Abstract
Objective:
Prospectively evaluate whether for patients having laparoscopic cholecystectomy with failed trans-cystic duct clearance of bile duct (BD) stones they should have laparoscopic choledochotomy or postoperative endoscopic retrograde cholangiography (ERCP).
Summary Background Data:
Clinical management of BD stones found at laparoscopic cholecystectomy in the last decade has focused on pre-cholecystectomy detection with ERCP clearance in those with suspected stones. This clinical algorithm successfully clears the stones in most patients, but no stones are found in 20% to 60% of patients and rare unpredictably severe ERCP morbidity can result in this group. Our initial experience of 300 consecutive patients with fluoroscopic cholangiography and intraoperative clearance demonstrated that, for the pattern of stone disease we see, 66% of patients’ BD stones can be cleared via the cystic duct with dramatic reduction in morbidity compared to the 33% requiring choledochotomy or ERCP. Given the limitations of the preoperative approach to BD stone clearance, this trial was designed to explore the limitations, for patients failing laparoscopic trans-cystic clearance, of laparoscopic choledochotomy or postoperative ERCP.
Methods:
Across 7 metropolitan hospitals after failed trans-cystic duct clearance, patients were intraoperatively randomized to have either laparoscopic choledochotomy or postoperative ERCP. Exclusion criteria were: ERCP prior to referral for cholecystectomy, severe cholangitis or pancreatitis requiring immediate ERCP drainage, common BD diameter of less than 7 mm diameter, or if bilio-enteric drainage was required in addition to stone clearance. Drain decompression of the cleared BD was used in the presence of cholangitis, an edematous ampulla due to instrumentation or stone impaction and technical difficulties from local inflammation and fibrosis. The ERCP occurred prior to discharge from hospital. Mechanical and extracorporeal shockwave lithotripsy was available. Sphincter balloon dilation as an alternative to sphincterotomy to allow stone extraction was not used. Major endpoints for the trial were operative time, morbidity, retained stone rate, reoperation rate, and hospital stay.
Results:
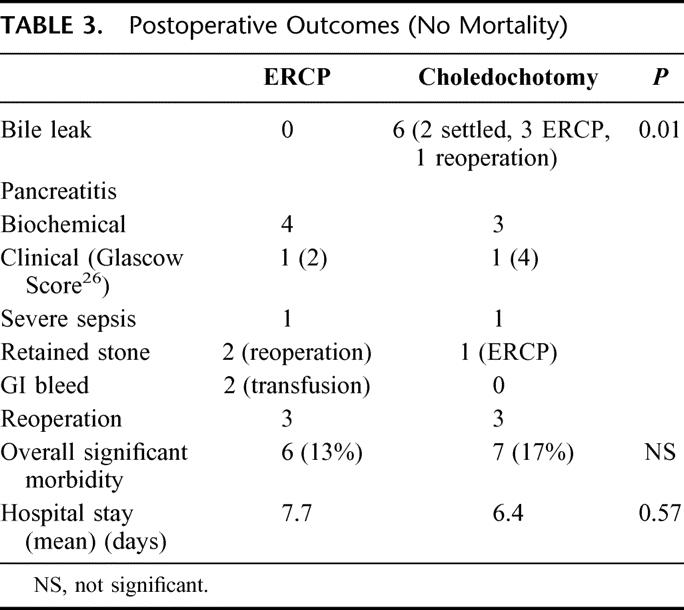
From June 1998 to February 2003, 372 patients with BD stones had successful trans-cystic duct clearance of stones in 286, leaving 86 patients randomized into the trial. Total operative time was 10.9 minutes longer in the choledochotomy group (158.8 minutes), with slightly shorter hospital stay 6.4 days versus 7.7 days. Bile leak occurred in 14.6% of those having choledochotomy with similar rates of pancreatitis (7.3% versus 8.8%), retained stones (2.4% versus 4.4%), reoperation (7.3% versus 6.6%), and overall morbidity (17% versus 13%).
Conclusions:
These data suggest that the majority of secondary BD stones can be diagnosed at the time of cholecystectomy and cleared trans-cystically, with those failing having either choledochotomy or postoperative ERCP. However, because of the small trial size, a significant chance exists that small differences in outcome may exist. We would avoid choledochotomy in ducts less than 7 mm measured at the time of operative cholangiogram and severely inflamed friable tissues leading to a difficult dissection. We would advocate choledochotomy as a good choice for patients after Billroth 11 gastrectomy, failed ERCP access, or where long delays would occur for patient transfer to other locations for the ERCP.
For 372 patients with bile duct stones detected on operative cholangiography, after failed laparoscopic trans-cystic duct stone clearance in 86, laparoscopic choledochotomy was randomly compared with postoperative ERCP. Retained stone rate 2.4% versus 4.4%, reoperation 7.3% versus 6.6%, overall morbidity and hospital stay, 6.4 days versus 7.7 days, appeared comparable. These data suggest surgical experience, ERCP availability, and patient factors may be the most important determinants of which modality is chosen.
The ideal management of bile duct (BD) stones in the era of laparoscopic cholecystectomy remains controversial. Options range from endoscopic retrograde cholangiography (ERCP) in all or selected patients, through to clearance of theBD through the cyctic duct or via laparoscopic choledochotomy.
Clinical management of BD stones in the last decade has focused on precholecystectomy detection with ERCP clearance in those with suspected stones.2,3,11,14 This clinical algorithm successfully clears the stones in most patients, but no stones are found in 20% to 60% of patients, and rare unpredictable severe morbidity can result in this group. Increasing efforts to reduce the number of nontherapeutic ERCPs using MRCP3 and endoscopic ultrasound11 are being undertaken. Our initial experience of 300 consecutive patients with fluoroscopic cholangiography and intraoperative clearance demonstrated that, for the pattern of stone disease we see, 66% of patients’ BD stones can be cleared via the cystic duct with dramatic reduction in morbidity compared with the 33% requiring choledochotomy or ERCP.23 Furthermore, increased accuracy of detecting BD stones prior to cholecystectomy has not yet been able to predict which stones will be able to be extracted via the cystic duct and which patients would require choledochotomy or ERCP.
Given the limitations of the preoperative approach to BD stone clearance, this trial was designed to explore the limitations of the alternative approach where, for patients failing laparoscopic transcystic BD stone clearance during cholecystectomy, we compared the outcomes of BD stone clearance by laparoscopic choledochotomy or postoperative ERCP.
METHODS
Within 7 Brisbane metropolitan hospitals, patients with symptomatic gallstones and suspected BD calculi on the basis of clinical presentation of raised liver function tests, jaundice, biliary pancreatitis, cholangitis, or imaging showing BD stones or BD dilation were consented for the trial.
Exclusion criteria were: ERCP prior to referral for cholecystectomy, severe cholangitis or pancreatitis requiring immediate ERCP drainage, common BD diameter of less than 7 mm diameter at operative cholangiography, or if bilioenteric drainage was required in addition to stone clearance.
Laparoscopic exposure was obtained using one 11-mm Hasson port for the telescopes and three 5-mm subcostal ports. Additional ports were placed if improved exposure was required. All suspected BD calculi had these confirmed by operative cholangiogram. Where feasible, these were removed by transcystic clearance. Inability to clear the stones transcystically led to intraoperative randomization for either choledochotomy or postoperative ERCP. Randomization was achieved by phone call to the trial center available 24 hours a day.
Prophylactic antibiotics were used, usually third-generation cephalosporins. Choledochotomy was by supraduodenal exposure of common BD and longitudinal incision to a length sufficient to easily deliver stones. Stone clearance was achieved using irrigation, Fogarty balloon sweeps, and Dormia basket deployment with flexible choledochoscopic guidance. Complete clearance was finally checked using both choledochoscopy and then proximal, and distal fluoroscopic cholangiography. Choledochotomy closure was achieved with monofilament absorbable sutures.
Drain decompression of the cleared BD was used in the presence of cholangitis, an edematous ampulla due to instrumentation or stone impaction and technical difficulties from local inflammation and fibrosis. When BD decompression was used, the choice of passing an antegrade 10-Fr stent across the ampulla of Vater27 or T-tube insertion was left up to individual surgeon's choice. Closure of the cystic duct was by clips or endoloop. Subhepatic peritoneal closed suction drainage was routinely used in all cases.
T-tube removal after check cholangiography was performed after a minimum of 3 weeks. Antegrade stents were removed by endoscopy after 4 weeks.
The patients randomized to ERCP BD clearance proceeded to cholecystectomy with cystic duct ligation with an endoloop. Subrandomization of this group occurred with half of the patients having transcystic antegrade 10-Fr transampullary stent insertion.27 A subhepatic peritoneal closed suction drain was placed and ERCP clearance of the BD was planned by immediate postoperative phone contact with the participating gastroenterologist. The ERCP occurred prior to discharge from hospital.
ERCP clearance was performed with the assistance of an anesthetist. Side viewing duodenoscopes were used with standard and needle knife papillotomes when precut papillotomy was required. Mechanical and extracorporeal shockwave lithotripsy was available. Sphincter balloon dilation as an alternative to sphincterotomy to allow stone extraction was not used.
Operative time was calculated on the basis of the surgical procedure(s) added to time taken to perform ERCP(s). Bile leak was defined as the presence of any bile in the subhepatic peritoneal suction drains. Hospital stay was calculated from the date of operation until discharge. Major endpoints for the trial were operative time, morbidity, retained stone rate, reoperation rate, and hospital stay.
Participating surgeons were experienced laparoscopic biliary surgeons with a large published experienced in laparoscopic choledochotomy and suture techniques.23 Initial trial design estimates of 262 patients were based on the desire to detect a 15% difference of means of endpoints with a 80% power at the 5% level. The trial was concluded after 5 years of patient accrual and prior to reaching our target numbers. Monitoring of slow accrual led to attempts to broaden the trial to multiple centers around Australia but was not successful. Recalculation of trial power with a total of 86 patients gives an 80% expectation that a 25% difference in endpoints would have been detected at the 5% level.1
Analysis of results was based on the intention-to-treat randomization.
Trial design, informed consent, and procedures were carried out according to the Declaration of Helsinki 1976 as subsequently modified by the Australian Health and Medical Research Council on Human Experiments and on Scientific Practice. Ethical review and agreement for the conduct of the trial within the Brisbane metropolitan area were granted by each of the 7 separate participating hospitals’ human ethics trial review committees.
RESULTS
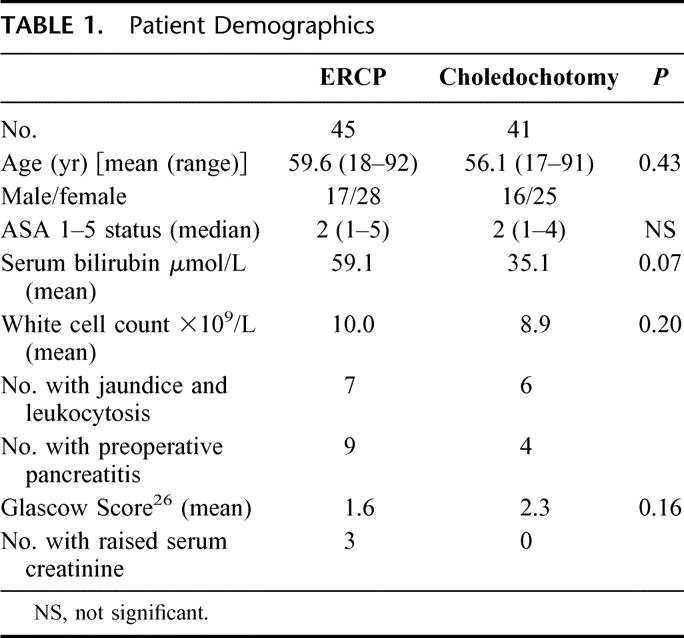
From June 1998 to February 2003, 372 patients had BD stones documented by transcystic cholangiography at the time of laparoscopic cholecystectomy; 286 patients had successful transcystic duct clearance of stones, leaving 86 patients randomized into the trial (Fig. 1). All patients randomized had the allocated treatment performed. The patient demographics are shown in Table 1. There was a trend to higher mean bilirubin in the ERCP group. Those patients with preoperative pancreatitis had mild to moderate disease as evident on their Glasgow scoring. Only 1 patient in this group continued with pancreatitis as a feature of the postoperative course.
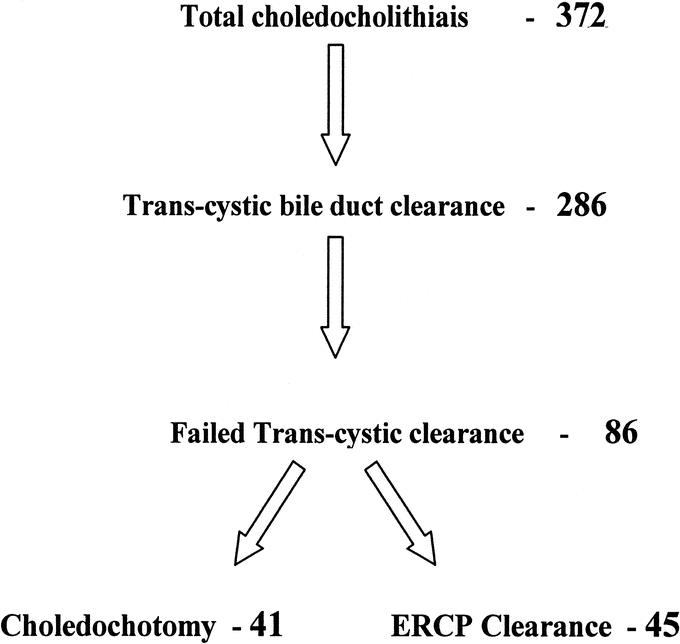
FIGURE 1. Trial Randomization.
TABLE 1. Patient Demographics
In the postoperative recovery, bile was detected in the subhepatic drain of 5 patients, 2 settling after a few days observation. In the 3 with ongoing bile leak, 2 were treated by ERCP, and 1 by laparoscopic reoperation and cystic duct stump religation. Bile leak occurred in 4 of 24 primary duct closures and 1 of the 10 with primary closure and stent. One patient after removal of T-tube 22 days postoperatively developed bile peritonitis requiring ERCP to control.
Pancreatitis developed in the postoperative period in 9 patients. In 7 patients, this was entirely biochemical, with untroubled recovery. One further patient in each group, however, developed clinical pancreatitis of moderate severity, neither requiring reoperation.
Early reoperation was required in 4 patients. Two ERCP patients required operation for failed ERCP clearance of stones. As mentioned above, 1 patient in the choledochotomy arm had reoperation for cystic stump leak and another for signs of sepsis (nil found) prior to being transferred to the ICU.
Perioperative details are contrasted in Table 2. No patient in the ERCP group had more than 2 ERCPs.
TABLE 2. Operative Data
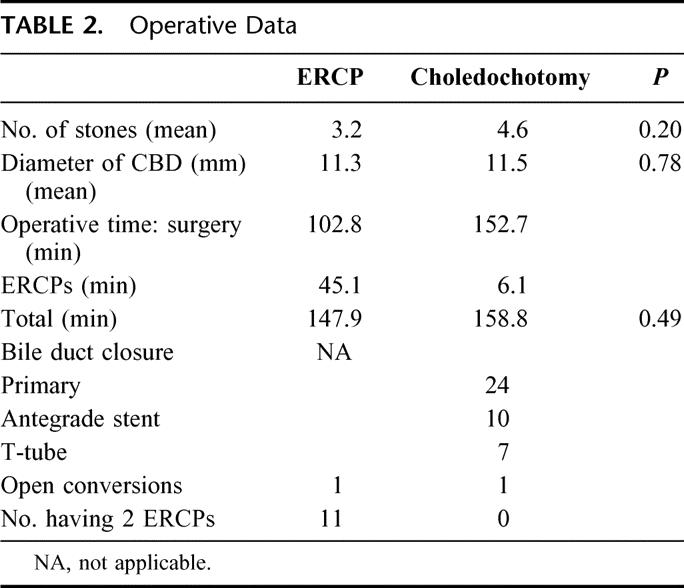
For those having choledochotomy, BD diameters in the groups were similar: 9.6 mm in the T-tube group, 12 mm in the primary closure group, and 12 mm in the primary closure with stent group. However, operative times for the groups, 202 minutes, 121 minutes, and 192 minutes, respectively, were different (P < 0.006). This probably reflected the surgeon's choice of reserving drainage for the more technically complex cases. One late reoperation has occurred in each patient group. The choledochotomy patient 12 months after primary closure of an 11-mm diameter duct developed a stricture in that area, which was repaired by Roux-en-Y jejunal reconstruction. The ERCP patient presented 10 months postoperatively with a stricture at the cystic duct stump level (9-mm duct) and also required Roux-en-Y reconstruction.
One patient in the choledochotomy group proved to have a carcinoma of the lung, and 1 in the ERCP group was found to have a carcinoma of the head of pancreas.
DISCUSSION
Bile duct stones seen in Australia are largely a result of migration down the cystic duct with a small percentage of older patients having primary duct stones. Presentation with Asian recurrent pyogenic cholangitis is rare. For most of our patients, cholecystectomy remains central to prevent stone reformation.17
Laparoscopic cholecystectomy has tended to encourage surgeons to clear the BD of stones preoperatively by ERCP.2,3,11,14,16,21,24 Indeed, most efforts in this area center on efforts to make these ERCPs more frequently therapeutic and less often diagnostic given its inherent cost and morbidity.3,12,13,15 This trend occurred despite data in the open cholecystectomy era to suggest one-stage surgical clearance was superior to 2-stage clearance using ERCP preoperatively.28 Patients still have stones detected on operative cholangiograms by surgeons using this approach, who are then left with the dilemma of relying on postoperative ERCP, a laparoscopic exploration and its technical demands, or a more familiar open choledochotomy.
Our initial approach at cholecystectomy as it evolved as a laparoscopic procedure was to continue the logic of single-stage surgical approach if possible.4,5,7,9,10,19 Interestingly, improved laparoscopic transcystic BD stone extraction techniques evolved (not exploited in open cholecytectomy), allowing two thirds of these stones, detected on operative cholangiogram at the time, to be removed transcystically, and patients recover in a manner very similar to uncomplicated laparoscopic cholecystectomy18–25 (Fig. 1). This approach not only avoids the risks inherent in ERCP to healthy young patients without BD stones, but preoperatively simplifies most patient investigation to an ultrasound and liver function tests.6 The cholangiogram also adds increased security to the dissection by increased information about biliary anatomy. This clinical approach does, however, hinge on the simple technique of performing an operative cholangiogram.19 Reviewing our early laparoscopic BD stone experience andseeing it mirrored in other groups around the world,4,5,9,18,20,24,25 we became much more focused on the relative merits of laparoscopic choledochotomy and postoperative ERCP in the remaining one third of patients. Clinical equipoise in this group with regard to retained stones, reoperation rate, and morbidity appeared to be present, and is what prompted this trial.18,20,21,25
The widely held view is that detection of BD stones at operation and then reliance on postoperative ERCP clearance is likely to increase patient morbidity from ERCP failure and subsequent feared need for further surgery.2,8 The often unstated assumption of proponents of preoperative ERCP clearance is that failure of ERCP preoperatively will allow surgical clearance as a single procedure (laparoscopic or open) without the need for a third procedure. Indeed, reoperation for a variety of reasons postcholedochotomy is well documented in 5% of cases, which approximates the rate of 4% to 8% failures requiring surgery after postoperative ERCP.21,23–25 In this trial, reoperation occurred in 7.3% choledochotomy patients versus 6.6% in the ERCP group (Table 3).
TABLE 3. Postoperative Outcomes (No Mortality)
Many skeptical surgeons assessing the applicability of this trial to the wider community setting should appreciate that it involved a number of surgeons and occasionally surgeons in training and gastroenterologists performing ERCP with a variety of experience in 7 separate hospitals with quite marked variations in equipment available. The costing of either the ERCP or choledochotomy approach was not addressed in the execution of this trial because the required resourcing to carry it out accurately was not available.
These short-term data suggest in our view that the majority of secondary BD stones can be diagnosed at the time of cholecystectomy and cleared via the cystic duct, with those failing having either choledochotomy or postoperative ERCP.
We would avoid choledochotomy in ducts less than 7mm measured at the time of operative cholangiogram and severely inflamed friable tissues leading to a difficult dissection. We would advocate choledochotomy as a good choice for patients after Billroth 11 gastrectomy, failed ERCP access, or where long delays would occur for patient transfer to other locations for the ERCP.
The small trial size after 5 years of recruitment carries the inherent likelihood of a type II error and so miss a small difference in endpoints. Our hope is that with publication of similar experience from other centers in years to come, meta-analysis may help to improve this flaw.
Footnotes
Supported by Cook Australia.
Reprints will not be available from the author(s).
Correspondence: Leslie K. Nathanson, Level 4, 30 Chasely St, Auchenflower 4066, Brisbane, Australia. E-mail: lnathanson@wesley.com.au.
REFERENCES
- 1.Casagrande JT, et al. The power function of the ‘exact’ test for comparing two binomial distributions. Appl Stat. 1978;27:176–180. [Google Scholar]
- 2.Trondsen E, Edwin B, Reiertsen O, et al. Prediction of common bile duct stones prior to cholecystectomy. Arch Surg. 1998;133:162–166. [DOI] [PubMed] [Google Scholar]
- 3.Liu TH, Consorti ET, Kawashima A, et al. Patient evaluation and management with selective use of magnetic resonance cholangiography and endoscopic retrograde cholangiopancreatography before laparoscopic cholecystectomy. Ann Surg. 2001;234:33–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Phillips EH, Carrol BC, Pearlstein AR, et al. Laparoscopic choledochoscopy and extraction common bile duct stones. World J Surg. 1993;17:22–28. [DOI] [PubMed] [Google Scholar]
- 5.Petelin JB. Clinical results of common bile duct exploration. Endosc Surg Allied Technol. 1993;1:125–129. [PubMed] [Google Scholar]
- 6.Liberman MA, Phillips EH, Carroll BJ, et al. Cost-effective management of complicated choledocholithiasis: laparoscopic transcystic duct exploration or endoscopic sphincterotomy. J Am Coll Surg. 1996;182:488–494. [PubMed] [Google Scholar]
- 7.Berthou JC, Droud F, Charbonneau P, Moussalier K. Laparoscopic management of common bile duct stones: technique and results about 200 cases. Eur J Celiosurg. 1997;1:22–30. [Google Scholar]
- 8.Taylor TV, Torrance B, Rimmer S, et al. Operative cholangiography: is there a statistical alternative? Am J Surg. 1983;145:640–643. [DOI] [PubMed] [Google Scholar]
- 9.Lezoche E, Paganini AM, Carlei F, et al. Laparoscopic treatment of gallbladder and common bile duct stones: a prospective study. World J Surg. 1996;20:535–541. [DOI] [PubMed] [Google Scholar]
- 10.Millat B, Fingerhut A, Deleuze A, et al. Prospective evaluation in 121consecutive unselected patients undergoing laparoscopic treatment of choledocholithiasis. Br J Surg. 1995;82:1266–1269. [DOI] [PubMed] [Google Scholar]
- 11.Prat F, Amouyal G, Amouyal P, et al. Prospective controlled study of endoscopic ultrasonography and endoscopic retrograde cholangiography in patients with suspected common bile duct lithiasis. Lancet. 1996;347:75–79. [DOI] [PubMed] [Google Scholar]
- 12.Hammerstrom L-E, Holmin T, Stridbeck H, et al. Routine preoperative infusion cholangiography at elective cholecystectomy: a prospective study in 694 patients. Br J Surg. 1996;83:750–754. [DOI] [PubMed] [Google Scholar]
- 13.Bloom ITM, Gibbs SL, Keeling-Roberts CS, et al. Intravenous infusion cholangiography for investigation of the bile duct: a direct comparison with ERCP. Br J Surg. 1996;83:755–757. [DOI] [PubMed] [Google Scholar]
- 14.Joyce WP, Keane R, Burke GJ, et al. Identification of bile duct stones in patients undergoing laparoscopic cholecystectomy. Br J Surg. 1991;78:1174–1176. [DOI] [PubMed] [Google Scholar]
- 15.Leese T, Neoptolemos JP, Carr-Locke DL. Successes, failures, early complications and their management: results of 394 consecutive patients from a single centre. Br J Surg. 1985;72:215–219. [DOI] [PubMed] [Google Scholar]
- 16.Vaira D, Ainley C, Williams S, et al. Endoscopic sphincterotomy in 1000 consecutive patients. Lancet. 1989;2:431–434. [DOI] [PubMed] [Google Scholar]
- 17.O'Donnell LDJ, Heaton KW. Recurrence and re-recurrence of gallstones after medical dissolution: a long-term follow-up. Gut. 1988;29:655–658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Khoo D, Walsh CJ, Murphy C, et al. Laparoscopic common bile duct exploration: evolution of a new technique. Br J Surg. 1996;83:341–346. [DOI] [PubMed] [Google Scholar]
- 19.Rhodes M, Nathanson L, O'Rourke N, et al. Laparoscopic exploration of the common bile duct: lessons learned from 129 consecutive cases. Br J Surg. 1995;82:666–668. [DOI] [PubMed] [Google Scholar]
- 20.Petelin JB. Clinical results of common bile duct exploration. Endosc Surg Allied Technol. 1993;1:125–129. [PubMed] [Google Scholar]
- 21.Berci G, Morgenstern L. Laparoscopic management of common bile duct stones: a multi-institutional SAGES study. Society of American Gastrointestinal Endoscopic Surgeons. Surg Endosc. 1994;8:1168–1174. [DOI] [PubMed] [Google Scholar]
- 22.Ochi Y, Mukawa K, Kiyosawa K et al. Comparing the treatment outcomes of endoscopic papillary dilation and endoscopic sphincterotomy for removal of bile duct stones. J. Gastroenterol Hepatol. 1999;14(1):90–96. [DOI] [PubMed] [Google Scholar]
- 23.Martin IJ, Bailey IS, Rhodes M, et al. Towards T-tube free laparoscopic bile duct exploration: a methodologic evolution during 300 consecutive procedures. Ann Surg. 1998;228:29–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cuschieri A, Lezoche E, Morino M, et al. E.A.E.S. multicentre prospective randomised trial comparing two-stage vs. single-stage management of patients with gallstone disease and ductal calculi. Surg Endosc. 1999;13:952–7. [DOI] [PubMed] [Google Scholar]
- 25.Rhodes M, Sussman L, Cohen L, et al. Randomised trial of laparoscopic exploration of common bile duct versus postoperative endoscopic retrograde cholangiography for common bile duct stones. Lancet. 1998;351:159–161. [DOI] [PubMed] [Google Scholar]
- 26.Blamey SL, Imrey CW, O'Neill J, et al. Prognostic factors in acute pancreatitis. Gut. 1984;25:1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.O'Rourke N, Fielding G. Laparoscopic antegrade biliary stenting. Endoscopy. 1995;27:666–678. [DOI] [PubMed] [Google Scholar]
- 28.Neoptolemos JP, Carr-Locke DL, Fossard NP. A prospective randomised study of pre-operative endoscopic sphincterotomy versus surgery alone for common bile ductstones. Br Med J. 1987;294:470–474. [DOI] [PMC free article] [PubMed] [Google Scholar]


