Abstract
We describe replication-competent, vaccine strain-based rabies viruses (RVs) that lack their own single glycoprotein and express, instead, a chimeric RV-human immunodeficiency virus type 1 (HIV-1) envelope protein composed of the ectodomain and transmembrane domains of HIV-1 gp160 and the cytoplasmic domain of RV G. The envelope proteins from both X4 (NL4-3)- and R5X4 (89.6)-tropic HIV-1 strains were utilized. These recombinant viruses very closely mimicked an HIV-1- like tropism, as indicated by blocking experiments. Infection was inhibited by SDF-1 on cells expressing CD4 and CXCR4 for both viruses, whereas RANTES abolished infection of cells expressing CCR5 in addition to CD4 in studies of the RV expressing HIV-189.6 Env. In addition, preincubation with soluble CD4 or monoclonal antibodies directed against HIV-1 gp160 blocked the infectivity of both G-deficient viruses but did not affect the G-containing RVs. Our results also indicated that the G-deficient viruses expressing HIV-1 envelope protein, in contrast to wild-type RV but similar to HIV-1, enter cells by a pH-independent pathway. As observed for HIV-1, the surrogate viruses were able to target human peripheral blood mononuclear cells, macrophages, and immature and mature human dendritic cells (DC). Moreover, G-containing RV-based vectors also infected mature human DC, indicating that infection of these cells is also supported by RV G. The ability of RV-based vectors to infect professional antigen-presenting cells efficiently further emphasizes the potential use of recombinant RVs as vaccines.
Rabies virus (RV), a member of the Rhabdoviridae family, is a nonsegmented negative-strand RNA virus. The viral genome encodes five structural proteins, including one transmembrane glycoprotein (G). RV G forms homotrimers that are capable of binding to several cellular receptors (27,56). Once binding and engulfment of the virus particle occur, the viral and cellular endosomal membranes fuse due to the pH-dependent fusogenic properties of RV G and thus release the infectious RV ribonucleoprotein into the host cell cytoplasm (56).
It has been shown that RV G is not required for the budding of RV particles, but deletion of G reduces particle production 30-fold and completely abolishes infectivity (42). We have recently demonstrated that the glycoprotein of a vaccine strain of RV can be functionally replaced with a chimeric RV/VSV (vesicular stomatitis virus) glycoprotein containing the ectodomain and transmembrane domain of VSV G and the cytoplasmic domain of RV G. Replacement of the cytoplasmic tail with the corresponding domain of RV glycoprotein was proposed to be necessary due to its role in sorting and incorporation of glycoproteins into the RV envelope (40, 42). This chimeric virus grew to high titers and incorporated quantities of the RV/VSV glycoprotein into virions similar to those incorporated by wild-type RV G.
Human immunodeficiency virus type 1 (HIV-1) envelope glycoprotein gp160 mediates viral attachment, membrane fusion, and entry into permissive host cells. Typically, gp160 requires the presence of human CD4 (hCD4) and a seven-transmembrane chemokine receptor for entry into host cells (R. W. Doms, A. L. Edinger, and J. P. Moore, http://hiv-web.lanl.gov/HTML/reviews/Doms98.html, 1998). Important coreceptors for HIV-1 include CCR5, which is used by R5-tropic HIV-1 strains, and CXCR4, which is employed by X4-tropic HIV-1 strains (7). Primary T cells express both of these coreceptors in addition to CD4 and are permissive for both X4 and R5 viruses, while macrophages are predominantly permissive for R5 viruses (57).
In recent studies, our laboratory demonstrated the ability of RV to serve as a potential live-virus vector for HIV-1 vaccines (38, 39,53). After developing a vaccine strain-based RV that contains an additional transcription unit, we were able to clone and recover infectious recombinant RVs expressing the glycoprotein of HIV-1NL4-3 or HIV-189.6 in addition to the five proteins of RV. Immunization studies with mice indicated the induction of neutralizing antibodies and a potent cross-reactive cytotoxic T-lymphocyte response specific for gp160s from different HIV-1 strains (38,53).
The purpose of this study was to determine if a recombinant RV with an HIV-1-like tropism could be generated. Such a vector may be useful as an HIV-1 vaccine based on studies in which macaques immunized with live, nef-deficient simian immunodeficiency virus (SIV) were protected against a challenge with a pathogenic strain of SIV (19). However, infant and adult monkeys immunized with nef-deficient SIV later developed an AIDS-like disease (2, 3). Nevertheless, these results suggest that another live virus displaying an HIV-1-like tropism and HIV-1 antigens may elicit a protective immune response.
Furthermore, it has been suggested that targeting of live viral vectors to dendritic cells (DC) may increase cellular responses against the foreign antigens expressed by the vector. DC are potent antigen-presenting cells that capture antigen in the periphery and migrate to local draining lymph nodes. During migration, DC undergo a phenotypic change, or maturation, in which their ability to take up antigen decreases while their expression of major histocompatibility complex molecules and other costimulatory molecules increases. DC can then activate naive T cells and stimulate cellular immunity (for reviews, see references 6 and 15). While intramuscular injections with canarypox virus expressing HIV-1 proteins have elicited only inconsistent or transient cellular immunity, the same vectors were capable of infecting mature DC and stimulating strong HIV-1-specific CD4+ and CD8+ T-cell responses in vitro (23). These data suggest that live vectors capable of targeting DC may stimulate more robust cellular immunity against foreign antigens.
Here we describe two G-deficient RVs expressing HIV-1NL4-3 or HIV-189.6 gp160. These viruses displayed HIV-1 tropism in that they could only infect cells expressing CD4 and a cognate coreceptor. Our results suggest that G-deficient RVs expressing HIV-1 gp160 may serve as a potential HIV-1 vaccine due to their HIV-1-like tropism and their ability to target both immature and mature DC. Since G-deficient RVs are unable to integrate into host DNA, these viruses may provide a safer alternative to live-HIV-1 immunization.
MATERIALS AND METHODS
Plasmid construction.
The envelope gene of HIV-1 strains 89.6 and NL4-3 was PCR amplified from the infectious full-length clones of HIV-1 (p89.6, pNL4-3; AIDS Research and Reference Reagent Program [ARRRP]) with VENT polymerase (New England BioLabs) using forward primer RP27 (5′-GGG CTG CAG CTC GAG CGT ACG AAA ATG AGA GTG AAG GAG ATC AGG-3′) and reverse primer RP8 (5′-CCT CTA GAT TAC AGT CTG GTC TCA CCC CC-3′) for 89.6 and reverse primer RP6 (5′-CCT CTA GAT TAT AGC AAA GCC CTT TCC AAG-3′) for NL4-3. RP6 and RP8 contain an XbaI site (italicized), and RP27 contains PstI, XhoI, and BsiWI sites (all are italicized). The PCR products were digested with PstI and XbaI and cloned into pBluescript SK+ (Stratagene) that had been previously digested with the same enzymes. The resulting plasmids were named pBS2-NL4-3 and pBS2-89.6. To exchange the cytoplasmic domain of HIV-1 gp160 with the corresponding domain of RV G, an HpaI site was first introduced immediately upstream of the cytoplasmic domain of gp160 by site-directed mutagenesis (Promega) with primer RP28 (5′-CTG TAC TTT CTA TAG TTA ACA GAG TTA GGC AGG G-3′) (the HpaI site is italicized). The new plasmids were termed pBS2H-NL4-3 and pBS2H-89.6. To remove the gp160 tail, both plasmids pBS2H-NL4-3 and pBS2H-89.6 were digested with HpaI and XbaI. The RV G cytoplasmic domain was amplified by PCR with RP29 (5′-CCC GGG TTA ACA GAA GAG TCA ATC GAT CAG AAC-3′) (the HpaI site is italicized) and reverse primer RP8. The PCR product was digested with HpaI and XbaI and cloned into previously digested pBS2H-NL4-3 and pBS2H-89.6, resulting in plasmids pBS2H-NL4-3-G and pBS2H-89.6-G.
To introduce the HIV-1/RV chimeric glycoprotein into the RV vector, pBS2H-NL4-3-G and pBS2H-89.6-G were digested with BsiWI and XbaI and the 2.5-kb fragments were eluted and cloned into previously digested pSBN (53). The new plasmids were named pNL4-3-G and p89.6-G. To delete the RV glycoprotein from these two constructs, both pNL4-3-G and p89.6-G were digested with XbaI and BsiWI, the RV vector was purified, and the 5′ overhangs were filled in with DNA polymerase I large fragment (Klenow) and religated. These constructs were named pΔG-NL4-3-G and pΔG-89.6-G, respectively.
Generation of recombinant viruses.
The recombinant G-deficient viruses were recovered by using a modified version of the RV recovery method (25). BSR-T7 cells, which stably express T7 polymerase (11), were transfected with 5 μg of full-length RV cDNA (pΔG-NL4-3-G or pΔG-89.6), 2.5 μg of pTIT-N, 1.25 μg of pTIT-P and pTIT-L, and 1 μg of pTIT-G by using a calcium phosphate transfection kit (Stratagene). Three days later, tissue culture supernatants were pooled and transferred to SupT1 cells in T25 flasks. Cultures were analyzed for syncytium formation, indicating the presence of virus.
Virus incorporation assays.
BSR cells were grown to ∼70% confluency and infected with recombinant RVs at a multiplicity of infection (MOI) of 5 overnight. Dulbecco modified Eagle medium (DMEM) containing 0.3% bovine serum albumin and lacking methionine was used to replace the original cell medium of the first well, after which 250 μCi of [35S]methionine was added. At 24 h later, virions were purified by ultracentrifugation over 20% sucrose. Virus pellets were resuspended in 100 μl of phosphate-buffered saline (PBS), and viral proteins were separated by sodium dodecyl sulfate (SDS)-polyacrylamide gel electrophoresis (PAGE). Viral proteins were quantified by phosphorimaging.
WBs.
Human T-lymphocytic (SupT1) cells were infected with HIV-1NL4-3 (MOI of 0.05), NL4-3-G (MOI of 10), ΔG-NL4-3-G (MOI of 0.05), SBN-89.6 (MOI of 10), 89.6-G (MOI of 10), or ΔG-89.6-G (MOI of 0.05). Twenty-four hours later for cells infected with G-containing RVs and 48 h later for all other infections, cells were pelleted and resuspended in lysis buffer (50 mM Tris [pH 7.4], 150 mM NaCl, 1% Nonidet P-40, 0.1% SDS, 1× protease inhibitor cocktail [Sigma]). Cell debris was pelleted at 10,000 × g for 2 min, and the protein supernatant was transferred to a microcentrifuge tube. Proteins were separated by SDS-10% PAGE and transferred to a polyvinylidene difluoride membrane (PVDF-Plus; Osmonics, Minnetonka, Minn.). Membranes were blocked with 5% milk powder in PBS (pH 7.4) for 1 h at room temperature (RT) and then probed with 2F5 (1:5,000; ARRRP), a human monoclonal antibody directed against gp41, or a polyclonal antibody directed against the cytoplasmic tail of RV G (rabbit anti-G tail; 1:15,000) (26) in Western blot (WB) wash buffer (0.1% Tween 20, PBS [pH 7.4]) overnight at 4°C. After three 10-min washes with WB wash buffer, blots were probed for 2 h with horseradish peroxidase-conjugated 1:25,000 goat anti-human antibody (Jackson ImmunoResearch Laboratories) or horseradish peroxidase-conjugated 1:25,000 sheep anti rabbit antibody, both diluted in WB wash buffer. After three 10-min washes with WB wash buffer and one wash with PBS, a chemiluminescence assay was performed as instructed by the manufacturer (NEN).
Immunofluorescence assays.
NIH 3T3-CD4, NIH 3T3-CD4-CXCR4, and NIH 3T3-CD4-CCR5 (33) cells were plated at a density of 104 cells per well in Lab-Tek II chamber slides (Nunc Nalgene) and incubated overnight at 37°C. Cells were infected on the following day at an MOI of 1 with SBN, SBN-NL4-3 (53), SBN-89.6 (53), NL4-3-G, 89.6-G, ΔG-89.6-G, or ΔG-NL4-3-G (for constructs, see Fig.1 ). Two days later, cells were fixed with 50/50 methanol-acetone (25 min at −20°C). Slides were air dried and blocked with 5% milk in PBS (blocking solution) for 30 min at RT. After removal of the blocking solution, cells were incubated with serum from an HIV-positive patient diluted 1:100 in blocking solution for 30 min in a humid chamber at RT. Slides were carefully washed twice with PBS. Secondary antibody (Texas Red-conjugated donkey anti-human antibody; Jackson ImmunoResearch Laboratories) was diluted 1:100 in blocking solution and added to each well. Slides were incubated at 37°C in a humid chamber for 30 min. After gentle washing with PBS, chambers were removed and infections were evaluated by fluorescence microscopy.
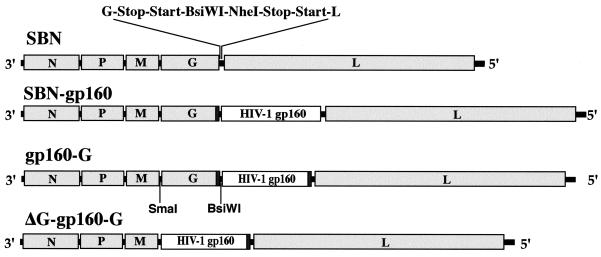
FIG. 1.
Construction of recombinant RVs. (A) SBN, an RV vaccine strain-based vector, contains an additional transcription stop-start signal flanked by two unique restriction sites. (SBN) (B) HIV-1 gp160, strains NL4-3 and 89.6, was cloned into the new transcription stop-start sequence, resulting in SBN-NL4-3 and SBN-89.6, respectively (SBN-gp160). (C) The cytoplasmic tail of HIV-1NL4-3 or HIV-189.6 gp160 was replaced with the corresponding domain of RV G (gp160-G). (D) To construct the G-deficient RVs, 89.6-G and NL4-3-G were digested with XbaI and Bsi WI sand the 5′ overhangs were filled in with Klenow and religated
Blocking experiments.
NIH 3T3-CD4-CXCR4 or NIH 3T3-CD4-CCR5 cells were plated to approximately 60% confluency in 24-well plates and incubated overnight. Supernatants were aspirated and replaced with various concentrations (0, 250, 500, 1,000, and 1,500 ng/ml) of stromal cell-derived factor 1 (SDF-1; R & D Systems) or RANTES (ARRRP) in complete DMEM. Plates were incubated for 30 min at room temperature. One hundred fifty focus-forming units (FFU) of ΔG-NL4-3-G or ΔG-89.6-G was added to each well. To block the infectivity of the G-deficient viruses, ΔG-NL4-3-G or ΔG-89.6-G was incubated at 37°C with a human anti-gp160 monoclonal antibody cocktail (2F5, 2G12, and F105 [each at 1:50]), human anti-RV serum (1:50), or soluble CD4 (ARRRP) at 0.02 mg/ml and added to the cells 30 min later. Plates were incubated for 2 days at 37°C and then fixed with 80% acetone and immunostained with a fluorescein isothiocyanate (FITC)-conjugated anti-RV-N antibody. With a fluorescence microscope, foci were counted and the percentage of inhibition was calculated by dividing the number foci in the test well by the number of foci in the positive control well.
Infection of HOS cells.
HOS (human osteosarcoma) cells expressing HIV-1 coreceptors and/or hCD4 (ARRRP) were plated at 60% confluency in a 24-well plate. Cells were infected with approximately 400 FFU of ΔG-NL4-3-G or ΔG-89.6-G and incubated for 2 days. Cells were fixed and immunostained with an FITC-conjugated RV-specific antibody.
pH-independent entry of G-deficient RVs.
NIH 3T3-CD4-CXCR4 cells were plated at 60% confluency in a 24-well plate and incubated overnight at 37°C. Ammonium chloride was added to each well at different concentrations (0, 5, 10, 15, 20, and 25 mM). After 1 h at 37°C, 150 FFU of SBN, ΔG-NL4-3-G, or ΔG-89.6-G was added per well. Two days later, cells were fixed with 80% acetone (4°C for 30 min) and incubated with an FITC-conjugated anti-RV-N antibody. Wells were analyzed for viral foci by fluorescence microscopy. Assays were performed in triplicate.
Electron microscopy.
Human SupT1 cells were infected with ΔG-NL4-3-G for 48 h. Cells were fixed at room temperature in neutral buffered 2.5% glutaraldehyde and gelled into warm agar. They were postfixed in 1% OsO4, dehydrated in graded ethanol and propylene oxide, and embedded in Spurr’s epoxy. Thin sections were cut and stained with uranyl acetate and lead citrate and examined with a LEO EM10 electron microscope at 60 kV.
Human PBMCs and macrophage infections.
Human peripheral blood mononuclear cells (PBMCs) were stimulated for 4 days with phytohemagglutinin (10 μg/ml) and interleukin-2 (4 ng/ml). Cells were infected with approximately 5 × 104 50% tissue culture infective doses of ΔG-NL4-3-G or ΔG-89.6-G, and cultures were examined daily for syncytium formation. For immunostaining, cells were fixed with 80% acetone and stained with an FITC-conjugated monoclonal antibody specific for RV N. For infection of human macrophages, PBMCs were isolated and transferred to 60-mm-diameter dishes and supplemented with 50 U of macrophage colony-stimulating factor (CSF; Sigma) and granulocyte-macrophage CSF (Sigma) in a 50:50 mixture of RPMI 1640 medium-DMEM containing 10% fetal bovine serum. After 2 weeks, cells were carefully washed to remove lymphocytes and infected with approximately 5 × 104 50% tissue culture infective doses of ΔG-NL4-3-G and ΔG-89.6-G. Six days later, cells were fixed and immunostained as described above.
DC.
Human PBMCs were isolated from buffy coats by Ficoll purification. After overnight incubation at 4°C in 1% autologous serum, monocytes were isolated by magnetic cell sorting (AutoMACS; Miltenyi Biotech) using CD14 antibodies (MACS CD14 MicroBeads; Miltenyi Biotech). Isolation efficiency was confirmed by immunostaining with FITC-conjugated anti-CD14 antibody (Miltenyi Biotech), and 99% were found to be positive for CD14. Cells positive for CD14 were plated in six-well plates at a density of 3 × 106 per well and cultured in the presence of 100 U of granulocyte-macrophage CSF (R & D Systems, Inc.) and 100 U of interleukin-4 (R & D Systems, Inc.). Six days later, immature DC were collected and counted. Cells were infected with SBN (MOI of 10), 89.6-G (MOI of 10), or ΔG-89.6-G (MOI of 1). Two days postinfection, or 3 days in the case of ΔG-89.6-G infections, cells were fixed with 80% acetone and immunostained with an anti-RV N monoclonal antibody conjugated with FITC. Alternatively, at 6 days postpurification, DC were matured by the addition of 100 U of tumor necrosis factor alpha. Two days later, cells were examined with a fluorescence-activated cell sorter for the presence of CD83 (anti-CD83; PharMingen). CD83+ cells were infected with 89.6-G (MOI of 10) or ΔG-89.6-G (MOI of 1). Cells were fixed and immunostained as described above.
RESULTS
Construction and recovery of G-deficient RVs expressing HIV-1 gp160.
SBN, a previously described RV-based vector (53), contains an additional transcription unit to express foreign genes (Fig.1 SBN). This vector has been used to express several HIV-1 proteins, such as HIV-1 gp160 (53) (Fig.1, SBN-gp160) or Gag (39). Previous results obtained by our group and others indicated the necessity of the RV G cytoplasmic domain for efficient incorporation of HIV-1 gp160 into rhabdovirus virions (34,40, 41). We therefore constructed two recombinant RVs in which the cytoplasmic domain of HIV-1NL4-3 or HIV-189.6 gp160 was replaced with the corresponding domain of RV G (Fig.1, gp160-G). The RV vector was designed to contain a single SmaI site after the transcription stop-start sequence in the M-G gene junction and a single BsiWI site after the transcription start signal sequence used to express the foreign gene. These two sites were used to delete the G gene from 89.6-G and NL4-3-G (Fig. 1, ΔG-gp160-G). The resulting plasmids were designated pΔG-89.6-G and pΔG-NL4-3-G.
Due to the lack of the G gene in the viral genome, a modified RV recovery system was required. Therefore, we included a fifth plasmid encoding RV G into the transfection protocol (25) to trans complement the G-deficient RVs and support the initial spread on the transfected cells. Three days after transfection, the supernatants from transfected cells were transferred onto a human T-cell line (SupT1). Large-syncytium formation in some of the cell cultures indicated successful infection and the expression of HIV-1 gp160 from the recombinant RVs (not illustrated).
The titers of the G-deficient recombinant RVs expressing HIV-1 Env were reduce 10,000- to 200-fold, depending on the cell line used, and reached about 2 × 104 on SupT1 cells and 5 × 105 on HOS cells expressing CD4 and CCR3.
Expression of HIV-1 gp160 by RV vectors.
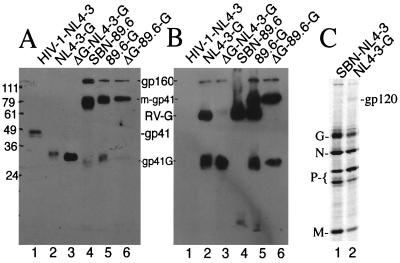
To analyze the expression of the chimeric gp160/RV protein from the G-deficient RVs, human SupT1 cells were infected with HIV-1NL4-3, ΔG-NL4-3-G, ΔG-89.6-G (MOI of 0.05), NL4-3-G, SBN-89.6, or 89.6-G (MOI of 10) and lysed 24 to 48 h later. Cell extracts were separated by SDS-PAGE and analyzed by WB assay. As shown in Fig. 1A, an antibody directed against HIV-1 gp41 (10, 48, 49) detected a protein with the expected size of gp41 in the case of the HIV-1NL4-3-infected cells (panel A, lane 1, gp41) and a faster-migrating protein in extracts from NL4-3-G-, ΔG-NL4-3-G-, 89.6-G-, and ΔG-NL4-3-G-infected cells (panel A, lanes 2, 3, 5, and 6, gp41G). In the case of the RVs expressing HIV-189.6 envelope protein, an additional protein of about 80 kDa was detected, indicating multimers of gp41 (panel A, lanes 4, 5, and 6, m-gp41).
An antibody specific for the RV G cytoplasmic domain (26) detected RV G in lysates of cells infected with G-containing viruses (Fig.2B, lanes 2, 4, and 5). Additionally, gp41 and gp160 were detected in lysates of cells infected with NL3-4-G, 89.6-G, ΔG-NL4-3-G, and ΔG-89.6-G (Fig.2B, lanes 2, 3, 5, and 6) but not in lysates of cells infected with SBN-89.6, which expresses the wild-type HIV-1 envelope protein (Fig.2B, lane 4).
FIG. 2.
Analysis of expression and incorporation of HIV-1 gp160 by RV vectors. Human SupT1 cells were infected with HIV-1NL4-3, ΔG-NL4-3-G, ΔG-89.6-G (MOI of 0.05), NL4-3-G, SBN-89.6, or 89.6-G (MOI of 10) and lysed 24 to 48 h later. Proteins were separated by SDS-PAGE and subjected to WB assays with antibodies specific for HIV-1 gp41 (A) and the RV G cytoplasmic tail (B). As shown in panel A, a protein with the expected size of gp41 was detected when HIV-1NL4-3-infected cells (panel A, lane 1, gp41) were used and a faster-migrating protein was found in NL4-3-G-, ΔG-NL4-3-G-, 89.6-G-, and ΔG-NL4-3-G-infected cell extracts (panel A, lanes 2, 3, 5, and 6, gp41G). An additional protein of about 80 kDa was detected in lysates of cells infected with 89.6-expressing viruses, indicating multimers of gp41 (panel A, lanes 4, 5, and 6, m-gp41). The antibody specific for the RV G cytoplasmic tail detected RV G in G-containing virus-infected cell lysates (panel B, lanes 2, 4, and 5) and gp41 and gp160 in lysates of cells infected with NL3-4-G, 89.6-G, ΔG-NL4-3-G, and ΔG-89.6-G (panel B, lanes 2, 3, 5, and 6). Protein sizes are indicated in kilodaltons. (C) BSR cells were infected overnight with recombinant RVs at an MOI of 5 and labeled with [35S]methionine for 24 h. Virions were purified by ultracentrifugation over 20% sucrose and resuspended, and viral proteins were separated by SDS-PAGE. Viral proteins were quantified by phosphorimaging.
Studies indicate that the cytoplasmic domain of RV G is required for incorporation of foreign glycoproteins into RV virions. To determine the level of incorporation of the chimeric HIV-1/RV gp160, BSR cells were infected with SBN-NL4-3 and NL4-3-G and labeled with [35S]methionine for 24 h. We only detected incorporation of the HIV-1 Env protein containing the RV cytoplasmic domain, whereas wild-type gp160 was not detected in the recombinant virions. Quantification indicated that the incorporation efficiency was about 10% of that of RV G.
G-deficient RVs expressing gp160 require CD4 and an HIV-1 coreceptor.
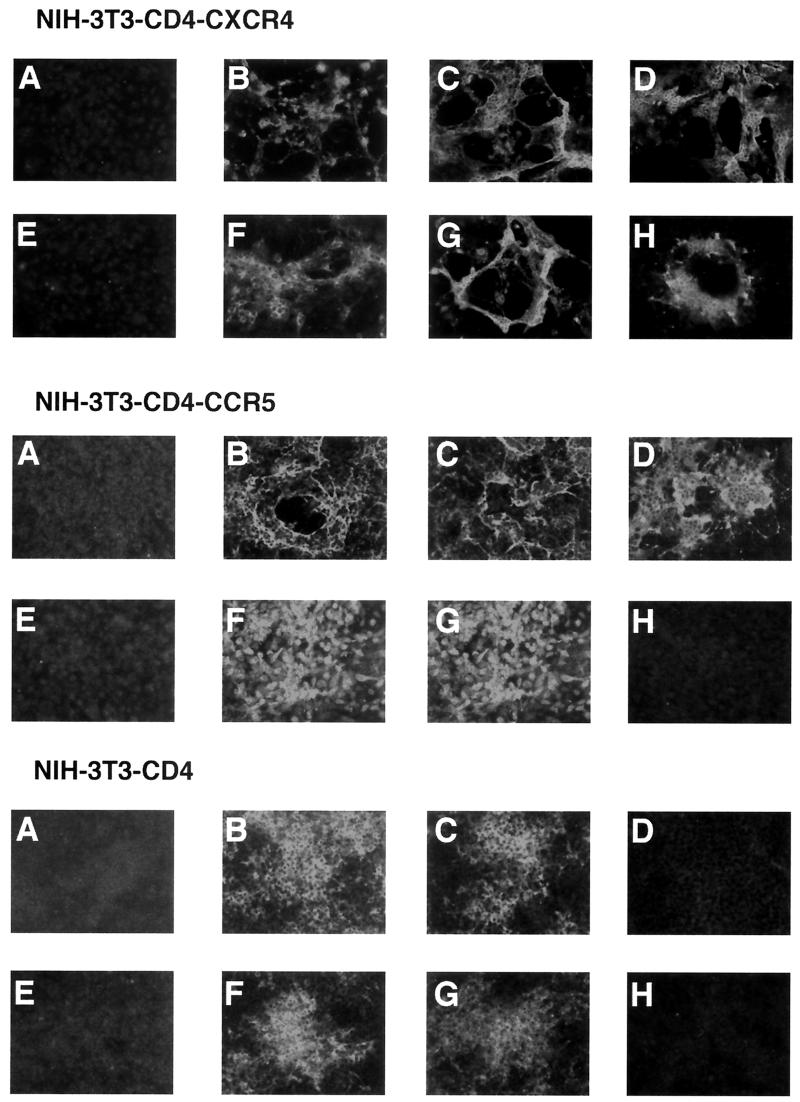
RV has a broad host range and can infect many cell types, both human and nonhuman (50, 51). In contrast, HIV-1 only causes a productive infection in human cells expressing CD4 in addition to a seven-transmembrane chemokine receptor (for a review, see reference 8). Replacement of RV G with HIV-1 gp160 should alter the tropism of the chimeric RVs to mimic the tropism of the parental HIV-1 strain. HIV-1NL4-3 is an X4 laboratory-adapted strain that requires hCD4 and hCXCR4, while HIV-189.6, a primary R5X4-tropic isolate, requires hCD4 and either hCXCR4 or hCCR5. To analyze the tropism of the RVs, we infected NIH 3T3 cells expressing hCD4, hCD4, and hCXCR4 or hCD4 and hCCR5 with the SBN, SBN-89.6, 89.6-G, ΔG-89.6-G, SBN-NL4-3, NL4-3-G, or ΔG-NL4-3-G virus. As expected, all of the G-containing RVs were able to infect the NIH 3T3-CD4 cells (Fig. 3B, C, F, and G, 3T3-CD4). Due to the lack of an HIV-1 coreceptor on these cells, no syncytium formation was observed, even after expression of HIV-1 Env. Moreover, neither strain of the G-deficient RVs infected these cells due to the lack of an HIV-1 coreceptor (Fig.3D and H, 3T3-CD4).
FIG. 3.
Tropism of G-deficient RVs expressing HIV-1 Env. NIH 3T3 cells expressing hCD4 and hCXCR4 (NIH 3T3-CD4-CXCR4), hCD4 and hCCR5 (NIH 3T3-CD4-CCR5), or hCD4 (NIH 3T3-CD4) were infected with SBN (A), SBN-89.6 (B), 89.6-G (C), ΔG-89.6-G (D), SBN-NL4-3 (F), NL4-3-G (G), or ΔG-NL4-3-G (H) or left uninfected (E). At 48 h later, cells were fixed and immunostained with serum from an HIV-1-seropositive patient.
Infection of NIH 3T3-CD4-CCR5 cells with the same panel of viruses produced different results. As noted for NIH 3T3-CD4 cells, all G-containing RVs were able to infect and replicate within these cells but the cells were also permissive for ΔG-89.6-G but not for ΔG-NL4-3-G. The functionality of the chimeric HIV-189.6 envelope protein was further confirmed by syncytium formation in cultures infected with RVs expressing 89.6 Env. As expected, no virus expressing NL4-3 Env was able to induce fusion nor was ΔG-NL4-3-G able to infect this cell line.
NIH 3T3-CD4-CXCR4 cells were permissive for all chimeric viruses, regardless of the presence or absence of RV G. G-containing viruses most likely entered the cells using RV G, while G-deficient viruses must use the chimeric HIV-1 envelope protein. Since HIV-1 strains NL4-3 and 89.6 both use CXCR4 as a coreceptor for entry into cells, fusion was induced due to the interaction of hCD4, hCXCR4, and HIV-1 gp160 on the cell surfaces. In summary, these results indicate that the chimeric gp160 can functionally substitute for RV G and that these chimeric viruses require CD4 and a cognate coreceptor.
Recent reports indicate that certain specific HIV-1 strains can infect human cells expressing only HIV-1 coreceptors and not CD4 (22, 36). To analyze if the G-deficient RVs expressing gp160 are able to infect cells utilizing only an HIV-1 coreceptor, HOS cells expressing a variety of coreceptors with and without CD4 were infected with approximately 400 FFU of ΔG-NL4-3-G or ΔG-89.6-G and incubated for 2 days. Cells were fixed and immunostained with an FITC-conjugated RV-specific antibody. As shown in Table 1 neither strain of G-deficient RV expressing gp160 could infect cells expressing only CXCR4 or CCR5, indicating the necessity of the expression of CD4 for entry. Low-level infection did occur in HOS-CD4 cells, and this was probably due to the low level of expression of CXCR4 on these cells (20, 31).
TABLE 1.
Tropism of G-deficient RVs expressing HIV-1 gp160
| Cell line | Level of infectiona
|
|
|---|---|---|
| ΔG-NL4-3-G | ΔG-89.6-G | |
| HOS-CD4 | +++ | ++ |
| HOS-CXCR4 | - | - |
| HOS-CCR5 | - | - |
| HOS-CD4-CXCR4 | +++ | ++ |
| HOS-CD4%minus;CCR5 | +++/++ | +++ |
| HOS-CD4-CCR1 | +++ | +++ |
| HOS-CD4-CCR2b | + | + |
| HOS-CD4-CCR3 | ++++ | ++++ |
| HOS-CD4-CCR4 | ++ | ++ |
Symbols: -, no infection; +, 10 to 25% infection; ++, 25 to 50% infection; +++, 50 to 75% infection; ++++, 75 to 100% infection.
Infection by G-deficient RVs is blocked by soluble CD4, chemokines, and antibodies against gp160.
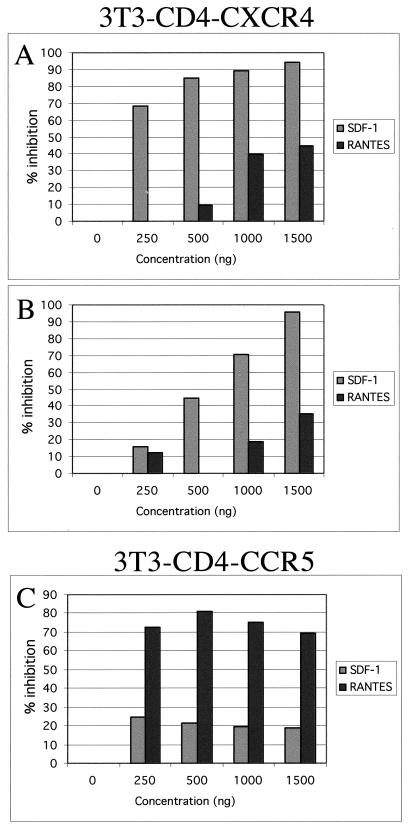
Our results indicate that hCD4 and hCXCR4 or hCCR5 are necessary for the entry of G-deficient RVs expressing HIV-1 envelope protein. To investigate whether the natural ligands of the chemokine receptors can block infection by G-deficient RVs, as shown previously for HIV-1 (9, 16, 44), we performed blocking experiments. NIH 3T3-CD4-CXCR4 cells were incubated with increasing concentrations of soluble human SDF-1, the natural ligand of CXCR4, or soluble human RANTES, which binds to CCR5. As expected, RANTES had no specific effect on the entry of ΔG-NL4-3-G while SDF-1 was able to inhibit the entry of this virus (Fig. 4A). As shown in Fig.4B, SDF-1 also inhibits ΔG-89.6-G on 3T3-CD4-CXCR4 cells in a dose-dependent manner. To analyze the use of CCR5 by ΔG-89.6-G, 3T3-CD4-CCR5 cells were pretreated with SDF-1 or RANTES and infected with ΔG-89.6-G. The results in Fig.4C demonstrate that binding of RANTES to CCR5 inhibits the entry of ΔG-89.6-G whereas SDF-1 has no effect on the entry of this virus into CCR5 cells. These results further indicate the necessity of the chemokine receptors for entry of G-deficient RVs expressing gp160.
FIG. 4.
Effects of SDF-1 and RANTES on the entry of ΔG-NL4-3-G and ΔG-89.6-G. NIH 3T3-CD4-CXCR4 cells (A and B) or NIH 3T3-CD4-CCR5 cells (C) were pretreated with 0, 250, 500, 1,000, or 1,500 ng of SDF-1 or RANTES as indicated and infected with 150 FFU of ΔG-NL4-3-G (A) or ΔG-89.6-G (B and C). Cells were fixed and immunostained with an RV-N-specific antibody conjugated to FITC. Foci were counted, and percent inhibition was calculated.
In addition to blocking with a specific ligand for an HIV-1 coreceptor, HIV-1 entry can also be efficiently blocked by soluble hCD4 or neutralizing antibodies against HIV-1 Env. Therefore, we incubated G-deficient RVs expressing HIV-1 Env with soluble hCD4, a cocktail of three human monoclonal antibodies specific for gp160 (2G12, F105, and 2F5) (45, 55), or human anti-RV serum. As shown in Table 2, the RV-specific serum did not neutralize the G-deficient viruses but did efficiently block infection by the RV G-containing vector. In contrast, soluble CD4, which binds to gp120, almost completely abolished infection by both ΔG-NL4-3-G and ΔG-89.6-G (Table 2) but had no effect on infection with RV wild-type (data not shown). A mixture of human monoclonal antibodies specific for three different epitopes in gp160 was also able to inhibit infection by both G-deficient RVs expressing gp160. These results further confirm that gp160 is required for entry by the chimeric RV/HIV-1 viruses.
TABLE 2.
Blockage of G-deficient RVs expressing HIV-1 gp160
| Antibody | Blockage of infection by indicated virus in cell line:
|
||
|---|---|---|---|
| 3T3-CD4-CXCR4
|
3T3-CD4-CCR5
|
||
| ΔG-NL4-3-G | ΔG-89.6-G | ΔG-89.6-G | |
| None | 0 | 0 | 0 |
| Anti-RV-G | 0 | 0 | 0 |
| Anti-gp160 | 98 | 66.20 | 100 |
| sCD4a | 99.30 | 100 | 100 |
sCD4, soluble CD4.
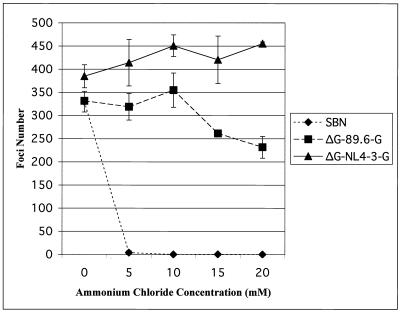
Entry of G-deficient RVs is pH independent. After attachment and endocytosis of RV particles into a host cell, the viral and cellular membranes fuse due to the lower pH and the conformation of RV G (56). HIV-1, however, can fuse directly to the cellular membrane via a pH-independent mechanism (37). Because the G-deficient RVs contain only HIV-1 gp160 as a viral transmembrane glycoprotein, the chimeric virus should mimic the pH-independent HIV-1 entry pathway. To analyze this, NIH 3T3-CD4-CXCR4 cells were pretreated for 1 h with increasing concentrations of ammonium chloride, a weak base that inhibits acidification of endosomes (32). Cells were then infected with wild-type RV, ΔG-NL4-3-G, or ΔG-89.6-G. Two days later, cells were fixed and stained with an FITC-conjugated anti-RV N antibody and foci were counted. As shown in Fig.5, SBN (wild-type RV) no longer infected cells in the presence of 5 mM ammonium chloride. In contrast, both strains of G-deficient RVs expressing gp160 were unaffected by the increasing concentrations of ammonium chloride, thus indicating a pH independent mechanism of entry, similar to that of HIV-1.
FIG. 5.
Delineation of the mechanism of entry of G-deficient RVs expressing HIV-1 gp160. NIH 3T3-CD4-CXCR4 cells were pretreated with increasing concentrations of ammonium chloride (0, 5, 10, 15, and 20 mM) for 1 h and then infected with SBN, ΔG-NL4-3-G, or ΔG-89.6-G. Two days later, cells were fixed and immunostained with an antibody specific for RV-N protein and foci were counted. Error bars indicate the standard deviation of three independent experiments.
Chimeric G-deficient HIV/RV particles maintain wild-type RV morphology.
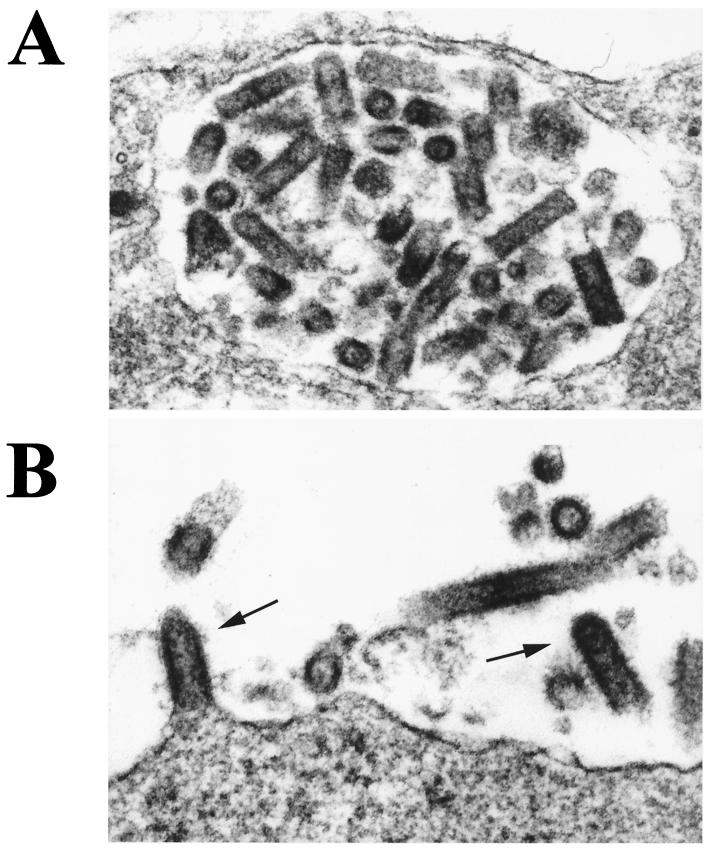
Viruses from the family Rhabdoviridae typically display a bullet-shaped morphology. Others have examined the structure of G-deficient RV particles and found that they retain the typical RV morphology (42), which probably can be attributed to the RV matrix protein (M) (43). To determine if the presence of HIV-1 gp160 affects the structure of G-deficient budding virions, SupT1 cells were infected with ΔG-NL4-3-G for 48 h. Cells were then fixed and analyzed by transmission electron microscopy. Figure 6 shows characteristically sized, bullet-shaped RV particles in either a cytoplasmic vacuole or a cross section from a depression in the cellular membrane (A) and budding from the plasma membrane (B, arrows). These data indicate that neither deletion of the RV G protein nor introduction of the chimeric HIV-1/RV protein alters the morphology of the recombinant RV particles.
FIG. 6.
Evaluation of the morphology of ΔG-NL4-3-G by electron microscopy. A human T-cell line (SupT1) was infected with ΔG-NL4-3-G for 48 h. Cells were fixed and analyzed by electron microscopy at 60 kV. Shown are regular-size, bullet-shaped RV particles in a cytoplasmic vacuole (A) and budding from the plasma membrane (B, arrows). Magnification, ×131,000.
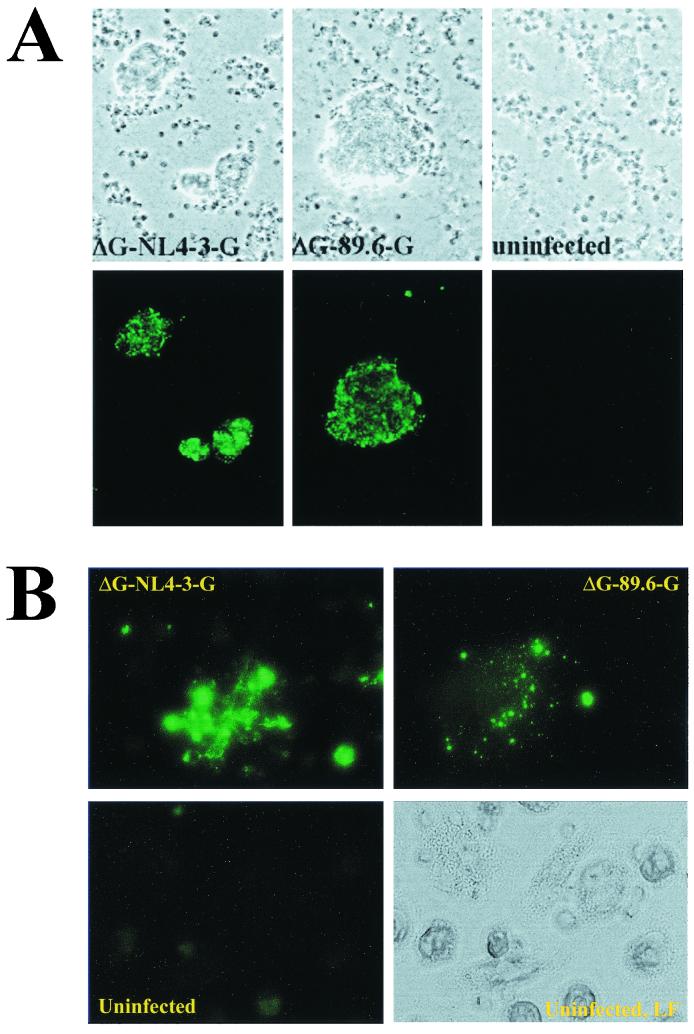
G-deficient RVs expressing HIV-1 gp160 infect human PBMCs and monocyte-derived-macrophages. An important target of HIV-1 in vivo is CD4+ T lymphocytes. These cells have been shown to express both CXCR4 and CCR5 chemokine receptors, making them permissive for X4-, R5X4-, and R5-tropic viruses. To analyze weather G-deficient RVs expressing gp160 are able to target human primary T lymphocytes, human PBMCs were infected with ΔG-NL4-3-G or ΔG-89.6-G. Two days later, cells were fixed and immunostained against the RV N protein. Syncytium formation and positive immunostaining indicated both entry and replication of both ΔG-NL4-3-G and ΔG-89.6-G (Fig. 7A).
FIG. 7.
Infection of human PBMCs with G-deficient RVs expressing HIV-1 gp160. Human PBMCs were isolated and infected with ΔG-NL4-3-G or ΔG-89.6-G. Syncytium formation and a positive signal obtained by immunostaining with an RV N-specific antibody indicated entry and replication of both G-deficient RVs. (B) Infection of human monocyte-derived-macrophages with G-deficient RVs expressing HIV-1 gp160. Monocytes were isolated from human PBMCs and differentiated into macrophages. Cultures of macrophages were infected with ΔG-NL4-3-G or ΔG-89.6-G. Cells were fixed 2 days later and immunostained with an antibody specific for RV N protein. A positive signal for RV N indicates infection by both G-deficient RVs expressing gp160. LF denotes light field.
Macrophages are involved at all stages of the immune response and are important as antigen-presenting cells. Because RV-based vectors do not kill infected cells, these vectors may support long-term expression of HIV-1 antigen(s) in macrophages. To determine if ΔG-NL4-3-G or ΔG-89.6-G can target primary human macrophages, we isolated and infected cultures of human macrophages with ΔG-NL4-3-G or ΔG-89.6-G. Cells were fixed 2 days later and immunostained with an antibody specific for the RV N protein. Both strains of the G-deficient HIV-1/RVs were able to infect and replicate in human macrophages, indicating HIV-1-like tropism (Fig. 7B). Others have shown recently that some laboratory-adapted strains of HIV-1 can gain entry into primary macrophages by CXCR4 but do not replicate due to postentry blocks (4). Since RV is capable of replicating in macrophages, we were able to confirm, by using ΔG-NL4-3-G, the ability of the envelope protein from a T-tropic strain of HIV-1 to support entry into macrophages using CD4 and CXCR4.
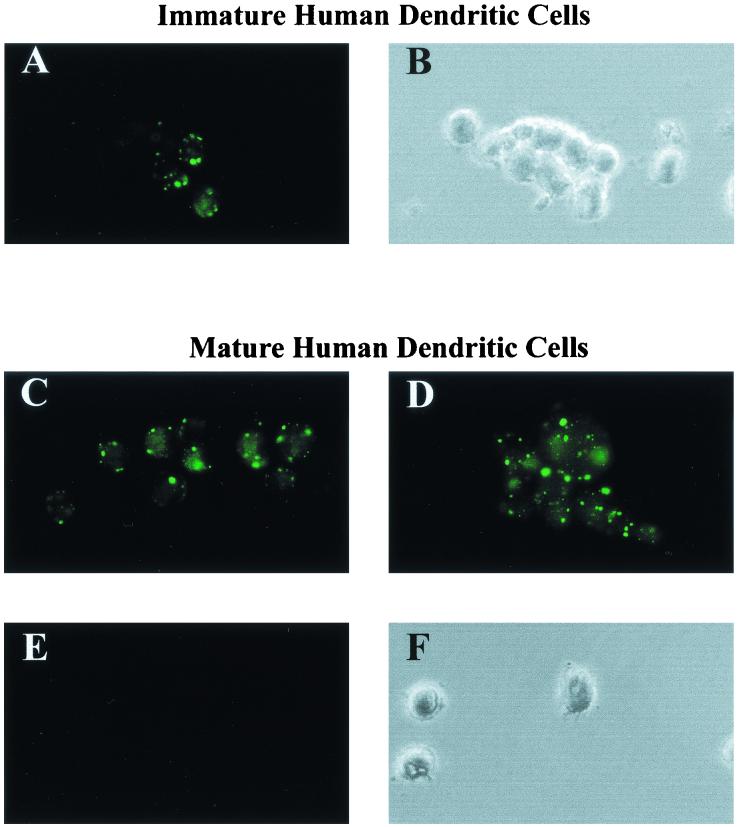
G-deficient RVs infect human DC.
Although it has been reported that some R5 strains of HIV-1 can infect and replicate within immature DC due to the low level of CCR5 expression on these cells (29), mature DC do not support efficient replication of HIV-1 due to postentry blocks (5, 29). Overall, the permissiveness of immature and mature DC has not been completely delineated. However, DC play an important role in the transmission of HIV-1 to other cells, such as T lymphocytes (12, 13, 28, 29). Recently, it was shown that DC bind HIV-1 gp120 by DC-SIGN, a DC-specific C-type lectin, and possibly serve as a transport vehicle for the virus to the lymph node, a major site of CD4+ T lymphocytes (28). To analyze if RV vectors can target DC, immature and mature human monocyte-derived DC were infected with 89.6-G (MOI of 10) and 2 days later fixed and immunostained with a monoclonal antibody directed against RV N. The results shown in Fig. 8 indicate that DC were highly susceptible to infection by 89.6-G, and similar findings obtained with the RV vector SBN indicate that infection was probably mediated by the RV G protein (data not shown). The goal of this study was to construct a second-generation RV-based vector that is specifically targeted to important antigen-presenting cells. The experiments with the G-containing RVs on DC indicated the possibility that RVs can replicate efficiently in these cell types. In the next step, we analyzed if the chimeric HIV/RV envelope protein expressed by a G-deficient RV is able to mediate infection of human DC. We therefore infected immature and mature human monocyte-derived DC with ΔG-89.6-G (MOI of 1) and fixed and immunostained the cells 3 days later. As shown in Fig. 9 at least 50% of both mature and immature DC were infected by the G-deficient RVs, as indicated by expression of the RV N protein. Moreover, the mature DC maintained their characteristic shape, indicating that RV does not induce a cytopathic effect on DC, which may result in long-term presentation of the expressed antigens.
FIG. 8.
Infection of immature and mature human DC with 89.6-G. Immature human monocyte-derived DC were infected with 89.6-G (MOI of 10) and, 2 days later, fixed and immunostained with an antibody directed against RV N (A). Mature CD83+ human monocyte-derived DC were infected with 89.6-G (MOI of 10; C and D) or mock infected (E). Two days later, cells were fixed and immunostained with an antibody directed against RV N. Panels B and F show the light fields of the immunostained cells in panels A and E.
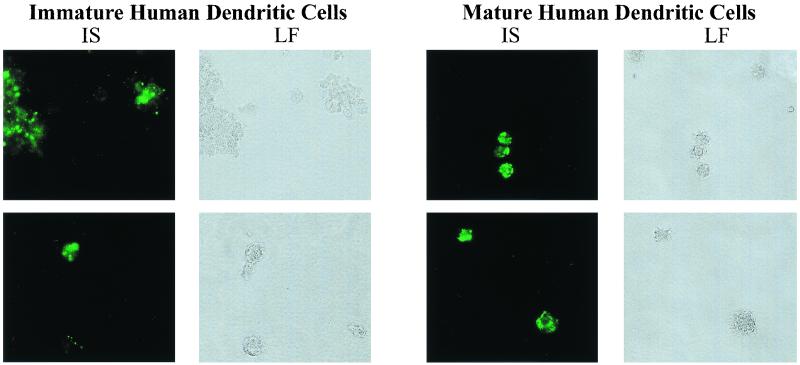
FIG. 9.
Infection of immature and mature human DC with ΔG-89.6-G. Immature human monocyte-derived DC or mature CD83+ human monocyte-derived DC were infected with ΔG-89.6-G (MOI of 1). Three days after infection, cells were fixed and immunostained against RV N 3 days after infection. IS denotes immunostaining, and LF denotes light field.
DISCUSSION
We have constructed replication-competent, G-deficient RV vectors expressing a chimeric glycoprotein consisting of the ectodomain and transmembrane domain of HIV-1 gp160 from an X4- or R5X4-tropic HIV-1 strain and the cytoplasmic domain of RV G. The chimeric RV/HIV-1 glycoproteins were functionally expressed on the surfaces of infected cells and incorporated into RV virions. The recombinant G-deficient RVs were able to specifically infect cells expressing hCD4 and one of the HIV-1 coreceptors used by the HIV-1 strain from which the envelope protein was derived. As observed for HIV-1, entry of ΔG-89.6-G or ΔG-NL4-3-G was blocked by a mixture of monoclonal antibodies that neutralize HIV-1, soluble CD4, and specific chemokines for the respective HIV-1 coreceptor. Moreover, the G-deficient RVs expressing gp160 were able to target professional antigen-presenting cells such as macrophages and DC.
Whereas the ability of the G-deficient RVs expressing envelope protein from R5X4-tropic HIV-1 isolates to infect human macrophages is similar to that observed for macrophage-tropic or dual-tropic HIV-1 strains, the results for ΔG-NL4-3-G were different. Although macrophages can express low levels of CXCR4, it has been somewhat unclear whether X4-tropic strains of HIV-1 may enter and replicate within these cells (8, 54). Since RV is capable of replicating in macrophages (50), we were able to confirm, by using ΔG-NL4-3-G, the ability of gp160 from a T-tropic strain of HIV-1 to support entry into macrophages, indicating that there exists a postentry block of X4-tropic HIV-1 strains.
The ability of both G-containing and G-deficient, replication-competent RVs expressing HIV-1 gp160 to infect and replicate in immature and mature DC strengthens the significance of these vectors as vaccine candidates. Our results obtained with G-containing RV vectors indicate that the RV G protein is able to mediate infection of human DC, which may explain the vigorous immune responses detected after a single immunization with these vectors expressing HIV-1 Env or Gag (38, 39). The finding that ΔG-89.6-G also efficiently infects mature human DC is encouraging and differs from the findings obtained with R5- or R5X4-tropic HIV-1 strains. When mature human DC are infected with an M-tropic HIV-1 strain, reverse transcription is blocked and only early transcripts can be detected (29). Because such a block does not affect RV transcription, efficient expression of virus-derived proteins occurs after infection of mature DC. Because RV-based vectors do not kill the infected cells, the expression of a foreign antigen may be longer then with cytopathogenic vectors.
In recent reports, we have shown the potential efficacy of G-containing RV-based vectors as potential HIV-1 vaccines (26, 38, 5). Our results indicate that RVs expressing HIV-1 gp160 or Gag induce strong immune responses against the expressed HIV-1 antigens in mice. Studies with nef-deficient SIV indicated that a live, attenuated virus is the most effective method by which to protect against a challenge with a highly pathogenic SIV strain (19). A major concern in the use of attenuated lentiviruses as vaccines is the finding that even nef-deficient SIV can give rise to an AIDS-like disease in both neonatal and adult macaques (2, 3). Additional concerns arise from the finding that recombination of live, attenuated SIV with the challenge virus, in some cases, results in an even more virulent strain (30). A G-deficient RV expressing HIV-1 Env, whose tropism closely mimics that of HIV-1, may be a safer alternative to live-HIV-1 immunization. The life cycle of rhabdoviruses is restricted to the cytoplasm of the infected cell, and the viral genome does not integrate into the host cell genome (52). Therefore, an RV vaccine vector should be cleared by the immune system. In addition, the backbone of our RV vector is derived from a highly attenuated RV vaccine strain used for oral immunization of wildlife animals in Europe (18). Further evidence that a G-deficient, RV-based vector may be a safe vaccine vehicle is in a recent report that shows that G-deficient RVs do not cause rabies (24).
One concern with the use of G-deficient RVs is the approximately 1,000-fold lower titers reached compared to those of G-containing RVs. A previous study by Mebatsion and Conzelmann indicates that deletion of RV G reduces particle production by only 30-fold (42). The lower titers observed here are probably due to both a lower budding efficiency and a lower incorporation rate of chimeric HIV-1 (26). However, the lower level of replication of the G-deficient RVs expressing HIV-1 Env does not imply that these vaccine vehicles will induce less potent immune responses than those induced by G-containing RVs. The results described herein indicate that these vectors mainly target professional antigen-presenting cells, which may result in a vigorous immune response against the expressed antigens. Due to the lack of a small-animal model, studies with G-deficient RV vectors expressing HIV-1 require analysis in the macaque-SIV model system and the results will indicate if these vectors may be used alone or in conjunction with immunization schedules utilizing full-length RV vaccine vectors.
Acknowledgments
Human monoclonal antibody directed against HIV-1 gp160 (10, 14, 46–49), HOS cells expressing HIV-1 coreceptors and/or hCD4 (20, 31), plasmids pNL4-3 and p89.6, encoding an infectious clone of HIV-1NL4-3 (1) or HIV-189.6 (17, 21, 35), and the recombinant RANTES protein were obtained through the ARRRP, Division of AIDS, National Institute of Allergy and Infectious Diseases, National Institutes of Health. This study was supported in part by National Institutes of Health grants AI44340 and AI49153, internal Thomas Jefferson University funds to M.J.S, and the Center for Human Virology.
We thank Catherine Siler for excellent technical assistance.
REFERENCES
- 1.Adachi, A., H. E. Gendelman, S. Koenig, T. Folks, R. Willey, A. Rabson, and M. A. Martin. 1986. Production of acquired immunodeficiency syndrome-associated retrovirus in human and nonhuman cells transfected with an infectious molecular clone J. Virol. 59:284–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baba, T. W., Y. S. Jeong, D. Pennick, R. Bronson, M. F. Greene, and R. M. Ruprecht. 1995. Pathogenicity of live, attenuated SIV after mucosal infection of neonatal macaques. Science 267:1820–1825. [DOI] [PubMed] [Google Scholar]
- 3.Baba, T. W., V. Liska, A. H. Khimani, N. B. Ray, P. J. Dailey, D. Pennick, R. Bronson, M. F. Greene, H. M. McClure, L. N. Martin, and R. M. Ruprecht. 1999. Live attenuated, multiply deleted simian immunodeficiency virus causes AIDS in infant and adult macaques. Nat. Med. 5:194–203. [DOI] [PubMed] [Google Scholar]
- 4.Bakri, Y., S. Amzazi, A. Mannioui, and A. Benjouad. 2001. The susceptibility of macrophages to human immunodeficiency virus type 1 X4 isolates depends on their activation state. Biomed. Pharmacother. 55:32–38. [DOI] [PubMed] [Google Scholar]
- 5.Bakri, Y., C. Schiffer, V. Zennou, P. Charneau, E. Kahn, A. Benjouad, J. C. Gluckman, and B. Canque. 2001. The maturation of dendritic cells results in postintegration inhibition of HIV-1 replication. J. Immunol. 166:3780–3788. [DOI] [PubMed] [Google Scholar]
- 6.Banchereau, J., and R. M. Steinman. 1998. Dendritic cells and the control of immunity. Nature 392:245–252. [DOI] [PubMed] [Google Scholar]
- 7.Berger, E. A., R. W. Doms, E. M. Fenyo, B. T. Korber, D. R. Littman, J. P. Moore, Q. J. Sattentau, H. Schuitemaker, J. Sodroski, and R. A. Weiss. 1998. A new classification for HIV-1. Nature 391:240. [DOI] [PubMed] [Google Scholar]
- 8.Berger, E. A., P. M. Murphy, and J. M. Farber. 1999. Chemokine receptors as HIV-1 coreceptors: roles in viral entry, tropism, and disease. Annu. Rev. Immunol. 17:657–700. [DOI] [PubMed] [Google Scholar]
- 9.Bleul, C. C., M. Farzan, H. Choe, C. Parolin, I. Clark-Lewis, J. Sodroski, and T. A. Springer. 1996. The lymphocyte chemoattractant SDF-1 is a ligand for LESTR/fusin and blocks HIV-1 entry. Nature 382:829–833. [DOI] [PubMed] [Google Scholar]
- 10.Buchacher, A., R. Predl, K. Strutzenberger, W. Steinfellner, A. Trkola, M. Purtscher, G. Gruber, C. Tauer, F. Steindl, and A. Jungbauer. 1994. Generation of human monoclonal antibodies against HIV-1 proteins; electrofusion and Epstein-Barr virus transformation for peripheral blood lymphocyte immortalization. AIDS Res. Hum. Retrovir. 10:359–369. [DOI] [PubMed] [Google Scholar]
- 11.Buchholz, U. J., S. Finke, and K. K. Conzelmann. 1999. Generation of bovine respiratory syncytial virus (BRSV) from cDNA: BRSV NS2 is not essential for virus replication in tissue culture, and the human RSV leader region acts as a functional BRSV genome promoter. J. Virol. 73:251–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cameron, P. U., P. S. Freudenthal, J. M. Barker, S. Gezelter, K. Inaba, and R. M. Steinman. 1992. Dendritic cells exposed to human immunodeficiency virus type-1 transmit a vigorous cytopathic infection to CD4+ T cells. Science 257:383–387. [DOI] [PubMed] [Google Scholar]
- 13.Cameron, P. U., M. Pope, S. Gezelter, and R. M. Steinman. 1994. Infection and apoptotic cell death of CD4+ T cells during an immune response to HIV-1-pulsed dendritic cells. AIDS Res. Hum. Retrovir. 10:61–71. [DOI] [PubMed] [Google Scholar]
- 14.Cavacini, L. A., C. L. Emes, J. Power, A. Buchbinder, S. Zolla-Pazner, and M. R. Posner. 1993. Human monoclonal antibodies to the V3 loop of HIV-1 gp120 mediate variable and distinct effects on binding and viral neutralization by a human monoclonal antibody to the CD4 binding site. J. Acquir. Immune Defic. Syndr. 6:353–358. [PubMed] [Google Scholar]
- 15.Cella, M., F. Sallusto, and A. Lanzavecchia. 1997. Origin, maturation and antigen presenting function of dendritic cells. Curr. Opin. Immunol. 9:10–16. [DOI] [PubMed] [Google Scholar]
- 16.Cocchi, F., A. L. DeVico, A. Garzino-Demo, S. K. Arya, R. C. Gallo, and P. Lusso. 1995. Identification of RANTES, MIP-1 alpha, and MIP-1 beta as the major HIV-suppressive factors produced by CD8+ T cells. Science 270:1811–1815. [DOI] [PubMed] [Google Scholar]
- 17.Collman, R., J. W. Balliet, S. A. Gregory, H. Friedman, D. L. Kolson, N. Nathanson, and A. Srinivasan. 1992. An infectious molecular clone of an unusual macrophage-tropic and highly cytopathic strain of human immunodeficiency virus type 1. J. Virol. 66:7517–7521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Conzelmann, K.-K. J. H. Cox, L. G. Schneider, and H. J. Thiel. 1990. Molecular cloning and complete nucleotide sequence of the attenuated rabies virus SAD B19. Virology 175:485–499. [DOI] [PubMed] [Google Scholar]
- 19.Daniel, M. D., F. Kirchhoff, S. C. Czajak, P. K. Sehgal, and R. C. Desrosiers. 1992. Protective effects of a live attenuated SIV vaccine with a deletion in the nef gene. Science 258:1938–1941. [DOI] [PubMed] [Google Scholar]
- 20.Deng, H., R. Liu, W. Ellmeier, S. Choe, D. Unutmaz, M. Burkhart, P. Di Marzio, S. Marmon, R. E. Sutton, C. M. Hill, C. B. Davis, S. C. Peiper, T. J. Schall, D. R. Littman, and N. R. Landau. 1996. Identification of a major co-receptor for primary isolates of HIV-1. Nature 381:661–666. [DOI] [PubMed] [Google Scholar]
- 21.Doranz, B. J., J. Rucker, Y. Yi, R. J. Smyth, M. Samson, S. C. Peiper, M. Parmentier, R. G. Collman, and R. W. Doms. 1996. A dual-tropic primary HIV-1 isolate that uses fusin and the beta-chemokine receptors CKR-5, CKR-3, and CKR-2b as fusion cofactors Cell 85:1149–1158. [DOI] [PubMed]
- 22.Dumonceaux, J., S. Nisole, C. Chanel, L. Quivet, A. Amara, F. Baleux, P. Briand, and U. Hazan. 1998. Spontaneous mutations in the env gene of the human immunodeficiency virus type 1 NDK isolate are associated with a CD4-independent entry phenotype. J. Virol. 72:512–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Engelmayer, J., M. Larsson, A. Lee, M. Lee, W. I. Cox, R. M. Steinman, and N. Bhardwaj. 2001. Mature dendritic cells infected with canarypox virus elicit strong anti-human immunodeficiency virus CD8+ and CD4+ T-cell responses from chronically infected individuals. J. Virol. 75:2142–2153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Etessami, R., K. K. Conzelmann, B. Fadai-Ghotbi, B. Natelson, H. Tsiang, and P. E. Ceccaldi. 2000. Spread and pathogenic characteristics of a G-deficient rabies virus recombinant: an in vitro and in vivo study. J. Gen. Virol. 81:2147–2153. [DOI] [PubMed] [Google Scholar]
- 25.Finke, S., and K. K. Conzelmann. 1999. Virus promoters determine interference by defective RNAs: selective amplification of mini-RNA vectors and rescue from cDNA by a 3′ copy-back ambisense rabies virus. J. Virol. 73:3818–3825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Foley, H. D., J. P. McGettigan, C. A. Siler, B. Dietzschold, and M. J. Schnell. 2000. A recombinant rabies virus expressing vesicular stomatitis virus glycoprotein fails to protect against rabies virus infection. Proc. Natl. Acad. Sci. USA 97:14680–14685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gaudin, Y., R. W. Ruigrok, C. Tuffereau, M. Knossow, and A. Flamand. 1992. Rabies virus glycoprotein is a trimer. Virology 187:627–632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Geijtenbeek, T. B., D. S. Kwon, R. Torensma, S. J. van Vliet, G. C. van Duijnhoven, J. Middel, I. L. Cornelissen, H. S. Nottet, V. N. KewalRamani, D. R. Littman, C. G. Figdor, and Y. van Kooyk. 2000. DC-SIGN, a dendritic cell-specific HIV-1-binding protein that enhances trans-infection of T cells. Cell 100:587–597. [DOI] [PubMed] [Google Scholar]
- 29.Granelli-Piperno, A., E. Delgado, V. Finkel, W. Paxton, and R. M. Steinman. 1998. Immature dendritic cells selectively replicate macrophage-tropic (M-tropic) human immunodeficiency virus type 1, while mature cells efficiently transmit both M- and T-tropic virus to T cells. J. Virol. 72:2733–2737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gundlach, B. R., M. G. Lewis, S. Sopper, T.Schnell, J. Sodroski, U. Dittmer, C. Stahl-Hennig, and K. Uberla. 2000. Evidence for recombination of live, attenuated immunodeficiency virus vaccine with challenge virus to a more virulent strain. J. Virol. 74:3537–3542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.He, J., and N. R. Landau. 1995. Use of a novel human immunodeficiency virus type 1 reporter virus expressing human placental alkaline phosphatase to detect an alternative viral receptor. J. Virol. 69:4587–4592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Helenius, A., M. Marsh, and J. White. 1982. Inhibition of Semliki Forest virus penetration by lysosomotropic weak bases. J. Gen. Virol. 58:47–61. [DOI] [PubMed] [Google Scholar]
- 33.Hill, C. M., H. Deng, D. Unutmaz, V. N. Kewalramani, L. Bastiani, M. K. Gorny, S. Zolla-Pazner, and D. R. Littman. 1997. Envelope glycoproteins from human immunodeficiency virus types 1 and 2 and simian immunodeficiency virus can use human CCR5 as a coreceptor for viral entry and make direct CD4-dependent interactions with this chemokine receptor. J. Virol. 71:6296–6304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Johnson, J. E., M. J. Schnell, L. Buonocore, and J. K. Rose. 1997. Specific targeting to CD4+ cells of recombinant vesicular stomatitis viruses encoding human immunodeficiency virus envelope proteins. J. Virol. 71:5060–5068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kim, F. M., D. L. Kolson, J. W. Balliet, A. Srinivasan, and R. G. Collman. 1995. V3-independent determinants of macrophage tropism in a primary human immunodeficiency virus type 1 isolate. J. Virol. 69:1755–1761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.LaBranche, C. C., T. L. Hoffman, J. Romano, B. S. Haggarty, T. G. Edwards, T. J. Matthews, R. W. Doms, and J. A. Hoxie. 1999. Determinants of CD4 independence for a human immunodeficiency virus type 1 variant map outside regions required for coreceptor specificity. J. Virol. 73:10310–10319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McClure, M. O., M. Marsh, and R. A. Weiss. 1988. Human immunodeficiency virus infection of CD4-bearing cells occurs by a pH-independent mechanism. EMBO J. 7:513–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.McGettigan, J. P., H. D. Foley, I. M. Belyakov, J. A. Berzofsky, R. J. Pomerantz, and M. J. Schnell. 2001. Rabies virus-based vectors expressing human immunodeficiency virus type-1 (HIV-1) envelope protein induce a strong, cross-reactive cytotoxic T-lymphocyte response against envelope proteins from different HIV-1 isolates. J. Virol. 75:4430–4434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McGettigan, J. P., S. Sarma, J. M. Orenstein, R. J. Pomerantz, and M. J. Schnell. 2001. Expression and immunogenicity of human immunodeficiency virus type I Gag expressed by a replication-competent rhabdovirus-based vaccine vector J. Virol. 75:8724–8732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mebatsion, T., and K.-K. Conzelmann. 1996. Specific infection of CD4+ target cells by recombinant rabies virus pseudotypes carrying the HIV-1 envelope spike protein. Proc. Natl. Acad. Sci. USA 93:11366–11370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mebatsion, T., S. Finke, F. Weiland, and K.-K. Conzelmann. 1997. A CXCR4/CD4 pseudotype rhabdovirus that selectively infects HIV-1 envelope protein-expressing cells. Cell 90:841–847. [DOI] [PubMed] [Google Scholar]
- 42.Mebatsion, T., M. Konig, and K.-K. Conzelmann. 1996. Budding of rabies virus particles in the absence of the spike glycoprotein. Cell 84:941–951. [DOI] [PubMed] [Google Scholar]
- 43.Mebatsion, T., F. Weiland, and K.-K. Conzelmann. 1999. Matrix protein of rabies virus is responsible for the assembly and budding of bullet-shaped particles and interacts with the transmembrane spike glycoprotein G. J. Virol. 73:242–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Oberlin, E., A. Amara, F. Bachelerie, C. Bessia, J. L. Virelizier, F. Arenzana-Seisdedos, O. Schwartz, J. M. Heard, I. Clark-Lewis, D. F. Legler, M. Loetscher, M. Baggiolini, and B. Moser. 1996. The CXC chemokine SDF-1 is the ligand for LESTR/fusin and prevents infection by T-cell-line-adapted HIV-1. Nature 382:833–835. [DOI] [PubMed] [Google Scholar]
- 45.Posner, M. R., L. A. Cavacini, C. L. Emes, J. Power, and R. Byrn. 1993. Neutralization of HIV-1 by F105, a human monoclonal antibody to the CD4 binding site of gp120. J. Acquir. Immune Defic. Syndr. 6:7–14. [PubMed] [Google Scholar]
- 46.Posner, M. R., H. Elboim, and D. Santos. 1987. The construction and use of a human-mouse myeloma analogue suitable for the routine production of hybridomas secreting human monoclonal dantibodies. Hybridoma 6:611–625. [DOI] [PubMed] [Google Scholar]
- 47.Posner, M. R., T. Hideshima, T. Cannon, M. Mukherjee, K. H. Mayer, and R. A. Byrn. 1991. An IgG human monoclonal antibody that reacts with HIV-1/GP120, inhibits virus binding to cells, and neutralizes infection. J. Immunol. 146:4325–4332. [PubMed] [Google Scholar]
- 48.Purtscher, M., A. Trkola, A. Grassauer, P. M. Schulz, A. Klima, S. Dopper, G. Gruber, A. Buchacher, T. Muster, and H. Katinger. 1996. Restricted antigenic variability of the epitope recognized by the neutralizing gp41 antibody 2F5. AIDS 10:587–593. [DOI] [PubMed] [Google Scholar]
- 49.Purtscher, M., A. Trkola, G. Gruber, A. Buchacher, R. Predl, F. Steindl, C. Tauer, R. Berger, N. Barrett, and A. Jungbauer. 1994. A broadly neutralizing human monoclonal antibody against gp41 of human immunodeficiency virus type 1. AIDS Res. Hum.Retrovir. 10:1651–1658. [DOI] [PubMed] [Google Scholar]
- 50.Ray, N. B., L. C. Ewalt, and D. L. Lodmell. 1995. Rabies virus replication in primary murine bone marrow macrophages and in human and murine mac rophage-like cell lines: implications for viral persistence. J. Virol. 69:764–772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ray, N. B., C. Power, W. P. Lynch, L. C. Ewalt, and D. L. Lodmell. 1997. Rabies viruses infect primary cultures of murine, feline, and human microglia and astrocytes. Arch. Virol. 142:1011–1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rose, J. K., and M. Schubert. 1987. Rhabdovirus genomes and their products. Plenum Publishing Corp., New York, N.Y.
- 53.Schnell, M. J., H. D. Foley, C. A. Siler, J. P. McGettigan, B. Dietzschold, and R. J. Pomerantz. 2000. Recombinant rabies virus as potential live-viral vaccines for HIV-1. Proc. Natl. Acad. Sci. USA 97:3544–3549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Simmons, G., J. D. Reeves, S. Hibbitts, J. T. Stine, P. W. Gray, A. E. Proudfoot, and P. R. Clapham. 2000. Co-receptor use by HIV and inhibition of HIV infection by chemokine receptor ligands. Immunol. Rev. 177:112–126. [DOI] [PubMed] [Google Scholar]
- 55.Trkola, A., A. B. Pomales, H. Yuan, B. Korber, P. J. Maddon, G. P. Allaway, H. Katinger, C. F. Barbas, D. R. Burton, and D. D. Ho. 1995. Cross-clade neutralization of primary isolates of human immunodeficiency virus type 1 by human monoclonal antibodies and tetrameric CD4-immunoglobulin G. J. Virol. 69:6609–6617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Whitt, M. A., L. Buonocore, C. Prehaud, and J. K. Rose. 1991. Membrane fusion activity, oligomerization, and assembly of the rabies virus glycoprotein. Virology 185:681–688. [DOI] [PubMed] [Google Scholar]
- 57.Yi, Y., S. Rana, J. D. Turner, N. Gaddis, and R. G. Collman. 1998. CXCR-4 is expressed by primary macrophages and supports CCR5-independent infection by dual-tropic but not T-tropic isolates of human immunodeficiency virus type 1. J.Virol. 72:772–777. [DOI] [PMC free article] [PubMed] [Google Scholar]