Abstract
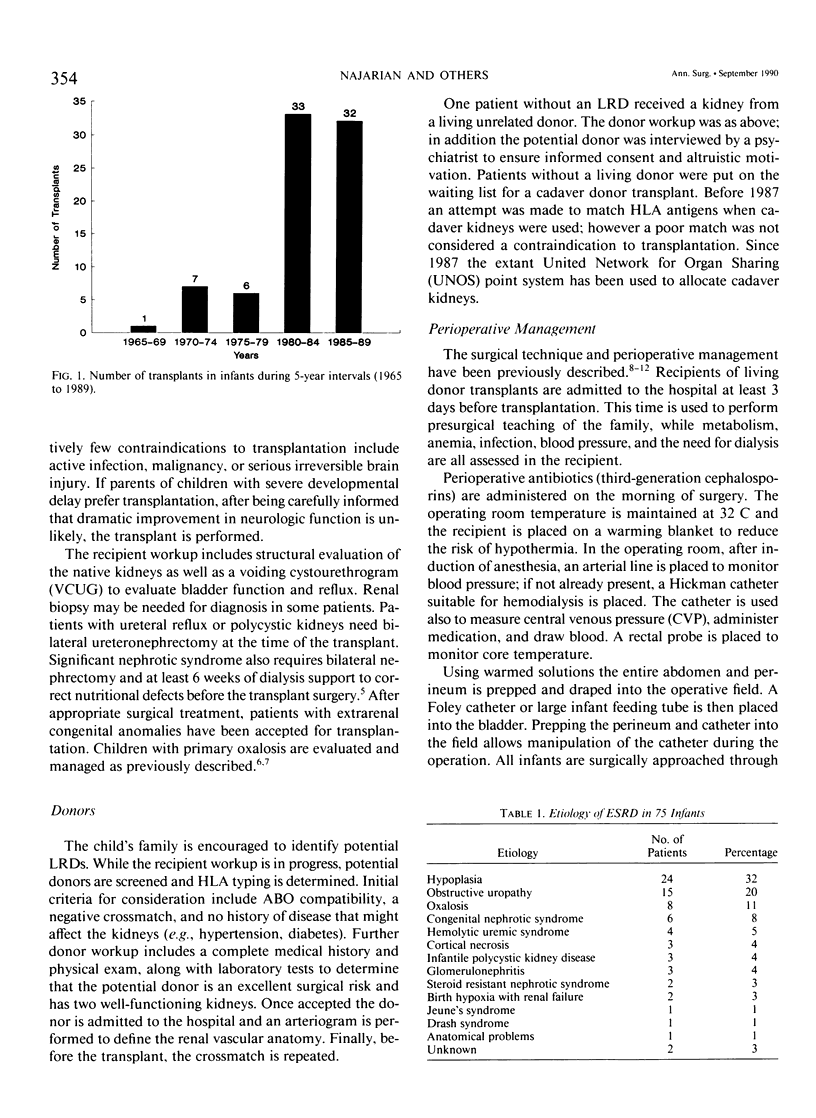
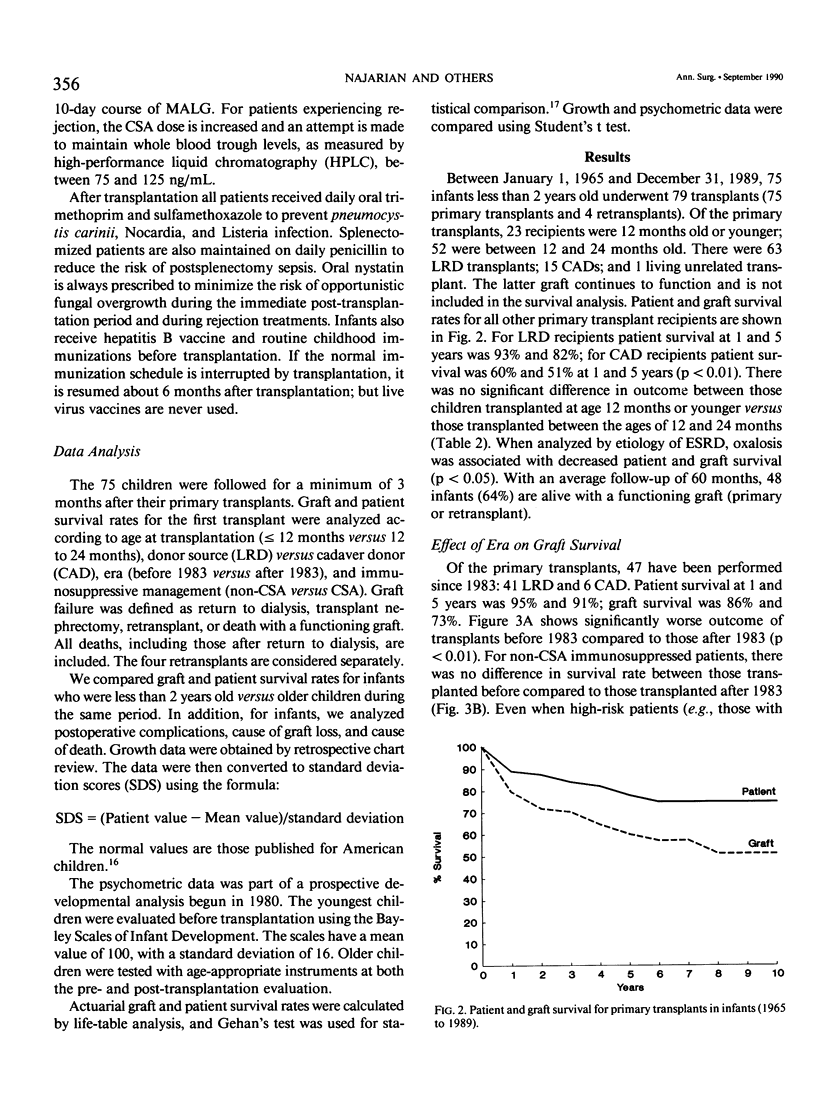
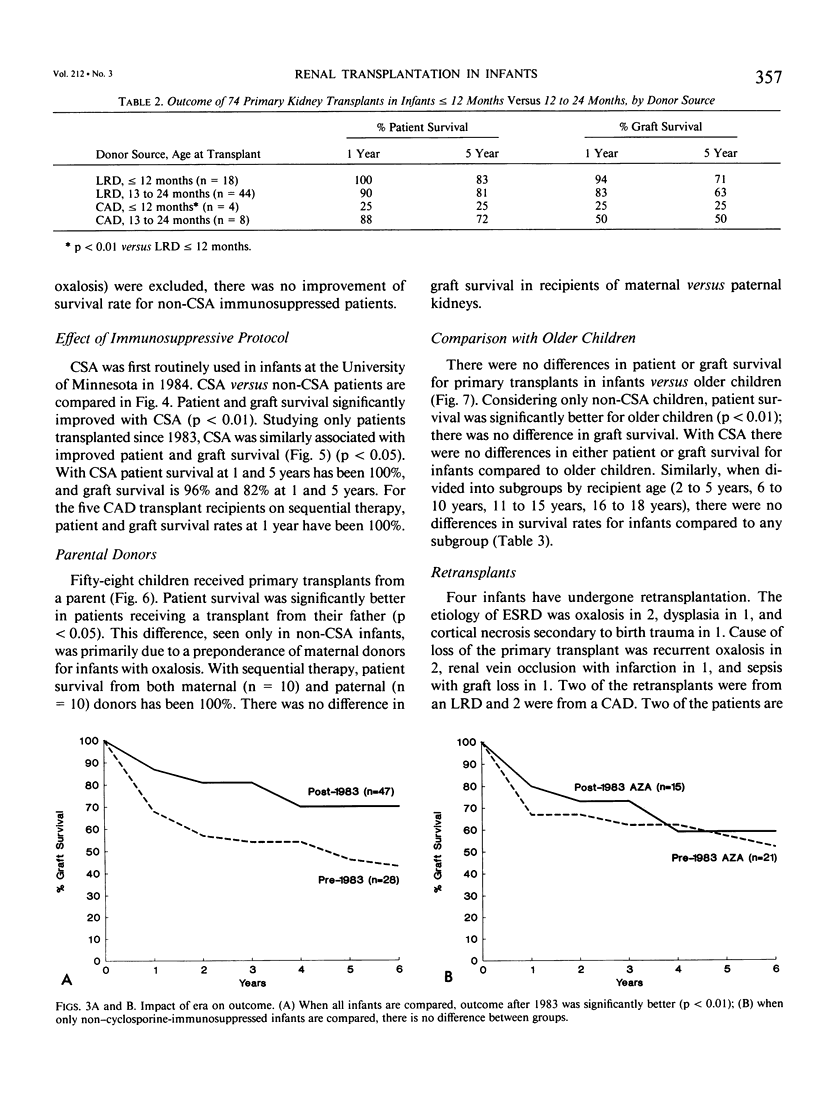
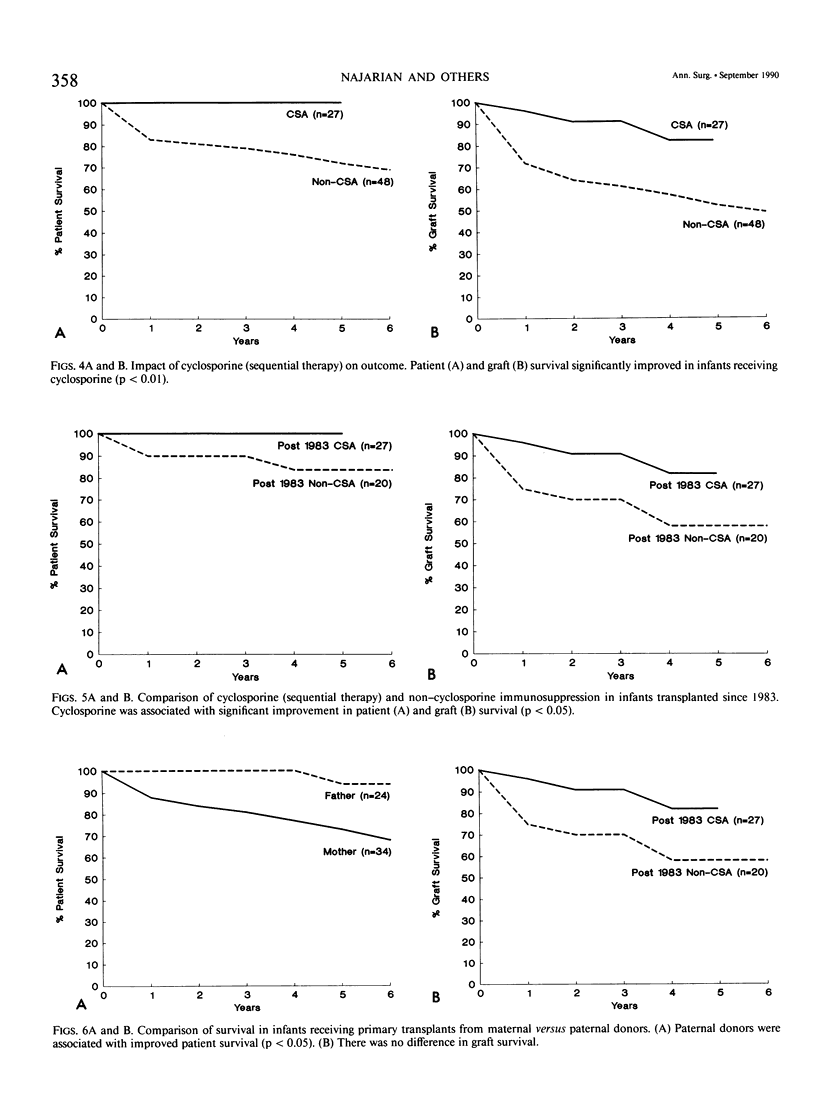
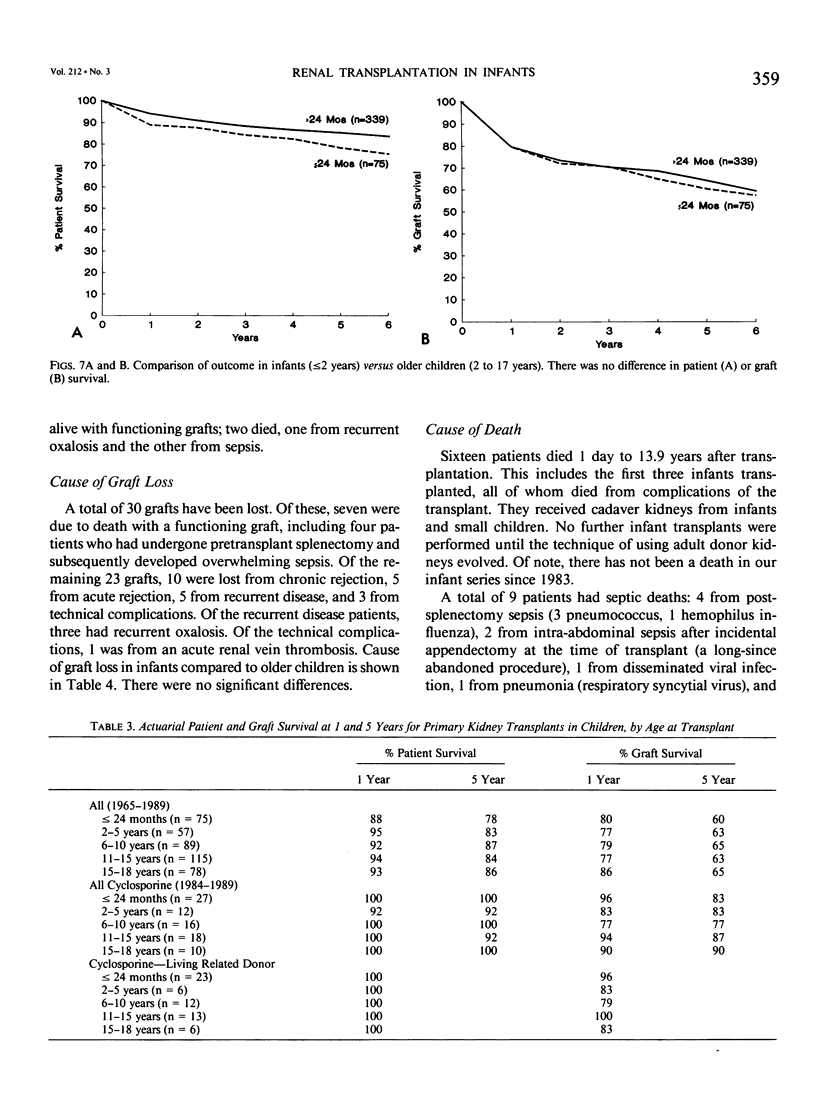
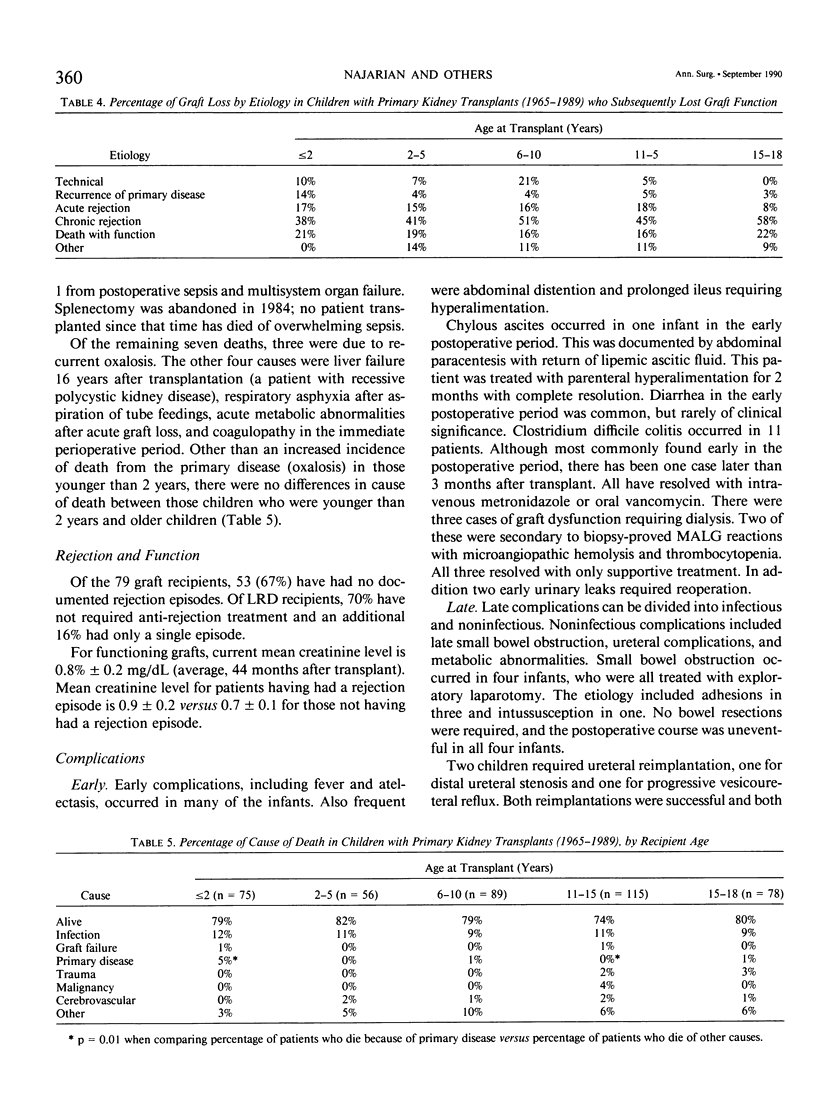
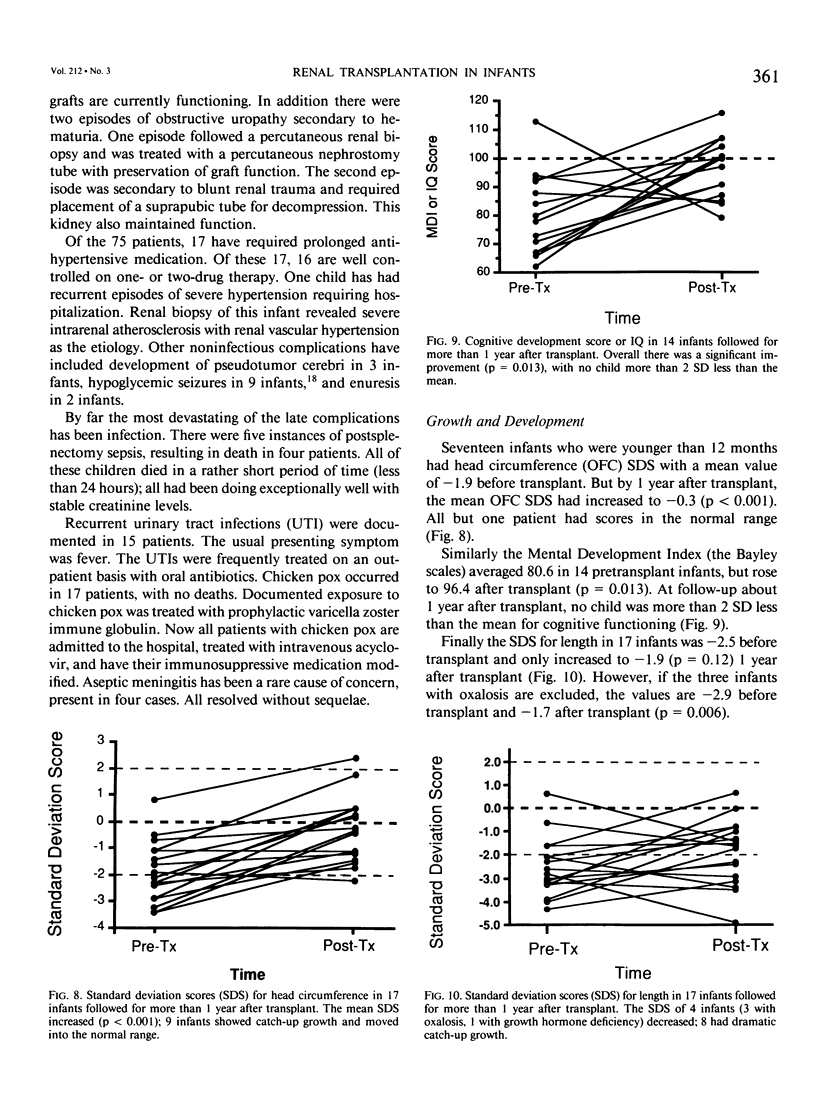
The timing of renal transplantation in infants is controversial. Between 1965 and 1989, 79 transplants in 75 infants less than 2 years old were performed: 23 who were 12 months or younger, 52 who were older than 12 months; 63 donors were living related, 1 was living unrelated, and 15 were cadaver donors; 75 were primary transplants and 4 were retransplants. Infants were considered for transplantation when they were on, or about to begin, dialysis. All had intra-abdominal transplants with arterial anastomosis to the distal aorta. Sixty-four per cent are alive with functioning grafts. The most frequent etiologies of renal failure were hypoplasia (32%) and obstructive uropathy (20%); oxalosis was the etiology in 11%. Since 1983 patient survival has been 95% and 91% at 1 and 5 years; graft survival has been 86% and 73% at 1 and 5 years. For cyclosporine immunosuppressed patients, patient survival is 100% at 1 and 5 years; graft survival is 96% and 82% at 1 and 5 years. There was no difference in outcome between infants who were 12 months or younger versus those who were aged 12 to 24 months; similarly there was no difference between infants and older children. Sixteen (21%) patients died: 5 after operation from coagulopathy (1) and infection (4); and 11 late from postsplenectomy sepsis (4), recurrent oxalosis (3), infection (2), and other causes (2). Routine splenectomy is no longer done. There has not been a death from infection in patients transplanted since 1983. Rejection was the most common cause of graft loss (in 15 patients); other causes included death (with function) (7), recurrent oxalosis (3), and technical complications (3). Overall 52% of patients have not had a rejection episode; mean creatinine level in patients with functioning grafts is 0.8 +/- 0.2 mg/dL. Common postoperative problems include fever, atelectasis, and ileus. At the time of their transplants, the infants were small for age; but with a successful transplant, their growth, head circumference, and development have improved. Transplantation in infants requires an intensive multidisciplinary approach but yields excellent short- and long-term survival rates that are no different from those seen in older children or adults. Living donors should be used whenever possible. Patients with a successful transplantation experience improved growth and development, with excellent rehabilitation.
Full text
PDF




Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Arbus G. S., Hardy B. E., Balfe J. W., Churchill B. M., Steele B. T., Baumal R., Curtis R. N. Cadaveric renal transplants in children under 6 years of age. Kidney Int Suppl. 1983 Nov;15:S111–S115. [PubMed] [Google Scholar]
- Betts P. R., Magrath G. Growth pattern and dietary intake of children with chronic renal insufficiency. Br Med J. 1974 Apr 27;2(5912):189–193. doi: 10.1136/bmj.2.5912.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broyer M. Growth in children with renal insufficiency. Pediatr Clin North Am. 1982 Aug;29(4):991–1003. doi: 10.1016/s0031-3955(16)34224-9. [DOI] [PubMed] [Google Scholar]
- Cerilli G. J., Nelsen C., Dorfmann L. Renal homotransplantation in infants and children with the hemolytic-uremic syndrome. Surgery. 1972 Jan;71(1):66–71. [PubMed] [Google Scholar]
- Chavers B. M., Nevins T. E., Knaack M., Melvin T., Mauer S. M. Early acute tubular necrosis, late rejection in pediatric renal transplantation with donor-specific transfusions. Transplant Proc. 1987 Feb;19(1 Pt 2):1526–1527. [PubMed] [Google Scholar]
- Churchill B. M., Sheldon C. A., McLorie G. A., Arbus G. S. Factors influencing patient and graft survival in 300 cadaveric pediatric renal transplants. J Urol. 1988 Nov;140(5 Pt 2):1129–1133. doi: 10.1016/s0022-5347(17)41979-3. [DOI] [PubMed] [Google Scholar]
- DeShazo C. V., Simmons R. L., Bernstein D. M., DeShazo M. M., Wilmert J., Kjellstrand C. M., Najarian J. S. Results of renal transplantation in 100 children. Surgery. 1974 Sep;76(3):461–468. [PubMed] [Google Scholar]
- Ettenger R. B., Blifeld C., Prince H., Gradus D. B., Cho S., Sekiya N., Salusky I. B., Fine R. N. The pediatric nephrologist's dilemma: growth after renal transplantation and its interaction with age as a possible immunologic variable. J Pediatr. 1987 Dec;111(6 Pt 2):1022–1025. doi: 10.1016/s0022-3476(87)80049-5. [DOI] [PubMed] [Google Scholar]
- Ettenger R. B., Rosenthal J. T., Marik J., Salusky I. B., Kamil E., Malekzadeh M. H., Fine R. N. Successful cadaveric renal transplantation in infants and young children. Transplant Proc. 1989 Feb;21(1 Pt 2):1707–1708. [PubMed] [Google Scholar]
- Fine R. N. Renal transplantation of the infant and young child and the use of pediatric cadaver kidneys for transplantation in pediatric and adult recipients. Am J Kidney Dis. 1988 Jul;12(1):1–10. doi: 10.1016/s0272-6386(88)80064-7. [DOI] [PubMed] [Google Scholar]
- GEHAN E. A. A GENERALIZED WILCOXON TEST FOR COMPARING ARBITRARILY SINGLY-CENSORED SAMPLES. Biometrika. 1965 Jun;52:203–223. [PubMed] [Google Scholar]
- GOODWIN W. E., KAUFMAN J. J., MIMS M. M., TURNER R. D., GLASSOCK R., GOLDMAN R., MAXWELL M. M. Human renal transplantation. I. Clinical experiences with six cases of renal homotransplantation. J Urol. 1963 Jan;89:13–24. doi: 10.1016/S0022-5347(17)64491-4. [DOI] [PubMed] [Google Scholar]
- Ingelfinger J. R., Grupe W. E., Harmon W. E., Fernbach S. K., Levey R. H. Growth acceleration following renal transplantation in children less than 7 years of age. Pediatrics. 1981 Aug;68(2):255–259. [PubMed] [Google Scholar]
- Katz A., Kim Y., Scheinman J., Najarian J. S., Mauer S. M. Long-term outcome of kidney transplantation in children with oxalosis. Transplant Proc. 1989 Feb;21(1 Pt 2):2033–2035. [PubMed] [Google Scholar]
- Kleinknecht C., Broyer M., Gagnadoux M. F., Martihenneberg C., Dartois A. M., Kermanach C., Pouliquen M., Degoulet P., Usberti M., Roy M. P. Growth in children treated with long-term dialysis. A study of 76 patients. Adv Nephrol Necker Hosp. 1980;9:133–163. [PubMed] [Google Scholar]
- Kwun Y. A., Butt K. M., Kim K. H., Kountz S. L., Moel D. I. Successful renal transplantation in a 3-month-old infant. J Pediatr. 1978 Mar;92(3):426–429. doi: 10.1016/s0022-3476(78)80435-1. [DOI] [PubMed] [Google Scholar]
- Lawson R. K., Talwalkar Y. B., Musgrave J. E., Campbell R. A., Hodges C. V. Renal transplantation in pediatric patients. J Urol. 1975 Feb;113(2):225–229. doi: 10.1016/s0022-5347(17)59450-1. [DOI] [PubMed] [Google Scholar]
- Lum C. T., Fryd D. S., Polta T. A., Najarian J. S. Results of kidney transplantation in the young child. Transplantation. 1982 Oct;34(4):167–171. doi: 10.1097/00007890-198210000-00002. [DOI] [PubMed] [Google Scholar]
- MacDonell R. C., Jr, Johnson K., Richie R., Nylander W., McMahon Y., Niblack G., Green W., Morrissey J., Ynares C. Pediatric renal transplantation results are improved with triple drug therapy with cyclosporine, azathioprine, and prednisone. Transplant Proc. 1989 Feb;21(1 Pt 2):1701–1704. [PubMed] [Google Scholar]
- Mahan J. D., Mauer S. M., Sibley R. K., Vernier R. L. Congenital nephrotic syndrome: evolution of medical management and results of renal transplantation. J Pediatr. 1984 Oct;105(4):549–557. doi: 10.1016/s0022-3476(84)80418-7. [DOI] [PubMed] [Google Scholar]
- McGraw M. E., Haka-Ikse K. Neurologic-developmental sequelae of chronic renal failure in infancy. J Pediatr. 1985 Apr;106(4):579–583. doi: 10.1016/s0022-3476(85)80075-5. [DOI] [PubMed] [Google Scholar]
- Miller L. C., Lum C. T., Bock G. H., Simmons R. L., Najarian J. S., Mauer S. M. Transplantation of the adult kidney into the very small child. Technical considerations. Am J Surg. 1983 Feb;145(2):243–247. doi: 10.1016/0002-9610(83)90071-5. [DOI] [PubMed] [Google Scholar]
- Moel D. I., Butt K. M. Renal transplantation in children less than 2 years of age. J Pediatr. 1981 Oct;99(4):535–539. doi: 10.1016/s0022-3476(81)80249-1. [DOI] [PubMed] [Google Scholar]
- Najarian J. S., Simmons R. L., Tallent M. B., Kiellstrand C. M., Buselmeier T. J., Vernier R. L., Michael A. F. Renal transplantation in infants and children. Ann Surg. 1971 Oct;174(4):583–601. doi: 10.1097/00000658-197110000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Najarian J. S., So S. K., Simmons R. L., Fryd D. S., Nevins T. E., Ascher N. L., Sutherland D. E., Payne W. D., Chavers B. M., Mauer S. M. The outcome of 304 primary renal transplants in children (1968-1985). Ann Surg. 1986 Sep;204(3):246–258. doi: 10.1097/00000658-198609000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson K. B., Deutschberger J. Head size at one year as a predictor of four-year IQ. Dev Med Child Neurol. 1970 Aug;12(4):487–495. doi: 10.1111/j.1469-8749.1970.tb01944.x. [DOI] [PubMed] [Google Scholar]
- Polinsky M. S., Kaiser B. A., Stover J. B., Frankenfield M., Baluarte H. J. Neurologic development of children with severe chronic renal failure from infancy. Pediatr Nephrol. 1987 Apr;1(2):157–165. doi: 10.1007/BF00849288. [DOI] [PubMed] [Google Scholar]
- Prensky A. L. Time--a fourth dimension for encephalopathies. N Engl J Med. 1984 Jun 7;310(23):1527–1528. doi: 10.1056/NEJM198406073102310. [DOI] [PubMed] [Google Scholar]
- Reinhart J. B. The doctor's dilemma: whether or not to recommend continuous renal dialysis or renal homotransplantation for the child with end-stage renal disease. J Pediatr. 1970 Sep;77(3):505–507. doi: 10.1016/s0022-3476(70)80026-9. [DOI] [PubMed] [Google Scholar]
- Rizzoni G., Malekzadeh M. H., Pennisi A. J., Ettenger R. B., Uittenbogaart C. H., Fine R. N. Renal transplantation in children less than 5 years of age. Arch Dis Child. 1980 Jul;55(7):532–536. doi: 10.1136/adc.55.7.532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotundo A., Nevins T. E., Lipton M., Lockman L. A., Mauer S. M., Michael A. F. Progressive encephalopathy in children with chronic renal insufficiency in infancy. Kidney Int. 1982 Mar;21(3):486–491. doi: 10.1038/ki.1982.50. [DOI] [PubMed] [Google Scholar]
- Scheinman J. I., Najarian J. S., Mauer S. M. Successful strategies for renal transplantation in primary oxalosis. Kidney Int. 1984 May;25(5):804–811. doi: 10.1038/ki.1984.93. [DOI] [PubMed] [Google Scholar]
- So S. K., Najarian J. S., Nevins T. E., Fryd D. S., Knaak M., Chavers B., Mauer S. M., Simmons R. L. Low-dose cyclosporine therapy combined with standard immunosuppression in pediatric renal transplantation. J Pediatr. 1987 Dec;111(6 Pt 2):1017–1021. doi: 10.1016/s0022-3476(87)80048-3. [DOI] [PubMed] [Google Scholar]
- Sutherland D. E., Fryd D. S., So S. K., Bentley F. R., Ascher N. L., Simmons R. L., Najarian J. S. Long-term effect of splenectomy versus no splenectomy in renal transplant patients. Reanalysis of a randomized prospective study. Transplantation. 1984 Dec;38(6):619–624. doi: 10.1097/00007890-198412000-00015. [DOI] [PubMed] [Google Scholar]
- Wells T. G., Ulstrom R. A., Nevins T. E. Hypoglycemia in pediatric renal allograft recipients. J Pediatr. 1988 Dec;113(6):1002–1007. doi: 10.1016/s0022-3476(88)80571-7. [DOI] [PubMed] [Google Scholar]
- Winick M., Rosso P. Head circumference and cellular growth of the brain in normal and marasmic children. J Pediatr. 1969 May;74(5):774–778. doi: 10.1016/s0022-3476(69)80140-x. [DOI] [PubMed] [Google Scholar]


