about the Coding Committee, or, as we affectionately call them at the College, the “codeheads.” Most of us, although interested in reimbursement, don't know very much about it. I read this paper 3 times last night, and it is still very difficult to get used to this “alphabet soup” of the language used in coding.
This reimbursement and coding committee is made up of knowledgeable, hardworking, and dedicated individuals who use consultants appropriately. I am in awe of the work they do for all of us. I think we all owe a real debt of gratitude for these volunteers.
The other worthy issue to point out is all specialties are involved. It is not just the surgeons but it is the pediatricians, it is the public health doctors, it is the internists. Everybody feels that they are disadvantaged and are being underpaid and undervalued for their work. Thus, we as surgeons need good representation.
And one question that I am often asked by fellows as I travel around the country is: What has the ACS done for me recently? I think this paper has one component of what we do.
I have a question. There is another big issue that is affecting reimbursement for surgeons today, and that is the drug costs, these expensive chemotherapeutic drugs that come directly out of part B. And I would like to ask Dr. Gage, who will be closing this paper, what effect do these costs have on the reimbursement of the surgical component?
Dr. John T. Preskitt (Dallas, Texas): Obviously, the College has not been in the position of advocating a decrease in the value of any of the codes, but in fact at the 5-year reviews there were some high-volume codes that went down in value. Why does this happen? Were they overvalued to start with? Or in fact do payers not recognize the fact that as we get a little faster in our procedures our intensity goes up? So why did those that did go down go down?
We have the largest number of unlisted codes in the book right now than we have ever had. Those of course have no RVUs associated with them. When we submit them, we have to beg for an evaluation. Would there not be a simplified methodology based on an agreed-upon IWPUT scale where we could submit and request a value? We know our times, those are documented, and we would simply have to agree on intensity.
Dr. A. Osama Gaber (Memphis, Tennessee): I want to congratulate the authors on this paper. I think transplant surgeons and the American Society of Transplant Surgeons recognize the work that the College has been doing on behalf of all surgeons, and the work through the College has resulted in adding new codes to some of our procedures. And I want to thank you for doing that for us.
The question now is what is the impact of using the building block methodology for specialty surgeons, surgeons like transplantation and bariatric surgeons, who have large amounts of work and time vested in pre- and postoperative care. The methodology puts a lot of value to such work, which in these cases is appropriate. Yet, since this is a zero-sum gain process and I don't know if the reimbursement is balanced just between all the surgeons or between all the various specialties, my question is, is using this methodology going to be detrimental to the specialties as we go through this? How are we going to avoid having a conflict in assigning these codes?
Dr. John O. Gage (Pensacola, Florida): I would like to thank all of the discussants for their very kind and generous remarks. Sometimes I think maybe everybody thinks that we on this committee own the pursestrings and the tension on the pursestrings of budget, which I can assure you is not the case and is not true.
However, I think as pointed out by Dr. Mabry and Dr. Copeland, 1992 was a critical moment in time. What really happened that made so many mistakes: the school of public health and Hsiao and the government had put so much money into a working analysis on how to value physician work. In my estimation what happened—the government disagrees with me; I can't imagine why—was that in 1992, Shou did all this work evaluating physician work. He had the numbers, the RVWs for work. The government took the usual and customary reimbursement dollars.
Let's take an example, an ophthalmologic code for cataract. Let's say Hsiao said that was 10 work-value units. In 1992, for simplicity's sake let's say the conversion factor was $32. So $320 was for work; 5% of the usual and customary reimbursement at that time was $2400; 5% of $2400 went into malpractice.
Immediately, somebody should have known something was wrong. You know, I have got $320 worth of work and we are paying them $2400 for a cataract. That doesn't fit you correctly. But they didn't do anything to change that. They didn't do the relevance of Hsiao’s work and make the fee schedule appropriately. They took the dollars, dumped it into the fee schedule, and made it fit the formula. So the money went into what excess column was left, practice expense.
That then started the problem where there was this gross inequity because it was all based on the usual and customary, which they didn't change, regardless of the fact of what Hsiao's work said they should have done. And that is what started the problem. That is what led us to the idea we had to do something to try and improve the problem; consequently, this paper.
Are there things that we can do? Do other organizations hinder or help us, Dr. Copeland? They help us now. ASGS has a member on our committee. And I think once they saw the detailed effort that went into the code and tried to get 1 value through the RUC, they have become an asset to help us and no longer hinder us. I don't think anybody hinders us. I think the College and the General Surgery Coding and Reimbursement Committee at the level of the RUC have developed an expertise that is well respected.
Dr. Turner asked 3 very important questions. The question I guess was, do we think that the E&M proponent of the building block methodology is fairly valued versus the standalone? A component of the building block methodology in the postoperative period only has a 15% reduction in the postservice work of the E&M, which is only minuscule in dollars. That was the only way to get the building block methodology accepted by the RUC. We accepted that 15% reduction. Is that a lot of money? No.
The one thing we don't have to worry about that the E&M standalones have to worry, we don't have to demonstrate medically documented in every record the intensity of documentation for the E&M level of service that we provide in the hospital and in the office that the primary care or standalone E&M code users have to do. That may be onerous, and because it may be a tradeoff, we decide, let's don't play that game, let's stay out of that arena, because we are doing fairly well.
The other question, with the modifier 57, does that discount the E&M? No, to our knowledge it doesn't.
And the third question, is there more money left in this arena and RBRVS in general surgery coding that was left hanging out because of the inappropriate way we think the RUC and CMS valued this in last 5-year review? Yes, we think there are some dollars there. And we think that there is value in going after those dollars: 5-year review process.
However, is that the place, as Dr. Russell alluded, the place that we should be devoting our efforts? I am not really sure there is a whole lot more value and dollars left in the work component. Forty-five percent of all reimbursement is in the practice expense arena. We haven't even touched the practice expense; 3.5% is in the malpractice arena. And I think general surgery and surgeons by and large are grossly undervalued in practice expense. And because it has 45% of all dollars in that column, we think that is where our efforts should go.
Dr. Russell brings up a question that is dear to my heart, and Dr. Townsend asked me to address the Board of Governors with the same question: Do I think codes that represent drugs are a problem and does that affect the fee schedule? It makes me cry how bad it affects the fee schedule.
We have taken medical oncologists and we have made them wealthy. The federal government in its infinite wisdom gave them that proverbial mask, the .357 Magnum, and a license issued by the federal government to steal. We give you permission, we endorse it, we license you to do it.
How do they do that? It is simple. They paid them actual wholesale price for the drugs that they were giving the patient. Well, let's say the drug cost $4000 a pop. They didn't buy it for the actual average wholesale price; they got it from the pharmacy company for 20% of that, 30% of that, 40% of that. Well, if it cost me $2000 to do an operation and I can find a way to do it for $500 and the patient will pay me $2000 for it, that is called profit. You stuff it in your pocket. These guys have been doing that for years. And then they cried, “Well, we can't treat cancer patients, they are all going to die.”
No, they can treat the patient if they want to get paid a nickel, we do it at 2 o'clock in the morning, or they come in shot in the chest or in the belly. And they don't come in with a wallet full of money and their insurance card. They don't even have a name. John Doe, almost DOA, but snatched from the jaws of death. We didn't say we can't treat them: just treat them for nothing. That is too bad, guys, that is the name of the game.
So, yes, it is a problem. It is costing millions. And it comes out of our pocket. The convergent factor that should go up goes down because their pockets get fatter. I am a little bit emotional when it comes to this.
Should there be an easier methodology? Sure there should, if we accept IWPUT and if this paper makes the RUC become more cognizant of the value of IWPUT and CMS. Should we use a simplified methodological approach? You know it. I know it. And we agree. Of course there should be. Will it happen? I don't know. We will do everything in our power to continue the work to hopefully make that a reality.
Footnotes
Reprints: Charles D. Mabry, MD, FACS, Department of Surgery, Slot 520, College of Medicine, University of Arkansas for Medical Sciences, Little Rock, AR 72201. E-mail: cdmabry@facs.org.
REFERENCES
- 1.Hsiao WC, et al. Resource-based relative values: an overview. JAMA. 1988;260:2347–2446. [PubMed] [Google Scholar]
- 2.Hsiao WC, Braun P, Becker ER, et al. A National Study of Resource-Based Relative Value Scales for Physician Services: Phase I Final Report to the Health Care Financing Administration. Boston, MA: Harvard School of Public Health; 1988. HCFA Contract No. 18-C-98795/1–03.
- 3.Hsiao WC, Braun P, Becker ER, et al. A National Study of Resource-Based Relative Value Scales for Physician Services: Phase II Final Report to the Health Care Financing Administration. Boston, MA: Harvard School of Public Health; 1990. HCFA Contract No. 18-C-98795/1–03.
- 4.Hsiao WC, Braun P, Becker ER, et al. A National Study of Resource-Based Relative Value Scales for Physician Services: Phase III Final Report to the Health Care Financing Administration. Boston, MA: Harvard School of Public Health; 1992. HCFA Contract No. 18-C-98795/1–03.
- 5.Health Care Financing Administration. Medicare program: fee schedule for physicians’ services for calendar year 1993: final rule. Fed Reg. 1992;57:55914. [PubMed] [Google Scholar]
- 6.Health Care Financing Administration. Medicare program: five-year review of work relative value units under the physician fee schedule: notice. Fed Reg. 1996;61:19991. [Google Scholar]
- 7.The use of intensity measures in the development of physician work relative value units (RVWs). Monograph presented to the AMA/RUC September 2002 by the American College of Surgeons and American Association of Neurological Surgeons.
- 8.Health Care Financing Administration. op. cit. November 22, 1996.
- 9.Mabry CD. In their own words: the five-year review, E&M services, and ACS leadership. Bull Am Coll Surg. 1998;83:41–45. [PubMed] [Google Scholar]
- 10.Mabry CD. On the cutting edge of reimbursement strategies: the ACS develops new techniques. Bull Am Coll Surg. 2000;85Q13–21. [PubMed] [Google Scholar]
- 11.Florin RE. Rasch analysis in measurement of physician work. J Outcome Meas. 2000;4:564–578. [PubMed] [Google Scholar]
- 12.Zwolak RM, Trout HH 3rd. Vascular surgery and the resource-based relative value scale five-year review. J Vasc Surg. 1997;25:1077–1086. [DOI] [PubMed] [Google Scholar]
- 13.Health Care Financing Administration. Medicare program: five-year review of work relative value units under the physician fee schedule: notice. Fed Reg. 2001;66:31027. [Google Scholar]
- 14.Action of the AMA Relative Value Update Committee (AMA RUC). Minutes available from the American Medical Association. 2002.
- 15.The use of intensity measures in the development of physician work relative value units (RVWs). Monograph presented to the AMA/RUC September 2002 by the American College of Surgeons and American Association of Neurological Surgeons.
- 16.Hsiao WC, Braun P, Becker ER, et al. A National Study of Resource-Based Relative Value Scales for Physician Services: Phase III Final Report to the Health Care Financing Administration. Boston, MA: Harvard School of Public Health; 1992:179, 215. HCFA Contract No. 18-C-98795/1–03.
- 17.McCall NT, Cromwell J, Griggs M, et al. Five year review of work relative value units: final report, HCFA prime contract no. 500-97-0443, task order no. 2004, June 14, 1999:171.
- 18.Health Care Financing Administration. Medicare program: five-year review of work relative value units under the physician fee schedule: notice. Fed Reg. 1996;61:20033. [Google Scholar]
- 19.Hsiao WC, Braun P, Becker ER, et al. A National Study of Resource-Based Relative Value Scales for Physician Services: Phase III Final Report to the Health Care Financing Administration. Boston, MA: Harvard School of Public Health; 1992:6–7. HCFA Contract No. 18-C-98795/1–03.