Abstract
Objectives:
We examined the influence of surgeon age and other factors on proficiency in laparoscopic or open hernia repair.
Summary Background Data:
In a multicenter, randomized trial comparing open and laparoscopic herniorrhaphies, conducted in Veterans Administration hospitals (CSP 456), we reported significant differences in recurrence rates (RR) for the laparoscopic procedure as a result of surgeons’ experience. We have also reported significant differences in RR for the open procedure related to resident postgraduate year (PGY) level.
Methods:
We analyzed data from unilateral laparoscopic and open herniorrhaphies from CSP 456 (n = 1629). Surgeon's experience (experienced ≥250 procedures; inexperienced <250), surgeon's age, median PGY level of the participating resident, operation time, and hospital observed-to-expected (O/E) ratios for mortality were potential independent predictors of RR.
Results:
Age was dichotomized into older (≥45 years) and younger (<45 years). Surgeon's inexperience and older age were significant predictors of recurrence in laparoscopic herniorrhaphy. The odds of recurrence for an inexperienced surgeon aged 45 years or older was 1.72 times that of a younger inexperienced surgeon. For open repairs, although surgeon's age and operation time appeared to be related to recurrence, only median PGY level of <3 was a significant independent predictor.
Conclusion:
This analysis demonstrates that surgeon's age of 45 years and older, when combined with inexperience in laparoscopic inguinal herniorrhaphies, increases risk of recurrence. For open repairs, only a median PGY level of <3 was a significant risk factor.
Data from the Veterans Administration inguinal hernia trial were analyzed to determine factors contributing to recurrence. Surgeon's age of 45 years and older, when combined with inexperience in laparoscopic repair, increases risk of recurrence. For open repairs, only a median resident postgraduate year level of less than 3 was a significant factor.
We have published results of a large multicenter, randomized clinical trial comparing open mesh and laparoscopic mesh herniorrhaphies, including a finding that surgeon's experience, as measured by number of laparoscopic herniorrhaphy procedures previously performed, was a significant predictor of recurrence in the laparoscopic group.1,2 Briefly, 2164 men were randomized to open mesh (Lichtenstein) or laparoscopic mesh repair. Of these, 1984 underwent repair and 1696 were available for assessment of recurrence at 2 years. We found a significantly higher recurrence rate in the laparoscopic group (10%) than the open group (5%). Surgeons reporting experience with more than 250 laparoscopic herniorrhaphies before the beginning of the study, however, had recurrence rates with laparoscopic repair equivalent to that with open repair (5%). We also found a higher complication rate with the laparoscopic technique.1 In a further analysis, we examined the influence of the participating resident's training experience on recurrence rates in both laparoscopic and open repairs. We found that a postgraduate year (PGY) level <4 was a strong independent predictor for recurrence in the open but not the laparoscopic group.2
Whether the association between recurrence and experience results from the degree of specific experience with the procedure alone or from other factors contribute to this finding is unknown. In this report, we examine the effect of surgeon's age, volume of experience in laparoscopic or open tension-free hernia repair, operation time, and institutional factors on the recurrence rate. These potential predictors were chosen based on the studies of others identifying these factors as influences on surgical outcomes.3–5
MATERIALS AND METHODS
For this study, we analyzed data from the 1629 patients who underwent unilateral hernia repair; 814 had a laparoscopic repair and 815 had an open repair. Surgeon's experience surgeon's age, and years since board certification, derived from the Directory of the American Board of Medical Specialties,6 and birth dates from the American College of Surgeons Fellowship database,7 PGY of resident participating in the procedure (PGY level), operation time, and hospital observed-to-expected events ratio from the National Surgical Quality Improvement Program (O/E ratio)5 were considered as potential factors contributing to recurrence.
Following our previous findings, we dichotomized surgeon's experience in laparoscopic repair into greater than 250 repairs (experienced) and less than 250 repairs (inexperienced). The bivariate relationships between each of the factors (years since board certification, surgeon's age, surgeon's experience, PGY level, operation time, O/E ratio) and recurrence were analyzed to determine if a relationship existed and if so, whether it was linear, dichotomous, or otherwise.
Statistical analysis was performed based on the intention-to-treat principle. The associations were analyzed by group (laparoscopic or open) to determine if there were consistent or divergent findings based on technique. The correlations between each factor were examined to avoid collinearity. Years since board certification was found to be highly correlated with surgeon's age (correlation coefficient = 0.9); we chose age as the factor to examine. Scatterplots and contingency tables were used to explore possible relationships. Factors with an apparent relationship to recurrence were then analyzed. Recurrence rates for each individual attending surgeon were taken as the outcome and calculated by the number of recurrences divided by the number of cases. Analyses were based on each attending surgeon; the median PGY level of residents assisting that surgeon was calculated and used for the analyses. Multivariable logistic regression for binary-response data was applied to examine the association between recurrence rates and explanatory variables. Two-way interactions of the explanatory variables were also examined and included in the model if significant. The predictive accuracy of the multivariate models was evaluated by using both the concordance index (c-index) and the Hosmer-Lemeshow goodness-of-fit test statistics.8 All statistical values are 2-sided, and the statistical significance level was set at 0.05. We considered any factor with statistical significance in regression analysis to be significantly associated with recurrence.
RESULTS
Information on surgeon's age was available for 812 of the laparoscopic repairs (55 surgeons) and 810 of the open repairs (77 surgeons). The total number of surgeons was 86. Surgeons participating in this trial ranged in age from 27 to 70 with a median of 42 years in the laparoscopic group (55 surgeons) and from 30 to 76 with a median of 42 in the open group (77 surgeons). The average recurrence rate for these 1622 repairs was 4.4% in the open group and 8.6% in the laparoscopic group. There were no apparent relationships between surgeon age and level of resident training in either the open or the laparoscopic groups.
Laparoscopic Repair
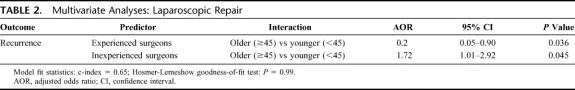
In the initial univariate analysis, surgeon's experience and age showed significant associations with recurrence, whereas operation time, hospital O/E ratio, and PGY level of participating resident did not. The relationship of surgeon's age and recurrence was dichotomous with an increase in average recurrence rates for surgeons aged 45 years and above (Table 1). Multivariable logistic regression analysis revealed significant interaction between surgeon's experience and surgeon's age (Table 2). For inexperienced surgeons, the adjusted odds ratio of recurrence for older compared with younger surgeons was 1.72 (P = 0.045).
TABLE 1. Recurrence Rates in the Laparoscopic Group by Surgeon's Experience and Age
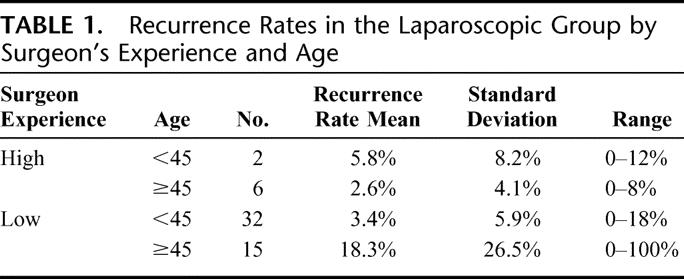
TABLE 2. Multivariate Analyses: Laparoscopic Repair
Open Repair
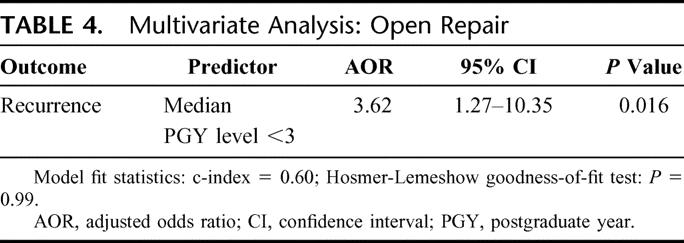
In initial analysis of open hernia repairs, the factors associated with recurrence were surgeon's age, the PGY level of the participating resident, and operation time. Hospital O/E ratio and surgeon experience were not associated with recurrence. The relationship between recurrence and surgeon age was dichotomous with an increase in mean recurrence rates for surgeons aged 45 years and above (Table 3). In multivariable logistic regression analysis, only the PGY level of the participating resident was significant; surgeon's age and operation time were not. The estimated odds of recurrence when the median PGY level of the participating resident was <3 was 3.62 times that for a resident at a median PGY level of 3 or more (P = 0.016, Table 4).
TABLE 3. Recurrence Rates in the Open Group by Surgeon's Age
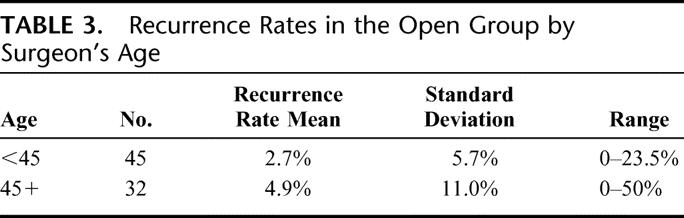
TABLE 4. Multivariate Analysis: Open Repair
DISCUSSION
We have long believed that more experience produces improved outcomes for surgeons. The strong association of high volume with good outcomes for certain major procedures such as pancreatic resection has reinforced the assumption that “practice makes perfect.”9–11 We have found a potential qualification, however, for this view.
In this cross-sectional post hoc analysis of the results of a multicenter clinical trial of hernia treatments, we did find that a large experience in laparoscopic hernia repair is associated with a low recurrence rate, regardless of the surgeon's age. Overall hospital performance, as measured by the O/E ratio for surgical morbidity, was not a significant contributor to outcome. Neither was operation time, indicating that a plateau in operation time is not a sufficient measure of proficiency. Unexpected, however, was the finding that inexperienced surgeons 45 years of age or older had recurrence rates significantly higher than equally inexperienced but younger surgeons. The explanation for this difference is not readily evident but is likely multifactorial. Potential contributors to the difference include intrinsic factors (such as aging) as well as extrinsic factors (environment and continuing medical education methods).
That older inexperienced surgeons are less proficient than younger surgeons is consistent with the results of other studies. Choudhry and colleagues systematically analyzed all available reports assessing physician age or time in practice and their performance in a variety of measurements such as knowledge and clinical outcomes.12 Of the 59 studies surveyed, all but one found some degree of decline in performance with increasing age or time in practice, and most found a global decline in all measures regardless of risk adjustment. All studies that tested knowledge showed a negative association of age with knowledge, and a very large study of the clinical outcomes of patients with acute myocardial infarction showed that mortality increased by 0.5% for every year since medical school graduation of the treating physician. Similar results were reported by Hartz and associates in a study of coronary artery bypass; after adjusting for patient and surgeon variables, surgeons who had been in practice longer and were older had higher operative mortality rates despite a large total experience in cardiac surgery.13 O'Neill and associates found the same relationship for carotid endarterectomy; years since licensure was the strongest predictor of mortality.14
The ability to learn and perform complex new procedures may be compromised by aging. An age-dependent decline in training-dependent plasticity (cortical encoding of kinematic details of practiced movements) has been reported, suggesting that the ability of the healthy aging motor cortex to reorganize in response to training decreases with age.15 Others, studying the performance of motor vehicle operational skills in healthy young and elderly drivers, found that the diminished performance of older drivers was related to visual–spatial attentional declines and diminished useful field of vision associated with normal aging.16 Visual–spatial abilities are related to performance of simulated complex surgical tasks; studies of proficiency in visual–spatial perception have determined that the performance of surgeons in simulated complex tasks required high-level visual–spatial perception abilities.17,18 It is no surprise, then, to find that older surgeons have less proficiency in performance of laparoscopic herniorrhaphy; in addition to factors related to normal aging, these surgeons did not have the advantage of structured learning programs akin to those in a residency program through which to learn a new technique.
There are few data about effectiveness of teaching new skills and techniques once surgeons have completed their structured training.12 Both the laparoscopic and the Lichtenstein hernia repairs are relatively new to surgical practice. Of the 2 herniorrhaphy procedures, the laparoscopic technique is more complex and requires a new set of skills. Surgeons 45 years and older at the beginning of our study would have learned these techniques after completion of a surgical residency through a variety of means, including short courses and formal or informal preceptorships. Prior experience with 25 laparoscopic hernia procedures was a requirement for surgeons’ participation in this study, although we did not obtain information on how, when, or where the participating surgeons learned the technique. Our inclusion of the O/E ratio for each study site suggests that the local environment was not a factor in surgeon performance.
The nearly linear decrease in recurrence rates for the open repair as residents advance, however, demonstrates a progressive learning curve during surgical residencies and suggests that structured learning taking place in a residency program becomes effective as experience is gained. We observed that experience overcame the effect of age for surgeons performing laparoscopic herniorrhaphies, but the inadequacy of effective learning programs was sharply evident when experience was lacking.
It is necessary to explain why, even when an attending surgeon was present and participating throughout the operation; junior-level residents had higher recurrence rates when performing open repairs than did residents at a more senior level. In laparoscopic procedures, the role of the attending surgeon is paramount; the participating resident and attending surgeon see the same operative field in the same perspective, and placement of mesh and sutures are under the complete control of the attending surgeon whose level of experience is the deciding factor. In open repairs, in which the resident is often the surgeon and the attending surgeon the assistant, the same degree of vigilance should have been expected; the attending surgeon could have verified each step of the placement and suturing of the mesh according to the standard protocol adopted by this study.19 Perhaps the altered perspective of the operative field that occurs when the surgeon and resident are on opposite sides of the patient was partly responsible for the pronounced effect of resident PGY level; experience of the resident, then, would play the major role. It could also be that overfamiliarity with open herniorrhaphy leads to inattention to details critical to success in this technique such as an overlap of 2 cm of mesh beyond the pubic tubercle. These might be overcome by a skilled senior resident but not recognized by residents who are inexperienced. To assure our patients that the outcomes of their operation are optimal, however, the way in which procedures are taught and supervised in residency programs deserves careful consideration.
Our study is limited in part by the design. It was a retrospective analysis of data that were immediately available to us. The analyses were exploratory in an effort to identify potential explanations for our previously published findings of the strong effect of experience (volume for attending surgeons, level of training for residents). Our study is also limited by the small number of surgeons involved in this analysis (86). Only 8 of the 55 laparoscopic surgeons in our study were experienced, therefore making conclusions from a subanalysis of this group unreliable. Our findings for inexperienced surgeons, however, are robust and consistent with those of others, meriting further investigation of the potential association between surgical outcomes and the age of the surgeon.
We are not suggesting that older surgeons are inherently incompetent or unsafe. The learning process of aging surgeons, particularly for complex new techniques, deserves further investigation.20 The methods of teaching older surgeons new techniques may need to be modified. Optimum outcomes for patients is the ultimate consideration as recommendations for the design of structured courses and for credentialing in new technology are developed.20–23
APPENDIX
VA Cooperative Study #456: Tension-Free Inguinal Hernia Repair: Comparison of Open and Laparoscopic Surgical Techniques
Participants: Chairperson: L. Neumayer, Salt Lake City VAMC
Biostatistician: A. Giobbie-Hurder
Health Scientist: J. O. Gibbs
Lead Health Economist: D. M. Hynes
Health Economist: K. Stroupe
National Study Coordinator: R. Denwood*
Clinical Nurse Coordinator: S. Hatton-Ward
Data and Safety Monitoring Board: R. Bell, Northwestern University Medical School; H. Buchwald (Chair), University of Minnesota School of Medicine; K. S. Ephgrave, VAMC Iowa City; R. Woolson, Medical University of South Carolina
Executive Committee: C. J. Carrico, University of Texas Southwestern Medical Center (deceased); D. Dunlop, Northwestern University; R. J. Fitzgibbons, Jr., Creighton University; J. O. Gibbs, Northwestern University; W.G. Henderson, University of Colorado Health Outcomes Program; A. Giobbie-Hurder, Cooperative Studies Program Coordinating Center, Hines, IL; D. M. Hynes, Cooperative Studies Program Coordinating Center, Hines, IL; K. Itani, Houston VAMC; O. Jonasson, University of Illinois College of Medicine; L. Kim, Dallas VAMC; M. J. London, San Francisco VAMC; L. Neumayer (Chair), Salt Lake City VAMC; T. N. Pappas, Durham VAMC; D. Reda, Acting Director Cooperative Studies Program Coordinating Center, Hines, IL
Endpoints Committee: M. E. Arregui, Indianapolis IN (Surgery); M. J. Bishop, Seattle VAMC (Anesthesiology); E. Jensen, MD, Salt Lake City VAMC (Pathology)
VA Central Office: J. Feussner, Chief Research & Development Officer; S. Berkowitz, Assistant Director, Cooperative Studies Program; J. Gough, Program Assistant, Cooperative Studies Program
Site Personnel: Baltimore, MD: B. Bass, G. Bochicchio, C. Alvarez,* K. B. Stem
Birmingham, AL: J. J. Gleysteen, K. Mitchell, R. Ragoza*
Boston, MA/Manchester, NH: G. Rodkey, R. Dennis, D. Soybel,* J. Gordon,* M. Campasano, B. Dionian,* J. Moriuchi*
Columbia, MO: B. Miedema, K. Crews
Dallas, TX: T. Anthony, L. Kim,* C. Willis, C. Rowder*
Detroit, MI: S. Tennenberg, R. Kozol,* C. Yales
Durham, NC: T. N. Pappas, N. Lee
Houston, TX: K. Itani, S. Brown
Little Rock, AR: L. Kim, R. Muldoon,* D. Johnson,* K. Marchant
Memphis, TN: E. Mangiante, K. Phillips, K. VanFrank, F. Hatmaker,* A. Collins*
Salt Lake City, UT: D. M. Hinson, B. Salabsky
San Francisco, CA: Q. Yang Duh, M. Marovich
Tampa, FL: C. Mendez, T. Durant, B. Wright*
West Los Angeles, CA: G. Glantz, E. H. Livingston,* W. Murphy
Chair's Office: S. Hatton-Ward
Salt Lake City, UT: B. Redfield
Hines CSPCC: K. Tir, S. Heard, J. Motyka, C. Sullivan*
*Former participant.
Discussions
Dr. Lawrence W. Way (San Francisco, California): This is the second publication to present results from the large VA multi-institutional randomized trial that compared laparoscopic and open tension-free mesh repairs of inguinal hernias. The data in the present study concern 814 of the unilateral laparoscopic repairs for which the age of the surgeon was known. The data indicate that 55 surgeons were involved, which means that on the average, each laparoscopic surgeon performed 15 laparoscopic operations. Data on the range and median number of repairs by these surgeons were not given, but would be of interest.
The previous publication reported that highly experienced surgeons had recurrence rates that were less by half than less experienced surgeons. The definition of highly experienced, which was empirically set after reviewing the results, was 250 or more laparoscopic hernia repairs.
The principal conclusion of the previous study, “The open technique is superior to the laparoscopic technique for mesh repair of primary hernias,” could be criticized as inflated, since both studies show the difference was not an immutable feature of the technique itself but was more a reflection of the experience of the operator. Thus, I would have preferred a statement to the effect that “the open technique was (not is) superior to…under the circumstances of the trial.” The current report is open to similar objections, because of how the authors dealt with the correlation between increasing age of the surgeon and the recurrence rates for the repairs. Table 1 sums it up: the recurrence rate was 18% for surgeons 45 years or older and was 3% for surgeons younger than age 45—just the inexperienced surgeons, that is.
Less was made of the observation that among experienced surgeons, the recurrence rates were substantially lower for the older than for the younger group. The cautionary point is that one should hesitate to conclude, as the authors appear to have done, that age per se was the dominant variable. The very best results were in the hands of the older surgeons. It seems more likely that age was a correlate of other variables that have not been identified (because data were not collected on them), such as training, recent experience, extent of laparoscopic activity, overall intensity of clinical practice, etc. In any event, the superior performance of the more experienced laparoscopic surgeons over age 45 raises questions about the relevance of other statements in the discussion regarding the negative relationship between age and performance. The current literature on this subject is not as one-sided as portrayed, for numerous observations demonstrate that healthy individuals can maintain excellent levels of verbal and procedural knowledge as they age, remaining active (ie, practice) being the major factor.
There is no doubt, however, as to the importance and long-lasting impact of the findings from this trial. To analyze it further, one would want more detail on the surgeons’ training and experience, since recurrence rates that vary from 0% to over 20% reflect a very heterogeneous group.
I have some questions and a final comment.
The original NEJM article counted 58 surgeons with fewer and 20 surgeons with more than 250 laparoscopic repairs who participated in the study. What happened to the missing 28 surgeons between the first report and this one, and why were they disproportionately from the experienced group?
This paper did not mention complication rates. How did they correlate with age?
It would be interesting to see scatter diagrams relating experience, age, and recurrence rates. The data are probably very heterogeneous, but lumping them into such large categories (ie, over and under age 45; more or less than 250 cases) gives a different impression and deprives the reader of information that would aid understanding.
In my opinion, the results of the VA trial suggest 1 over-riding conclusion about laparoscopic hernia repair: It is an effective operation, which some surgeons in this trial had figured out how to do well, and others had not. The declarations about which is a superior technique and the role of age per se may be oversimplifications. I think the data give more intriguing leads than finite conclusions. For example, I am most interested in finding out what the successful surgeons had learned that the unsuccessful ones had not. In retrospect, the missing link is video records of the operations. If the operations had all been recorded, the situations where error occurred could be identified, the way to cope with these situations could be identified, and the mistakes of those with high recurrence rates could be pinpointed and rectified. This would lead to more specific courses of instruction, which should improve outcomes. It almost certainly would shorten the average learning curve from 250 cases to a more practical number. The extra expense would be offset by savings resulting from the improved outcomes. A commitment to making video records a routine aspect of future trials on surgical technique has much to recommend it.
Lastly, I wonder whether the authors think that their trial creates professional obligations to deal with the problems that were discovered? Is there a responsibility to follow through and provide additional training for those who are not working at a satisfactory level? Has the issue been discussed? And who is responsible?
My duty as a discussant is to add new thoughts if I can, not just to praise. But before closing I would like to express sincere Congratulations to all who participated in this truly superb and provocative project. Thank you.
Dr. Leigh A. Neumayer (Salt Lake City, Utah): Thank you, Dr. Way. I agree that we can only comment on what we have measured. Certainly there are many things in our trial that were probably surrogates for items that we didn't measure.
What happened to all the surgeons? When we reported our results in The New England Journal of Medicine, we had self-reported surgeon experience data. As we sought to identify further those surgeons and verify their experience level, and obtain their ages, we found that some of the surgeons had been coded with 2 different codes. We feel that we have complete data now, and there are fewer surgeons in the laparoscopic group than we had originally reported.
I do have the scatter plots, and they are very intriguing. Going from lower age to higher age, a bump occurs around age 38 to 45 where more surgeons are found with a recurrence rate above 5% in the laparoscopic group. Similarly that happens for open repairs, although the recurrence rates are not as high. So these are important findings. The findings were similar for surgeons with experience greater than 250 laparoscopic repairs. This is what we used for our initial analyses and then we went on with the regression analysis.
As far as who is responsible or what are we doing about these findings, we haven't done anything at the individual sites with the surgeons except provide them with the data, which I think is really important. Especially as you introduce new techniques into your practices, you must be critically looking at and analyzing your data to the extent that Dr. Duh has done in his early laparoscopic experience. He presented some of that information at the American College of Surgeons meeting this fall.
I believe there is a responsibility for us as surgeons to look at outcomes, and whenever we have data or concerns presented to us, rather than being offended, we should use this information as an opportunity to examine the problem further and determine whether we need to make new policies or structure things differently.
Dr. Polk in his Presidential Address suggested that they had done just that in Kentucky when they found 2 surgeons whose results for carotid endarterectomy were not up to par. And I think he said 1 person retired from doing that operation and the other person went back for more training. Those are both important points.
Dr. Lazar J. Greenfield (Ann Arbor, Michigan): I would like to add my congratulations to the authors and express my appreciation for the opportunity to review the manuscript.
With more attention now focused on the consequences of aging and physicians, this is a timely and of course very touchy subject. The authors have found a correlation between hernia recurrences and older age, inexperience and junior status of the resident assisting the repair. Missing from the report is information concerning the balance of pertinent risk factors in the patients such as nutrition, smoking, history, et cetera. But assuming there was equitable distribution, what is the explanation for technical deterioration with age?
Aside from anecdotal experience, data from studies we and others have conducted over the past 10 years show that surgeons suffer the same visual and cognitive decline with aging as nonsurgeons. Other tests in industrial settings show that age is accompanied by resistance to change, loss of strength, and irritability, a combination not conducive to learning new technology or new techniques.
But before we convict surgeons of having too many birthdays or residents for not having enough, we need better performance data for individual surgeons over time.
Over the past 4 years we have tested volunteer surgeons over age 45 attending the Clinical Congress of the College using a sensitive Cambridge computer test of cognition and reaction times. The results confirm the cognitive decline with age but show the unexpected finding of remarkably fast reaction and movement times that are uneffected by age. Whether this is a feature of selection or training will require further investigation. Our study will be completed this year when we retest the participants. So if any of you took the test, please plan to come back for retesting at this year's College meeting.
The best defense against assumption of deterioration is data to the contrary, or, if changes have occurred, a definitive measurement of their extent. It is a major leap from the controlled environment of a test to the operating room, but the authors have shown us that outcomes may well be different for older surgeons. We need to address this issue before outside groups rush to judgment.
I would like to ask 2 questions. Are you contemplating further studies of other procedures where technical impairment may have consequences more serious than hernia recurrence? And if conclusions are valid as far as age-related performance is concerned, what should we do about it?
Dr. Leigh A. Neumayer (Salt Lake City, Utah): Thank you, Dr. Greenfield. We actually are considering further study. Especially because of my involvement in the NSQIP we plan to try to use that database to look at surgeon age and outcomes. This will require the merging of a couple of databases, though, but we are in the process of preparing that proposal.
Further, what should we do about it if we do find an age-related difference? There are several things we should do about it. The American Board of Surgery has already taken steps with the new requirements for maintenance of certification, and hopefully we will be able to make some new evidence-based recommendations.
I do feel, as you do, though, that we need further data. All we did with this study was a secondary analysis of some data we already had. A study should be designed to specifically look at the effect of aging, and how surgeons learn new techniques.
I think it became a large issue with laparoscopic hernia repair, because for many of our surgeons, not only was the view of the operative field different, but the actual technical challenge of operating in 2 dimensions when you are used to operating in 3 was quite different. Hopefully we can design and conduct more studies. Most laparoscopic skill studies have actually been done with medical students and residents, not with older surgeons.
Dr. Anthony A. Meyer (Chapel Hill, North Carolina): I greatly enjoyed the paper. Two points.
You described that actual age and experience were additive in terms of the reduced rate of recurrence, showing that surgeons over the age of 45—which I am long since passed—actually can have better outcomes.
But the more important thing, I think, had to do with the fact that possibly surgeons over the age of 45 are possibly less able, though there is variable in that group, to learn the new techniques. The implication for workforce is going to be important, because the new technology and new techniques that are coming out are doing so at an accelerating pace. And as that happens, surgeons who are very good at doing operations into their 50s, 60s, and 70s may not be as good at learning the new techniques. And being able to have that number of surgeons able to do all those new things may significantly impact the number of people who can perform surgery around the country, especially the newest techniques. I think that the implications for this regarding the surgical workforce are significant and wonder if you have any plans to look at that, trying to quantify the rate of technology change.
Dr. Leigh A. Neumayer (Salt Lake City, Utah): That is a very important point. When I finished my residency in 1990 it seemed that the jury was in as far as hernia repair and techniques for appendectomy were concerned. As we all know, in the last 15 years both of these assumptions have been turned upside down by new imaging and operative techniques. We are very interested in that and hope to study it further.
Dr. Murray F. Brennan (New York, New York): This morning I was just perplexed; now I am confused. If my older age impairs my performance but my greater experience improves my performance, the generic question is: How do I get the experience without getting older?
Dr. Leigh A. Neumayer (Salt Lake City, Utah): Well, learning can't be restricted to 80 hours a week. I think that is part of it. Although I personally think that work hours restrictions are a good thing.
Dr. David I. Soybel (Boston, Massachusetts): I wanted to comment as one of the investigators who participated in the trial. And this study emphasizes if nothing else that there is no such thing in surgery as a routine procedure.
First, the data that you show about the PGY level of the resident in open repairs affecting the ultimate outcome should be a very disturbing observation. If we in the VA honestly couldn't do as good a job with a PG 1 as with a PG 3, that is very bad news. I am wondering whether you looked at that in a little bit more detail to try to figure out what might have been the root cause of that particular observation.
The second observation is that in standardizing the procedure we may actually have gone to too high a level of standardization. I wonder if one of the reasons particularly for the higher recurrence rate among older surgeons was not so much what we might infer about technical deterioration with age, but the fact that somewhat more complicated hernias may have been referred to more experienced people on thestaff.
I do think one of the weak links in the study design was that we were so standardized in the size of the mesh that we were using that for some of these large direct defects, we may not have been actually using the right size mesh in relationship to the size of the defect. I don't remember us being able to note the dimensions of the defect or recording of that. And I would hate for that to become the reason that laparoscopic repair is not viewed as being as good as open repair in terms of recurrence rates.
Dr. Leigh A. Neumayer (Salt Lake City, Utah): Thank you, Dr. Soybel. Actually, we did have in the protocol that the mesh had to overlap the defect by 2 centimeters. So you could use more pieces of mesh. But I do think you are on point in that we didn't allow people to slit the mesh. If they did, they had to file a protocol deviation. Dr. Duh can address that better than I.
We did look at the sizes of mesh because we did record that, and we found, as others have found, that it is the vertical size in the laparoscopic repair that matters, and that needs to be at least 8 if not 10 centimeters. The studies indicating a larger vertical dimension were originally published about 2 years into our study and we became aware of it shortly thereafter. By that time nearly all the patients had been operated on. Luckily, most of our surgeons already were taking advantage of that information.
The relationship of recurrence to PGY in the open repair may be because we are across the table from each other, or maybe it is actually the feel of putting in a stitch in that they learn over time.
Bob Fitzgibbons, who can't be here today, in the watchful waiting trial reports that in Omaha for that study, he has no recurrences in the open group. It may be just that because we are so familiar with the repair we don't pay as much attention as we should.
Dr. Quan-Yang Duh (San Francisco, California): Just to follow up on Dr. Soybel's point. It is possible that the experienced surgeons were more willing to deviate from the protocol, and in some situations that may actually give you the better results.
I have 2 questions.
One concerns methodology. Age and number of cases are continuous variables, which you have made dichotomous. How many surgeons crossed these thresholds from 1 group to the other during the study and how did assign these cases?
The second question is: Did you look at the recurrent hernia group? Since repair of recurrent hernia is more complex than that of primary hernia, one may expect experience to make even a bigger difference.
Dr. Leigh A. Neumayer (Salt Lake City, Utah): For the first question, we did make age a dichotomous variable. We actually calculated the age of each surgeon in the year that they did the hernia repair for that individual patient. Age was treated dichotomously but we had varying ages. We did not determine how many people went from under 45 to over 45 in the course of the trial. Approximately 3 surgeons went from low experience to high experience groups during this study.
For the recurrent hernias, if you remember, the recurrent hernias were about 10–14% in both groups. There were only about 100 recurrent hernias in each group. We analyzed recurrent versus primary hernias as a factor when we did the regression analysis.
Dr. Eric W. Fonkalsrud (Santa Monica, California): Just a brief question about the role of the resident or trainee in this series of patients. Hernias are traditionally one of the first operations that surgeons assist junior residents during surgery training. If the senior surgeon allows the resident more independence, does that count against the senior faculty, and how does this setting relate to the younger surgeon actually doing the surgery? Do you have any information regarding the role of the trainee versus the surgeon in charge in these operations?
Dr. Leigh A. Neumayer (Salt Lake City, Utah): We believe in the majority of open repairs, that the resident was on the side of the hernia, and presumably was the person making the cut and putting the stitches in. In the laparoscopic repair, both people participated. We did not record who had their hands on the instruments versus the camera, which may have been helpful, so I can't tell you that. We do think there may have been more attention paid during laparoscopic repairs than open repairs because they were less familiar to the attendings.
Dr. Donald D. Trunkey (Portland, Oregon): Was an attending surgeon available for all cases or did the chief residents do some of the supervision?
Dr. Leigh A. Neumayer (Salt Lake City, Utah): Not only were they available, but the attending surgeon had to be scrubbed. A protocol deviation was filed if they weren't. We only had about 10 of those out of 1800 repairs.
Footnotes
Supported by the Cooperative Studies Program of the Department of Veterans Affairs Office of Research and Development.
Reprints: Leigh A. Neumayer, MD, MS, VAMC-112, 500 Foothill Drive, Salt Lake City, UT 84148. E-mail: leigh.neumayer@hsc.utah.edu.
REFERENCES
- 1.Neumayer L, Giobbie-Hurder A, Jonasson O, et al. Open mesh versus laparoscopic mesh repair of inguinal hernia. N Engl J Med. 2004;350:1819–1827. [DOI] [PubMed] [Google Scholar]
- 2.Wilkemeyer M, Pappas TN, Hurder A, et al. Does resident post graduate year influence the outcomes of inguinal hernia repair? Ann Surg. 2005;241:879–884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Killian CA, Graffunder EM, Vinciguerra TJ, et al. Risk factors for surgical-site infections following cesarean section. Infect Control Hosp Epidemiol. 2001;22:613–617. [DOI] [PubMed] [Google Scholar]
- 4.Smabrekke A, Havelin LI, Furnes O. Operating time and survival of primary total hip replacements: an analysis of 31,745 primary cemented and uncemented total hip replacements from local hospitals reported to the Norwegian Arthroplasty Register 1987–2001. Acta Orthop Scand. 2004;75:524–532. [DOI] [PubMed] [Google Scholar]
- 5.Khuri S, Daley J, Henderson W, et al. and participants in the National Veterans Administration Surgical Risk Study. The national Veterans Administration surgical risk study: risk adjustment for the comparative assessment of the quality of surgical care. J Am Coll Surg. 1995;180:519–531. [PubMed] [Google Scholar]
- 6.American Board of Medical Specialties. The Official ABMS Directory of Board Certified Medical Specialists. Philadelphia: WB Saunders/Elsevier; 2004. [Google Scholar]
- 7.American College of Surgeons Fellowship Database. Accessed February 2, 2005.
- 8.Hosmer DW Jr, Lemeshow S. Applied Logistic Regression. New York: John Wiley & Sons; 1989. [Google Scholar]
- 9.Begg CB, Cramer LD, Hoskins WJ, et al. Impact of hospital volume on operative mortality for major cancer surgery. JAMA. 1998;280:1747–1751. [DOI] [PubMed] [Google Scholar]
- 10.Halm EA, Lee C, Chassin MR. Is volume related to outcome in health care? A systematic review and methodologic critique of the literature. Ann Intern Med. 2002;137:511–520. [DOI] [PubMed] [Google Scholar]
- 11.Birkmeyer JD, Stukel TA, Siewers AE, et al. Surgeon volume and operative mortality in the United States. N Engl J Med. 2005;349:2117–2127. [DOI] [PubMed] [Google Scholar]
- 12.Choudhry NK, Fletcher RH, Soumerai SB. Systematic review: the relationship between clinical experience and quality of health care. Ann Intern Med. 2005;142:260–273. [DOI] [PubMed] [Google Scholar]
- 13.Hartz AJ, Kuhn EM, Pulido J. Prestige of training programs and experience of bypass surgeons as factors in adjusted patient mortality rates. Med Care. 1999;37:93–103. [DOI] [PubMed] [Google Scholar]
- 14.O'Neill L, Lanska DJ, Hartz AJ. Surgeon characteristics associated with mortality and morbidity following carotid endarterectomy. Neurology. 2000;55:773–781. [DOI] [PubMed] [Google Scholar]
- 15.Sawaki L, Yaseen Z, Kopylev L, et al. Age-dependent changes in the ability to encode a novel elementary motor memory. Ann Neurol. 2003;53:521–524. [DOI] [PubMed] [Google Scholar]
- 16.Perryman KM, Fitten LJ. Effects of normal aging on the performance of motor-vehicle operational skills. J Geriatr Psychiatry Neurol. 1996;9:136–141. [DOI] [PubMed] [Google Scholar]
- 17.Wanzel KR, Hamstra SJ, Caminiti MF, et al. Visual–spatial ability correlates with efficiency of hand motion and successful surgical performance. Surgery. 2003;134:750–757. [DOI] [PubMed] [Google Scholar]
- 18.Risucci DA. Visual spatial perception and surgical competence. Am J Surg. 2002;184:291–295. [DOI] [PubMed] [Google Scholar]
- 19.Neumayer L, Jonasson O, Fitzgibbons RJ Jr, et al. Tension-free inguinal hernia repair: the design of a trial to compare open and laparoscopic surgical techniques. J Am Coll Surg. 2004;196:743–752. [DOI] [PubMed] [Google Scholar]
- 20.Rogers DA, Elstein AS, Bordage G. Improving continuing medical education for surgical techniques: applying the lessons learned in the first decade of minimal access surgery. Ann Surg. 2001;233:159–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.American College of Surgeons. Approval of courses in new skills. Bull Am Coll Surg. 1998;83:35–36. [PubMed] [Google Scholar]
- 22.American College of Surgeons. Statement on emerging surgical technologies and the evaluation of credentials. Bull Am Coll Surg. 1994;79:40–41. [PubMed] [Google Scholar]
- 23.American College of Surgeons. Statement on issues to be considered before new surgical technology is applied to the care of patients. Bull Am Coll Surg. 1995;80:46–47. [PubMed] [Google Scholar]