Abstract
Objective:
We set out to compare the malpractice lawsuit risk and incidence in trauma surgery, emergency surgery, and elective surgery at a single academic medical center.
Summary and Background Data:
The perceived increased malpractice risk attributed to trauma patients discourages participation in trauma call panels and may influence career choice of surgeons. When questioned, surgeons cite malpractice risk as a rationale for not providing trauma care. Little data substantiate or refute the perceived high trauma malpractice risk. We hypothesized that the malpractice risk was equivalent between an elective surgical practice and a trauma/emergency practice.
Methods:
Three prospectively maintained institutional databases were used to calculate and characterize malpractice incidence and risk: a surgical operation database, a trauma registry, and a risk management/malpractice database. Risk groups were divided into elective general surgery (ELECTIVE), urgent/emergent, nontrauma general surgery (URGENT), and trauma surgery (TRAUMA). Malpractice claims incidence was calculated by dividing the total number of filed lawsuits by the total number of operative procedures over a 12-year period.
Results:
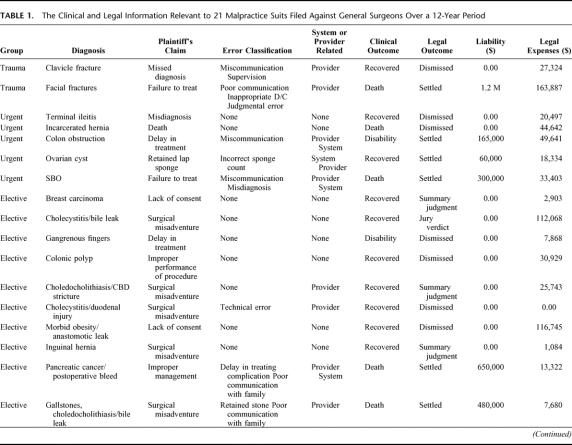
Over the study period, 62,350 operations were performed. A total of 21 lawsuits were served. Seven were dismissed. Three were granted summary judgments to the defendants. Ten were settled with payments to the plaintiffs. One went to trial and resulted in a jury verdict in favor of the defendants. Total paid liability was $4.7 million ($391,667/year). Total legal defense costs were $1.3 million ($108,333/year). The ratio of lawsuits filed/operations performed and incidence in the 3 groups is as follows: ELECTIVE 14/39,080 (3.0 lawsuits/100,000 procedures/year), URGENT 5/17,958, (2.3 lawsuits/100,000 procedures/year), and TRAUMA 2/5312 (3.1/100,000 procedures/year). During the study period, there were an estimated 49,435 trauma patients evaluated. The incidence of malpractice lawsuits using this denominator is 0.34 lawsuits/100,000 patients/year.
Conclusions:
These data demonstrate no increased risk of lawsuit when caring for trauma patients, and the actual risk of a malpractice lawsuit was low.
We set out to compare the malpractice lawsuit risk and incidence in trauma, emergency, and elective surgery. The lawsuit risk was 3.0 lawsuits/100,000 procedures/year for elective surgery, 2.3 lawsuits/100,000 procedures/year for urgent general surgery, and 3.1/100,000 procedures/year for trauma. These data demonstrate no increased risk of lawsuit in trauma patients.
Rising medical malpractice premiums have reached a crisis point in many areas of the United States.1 The economic and emotional costs of malpractice claims are driving physicians and surgeons away from high-risk specialties.2 Trauma care is perceived by many as a high malpractice risk specialty.3 The perceived increased malpractice risk attributed to trauma patients discourages participation in trauma call panels and may influence career choice of surgeons.4 When questioned, surgeons cite malpractice risk as a rationale for not providing trauma care.5 Little data substantiate or refute the perceived high-trauma malpractice risk. We hypothesized that the malpractice risk was equivalent between an elective surgical practice and a trauma/emergency practice.
METHODS
Study Setting
The study was performed in a single self-insured academic medical center which consists of 3 major components: University of Texas Health Science Center at San Antonio (UTHSCSA), a state medical school; the University Hospital, San Antonio, Texas, the major teaching hospital for the medical school; and the Audie L. Murphy Veterans Administration Hospital. The setting for this study includes the medical school and the University Hospital. The medical school faculty and resident physicians were the sole physician care providers for the University Hospital during the study period. The UTHSCSA is governed by the University of Texas System. As a part of that system, the University participates in a self-insured malpractice plan and maintains its own risk management office, which includes legal counsel, a full-time director, and administrative support. UTHSCSA employs a full range of clinical faculty who provide comprehensive patient care at the University Hospital. The University Hospital is a 604-bed, county tax-supported hospital, with governance separate from that of the medical school. The hospital functions as a tertiary referral center for a wide range of medical conditions. It is also the primary indigent care facility for Bexar County. As a part of its tertiary care role, University Hospital, an American College of Surgeons verified level I trauma center, serves as the lead trauma center for 22 counties in South Central Texas. The primary catchment area for University Hospital (Trauma Service Area P) encompasses a 26,904 square mile region with 2.1 million residents. The secondary catchment area includes the Trauma Service Areas S, T, U, and V, extending from Laredo to Brownsville. This secondary catchment area includes an additional 26,102 square miles and an additional 2.0 million residents.
Medical Records Data Source
The UTHSCSA risk management office maintains records on all reported medical adverse events, medical malpractice claims, and medical malpractice lawsuits. A record is considered closed when the case is settled, a judgment is rendered, or the statute of limitations expires. The office maintains pertinent medical records and/or medical record summaries, transcripts of depositions, expert witness testimony/consultation, court records, and minutes of the UTHSCSA risk management committee. In addition to these hard files, the office maintains an electronic database of pertinent aspects of each file. A record of all defense costs (attorney and expert witness fees), and payment to plaintiffs is maintained in these files. These records are prospectively maintained and were retrospectively reviewed for this study.
The Department of Surgery of the University of Texas Health Science Center maintains a computerized operative database of all procedures performed at University Hospital. This database has been continuously maintained since 1979 and has been previously described in the literature.6,7 The information in the database is completed at the time of each operative procedure and serves as a computer-generated operative note. This database captures every operation performed by the general surgery services at University Hospital. Since 1999, the operative database also has included minor procedures done by general surgeons outside of the operating room, such as tube thoracostomy and minor operations. The operative database has 179 separate fields and, since 1998, includes a text narrative of the operation. This computerized database was used to obtain the patient cohort. Procedures were classified into 3 groups based on the operative note: elective, urgent/emergent general surgery, and trauma.
The University Hospital has maintained a trauma registry since 1995. This registry was maintained using the Trauma Registry of the American College of Surgeons. In 2003, the registry was converted to Digital Innovations Collector software. The trauma registry was used to obtain total trauma admissions from 1996 until 2004.
Definitions and Statistics
The study period was defined from July 1, 1992 until July 1, 2004. The risk management database was queried for all malpractice claims and lawsuits filed during this period. Cases still open as of July 1, 2004 were excluded. All claims involving surgeons were reviewed. All lawsuits filed involving surgeons other than the general surgery faculty and residents were excluded. The record review included the date of occurrence and the date of the suit, the physicians involved, patient age, gender, employment status, education level, occupation, diagnosis, outcome, presence of disability, procedures performed, the plaintiff's claim of malpractice, internal review classification, root cause leading to the claim, total paid liability, and legal expenses.
If the patient was being seen or treated for external or internal injuries due to mechanical or thermal injury, they were classified as a trauma patient (TRAUMA). Nontrauma patients were classified as elective (ELECTIVE) or urgent/emergent general surgery (URGENT). Each individual adverse event or claim was classified as either provider or system-related based on a review of the records and the internal review by the risk management committee.
The surgical operative database was queried for all surgical cases during the study time period. All procedures performed by either the elective or emergency/trauma general surgical services were included for the purposes of the study. These procedures were classified as elective general surgery, urgent/emergent general surgery, or trauma general surgery. Laparoendoscopic and open procedures were included. Central venous access was excluded, unless the line was being placed as a tunneled catheter in the operating room. Tube thoracostomy, percutaneous endoscopic gastrostomy, and dilatational tracheostomy were included as procedures.
Malpractice suit incidence was calculated by dividing the total number of filed lawsuits by the total number of operative procedures over a 12-year period for each of the 3 risk groups: ELECTIVE, URGENT, and TRAUMA. The malpractice suit risk was calculated by dividing the total number of filed suits by the total number of procedures performed over the study period. Relative risk for elective, urgent/emergent, and trauma procedures was calculated by dividing the incidence of the group exposed to the risk factor by the incidence of the group not exposed to the risk factor. Confidence intervals, ANOVA, χ2, and Fisher exact test were calculated using MedCalc for Windows, version 7.5 (MedCalc Software, Mariakerke, Belgium) and Microsoft Excel for Windows XP.
RESULTS
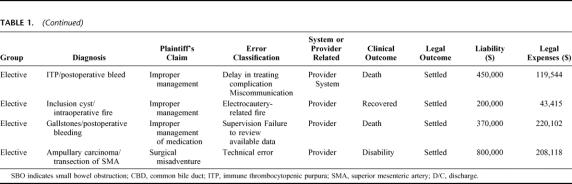
Over the study period, 62,350 operations were performed by general surgeons at University Hospital. A total of 21 lawsuits were served (Table 1). Seven were dismissed. Three were granted summary judgment. Ten were settled with payments to the plaintiffs. One went to trial and resulted in a jury verdict in favor of the defendants. Total paid liability was $4.7 million, $391,667/year. Total legal defense costs were $1.3 million, $108,333/year. The ratio of lawsuits filed/operations performed and incidence in the 3 groups is as follows: ELECTIVE 14/39,080 (3.0 lawsuits/100,000 procedures/year), URGENT 5/17,958, (2.3 lawsuits/100,000 procedures/year), TRAUMA 2/5,312 (3.1/100,000 procedures/year). There were no statistically significant differences between groups. Considering trauma as a risk factor for increased malpractice, the relative risk for trauma was 1.1 (95% CI, 0.2632–4.8494) (Fig. 1). Considering emergent/urgent general surgery as a risk factor for malpractice suit, the relative risk was 0.77 (95% CI, 0.2830–2.1084). These relative risk calculations for all groups were based on the number of procedures performed.
TABLE 1. The Clinical and Legal Information Relevant to 21 Malpractice Suits Filed Against General Surgeons Over a 12-Year Period
TABLE 1.(Continued)
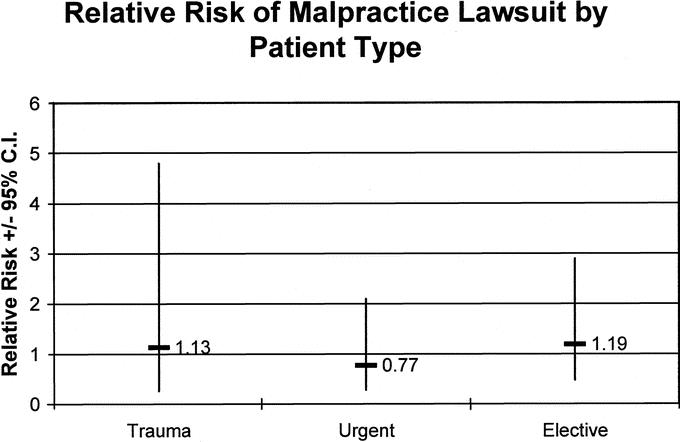
FIGURE 1. The relative risk was similar between patient groups. This risk estimation is based upon procedures performed, not patients seen, so the trauma malpractice risk is probably overestimated using these methods.
A more meaningful denominator would be total number of patients seen both inside and outside the operating room. Unfortunately, those data are not available for the elective or emergent general surgery patients and only partially available from 1995 to 2004 for the trauma patients. Extrapolating conservative (low) estimates of patient volume for the years between 1992 and 1995, there were 19,715 trauma patients admitted for more than 48 hours over the entire 12-year period. Again using conservative estimates, an additional 9720 patients were evaluated and treated by the trauma team following a full trauma team activation but were not admitted for greater than 48 hours. A third group of trauma patients were evaluated by the trauma service but did not meet trauma activation criteria. Estimates for these patients over the 12-year period are approximately 20,000.
In the ELECTIVE group, 6/14 settled for $2.95 million total. In the URGENT group 3/5 settled for $0.53 million, and in the TRAUMA group 1/2 settled for $1.2 million. One lawsuit in the ELECTIVE group went to trial with a judgment to the defendants. Total defense legal fees for each group were as follows: ELECTIVE $909,522, URGENT $166,517, and TRAUMA $191,211. Including the cost of defense along with total settlement costs, the total cost for each group was:ELECTIVE $3.76 million, URGENT $691,518, and TRAUMA $1.39 million (F = 1.7, P = 0.20, Anova). Although total costs were not statistically significantly different between groups, trauma cases accounted for 10% of the lawsuits but 24% of the cost.
DISCUSSION
These data demonstrate no increased risk of litigation when caring for trauma patients. These data support this conclusion, even though we have purposefully chosen to be conservative in this interpretation. By using operations as the denominator instead of admissions or total patients evaluated, we elevate the incidence of malpractice lawsuits in the trauma group, as there is a disproportionately large group of nonoperatively managed patients in the trauma group. Indeed, the 2 trauma patients who sued never had an operation, so technically they could have been excluded from the incidence calculation making the incidence of lawsuits in operatively managed trauma patients zero over the time frame. Using the estimated volume of trauma patients seen and evaluated by the trauma team would result in a more accurate estimate of malpractice lawsuit incidence. There were an estimated 49,435 trauma patients examined and evaluated over the 12-year study period, so estimated malpractice incidence over the study period is 2 lawsuits/49,435 patients or only 0.34 lawsuits/100,000 patients/year.
These data clearly have limitations that should be considered when interpreting the results of this work. Although the risk of lawsuit was not greater in the trauma or emergency general surgery patient, there was a trend toward higher liability payment in the trauma group. With only 2 lawsuits in the trauma group, the total cost including liability and legal fees was $1.39 million. This was due to a single large settlement to a patient who died following unexpected complications. There was no statistically significant difference in total cost between elective surgery, urgent/emergent general surgery, and trauma surgery; however, if there had been one more settlement or judgment to the plaintiffs of greater than $1 million in the trauma group, the difference would have been significant. The very nature of a high risk, critically ill trauma patient population makes the probability of severe disability or death greater than in an elective practice. Brennan et al have previously shown that the key predictor of payment is the patient's degree of disability, being significantly more important than the presence of negligence.8 This is supported by our data. Of the 21 patients who filed lawsuits, 7 died and 3 had a major long-term disability, and the total paid liability and legal defense costs in these patients was $5.19 million. In comparison, the total liability and legal defense costs of the 11 patients who fully recovered was $659,042. Ninety-five percent of the liability payment and 89% of total cost went to the 10 patients who died or were disabled (Table 1; Fig. 2).
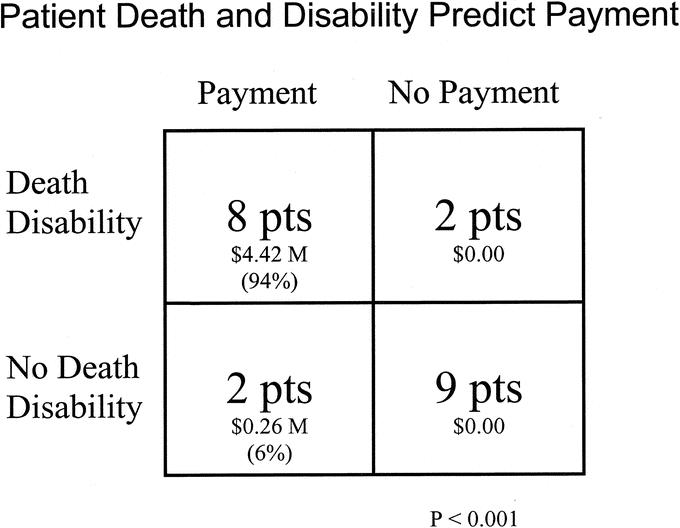
FIGURE 2. The presence of death or permanent disability predicted eventual settlement to the patient. All of the payments to the plaintiffs were on the basis of settlement. There was one trial with a jury verdict to the defendants.
Another limitation of this study is that it is localized to a single hospital with a single group of physicians and patients. There are clearly regional differences with respect to the malpractice climate, and there may be some unique local factors that attenuate trauma malpractice risk in South Texas trauma patients, although South Texas is considered a high-risk area with respect to medical malpractice.9 We limited our study to General Surgery because the surgical specialty operations were not included in our operative database over the full study period; however, it is possible that these findings could be unique to general surgery patients in our institution and not be broadly applicable to the surgical subspecialty patients.
This is the first report of which we are aware that specifically compares the actual risk of being sued between elective general surgery, urgent or emergent general surgery, and trauma surgery. Eastman et al conducted a survey of trauma centers in 1991.10 Questions concerning malpractice were a part of that survey. Ninety-two percent reported no malpractice problems specific to trauma. There was mention in the survey that the hospitals perceived no increased risk, but physicians were concerned about it.
Morris et al performed a comprehensive single-institution study examining the link between surgical adverse events, risk management, malpractice claims, and resulting payment to plaintiffs.11 These authors could find no rational link between the tort system and the reduction of adverse events. These authors did find widely varying indemnity costs between different patient groups, with trauma having a significantly higher rate of indemnity payment per admission and per hospital day. These authors speculated on reasons why indemnity payments were higher in the trauma group, citing differing expectations as a potential cause for why some patients sue whereas others do not. Specifically, they described the trauma patient expectations as the most difficult to manage since there is no preinjury physician-patient relationship. They cite families’ lack of understanding of the disease process, and anger that is frequently transferred from the perpetrator to the care provider, as other reasons why expectations are difficult to manage in the trauma patient group and why this may have led to greater indemnity payments in their trauma patients.
Our trauma patients were not more likely to sue, and there was no significant increase in indemnity payments, although there was one very high indemnity payment in the trauma patient group. We think that trauma patient expectations present fewer challenges than those of the elective surgery patient. Although there is no preinjury physician-patient relationship in either trauma or emergency general surgery, in most cases the gravity of the situation is obvious to both patients and care providers, and in most cases the bad outcomes are reasonably easy to predict given the patient's initial anatomic injuries and physiologic condition. Trauma patient family expectations can be assessed by an initial conversation between the senior trauma surgeon and the patient's family shortly after admission to the hospital. Although we have no hard data to support this claim, we think an empathetic, realistic, and thorough conversation at this time can save many hours of conversations (and possibly depositions) later.
In general, trauma patient expectations are not unreasonably high. It is true that the families of trauma patients often have a significant amount of anger and guilt, but again, this can be ameliorated by allowing them to express their anger appropriately during the time in the hospital. Dealing with patient anger is probably one of the most important ways to avert malpractice litigation, as unhappiness and anger are common denominators of patients who sue their physicians. Trauma care providers are in an ideal situation to help patients manage their anger, which benefits the patients and reduces risk to the providers.
Since there are few published reports, it is difficult to compare our risk of malpractice to other similar institutions, but our trauma malpractice risk may be atypically low. If this is true, there are invariably multiple factors that could explain a lower than expected malpractice incidence. An important next step will be to define actual malpractice incidence and risk at other institutions, establishing a benchmark for future comparisons. Our data define a low risk of malpractice but do not answer the question as to specifically why the risk is low. This is an important area for future study.
We do have a specific approach for dealing with errors, adverse events, and complications. Philosophically, we think that dealing with the patient in an honest and straightforward way, treating them as you would a family member or neighbor, minimizes risk. In our experience, when things go wrong, if we are honest and earnestly trying to do everything possible to remedy the situation, the patient or his/her family will almost always give us the benefit of the doubt when we are in a vulnerable situation. Listening, assuming responsibility (taking care to avoid scapegoating), apologizing for situations where we or our team were responsible, and finally doing everything possible we can do to make the situation right with the patient greatly diffuses anger and thus reduces the risk of a malpractice lawsuit. We understand this may be naive in today's world and goes counter to what many experts would advise. It may seem paradoxical, but sincere contrition manages the patient's (or family members') anger, and establishes a personal bond, helping both the patient and the physician.12,13
Around the first quarter of the last century, shortly before his death, Francis Weld Peabody wrote an essay entitled, “The Care of the Patient.”14
“The good physician knows his patients through and through, and his knowledge is bought dearly. Time, sympathy, and understanding must be lavishly dispensed, but the reward is to be found in that personal bond which forms the greatest satisfaction of the practice of medicine. One of the essential qualities of the clinician is interest in humanity, for the secret of care of the patient is in caring for the patient.”14
His advice is not only directly relevant to care of the patient today, but it is also sound guidance for minimizing malpractice risk and increasing the satisfaction of the practice of medicine today. A particularly modern trap, brought, at least in part, by the perceived high risk of malpractice suits against doctors, is to view the patient as a potential adversary. A patient with a personal bond to their physician, who has lavishly dispensed time, sympathy, and understanding, is unlikely to file a lawsuit when problems arise; however, adversaries, almost by definition, routinely sue each other even when there are no problems.
In a health policy report, Studdert et al cite a “deep seated tension between the malpractice system and the goals and initiatives of the patient-safety movement.”15 In matters of disclosure and reporting, transparency is a key initiative of the patient safety movement. To correct errors, one must be free to discuss them frankly and openly with all care providers in the system. Thus, key patient safety proponents emphasize the importance of openness with respect to errors.16–18 In contrast, the tort system targets individual physicians and organizations, focusing on punishment, blame, and compensation based on the foundation of negligence in patient care. This system encourages secrecy and denial of errors. An important question remains: can the goals of the patient safety movement be met with the current tort system, or does openly discussing errors put care providers and healthcare institutions at unacceptably high malpractice risk? Our experience and our data lend support to the notion that transparency and openness do not lead to unacceptably high risk.
The performance improvement program of University Hospital and the UTHSCSA trauma program are modeled on the American College of Surgeons Committee on Trauma's performance improvement model.18,19 Consistent with our interpretation of this model, the surgery faculty, residents, and nurses openly discuss errors and deaths in a weekly conference that is open to all members of the healthcare team, including nurses and students. In this manner, a frank discussion of errors, complications, and adverse events is fostered. Honest, open discussions and full participation are encouraged. Hundreds of adverse events, provider errors, and system problems have been openly discussed through this conference, and in the 12-year period, the rate of malpractice lawsuit has been very low. An open discussion of complications does not appear to increase malpractice risk.
This may seem paradoxical, but the difference relates only to the quality and nature of the discussions, not the presence or absence of a discussion. Almost unavoidably, physicians, nurses, and students discuss errors and complications. In the absence of an accepted forum to accurately and openly discuss errors and complications, these problems still get discussed, albeit through rumor, secrecy, and innuendo, often with the truth grossly distorted. We think that a frank discussion of errors and complications, with the goal of improving outcomes, is not only good for patient care, but it also fosters a cultural attitude that minimizes litigation. Heavy-handed attempts at secrecy spawn mistrust between care providers and between care providers and patients. Soil tilled with secrecy and mistrust is fertile ground for the malpractice attorney.
CONCLUSION
Trauma or emergency surgery patients at our institution are no more likely to sue their surgeon than elective surgery patients. The risk of a trauma malpractice suit being filed was very low. Among those who sued, death or permanent disability was highly associated with payment to the plaintiff. Although the risk was low, critically ill subsets of patients, including trauma, have a greater potential for permanent disability or death, so when sued, the potential for a large settlement may be greater.
Discussions
Dr. J. David Richardson (Louisville, Kentucky): When Dr. Stewart asked me to discuss this paper, I told him that I wasn't sure that I believed the conclusions, even though I didn't disbelieve his data. However, I felt compelled to review our data at the University of Louisville. In our data, it was not possible to determine the denominator on operative or treated patients, so a direct comparison with the numbers that Dr. Stewart presented was not entirely possible. However, I have data on the malpractice cases that were filed. I examined all the cases that had been filed in our practice in 10 years and not just those that had been closed. One question I would have is: what is out there waiting for you? How many cases have been filed but not closed? Given the very long time it takes to close a case, that would be an important number to have.
In the past 10 years, we have had 13 suits involving faculty from our department in the care of trauma patients. And our department includes general surgery, thoracic, urology, plastics, and ENT, but very importantly, does not include orthopedics or neurosurgery. These latter 2 are believed at a perceptional level to be very high-risk areas, and I do not have any data on those disciplines and their malpractice experience.
Eight cases involved primarily the general surgeon or the trauma surgeon and one involved the thoracic service. There were 2 cases each involving plastics and ENT. There were no urologic patients that brought suit against our urologists. The 8 general surgical cases involved injuries that often are thought to be at high risk for litigation. We had one from a posterior knee dislocation with a popliteal artery injury and one from a traumatic amputation, one from a spine fracture with an alleged delayed neurologic injury. Either missed or delayed diagnoses in 5 patients resulted in 4 suits, with fractures that were missed, including 2 spine fractures, and one with a delayed diagnosis of a carotid artery injury in a patient that had a stroke.
Three of the 4 cases on ENT and plastics involved issues of facial fractures, as one of yours did. The thoracic case was in a patient who had a stroke in repair of a transsected thoracic aorta thought to be due to placement of the cramp across the left carotid while trying to get proximal aortic control.
There have been 34 suits against general surgery and its divisions in 10 years on the elective side in what are some very large practices: 9 in the area of bariatric cases, 7 colorectal, 3 transplant, 2 vascular, 2 oncology, and 11 from other general surgical areas. Now the majority of these have already been dismissed, and there have only been a couple of small settlements there, but again, several of those are still pending.
I attempted to calculate rates of suits based and did not know how to do that. Do we use total patient encounter or only operative cases? Nonetheless, we have over 45,000 trauma admissions in 10 years so the rate is quite low.
Now, if those data are true, and it appears at least on current numbers that we have more suits in elective cases than in the trauma patients, why is this perception about malpractice risk in trauma patients such a pervasive one?
Part of it is that less than half of the suits that we had in the trauma patients were in patients that had any type of operation or any type of procedure. That was certainly true in those missed injuries. If you look at missed fractures in 45,000 patients times the number of bones in the body, it sure gives you an awful big denominator in terms of the number of fractures that you can potentially miss.
Additionally, many of the untoward events that happen to these patients clearly are out of the surgeon's control. They are not in the operating room. And that hazard seems different than in elective surgery.
The risk of a catastrophic death or disability in a young patient is ever present in trauma. Within the past few months, we had a patient with a spine fracture become paraplegic while they were attempting to logroll him onto the bed to have his femur fracture fixed. A family was furious at our service recently because we refused to replant a severed foot in a patient who came in with a traumatic amputation. The family brought the foot in an hour and a half later demanding that it be sewn back on. So there are some of those things that are just simply very hard to deal with by any data analysis.
I am reminded of an eastern Kentucky retort of a fellow to his wife, who caught him cheating with another woman, “Are you going to believe me or believe your lying eyes?” So are we going to believe Dr. Stewart's excellent data or are we going to continue to have this sense of unease and perception that caring for trauma patients really is a pretty risky business. I am going to continue to be uneasy regardless of what the data show.
Dr. Lewis M. Flint, Jr. (Tampa, Florida): I do have some observations from the state of Florida. If you watched over the past 3 years the behavior of surgeons and other physicians, politicians, attorneys, and insurance executives in our state, you could very easily come to the conclusion that malpractice causes insanity. The problem here is enormous. I think that the key word in the title of this paper is “perception.” I do think that it is a problem that is not going to yield to science or aggregate statistics.
The largest number of refusals to join a trauma call panel in the state of Florida are found in the specialties of maxillofacial surgery, orthopedics, and neurosurgery. If you don't have an idea about what the liability risk is in those specialties, then we are not getting a good view of what the problem is.
Also, do you have data that extend over the long term? Our trauma orthopedic surgeons say that their biggest problems with trauma patients are nerve injuries that are discovered in a delayed fashion that cause disability as well as infected nonunions of open fractures. Our maxillofacial people say that their problems lie in the areas of decreased vision and decreased nerve function discovered late in their patients. Our neurosurgeons say that their biggest problems are unexpected complications or death from brain injury and instances of unexpected profound disability from spinal cord injury that for one reason or another wasn't discovered early.
Unless you have data on those, and those claims may not be available for sometimes 2, 3, 4, 5 years, down the line, I don't think we can categorically state that the perception is in error. And I would caution that there is a risk here that the wrong message is being sent.
Dr. Martin A. Croce (Memphis, Tennessee): I do agree with Dr. Richardson anecdotally, at least, it appears that, at least in Memphis where there is a fairly busy trauma center, this is not our experience whatsoever. So I was wondering if Dr. Stewart would comment on perhaps the different region differences relative to lawsuits and subspecialties and specialties. And if, in fact, you are correct, Dr. Stewart, about San Antonio, then I think W.C. Fields clearly had it wrong, because on the whole I would rather be in San Antonio.
Dr. J. Patrick O'Leary (New Orleans, Louisiana): Was there an increased incidence in the suits that were filed over the period of observation?
Dr. Ronald M. Stewart (San Antonio, Texas): A couple of issues that Dr. Richardson raised were the surgical specialists and the nature of the closed cases, which Dr. Flint also basically alluded to. I do think that is a limitation of our study. And we limited it to general surgery for a reason, although I agree that general surgery is not probably the main offender with respect to not wanting to take trauma call. We did it for a practical reason in that in our institution we have a solid denominator for those general surgery cases, and we felt that it was a good comparison to compare the elective surgical practice to the trauma cases.
Concerning the issue of closed claims, it is definitely true that these are gifts that keep on giving. If we have an event today, it may be 5 years before it comes to fruition. In the methods, though, if a case were filed between 1992 and 2004, we included that, even though the operation was not done in a study period. So it takes that into account.
I would agree with both Dr. Richardson and Dr. Flint that this study needs to be studied in surgical specialists. It probably is true that the malpractice risk is higher in neurosurgery and orthopedics. But to be honest, probably the malpractice risk is higher at least in neurosurgery and the elective practice as well just because of the issue of disability.
Concerning Dr. Croce, I thank you for your question. There is little doubt in my mind that there are significant regional differences in the malpractice climate. And San Antonio may be favorable, although south Texas is thought to be a hotbed of litigation. But the difference may actually not be we may not have as big a difference as what you think if you look at your denominator of suits because Memphis is considerably busier than we are. So there may not be a difference in incidence.
One thing I would say, though, about the limitations of the study point to I want to comment on, is that you are talking about a small number of events. In the trauma group, we had 2 suits. To statistically make a difference so that there would be a significant difference in the incidence of trauma, there would need to have been more than 6 lawsuits over the time frame.
Now, it seems like tripling would be a lot. But I was talking to Dr. Richardson at dinner the other night, and he was explaining the horse racing business to me. And he described it that you sometimes make a lot and sometimes you lose a lot. And that is true with respect to malpractice in that you may go long with no suits, but all you need are a couple and you are really in bad shape. So 4 more cases over a period of 12 years, it may just be that we have some degree of luck with respect to that. If you look at the dollars, all it would have taken to make the dollars statistically significant in trauma would be one or 2 big cases. So if we had a million- or multimillion-dollar trauma lawsuit, which is a potential, then that would have shifted trauma to statistically different.
One of the things that I would say, with respect, a number of the discussants commented on, if you look at why patients sue, there are some common denominators in what we have. In trauma, both of our patients had either missed injuries or delay in recognition of injury, and that is a high-risk group. I do think, though, the most common reason why patients sue us is because they are angry. So managing that anger or dealing with that is a critical point. I definitely want to make it clear that I don't think the difference if our incidence is lower, it is not because we have fewer problems. If you look over the study period, we have hundreds of adverse events over a 12-year period. And really it is pretty clear from the data that most of the patients don't want to really sue us.
Footnotes
Reprints: Ronald M. Stewart, MD, Department of Surgery, University of Texas Health Science Center at San Antonio, 7703 Floyd Curl Drive, San Antonio, TX 78229. E-mail: stewartr@uthscsa.edu.
REFERENCES
- 1.Mello MM, Studdert DM, Brennan TA. The new medical malpractice crisis. N Engl J Med. 2003;348:2281–2284. [DOI] [PubMed] [Google Scholar]
- 2.Albert T. Texas doctors say liability costs are driving them away. AMA News. April 22, 2002.
- 3.Hall J, Davis C, Mahaffey S. Trauma center needed? Fredericksburg Free Lance-Star. November 10, 2004.
- 4.Richardson JD, Miller FB. Will future surgeons be interested in trauma care? Results of a resident survey. J Trauma. 1992;32:229–233. [DOI] [PubMed] [Google Scholar]
- 5.Esposito TJ, Maier RV, Rivara FP, et al. Why surgeons prefer not to care for trauma patients. Arch Surg. 1991;126:292–297. [DOI] [PubMed] [Google Scholar]
- 6.Stewart RM, Page CP, Brender J, et al. The incidence and risk of early postoperative small bowel obstruction: a cohort study. Am J Surg. 1987;154:643–647. [DOI] [PubMed] [Google Scholar]
- 7.Pittman-Waller VA, Myers JG, Stewart RM, et al. Appendicitis: why so complicated? Analysis of 5755 consecutive appendectomies. Am Surgeon. 2000;66:548–554. [PubMed] [Google Scholar]
- 8.Brennan TA, Sox CM, Burstin HR. Relation between negligent adverse events and the outcomes of medical malpractice litigation. N Engl J Med. 1996;335:1963–1967. [DOI] [PubMed] [Google Scholar]
- 9.Pinkerton J. Valley at the epicenter of debate on malpractice caps. Houston Chronicle. August 30, 2003.
- 10.Eastman AB, Bishop GS, Walsh JC, et al. The economic status of trauma centers on the eve of health care reform. J Trauma. 1994;36:835–846. [PubMed] [Google Scholar]
- 11.Morris JA, Carrillo Y, Jenkins JM, et al. Surgical adverse events, risk management and malpractice outcome: morbidity and mortality review is not enough. Ann Surg. 2003;237:844–852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zimmerman R. Doctors’ new tool to fight lawsuits: saying ‘I'm sorry.’ Wall Street Journal. May 18, 2004:A1.
- 13.Kraman SS, Hamm G. Risk management: extreme honesty may be the best policy. Ann Intern Med. 1999;131:963–967. [DOI] [PubMed] [Google Scholar]
- 14.Peabody FW. The care of the patient. JAMA. 1927;88:877–882. [PubMed] [Google Scholar]
- 15.Studdert DM, Mello MM, Brennan TA. Medical malpractice. N Engl J Med. 2004;350:283–290. [DOI] [PubMed] [Google Scholar]
- 16.Reason J. Human error: models and management. BMJ. 2000;320:768–770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Berwick DM, Leape LL. Reducing errors in medicine. BMJ. 1999;319:136–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Committee on Trauma, American College of Surgeons. Resources for Optimal Care of the Injured Patient. Committee on Trauma, American College of Surgeons, 1998.
- 19.American College of Surgeons Committee on Trauma. Trauma Performance Improvement: A reference manual. http://www.facs.org.trauma/publications/manual.pdf