Abstract
A chimeric yellow fever (YF) virus/Japanese encephalitis (JE) virus vaccine (ChimeriVax-JE) was constructed by insertion of the prM-E genes from the attenuated JE virus SA14-14-2 vaccine strain into a full-length cDNA clone of YF 17D virus. Passage in fetal rhesus lung (FRhL) cells led to the emergence of a small-plaque virus containing a single Met→Lys amino acid mutation at E279, reverting this residue from the SA14-14-2 to the wild-type amino acid. A similar virus was also constructed by site-directed mutagenesis (J. Arroyo, F. Guirakhoo, S. Fenner, Z.-X. Zhang, T. P. Monath, and T. J. Chambers, J. Virol. 75:934-942, 2001). The E279 mutation is located in a beta-sheet in the hinge region of the E protein that is responsible for a pH-dependent conformational change during virus penetration from the endosome into the cytoplasm of the infected cell. In independent transfection-passage studies with FRhL or Vero cells, mutations appeared most frequently in hinge 4 (bounded by amino acids E266 to E284), reflecting genomic instability in this functionally important region. The E279 reversion caused a significant increase in neurovirulence as determined by the 50% lethal dose and survival distribution in suckling mice and by histopathology in rhesus monkeys. Based on sensitivity and comparability of results with those for monkeys, the suckling mouse is an appropriate host for safety testing of flavivirus vaccine candidates for neurotropism. After intracerebral inoculation, the E279 Lys virus was restricted with respect to extraneural replication in monkeys, as viremia and antibody levels (markers of viscerotropism) were significantly reduced compared to those for the E279 Met virus. These results are consistent with the observation that empirically derived vaccines developed by mouse brain passage of dengue and YF viruses have increased neurovirulence for mice but reduced viscerotropism for humans.
The study of chimeric viruses has afforded new insights into the molecular basis of virulence and new prospects for vaccine development. For example, molecular clones of positive-strand alphaviruses (29, 39) and flaviviruses (4, 7, 13, 15) have been modified by insertion of structural genes encoding the viral envelope and determinants involved in neutralization, cell attachment, fusion, and internalization. The replication of these chimeric viruses is controlled in part by nonstructural proteins and the noncoding termini expressed by the parental strain, while the structural proteins from the donor genes afford specific immunity. The biological characteristics of chimeric viruses are determined by both the donor and recipient virus genes. By comparing constructs with nucleotide sequence differences across the donor genes, it is possible to dissect out the functional roles of individual amino acid residues in virulence and attenuation.
Using a chimeric yellow fever (YF) virus that incorporated the prM-E genes from an attenuated strain (SA14-14-2) of Japanese encephalitis (JE) virus, a detailed examination of the roles of 10 amino acid mutations that distinguished the attenuated JE virus from virulent, wild-type JE Nakayama virus was made (3). The virulence factors were defined by reverting each mutation singly or as clusters to the wild-type sequence and determining the effects on neurovirulence for young adult mice inoculated by the intracerebral (i.c.) route with 104 PFU. All of the single-site revertant viruses remained highly attenuated, and reversions at three or four residues were required to restore a neurovirulent phenotype. Only one single-site revertant (E279 Met→Lys) showed any evidence of a change in virulence, with one of eight animals succumbing after i.c. inoculation. The revertant was sequenced across prM-E only, so a mutation elsewhere in the genome could have influenced the virulence phenotype.
In order to explore further the functional role of the E279 determinant, we compared chimeric YF/JE viruses that differed at this amino acid residue for their ability to cause encephalitis in suckling mice and monkeys. i.c. inoculation of monkeys is routinely used as a test for safety of flavivirus and other live vaccines, and quantitative pathological examination of brain and spinal cord tissue provides a sensitive method for distinguishing strains of the same virus with subtle differences in neurovirulence (19). Suckling mice provide a more sensitive model than older animals, since susceptibility to neurotropic flaviviruses is age dependent (28). The results confirmed that the single Met→Lys amino acid mutation at E279 conferred an increase in neurovirulence for these animals. This mutation is located in the hinge region of the E protein, which is responsible for a pH-dependent conformational change during virus penetration from the endosome into the cytoplasm of the infected cell (31). Importantly, the suckling mouse was shown to predict the virulence profile in rhesus monkeys. Based on the detection of a change in neurovirulence conferred by a point mutation, we propose that the suckling mouse is an appropriate host for safety testing of flavivirus vaccine candidates for neurotropism.
While enhancing neurovirulence, the E279 mutation appeared to have the opposite effect on viscerotropism, as measured by decreased viremia and antibody response in monkeys, which are accepted markers of this viral trait (38).
MATERIALS AND METHODS
Viruses.
Development of the ChimeriVax-JE vaccine began by cloning a cDNA copy of the entire 11-kb genome of YF 17D virus (7). To accomplish this, YF 17D virus genomic sequences were propagated in two plasmids, which carry the YF virus sequences from nucleotide (nt) 1 to 2276 and 8279 to 10861 (plasmid YF5"3"IV), and from nt 1373 to 8704 (plasmid YFM5.2). Full-length cDNA templates were generated by ligation of appropriate restriction fragments derived from these plasmids. YF virus sequences within the YF5"3"IV and YFM5.2 plasmids were replaced by the corresponding JE (SA14-14-2) prM-E sequences, resulting in the generation of YF5"3"IV/JE (prM-E") and YFM5.2/JE (E"-E) plasmids. These plasmids were digested sequentially with restriction endonucleases NheI and BspEI. Appropriate fragments were ligated with T4 DNA ligase, cDNA was digested with XhoI enzyme to allow transcription, and RNA was produced from an Sp6 promoter. Transfection of diploid fetal rhesus lung (FRhL) cells with full-length RNA was performed by electroporation. Supernatant containing virus was harvested when cytopathic effect was observed (generally at day 3), clarified by low-speed centrifugation, and sterile filtered with a 0.22-μm-pore-size filter. Fetal bovine serum (50% [vol/vol] final concentration) was added as a stabilizer. The virus was titrated by plaque assay in Vero cells, as previously described (27). The chimeric virus was sequentially passed in FRhL or Vero cells (Vero-PM; Aventis Pasteur, Marcy l'Étoile, France) at a multiplicity of infection of approximately 0.001.
Commercial yellow fever 17D vaccine (YF-VAX) was obtained from Aventis Pasteur (formerly Pasteur-Mérieux-Connaught), Swiftwater, Pa.
Site-directed mutagenesis.
Virus containing a single-site Met→Lys reversion at residue E279 was generated by oligonucleotide-directed mutagenesis as described previously (3). Briefly, a plasmid (pBS/JE SA14-14-2) containing the JE SA14-14-2 E gene region from nt 1108 to 2472 (7) was used as the template for site-directed mutagenesis. Mutagenesis was performed using the Transformer site-directed mutagenesis kit (Clontech, Palo Alto, Calif.) and oligonucleotide primers synthesized at Life Technologies (Grand Island, N.Y.). Plasmids were sequenced across the E region to verify that the only change was the engineered mutation. A region encompassing the E279 mutation was then subcloned from the pBS/JE plasmid into pYFM5.2/JE SA14-14-2 (7) using the NheI and EheI (KasI) restriction sites. Assembly of full-length DNA and SP6 transcription were performed as described above; however, RNA transfection of Vero cells was performed using Lipofectin (Gibco/BRL).
Sequencing.
RNA was isolated from infected monolayers by use of Trizol (Life Technologies). Reverse transcription was performed with Superscript II reverse transcriptase and a long-reverse-transcription protocol (Life Technologies), followed by RNase H treatment (Promega) and long-PCR (XL PCR; Perkin-Elmer/ABI). Reverse transcription, PCR, and sequencing primers were designed the using YF virus strain 17D sequence (GenBank accession number K02749) and the JE virus strain SA14-14-2 sequence (GenBank accession number D90195) as references. PCR products were gel purified (Qiaquick gel extraction kit from Qiagen) and sequenced using the Dye-Terminator dRhodamine sequencing reaction mix (Perkin-Elmer/ABI). Sequencing reactions were analyzed on a model 310 Genetic Analyzer (Perkin-Elmer/ABI), and DNA sequences were evaluated using Sequencher 3.0 (GeneCodes) software.
Plaque assays and neutralization tests.
Plaque assays were performed in six-well plates of monolayer cultures of Vero cells. After adsorption of virus for 1 h at 37°C, the cells were overlaid with agarose in nutrient medium. On day 4, a second overlay containing 3% neutral red was added. Serum dilution, plaque reduction neutralization tests were performed as previously described (27).
Weaned-mouse model.
Groups of 8 to 10 female 4-week-old ICR mice (Taconic Farms, Inc. Germantown, N.Y.) were inoculated i.c. with 30 μl of chimeric YF/JE SA14-14-2 (ChimeriVax-JE) constructs with or without the E279 mutation. An equal number of mice were inoculated with YF-VAX or diluent. Mice were monitored for illness and death for 21 days.
Suckling mouse model.
Pregnant female ICR mice (Taconic Farms) were observed through parturition in order to obtain litters of suckling mice of an exact age. Suckling mice from multiple litters born within a 48-h interval were pooled and randomly redistributed to mothers in groups of up to 12 mice. Litters were inoculated i.c. with 20 μl of serial 10-fold dilutions of virus and monitored for signs of illness and death for 21 days. The virus inocula were back titrated. Fifty percent lethal doses (LD50s) were calculated by the method of Reed and Muench (30). Univariate survival distributions were plotted and compared by the log rank test. The effect of the E279 reversion was examined in a regression model analyzing mortality by virus dose. The data from the two virus strains were examined using a probit analysis for each virus to check the assumption of equal slopes. The combined data were then analyzed using a parallel-line bioassay probit model in SAS PROC LOGISTIC. The estimates and their covariances were output to a data set, which was merged with the original data. The potency (virulence) ratio estimate and the 95% fiducial limits for the potency ratio were then derived using the formulae in reference 9.
Monkey model.
The monkey neurovirulence test was performed as described by Levenbook et al. (19) and prescribed by World Health Organization (WHO) regulations for safety testing of YF 17D seed viruses (38). This test has previously been applied to the evaluation of ChimeriVax-JE vaccines, and results of tests on FRhL3 virus were described (26, 27). In a previous publication, we showed that the test is applicable to testing both YF 17D and ChimeriVax-JE viruses with respect to the structural localization of neuronal and inflammatory lesions (26). Tests were performed at Sierra Biomedical Inc. (Sparks, Nev.) according to the U.S. Food and Drug Administration Good Laboratory Practice regulations (21 CFR, part 58). On day 1, 10 rhesus monkeys (5 male and 5 female) weighing 3.0 to 6.5 kg received a single inoculation of 0.25 ml of undiluted ChimeriVax-JE virus with or without the E279 Met→Lys mutation or YF-VAX into the frontal lobe of the brain. Monkeys were evaluated daily for clinical signs and scored as 0 (no signs), 1 (rough coat, not eating), 2 (high-pitched voice, inactive, slow moving), 3 (shaky movements, tremors, incoordination, limb weakness), or 4 (inability to stand, limb paralysis, death). The clinical score for each monkey is the mean of the animal's daily scores, and the clinical score for the treatment group is the arithmetic mean of the individual clinical scores. Viremia levels were measured by plaque assay in Vero cells using sera collected on days 2 to 10. On day 31, animals were euthanized and perfused with isotonic saline-5% acetic acid followed by neutral-buffered 10% formalin, and necropsies were performed. Brains and spinal cords were fixed, sectioned, and stained with gallocyanin. Neurovirulence was assessed by the presence and severity of lesions in various anatomical formations of the central nervous system. Severity was scored within each tissue block using the scale specified by WHO (38): grade 1, minimal (one to three small focal inflammatory infiltrates; a few neurons may be changed or lost); grade 2, moderate (more extensive focal inflammatory infiltrates; neuronal changes or loss affects not more than one-third of neurons); grade 3, severe (neuronal changes or loss affects 33 to 90% of neurons; moderate focal or diffuse inflammatory changes are present); and grade 4, overwhelming (more than 90% of neurons are changed or lost, with variable but frequently severe inflammatory infiltration).
Structures involved in the pathological process most often and with greatest severity were designated target areas, while those structures discriminating between wild-type JE virus and ChimeriVax-JE were designated discriminator areas. The substantia nigra constituted the target area, and the caudate nucleus, globus pallidus, putamen, anterior/medial thalamic nucleus, lateral thalamic nucleus, and spinal cord (cervical and lumbar enlargements) constituted discriminator areas (26), as previously shown for YF 17D virus (19). All neuropathological evaluations were done by a single experienced investigator (I.L.) who was blinded to the treatment code. Separate scores for target area, discriminator areas, and target plus discriminator areas were determined for each monkey, and test groups were compared with respect to average scores. Other areas of the brain stem (nuclei of the midbrain in addition to substantia nigra, pons, medulla, and cerebellum) and the leptomeninges were also examined. Statistical comparisons of mean neuropathological scores (for the target area, discriminator areas, and target plus discriminator areas) were performed with the two-tailed Student t test. In addition to neuropathological examination, the liver, spleen, adrenal glands, heart, and kidneys were examined for pathological changes by light microscopy.
Genome stability.
To ascertain the genetic stability of the YF/JE chimeric virus and to search for hot spots in the vaccine genome that are susceptible to mutation, multiple experiments were performed in which RNA was used to transfect cells and the progeny virus was serially passaged in vitro, with partial or complete genomic sequencing performed at low and high passage levels. Passage series were performed starting with the transfection step in FRhL or Vero-PM cells. Serial passage of the virus was performed at a low multiplicity of infection in cell cultures grown in T25 or T75 flasks. At selected passage levels, duplicate samples of viral genomic RNA were extracted, reverse transcribed, and amplified by PCR, and the prM-E region or full genomic sequence was determined.
RESULTS
Generation of single-site mutant viruses by empirical passage.
The chimeric YF/JE SA14-14-2 (ChimeriVax-JE) virus recovered from transfected FRhL cells (FRhL1) was passed sequentially in fluid cultures of these cells at a multiplicity of infection of approximately 0.001. As described below, at passage 4 we noted a change in plaque morphology, which was subsequently shown to be associated with a T→G transversion at nucleotide 1818 resulting in an amino acid change (Met→Lys) at position 279 of the E protein.
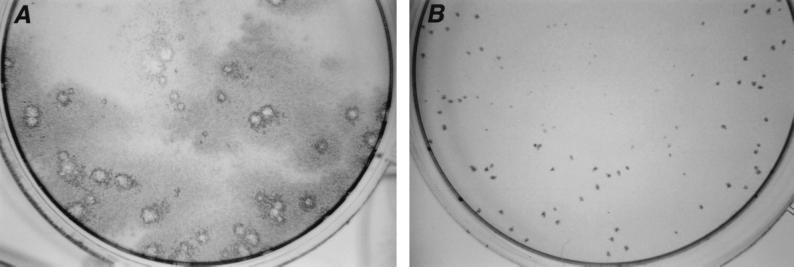
Plaques were characterized at each passage level and classified into three categories based on their sizes measured on day 6 (large [L], >≈1.0 mm; medium, ≈0.5 to 1 mm; and small [S], <≈0.5 mm); the plaque size distribution was determined by counting 100 plaques. FRhL3 (third-passage) virus contained 80 to 94% L and 6 to 20% S plaques. At FRhL5 (fifth passage), a change in plaque size was detected, with the emergence of S plaques comprising >85% of the total plaque population (Fig. 1). The FRhL4 virus was intermediate, with 40% L and 60% S plaques. Full genomic sequencing of the FRhL5 virus demonstrated a single mutation at E279. The full genome consensus sequence of the FRhL5 chimera, with careful inspection for codon heterogeneity, confirmed that this was the only detectable mutation present in the virus. The full genome consensus sequence of the FRhL3 virus revealed no detectable mutations compared to the parental YF/JE SA14-14-2 chimeric virus (4) (Table 1).
FIG. 1.
Plaque size variation. (A) ChimeriVax-JE FRhL3 (large plaque); (B) ChimeriVax-JE FRhL5 (small plaque). Plaques were stained using rabbit anti-JE virus antiserum followed by anti-rabbit immunoglobulin G-horseradish peroxidase.
TABLE 1.
Comparison of the amino acid differences in the E proteins of ChimeriVax-JE FRhL3 and ChimeriVax-JE FRhL5 viruses with published sequences of JE SA14-14-2 vaccine, wild-type JE parental SA14, and JE Nakayama virusesa
| Virus (reference) | Mutation at:
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| E107 | E138 | E176 | E177 | E227 | E244 | E264 | E279 | E315 | E439 | |
| ChimeriVax-JE FRhL3 E279 Met | F | K | V | A | S | G | H | M | V | R |
| ChimeriVax-JE FRhL5 E279 Lys | F | K | V | A | S | G | H | K | V | R |
| JE SA14-14-2 PDKb (29b) | F | K | V | T | S | G | Q | M | V | R |
| JE SA14-14-2 PHKc (29a) | F | K | V | A | S | G | H | M | V | R |
| JE SA14 (1, 29b) | L | E | I | T | S | G | Q | K | A | K |
| JE Nakayama (22a) | L | E | I | T | P | E | Q | K | A | K |
The ChimeriVax-JE FRhL3 and FRhL5 viruses were sequenced across their entire genomes, and the mutation at E279 was the only difference found.
PDK, primary dog kidney cells.
PHK, primary hamster kidney cells.
Ten large, medium, and small plaques were picked from FRhL3, FRhL4, and FRhL5 and amplified by passage in fluid cultures of FRhL cells. After amplification, the supernatant fluid was plaqued on Vero cells. Attempts to isolate the S plaque phenotype from FRhL3 failed, and all isolated L or S plaques produced a majority of L plaques after one round of amplification in FRhL cells. At the next passage (FRhL4), where 60% of plaques were S, it was possible to isolate these plaques by amplification in FRhL cells. At FRhL5, the majority of plaques (85 to 99%) were S, and amplification of both L and S individual plaques resulted in a majority of S plaques. Sequencing the prM-E genes of the S and L plaque phenotypes from FRhL3 revealed sequences identical to those of the parent SA14-14-2 genes used for construction of ChimeriVax-JE, whereas S plaques isolated from either FRhL4 or FRhL5 virus revealed the mutation (Met→Lys) at E279.
Animal protocols.
All studies involving mice and nonhuman primates were conducted in accordance with the U.S. Department of Agriculture Animal Welfare Act (9 CFR, parts 1 to 3) as described in the Guide for Care and Use of Laboratory Animals. Protocols were approved by the Animal Care and Use committees of the institutions undertaking the work.
Virulence for weaned mice.
Ten female ICR mice 4 weeks of age were inoculated i.c. with approximately 3.0 log10 PFU of FRhL3, FRhL4, or FRhL5 virus in separate experiments; in each study 10 mice received an equivalent dose (approximately 3.3 log10 PFU) of commercial YF vaccine (YF-VAX; Aventis Pasteur). None of the mice inoculated with chimeric viruses showed signs of illness or died, whereas 70 to 100% of control mice inoculated with YF-VAX developed paralysis or died. In another experiment, eight mice were inoculated i.c. with FRhL5 (3.1 log10 PFU) or the YF/JE single-site E279 revertant virus (4.0 log10 PFU) and nine mice received YF-VAX (2.3 log10 PFU). None of the mice inoculated with the chimeric constructs became ill, whereas six of nine (67%) of mice inoculated with YF-VAX died.
Virulence for suckling mice.
Two separate experiments were performed in which YF/JE SA14-14-2 chimeric viruses with and without the E279 mutation were inoculated i.c. at graded doses into suckling mice (Table 2). YF-VAX was used as the reference control in these experiments. LD50s and average survival times were determined for each virus.
TABLE 2.
Neurovirulence for suckling mice of ChimeriVax-JE viruses with and without a mutation at E279 and of YF 17D vaccine
| Expt | Mouse age (days) | Virus, passage, and E279 amino acid | i.c. dose (log10 PFU) | Mortality (%) | Avg survival time (days) | LD50 (log10 PFU) |
|---|---|---|---|---|---|---|
| 1 | 8.6 | YF-VAX | 1.15 | 10/10 (100) | 8.4 | 0.11 |
| 0.15 | 5/10 (50) | 10 | ||||
| −0.85 | 1/10 (10) | 14 | ||||
| ChimeriVax-JE, FRhL3, E279 Met | 2.60 | 1/10 (10) | 15 | >2.6 | ||
| 1.6 | 1/10 (10) | 13 | ||||
| 0.6 | 0/10 (0) | NAa | ||||
| −0.45 | 0/10 (0) | NA | ||||
| ChimeriVax-JE, FRhL5, E279 Lys | 3.0 | 10/10 (100) | 10.3 | 1.64 | ||
| 2.0 | 8/10 (80) | 11.25 | ||||
| 1.0 | 2/10 (20) | 14.5 | ||||
| 0 | 2/10 (20) | 16 | ||||
| 2 | 4 | YF-VAX | 0.95 | 11/11 (100) | 8.4 | −0.3 |
| −0.05 | 9/11 (82) | 8.8 | ||||
| −1.05 | 2/12 (17) | 10 | ||||
| ChimeriVax-JE, FRhL3, E279 Met | 2.69 | 7/12 (58) | 10.6 | 2.5 | ||
| 1.69 | 4/12 (33) | 11.5 | ||||
| 0.69 | 0/12 (0) | NA | ||||
| ChimeriVax-JE, FRhL5, E279 Lys | 2.88 | 10/12 (83) | 9.3 | 1.45 | ||
| 1.88 | 11/12 (92) | 10.3 | ||||
| 0.88 | 4/12 (33) | 12.2 | ||||
| −0.11 | 2/12 (17) | 14 | ||||
| −1.11 | 0/12 (0) | NA | ||||
| YF/JE279 site-specific revertant, E279 Lys | 3.55 | 12/12 (100) | 9.4 | 1.15 | ||
| 2.55 | 11/12 (92) | 10.1 | ||||
| 1.55 | 11/12 (92) | 10.2 | ||||
| 0.55 | 3/12 (25) | 10.7 | ||||
| −0.44 | 2/12 (17) | 14 |
In the first experiment, using mice 8.6 days old, FRhL5 virus containing the single-site reversion (Met→Lys) at E279 was neurovirulent, with a log10 LD50 of 1.64, whereas the FRhL3 virus lacking this mutation was nearly avirulent, with only 1 of 10 mice in the highest-dose groups dying (Table 2). At the highest dose (approximately 3 log10 PFU), the average survival time with the FRhL5 virus was shorter (10.3 days) than that with the FRhL3 virus (15 days).
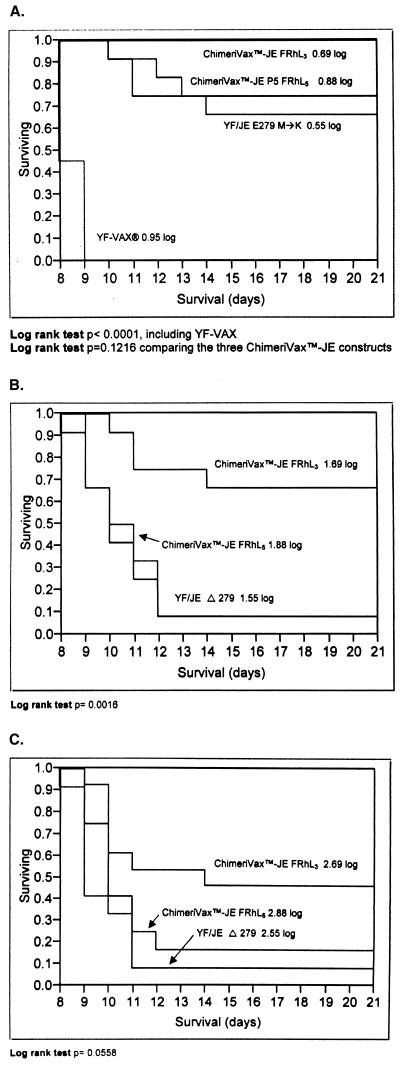
A second experiment was subsequently performed to verify statistically that a single-site mutation in the E gene is detectable by the neurovirulence test in suckling mice. In this experiment outbred mice 4 days of age were inoculated i.c. with graded doses of ChimeriVax-JE FRhL3 (no mutation), ChimeriVax-JE FRhL5 (E279 Met→Lys), or a YF/JE chimera in which a single mutation at E279 (Met→Lys) was introduced by site-directed mutagenesis (3). The LD50s of the two viruses containing the E279 mutation were >10-fold lower than that of the FRhL3 construct without the mutation (Table 2), indicating that the E279 Met→Lys mutation increased the neurovirulence of the chimeric virus. There were statistically significant differences between the viruses in the survival distributions (Fig. 2). At the lowest dose (≈0.7 log10 PFU), the YF/JE chimeric viruses were significantly less virulent than YF-VAX (log rank P < 0.0001). The viruses with the E279 Met→Lys mutation had similar survival curves that differed from that of the FRhL3 virus (no mutation), but the difference did not reach statistical significance (log rank P = 0.1216). However, at higher doses (≈1.7 and ≈2.7 log10 PFU), the survival distributions of the E279 mutant viruses were significantly different from that of FRhL3 virus.
FIG. 2.
Survival distributions for YF-VAX and ChimeriVax-JE constructs with and without a mutation at E279 (M→K). Four-day-old suckling mice were inoculated by the i.c. route with approximately 0.7 log10 PFU (A), approximately 1.7 log10 PFU (B), and approximately 2.7 log10 PFU (C).
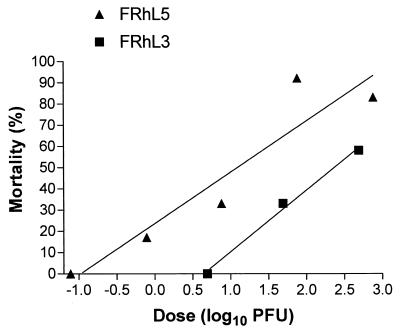
Analysis of the mortality ratio by virus dose revealed similar slopes and parallel regression lines (Fig. 3). The FRhL5 virus was 18.52 times more potent (virulent) than FRhL3 (95% fiducial limits of 3.65 and 124.44; P < 0.0001).
FIG. 3.
Regression analysis of mortality versus virus dose, showing similar slopes and parallel lines for viruses with (FRhL5) and without (FRhL3) the Met→Lys reversion, allowing statistical comparison. The FRhL5 virus was 18.52 times more potent (virulent) than FRhL3 (P < 0.0001).
Monkey neurovirulence test.
None of the 20 monkeys inoculated with ChimeriVax-JE FRhL3 or FRhL5 viruses developed signs of encephalitis, whereas 4 of 10 monkeys inoculated with YF-VAX developed grade 3 signs (tremors) between days 15 and 29, which resolved within 6 days of onset. Mean and maximum mean clinical scores were significantly higher in the YF-VAX group than in the two ChimeriVax-JE groups There was no difference in clinical score between groups receiving ChimeriVax-JE viruses with and without the E279 mutation (Table 3).
TABLE 3.
Neuropathological evaluation of monkeys inoculated i.c. with ChimeriVax-JE FRhL3 FRhL5 or YF 17D (YF-VAX) and necropsied on day 30 postinoculation
| Test virus | Monkey | Sex | Dosea (log10 PFU/ 0.25 ml) | Clinical scoreb maximum score/ mean daily score | Individual and group mean histopathological score
|
||
|---|---|---|---|---|---|---|---|
| Target areac | Discriminactor areasd | Target plus discrim- inator areas | |||||
| YF-VAX (Connaught lot no. 0986400) | RT702M | M | 4.05 | 1/0 | 2.00 | 0.51 | 1.26 |
| RT758M | M | 4.28 | 1/0 | 0.25 | 0.01 | 0.13 | |
| RT653M | M | 4.07 | 1/0 | 2.00 | 0.39 | 1.20 | |
| RT776M | M | 4.25 | 3/1 | 2.00 | 1.29 | 1.65 | |
| RT621M | M | 4.34 | 3/2 | 1.00 | 0.46 | 0.73 | |
| RAH80F | F | 4.14 | 3/1 | 1.50 | 0.71 | 1.10 | |
| RAL02F | F | 4.13 | 1/1 | 2.00 | 0.80 | 1.40 | |
| RT698F | F | 3.78 | 3/1 | 1.50 | 0.64 | 1.07 | |
| RAI12F | F | 4.11 | 1/1 | 2.00 | 1.45 | 1.73 | |
| RP942F | F | 4.05 | 1/0 | 2.00 | 0.81 | 1.41 | |
| Mean | 4.12 | 1 | 1.63 | 0.71 | 1.17 | ||
| SD | 0.16 | 1 | 0.59 | 0.42 | 0.47 | ||
| ChimeriVax-JE, FRhL3 (lot no. 1031299A) | RT452M | M | 3.55 | 1/0 | 0.50 | 0.08 | 0.29 |
| RR257M | M | 3.52 | 1/0 | 1.00 | 0.14 | 0.57 | |
| RT834M | M | 3.71 | 1/0 | 0.50 | 0.38 | 0.44 | |
| RT620M | M | 3.71 | 1/0 | 1.00 | 0.14 | 0.57 | |
| RT288M | M | 3.76 | 1/0 | 0.50 | 0.19 | 0.35 | |
| RAJ98F | F | 3.79 | 1/1 | 0.00 | 0.11 | 0.05 | |
| RAR08F | F | 3.52 | 1/0 | 0.00 | 0.13 | 0.07 | |
| RV481F | F | 3.52 | 1/0 | 0.00 | 0.06 | 0.03 | |
| RT841F | F | 3.71 | 1/0 | 0.50 | 0.05 | 0.28 | |
| RT392F | F | 3.76 | 1/0 | 0.50 | 0.07 | 0.29 | |
| Mean | 3.66 | 0 | 0.45 | 0.14 | 0.29 | ||
| SD | 0.11 | 0 | 0.37 | 0.10 | 0.20 | ||
| P value (t teste) vs YF-VAX | 0.037/0.025 | 0.00008 | 0.00191 | 0.00014 | |||
| ChimeriVax JE, FRhL5 (lot no. 99B01) | RT628M | M | 4.20 | 1/0 | 0.50 | 0.57 | 0.54 |
| RT678M | M | 4.19 | 1/0 | 1.00 | 0.12 | 0.60 | |
| RT581M | M | 4.17 | 1/0 | 1.00 | 0.46 | 0.73 | |
| RR726M | M | 4.32 | 1/0 | 1.00 | 0.66 | 0.83 | |
| RR725M | M | NDf | 1/0 | 1.00 | 0.33 | 0.67 | |
| RAJ55F | F | 4.27 | 0/0 | 1.00 | 0.14 | 0.57 | |
| RT769F | F | 4.44 | 1/0 | 1.00 | 0.58 | 0.79 | |
| RAK22F | F | 4.24 | 1/0 | 0.00 | 0.12 | 0.06 | |
| RT207F | F | 4.49 | 1/1 | 1.00 | 0.22 | 0.61 | |
| RT490F | F | 4.34 | 1/0 | 0.00 | 0.04 | 0.02 | |
| Mean | 4.30 | 0 | 0.75 | 0.32 | 0.54 | ||
| SD | 0.11 | 0 | 0.42 | 0.23 | 0.28 | ||
| P value (t test) vs YF-VAX | 0.024/0.025 | 0.00154 | 0.02436 | 0.00248 | |||
| P value (t test) vs ChimeriVax-JE, FRhL3 | 0.343/1.00 | 0.10942 | 0.03223 | 0.03656 | |||
Back titration.
Clinical score: 0, no signs; 1, rough coat, not eating; 2, high-pitched voice, inactive, slow moving; 3, tremor, incoordination, shaky movements, limb weakness; 4, inability to stand, paralysis, moribund, or dead. The maximum score on any day and the mean score over the 30-day observation period are shown.
Substantia nigra.
Corpus striatum and thalamus, right and left side (caudate nucleus, globus pallidus, putamen, anterior/medial thalamic nucleus, lateral thalamic nucleus, and cervical and lumbar enlargements of the spinal cord [six levels]).
Student's t test (two sided, heteroscedastic), comparing YF-VAX and ChimeriVax-JE viruses.
ND, not done.
There were no differences in weight changes between treatment groups during the experiment. Pathological examination revealed no alterations of liver, spleen, kidney, heart, or adrenal glands attributable to the viruses and no differences between treatment groups.
Histopathological examination of the brain and spinal cord revealed significantly higher lesion scores for monkeys inoculated with YF-VAX than for those inoculated with ChimeriVax-JE viruses FRhL3 and FRhL5 (Table 3). The combined target plus discriminator score (mean ± standard deviation) for YF-VAX was 1.17 ± 0.47. The scores for the ChimeriVax-JE FRhL3 (E279 Met) and FRhL5 (E279 Lys) were 0.29 ± 0.20 (P = 0.00014 versus YF-VAX) and 0.54 ± 0.28 (P = 0.00248 versus YF-VAX), respectively.
The discriminator area score and combined target plus discriminator area score for ChimeriVax-JE FRhL5 containing the Met→Lys reversion at E279 were significantly higher than the corresponding scores for ChimeriVax-JE FRhL3 (Table 3).
The main symptom in monkeys inoculated with YF-VAX was tremor, which may reflect lesions of the cerebellum, thalamic nuclei, or globus pallidus. No clear histological lesions were found in the cerebellar cortex, nucleus dentatus, or other cerebellar nuclei, whereas inflammatory lesions were present in the thalamic nuclei and globus pallidus in all positive monkeys.
Interestingly, there was an inverse relationship between neurovirulence and viscerotropism of the E279 revertant as reflected by viremia. The WHO monkey neurovirulence test includes quantitation of viremia as a measure of viscerotropism (38). This is rational based on observations that i.c. inoculation results in immediate seeding of extraneural tissues (35). In our study, 9 (90%) of 10 monkeys inoculated with YF-VAX and 8 (80%) of 10 monkeys inoculated with ChimeriVax-JE FRhL3 became viremic after i.c. inoculation. The level of viremia tended to be higher in the YF-VAX group than in the ChimeriVax-JE FRhL3 group, reaching significance on day 4. In contrast, only 2 (20%) of the animals given FRhL5 virus (E279 Met→Lys) had detectable, low-level viremias (Table 4), and the mean viremia was significantly lower than that with FRhL3 virus on days 3 and 4 (and nearly significant on day 5). Thus, the FRhL5 revertant virus displayed increased neurovirulence but decreased viscerotropism compared to the FRhL3 virus. Sera from monkeys inoculated with ChimeriVax-JE FRhL3 and FRhL5 were examined for the presence of plaque size variants. Only L plaques were observed in sera from monkeys inoculated with the FRhL3 virus, whereas the virus in blood of monkeys inoculated with FRhL5 had the appropriate S plaque morphology.
TABLE 4.
Viremia in rhesus monkeys inoculated i.c. with YF-VAX or ChimeriVax JE FRhL3 and FRhL5 virusesa
| Test virus | Animal | Serum virus titer (log10 PFU/mL) on day:
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | ||
| YF-VAX control | RT702M | —b | — | 1.6 | 3.0 | — | — | — | — | — |
| RAH80F | — | — | — | 3.3 | 2.5 | — | — | — | — | |
| RT758M | — | — | 2.1 | 3.2 | 2.8 | — | — | — | — | |
| RAL02F | — | — | — | 1.3 | — | — | — | — | — | |
| RT653M | — | — | — | 2.7 | — | — | — | — | — | |
| RT698F | — | 1.0 | 2.3 | 3.7 | 2.5 | — | 1.0 | — | — | |
| RT776M | — | — | — | — | — | — | — | — | — | |
| RAI12F | — | — | — | 2.0 | 2.5 | 2.5 | 2.0 | — | — | |
| RT621M | — | 1.0 | 2.0 | 3.3 | 2.0 | — | — | — | — | |
| c> | ||||||||||
| RP942F | — | 1.0 | 2.6 | 3.6 | 2.0 | — | — | — | — | |
| Meanc | 0.8 | 1.4 | 2.7 | 1.7 | 0.9 | 0.9 | ||||
| SD | 0.1 | 0.8 | 1.0 | 0.9 | 0.6 | 0.4 | ||||
| ChimeriVax-JE FRhL3, E279 Met | RAJ98F | — | — | 1.9 | 1.3 | — | — | — | — | — |
| RT452M | — | 1.3 | 2.1 | 1.6 | — | — | — | — | — | |
| RAR08F | — | — | 1.3 | 2.2 | 2.2 | 1.8 | — | — | — | |
| RR257M | — | — | 1.9 | 2.2 | 1.8 | — | — | — | — | |
| RV481F | — | — | 2.1 | 1.8 | 1.5 | — | — | — | — | |
| RT834M | — | — | 2.5 | 1.3 | — | — | — | — | — | |
| RT841F | — | — | 2.4 | 1.7 | — | — | — | — | — | |
| RT620M | — | — | 1.6 | 1.0 | — | — | — | — | — | |
| RT392F | — | — | — | — | — | — | — | — | — | |
| RT288M | — | — | — | — | — | — | — | — | — | |
| Mean | 0.8 | 1.7 | 1.5 | 1.0 | 0.8 | |||||
| SD | 0.2 | 0.6 | 0.5 | 0.6 | 0.3 | |||||
| P valued | 0.696 | 0.386 | 0.003 | 0.065 | 0.745 | |||||
| ChimeriVax-JE FRhL5 E279 Lys | RT628M | — | — | — | — | — | — | — | — | — |
| RAJ55F | — | — | — | — | — | — | — | — | — | |
| RT678M | — | — | — | — | — | — | — | — | — | |
| RT769F | — | — | — | 2.0 | — | — | — | — | — | |
| RT581M | — | — | — | — | — | — | — | — | — | |
| RAK22F | — | — | — | — | — | — | 1.8 | — | — | |
| RR726M | — | — | — | — | — | — | — | — | — | |
| RT207F | — | — | — | — | — | — | — | — | — | |
| RR725M | — | — | — | — | — | — | — | — | — | |
| RT490F | — | — | — | — | — | — | — | — | — | |
| Mean | 0.7 | 0.7 | 0.8 | 0.7 | 0.7 | 0.8 | ||||
| SD | 0.0 | 0.0 | 0.4 | 0.0 | 0.0 | 0.4 | ||||
| P valuee | 0.331 | <0.000 | 0.010 | 0.076 | 1.0 | 1.0 | ||||
For the dose inoculated, see Table 3. In most tests undiluted serum was tested, with the cutoff being 1.0 log10 PFU/ml, in some cases, undiluted serum was toxic to cells, and serum diluted 1:2 or 1:5 was used (cutoff, 1.3 or 1.7 log10 PFU/ml).
—, no detectable viremia.
For the purpose of calculating mean titers and standard deviations, 0.7 was used in place of<1.0, 1.0 was used in place of <1.3, and 1.4 was used in place of <1.7.
Comparison with YF-VAX by two-tailed t test.
Comparison with ChimeriVax-JE FRhL3 by two-tailed t test.
Immunogenicity.
All monkeys in all three groups developed homologous neutralizing antibodies virus at 31 days postinoculation to YF virus (YF-VAX group) or ChimeriVax-JE (ChimeriVax groups), with the exception of one animal (FRhL5, RAK22F) which was not tested due to sample loss. However, the geometric mean antibody titer was significantly higher in the monkeys inoculated with FRhL3 (501) than in those inoculated with FRhL5 (169) (P = 0.0386 [t test]).
Genome stability.
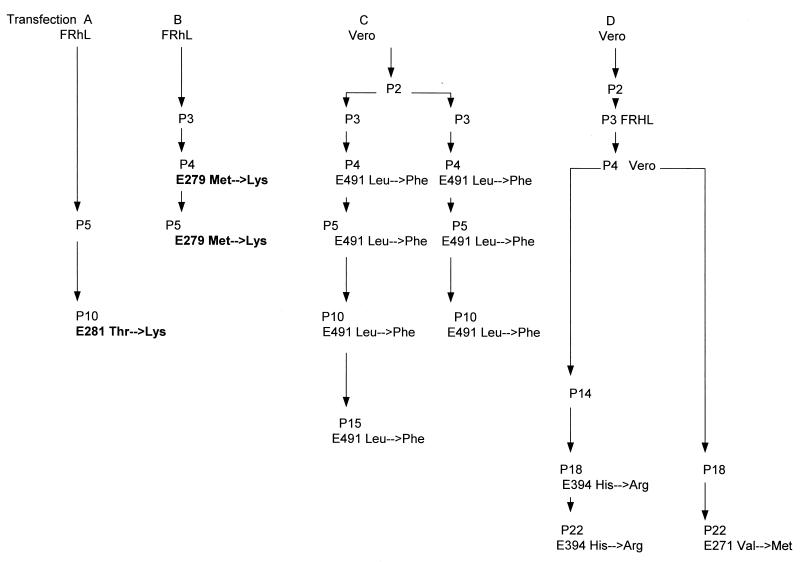
Two separate transfections of ChimeriVaxJE RNA were performed in each of two cell strains, FRhL and Vero, and progeny viruses were passed, as shown in Fig. 4. The FRhL passage series B resulted in appearance of the E279 reversion at FRhL4 as described above. Interestingly, a separate passage series (passage A) in FRhL cells also resulted in the appearance of a mutation (Thr→Lys) in an adjacent residue at E281, and one of the passage series in Vero cells resulted in a Val→Lys mutation at E271. Other mutations selected in Vero cells were in domain III or within the transmembrane domain. All viruses containing mutations shown in Fig. 2 were evaluated in the adult mouse neurovirulence test and were found to be avirulent (data not shown).
FIG. 4.
Independent RNA transfection and passage series of ChimeriVax-JE virus in FRhL and Vero cells, showing emergence of mutations in the prM-E genes by passage level.
DISCUSSION
The use of a chimeric virus as a vaccine requires a careful evaluation of its genetic stability and safety profile, since the virus may change on passage in vitro or in the host and mutations may affect cell tropism and virulence.
We noted the appearance of a point mutation (reversion from the attenuated SA14-14-2 amino acid [Met] to the wild-type residue [Lys]) at E279 in the ChimeriVax-JE virus. The mutation was associated with a change in plaque size after only four passages in FRhL cells. This mutation was not noted in a previous analysis of the immunogenicity of FRhL virus at passage 5 in monkeys (in that study, the transfection A series was used [Fig. 3]) (27). Attempts to isolate the S plaque phenotype from FRhL3 failed, and all isolated L or S plaques produced a majority of L plaques after one round of amplification in FRhL cells. These data suggest that the S plaque phenotype observed in FRhL5 was probably not present in FRhL3 or was present at too low a concentration to be recovered by plaque isolation. All S plaques isolated from either FRhL4 or FRhL5 virus revealed the Met→Lys mutation at E279. These results suggested that the S plaque E279 mutant virus observed at FRhL4 and FRhL5 either was present in the RNA transcripts used for transfection or emerged by mutation posttransfection and was quickly selected in FRhL cells after a few passages. The absence of the E279 mutation in progeny of other transfections and passage series (Fig. 4) supports the latter hypothesis. The S plaque phenotype and E279 reversion were associated with changes in virulence, as described below.
The influence of a point mutation on virulence was most clearly demonstrated by i.c. inoculation of suckling mice with graded doses of virus. Both the age of the mice and the virus dose influenced the outcome measures, i.e., mortality ratio and survival time. Mice exhibit increased resistance to direct i.c. inoculation of flaviviruses with advancing age (28), although the mechanism has not been defined. By 9 days of age, suckling mice were nearly fully resistant to i.c. inoculation of ChimeriVax-JE FRhL3 without the E279 mutation, whereas the FRhL5 E279 Met→Lys mutant was lethal, with an LD50 of 1.64 (Table 2). In more susceptible mice at 4 days of age, in which both FRhL3 and FRhL5 viruses were lethal, differences between virus strains were subtler. The most valuable discriminator was the Kaplan-Meier survival distribution (Fig. 2) at a virus dose that was not so high as to obscure differences in survival (in this case, a dose of ≈1.7 log10 PFU gave the strongest P value). The sensitivity of the suckling mouse to reveal subtle differences in neurovirulence suggests the use of this model as an appropriate safety test for detecting changes in the neurovirulence phenotypes of seed viruses and vaccine lots of live vaccines such as ChimeriVax-JE, -dengue (12), and -West Nile (2, 25). The fact that a virus with a reversion affecting a virulence determinant is still significantly less neurovirulent than commercial YF 17D vaccine (Table 2; Fig. 2) is reassuring, and thus YF 17D virus should be included as a reference control in the suckling mouse safety test of chimeric vaccine candidates.
Identification of the increased neurovirulence associated with a mutation at E279 in suckling mice was further evaluated in the rhesus monkey model. The monkey safety test was established in the 1940s for detecting changes in the neurotropism, viscerotropism, and immunogenicity of YF 17D vaccine. This concern arose because uncontrolled passage of the vaccine virus during manufacturing led to lots that caused encephalitis in humans or that were poorly immunogenic (10). The monkey safety test was subsequently refined and standardized, as described in Materials and Methods (19, 38). The test has proven to be useful in discriminating subtle differences in neurovirulence during recent attempts to prepare cell culture-derived YF 17D vaccine (21), and it has been qualified as an appropriate method for safety testing of chimeric vaccines constructed from the YF 17D infectious clone (26, 27). The sensitivity of the monkey to detect differences in virus virulence was also suggested by a study of YF 17D virus recovered from a fatal case of postvaccination encephalitis (17). This virus differed from YF 17D vaccine at three residues (E155, E303, and NS4b72) and was found to have increased neurovirulence for mice and for a limited number of monkeys. The E303 Thr→Lys mutation in domain III was suspected to be the mediator of increased neurovirulence.
Our study is the first to determine the changes in monkey neurovirulence clearly associated with a single mutation and defined by a full neurovirulence test in groups of 10 monkeys as prescribed by WHO (38). Histopathological examination of discriminator areas of the brain (caudate nucleus, globus pallidus, putamen, anterior/medial thalamic nucleus, lateral thalamic nucleus, and spinal cord cervical and lumbar enlargements) revealed an increase in neurovirulence associated with the Met→Lys reversion at E279, the only genetic change present in the FRhL5 virus. In agreement with results for adult and suckling mice (Table 2), both FRhL3 and FRhL5 viruses were significantly less neurovirulent for monkeys than YF 17D vaccine. This implies that single-site reversions would probably not adversely affect the safety of the vaccine in humans. However, even a slight increase in neurovirulence was troublesome, and based on this observation and the fact that the chimeric virus was altered at one of the SA14-14-2-specific sites associated with attenuation, we elected not to pursue the candidate seed grown in FRhL cells for development.
The concordance between the neurovirulence profiles in suckling mice and rhesus monkeys suggests that the former could be substituted as an appropriate safety test for neurovirulence of flavivirus vaccines, thereby avoiding the high cost and long time requirements of the monkey test and the destruction of large numbers of nonhuman primates. Previous studies also demonstrated that the neurovirulence of flaviviruses for mice accurately predicts neurovirulence for monkeys (24), although the areas of the brain affected in the two species differ, with the hippocampus being the principal target area in the mouse and the substantia nigra being the principal target area in the monkey. Substitution of mice for monkeys in neurovirulence tests has been accomplished in the case of oral poliovirus vaccine and should be an objective for flavivirus vaccines. We are currently assessing the comparative neurovirulences of chimeric YF viruses incorporating the prM-E genes of dengue type 2 and West Nile viruses in both mice and monkeys in order to provide a firm basis for safety tests with mice.
Recent reports of disease resembling wild-type YF in humans caused by YF 17D vaccine (22, 36) illustrate that the vaccine has residual, heretofore unrecognized, viscerotropic properties. Those reports did not implicate genetic changes of the vaccine lots used but rather suggested a rare genetic and/or acquired susceptibility of individual hosts to YF 17D virus. Quantitative measurement of viremia in monkeys inoculated i.c. is incorporated in the WHO safety test as a measure of viscerotropism (38). i.c. inoculation is believed to result in intravenous deposition of virus and infection of extraneural tissues responsible for viremia (35). It is uncertain, however, whether the viremia marker would detect a change in the ability of a vaccine lot to cause hepatic disease in humans. A study in which YF 17D virus was inoculated directly into the livers of rhesus monkeys failed to show evidence of pathology on liver biopsies or elevation of serum transaminase levels (R. Marchevsky, personal communication). Recently, a rodent (hamster) model of viscerotropic YF has been described (34). This host is significantly less susceptible than monkeys and cannot be used to discriminate between vaccine viruses with different virulence properties, although it may be a useful system for defining the molecular basis of viscerotropism of wild-type YF. In vitro systems employing human hepatoma cells (9) may prove useful once these molecular determinants are known.
One of the most intriguing observations in the present study was the significantly lower viremia in monkeys inoculated i.c. with ChimeriVax-JE FRhL5 (Table 4). This finding suggests that the E279 Met→Lys mutation decreased viscerotropism (extraneural infection), presumably by reducing fusion activity in a cell type-specific fashion. Since neither YF-VAX, ChimeriVax-JE FRhL3, nor ChimeriVax-JE FRhL5 caused lesions in monkey liver or other organs examined and did not result in hepatic dysfunction detectable by liver function tests, the only measure of viscerotropism was viremia. The cell types and tissues supporting the low level of replication of YF 17D and ChimeriVax-JE viruses in monkeys have not been defined. Monkeys inoculated with FRhL5 virus also had significantly lower neutralizing antibody responses, consistent with lower viremia and extraneural replication. Further studies to determine whether other reversions in the hinge region also have the inverse effects on neuro- and viscerotropism in monkeys are indicated.
Comparison of the sequences of the prM-E genes of the virulent JE Nakayama virus and the attenuated vaccine strain SA14-14-2 identified up to 10 amino acid mutations in SA14-14-2 that could potentially explain the virulence difference between chimeric constructs (3, 7,13). The functional roles of these individual mutations were partially dissected by Arroyo et al. (3), who implicated residues E107, E138, and E176/177 as well as E279 in neurovirulence for mice. The E279 reversion from Met in the attenuated (SA14-14-2) sequence to Lys (wild type) was the only one that appeared to slightly increase virulence as a single-site change when tested in adult mice, which are a relatively insensitive host for detection of neurovirulence. When the E279 reversion was added to a cluster of two other single-site reversions, the virulence of the triple revertant for adult mice increased (3).
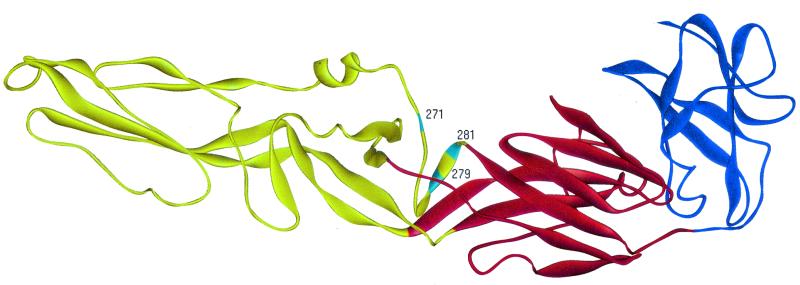
Analysis of the three-dimensional structures of the ectodomains of the E proteins of tick-borne encephalitis (TBE) and JE viruses have shown them to be nearly identical, despite a sequence homology of only 40% (18, 31). Localization within the three-dimensional structures of mutant proteins that affect flavivirus virulence has led to the identification of a cluster of molecular determinants in the base of domain II and at the interface between domains I and II, representing the putative hinge region. E279 is found within this region (Fig. 5). The hinge region plays an important role in early events during infection of the cell. It undergoes a conformational change under low-pH conditions, resulting in conversion of the E protein from a dimeric to a trimeric form and outward projection of domain II, bringing its tip into juxtaposition with the endosomal membrane (1, 32). The result is fusion of the viral envelope and the endosomal membrane and subsequent virus release into the cytoplasm. Mutations in the hinge region, such as those at E138 and E279 in JE virus, may alter the ability of the E protein to undergo the required conformational alteration at acidic pH (5, 6, 8, 11, 14, 23, 33). Due to the dipolar nature of amino acids and significant differences in pK values, amino acid substitutions may result in marked differences in charge and hydrophilicity. In the case of the E279 mutation, the change from Met to a more positively charged amino acid (Lys) appears to increase virulence of the virus, presumably by altering electrostatic protein-protein interactions, locking the E protein in trimer conformation, and enhancing fusogenic activity under low-pH conditions. Lys is the predominant amino acid at E279 in wild-type viruses within the JE virus antigenic complex (3).
FIG. 5.
Three-dimensional model of the JE virus envelope glycoprotein ectodomain showing locations of mutations in the hinge region occurring with adaptation in FRhL or Vero cells (see Fig. 3). The sequence of the JE virus envelope glycoprotein (strain JaOArS982) (32) was aligned to one of the TBE virus structural template (31) as an input for automated homology modeling building by the method of SegMod (segment match modeling) using LOOK software (Molecular Application Group, Palo Alto, Calif.). The three domains are colored red (domain I), yellow (domain II), and blue (domain III).
Site-directed mutagenesis of the closely juxtaposed E277 residue in the hinge region of Murray Valley encephalitis virus resulted in attenuation of the virus (16). In this case, replacement of the wild-type hydrophilic Ser residue with the hydrophobic amino acid Ile resulted in a marked reduction in neuroinvasiveness. The E277 Ser→Ile mutation also diminished replication in Vero cells and mouse brain and abolished the ability of the virus to agglutinate red blood cells at low pH, a surrogate for fusion of the viral envelope with the endosomal membrane. The region of the E protein between amino acids 266 and 284 has been designated hinge 4 (16). In addition to E277 and E279, a mutation at E270 resulted in attenuation of JE viral neurotropism (6, 8).
It is well known that flaviviruses undergo selective mutational pressure during replication in different host systems. For example, serial passage in mouse brain typically results in an increase in neurovirulence for mice (9, 5, 35). In the case of dengue type 2 virus, the increase in neurovirulence appears to be due to a mutation from an acidic to a basic residue (Glu→Lys) at E126 within the hinge region (5). We evaluated the influence of passage level on ChimeriVax-JE virus mutagenesis in two cell substrates, FRhL and Vero cells. Both cell strains appeared to promote instability in the hinge region. In three of the six independent passage series shown in Fig. 4, mutations appeared within hinge 4 (at E271, E279, and E281) (Fig. 5). This hinge region appears to be particularly susceptible to adaptive mutation during passage, suggesting a basis for the appearance in nature of virus strains that vary in virulence. Two of the mutations (at positions E279 and E281) are within the beta-strand of the secondary structure, and all three mutations increase the net positive charge of the protein by introducing the Lys amino acid. The Met→Lys reversion at E279 also results in a shortening of the beta-strand secondary structure. Adaptation of TBE virus by serial passage in BHK-21 cells also resulted in mutations which increased the net positive charge of external determinants in the E protein, increased binding affinity for BHK-21 cells, and altered plaque phenotype but reduced neuroinvasiveness of the virus in adult mice (20).
The E271 and E281 hinge region mutations in ChimeriVax-JE that resulted from passage in FRhL or Vero monkey cells did not result in a change in neurovirulence when assessed in adult mice; however, subtle changes detectable only in suckling mice or monkeys were not evaluated. Subsequent studies will determine whether these mutations result in phenotypic changes similar to those described for E279 and whether a consistent inverse relationship exists between increased neurovirulence and decreased replication in extraneural tissues. The latter is particularly important because it may explain the empirical observation that adaptation by serial passage of dengue and YF viruses in mouse brain resulted in enhanced neurovirulence but attenuation of viscerotropism (5, 35). This was the approach taken in the development of live, attenuated dengue virus vaccines and the French neurotropic YF (FNV) vaccine. The phenotypic changes in neuroadapted dengue type 2 virus and FNV are associated with mutations in the hinge region. In the case of dengue type 2 vaccine a single mutation in this region (E126 Glu→Lys) appeared to play a major role (5). Neuroadaptation of dengue type 1 virus resulted in a conservative mutation in hinge 3 (E196 Met→Val) (as well as mutations in domains III and the stem-anchor region) associated with attenuation in human hepatoma cells, a presumed marker of viscerotropism (9). In the case of FNV, however, where 35 amino acid substitutions separate wild-type and vaccine strains, the molecular basis of adaptation remains obscure (37).
Acknowledgments
We thank Rick Nichols, Chuck Miller, Penny Papasthakis, and Nancy Tobin for excellent technical assistance. W. Tad Archambault (VirtuStat Ltd., North Wales, Pa.) provided statistical expertise.
REFERENCES
- 1.Aihara, S., C. M. Rao, Y. X. Yu, T. Lee, K. Watanabe, T. Komiya, H. Sumiyoshi, H. Hashimoto, and A. Nomoto. 1991. Identification of mutations that occurred on the genome of Japanese encephalitis virus during the attenuation process. Virus Genes 5:95-109. [DOI] [PubMed] [Google Scholar]
- 1a.Allison, S. L., J. Shalich, K. Stiasny, C. W. Mandl, C. Kunz, and F. X. Heinz. 1995. Oligomeric rearrangement of tick-borne encephalitis virus envelope proteins induced by an acidic pH. J. Virol. 69:695-700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Arroyo, J., C. A. Miller, J. Catalan, and T. P. Monath. 2001. Yellow fever vector live-virus vaccines: West Nile vaccine development. Trends Mol. Med. 7:329-377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Arroyo, J., F. Guirakhoo, S. Fenner, Z.-X. Zhang, T. P. Monath, and T. J. Chambers. 2001. Molecular basis for attenuation of neurovirulence of a yellow fever/Japanese encephalitis (ChimeriVax-JE) viral vaccine. J. Virol. 75:934-942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bray, M., and C.-J. Lai. 1991. Construction of intertypic chimeric dengue viruses by substitution of structural protein genes. Proc. Natl. Acad. Sci. USA 88:10342-10346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bray, M., R. Men, I. Tokimatsu, and C.-J. Lai. 1998. Genetic determinants responsible for acquisition of dengue type 2 virus mouse neurovirulence. J. Virol. 72:1647-1651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cecilia, D., and E. A. Gould. 1991. Nucleotide changes responsible for loss of neuroinvasiveness in Japanese encephalitis virus neutralization-resistant mutants. Virology 181:70-77. [DOI] [PubMed] [Google Scholar]
- 7.Chambers, T. J., A. Nestorowicz, P. W. Mason, K. H. Eckels, and C. M. Rice. 1999. Yellow fever/Japanese encephalitis chimeric viruses: construction and biological properties. J. Virol. 73:3095-3101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen, L.-K., Y.-L. Lin, C.-L. Liao, C.-G. Lin, Y.-L. Huang, C.-T. Yeh, S.-C. Lai, J.-T. Jan, and C. Chin. 1996. Generation and characterization of organ-tropism mutants of Japanese encephalitis virus in vivo and in vitro. Virology 223:79-88. [DOI] [PubMed] [Google Scholar]
- 9.Duarte dos Santos, C. N., M.-P. Frenkiel, M.-P. Courageot, C. F. S. Rocha, M.-C. Vazielle-Falcoz, M. W. Wien, F. A. Rey, V. Deubel, and P. Després. 2000. Determinants in the envelope E protein and viral RNA helicase NS3 that influence the induction of apoptosis in response to infection with dengue type 1 virus. Virology 274:292-308. [DOI] [PubMed] [Google Scholar]
- 9a.Finney, D. J. 1971. Probit analysis, 3rd ed. Cambridge University Press, Cambridge, United Kingdom.
- 10.Fox, J. P., and H. A. Penna. 1943. Behavior of 17D yellow fever virus in rhesus monkeys. Relation to substrain, dose and neural or extraneural inoculation. Am. J. Hyg. 38:152-172. [Google Scholar]
- 11.Gualano, R. C., M. J. Pryor, M. R. Cauchi, P. J. Wright, and A. D. Davidson. 1998. Identification of a major determinant of mouse neurovirulence of dengue virus type 2 using stably cloned genomic-length cDNA. J. Gen. Virol. 79:437-446. [DOI] [PubMed] [Google Scholar]
- 12.Guirakhoo, F., J. Arroyo, K. V. Pugachev, C. Miller, Z.-X. Zhang, R. Weltzin, K. Georgakopoulos, J. Catalan, S. Ocran, K. Soike, M. Ratterree, and T. P. Monath. 2001. Construction, safety, and immunogenicity in nonhuman primates of a chimeric yellow fever-dengue tetravalent vaccine. J. Virol. 75:7290-7304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guirakhoo, F., Z. Zhang, T. J. Chambers, S. Delagrave, J. Arroyo, A. D. T. Barrett, and T. P. Monath. 1999. Immunogenicity, genetic stability and protective efficacy of a recombinant, chimeric yellow fever-Japanese encephalitis virus (Chimerivax™-JE) as a live, attenuated vaccine candidate against Japanese encephalitis. Virology 257:363-372. [DOI] [PubMed] [Google Scholar]
- 14.Hasegawa, H., M. Yoshida, T. Shiosaka, S. Fujita, and Y. Kobayashi. 1992. Mutations in the envelope protein of Japanese encephalitis virus affect entry into cultured cells and virulence in mice. Virology 191:158-165. [DOI] [PubMed] [Google Scholar]
- 15.Huang, C. Y.-H., S. Butrapet, D. J. Pierro, G.-J. Chang, A. R. Hunt, N. Bhamarapravati, D. J. Gubler, and R. M. Kinney. 2000. Chimeric dengue type 2 (vaccine strain PDK-53)/dengue type 1 virus as a potential candidate dengue type 1 virus vaccine. J. Virol. 74:3020-3028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hurrelbrink, R. J., and P. C. McMinn. 2001. Attenuation of Murray valley encephalitis virus by site-directed mutagenesis of the hinge and putative receptor-binding regions of the envelope protein. J. Virol. 75:7692-7702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jennings, A. D., C. A. Gibson, B. R. Miller, J. H. Matthews, C. J. Mitchell, J. T. Roehrig, D. J. Wood, F. Taffs, B. K. Sil, S. N. Whitby, J. E. Whitby, T. P. Monath, P. D. Minor, P. G. Sanders, and A. D. T. Barrett. 1994. Analysis of a yellow fever virus isolated from a fatal case of vaccine-associated human encephalitis. J. Infect. Dis. 169:512-518. [DOI] [PubMed] [Google Scholar]
- 18.Kolaskar, A. S., and U. Kulkarni-Kale. 1999. Prediction of three-dimensional structure and mapping of conformational epitopes of envelope glycoprotein of Japanese encephalitis virus. Virology 261:31-42. [DOI] [PubMed] [Google Scholar]
- 19.Levenbook, I. S., L. J. Pelleu, and B. L. Elisberg. 1987. The monkey safety test for neurovirulence of yellow fever vaccines: the utility of quantitative clinical evaluation and historical examination. J. Biol. Stand. 15:305-313. [DOI] [PubMed] [Google Scholar]
- 20.Mandl, C. W., H. Kroschewski, S. L. Allison, R. Kofler, H. Holzmann, T. Meixner, and F. X. Heinz. 2001. Adaptation of tick-borne encephalitis virus to BHK-21 cells results in the formation of multiple heparan sulfate binding sites in the envelope protein and attenuation in vivo. J. Virol. 75:5627-5637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marchevsky, R. S., J. Mariano, V. S. Ferreira, E. Almeida, M. J. Cerqueira, J. E. Pissurno, A. P. A. Travassos da Rosa, M. C. Simoes, C. N. D. Santos, I. I. Ferreira, I. R. Muylaert, G. E. Mann, C. M. Rice, and R. Galler. 1995. Phenotypic analysis of yellow fever virus derived from complementary DNA. Am. J. Trop. Med. Hyg. 52:70-80. [DOI] [PubMed] [Google Scholar]
- 22.Martin, M., T. F. Tsai, B. Cropp, G.-J. J Chang, D. A. Holmes, J. Tseng, W.-J. Shieh, S. R. Zaki, I. Al-Sanouri, A. F. Cutrona, G. Ray, L. H. Weld, and M. S. Cetron. 2001. Fever and multisystem organ failure associated with 17D-204 yellow fever vaccination: a report of four cases. Lancet 358:98-104. [DOI] [PubMed] [Google Scholar]
- 22a.McAda, P. C., P. W. Mason, C. S. Schmaljohn, J. M. Dalrymple, T. L. Mason, and M. J. Fournier. 1987. Partial nucleotide sequence of the Japanese encephalitis virus genome. Virology 158:348-360. [DOI] [PubMed] [Google Scholar]
- 23.McMinn, P. C., I. D. Marshall, and L. Dalgarno. 1995. Neurovirulence and neuroinvasiveness of Murray Valley encephalitis virus mutants selected by passage in a monkey kidney cell line. J. Gen. Virol 76:865-872. [DOI] [PubMed] [Google Scholar]
- 24.Monath, T. P., C. B. Cropp, G. S. Bowen, G. E. Kemp, C. J. Mitchell, and J. J. Gardner. 1980. Variation in virulence for mice and rhesus monkeys among St. Louis encephalitis virus strains of different origin. Am. J. Trop. Med. Hyg. 29:948-962. [DOI] [PubMed] [Google Scholar]
- 25.Monath, T. P., J. Arroyo, C. Miller, and F. Guirakhoo. 2001. West Nile vaccine. Curr. Drugs Infect. Dis. 1:37-50. [DOI] [PubMed] [Google Scholar]
- 26.Monath, T. P., K. Soike, I. Levenbook, Z.-X. Zhang, J. Arroyo, S. Delagrave, G. Myers, A. D. T. Barrett, R. E. Shope, T. J. Chambers, and F. Guirakhoo. 1999. Recombinant, chimaeric live, attenuated vaccine (ChimeriVaxTM) incorporating the envelope genes of Japanese encephalitis (SA14-14-2) virus and the capsid and nonstructural genes of yellow fever (17D) virus is safe, immunogenic and protective in non-human primates. Vaccine 17:1869-1882. [DOI] [PubMed] [Google Scholar]
- 27.Monath, T. P., K. Soike, Z.-X. Zhang, M. Ratterree, K. Draper, A. D. T. Barrett, R. Nichols, R. Weltzin, J. Arroyo, and F. Guirakhoo. 2000. Live, attenuated recombinant chimeric yellow fever-Japanese encephalitis vaccine: extended safety and immunogenicity studies in rhesus monkeys. J. Virol. 74:1742-1751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Monath, T. P. 1986. Pathobiology of the flaviviruses, p. 375-440. In S. Schlesinger and M. J. Schlesinger (ed.), The Togaviridae and Flaviviridae. Plenum, New York, N.Y.
- 29.Morris-Downes, M. M., B. J. Sheahan, M. N. Fleeton, P. Lilestrom, H. W. Reid, and G. J. Atkins. 2001. A recombinant Semliki Forest virus particle vaccine encoding the prME and NS1 proteins of louping ill virus is effective in a sheep challenge model. Vaccine 19:3877-3884. [DOI] [PubMed] [Google Scholar]
- 29a.Ni, H. N. J. Burns, G. J. Chang, M. J. Zhang, M. R. Wills, D. W. Trent, P. G. Sanders, and A. D. Barrett. 1994. Comparison of nucleotide and deduced amino acid sequence of the 5" non-coding region and structural protein genes of the wild-type Japanese encephalitis virus strain SA14 and its attenuated vaccine derivatives. J. Gen. Virol. 75:1505-1510. [DOI] [PubMed] [Google Scholar]
- 29b.Nitayaphan, S., J. A. Grant, G. J. Chang, and D. W. Trent. 1990. Nucleotide sequence of the virulent SA-14 strain of Japanese encephalitis virus and its attenuated vaccine derivative, SA-14-14-2. Virology 177:541-552. [DOI] [PubMed] [Google Scholar]
- 30.Reed, L. J., and H. Muench. 1938. A simple method of estimating fifty percent endpoints. Am. J. Hyg. 27:493-497. [Google Scholar]
- 31.Rey, F. A., F. X. Heinz, C. Mandl, C. Kunz, and S. C. Harrison. 1995. The envelope glycoprotein from tick-borne encephalitis virus at 2 A resolution. Nature 375:291-298. [DOI] [PubMed] [Google Scholar]
- 32.Stiasny, K., S. L. Allison, A. Marchler-Bauer, C. Kunz, and F. X. Heinz. 1996. Structural requirements for low-pH-induced rearrangements in the envelope glycoprotein of tick-borne encephalitis virus. J. Virol. 70:8142-8147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32a.Sumiyoshi, H. C. Mori, I. Fuke, K. Morita, S. Kuhara, J. Kondou, Y. Kikuchi, H. Nagamutu, and A. Igarashi. 1987. Complete nucleotide sequence of the Japanese encephalitis virus genome RNA. Virology 161:497-510. [DOI] [PubMed] [Google Scholar]
- 33.Sumiyoshi, H., G. H. Tignor, and R. E. Shope. 1995. Characterization of a highly attenuated Japanese encephalitis virus generated from molecularly cloned cDNA. J. Infect. Dis. 171:1144-1151. [DOI] [PubMed] [Google Scholar]
- 34.Tesh, R. B., H. Guzman, A. P. da Rosa, P. F. Vasconcelos, L. B. Dias, J. E. Bunnell, H. Zhang, and S. Y. Xiao. 2001. Experimental yellow fever virus infection in the Golden Hamster (Mesocricetus auratus). I. Virologic, biochemical, and immunologic studies. J. Infect. Dis. 183:1431-1436. [DOI] [PubMed] [Google Scholar]
- 35.Theiler, M. 1951. The virus, p. 46-136. In G. K. Strode (ed.), Yellow fever. McGraw Hill, New York, N.Y.
- 36.Vasconcelos, P. F. C., E. J. Luna, R. Galler, L. Silva, T. L. Coimbra, V. R. L. S. Barros, T. P. Monath, S. G. Rodrigues, C. Laval, Z. G. Cosata, M. F. G. Vilela, C. L. S. Santos, C. M. O. Papaiordanou, V. A. F. Alves, L. D. Andrade, H. K. Sato, E. S. T. Rosa, G. B. Froguas, E. Lacava, L. M. R. Almeida, A. C. R. Cruz, I. M. Rocco, R. T. M. Santos, and O. F. P. Oliva. 2001. Serious adverse events associated with yellow fever 17DD vaccine in Brazil: a report of two cases. Lancet 358:91-97. [DOI] [PubMed] [Google Scholar]
- 37.Wang, E., K. D. Ryman, A. D. Jennings, D. J. Wood, F. Taffs, P. D. Minor, P. G. Sanders, and A. D. T. Barrett. 1995. Comparison of the genomes of the wild-type French viscerotropic strain of yellow fever virus with its vaccine derivative French neurotropic vaccine. J. Gen. Virol. 76:2749-2755. [DOI] [PubMed] [Google Scholar]
- 38.World Health Organization. 1998. Requirements for yellow fever vaccine. WHO Tech. Rep. Ser. 872(Annex 2):31-68. [Google Scholar]
- 39.Xiong, C., R. Levis, P. Shen, S. Schlesinger, C. Rice, and H. V. Huang. 1989. Sindbis virus: an efficient, broad host-range vector for gene expression in animal cells. Science 243:1188-1191. [DOI] [PubMed] [Google Scholar]