Abstract
Summary and Background Data:
As a result of many factors, the availability of neurosurgeons (NS) to care for trauma patients (TP) is increasingly sparse. This has precipitated a crisis in access to neurosurgical support in many trauma systems, often placing undue burden on level I centers. This study examines the profile of head-injured (HI) trauma patients and their actual need for the specific expertise of a neurosurgeon.
Methods:
The National Trauma Data Bank (NTDB) was queried for specific information relating to the volume, nature, timeliness, and outcome of HI TP. Study patients were identified by reported International Classification of Diseases, 9th Edition (ICD-9) codes denoting open (OHI) or closed head injury (CHI) in isolation or in combination with other injuries.
Results:
Total number of NTDB patients studied was 731,823, of which 213,357 (29%) had a reported HI. CHI represented 22% of all TP and 74% of HI. OHI was reported in 8% of all TP and was 26% of HI. Craniotomy (crani) was performed in 3.6% of all HI (1% of all TP). This was in 2.8% of OHI and 2.6% of CHI. Mean Glasgow Coma Scale score (GCS) of crani patients was 9, and 13 for the noncrani group. Subdural hematoma occurred in 18% of HI (5% of TP), with 13% undergoing crani. Epidural hematoma occurred in 10% of HI (3% of all TP), with 17% undergoing crani. Median time to OR for all cranis was 195 minutes (195 for CHI; 183 for OHI). Of all cranis, 6.5% were performed within 1 hour of hospital admission. intracranial pressure (ICP) monitoring was reportedly used in 0.7% of TP and 2.2% of HI.
Conclusions:
Care of TP with HI rarely requires the explicit expertise and immediate presence of a neurosurgeon due to volume and nature of care. HI was diagnosed in <30% of TP reported to the NTDB. Over 95% required nonoperative management alone, with only 1% of all TP and 2%–4% of HI TP requiring crani and/or ICP monitoring. Immediate availability of NS is not essential if a properly trained and credentialed trauma surgeon or other health care provider can appropriately monitor patients for neurologic demise and effect early transfer to a center capable of, and committed to, operative and postoperative neurosurgical care. A subgroup of patients known to have a high propensity for the specific expertise of a neurosurgeon may be able to be identified for direct transport to these committed centers.
Due to the frequency, severity, nature, and timeliness of head injury care, the explicit expertise and immediate presence of a neurosurgeon is not essential to achieve acceptable treatment of neurotrauma. Appropriately trained and credentialed trauma surgeons or other nonneurosurgeons may be able to fill this role in trauma care.
It is estimated that 1.5 million Americans sustain traumatic brain injuries each year.1 As a result of many factors, the availability of neurosurgeons (NS) to care for trauma patients (TP) is increasingly sparse. One factor is lack of availability due to the limited number of NS nationally, particularly in rural areas. There are reportedly 3047 board-certified NS practicing in the United States (personal communication: American Board of Neurologic Surgery). Approximately 150 new NS are certified each year, with approximately the same number reportedly leaving active practice. There are approximately 800 neurosurgical residents in training in any given year. The average age of active American Association of Neurological Surgeons members is 56 (personal communication: American Association of Neurological Surgeons).
Other factors affecting the availability of neurosurgical services include issues related to perceived medicolegal risk, disproportionate reimbursement with regard to work effort in comparison to elective cases, and increased malpractice premium rates for inclusion of trauma within the scope of practice.2–4 These issues have caused many NS to abandon trauma care or relinquish craniotomy privileges at their hospitals. One study, done in 1993, revealed that at that time at least 20% of NS preferred not to treat TP.4 The medicolegal, as well as the reimbursement, climates have certainly not improved since that time.
The resultant physical and functional lack of NS available to care for TP has precipitated a crisis in access to neurosurgical support in many trauma systems, often placing undue burden on level I and II trauma centers. Even at these facilities, which by definition have declared a commitment to trauma care, full neurosurgical support is often absent or difficult and/or costly to maintain.5
The American College of Surgeons Committee on Trauma document on the resources required for optimal TP care mandates that immediate neurosurgical availability is essential for verification as a level I or level II trauma center.6 This may not be achievable, feasible, or maintainable in the current health and trauma care milieu. Trauma surgeons can potentially fill this void of neurosurgical support, if they are appropriately trained, credentialed, and monitored. The neurosurgical community must also accept them in this role.
This concept of non-NS caring for neurotrauma patients is predicated on the hypothesis that the only explicit need for a NS is to perform a craniotomy. Nonoperative management of mild to severe injuries, with or without intracranial hypertension, may be equally well managed by providers outside the discipline of neurosurgery. This concept is also founded on a reduced emphasis on the time-critical nature of lesions requiring craniotomy and a lesser immediacy of craniotomy need. It is conceivable that there are factors associated with a subsequent need for craniotomy which can be identified in the prehospital environment, or early on during initial hospital treatment, making patients who exhibit such characteristics candidates for bypass of certain hospitals or transfer to definitive neurosurgical care within a time period correlating with optimal outcome. There may also be identifiable characteristics that deem the patient unsalvageable and therefore not candidates for triage and transfer for neurosurgical care. The purpose of this study is to examine the profile of head-injured TP nationally and determine their actual need for the specific expertise of a NS, as well as the timeliness of that care.
METHODS
The National Trauma Data Bank (NTDB) version 3.07 was queried for specific information relating to the volume, nature, timeliness, and outcome of head-injured TP. The NTDB is the most complete national clinical database of injured patients currently available. It is maintained by the American College of Surgeons and includes data voluntarily submitted by trauma centers of all levels of designation. The data are monitored for quality using mechanisms that are a part of the National Trauma Registry of the American College of Surgeons (NTRACS) software and additional monitors as dictated by the NTDB administrators. The NTDB includes data pertaining to demographics, injury severity, mechanism, associated injuries, complications, and mortality, among other information. All NTDB data management is HIPAA compliant. The data used for this study included all patients entered into the NTDB from 1994 through 2003, during which time 268 trauma centers contributed data. Thirty-five percent (n = 94) were designated or verified level I trauma centers.
The database was queried using Microsoft SQL server 2000 and Microsoft Access 2000 to select patients appropriate for inclusion in the study. Study patients were identified by reported ICD-9 codes denoting open head injury (OHI) or closed head injury (CHI) in isolation or in combination with other injuries. ICD-9 codes indicative of OHI or CHI were considered to be 800–801.99, 803–804.99, 850–854.19, 873.0, 873.1, 873.9, 959.0, and 959.01. In addition to standard demographics, specific data elements analyzed related to the nature of head injury, head AIS, performance of craniotomy, performance of intracranial pressure monitoring, Glasgow Coma Scale score, time to craniotomy, and mortality.
RESULTS
A summary of results is displayed in Tables 1 and 2. The total number of NTDB patients studied was 731,823, of which 213,357 (29%) had an ICD-9 code denoting head injury that was reported. CHI comprised 22% of all TP and 74% of those reported to have head injury. OHI was reported in 8% of all TP and represented 26% of reported head injuries. Craniotomy was performed in 3.6% of all head-injured patients, which represents 1% of all TP studied. The frequency of craniotomy was 2.8% in OHI and 2.6% in CHI.
TABLE 1. Profile of Head Injury From the NTDB
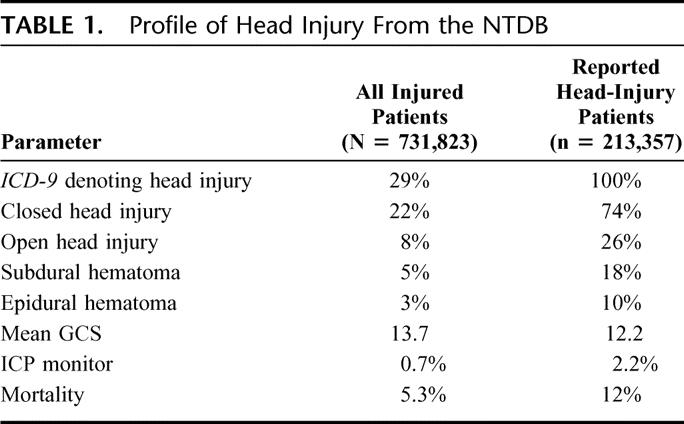
TABLE 2. Profile of Patients Undergoing Craniotomy
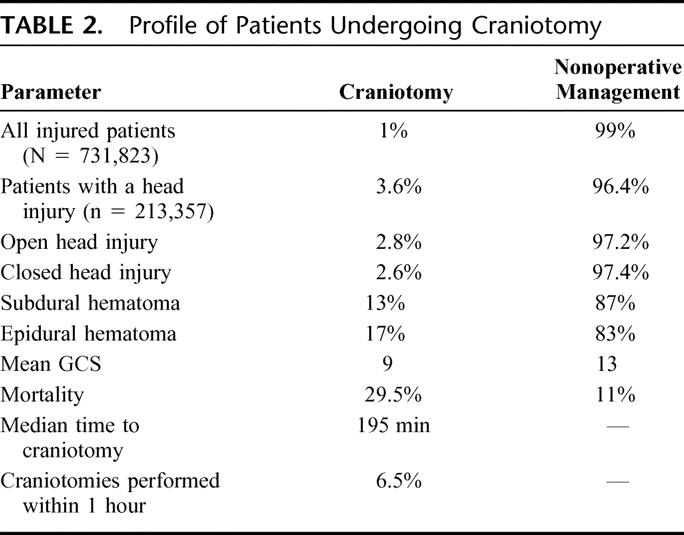
The mean GCS of all TP was 13.7. The mean GCS of head-injured patients was 12.2, and for non–head-injured, it was 14.4. The mean GCS of craniotomy patients was 9, and for the patients not undergoing craniotomy, it was 13.
Subdural hematoma occurred in 18% of head-injured patients (5% of all TP), with 13% of those undergoing craniotomy. Epidural hematoma occurred in 10% of the head-injured patients (3% of all TP), with 17% of those undergoing craniotomy. The median time to operation for all craniotomies was 195 minutes (195 minutes for CHI; 183 minutes for OHI). For patients with epidural hematoma, the median time to operation was 156 minutes; for those with subdural hematoma, the median time to operation was 180 minutes. For all craniotomies performed, 6.5% were performed within 1 hour of hospital admission. Intracranial pressure monitoring was reportedly used in 2.2% of all head-injured patients, which represents 0.7% of all TP.
Mortality of all TP was 5.3%; for those with head injuries, it was 12%. In patients with reported head injuries, the mortality for those not undergoing craniotomy or ICP monitoring was 11%, and in those patients receiving such intervention, it was 29.5%. Mortality for patients undergoing craniotomy within 195 minutes was 21%. For craniotomies performed at greater than 195 minutes but within 24 hours, mortality was 15%.
The majority of patients undergoing craniotomy within 1 hour had a GCS of 9 or less recorded at the scene (Fig. 1). These patients represent an exceedingly small proportion of the total number of patients presenting with a GCS score in any category (Fig. 2). When stratified by time to craniotomy, ED GCS score, and mortality, it appears there is little difference in mortality related to performance of craniotomy, within 1, 2, or 3 hours (Fig. 3). This is borne out when comparing mortality for head AIS between the different time intervals of craniotomy performance (Fig. 4). A noteworthy increase in mortality approaching 60% is seen in patients with ED GCS of 7 or less independent of craniotomy timing.
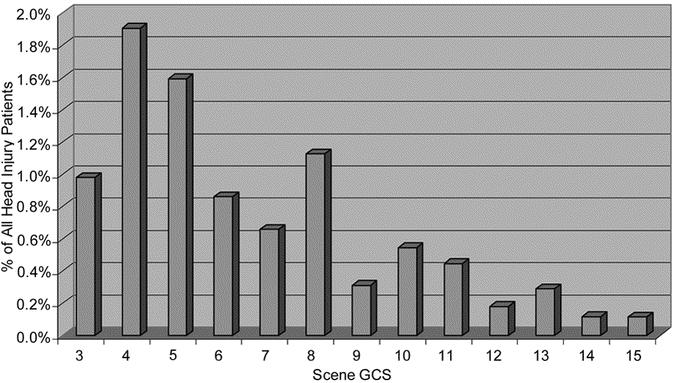
FIGURE 1. Percent of head injury patients undergoing craniotomy within 1 hour by scene GCS.
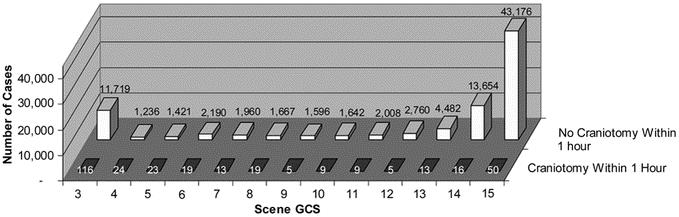
FIGURE 2. Head injury patients with and without craniotomies within 1 hour by scene GCS.
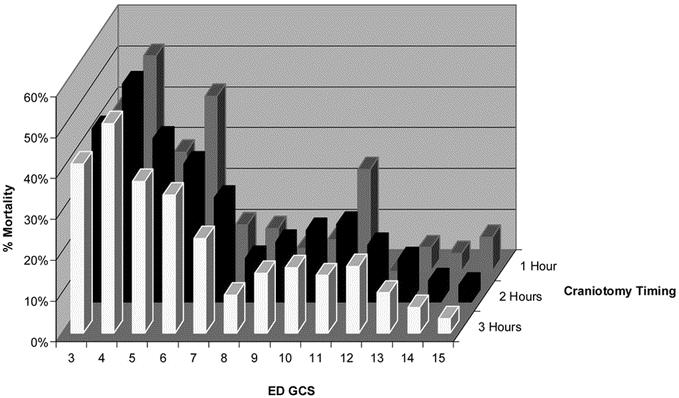
FIGURE 3. Percent mortality by ED GCS and craniotomy timing.
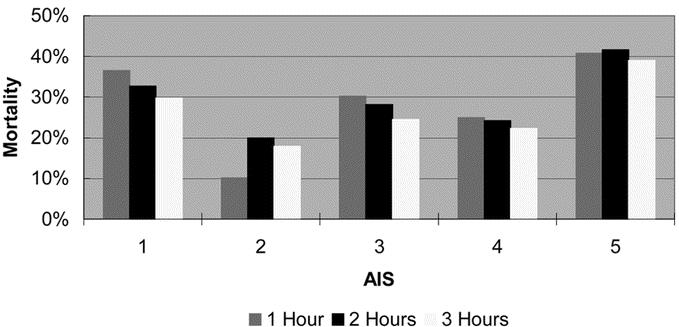
FIGURE 4. Percent mortality by time to craniotomy and AIS head.
DISCUSSION
This study suggests that the care of TP with head injury rarely requires the explicit expertise and immediate presence of a NS due to the volume and type of injuries sustained, as well as the nature of their care. Head injury is reported to be present in less than 30% of TP cataloged in the NTDB. Over 95% required nonoperative management, with only 1% of all TP and 2%–4% of head-injured TP requiring craniotomy and/or intracranial pressure monitoring. This is consistent with the low frequency of neurosurgical intervention demonstrated by other studies, which ranges from 0%–5.9% in the head injured.8–13 The preponderance of mild to moderate head injury severity revealed in the NTDB is corroborated by other series as well.14,15
The immediate availability of a NS does not appear to be essential if a properly trained and credentialed general trauma surgeon, or perhaps other health care provider, can appropriately evaluate and monitor patients for neurologic injury and demise. The responsibility of these non-NS should also encompass the knowledge and ability to effect early transfer to a center capable of, and committed to, operative and postoperative neurosurgical care. A subgroup of patients known to have a high propensity for the specific expertise of a NS should be identified and targeted for direct transport or immediate transfer to centers that are committed to sophisticated neurosurgical management.
From a provocative, if not realistic, perspective, the only true need for intimate neurosurgical involvement in TP care revolves around the performance of craniotomy and the decision to do so. Clearly, this study shows that from the standpoint of volume of those types of injuries generally thought to require craniotomy, as well as the number of craniotomies actually performed, neurosurgical availability does not appear to be crucial. Most of all TP, and in particular the head injured, were managed without craniotomy. Even in the case of space-occupying lesions and open head injuries, this study suggests that the majority do not undergo craniotomy. From the standpoint of timeliness to craniotomy, a median time of over 3 hours would again speak against the essential need for a NS to be “immediately” available. Only 6.5% of craniotomies in this study were performed within 1 hour of hospital admission.
The lack of ability to show an association between more rapid craniotomy and improved outcome in this series runs counter to the work of Seelig et al,16 which did demonstrate such a positive correlation between craniotomy time and outcome. The reason for the discrepancy between studies is not entirely clear. It may be that many patients included in this study died prior to receiving craniotomy. Time from injury to death was not examined. Regardless, it remains impossible to know whether mortality or subsequent neurosurgical morbidity would have been improved if those patients in this study who did survive to craniotomy had undergone that operation more rapidly.
The higher mortality rate in patients undergoing rapid craniotomy (within 1 hour) versus delayed craniotomy (>195 minutes but less than 24 hours.) is more than likely explained by the increased severity of their head and/or associated injuries. Mortality appears to be associated with severity of injury and presenting GCS rather than timing of craniotomy. It also appears a GCS of 7 or less may present a significant and prohibitive risk of mortality. This renders rapid, or perhaps any, craniotomy more than likely futile and therefore not warranting the availability of a NS and the expenditure of already limited resources.
Certainly, the decision to perform craniotomy and the importance of neurosurgical involvement in that decision cannot be ignored. However, with the advent of telemedicine and particularly teleradiography, the physical presence and/or close proximity of a NS need not be the rule. It would also seem that in most systems, a decision to operate and transfer can be accomplished within the median time of 195 minutes for all craniotomies, or even the 156 minutes demonstrated for epidural hematomas in this study. In a properly tooled system, many, if not all, of these transfers might well be directly to the operating room at the second facility.
Slightly over 2% of those patients identified as having a head injury underwent ICP monitoring. The identification and management of intracranial hypertension is, without doubt, within the purview of the trauma surgeon and surgical intensivist.17 One might argue that it is optimally managed by these specialists who view the patient from a more global perspective and manage this specific neurosurgical condition within the context of other coexistent conditions and multiple injuries.
In addition to an undersupply, there is unquestionably a functional lack of NS available to be involved in the care of TP. This may be particularly true for those TP not requiring surgical intervention, with many NS abdicating neurosurgical critical care to other physicians such as neurologists, trauma surgeons, and intensivists. Valadka et al18 have shown that only 32% of NS surveyed indicated that in their experience, a NS is in charge of neurosurgical trauma care if no operation has been performed. There are initiatives to expand the scope of practice for general trauma surgeons in an effort to maintain viability and fill the voids in trauma care that currently exist.19 The Leapfrog initiative20 will also increase the availability and responsibility of intensivists for the provisions of care to TP. Given these facts, it would appear to be prudent to formalize and legitimize this nonoperative neurosurgical care, setting standards for performance and competency under the advisement of neurosurgical leadership.
There are data to support the safe and competent performance of intracranial pressure monitor placement and even emergency burr holes and craniotomies by trauma surgeons and non-NS.21,22 More than 40% of NS have indicated that non-NS should be allowed to insert ICP monitors, while only 14% endorsed performance of craniotomy by non-NS.18 When surveyed, 60% of practicing trauma surgeons favored the addition of limited neurosurgical procedures, short of craniotomy, to the training and scope of practice of future general trauma surgeons (Esposito and Jurkovich, unpublished data).
The degree of enthusiasm voiced by predominantly academic trauma surgeons may not be shared by community trauma surgeons in the current model of trauma care. Community general surgeon trauma practitioners show a similar rate of reluctance to treat TP in comparison to NS.2,4 Concerns of those community and academic general trauma surgeons not favoring an expanded role in neurotrauma care revolve around the potential for increased liability, as well as increased time and complexity of service required to manage intracranial hypertension and nonoperative head injury. It seems the liability issue is less potent if these trauma “specialists” are appropriately trained and credentialed.
It cannot be determined from this study whether the rate of intracranial monitoring is underreported, underused, or appropriately used. This study also does not answer whether outcome is improved with the use of intracranial pressure monitoring and treatment of intracranial hypertension. These are also important questions that must be answered if the issue of what provider institutes intracranial pressure monitoring and manages intracranial hypertension, in which patients, and with what frequency is to be resolved. The American Association of Neurologic Surgeons has proposed guidelines for the institution of intracranial pressure monitoring,23 but it is notclear whether these have been uniformly accepted or followed.
In addition to the need for ICP monitoring, the question of what type of monitor should be used is important from the standpoint of ease of insertion and technical expertise required. It may be that the Richmond bolt or Camino monitor, being less invasive and requiring less technical expertise for insertion, may be better for utilization by non-NS. This is, ofcourse, if it can be shown that they are of equal value incomparison to ventriculostomy and external ventricular drainage (EVD) in most patients.
Just as pertinent as the question of whether there is an undersupply of neurosurgical services is that of whether there is, perhaps, overutilization and inflated demand for such services. This may be true and inappropriate, regardless of the training background and professional credentials of the provider (ie, NS or trauma surgeon). Some authors have suggested that the propensity to obtain neurosurgical consultation is not indicated or associated with improved outcome.24 Questions revolving around the need for specific neurosurgical consultation in patients with minor and moderate head injury require an answer. It is not clear from this study, short of those patients requiring craniotomy and most likely intracranial pressure monitoring, how many received neurosurgical consultation. The need for utilization of intensive care unit monitoring to acquire serial neurologic examinations and the overutilization of these resources at trauma centers and nontrauma centers may also be in question.25,26 Finally, there is evidence to suggest that patients with suspected minor head injury and normal head CT findings can be safely discharged from the emergency department without neurosurgical or trauma surgical consultation if there are no other indications to request one.8,14,27
This overtriage of neurosurgical, trauma surgical, intensive care unit, and in-patient hospital services clearly taxes the system, adding to the crisis in access to care for those in whom it is appropriate. To a large extent, this overtriage is driven by medicolegal concerns that are often unfounded. This, in turn, creates a catch-22 situation. Liberal and unnecessary consultation for neurosurgical and/or trauma surgical evaluation to a great degree drives the reluctance to participate in trauma care. This issue needs to be addressed by healthcare policy makers, trauma system planners, and legislators of tort reform.
From a systems perspective, it is critical to identify factors that are associated with a high probability of need for craniotomy. This would allow for identification of such patients in the prehospital phase of care, making it appropriate to bypass hospitals without craniotomy services. It would also be the basis of strict transfer criteria from hospitals without those capabilities, thereby facilitating early transfer. In this study, it appears a GCS of 9 may be one of those criteria, that being the average GCS of those undergoing craniotomy and having a reasonable chance of survival. Interestingly, the mere presence of subdural hematoma or epidural hematoma does not necessarily equate with an absolute need for craniotomy. Prudence would certainly seem to suggest that EDH and SDH with or without lateralizing clinical signs and symptoms would best be initially included in such neurosurgical triage criteria. Size of lesion and corresponding clinical examination can certainly be added as qualifiers as a system matures and outcome data are available for analysis. Other considerations for early or direct transfer might be identified as well and evaluated for under- and overtriage.
One condition that should not be considered as an indication for transfer is impending, suspected, or confirmed brain death. In this study, a GCS score of 7 or less seems to fit such a parameter, being associated with a grave prognosis with or without craniotomy. There is no benefit to the patient or the system in transfer under these circumstances. Declaration of brain death does not require the specific expertise of a NS. The knowledge and skill to perform this examination is also, and should be, within the scope of practice of general trauma surgeons and neurologists who are on staff at trauma centers, as well as nontrauma centers. Organ and tissue procurement can be accomplished at these nontrauma centers or trauma centers without neurosurgical availability just as easily and more cost efficiently than by transfer of the brain dead solely for organ procurement.
The NTDB is the largest database of its kind. However, it has limitations that may affect the results of this study and conclusions drawn from them. The database is not population based. Voluntary submission of data from only a limited number of trauma centers may introduce selection bias. Variability of contributing hospital TP definition and trauma registry inclusion criteria, along with the absence of uniform ICD-9 coding practices and recording of procedures, may lead to an underestimation of the parameters analyzed in thisstudy.
This study does not include the spine-injured patient, which also oftentimes falls under the purview of the neurologic surgeon. These patients were specifically excluded from the study as they also oftentimes fall under the purview of orthopedic surgery. The inclusion of spine-injured patients in this study was felt to potentially dilute the results. This issue, however, warrants equal scrutiny from the same perspective. Likewise, the pediatric head-injured patients were not analyzed separately in this study. They would also seem to warrant special attention as there appears to be even greater reluctance on the part of community, and even some university NS, to treat this subpopulation of TP.
Finally, as mentioned previously, it is not possible to discern from this study whether the rates of craniotomy, ICP monitoring, neurosurgical consultation, or ICU or hospital admission extracted from the NTDB are accurate or represent over- or underutilization, appropriate utilization, or are associated with improved outcomes. It is assumed that the information gleaned from the NTDB represents benchmark data reflective of optimal management and outcome based on the fact it is submitted by hospitals committed to trauma care and willing to voluntarily contribute their data.
In conclusion, the abandonment of trauma care by rank-and-file NS has created a crisis in access to neurotrauma care. Despite any limitations of the study, the results presented provide evidence to support that the immediate availability of a NS to participate in the care of all TP, including those with documented head injury, may not be essential to providing optimal care. Given the volume, nature, and timeliness of head injury and its care, it appears this crisis can be resolved to a great extent by having trauma surgeons or other properly trained, credentialed, and monitored providers assume nonoperative in-patient neurotrauma care when hospital admission is actually indicated. While part of the solution lies in increased supply of neurotrauma services, regardless of provider type, a second component rests in decreasing demand for those services in cases of mild, as well as extremely severe, head injury. Such a solution seems feasible and advantageous in a number of respects and should be seriously considered by health care policy makers, trauma system planners, and the leaders of the neurosurgical and trauma surgery disciplines.
Discussions
Dr. Donald D. Trunkey (Portland, Oregon): This is a very provocative paper, much of which I agree with. It represents a fair assessment of a major problem and offers solutions that are practical and doable but, in my opinion, do not go far enough.
In the discussion, they address the limits of the National Trauma Data Bank. It is the largest registry ever. However, it does not even represent the majority of Level I and II centers, and none of the community hospitals that are undesignated or not part of a state trauma system.
There are some results in this study that run counter to those in the literature, especially the paper by Seelig and co-authors in The New England Journal of Medicine. Those authors in Virginia showed that time to operation was important in reducing mortality and neurologic disability, and was particularly true if the operation was done within 2 hours. How do the authors in this study rationalize this difference? Their time, 195 minutes, is very disturbing. Another disappointing result was that only 2.2% of the head-injured patients received an ICP. I would like to know of those patients that had GCS 8 or less how many had ICP, because the National Trauma Guidelines by the neurosurgeons say that an ICP is indicated.
The authors compare ED GCS and mortality in timing of operation at 1, 2, and 3 hours. Did this include the prehospital time? The mortality was quite high in those with GCS less 7. However, if we look carefully at their graphs, the GCS of 10, 11, and 12 also had mortalities of greater than 10%. This tends to refute their conclusion that these patients can be transferred for neurosurgical care at a higher level. It also refutes their first statement in the discussion that the care of patients with head injury rarely, underline “rarely,” requires the explicit expertise and immediate presence of a neurosurgeon.
I do agree with the authors that it is unrealistic to expect neurosurgeons to care for all head-injured patients. I agree that general surgeons should be able to place ICP monitors. However, I would go further. I think a general surgeon could be trained to perform a ventricular drainage and craniotomies for epidurals and subdurals. It has been done with good results in rural America and it has also been done in New Zealand, Malaysia, and in Darwin, Australia, with results equal to those achieved in neurosurgical centers.
I agree with the authors that GCS 7 or less portends a very bad outcome. However, before we pull the plug on the ventilator, you have to rule out other organic causes of coma such as substance abuse and alcohol. A quick CT should be done quickly to confirm the clinical impression.
I like this paper. I would like your comments on my discussion.
Dr. Fred A. Luchette (Maywood, Illinois): We knew this paper would be provocative and we wanted the most critical review possible to open the discussion.
Your first question involved reconciling our observations with the results published by Seelig et al from Virginia, which state that time to operation is important and improves morbidity and mortality. This was particularly true when the time was 2 hours or less. We agree with you and the Virginia groups conclusions that time is important. Clearly, when a neurosurgeon and an institution are committed to caring for injured patients, patient outcome is better. Our data from the NTDB was collected from multiple Level I and II trauma centers and non-trauma centers admitting injured patients throughout the country. We feel the data we presented today are much more representative of neurosurgical care for head-injured patients on a national basis. Trauma care should maintain the highest standards for all outcomes and strive to obtain the equivalent or better results as reported by the neurosurgeons from Virginia. Our data suggest that the current level of resources does not allow us to provide optimal care for all head-injured patients as we currently judge optimal care. The professions and entire healthcare system need to address these limited resources and systems issues and come up with new solutions so that all head-injured patients receive equivalent and appropriate care anywhere in the nation.
I don't stand here claiming that the general surgeons or trauma surgeons should be performing craniotomies. However, as you appropriately pointed out, general surgeons can be trained to do burr holes and craniotomies when needed. That is just one option to address the limited resources.
My point in presenting this paper today is 1) to bring this limited resource issue, ie, neurosurgeons, to the attention of the surgical community, and 2) to raise the question of whether the requirement by the ACS COT that Level I and Level II trauma centers must have a neurosurgeon immediately available for injured patients to be reevaluated. In Illinois, neurosurgeons at Level II trauma centers are not participating in the evaluation of injured patients. This lack of commitment is placing an extreme burden on the Level I centers. I am fortunate that I work with a talented group of neurosurgeons who have stepped up to the plate and accepted this increased workload willingly and capably. Our care of the head-injured patient remains excellent despite a significant increase in patient volume over the last 3 years. Perhaps in metropolitan areas we can streamline triaging from the scene when a patient has sustained a severe injury according to GSC score. Perhaps these patients should be transported directly to a Level I center with committed neurosurgeons willing to provide a craniotomy within 2 hours and reduce the mortality for those patients.
You asked about the low incidence of ICP monitor use reported to the NTDB. One of the weaknesses of the NTDB that has been recognized by other investigators is that some data, particularly complications, are underreported. The AANS guidelines do advocate use of ICP monitors early in the management of the severe head injury. I am not sure whether the frequency we reported is true underutilization or just the fact that usage is underreported to the NTDB. It is a valid criticism of our data. I cannot answer your question on how many patients with a CGS less than 8 had an ICP monitor utilized. It would be reasonable to conclude that of all the patients who had an ICP monitor placed the majority also had a GCS score less than 8.
You asked about the ED GCS and the time to craniotomy. These times were determined from time of admission to the hospital to time of craniotomy. It did not include prehospital time. As you know, the NTDB does not include data about cause of death. The high mortality in the groups with a GSC score of 10, 11, and 12 may very likely be as a result of the influences of other injuries. We cannot assume that all the deaths in this moderate head injury group were due to the head injury alone. Rather the high incidence of associated chest and other injuries most likely accounted for some of the deaths.
I agree with your comments in reference to patients presenting with a GSC score 7 due to a traumatic injury. This does indeed portend a poor prognosis. Let me make it clear that the data we presented does not imply that we should “pull the plug on the ventilator.” All these patients need a full neurologic evaluation including a CT scan of the head and maximal medical and surgical therapy. Our data do support that perhaps the GCS 7 can be used as a field triage criteria for transport to the nearest trauma center with a committed neurosurgeon rather than transport to a Level II trauma center without this expert willing to evaluate and treat the patient.
Dr. John M. Howard (Toledo, Ohio): Unquestionably, intracranial head injury is the foremost problem that the trauma surgeon faces. Progress has been extremely slow over the period of years. It is too big a problem to leave to the neurosurgeon. As you noticed in your presentation the vast majority of patients do not require operative intervention for their management.
May I suggest that appropriate trauma centers organize multidisciplinary task forces to study the problem? Such teams might include pharmacologists, physiologists, pathologists and perhaps other basic disciplines, as well as the appropriate clinical departments. Some teams might wish to include prevention.
Through regular meetings involving reviews of current casualties and various aspects of the current literature, new hypotheses may be proffered, modified, withdrawn or tested. Without extramural funding, new ideas may be crystallized and significant progress achieved. (In a comparable experience, maintenance and circulation of minutes proved worthwhile.)
Dr. Fred A. Luchette (Maywood, Illinois): Thank you for your comments, Dr. Howard. That is an excellent suggestion and I agree with you 100%.
Dr. L.D. Britt (Norfolk, Virginia): Dr. Luchette, thank you for adding my name to the provocative list. There is no doubt that a properly trained and credentialed trauma surgeon can appropriately monitor patients for neurologic demise. However, emphasizing that this same trauma surgeon will be able to consistently effect early transfer of the patient to a center where there are readily available neurosurgeons who are committed to expeditious operative and consensus-driven neurological guidelines is more idealistic than realistic. The waning commitment of neurosurgeons to do trauma care is now widespread, even at the highest level of comprehensive health care, and that includes the tertiary and quaternary medical care centers.
I would like the authors to comment on the proposed acute care surgery model in which the acute care surgeon will be trained to do the limited number of procedures, which are about five, which will make up essentially all of the neurosurgical operations that are required in the acute care setting. And then the toughest question—and I truly embrace the NTDB (our repository for trauma data) but just because we get that information from trauma data banks does not mean that it, necessarily, represents the standard of care. Your comments on that?
Dr. Fred A. Luchette (Maywood, Illinois): Thank you, Dr. Britt, for agreeing on short notice to review the manuscript and comment. And yes, you are included on the provocative list.
As systems develop, perhaps in light of and using this study's findings, early recognition and transfer ie, regionalization of care will become standard and feasible in systems of care, both for neurosurgical and general trauma care led by Acute Care Surgeons.
The current requirements for Level I and II trauma centers are indeed ideal and not realistic as our data show. The move afoot to begin a new redefined specialty of acute care surgeons trained in five neurological procedures, clearly if this is endorsed by all the specialties involved with trauma care, I think will offer us a great opportunity for improving care to a new level in this country. I am impressed in my 25 years with the amount of progress we have made in the management of head-injured patients. Most of the folks in this room will remember when the theory was that we had to dehydrate the patients. And we have seen dramatic changes in survival with the new consensus-developed guidelines.
About seven years ago Jack Wilberger from Allegheny General gave a report at the ACS Clinical Congress. This was a survey he conducted of his neurosurgery colleagues regarding the use of their own consensus-developed guidelines. The responses revealed that the most commonly utilized portion of the guideline was using cerebral perfusion pressure (CPP) as determined by an ICP monitor. There was very limited use of a ventriculostomy. It was concerning that the practitioners do not embrace and practice according to their own AANS guidelines. Alex Valadaka has also provided similar data on ICP monitoring in a survey of his neurosurgical colleagues. My colleagues and I at Loyola are very supportive of the AANS guidelines and use them for managing head-injured patients. We may be more compliant with the guidelines than most neurosurgeons.
Regarding the NTDB as representing the standard of care. The intent is not to say that the NTDB represents the standard of care. The intent, rather, is to say the NTDB data represents real-time practice, what is going on in hospitals. It is a snapshot of everyday practice and can even be used for trending changes. Distribution of contributing trauma centers includes 35% Level I trauma centers, 25% Level II centers, 13% Level III centers, and 11% of reported Level IV and Level V centers. So the data are a reasonable cross-sectional representation of the care delivered for the injured patient at various designated and non-designated trauma centers.
Dr. Ralph G. Dacey, Jr. (St. Louis, Missouri): I am the chairman of the American Board of Neurological Surgery right now. I think this is an interesting and provocative paper, as other people have noted. But I think that it brings up some of the problems that exist with interrogating retrospectively an administrative database.
For example, 26% of patients in this study were reported to have open head injuries, 18% subdural hematomas, 10% epidural hematomas, but only 3.6% underwent craniotomy. These data do not square with the prospectively collected data put together by Marshall and others in the Traumatic Coma Data Bank in the ’90s, and I would ask the authors how they would compare their data with this other prospectively collected data.
I would like to comment on Dr. Trunkey's comments, too. I have talked to Dr. Trunkey about this before and we have had some nice discussions about this. But I think there are a couple things that we should all keep in mind.
Burr holes are seldom indicated and/or effective in the management of acute head injury. Placing an external ventricular drain in a patient with shifted ventricles or small ventricles is something that is sometimes very difficult, and I don't think can be done by the occasional surgeon. Some craniotomies for trauma can be easy. But I have seen patients undergoing craniotomies for trauma die in the operating room, exsanguinating from lesions in the superior sagittal sinus and in the infratemporal area.
I think that, to summarize, cooperation between trauma surgeons and neurosurgeons is going to be the key to solving this problem, which has been rightly identified. At Washington University in St. Louis, Dr. Eberlein and I are both committed to taking care of trauma patients, and we take care of a lot of them. And I think that the conclusion of the study that almost all patients can be taken care of by non-neurosurgeons is kind of like saying that just because most patients with abdominal pain can be managed by any physician doesn't mean that anybody, me included, should be doing Whipple procedures. So I would be interested in your comments.
Dr. Fred A. Luchette (Maywood, Illinois): Let me start with your last comment regarding abdominal pain. I don't think anybody in this room would claim that every patient in this country who develops abdominal pain gets evaluated by a surgeon, nor should they. In fact, they probably get evaluated by their primary care physician or internist, who then screens them to see if they need a consultation from a surgeon. All that we are proposing is that given the supply and demand that currently exists in light of the severity and nature of injuries being seen, that a similar tact with head injury is safe and feasible.
The incidence of epidural, subdural, open and closed head injuries in the NTDB is what it is. The NTDB is not an administrative database but rather a clinical one, admittedly of debatable accuracy and quality. It is a weakness of the database that the majority of that data is gathered at discharge after medical record personnel code specific diagnoses. Nonetheless, the data are representative of care and resource utilization in the hospitals caring for injured patients in this country. Since the late '80s and early '90s, it is my anecdotal impression that much like the general surgeons approach to management of liver and splenic injuries has become nonoperative, the neurosurgeon has shifted away from operative management of subdural and epidural hematomas especially in patients without lateralizing signs or elevated ICP. Hence, this may explain some of the apparent discrepancy you pointout.
I agree with you 110% that there should be cooperation across the disciplines. Tuesday night when I was on call, I got a call from a hospital 45 minutes south of Loyola. The hospital's administrator was in an MVC and had a LOC lasting 10 minutes. Despite a negative head CT scan, the surgeon on call was reluctant to admit the patient and sent thepatient to me. She was admitted overnight and discharged the next day. This massive utilization of human and financial resources occurred because the on-call surgeon was “not comfortable” caring for her and there was no neurosurgeon available to see the patient or evaluate them at their own facility. This breakdown in cooperation across the disciplines only impairs our ability to achieve optimal, timely care like you and Dr. Eberlein are able to obtain.
Dr. William P. Schecter (San Francisco, California): Twenty years ago I reported a series of 50 emergency craniotomies with good results that we did when I spent 2 years living in American Samoa. So I understand what you are saying.
However, I do want to make a provocative remark. We can easily exchange you for an emergency physician standing up at the microphone making the same argument. If we lookat the nonoperative treatment for abdominal and chest trauma, many emergency physicians are making the same argument.
I would not argue that I gave the same level of care that my neurosurgical colleagues at San Francisco General Hospital provide to our patients.
My view is that we have to insist on the highest standards of care for our trauma patients—which means that, if possible and if available, neurosurgeons must see acutely injured patients as soon as possible after injury.
Dr. Fred A. Luchette (Maywood, Illinois): Dr. Schecter, thank you for your comments. I agree with you that we can interpret this study several ways. One is the verification that Level I and II trauma centers have a neurosurgeon immediately available; whether that is realistic with the limited resources in the real world that we work in today is questionable.
I think that your comment about Emergency Medicine physicians and trauma is accurate and insightful. We are concomitantly seeing a similar abdication of trauma care by general surgeons in the community as well. I believe the same issues of supply, demand, and nature of injury apply to trauma in general and we may see for a number of reasons the mantra that “trauma is a surgical disease” be softened, and a more intimate role of Emergency physicians evolving in trauma systems.
I agree with the comment of maintaining the highest standards of care; however, according to our data those high standards can still be met without the immediate availability of a resource that will be increasingly hard to come by in the future for many reasons.
Dr. J. Wayne Meredith (Winston-Salem, North Carolina): Dr. Luchette, this was a very interesting paper and I enjoyed it very much. I want to applaud your use of the National Trauma Data Bank data. I believe it is one of the first papers presented to the American Surgical Association on the NTDB, and it is a very useful paper.
It is useful, however, as a first step in defining the magnitude of the problem for which we need a treatment; it does not provide us any insight as to what that treatment needs to be. I think you define how often the neurosurgeon is currently operating on a patient with head injury; it does not do anything to define whether or not it is imperative for those patients who need it to have it immediately.
To that regard, I can't stand and not mention something about the American College of Surgeons verification program and its requirements. In the last several years we have changed those requirements to better define the necessity of a neurosurgeon being available to allow for the credentialing by the neurosurgeon of general surgeons or trauma surgeons in the initial care with the proviso that a neurosurgeon is immediately available. That being said, I think that is very logical, very reasonable, and it does help the lack of availability of neurosurgeons.
I would strongly disagree with your recommendation or your implication that your data mean that a neurosurgeon is anything other than essential in a Level I or Level II trauma center. Our requirements are defined by the title “Resources for the Optimal Care of the Injured Patient,” not the resources with which one can get by and still call itself a trauma center. And I think we are defining optimal resource for the care of the injured patient that is here. That means a neurosurgeon is available for those patients who are bleeding who have expanding intracranial hematomas.
Dr. Fred A. Luchette (Maywood, Illinois): Again, by some of the data we presented today, we would like to suggest that perhaps triaging can occur in the field according to GCS score determined by the prehospital personnel. And rather than going to the nearest trauma center, which might be a Level II center that does not have a neurosurgeon available, that we bypass the Level II center and take the patient to the Level I center that is 5–10 minutes away with a neurosurgeon. Perhaps the guidelines and the requirements for trauma systems should allow a little bit of judgment from the field. Certainly a GCS less than 9 needs to be taken to a facility with neurosurgical capability immediately available. Nearly half the patients in this study have a GCS over 9 and may be able to be managed by a general acute care surgeon.
I think the manuscript points out for both craniotomy and ICP monitoring that it cannot be determined whether the numbers in the NTDB are accurate due to underreporting and further whether their performance, or nonperformance, was appropriate based on AANS guidelines or any other standards of optimal care. The same qualifier applies to the timing of craniotomy performance.
I don't disagree that the COT and its VRC strive to set forth standards for optimal care, and that, currently, optimal care involves the immediate presence of a neurosurgeon. What we hope to accomplish with this study is having the neurosurgical and trauma surgical leadership take pause and consider whether at this juncture, based on data, reevaluation of what optimal care of head injury is, and what the optimal time needed to provide these resources is. Trauma systems can then use this information to craft appropriate resource allocation. In some instances this may be a neurosurgeon, in some instance it may not. The goal of systems is to assure that in either case it makes no difference in outcome.
Footnotes
Reprints: Thomas J. Esposito, MD, MPH, Loyola University Medical Center, Department of Surgery, 2160 S. First Avenue, Bldg. 110, Room 4235, Maywood, IL 60153. E-mail: tesposi@lumc.edu.
REFERENCES
- 1.National Center for Injury Prevention and Control. Injury Fact Book 2001–2002. Atlanta, GA: Centers for Disease Control and Prevention; 2001. [Google Scholar]
- 2.Esposito TJ, Maier RV, Rivara FP, et al. Why surgeons prefer not to care for trauma patients. Arch Surg. 1991;126:292–297. [DOI] [PubMed] [Google Scholar]
- 3.Esposito TJ, Kuby AM, Unfred C, et al. Perception of differences between trauma care and other surgical emergencies: results from a national survey of surgeons. J Trauma. 1994;37:996–1002. [DOI] [PubMed] [Google Scholar]
- 4.Esposito TJ, Kuby AM, Unfred C, et al. National Survey of Surgeons on Trauma Care Issues: Robert Wood Johnson Foundation Report. Newark, NJ: 1993. [Google Scholar]
- 5.Trunkey DD. What price commitment? Bull Am Coll Surg. 2003;88:9–16. [PubMed] [Google Scholar]
- 6.Committee on Trauma, American College of Surgeons. Resources for Optimal Care of the Injured Patient 1999. Chicago, IL: American College of Surgeons; 1999. [Google Scholar]
- 7.National Trauma Data Bank (NTDB™) American College of Surgeons. Available at: http://www.facs.org/trauma/ntdb.html.
- 8.Nagy KK, Joseph KT, Krosner SM, et al. The utility of head computed tomography after minimal head injury. J Trauma. 1999;46:268–270. [DOI] [PubMed] [Google Scholar]
- 9.Dacey RG, Alves WM, Rimel RW, et al. Neurosurgical complications after apparently minor head injury: assessment of risk in a series of 610 patients. J Neurosurg. 1986;65:203–210. [DOI] [PubMed] [Google Scholar]
- 10.Stein SC, Ross SE. The value of computed tomographic scans in patients with low-risk head injuries. Neurosurgery. 1990;26:638–640. [DOI] [PubMed] [Google Scholar]
- 11.Shackford SR, Wald SL, Ross SE, et al. The clinical utility of computed tomographic scanning and neurologic examination in the management of patients with minor head injuries. J Trauma. 1992;33:385–394. [DOI] [PubMed] [Google Scholar]
- 12.Miller EC, Holmes JF, Derlet RW. Utilizing clinical factors to reduce head ct scan ordering for minor head trauma patients. J Emerg Medic. 1997;15:453–457. [DOI] [PubMed] [Google Scholar]
- 13.Mohanty SK, Thompson W, Rakower S. Are CT scans for head injury patients always necessary? J Trauma. 1991;31:801–805. [DOI] [PubMed] [Google Scholar]
- 14.Taheri PA, Karamanoukian H, Gibbons K, et al. Can patients with minor head injuries be safely discharged home? Arch Surg. 1993;128:289–292. [DOI] [PubMed] [Google Scholar]
- 15.Steill IG, Wells GA, Vandemheen K, et al. Variation in ED use of computed tomography for patients with minor head injury. Ann Emerg Med. 1997;30:14–22. [DOI] [PubMed] [Google Scholar]
- 16.Seelig JM, Becker DP, Miller JD, et al. Traumatic acute subdural hematoma: major mortality reduction in comatose patients treated within four hours. N Engl J Med. 1981;304:1511–1518. [DOI] [PubMed] [Google Scholar]
- 17.American Association for the Surgery of Trauma and The Committee on Trauma of The American College of Surgeons. Guidelines for trauma care fellowships. J Trauma. 1992;33:491–494. [PubMed] [Google Scholar]
- 18.Valadka AB, Andrews BT, Bulock M, et al. How well do neurosurgeons care for trauma patients? a survey of the membership of the American Association for the Surgery of Trauma. Neurosurgery. 2001;48:17–25. [DOI] [PubMed] [Google Scholar]
- 19.Esposito TJ, Rotondo MF, and the EAST Future of Trauma Surgery Committee. The position of the Eastern Association for the Surgery of Trauma on the Future of Trauma Surgery. J Trauma. 2005;59:77–79. [DOI] [PubMed] [Google Scholar]
- 20.Birkmeyer JD. The Leapfrog Group's patient safety practices, 2003: the potential benefits of universal adoption. Available at: www.leapfroggroup.org/media/file/Leapfrog-Birkmeyer.pdf.
- 21.Rinker CF, McMurry FG, Groenewegdr VR, et al. Emergency craniotomy in a rural level III trauma center. J Trauma. 1998;44:984–990. [DOI] [PubMed] [Google Scholar]
- 22.Ko K, Conforti A. Training protocol for intracranial pressure monitor placement by non-neurosurgeons: 5 year experience. J Trauma. 2003;55:480–484. [DOI] [PubMed] [Google Scholar]
- 23.Chestnut RM. Guidelines for the management of severe head injury: what we know and what we think we know. J Trauma. 1997;42:19S–22S. [DOI] [PubMed] [Google Scholar]
- 24.Bishofberger TE, Daley BJ, Snyder WE, et al. Repeat head CT and neurosurgery consultation for minor traumatic head injury is not indicated in neurologically stable patients with GCS 14 or 15. J Trauma. 2004;57:457. [Google Scholar]
- 25.Santaniello JM, Esposito TJ, Luchette FA, et al. Mechanism of injury does not predict acuity or level of service need: field triage criteria revisited. Surgery. 2003;134:4. [DOI] [PubMed] [Google Scholar]
- 26.Stephan PJ, McCarley M, Clifann RN, et al. Twenty-three hour observation solely for identification of missed injuries after trauma: is it justified? J Trauma. 2002;53:895–900. [DOI] [PubMed] [Google Scholar]
- 27.Livingston DH, Loder PA, Koziol J, et al. The use of CT scanning to triage patients requiring admission following the minimal head injury. J Trauma. 1991;31:483–489. [PubMed] [Google Scholar]


