Abstract
Objective:
The purpose of this study was to review our experience with interfacility transfers to identify problems that could be addressed in the development of a statewide trauma system.
Background:
The fundamental tenet of a trauma system is to get the right patient to the right hospital at the right time. This hinges on well-defined prehospital destination criteria, interfacility transfer protocols, and education of caregivers. Patients arriving at local community hospitals (LOCs) benefit from stabilization and transfer to trauma centers (TCs) for definitive care. However, in the absence of a formalized trauma system, patients may not reach the TC in a timely fashion and may not be appropriately treated or stabilized at LOCs prior to transfer.
Methods:
Our facility is a level I TC and regional referral center for a compact geographic area without a formal trauma system. The Trauma Registry was queried for adult patients admitted to the trauma service between January 1, 2001 and March 30, 2003. Patients were divided into 2 groups: those received directly from the scene (DIR) and those transferred from another institution (TRAN). Medical records were reviewed to elucidate details of the early care. Data are presented as mean ± SEM. Continuous data were compared using Student t test, and categorical data using χ2. Transfer times were analyzed by one-way ANOVA.
Results:
A total of 3507 patients were analyzed. The TRAN group had a higher Injury Severity Score (ISS) (17.5 versus 11.0, P < 0.05), lower Glasgow Coma Score (GCS) (13.3 versus 14.1, P < 0.05), lower initial systolic blood pressure (SBP) (130 versus 140, P< 0.05), and higher mortality (10% versus 79%, P < 0.05) than the DIR group. The average time spent at the LOC was 162 ± 8 minutes. The subgroup of patients with hypotension spent an average of 134 minutes at the LOC, often receiving numerous diagnostic tests despite unavailability of surgeons to provide definitive care. Severe head injury (GCS = 3) triggered more prompt transfer, but high ISS was underappreciated and did not result in a prompt transfer in all but the most severely injured group (ISS > 40). Some therapeutic interventions were initiated at the LOCs, but many were required at the TC. A total of 23 (8%) TRAN patients required critical interventions within 15 minutes of arrival; mortality in this group was 52%. Mortality among those requiring laparotomy after transfer was 33%.
Conclusions:
All but the most severely injured patients spend prolonged periods of time in LOCs, and many require critical interventions upon arrival at the TC. It is unreasonable to expect immediate availability of surgeons or operating rooms in LOCs. Thus, trauma system planning efforts should focus on 1) prehospital destination protocols that allow direct transport to the TC; and 2) education of caregivers in LOCs to enhance intervention skill sets and expedite transfer to definitive care.
The establishment of a regional trauma center has increased the number and the severity of patients transferred to our tertiary center from outlying hospitals. Unfortunately, the lack of an organized statewide trauma system is associated with excessive emergency room times at the outlying hospitals, and many transferred patients arrive at our trauma center unstable.
Trauma care in the United States has progressed dramatically since 1976, when a plane crash involving an orthopedic surgeon and his family in rural Nebraska showed how poorly prepared both prehospital and hospital-based personnel were to handle victims of trauma.1 Development of prehospital care services and the creation of trauma centers had started a decade earlier with the publication of Accidental Death and Disability: The Neglected Disease of Modern Society, but this accident highlighted how these initial efforts had not reached their intended goal throughout the United States.2 The federal government's interest in improving trauma care is shown by the passing of the National Highway Safety Act of 1966 and Emergency Medical Services System Act of 1973, which authorized and funded development of systems to transfer injured patients to definitive care centers in a timely manner.3 The leadership role of the American College of Surgeon's Committee on Trauma's (ASC/COT) ATLS program and trauma center verification process has been critical in centralizing critically ill trauma patients in these trauma centers, which has resulted in improved outcomes.4–6
Unfortunately, development of prehospital and institutional trauma center care did not always grow in a coordinated manner. Development of statewide or regional trauma systems has been proposed to address this shortcoming. These systems ensure that patients are delivered to a facility with the appropriate level of resources in a timely manner. In communities without a trauma system, formal protocols for prehospital triage by Emergency Medical Service (EMS) providers are often absent and there are no formal lines of communication between community hospital and trauma center physicians. These deficiencies are likely to lead to transport of severely injured patients to facilities that are poorly equipped to treat the patient, where care may be substandard and outcomes compromised. The patient must then be transferred to a trauma center, resulting in a significant delay until institution of definitive care. Similarly, transport of patients with minor injuries to the trauma center may overload the center and reduce its efficiency. The absence of a coordinated state or regional trauma system makes it difficult to recognize the problems and develop solutions to solve them. The institution of formalized trauma systems addresses many of these flaws and has led to improved injury-related morbidity and mortality.7,8
Whether severely injured patients should be transported directly to a level I trauma center or whether they can be safely stabilized at community hospitals or level III/IV trauma centers and then transferred to a trauma center is still debatable.6,8–10 If severely injured patients are initially transported to a hospital not properly equipped to care for the patient, the initial stabilization needs be done quickly with good communication between the community hospital and the trauma center physicians and plans made for prompt transfer. Local factors such as the geographic distances between accident site and closest local hospital or tertiary care trauma center pose different challenges to each region of the country. Patients in regions where transport time is greater than one hour would certainly benefit from admission to a local community hospital for stabilization and interventions before transport to definitive care. However, patients in regions where transport times are less than 30 minutes may benefit by bypassing smaller, nondefinitive care facilities. We attained level I verification from the ASC/COT in 1995 but have noticed that many patients arrive at our center after inordinate delays and are often insufficiently stabilized. We sought to examine the process of transferring severely injured patients in our small geographic referral area to identify problems in our immature state trauma system that might be improved as we began the process of state trauma system development.
PATIENTS AND METHODS
The state of Rhode Island is 1045 square miles and has a population of just over 1 million, which is concentrated around the greater Providence area. The average driving distance to Rhode Island hospital (RIH) is 21 miles, and the average driving time is 28.5 minutes by passenger vehicle. A total of 80% of Rhode Island's population live within a 20-minute driving radius of RIH and 100% live within a driving radius of 50 minutes. Twenty-four hospitals transferred patients to RIH during the time of this study. None of these local hospitals possesses any level of trauma designation. The availability of an on-call surgeon varies, but none has an in-house surgeon. Some of these facilities have an operating room available on call 24 hours per day, while others have no operating room availability after daytime hours. In contrast, RIH has an in-house trauma attending and operating room facilities available within 5 minutes of arrival. RIH is a 719-bed acute care facility serving the entire state of Rhode Island, portions of southeastern Massachusetts, and eastern Connecticut. It is the only designated trauma center in this region. Our state has no centralized trauma system for injured patients but instead relies on scene EMS transportation protocols, which recommend transfer to our center for patients with severe injury if transportation time is less than 20 minutes but allows for transport to the nearest medical facility in patients injured outside this 20-minute radius. Rhode Island currently has 88 licensed EMS transportation agencies, a majority of which are based in fire departments. Of the approximately 100 rescue and ambulance squads in the state, only 5 to 10 have capacity for computerized data collection.
The Trauma Registry at Rhode Island Hospital was queried for adult patients admitted to the trauma service between January 1, 2001 and March 30, 2003. Patients were divided into 2 groups: those received directly from the scene (DIR) and those transferred from another institution (TRAN). The medical records including EMS, transferring hospital, and RIH records were reviewed for demographic, anatomic, physiologic data such as age, gender, Glasgow Coma Scale (GCS), Injury Severity Score (ISS), injuries, heart rate, respiratory rate, and blood pressure. Other data abstracted included emergency department time at referring hospital (EDT), interventions at referring hospital and RIH, and mortality. Comparison between groups was performed by unpaired Student t test and χ2 analysis as appropriate. Transfer times were analyzed by one-way ANOVA. Multivariant analysis was performed by logistic regression analysis (Statistica for Windows 5.1, 1997).
RESULTS
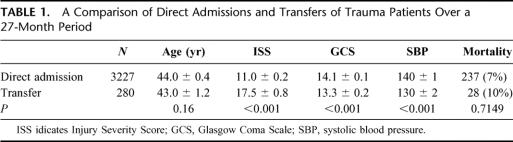
The issue of trauma transfers is an increasingly pressing problem. The establishment of our hospital as a level I trauma center in 1995 has been associated with an increasing number of transfers to our facility. For the 4 years before our level I designation, we averaged 348 patient transfers a year; yet in the 4 years after our designation, we averaged 426 transfers a year. In addition to the increased numbers of transfers, we have seen an increase in the severity of injury at our center. The State of Rhode Island Department of Health discharge diagnosis code database showed that from 1998 to 2002 Rhode Island Hospital shouldered an increased percentage of state's trauma patients with an ISS > 15 (Fig. 1).
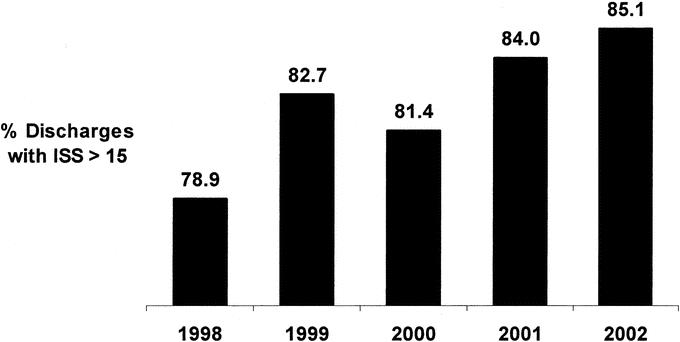
FIGURE 1. Patients discharged from RIH with a diagnosis of trauma and an ISS > 15 expressed as a percentage of total state of Rhode Island hospital discharges.
From January 1, 2001 to March 30, 2003, 3702 adult trauma patients were admitted to RIH. In 205 patients, the medical record contained insufficient data for evaluation or the patients were dead on arrival, leaving a total of 3507 patients for evaluation: 3227 direct admissions and 280 transfers. The average transport travel time was less than 30 minutes, with a range of 8 to 120 minutes. Recent Rhode Island Department of Health analysis of EMT crew run sheets show that 91.0% of patients were transported from the scene to hospital in less than 20 minutes and 96.1% are transported in less than 25 minutes. The mean time spent at the transferring hospital (EDT) was 162 minutes.
The direct admission group was compared with the transferred group: the groups were similar in age, but the transfer group was more severely injured, had more severe head injury, and had lower admission blood pressure (Table 1). Not surprisingly, the transfer group had a higher mortality, but this did not attain statistical significance.
TABLE 1. A Comparison of Direct Admissions and Transfers of Trauma Patients Over a 27-Month Period
Time spent at the transferring hospital was examined as it related to GCS, ISS, and type of injury. Patients with lower GCS tended to spend less time at the referring hospital with patients with a GCS < 3 spending an average of 110 minutes (P = 0.009; Table 2). The most severely injured patients, those with ISS > 40, did spend less time at the transferring hospital; however, other than this extremely injured group, the more severely injured patients were not triaged more promptly (P = 0.029; Table 3). One subgroup of severely injured patients, those with a documented episode of hypotension, also spent a significant amount of time at the referring hospitals, despite having an average GCS of 8.1 ± 0.9 and an ISS of 29.6 ± 3.3. In comparison to the normotensive patients, the hypotensive transfer patients did not have a significantly shorter EDT (167.1 versus 134.3, P = 0.11; Table 4). This cohort of patients had a mortality of rate of 38%. Patients with penetrating injury spent significantly less time in referring hospitals than patients with blunt mechanisms (P < 0.001; Fig. 2). This difference was not explained by differences in hemodynamic stability with rates of hypotension between the 2 groups essentially equal, 23% versus 16%, respectively.
TABLE 2. Time at Transferring Hospital (EDT) in Relation to Glasgow Coma Scale (P = 0.009)
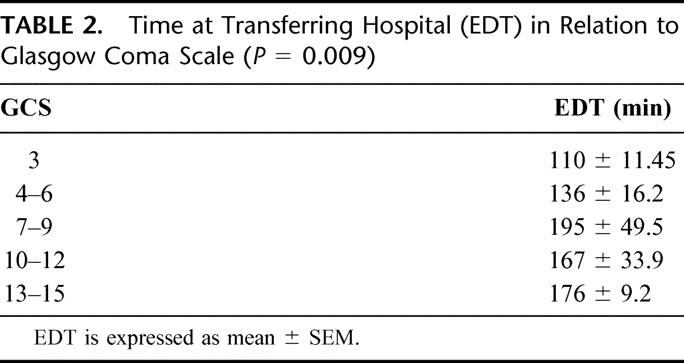
TABLE 3. Time at Transferring Hospital (EDT) in Relation to Injury Severity Score (P = 0.29)
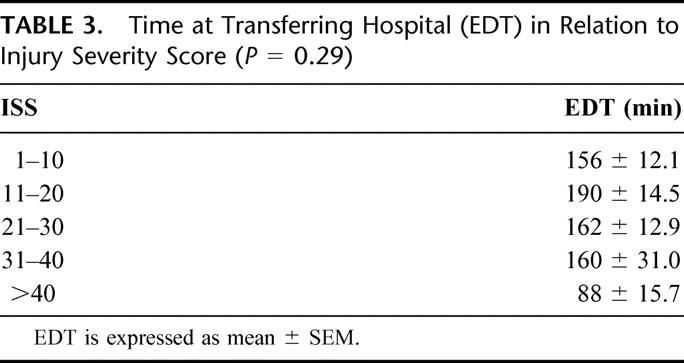
TABLE 4. Comparison of Hypotensive and Normotensive Patients Transported to RIH
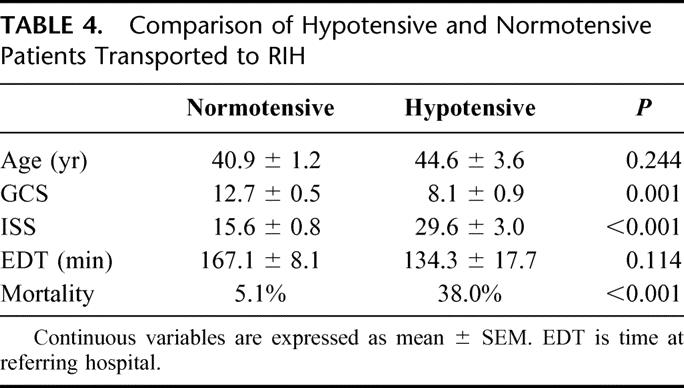
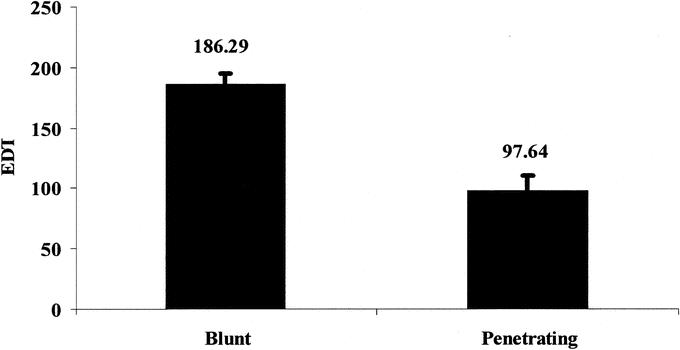
FIGURE 2. Time at transferring hospital in minutes (EDT) for patients with blunt or penetrating injury (P < 0.001). Error bars represent ± SEM.
Many factors may relate to the delayed transfer of patients to our trauma center. Patients transferred to our facility were severely injured and required multiple interventions at the outside facility. Ninety-five (31%) patients were intubated. Chest tubes were required in 31 (11%) patients. Blood transfusions were started in 30 (11%) patients and vasopressive agents begun in 6 (2%) patients. Three (1%) patients had laparotomies prior to transfer. While these interventions were warranted, patients had diagnostic testing, which may have slowed down the time to definitive care. Seven (3%) patients had aortic arch arteriography despite the nonavailability of a cardiothoracic surgeon at the referring hospital. Similarly, 99 (35%) patients had a CT scan of the head without neurosurgical support. Fifteen (5%) patients had CT scans of the abdomen with a documented period of hypotension. Most of these hospitals did not have a general surgeon promptly available. Finally, we discovered that interfacility transfer of patients necessitates the activation of a second ambulance crew since the town-based ambulance crews are not reutilized for interfacility transfer.
Despite an average time of 162 minutes at the referring hospitals, a significant number of patients required further interventions at our facility. Twenty-two (7%) patients required chest tubes and 28 (10%) patients had transfusions started for hypotension. Ten (4%) patients required thoracotomy and 20 (7%) patients required laparotomy. Many patients arrived unstable at our facility with 16 (6%) patients receiving blood transfusions for hypotension within 15 minutes of arrival. Within this same interval, 3 patients required chest tubes, 2 patients required laparotomy, and 1 patient required a thoracotomy. In this group of patients that received critical interventions within 15 minutes of arrival, the mortality rate was 52%.
Despite the inordinate delay in the outlying hospitals, there did not appear to be an association between EDT and mortality. Logistic regression analysis was performed for factors associated with mortality. The variables that entered the analysis in a statistically significant manner were age2 (P= 0.001), ISS (P = 0.001), and GCS (P = 0.004). EDT did not enter into the analysis in a significant manner (P= 0.120).
DISCUSSION
Trauma centers are well designed to care for injured patients because of physicians and support staff specially trained in trauma care, the presence of readily available multidisciplinary care specialists, commitment to quality improvement processes, and increased financial commitment to trauma care by these institutions. These commitments translate into improved outcomes.4,5,8,11 Since patients with severe injuries will have better outcomes at trauma centers, reduction of time to definitive care should improve patient outcomes. Patients that are directly transported to a definitive care facility have shorter hospital stays and lower mortality.8,9 The introduction of formalized trauma systems decreases mortality in injured patients.7
The establishment of a level I trauma center at RIH was associated with an increase in trauma transfers to our facility and an increase in the injury severity of these patients. This trend may be due to a tacit recognition of the improved care at centers of excellence. This same trend has been shown elsewhere, notably Delaware after establishment of their level I trauma center in 1998. The percentage of Delaware's severely injured patients cared for in their trauma center increased from 77% to 87% in the 5 years after verification. Unfortunately, the process whereby these patients arrive at our doors is not efficient and perhaps not even safe. In an immature trauma system, the lack of trauma protocols and guidelines makes the stabilization and transfer of injured patients an inefficient process. These inefficiencies may contribute to morbidity and mortality from delayed time to definitive care.
We analyzed data for consecutive transfers to our trauma center over a 27-month period. The mean time spent at the referring hospital was 162 minutes. Although patients with depressed levels of consciousness were quickly recognized and transferred for care, patients with evidence of other major injuries were not transferred in a timely fashion. Indeed, our data show that, as ISS increases up to a score of 40, the length of time spent in the referring hospital did not change. Only in this extremely injured group, ISS > 40, were transfers to definitive care more prompt. Patients with penetrating mechanisms were transferred more promptly than patients with blunt mechanisms, but even these patients spent an average of 97 minutes in the outlying hospitals. The reason for this delay in transfer of severely injured patients may be related to attempts at stabilization at the referring hospital, but frequently time was spent performing nontherapeutic testing. A number of patients were transferred with deficiencies in completion of their primary survey and basic testing. A review of trauma transfers in Wisconsin demonstrated numerous departures from standard ATLS guidelines, with 80% of patients with serious deficiencies in documentation or testing and 5% of patients with life-threatening deficiencies.12 Compliance with the ATLS guidelines of blood transfusion for hypotension and early transfer to definitive care for severely injured patients (ISS > 20 and GCS < 9) has been shown to independently improve outcomes.13 Improvements in mortality following institution of ATLS guidelines has been shown in developing nations.14 Mandating ATLS training for all emergency room practitioners improves compliance with ATLS standards and improves outcomes in patients with serious injury.15 The proficiency of the emergency staff at our referring hospitals is unknown. Currently, only 60% of Rhode Island emergency room physicians are emergency medicine board certified. The state does not mandate ATLS certification for emergency room physicians, and this lack of standardization may have factored into the treatment of our transferred patients. ATLS strongly advocates quick recognition of injuries and prompt transfer of patients found to overwhelm the facility's capacity. It is conceivable that the emergency room physicians often did not recognize the severity of injury, except for those patients with a severely depressed mental status or a penetrating mechanism of injury.
Attributing morbidity or mortality to the delayed transfers is difficult. While the transferred group had a higher mortality than our direct admission group, they also had a higher ISS. Multivariant analysis showed that age, ISS, and GCS determined survival, not EDT. Our multivariate analysis, however, is inadequate to detect differences in mortality. This evaluation of trauma transfers is not a randomized study; therefore, we cannot account for some potential selection bias created where transferred patients may have been selected for a better outcome in that they survived initial stabilization and transportation, while all the patients directly admitted to our hospital did not undergo this potential selection process. We feel that the excessive EDT at the outside hospitals do result in worse clinical outcomes. The instability of the transferred patients, as shown by the significant number of interventions done soon after arrival at our facility, may be a surrogate marker of this inadequate pretrauma center care.
Our experience is not universally applicable to all geographic areas. We are an extended urban environment with an average driving time of 25 minutes to our trauma center. A total of 100% of the population of Rhode Island is within a 50 minute driving radius. In this environment, stopping at a nontrauma center hospital for questions of instability may not be justified when an additional few minutes may get the patient to a definitive care facility. While a recent review of interfacility transfers in the urban environment of Seattle, Washington found no adverse clinical effects of initial transport and stabilization at level III or IV centers, those transferred patients had lower ISS and higher GCS than the patients directly admitted to their trauma center and may have been better able to tolerate time to transfer to definitive care. Their transferred patients spent an average of 186 minutes at the outlying hospital.10 Our transferred patients were much more severely injured than in the Seattle experience. Despite our experience in an extended urban community, a trauma system in a rural environment with transport times of 2 to 3 hours may certainly benefit from transportation to and stabilization at a level III or IV trauma hospital before transfer to definitive care.
We have been committed to developing a state trauma system in Rhode Island for over a decade. The Rhode Island Department of Health received federal funding as part of the 1990 Trauma Care Systems Planning and Development Act. The overseer of this grant established the Trauma System Advisory Committee (TSAC) which, with the Department of Health, is the main policy making body for trauma system planning. However, this initiative foundered when additional legislative authority for the Department of Health to oversee trauma development was not passed. The Department of Surgery at Brown attempted the creation of a voluntary trauma system in the late 1990s, but this attempt also failed. Recently, the TSAC asked for a trauma system consultative visit from the ASC/COT. The findings of this consultation were that a state trauma system did not exist and that existing legislative authority did give the Department of Health mechanisms to begin trauma system development. Their recommendations have been instrumental in our Department of Health beginning to tackle this issue. Our trauma task force is adopting guidelines for hospital trauma designation and triage protocols. Areas of greatest importance may be widening the catchment area for severely injured patients transported to Rhode Island Hospital from a 20- to a 40-minute radius. Mandatory ATLS training for all emergency medicine practitioners also is a high priority.
CONCLUSION
This review demonstrates shortcomings in the management of severely injured patients in a state without a trauma system. When transport times are relatively short between accident scene and trauma center as they are in our extended urban community, patients with severe injuries should be taken directly to a definitive care facility. Development of a state trauma system is necessary to improve the care of injured patients in our state.
Discussions
Dr. L. D. Britt (Norfolk, Virginia): The authors state that the group sizes were too small to allow for multivariate analysis to control for all factors. According to the manuscript that was sent to me, you had 280 patients in the TRAN group and 3327 patients in the DIR, the direct group. These would not be considered small numbers! Also, you do not have to control for all factors, only the ISS and a few other related to mortality. Why did you not identify these factors by performing a chi-square test with mortality and each of the other potential factors as categorical variables?
Also, the authors state that even a multivariate analysis could not account for potential biases between groups. Now, this is an inherent problem associated with analyzing observational data as opposed to data from design experiment, which sometimes has randomization. However, a multivariate analysis adjusting for relevant variables still should have been done.
Again, I enjoyed this paper. And it does support my bias. Hopefully you will be able to address those concerns.
Dr. J. Wayne Meredith (Winston-Salem, North Carolina): I enjoyed your paper, Dr. Harrington. And I think it makes a very important point that I would like many of us to take home. This is a well-run trauma center with readily available highly skilled surgeons present constantly. It is college verified. We know these facts to be true. There is, though, a degree of preventable injury, preventable death, which cannot be addressed by simply having a good trauma center in the middle of a population. That is the part where a trauma system comes in. These authors have looked at the ability of a trauma center to make that difference versus a trauma system to make that difference.
Just to place some order of magnitude of the difference, I draw your attention to Avery Nathens’ study, which looked at mature trauma systems and shows the death rate from motor vehicle crashes in states with mature trauma systems save lives on the order of magnitude, indeed slightly greater than the lives saved by placing a secondary violation seat belt law in a state.
So having a trauma system is an important thing. These authors have helped show that, and helped show partly why, that can be true. It is not that you need more patients, it is not that you need different patients, it is that you need your golden hour back in order to be able to save some of these lives.
The American College of Surgeons has created a Trauma System Consultation Committee and a Trauma System Consultation Process, which I appreciate that you highlighted some in this report. Just to bring that to your attention, this is available to any state or region. It is not a pass-or-fail system; it is a system that will help get the political process off top dead center and hopefully help move it along. And I would ask the authors if you found that to be helpful and if you think it will stimulate progress in your state. We hope that it will and intend for it to.
Another problem we see, and I would ask the authors if you have any insight into what creates this demand for delay, and specifically ask the question: Do you believe that a misinterpretation or intentional misuse of the EMTALA rules, laws, creates that. I believe we see it all across the country: commonly, folks who spend time with their patients doing more tests, taking more time, under the guise or under the misconception that patients must be stabilized more than they need to be.
I would also like to ask the authors how your trauma system, as you are proposing it, interfaces with your disaster preparedness plan in your state. I believe that the proper baseline for disaster preparedness is a proper state trauma system. And we need to be pushing this in all parts of our country.
Last, similar to what Dr. Britt asked, and this relates to the bias questions, have you done any preventable death analyses looking at these groups, which would be extremely helpful, or looked at the incidence of multiple organ failure, which would probably be your most sensitive indicator of problem and more sensitive than death as a difference in the outcomes.
Dr. Lewis M. Flint, Jr. (Tampa, Florida): Let me offer some comparative data from the Florida Trauma System. The Florida Trauma System has been a government-run and government-supervised system in the state of Florida for the last 23 years. Two other members of the Southern, Dr. Joseph Tepas and Dr. Larry Lottenberg, and I were commissioned by the state of Florida about 3 months ago to conduct a comprehensive assessment of the Florida Trauma System, and I would like to just share a couple of pieces of data from that study with you.
The Level 1 trauma centers in Florida see on average about 3300 trauma patients a year, and the average proportion of patients transferred from other facilities to the Level 1 trauma centers in Florida is about 38%. So over a third of our patients are transferred from outside facilities.
We are a mature trauma system. Does that solve the problem that you have identified? Categorically, no. So having a mature trauma system is not going to be the answer to your question. What does solve it? What does help?
We have mandatory ATLS training for every physician who has privileges to work in an emergency department in the state of Florida. Does that shorten the time to transfer? It does but not by much. The amount of time that we see patients spending in outside emergency departments is about 93 or 94 minutes. The average number of CT scans received by a patient in an outside hospital is slightly more than 2.
The problems that you have identified are not solved by ATLS training. Why? We think that the transfer process has something to do with it. We think it is important to make the transfer process easy.
Having RNs receive the transfer calls at a single number is helpful. We have found that if the emergency physician is able to talk to a surgeon at the initial hospital or at the receiving hospital, this advice shortens the time in the outside emergency department.
We think that the EMTALA law, because it is so difficult to interpret, has a great influence in keeping patients in emergency departments too long.
Finally, I think that the one thing that we have also found that helps is fairly elaborate air medical evacuation systems. If you have a helicopter available to go to the scene of an injury, then you don't have patients going to outside emergency departments.
The last thing I would say is that before you start going down the path to Level 3 and Level 4 centers, you should examine Rich Mullins’ data from the state of Oregon, which showed that those centers do not cause a decrease in trauma mortality.
Dr. David T. Harrington (Providence, Rhode Island): Dr. Britt, in regard to the questions as to why we did not do a multivariate analysis to assess the impact of delayed transfer on our clinical outcomes: as we looked at the groups of people who would most benefit from trauma center care, meaning ISS greater than 15 and therefore the group with potential survival benefit, our original 3000 study patients shrunk to a very small group that wouldn't allow for a multivariate analysis.
Second, I don't think we could ever overcome the selection bias inherent in the fact that the transfer patients had already spent over 2 hours at the referring hospital's emergency department. These patients therefore already have some selection bias. I don't think any amount of multivariate analysis would overcome that bias.
Dr. Meredith, you mentioned that we have a golden hour for the care of trauma patients. For our transfer trauma patients, unfortunately, it was actually a not-so-golden 3 hours because they spent an average of almost 3 hours at the outside hospital. We would like them at our hospital more promptly.
Your comments about whether we found the American College of Surgeons Committee on Trauma Consultation visit helpful: We found it extremely helpful. I think 3 things led our Department of Health to finally taking trauma system development seriously. One was our ACS/COT visit. The second was the Station fire, which was a conflagration at a nightclub called The Station in West Warwick, Rhode Island 2 years ago.
And third, the events of 9/11 solidified the idea that disaster management and emergency responses need to be taken seriously. The best disaster plan is a disaster plan you use every day, and a working state trauma system is an excellent disaster plan. The ACS/COT's consultation visit for trauma systems solidified and further legitimized the development of a trauma system in Rhode Island and really moved the process forward. Dr. Meredith asked what I felt was responsible for the delay in transfer. At least part of the delay is a poorly regulated pre-hospital system. Rhode Island has 88 ambulance crews. Some of them are town-based, some of them are hospital-based, and some of them are private ambulance services. The level of documentation of the pre-hospital course varies between these groups. Without this information, it is difficult to perform quality improvement on pre-hospital care. Also, when a town-based crew brings a patient to one of the outlying hospitals, they leave. If that patient later needs to be transferred from the outlying hospital to Rhode Island Hospital, the outlying emergency room has to mobilize a second ambulance crew for transportation. The time of that second mobilization may have prompted some of the unnecessary diagnostic testing that the outlying emergency room performed. Obviously, this is not an ideal way to care for the severely injured trauma patients.
Another issue that both Dr. Meredith and Dr. Flint mentioned is the EMTALA statutes. What is interesting here is that there is inherent conflict between EMTALA and Advanced Trauma Life Support (ATLS). The ATLS course states that if a patient outstrips your facility's ability to care for the patient, that patient should be transferred to the next highest-level facility as expeditiously as possible. The course teaches that delays will only worsen outcome and that once the patient has received care to the level of that institution's ability, yet the patient requires a still higher level of care, then the patient should be transferred. I also realize that many hospitals are concerned about the appearance of inappropriate transfers and the possibility that they could be accused of an EMTALA violation. I hope that the ATLS will win out in this debate.
However, the most obvious solution to the problem in a small geographical area such as ours is to get the sickest patients directly to our care and avoid the outlying smaller facilities.
As far as air crew: Dr. Flint, I don't believe our state, being so small geographically, with an average driving time of 35 minutes, would benefit from air ambulances. It certainly would be beneficial in a state the size of Florida. I think we could stack approximately 10 Rhode Islands in Florida and have some room left over.
Footnotes
Reprints: David T. Harrington, MD, Rhode Island Hospital, Department of Surgery, 593 Eddy Street, APC 443, Providence, RI 02903. E-mail: dharrington@usasurg.org.
REFERENCES
- 1.American College of Surgeons. Advanced Trauma Life Support for Doctors (ATLS) Student Course Manual, 7th ed. Chicago: American College of Surgeons, 2004. [Google Scholar]
- 2.Highway Safety Act of 1966, Public Law No. 89–564, 89 Stat. 3052.
- 3.Committee on Trauma, and Committee on Shock, Division of Medical Sciences, National Academy of Sciences/National Research Council (US). Accidental Death and Disability: The Neglected Disease of Modern Society. Washington, DC: National Academy of Sciences; 1966. [Google Scholar]
- 4.Demetriades D, Berne TV, Belzberg H, et al. The impact of a dedicated trauma program on outcome in severely injured patients. Arch Surg. 1995;130:216–220. [DOI] [PubMed] [Google Scholar]
- 5.Nathens AB, Jurchovick GJ, Maier RV, et al. Relationship between trauma center volume and outcomes. JAMA. 2001;285:1164–1171. [DOI] [PubMed] [Google Scholar]
- 6.Rogers FB, Osler TM, Shackford SR, et al. Population-based study of hospital trauma care in a rural state without a formal trauma system. J Trauma. 2001;50:409–413; discussion 414. [DOI] [PubMed]
- 7.Mullins RJ, Veum-Stone J, Helfand M, et al. Outcome of hospitalized injured patients after institution of a trauma system in an urban area. JAMA. 1994;271:1919–1924. [DOI] [PubMed] [Google Scholar]
- 8.Sampalis JS, Denis R, Lavoie A, et al. Trauma care regionalization: a process-outcome evaluation. J Trauma. 1999;46:565–579; discussion 579–581. [DOI] [PubMed]
- 9.Young JS, Bassam D, Cephas GA, et al. Interhospital versus direct scene transfer of major trauma patients in a rural trauma system. Am Surg. 1998;64:88–91; discussion 91–92. [PubMed]
- 10.Nathens AB, Maier RV, Brundage SI, et al. The effect of interfacility transfer on outcome in an Urban Trauma System. J Trauma. 2003;55:444–449. [DOI] [PubMed] [Google Scholar]
- 11.DiRusso S, Holly C, Kamath R, et al. Preparation and achievement of American College of Surgeons level I trauma verification raises hospital performance and improves patient outcome. J Trauma. 2001;51:294–299; discussion 299–300. [DOI] [PubMed]
- 12.Martin GD, Cogbill TH, Landercasper J, et al. Prospective analysis of rural interhospital transfer of injured patients to a referral trauma center. J Trauma. 1990;30:1014–1019; discussion 1019–1020. [DOI] [PubMed]
- 13.Hedges JR, Adams AL, Gunnels MD. ATLS practices and survival at rural level III trauma hospitals, 1995–1999. Prehosp Emerg Care. 2002;6:299–305. [DOI] [PubMed] [Google Scholar]
- 14.Ali J, Adam R, Butler AK, et al. Trauma outcomes improves following the advanced trauma life support program in a developing country. J Trauma. 1993;34:890–898; discussion 898–899. [DOI] [PubMed]
- 15.Olson CJ, Arthur M, Mullins RJ, et al. Influence of trauma system implementation on process of care delivered to seriously injured patients in rural trauma centers. Surgery. 2001;130:273–279. [DOI] [PubMed] [Google Scholar]