Abstract
Objective:
We sought to determine the ability of the Model for End-Stage Liver Disease (MELD) score to predict 30-day postoperative mortality for patients with cirrhosis undergoing nontransplant surgical procedures.
Summary Background Data:
The Child-Pugh class historically has been used by clinicians to assist in management decisions involving patients with cirrhosis. However, this classification scheme has a number of limitations. Recently, MELD was introduced. It has been shown to be highly predictive of mortality in a variety of clinical scenarios.
Methods:
Adult patients with a diagnosis of cirrhosis undergoing nontransplant surgical procedures between January 1, 1996, and January 1, 2002, at a single center were analyzed. The preoperative MELD score was calculated for all patients, and the MELD's performance in predicting 30-day mortality was determined using multivariate regression techniques.
Results:
A total of 140 surgical procedures were identified and analyzed. The 30-day mortality rate was 16.4%. The mean admission MELD score for the patients who died (23.3, 95% confidence interval 19.6–27.0) was significantly different from those patients surviving beyond 30 days (16.9, 15.6–18.2), P = 0.0003. The c-statistic for MELD score predicting 30-day mortality was 0.72. Further subgroup analysis of 67 intra-abdominal surgeries showed an in-hospital mortality of 23.9%. The mean MELD score for patients dying (24.8, 20.4–29.3) was significantly different from survivors (16.2, 14.2–18.2), P = 0.0001. The c-statistic for this subgroup was 0.80.
Conclusions:
The MELD score, as an objective scale of disease severity in patients with cirrhosis, shows promise as being a useful preoperative predictor of surgical mortality risk.
The Model for End-Stage Liver Disease (MELD) score is a recently developed, objective scoring system widely used to rate the severity of cirrhosis. This study evaluated the MELD score's performance in predicting postoperative death in patients with cirrhosis undergoing nonliver transplant surgical procedures. The MELD score was found to be a good predictor of postoperative mortality in this patient population.
Chronic liver failure affects multiple organ systems and results in a shortened life expectancy. Previous reports have demonstrated increased perioperative morbidity and mortality in patients with cirrhosis.1 This morbidity likely is related to the disruption that liver disease exerts on blood flow as well as on biochemical and metabolic pathways. The preprocedure use of diuretics and operative use of anesthetics further strains the liver and associated pathways. The morbidity and mortality of cirrhotic patients undergoing a variety of surgical procedures has been well documented.2 This documentation has contributed to the concern many surgeons express when confronted with individuals with known liver disease who may need surgical procedures. Despite this, as many as 10% of cirrhotic patients will require surgical procedures, often when their liver disease is poorly compensated.3 Risk stratification for these patients is difficult and often precludes surgical intervention.
Historically, the severity of cirrhotic liver disease has been calculated using the Child-Pugh (CP) class. The variables used in the calculation of the CP class were not the result of systematic analysis but rather emerged from clinical experience. The CP class has been shown to be valuable in determining prognosis in cirrhotic patients undergoing medical management.4 Additionally, the CP score has been shown to have significant prognostic influence on postoperative complications and mortality. This influence was demonstrated across a range of different surgical procedures and was significant by both univariate and multivariate analyses.2 However, other authors have reported the Child classification and Pugh score failed to predict postoperative 30-day mortality.1 This failure may be related to the limitations of the CP system, including the subjective interpretation of parameters such as ascites and encephalopathy, as well as a limited discriminatory ability.
The MELD score originally was developed and validated to assess the short-term prognosis of patients with cirrhosis undergoing the transjugular intrahepatic portosystemic shunt (ie, TIPS) procedure.5 The score consists of 3 objective, easily obtainable variables: serum International Normalized Ratio (INR), total bilirubin, and creatinine levels. It subsequently has been shown to be a reliable marker of mortality risk in both hospitalized and ambulatory patients with cirrhosis.6 The score's usefulness appears to be irrespective of underlying disease etiology. The predictive capabilities of the MELD score have been studied in a variety of conditions, including primary biliary cirrhosis and primary sclerosing cholangitis.6,7 Additionally, the MELD score has been demonstrated to be predictive of in-hospital and 1-year mortality in patients presenting with acute variceal bleeding.8 The MELD score also has been recently validated to predict 1-year and 5-year mortality in a large cohort of nontransplant cirrhosis patients with widely varying causes and severities of chronic liver disease.9 Since February 2002, the United Network for Organ Sharing (UNOS) has used a modified MELD score for liver transplantation organ allocation based on its utility as an easily verifiable, objective scoring system with multiple gradations, and its role as a superior disease severity index. The objective of this study is to determine the ability of the MELD score to predict 30-day mortality for patients with cirrhosis undergoing nontransplant surgical procedures.
MATERIALS AND METHODS
Using administrative, financial, and clinical databases, all adult patients admitted with cirrhosis, as documented by International Classification of Diseases, 9th Revision code, that underwent nontransplant surgical procedures at the University of Virginia Health System between January 1, 1996, and January 1, 2002, were identified. Patients younger than 18 years of age, those undergoing liver transplantation, and those undergoing outpatient-only procedures were excluded. Experienced study personnel reviewed the medical records of all subjects to verify the diagnosis of cirrhosis and the possible etiology of cirrhosis. Preoperative laboratory data were used to calculate a MELD score within the initial 24 hours of hospitalization. All eligible patients with laboratory data available were included in this study. Patients were excluded from the study if all 3 components of the MELD score were not available. In patients that had more than one surgical procedure, a preoperative MELD score was calculated before each procedure. The MELD score on the day of hospitalization was chosen because it was felt that this most accurately represented the patients’ level of underlying liver disease before surgery. The MELD scores changed remarkably after initial hospitalization because of blood product and plasma transfusions and other medical interventions aimed at improving the patients’ laboratory values prior to surgery. All-cause postoperative mortality within 30 days after surgery was the primary end point in the analysis. When patients were discharged before 30 days after the procedure, their status was verified by review of electronic death certificate information incorporated into the health system's clinical data repository.
As the original MELD score defined by Malinchoc, et al,5 has been modified from its original format, the modified MELD score was used in this study. We calculated the modified MELD score using the standard UNOS-based formula, which is the most widely used adaptation of the MELD score currently in use: MELD = 3.78 × loge (bilirubin in mg/dl) + 11.2 × loge (INR) + 9.57 × loge (creatinine in mg/dL) + 6.43. To maintain consistency with UNOS scoring systems, a bilirubin or creatinine value of less than 1.0 mg/dL was rounded to 1.0 mg/dL to avoid a negative score and the maximum creatinine allowed was 4.0 mg/dL. All patients undergoing dialysis received a creatinine of 4.0 mg/dL. Finally, the calculated MELD score was rounded to the nearest integer.
After the total population was analyzed, patients were stratified by type of surgical procedure performed, ie, intra-abdominal, cardiac, orthopedic and urologic, and individual subgroup analyses were separately performed. Data management and statistical analysis were performed using SAS®, Version 8 (Cary, NC). Univariate analyses were performed using the Student t test for parametric continuous variables and the Wilcoxon rank sum test for nonparametric continuous variables. Categorical variables were tested using the χ2 test or the Fisher exact test where appropriate. Multivariate logistic regression modeling using the method of likelihood estimates was performed with variables that could significantly affect the outcome as determined by the univariate analysis including age, MELD score, the individual components of the MELD (INR, bilirubin, creatinine), gender, race, and the presence of significant medical comorbidities. Sensitivities and specificities for the resulting model were calculated and used to derive a c-statistic for each model. The significance level for type I error (α) was set at 0.05 and all significance tests were 2-sided. Predicted mortality for all subgroups was calculated by back-transforming the regression equations using the original sample data. The local institutional review board, the University of Virginia Human Investigations Committee, reviewed and approved this investigational protocol.
RESULTS
A total of 140 separate nontransplantation surgical cases were identified in 131 patients. Table 1 shows the population characteristics. All cause 30-day postoperative mortality was 16.4% (23 of 140). The distribution of MELD scores for the study population is shown in Figure 1. This figure shows that a wide range of MELD scores were included in the study population although the data were somewhat skewed towards the lower scores. The mean MELD score was 18.0 (standard deviation 7.8), the median was 17.0, and the interquartile range (between the 25th and 75th percentile) was 11.0. Scores ranged from a minimum of 6 to a maximum of 43.
TABLE 1. Population General Characteristics
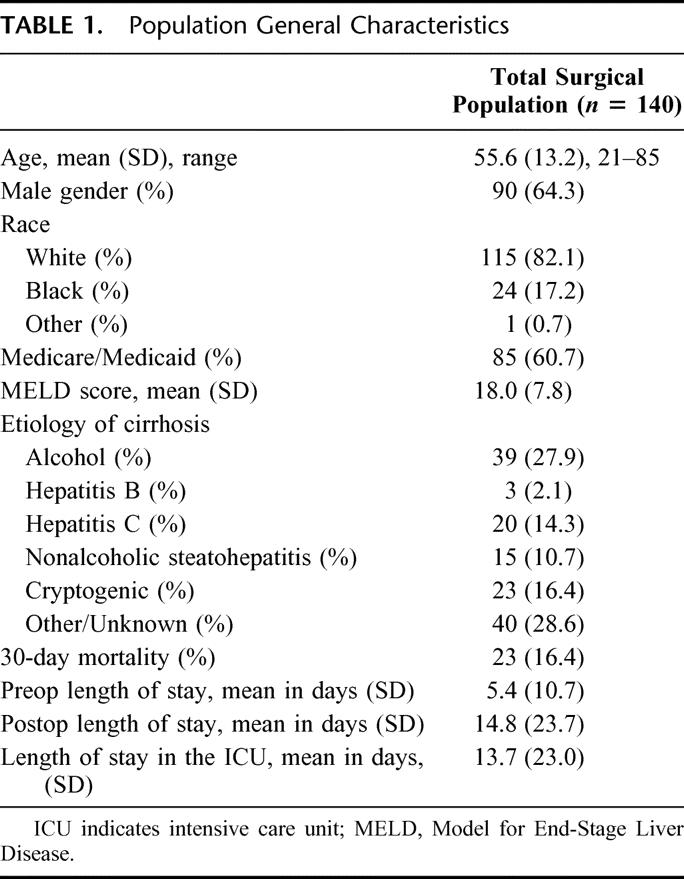
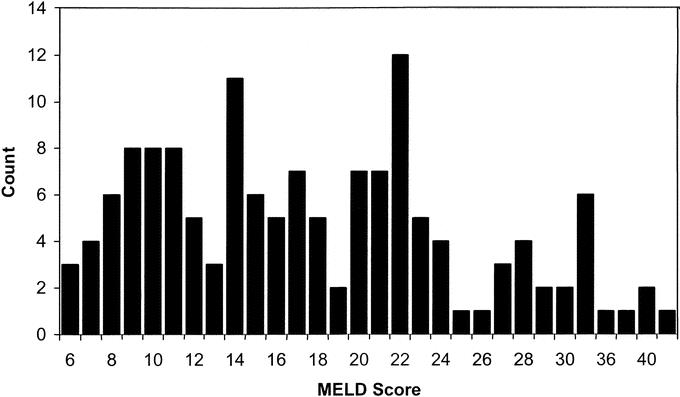
FIGURE 1. Distribution of MELD scores in study population.
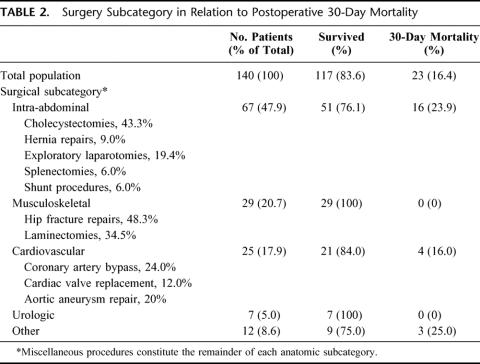
Table 2 shows the types of surgical procedures performed. Sixty-seven patients (47.9%) had an intra-abdominal procedure with the majority being cholecystectomies, hernia repairs, and exploratory laparotomies. Twenty-nine patients (20.7%) had musculoskeletal procedures such as repair of long bone fractures and laminectomies. Twenty-five (17.9%) had cardiovascular operations including coronary artery bypass grafting, heart valve replacement, and aortic aneurysm repairs. The remainder of the procedures were thoracic, neurosurgical, or urologic. Mortality rates for the individual surgical categories are also listed in Table 2.
TABLE 2. Surgery Subcategory in Relation to Postoperative 30-Day Mortality
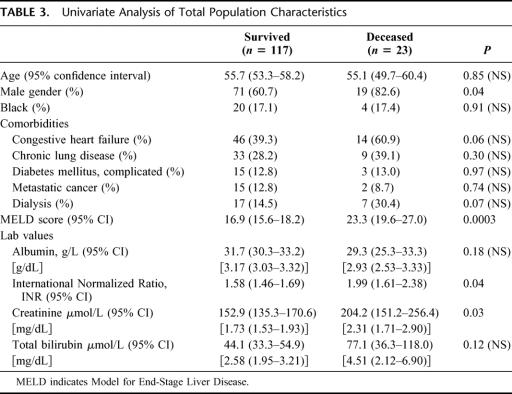
The characteristics of the 117 patients who survived and 23 who died postoperatively are shown in Table 3. Univariate analysis showed statistically significant survival differences in gender (relative risk [RR] of death for men = 1.16 with 95% confidence interval 1.02–1.33), MELD score (16.9 in survivors versus 23.3 in patients that died, P = 0.0003), INR (1.58 versus 1.99, P = 0.04), and creatinine (152.9 versus 204.2 μmol/L [1.73 versus 2.31 mg/dL], P = 0.03). Race, the presence of chronic lung disease, diabetes mellitus, metastatic cancer, hemodialysis, albumin level, and total bilirubin did not differ statistically between the survivors and nonsurvivors. Because of small sample sizes and low numbers of deaths in the musculoskeletal, cardiovascular, urologic, and other procedure groups, there were no statistically significant differences between survivors and the nonsurvivors in those subgroups.
TABLE 3. Univariate Analysis of Total Population Characteristics
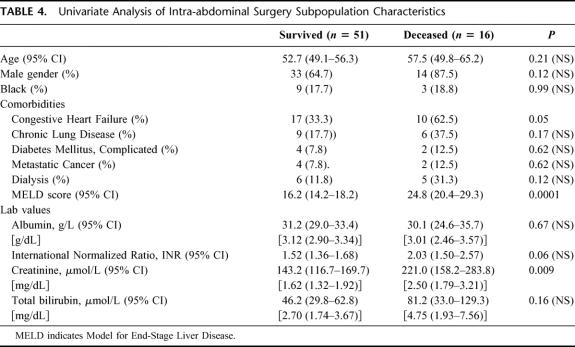
The all-cause 30-day mortality for the intra-abdominal procedure group was 23.9% (16 of 67). Table 4 shows the univariate subgroup analysis for the population undergoing intra-abdominal procedures. Statistically significant survival differences were found between groups in the presence of CHF (RR = 1.35, 0.98–1.85), the MELD score (16.2 versus 24.8, P = 0.0001 in survivors versus nonsurvivors, respectively), and serum creatinine (143.2 versus 221.0 μmol/L [1.62 versus 2.50 mg/dL], P = 0.009).
TABLE 4. Univariate Analysis of Intra-abdominal Surgery Subpopulation Characteristics
Multivariate logistic regression analyses using 30-day postoperative death as the dependent end point were performed on the total population and the intra-abdominal procedure subgroup. MELD score, age, albumin, INR, creatinine, total bilirubin, gender, race, and the presence of major comorbidities were entered into the model. The MELD score was the only statistically significant predictor of 30-day mortality after surgery (OR = 1.10 per unit increase in MELD score greater than the lowest possible score of 6, 1.04–1.17, P = 0.001) with a 71.6% concordance rate and a c-statistic (area under the ROC curve) of 0.72. Likewise, in the intra-abdominal procedure subgroup model, the MELD score again showed a statistically significant effect on the overall model (OR=1.15 per unit increase in MELD score above the lowest possible score of 6, 1.06–1.25, P = 0.001) with an 80.3% concordance rate and a c-statistic of 0.80. The total population model had a sensitivity of 47.8% and specificity of 78.3% in predicting a 20% mortality rate, whereas the intra-abdominal model had a sensitivity of 81.3% and specificity of 70.0% at that mortality rate.
Figures 2 and 3 show plots of the predicted mortality (based on the multivariate regression models) versus the MELD score for the total population and the intra-abdominal subgroup, respectively. Between MELD scores of 5 and 20 there is approximately a 1% increase in mortality risk with each integer increase in MELD score. As the slope of the regression equation increases as seen with MELD scores greater than 20, there is approximately an additional 2% increase in mortality risk with each integer increase in MELD.
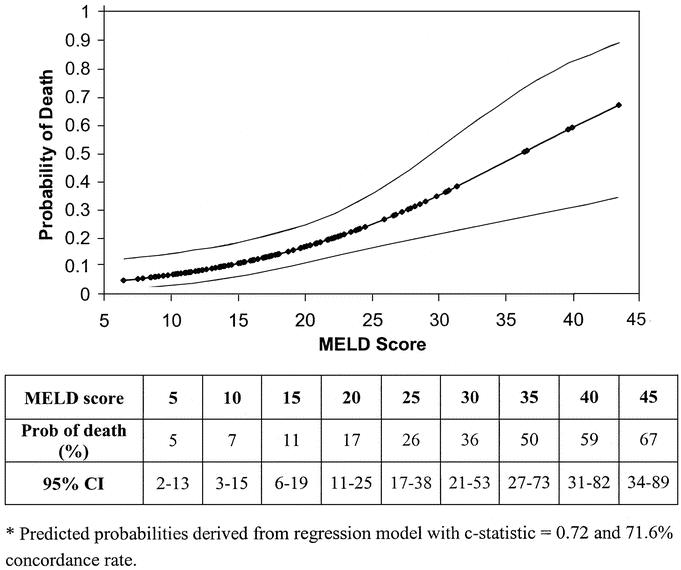
FIGURE 2. Predicted probability of postoperative death within 30 days by MELD score for total population with 95% confidence intervals. Predicted probabilities are derived from regression models with c-statistic = 0.72 and 71.6% concordance rate.
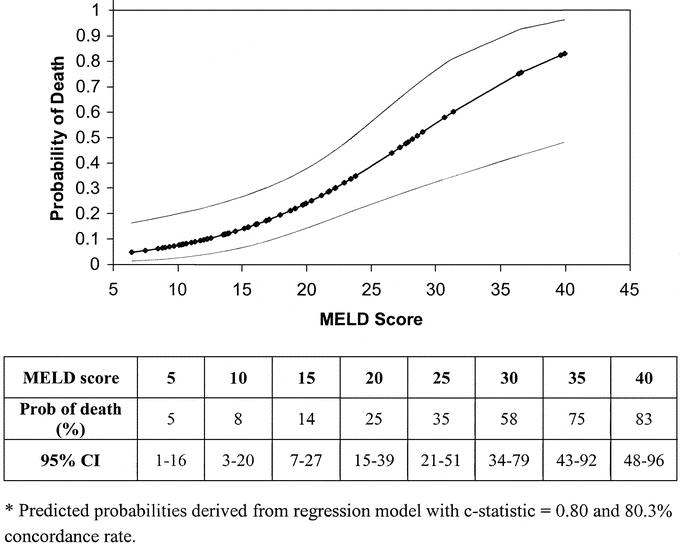
FIGURE 3. Probability of postoperative death within 30 days by MELD score for intra-abdominal surgery cohort with 95% confidence intervals. Predicted probabilities are derived from regression models with c-statistic = 0.80 and 80.3% concordance rate.
DISCUSSION
This study demonstrates a direct correlation between the MELD score and postoperative mortality in cirrhotic patients undergoing nontransplant operative procedures. The simple rule-of-thumb of a 1% increase per MELD point in mortality with MELD scores less than 20 and an additional 2% increase per MELD point greater than 20 provides useful information to the practicing physician when advising patients regarding procedure-associated mortality. We feel that the continuous, objective assessment obtained from the MELD score is more valuable than a categorical system with imprecise subjective parameters, such as the CP system, in individually assessing patient risk. This continuous system avoids categorizing patients with mildly decompensated disease along with patients with more moderately or severely decompensated disease. Finally, the MELD score offers a simple, objective, easily used tool that avoids the subjectivity of CP classification, ultimately making for more uniform risk assessment between patients and institutions.
In this study, 30-day postoperative mortality was found to be 16.4% in the total cohort of cirrhotic patients undergoing surgical procedures. The mortality identified in this study cohort is consistent with other published reports. Ziser et al2 reported an in-hospital total mortality of 9.8% in a retrospective review of 733 patients with cirrhosis undergoing surgical procedures. Rice et al1 reported a 30-day mortality of 28% in a smaller cohort of nonhepatic surgical procedures. Selection bias towards patients with less severely decompensated cirrhosis is likely to be present in all studies of surgical risk; however, the distribution of MELD scores in our study population includes a broad sample of decompensated and well-compensated patients. This distribution of MELD scores is relatively representative of the spectrum of cirrhotic patients treated at a large university medical center. More than 25% of the patients in our study had MELD scores above 22, which is very close to the mean MELD score for all patients undergoing liver transplantation in the U.S. in the year 2002.10
Approximately 50% of the patients in our study underwent intra-abdominal surgeries. In our opinion, this accurately reflects clinical experience. The 30-day mortality for this important subgroup is consistent with reported values in the literature.1,11 The distribution of the remaining surgical procedures in this study is typical of those seen in a large tertiary care center, especially with an aging population. Although the mortality in the cardiovascular subgroup approximates that of the intra-abdominal group, there was no in-hospital mortality in the cohort of patients undergoing musculoskeletal surgeries. This difference is likely related to the increased surgical complexity, longer anesthesia time, higher complication rates, and longer recovery times of the cardiovascular and intra-abdominal groups. Our data suggest that surgeries not involving the peritoneal or thoracic cavities may be better tolerated in cirrhotic patients.
We used univariate and multiple logistic regression analyses to determine which variables were most predictive of 30-day mortality. These findings confirmed previous studies that demonstrated congestive heart failure1,2 and creatinine1,2,5 as variables associated with mortality. The calculated MELD score also was highly statistically significant. Notably, other variables were not found to be significant in our statistical analysis including albumin and bilirubin. Clearly, renal function (as measured by creatinine) is a critical contributor to postsurgical mortality in patients with cirrhosis. This has obvious implications for both the internist and surgeon, as it is clinically understood that optimization of renal function should be a priority in this group of patients during the pre- and postoperative period.
Multiple logistic regression analysis identified the MELD score as the most significant independent risk factor for 30-day postoperative mortality. The MELD score performed well in classifying patients according to their risk of 30-day mortality. This is demonstrated by the significant c-statistics derived from the logistic regression models. In general, a c-statistic of 0.5 is associated with chance alone, whereas values greater than 0.7 are generally accepted as an indication of a useful test. Increasing values of the c-statistic entail increasingly significant diagnostic accuracy. In our study, the c-statistic values of 0.72 and 0.80 were obtained for the total population and intra-abdominal surgery cohorts, respectively. These compare favorably with current MELD literature. Kamath et al,6 reported c-statistics of 0.84–0.95 for 1-week mortality and 0.78–0.87 for 3-month mortality in patients awaiting liver transplantation. The in-hospital mortality associated with acute variceal bleeding demonstrated a c-statistic of 0.83 as studied by Chalasani et al.8 Sheth et al12 found a value of 0.82 for 30-day mortality in patients hospitalized with acute alcoholic hepatitis. C-statistics for the CP class’ predictive ability in nontransplant postoperative mortality are not reported in the literature.
Because of the retrospective nature of this study, we did not compare the MELD score to the Child-Pugh classification or score. Previous reports have demonstrated equivalence or superiority of MELD to CP in a variety of clinical scenarios.13,14 The retrospective nature and methodology of the current study would not permit accurate calculation of CP class in the patient population studied. Additionally, we feel that the MELD scoring system provides clinicians with an objective and predictive tool that allows easy point-of-care use. This stands in contrast to CP where clinicians must subjectively determine the degree of encephalopathy and ascites. Quantitative bedside assessment of ascites by physical examination is difficult even by experienced physicians.15,16 The availability and utilization of software and PDAs (ie, personal digital assistants) enable clinicians to quickly calculate a patient's MELD score in either the ambulatory or inpatient setting.
Because the indications and priority for various surgical procedures are so varied across the spectrum of surgical disease in cirrhotic patients, we cannot make a recommendation for an absolute cutoff point where surgery is “too risky,” based on the MELD score. However, the MELD score should be a useful tool in counseling cirrhotic patients regarding their risk for a surgical procedure. Certainly, the higher MELD scores indicate proportionally higher surgical risk while the lower MELD scores impart some sense of relative safety, especially when the MELD score is less than 10. Finally, with MELD scores above 20, the mortality risks increase dramatically.
The current study has a number of weaknesses. Administrative and clinical databases are limited by their retrospective nature. It was not possible to determine the number of patients with cirrhosis who were considered for surgical intervention in whom no surgical procedures were performed. Thus, one might expect to see a bias in the data towards surgical intervention in individuals with less advanced or well-compensated liver disease. However, Figure 1 shows that a significant proportion of the study population had relatively high MELD scores, confirming that our population reflects that of the general population of cirrhotic patients in a tertiary referral center. The MELD scores in this study are highly variable and the predicted mortality probabilities, relative risks, and odds ratios have wide confidence intervals, especially with the higher MELD scores. Review of the predictive value of the multivariate models also indicates that the models are not perfectly predictive, likely because other unknown factors contributing to postoperative mortality were not included in the models. Finally, because of the small sample sizes, especially in the subgroup analyses, the possibility of type II error is significant. This type of error might incorrectly lead us to find that a factor is not an important predictor of mortality. Further validation of the MELD score in large surgical datasets is needed to answer these concerns.
Despite the utility of the MELD score in a variety of clinical situations, it has notable limitations. Although it uses objective measures, these variables can be labile, causing sudden and dramatic changes in the MELD score as a result of infection, medication side-effects, or fluid shifts. Fluid changes are particularly important, as serum creatinine is a primary determinate of mortality. Yoo et al17 recently demonstrated that the MELD score does not correlate well with the severity of hepatic encephalopathy or ascites. Also, a familiar problem with the CP and other risk assessment strategies is determining the optimal timing for risk stratification. On the basis of the evidence presented here, we believe assessment at the time of admission is appropriate based on the strong correlation between MELD score at admission and postoperative mortality. Further studies are needed to address this issue, specifically to determine if therapeutic correction of MELD scores effects a change in postoperative mortality significantly after the initial day of hospitalization. Reanalysis of the variables (INR or creatinine) and recalculation of the MELD score may improve its predictive value for postoperative mortality.
Also at issue is the predictive value of the MELD score for emergent versus nonemergent procedures. Analysis of the indications for surgery in our cohort showed that 59 of 140 (42%) of the procedures were performed for nonelective indications. Despite this, our results may be more representative of elective or semi-urgent procedures rather than truly emergent procedures. This is supported by the mean preoperative length of stay of 5 days in our population, suggesting that time for evaluation and stabilization was available. Although unlikely to have a major influence on this study's results, this analysis may have missed patients undergoing true emergent procedures, as they might have been less likely to undergo a complete laboratory workup (eg, total bilirubin) prior to the operation. Therefore, some of those patients may have been excluded from our cohort because of the lack of valid laboratory values used in calculating the MELD scores. Likewise, we have no way of including patients in this retrospective cohort that were evaluated for elective surgery but were felt not to be surgical candidates because of their liver disease. These are inherent weaknesses in this study and in all retrospective evaluations of surgical procedures. However, with the lack of prospective, controlled studies, we feel that this study is thought provoking and provides clinicians with an additional tool useful in the preoperative evaluation of patients with cirrhosis.
To our knowledge, this is the first comprehensive evaluation of the MELD scoring system for patients undergoing a broad spectrum of nontransplant surgical procedures. The MELD score appears to be predictive of 30-day postoperative mortality in patients with varying degrees of cirrhosis. We feel the MELD score provides an additional tool for physicians and surgeons to use in counseling cirrhotic patients regarding postoperative surgical mortality. In this study, patients with low MELD scores tolerated a variety of surgical procedures with low relative mortality rates. Although reassuring, even a low MELD score of 10 is associated with a postoperative mortality of 5%. Thus, strong consideration should be given to performing procedures on this patient population at experienced centers with the appropriate resources required to care for them. Furthermore, referral to tertiary care centers with hepatologists or transplant teams should be considered for patients with higher MELD scores. Further refinement of this risk assessment strategy will come from prospective studies or large database reviews and should be pursued to validate these findings and examine the safety of a greater variety of surgical procedures in patients with cirrhosis.
Footnotes
Reprints: Patrick G. Northup, MD, Division of Gastroenterology and Hepatology, P.O. Box 800708, University of Virginia Health System, Charlottesville, VA 22908. E-mail: pgn5qs@virginia.edu.
REFERENCES
- 1.Rice HE, O'Keefe GE, Helton WS, et al. Morbid prognostic features in patients with chronic liver failure undergoing nonhepatic surgery. Arch Surg. 1997;132:880–884; discussion 884–885. [DOI] [PubMed]
- 2.Ziser A, Plevak DJ, Wiesner RH, et al. Morbidity and mortality in cirrhotic patients undergoing anesthesia and surgery. Anesthesiology. 1999;90:42–53. [DOI] [PubMed] [Google Scholar]
- 3.Probst A, Probst T. Prognosis and life expectancy in chronic disease. Dig Dis Sci. 1995;40:1805–1815. [DOI] [PubMed] [Google Scholar]
- 4.Christensen E, Schlichting P, Fauerholdt L, et al. Prognostic value of Child-Turcotte criteria in medically treated cirrhosis. Hepatology. 1984;4:430–435. [DOI] [PubMed] [Google Scholar]
- 5.Malinchoc M, Kamath PS, Gordon FD, et al. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts.[comment]. Hepatology. 2000;31:864–871. [DOI] [PubMed] [Google Scholar]
- 6.Kamath PS, Wiesner RH, Malinchoc M, et al. A model to predict survival in patients with end-stage liver disease.[comment]. Hepatology. 2001;33:464–470. [DOI] [PubMed] [Google Scholar]
- 7.Kim WR, Poterucha JJ, Wiesner RH, et al. The relative role of the Child-Pugh classification and the Mayo natural history model in the assessment of survival in patients with primary sclerosing cholangitis. Hepatology. 1999;29:1643–1648. [DOI] [PubMed] [Google Scholar]
- 8.Chalasani N, Kahi C, Francois F, et al. Model for end-stage liver disease (MELD) for predicting mortality in patients with acute variceal bleeding. Hepatology. 2002;35:1282–1284. [DOI] [PubMed] [Google Scholar]
- 9.Said A, Williams J, Holden J, et al. Model for end stage liver disease score predicts mortality across a broad spectrum of liver disease. J Hepatol. 2004;40:897–903. [DOI] [PubMed] [Google Scholar]
- 10.United Network for Organ Sharing. Liver Waiting List and Transplantation, 1993–2002: National Data. Richmond, VA; UNOS; 2002. [Google Scholar]
- 11.Aranha GV, Sontag SJ. Cholecystectomy in cirrhotic patients: a formidable operation. Am J Surg. 1982;143:55–60. [DOI] [PubMed] [Google Scholar]
- 12.Sheth M, Riggs M, Patel T. Utility of the Mayo End-Stage Liver Disease (MELD) score in assessing prognosis of patients with alcoholic hepatitis. BMC Gastroenterol. 2002;2:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Botero RC, Lucey MR. Organ allocation: model for end-stage liver disease, Child-Turcotte-Pugh, Mayo risk score, or something else. Clin Liver Dis 2003;7:715–727, ix. [DOI] [PubMed] [Google Scholar]
- 14.Forman LM, Lucey MR. Predicting the prognosis of chronic liver disease: an evolution from child to MELD. Mayo End-stage Liver Disease. Hepatology. 2001;33:473–475. [DOI] [PubMed] [Google Scholar]
- 15.Chongtham DS, Singh MM, Kalantri SP, et al. Accuracy of clinical manoeuvres in detection of minimal ascites. Indian J Med Sci. 1998;52:514–520. [PubMed] [Google Scholar]
- 16.Cattau EL Jr., Benjamin SB, Knuff TE, et al. The accuracy of the physical examination in the diagnosis of suspected ascites. JAMA. 1982;247:1164–1166. [PubMed] [Google Scholar]
- 17.Yoo HY, Edwin D, Thuluvath PJ. Relationship of the model for end-stage liver disease (MELD) scale to hepatic encephalopathy, as defined by electroencephalography and neuropsychometric testing, and ascites. Am J Gastroenterol. 2003;98:1395–1399. [DOI] [PubMed] [Google Scholar]