Abstract
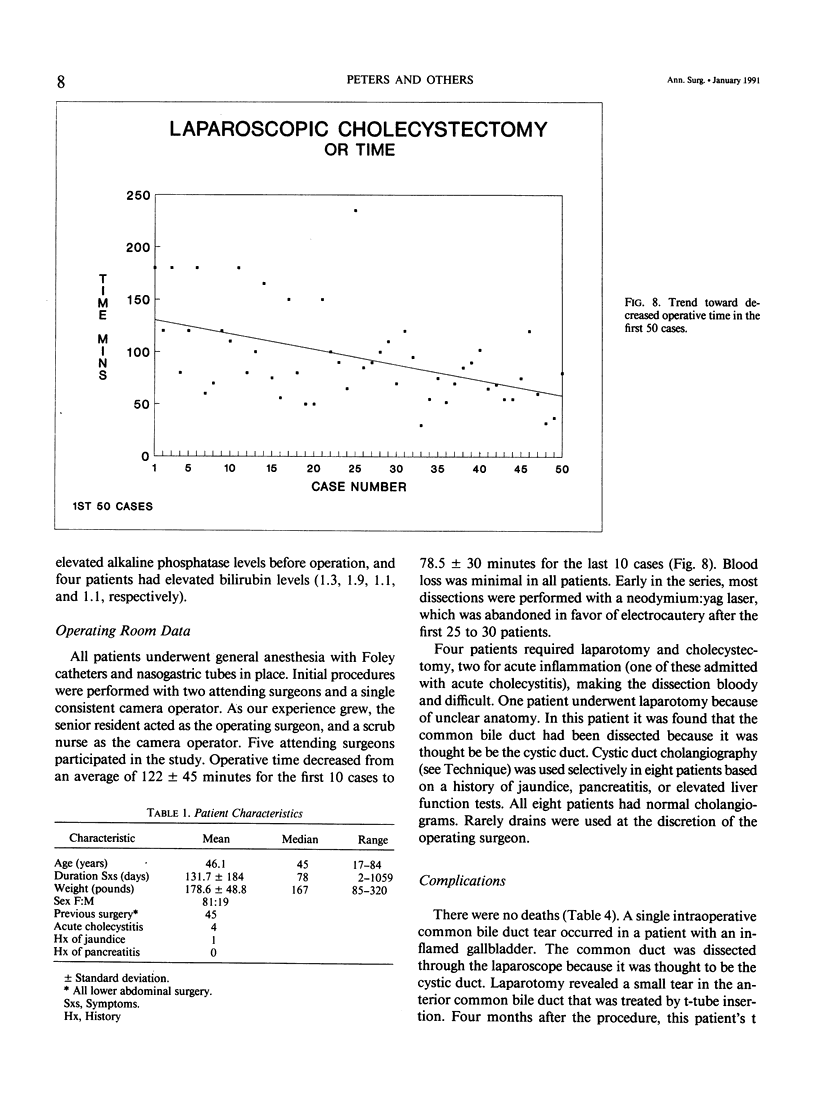
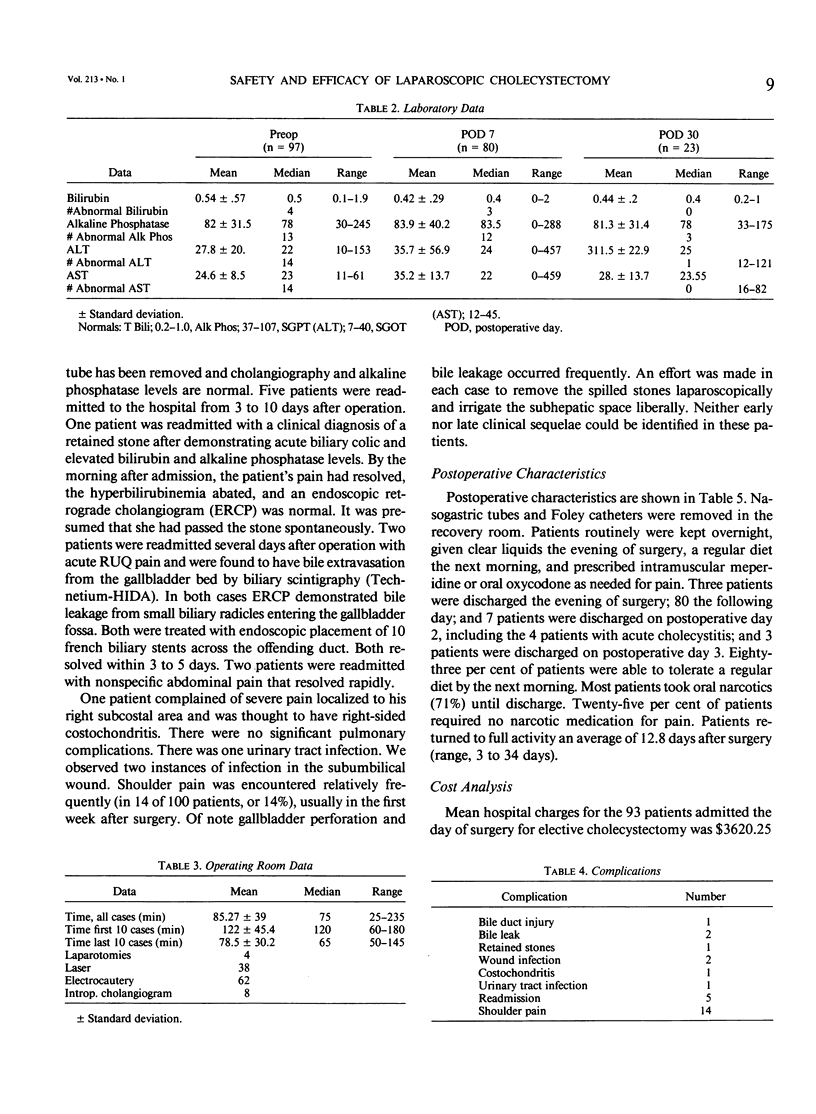
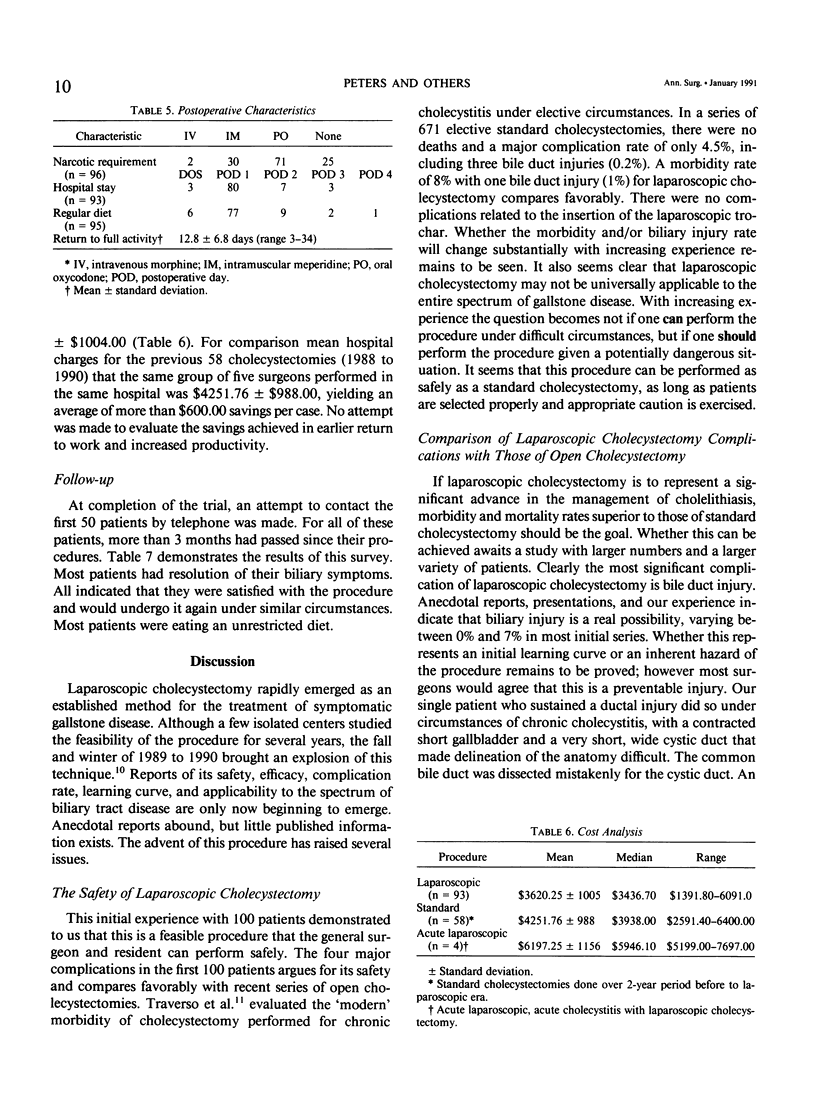
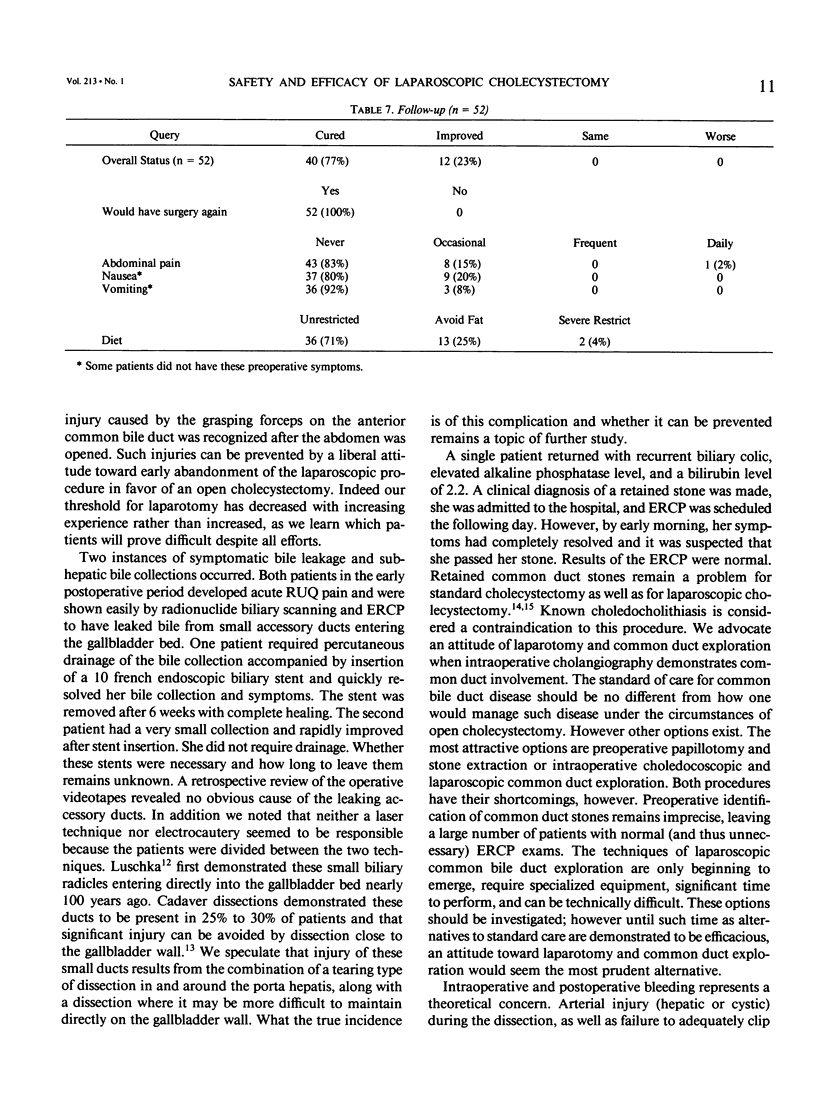
Laparoscopic cholecystectomy quickly emerged as an alternative to open cholecystectomy. However its safety, efficacy, and morbidity have yet to be fully evaluated. During the first 6 months of 1990, we performed 100 consecutive laparoscopic cholecystectomies with no deaths and a morbidity rate of 8% (8 of 100 patients; 4 major, 4 minor). There were 81 women and 19 men, with a mean age of 46.1 years (range, 17 to 84 years). All patients had a preoperative history consistent with symptomatic biliary tract disease, and most had proved gallstones by sonography. This included four patients with acute cholecystitis. Mean operating time improved significantly from month 1 to month 6 (122 +/- 45.4 minutes versus 78.5 +/- 30 minutes, respectively), indicating a rapid learning curve. Mean hospital stay was 27.6 hours, reflecting a policy of overnight stay. Postoperative narcotic requirements were limited to oral or no medications in more than 70% of patients. A regular diet was tolerated by 83% of the patients by the morning following the procedure. Median time of return to full activity was 12.8 +/- 6.8 days after operation. In addition analysis of the hospital costs of these 100 cases demonstrates a modest cost advantage over standard open cholecystectomy (n = 58) (mean, $3620.25 +/- $1005.00 versus $4251.76 +/- $988.00). There was one minor bile duct injury requiring laparotomy and t-tube insertion, two postoperative bile collections, and one clinical diagnosis of a retained stone that passed spontaneously. Four patients required conversion to open cholecystectomy because of technical difficulties with the dissection. Although there is a significant learning curve, laparoscopic cholecystectomy is a safe and effective procedure that can be performed with minimal risk. Laparoscopic cholecystectomy should be performed by surgeons who are trained in biliary surgery and knowledgeable in biliary anatomy, and, as with all operations, it should be performed with meticulous attention to technique.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Beal J. M. Historical perspective of gallstone disease. Surg Gynecol Obstet. 1984 Feb;158(2):181–189. [PubMed] [Google Scholar]
- Burhenne H. J., Stoller J. L. Minicholecystostomy and radiologic stone extraction in high-risk cholelithiasis patients. Preliminary experience. Am J Surg. 1985 May;149(5):632–635. doi: 10.1016/s0002-9610(85)80144-6. [DOI] [PubMed] [Google Scholar]
- Cuschieri A., Berci G., McSherry C. K. Laparoscopic cholecystectomy. Am J Surg. 1990 Mar;159(3):273–273. doi: 10.1016/s0002-9610(05)81214-0. [DOI] [PubMed] [Google Scholar]
- Dubois F., Icard P., Berthelot G., Levard H. Coelioscopic cholecystectomy. Preliminary report of 36 cases. Ann Surg. 1990 Jan;211(1):60–62. doi: 10.1097/00000658-199001000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilliland T. M., Traverso L. W. Modern standards for comparison of cholecystectomy with alternative treatments for symptomatic cholelithiasis with emphasis on long-term relief of symptoms. Surg Gynecol Obstet. 1990 Jan;170(1):39–44. [PubMed] [Google Scholar]
- Martin D. F., Tweedle D. E. Endoscopic management of common duct stones without cholecystectomy. Br J Surg. 1987 Mar;74(3):209–211. doi: 10.1002/bjs.1800740320. [DOI] [PubMed] [Google Scholar]
- McQuillan T., Manolas S. G., Hayman J. A., Kune G. A. Surgical significance of the bile duct of Luschka. Br J Surg. 1989 Jul;76(7):696–698. doi: 10.1002/bjs.1800760715. [DOI] [PubMed] [Google Scholar]
- McSherry C. K., Glenn F. The incidence and causes of death following surgery for nonmalignant biliary tract disease. Ann Surg. 1980 Mar;191(3):271–275. doi: 10.1097/00000658-198003000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pitt H. A., McFadden D. W., Gadacz T. R. Agents for gallstone dissolution. Am J Surg. 1987 Feb;153(2):233–246. doi: 10.1016/0002-9610(87)90822-1. [DOI] [PubMed] [Google Scholar]
- Reddick E. J., Olsen D. O. Laparoscopic laser cholecystectomy. A comparison with mini-lap cholecystectomy. Surg Endosc. 1989;3(3):131–133. doi: 10.1007/BF00591357. [DOI] [PubMed] [Google Scholar]
- Rogers A. L., Farha G. J., Beamer R. L., Chang F. C. Incidence and associated mortality of retained common bile duct stones. Am J Surg. 1985 Dec;150(6):690–693. doi: 10.1016/0002-9610(85)90410-6. [DOI] [PubMed] [Google Scholar]
- Sackmann M., Delius M., Sauerbruch T., Holl J., Weber W., Ippisch E., Hagelauer U., Wess O., Hepp W., Brendel W. Shock-wave lithotripsy of gallbladder stones. The first 175 patients. N Engl J Med. 1988 Feb 18;318(7):393–397. doi: 10.1056/NEJM198802183180701. [DOI] [PubMed] [Google Scholar]
- Thistle J. L., May G. R., Bender C. E., Williams H. J., LeRoy A. J., Nelson P. E., Peine C. J., Petersen B. T., McCullough J. E. Dissolution of cholesterol gallbladder stones by methyl tert-butyl ether administered by percutaneous transhepatic catheter. N Engl J Med. 1989 Mar 9;320(10):633–639. doi: 10.1056/NEJM198903093201004. [DOI] [PubMed] [Google Scholar]