Abstract
Objective:
To characterize the national epidemiology of adult osteomyelitis (OM) and, using a single institutions’ experience, test the hypothesis that early surgical therapy as compared with antibiotics alone results in an improved chance of wound healing and limb salvage.
Background:
Foot and digit OM is a very common problem for which management is variable and for which few guidelines exist.
Methods:
The Nationwide Inpatient Sample (NIS) and a single institution review from 1993 to 2000 form the basis of this study, using ICD-9CM codes for lower extremity foot and digit OM. Demographics, risk factors, and treatments were analyzed against the outcomes of a healed wound, limb salvage, and death.
Results:
The NIS included 51,875 patients (incidence = 9/10,000 patients per year) with a mean age of 60 years, and 59% were men. The median length of stay decreased from 9 to 6 days (P < 0.001), but the average admission charge of $19,000 did not significantly decrease over 7 years. Of these patients, 23% underwent a digit amputation and 8.5% suffered proximal limb loss. Single-institution analysis of 237 consecutive patients with OM confirmed a similar mean age (58 years), gender (67% men), and most presented with a foot or digit ulcer (56%). Wound healing was achieved in 56% and overall limb salvage was 80%. Decreased wound healing was associated with peripheral vascular occlusive disease (odds ratio, 0.4; 95% confidence interval, 0.2–0.8, P = 0.006) and preadmission antibiotic use (odds ratio, 0.2; 95% confidence interval, 0.05–1.1, P=0.07), while surgical debridement (odds ratio, 2.2; 95% confidence interval, 1.2–4.2, P = 0.02) was associated with increased healing. Limb salvage was improved with an arterial bypass (odds ratio, 3.9; 95% confidence interval, 1.1–14, P = 0.04), while preadmission solid organ transplant (odds ratio, 0.37; 95% confidence interval, 0.14–0.96, P = 0.04), peripheral vascular occlusive disease (odds ratio, 0.25; 95% confidence interval, 0.12–0.5, P = 0.001), and preadmission antibiotic use (odds ratio, 0.34; 95% confidence interval, 0.15–0.77, P = 0.009) were associated with greater limb loss.
Conclusion:
Digit OM is an expensive and morbid disease. Aggressive surgical debridement/digit amputation and selected use of arterial bypass should improve wound healing and limb salvage, respectively. In contrast, antibiotic therapy alone is associated with decreased wound healing and limb salvage.
The epidemiology, cost, and outcomes from a national administrative database of adult osteomyelitis are reported. A complementary local database suggests that antibiotic therapy as compared with surgical osteotomy or digital amputation is associated with less chance of wound healing and significantly lower limb salvage.
Osteomyelitis (OM) in adults usually involves the digits of the feet and is most often associated with diabetes mellitus (DM).1–3 As such, other diabetic complications such as peripheral vascular occlusive disease (PVOD), peripheral neuropathy, and chronic renal insufficiency (CRI) contribute to the clinical course of OM. These comorbidities produce a constellation of factors that impair wound healing, decrease tissue antibiotic penetration, and accentuate the underlying abnormal biomechanical pressure on the foot structures. Foot diseases are a common cause of hospitalization for patients with DM and are associated with high societal and economic cost.2,4
Contemporary therapy for adult digital OM includes the tenets of meticulous, intensive wound care, culture specific antibiotics, treatment of underlying nutritional and diabetic disease complications, and pressure reduction maneuvers to improve healing.1,3,5,6 Less well established is the optimal use and duration of antibiotics (without a bone culture), and what role surgery has in bone debridment and digital amputation.6–10 For example, there is no level I or II medical evidence to guide when medical therapy alone may suffice and when surgical therapy is indicated. A few small case series have yielded mixed results.10,11 Furthermore, no multidisciplinary consensus statements have been published regarding this topic. Antibiotics are often abused, with lack of cultures to guide use, and prolonged courses administered that do not affect healing nor eradicate the infection. Better consensus exists for vascular reconstruction in patients with chronic OM and ulceration, particularly in the setting of PVOD and DM. These procedures can be done with low morbidity and mortality, but revascularization may not always be timely enough to ensure limb salvage.2,12
The aim of this study was to characterize the current national epidemiology, cost, and outcomes of adult digital and foot OM, and to further characterize the specifics of treatment and its effect on outcomes of wound healing and limb salvage by examining a contemporary experience at an individual institution.
METHODS
This study used 2 databases. The first, the Nationwide Inpatient Sample (NIS), is an administrative database that is a 20% stratified random sample of all hospital discharges in the United States. The database is maintained by the Agency for Health Care Research and Quality as part of the Health Care Cost and Utilization Project.13 The study years included 1993 to 2000. Patients were identified by International Classification of Diseases, 9th Edition, Clinical Modification14 (ICD-9CM) hospital primary discharge codes for acute and chronic foot and digital OM: 730.06, 730.07, 730.16, 730.17, 730.26, and 730.27. Procedural codes assessed for the same hospitalizations as the index OM admission included: digital and forefoot amputation (84.11, 84.12), major amputations below the knee (BKA) or above the knee (AKA) (84.10, 84.15, 84.17), in-hospital antibiotic use (99.21), and whether or not a peripheral arterial bypass was performed (39.29). Outcome measures evaluated were: amputation rate, length of stay (LOS), mortality, unfavorable discharge (discharge to setting other than home), and inflation-adjusted cost of hospitalization.
The second database included consecutive patients treated at the University of Michigan over a period of 7 years (1993–2000) using the same diagnostic ICD-9CM codes for OM. This database captured all consecutive inpatients hospitalized for OM and did not bias toward surgical patients. Pediatric aged patients (<18 years) and those patients with orthopedic hardware infections were excluded. The patient's first hospitalization for OM was classified arbitrarily as time point zero (index admission) for consideration of preadmission therapies, such as antibiotics, and for timing subsequent admissions for medical or surgical therapy. Demographic data assessed included age, gender, comorbid diseases, and diagnostic studies used to delineate OM. Chronic renal insufficiency was defined by documented need for renal replacement therapy such as hemodialysis (HD) or peritoneal dialysis. Antibiotic use was assessed for timing (prehospitalization, during hospitalization, and posthospitalization), duration of use in weeks, oral or intravenous (IV) administration, and number of courses.
Characterization of surgical therapy for OM included localized debridement and ostectomy, as well as digital, forefoot, or major amputation (AKA or BKA). Clinic notes were used to determine the status of the ulcer or wound (if present) at the most recent follow-up and were categorized as: healed, chronic wound but no mention of OM, and chronic OM documented by radiograph or examination. Patient's use of both home health nursing services (HHS) and inpatient rehabilitation stays was determined as well. Notation was made if the patient had an arterial reconstruction, although the specifics such as type, conduit, and patency were not determined as this was not the focus of the current study. Patients who had only digital or partial foot amputations were considered to have maintained limb savage. For those patients who were lost to follow-up or deceased, the ambulatory status was abstracted from the last clinic note.
Statistical analysis used Mann Whitney U, or Student t test for continuous variables, and χ2 or Fisher exact test for univariate analysis. Data are presented as mean ± SEM where appropriate. Logistical regression of NIS data was done using dichotomous variables to determine independence of associated factors with specific outcomes of mortality, amputation, and unfavorable discharge with a P < 0.01 for entrance into the model. Data from the University of Michigan were compared using the same statistics, except logistical regression was used to assess association of factors with outcomes of mortality, wound healing, and limb salvage with a P < 0.05 required for entrance into the model. Kaplan-Meier life-table analysis was done to compare outcomes of limb salvage and mortality over time. The SPSS statistical software (Chicago, IL) was used. This study was approved by the University of Michigan Institutional Review Board.
RESULTS
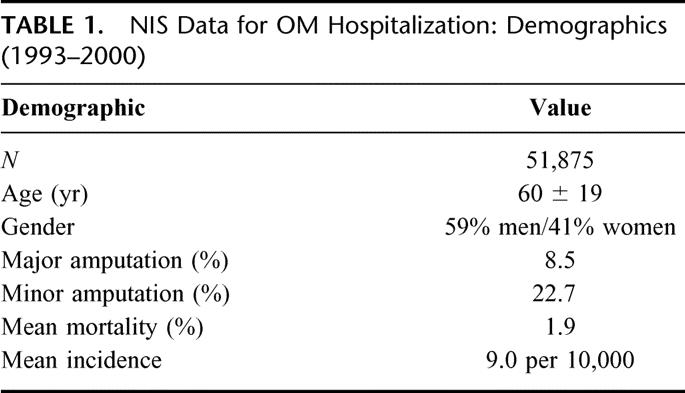
Nationally, from 1993 to 2000, OM-related diagnoses accounted for a mean of 9 per 10,000 patient admissions without significant change over time. In this cohort, 59% were men, with a mean age of 60 years and a median LOS of 7 days (Table 1). The median LOS decreased significantly from 9 days in 1993 to 6 days in 2000 (P < 0.0001). Mean inflation-adjusted hospital charges were $19,000 with little variation over the time period analyzed. Major amputation was performed in 8.5%, while digital amputation was performed in 23%. In-hospital mortality was 1.6%.
TABLE 1. NIS Data for OM Hospitalization: Demographics (1993–2000)
Logistical regression was done to determine independent factors associated with mortality, minor amputation, major amputation, and unfavorable discharge with the foreknowledge that administrative databases are limited with respect to specificity of patient factors that can be analyzed.15 Mortality was primarily associated with older age, emergent admission, and need for major amputation. In contrast, minor amputation was protective against mortality (Table 2). No effect of bypass procedure or antibiotic use was found on mortality. Major amputation was predicted by older age, renal failure, and black race (as compared with white). Antibiotic use was protective, as was nonelective admission status (Table 3). Minor amputation was again more common with increased age, black race, and renal disease. Antibiotic code and nonelective admission were associated with less risk for minor amputation (Table 4). Similarly, discharge to other than home was predicted by older age, female gender, major amputation, and arterial bypass (Table 5). In contrast, minor amputation code was associated with favorable discharge.
TABLE 2. NIS Data: Factors Associated With Mortality (1993–2000)
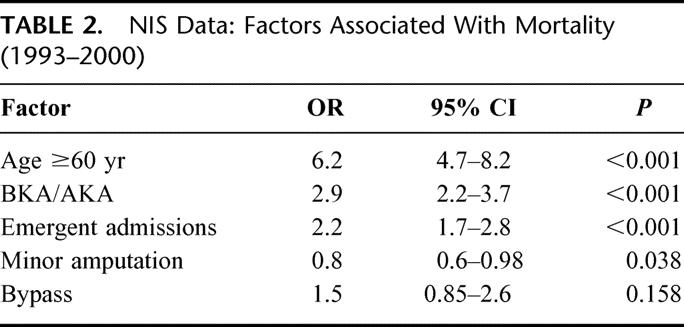
TABLE 3. NIS Data: Factors Associated With Major Amputation (1993–2000)
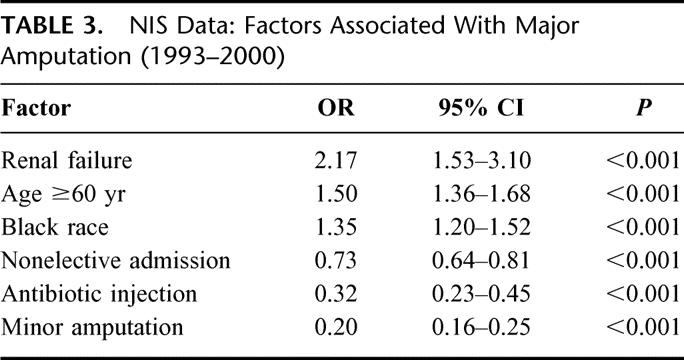
TABLE 4. NIS Data: Factors Associated With Minor Amputation (1993–2000)
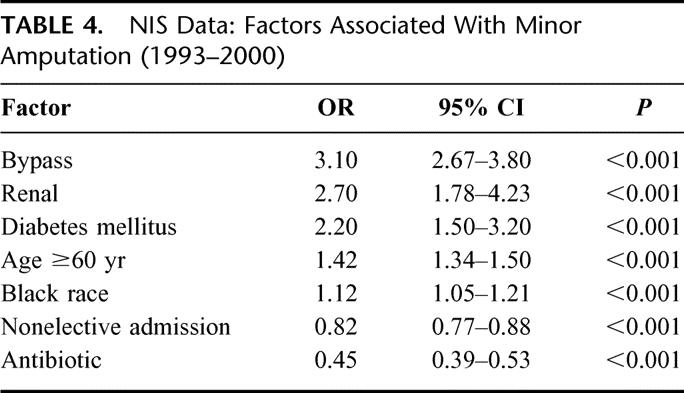
TABLE 5. NIS Data: Factors Associated With Unfavorable Discharge (1993–2000)

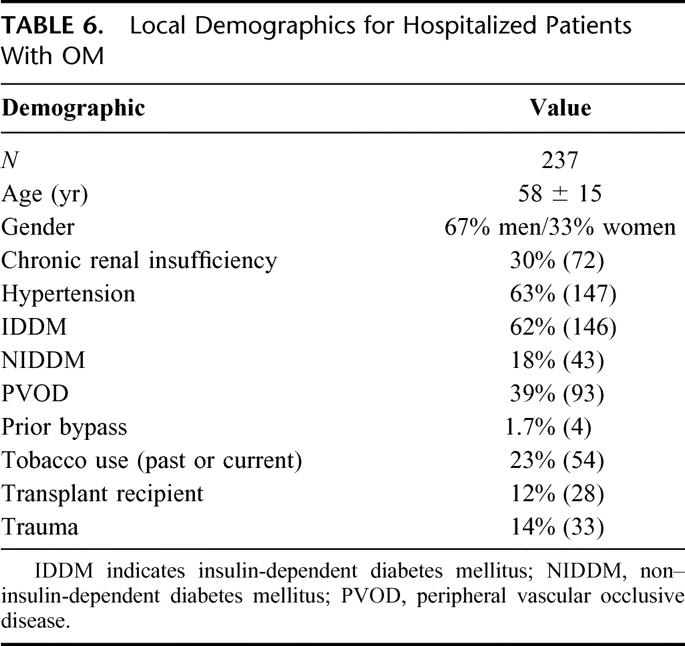
In our own experience, 237 patients were identified with digital OM, with a mean age of 58 years and 67% were men (Table 6). Age and gender distribution was similar to the NIS dataset. There was a high rate of DM (80%), as well as CRI (30%) and PVOD (39%), but only 25% used tobacco. Only 4 patients had a peripheral arterial reconstruction prior to their index OM admission, but 17 patients (16%) underwent a bypass at the same setting for the indication of tissue loss (eg, ulcer). Overall mortality was 24% (N = 57) during a mean follow-up of 31 months.
TABLE 6. Local Demographics for Hospitalized Patients With OM
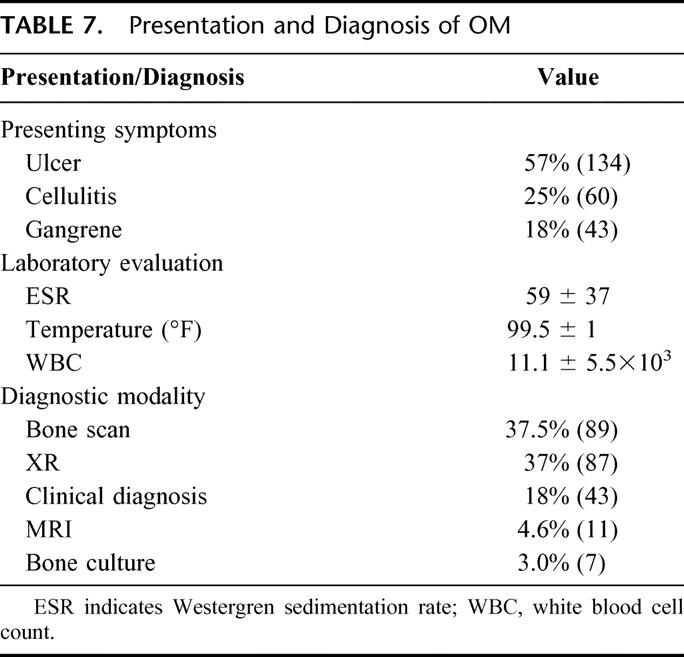
Most patients in the University of Michigan experience presented with a nonhealing foot ulcer, followed by cellulitis, and occasionally frank toe gangrene (Table 7). The mean admission laboratory values and patient temperature were often suggestive of a systemic infectious process. The diagnosis of OM was most commonly made by either plain radiographs of the feet, or a radionuclide bone scan. Clinical determination was the sole diagnostic measure in 18%, consisting usually of local wound exploration and probing of exposed bone. Only 7 patients had a positive preadmission bone culture confirming the existence of OM.
TABLE 7. Presentation and Diagnosis of OM
All patients at index admission were placed empirically on broad-spectrum IV antibiotics. The most commonly used antibiotics at admission were ampicillin/sulbactam, a flouroquinolone, piperacillin/tazobactam, or vancomycin. Slightly more than half of the patients had been on either outpatient IV antibiotics (19%) or on oral antibiotics (33%). In these cases, the mean preadmission duration of antibiotic usage was 5 ± 2 months. Overall, the number of separate preadmission antibiotic courses in all the patients was 1 ± 1.2, with 31% of patients having only 1 course, 15% having 2 courses, and 15% having ≥3 courses of antibiotic therapy. An antibiotic course was usually 6 to 12 weeks in duration.
Of those patients with more than 1 month follow-up (n=224) and excluding those with limb amputation on their index admission (n = 14), overall limb salvage was maintained by 168 patients (80%). Ninety-five patients (45%) underwent surgical therapy for OM at their index admission. Operations consisted of local debridement/ostectomy in 73 (77%), toe amputation in 19 (20%), and partial foot amputation in 3 (3%). Among these patients treated surgically, 3 (3%) required further local debridement, 8 (8.5%) required a later toe amputation, and 18 (18%) required a major amputation. Thus, patients who had initial surgical therapy had 82% limb salvage over 31 months of follow-up. Similarly, 24 patients undergoing medical therapy only (at their index admission) suffered major amputation over 31 months of follow-up. Thus, limb salvage for patients initially treated with medical therapy was 81% (P = not significant compared with surgical therapy).
HHS were used by 38 patients (16%) and in-hospital rehabilitation services were used by 43 patients (18%). Use of HHS was higher in those treated medically (21%) as compared with those undergoing surgical therapy (10%) (P = 0.034). No difference in utilization of in-hospital rehabilitation service was observed (medical 18%, surgical 18%). However, in those patients with limb salvage (n = 166), only 95 patients (57%) had a fully healed wound documented on the most recent clinical follow-up, whereas 64 (38%) had a chronic nonhealing wound, of which 53 had documented chronic OM. In 7 patients without major amputation (10%), it was not possible to determine the status of their wound.
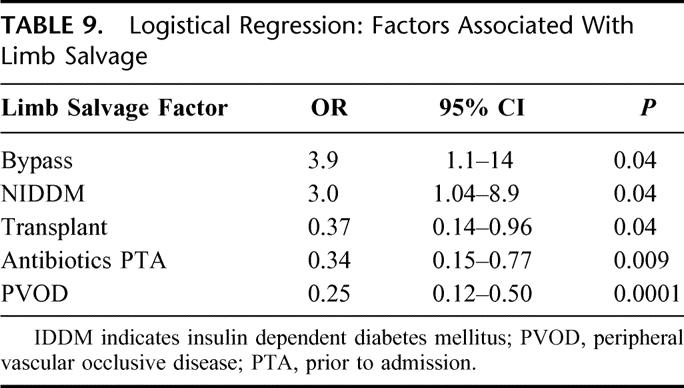
Adjusting for patient comorbidities and the effect of OM therapy on the outcomes of wound healing and limb salvage, patients were nearly threefold more likely to heal their wounds if their primary admitting symptoms were a cellulitis as compared with ulceration. An arterial reconstruction was highly protective for wound healing, while insulin-dependent DM and PVOD were associated with an increased incidence of a nonhealed wound (Table 8). Antibiotic use prior to index admission showed a strong association with worse wound healing (P = 0.07). Similarly, limb salvage was improved with an arterial bypass and presence of NIDDM (as compared with IDDM). Patients with a transplant (renal, kidney pancreas), PVOD, and antibiotics prior to admission were significantly less likely to maintain limb salvage (Table 9). Only the presence of CRI predicted shorter lifespan (odds ratio = 0.28; 95% confidence interval, 0.1–0.6; P = 0.0015).
TABLE 8. Logistical Regression: Factors Associated With a Healed Wound
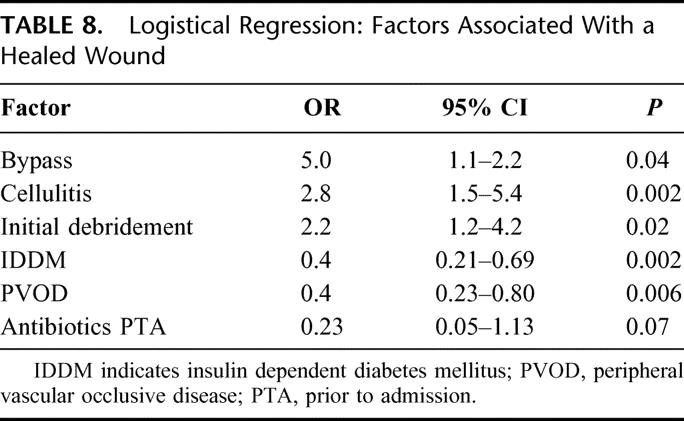
TABLE 9. Logistical Regression: Factors Associated With Limb Salvage
Kaplan-Meier analysis of limb salvage confirmed that patients with CRI and PVOD were less likely to maintain limb salvage as compared with the patients without these comorbidities (Fig. 1A, B). Mortality was increased in patients with CRI, but no other factors were significantly associated with death (Fig. 1C).
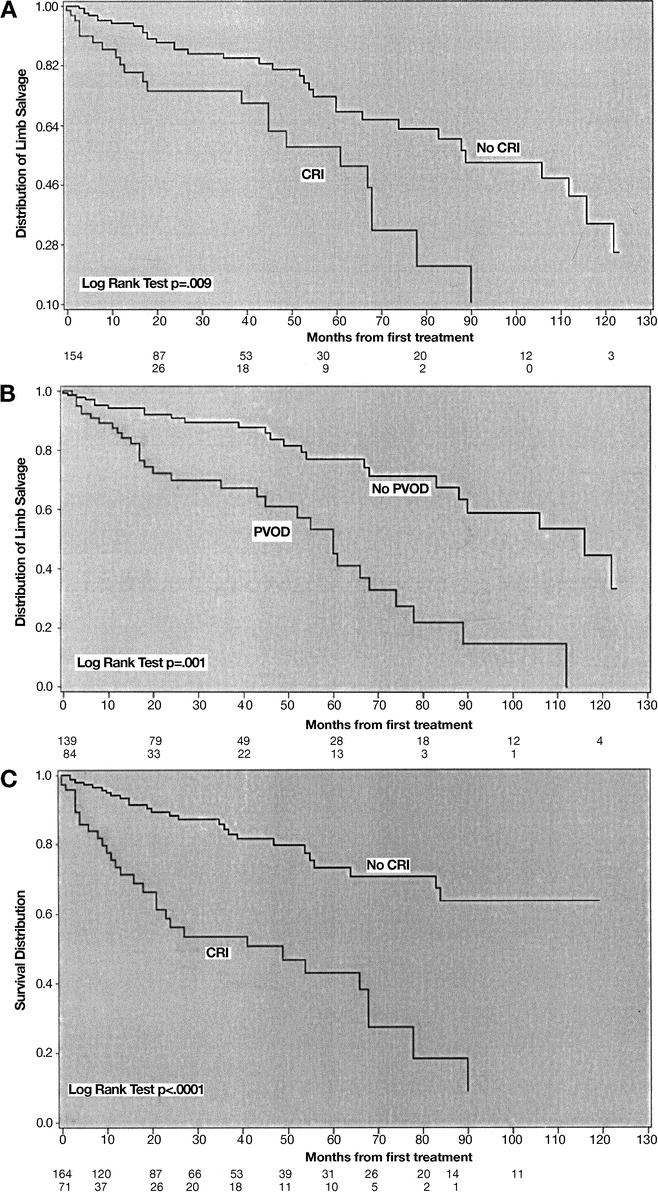
FIGURE 1. A, Kaplan-Meier life plot analysis of CRI and limb salvage. Limb salvage was significantly lower in those patients with CRI as compared with those without CRI (P = 0.009). The bottom numbers are patients at risk at each interval. B, Kaplan-Meier life plot analysis of PVOD and limb salvage. Limb salvage was significantly lower in those patients with PVOD as compared with those without (P = 0.001). The bottom numbers are patients at risk at each interval. C, Mortality was significantly worse in patients with CRI as compared with those without (P < 0.0001).
Discussion
This report substantiates the high cost of adult digital OM in both patient disability and resource utilization at the national level. Our series suggests that medical therapy alone is inferior to combined medical and surgical therapy for wound healing and limb salvage. Similar observations have been reported by others.3,6,16 Despite reports emphasizing the need for aggressive revascularization in patients with diabetes with tissue loss,2,12 such has not always been done in a timely manner. While initial surgical therapy was significantly associated with wound healing, it was not associated with limb salvage. This observation is supported by the fact that almost half of the patients with limb salvage had a wound that was not healed or had chronic OM, and underlies the fact that adequate arterial perfusion is the most important factor in maintaining limb salvage. This is further supported by the nearly fivefold increase in limb salvage in those who underwent an arterial bypass and a fourfold decrease in limb savage in those patients with concomitant PVOD. The patients in this report are different from the typical older patient with PVOD and tissue loss in that a minority had significant PVOD and tobacco use, but most were diabetic. However, a limb loss rate of 20% over approximately 3 years of follow-up is higher than that associated with claudication.17
Digital OM is extremely common in diabetic patients, particularly in the setting of PVOD.5,12,18 This report documents the significant interaction of these variables on lower extremity limb salvage. Older age was associated with a worse outcome in the national experience. One implication of this is that aggressive surgical therapy in the form of an arterial reconstruction is indicated, and early local surgical therapy in the elderly may be of greater benefit than in younger diabetic patients with OM. Importantly, a concomitant arterial reconstruction did not significantly increase mortality either at the national or local experience. Nevertheless, patients in the latter experience with CRI had a nearly 50% projected mortality at 5 years. This observation is consistent with the recent report by O'Hare et al that documented a 54% mortality in HD-dependent patients who required a peripheral bypass19 and the known annual death rate of HD-dependent renal failure patients of 16 of 100 patient-years.20 These patients represent an extremely high-risk group of patients for death and limb loss, regardless of therapy.
While the inpatient rate of major amputation was only 8%, our own experience suggests a substantially higher rate over time. Not surprisingly, patients admitted with OM had a twofold increased mortality and unfavorable discharge if they underwent a major amputation, whereas minor amputation was protective from mortality, risk of major amputation, and unfavorable discharge. Although difficult to demonstrate cause and effect from administrative databases at the patient level,15 these data suggest that minor amputation (eg, getting rid of the infection) may decrease the risk of major amputation as well as facilitate faster recovery (and more likely discharged to home). Interestingly, patients with emergent admission were less likely to receive either a major or minor amputation, suggesting that most patients with foot and digit OM had electively scheduled amputations. Geographic rates of major amputation in the setting of diabetic associated OM vary more than 10-fold,21 suggesting a lack of standardized care guidelines.
Our data suggest that prolonged preadmission antibiotic treatment may decrease the chance of wound healing, and is associated with significantly less chance of limb salvage. The reasons for this may include development of antibiotic-resistant organisms and delayed removal of an infected bone nidus that allows advanced contiguous spread of OM. For example, a small ulcer with underlying OM may develop a deep space infection, with subsequent sepsis. Urgent amputation then becomes necessary. However, it is more likely that a delay due to prolonged outpatient antibiotics may allow progressive tissue loss to occur and loss of the window of opportunity to maintain limb salvage with an arterial reconstruction. Two reports have promulgated antibiotic use alone in adults with OM. One report reviewed 48 patients with OM treated by antibiotics alone for 3 months with 1-year follow-up. However, 18 patients failed therapy and amputation was required in 9 (18% limb loss rate).11 Another study reported 51 patients with OM treated solely with antibiotics with a 19-month follow-up.10 Of these patients, 15 required major amputation (29%), which is higher than the rate in the current report.
While patients who received IV antibiotics at the national level were less likely to have a major or minor amputation, this only reflects antibiotic treatment during their inpatient stay. Thus, this observation is not inconsistent with our own series as prolonged preadmission antibiotics were associated with lower limb salvage, while most all patients treated surgically or medically received inpatient antibiotics during their index admission. The cost, inconvenience, and potential complications of fungal or bacterial superinfection (eg, Clostridium difficile colitis) were not specifically analyzed in this study but are relevant when considering prolonged antibiotic use.
Diagnostic measures for OM are variable and seemingly practitioner-dependent. Magnetic resonance imaging is probably the most sensitive and specific test for OM.3,16,22 However, simple clinical examination and ability to probe a bony structure beneath an ulcer are highly sensitive for OM presence.23 If bone is exposed or is easily probed, it is by definition infected, and therapy can commence without further expensive testing. Certainly, an ostectomy is not indicated if no OM is present. Patients with no exposed bone and those who present with cellulitis may benefit from radiologic tests to confirm the presence or absence of OM. Cellulitis alone, in contrast to an open ulcer, was also associated with a 2.8-fold increase in likelihood of wound healing.
Equally important is determining whether the patient has significant PVOD.3,24,25 Patients with DM and PVOD have a documented increased cost of care and risk of amputation.4 Noninvasive means of assessing foot perfusion are often inaccurate in the setting of DM and CRI because of medial vessel calcification.2,26 Thus, patients with nonpalpable distal pulses and tissue loss should probably have an arteriogram or MRA to assess the need for arterial reconstruction.24 In the current study, a bypass performed at index admission was highly protective for wound healing and limb salvage. Indeed, a recent review highlighted this in a treatment algorithm.3 This report also suggests that solid organ transplant recipient patients are at higher risk of limb loss with conservative OM management and may benefit to the same degree that patients with insulin-dependent DM do (Table 8). Although not analyzed in this study, a report suggested that kidney/pancreas transplants have a continued significant risk of PVOD complications.27
Significant costs accompany outpatient clinical visits, rehabilitation facility use, and HHS utilization for long-term wound care and antibiotics in patients with OM. Not surprisingly, most patients who failed to heal their wounds were those requiring prolonged HHS, and those patients not receiving initial surgical therapy were significantly more likely to use HHS. On the other hand, the advent of these services may have accounted for the patients’ significantly decreased LOS. Many patients had ulcers persisting for months to years after their index OM admission. The resulting costs and time lost were not able to be quantified in this study. However, other reports have suggested a typical outpatient cost of $28,000 per patient per ulcer.4 Since surgical therapy is likely to shorten the duration of outpatient therapy, it would also decrease direct and indirect patient cost for OM treatment. In this regard, a comprehensive, multidisciplinary care approach with consideration of the comorbidities of DM and the associated neuropathy is important in preventing OM recurrence.3,28
Limitations in the current study are several. First, it is neither randomized nor prospective, and its conclusions require validation by such a study. However, unlike the ease of randomizing patients to different medical therapies, patients may be hesitant to consent for an early operation without trying prolonged antibiotics first. Second, patient-specific outcomes from the NIS dataset need to be viewed with caution, as coding errors occur.15 Finally, while our criteria were consistent when evaluating the patient records in terms of wound healing, this was determined from clinical notes, which might not be as accurate as prospectively gathered data. However, it is likely that any misclassification of wound healing was equal between the 2 groups.
From these data, several conclusions can be made. First, aggressive comprehensive care of the diabetic patient with digital OM will likely improve outcomes, similar to other specialized multidisciplinary practices.3,25 Second, patients with insulin-dependent DM, PVOD, and an ulcer almost always require revascularization and digital debridement to maintain limb salvage. These patients should be treated aggressively if their overall condition allows. Lastly, these results beg for a randomized, multi-institutional, prospective trial comparing 1) prolonged antibiotic use with standard wound care, and 2) limited antibiotic use with surgical therapy, to definitively answer the questions raised in this review.
ACKNOWLEDGMENTS
The authors thank D. Segur for administrative support.
Discussions
Dr. Hiram C. Polk, Jr. (Louisville, Kentucky): This paper by Drs. Henke et al represents a second fundamental look at a common surgical problem that Dr. Henke has done within the last few years with awakening results. His previous assessment of the correct use of blood cultures in surgical ICU patients is a good example. I have some brief comments and a couple of simple questions.
First of all, this methodology of using the national database and then supplementing that with a more detailed look at a significant number of your own patients is really a good idea, and we need to apply this much more broadly. They are powerful tools, and they are very persuasive to some of our payors.
The constant costs despite shortening stays in the hospital are really very interesting. And if you pay attention and follow my bias, the extent of the home health care makes medical management of this without surgical intervention even more costly, in fact prohibitively costly. Most of you know that home health care far exceeds the cost of what surgeons get paid for taking care of these patients, and it is a pervasive problem not only for us but for those of us who contribute to the Medicare trust fund through our taxes.
I don't think anybody would be surprised by a paper by surgeons recommending surgery, and a foreign body, which a dead bone is, after all, needs to be removed. However, this is a particularly damning look at preadmission antibiotic use, perhaps the most dramatic figure in this whole paper, with the 5 ± 2 months of preadmission antibiotic use. I guess the right question would be to consider how many ID consultants were involved in that process, for how long, and how many laboratory cultures were done. In fact, President Townsend commented on some interest I had in antibiotics, where I spent the last half of my life trying to narrow the use of antibiotics both in spectrum and duration. It is obvious this is a clear area of clinical failure.
This paper may be even more timely than the Program Committee or the authors know. An important piece of the next round of Medicaid ASO contracts that will come out at the next level, under the influence of Medicare, CMS will focus upon diabetes, and a special piece of this is going to be the management of the diabetic foot. The management issue gives another chance for us to put surgical care in the ideal environment both as being effective and cost-effective.
Dr. James M. Seeger (Gainesville, Florida): This study indeed addresses an important but overlooked problem, the appropriate management of patients with pedal osteomyelitis. The authors’ conclusion from the study is that initial surgical debridement rather than prolonged antibiotic administration leads to improved wound healing and limb salvage, certainly a bias that I share, and the data presented here support that. However, the study design of a retrospective analysis of a local series from the University of Michigan and an examination of the National Inpatient Sample, a national administrative, limit the strength of this conclusion. It is these limitations that prompt my questions for the authors.
First, from the analysis of the National Inpatient Sample, the authors conclude that age, emergency admission, and amputation predict mortality, while age, renal failure, and black race predict amputation. While these findings are interesting, particularly the confirmation of the increased risk of amputation in black patients, an observation we have previously reported at this meeting, how does this information help in determining the best management of patients presenting with pedal osteomyelitis?
Second, from the analysis of your local series, you observed that patients presenting with cellulitis and those with arterial reconstructive procedures were more likely to achieve wound healing and limb salvage while those with insulin-dependent diabetes mellitus, peripheral arterial occlusive disease, chronic renal insufficiency, and, most interestingly, antibiotics prior to admission, were more likely to have non-healing wounds and limb loss.
With the exception of antibiotic use, these are all intuitively logical conclusions. But being a skeptic of intuitive conclusions, I am concerned about selection bias in this these observations from your retrospective analysis and hope you can help me with this.
Specifically, why were patients in your local series selected for antibiotic treatment alone versus surgical debridement? Were they sicker? Was their infection more chronic or more diffused? Did they have a less favorable pattern of occlusive disease for reconstruction? Furthermore, what happened to the patients treated with antibiotics alone? Did they have subsequent debridement, bypasses, simply proceed to major amputation? If amputation was the outcome, was it a delay in surgical referral that necessitated this or was there no other option for these patients even if they had been seen earlier? Finally, does prolonged antibiotic use simply predict elderly patients with ulcerations, insulin-dependent diabetes mellitis, chronic renal insufficiency, and unreconstructible arterial occlusive disease factors that predict limb loss regardless of the type of treatment used? Or is there an opportunity for limb salvage in a substantial number of patients presenting with pedal osteomyelitis by earlier debridement and revascularization?
Overall, I enjoyed your presentation and I commend you for your study of an important but overlooked problem. As expected from a good study, you have raised more questions than you have answered. I hope you continue to investigate this issue so that we can better understand the appropriate role of surgical debridement and revascularization.
Dr. William C. Lineaweaver (Jackson, Mississippi): The title of this presentation was “Lower Extremity Osteomyelitis.” But I gather that the lesions were predominantly amongst the toes. Was there any analysis made on specific sites, for example, distal phalangeal lesions versus metatarsophalangeal lesions? Because that particular distinction can make a huge difference.
Second of all, what were the criteria for diagnosis of osteomyelitis? We see a wide number of these lesions. Some of them simply are chronically infected synovium. Some of them are joint space infections that are relatively urgent. Some of them do involve bone, but many of them don't. We tend to restrict our diagnosis of osteomyelitis to cultured bone. So I would be interested to see what the criteria were for the diagnosis in this study.
Dr. Peter Henke (Ann Arbor, Michigan): Dr. Polk, I appreciate your kind comments. And just to note something you brought up, home health nursing utilization is significantly greater over the last several years, and I think that does account for some of the decreased length of stay over that same period of time. It is of interest that about 21% of the patients primarily treated medically required home health services while only 10% required this if they were surgically treated, and this was statistically significant. Unfortunately, I don't have any idea about the exact costs with this, but I suspect they are high.
In terms of your question about ID consultants: Almost every patient had a consult because to get formarily use of IV antibiotics, ID is automatically consulted, in part, because I guess we can't or don't know how to choose antibiotics.
Dr. Seeger, I appreciate your comments as well. As we have seen today, the strength of the administrative database is the large patient numbers in real world nonselected practice. Thus, mortality, length of stay, costs, and procedures are really quite accurate. But using the administrative data for patient level specific outcomes is less rigorous, and patient co-morbidities can be miscoded or noncoded depending on the number of ICD-9CM coding slots they have. Thus, increased age and black race may mask and this is a hunch more severe or advanced atherosclerotic disease or more advanced infection. So for older black patients, we should have a heightened awareness of OM.
In terms of your second question, we did use the same ICD 9 codes to capture all consecutive patients with a hospital admission, and we did not try to bias toward only patients who had had a surgical procedure or were just medical therapy. We did not include any of those who were treated primarily as outpatients. So I think we did lose some patients that way.
To more specifically address your question, the choice of medical versus surgical therapy was really attending and service dependent. We used medical or surgical therapy as a point of reference to determine their pre- and then postoperative or post-therapy courses, which is somewhat arbitrary. In general, they were not necessarily a sicker group of patients, except they were more likely to have peripheral vascular occlusive disease and diabetes by basis of our multivariate analysis.
You also bring up an important point that needs to be emphasized, and that is the patients who were initially treated surgically had a very similar overall limb salvage as those treated medically over a 31-month follow-up. For example, surgery patients had 18 amputations, whereas medical patients had 24 major amputations and the overall limb salvage, as was noted, was about 80%. Why initial surgical debridement predicted wound healing but not limb salvage emphasizes the point that limb salvage is mainly an issue of adequate blood flow to the limb.
I agree that one of the main points of the paper is antibiotic usage. Again, prolonged, or really pre-admission antibiotics, which is how we identified this, conferred both worse wound healing (almost statistically significant) and significantly worse limb salvage. I do believe this is an independent effect, as the other factors you mentioned were included in the multivariate analysis, and this still settled out as an independent variable. I do believe this may mask a true delay in surgical therapy, and you have a limited window in many of these patients for revascularization for limb salvage. Another hypothesis is that prolonged antibiotics may select out more virulent organisms that get within the bone and the foot that then even if you do a bypass “the cat is out of the bag” and improving blood flow will not help.
Dr. Lineaweaver, we did not specifically characterize each location of where the OM was on the foot. They were primarily digit or over the metatarsal heads. There were very few with heel ulcers, which are certainly harder to take care of. From the table, most of the patients had confirmed radiological studies such as MR, bone scan, with some clinical diagnoses as probing bone. And only 3% had bone cultures, which I think is also a real problem because you are unable to narrow your antibiotics nor confirm the organism.
Footnotes
Reprints: Peter K. Henke, MD, University of Michigan Health System, 1500 East Medical Center Drive, 2210 Taubman Health Care Center, Ann Arbor, MI 48109-0329. E-mail: henke@umich.edu.
REFERENCES
- 1.Caputo GM, Cavanagh PR, Ulbrecht JS, et al. Assessment and management of foot disease in patients with diabetes. N Engl J Med. 1994;331:854–860. [DOI] [PubMed] [Google Scholar]
- 2.Akbari CM, Pomposelli FB Jr, Gibbons GW, et al. Lower extremity revascularization in diabetes: late observations. Arch Surg. 2000;135:452–456. [DOI] [PubMed] [Google Scholar]
- 3.Boulton AJ, Kirsner RS, Vileikyte L. Clinical practice: neuropathic diabetic foot ulcers. N Engl J Med. 2004;351:48–55. [DOI] [PubMed] [Google Scholar]
- 4.Ramsey SD, Newton K, Blough D, et al. Incidence, outcomes, and cost of foot ulcers in patients with diabetes. Diabetes Care. 1999;22:382–387. [DOI] [PubMed] [Google Scholar]
- 5.Kellicut DC 3rd, Sidawy AN, Arora S. Diabetic vascular disease and its management. Semin Vasc Surg. 2003;16:12–18. [DOI] [PubMed] [Google Scholar]
- 6.Ha Van G, Siney H, Danan JP, et al. Treatment of osteomyelitis in the diabetic foot: contribution of conservative surgery. Diabetes Care. 1996;19:1257–1260. [DOI] [PubMed] [Google Scholar]
- 7.Venkatesan P, Lawn S, Macfarlane RM, et al. Conservative management of osteomyelitis in the feet of diabetic patients. Diabet Med. 1997;14:487–490. [DOI] [PubMed] [Google Scholar]
- 8.Chaytor ER. Surgical treatment of the diabetic foot. Diabetes Metab Res Rev. 2000;16(suppl 1):66–69. [DOI] [PubMed] [Google Scholar]
- 9.Lipsky BA, Berendt AR. Principles and practice of antibiotic therapy of diabetic foot infections. Diabetes Metab Res Rev. 2000;16(suppl 1):42–46. [DOI] [PubMed] [Google Scholar]
- 10.Bamberger DM, Daus GP, Gerding DN. Osteomyelitis in the feet of diabetic patients: long-term results, prognostic factors, and the role of antimicrobial and surgical therapy. Am J Med. 1987;83:653–660. [DOI] [PubMed] [Google Scholar]
- 11.Peterson LR, Lissack LM, Canter K, et al. Therapy of lower extremity infections with ciprofloxacin in patients with diabetes mellitus, peripheral vascular disease, or both. Am J Med. 1989;86(6 Pt 2):801–808. [DOI] [PubMed] [Google Scholar]
- 12.Faries PL, Brophy D, LoGerfo FW, et al. Combined iliac angioplasty and infrainguinal revascularization surgery are effective in diabetic patients with multilevel arterial disease. Ann Vasc Surg. 2001;15:67–72. [DOI] [PubMed] [Google Scholar]
- 13.Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project (HCUP-9): Nationwide Inpatient Sample, Release 9 2000. Agency for Healthcare Research and Quality, 2000.
- 14.Public Health Service UDoHaHS. International Classification of Diseases, 9th Revision [clinical modification]. Washington, DC: Public Health Service UdoHaHS, 1988. [Google Scholar]
- 15.Birkmeyer JD. Using administative data for clinical research. In: Souba W, Wilmore D, eds. Surgical Research. 2001.
- 16.Lipsky BA. Osteomyelitis of the foot in diabetic patients. Clin Infect Dis. 1997;25:1318–1326. [DOI] [PubMed] [Google Scholar]
- 17.Taylor LM, Jr. Natural history and nonoperative treatment of chronic lower extremity ischemia. In: Rutherford R, ed. Vascular Surgery, 5th ed. 2000.
- 18.Akbari CM, Macsata R, Smith BM, et al. Overview of the diabetic foot. Semin Vasc Surg. 2003;16:3–11. [DOI] [PubMed] [Google Scholar]
- 19.O'Hare AM, Sidawy AN, Feinglass J, et al. Influence of renal insufficiency on limb loss and mortality after initial lower extremity surgical revascularization. J Vasc Surg. 2004;39:709–716. [DOI] [PubMed] [Google Scholar]
- 20.Wolfe RA, Ashby VB, Milford EL, et al. Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. N Engl J Med. 1999;341:1725–1730. [DOI] [PubMed] [Google Scholar]
- 21.Wrobel JS, Mayfield JA, Reiber GE. Geographic variation of lower-extremity major amputation in individuals with and without diabetes in the Medicare population. Diabetes Care. 2001;24:860–864. [DOI] [PubMed] [Google Scholar]
- 22.Wakefield MC, Kan VL, Arora S, et al. Nonoperative management of diabetic foot infections. Semin Vasc Surg. 2003;16:79–85. [DOI] [PubMed] [Google Scholar]
- 23.Grayson ML, Gibbons GW, Balogh K, et al. Probing to bone in infected pedal ulcers: a clinical sign of underlying osteomyelitis in diabetic patients. JAMA. 1995;273:721–723. [PubMed] [Google Scholar]
- 24.LoGerfo FW, Gibbons GW, Pomposelli FB Jr, et al. Trends in the care of the diabetic foot: expanded role of arterial reconstruction. Arch Surg. 1992;127:617–620. [DOI] [PubMed] [Google Scholar]
- 25.American Diabetes Association. Peripheral arterial disease in people with diabetes. Diabetes Care. 2003;26:3333–3341. [DOI] [PubMed] [Google Scholar]
- 26.Pomposelli FB Jr, Marcaccio EJ, Gibbons GW, et al. Dorsalis pedis arterial bypass: durable limb salvage for foot ischemia in patients with diabetes mellitus. J Vasc Surg. 1995;21:375–384. [DOI] [PubMed] [Google Scholar]
- 27.Morrissey PE, Shaffer D, Monaco AP, et al. Peripheral vascular disease after kidney-pancreas transplantation in diabetic patients with end-stage renal disease. Arch Surg. 1997;132:358–361. [DOI] [PubMed] [Google Scholar]
- 28.Parkhouse N, Le Quesne PM. Impaired neurogenic vascular response in patients with diabetes and neuropathic foot lesions. N Engl J Med. 1988;318:1306–1309. [DOI] [PubMed] [Google Scholar]


