Abstract
Summary Background Data:
The REMATCH trial evaluated the efficacy and safety of long-term left ventricular assist device (LVAD) support in stage D chronic end-stage heart failure patients. Compared with optimal medical management, LVAD implantation significantly improved the survival and quality of life of these terminally ill patients. To date, however, there have been no analyses of the cost related to the LVAD survival benefit. This paper addresses the cost of hospital resource use, and its predictors, for long-term LVAD patients.
Methods:
Detailed cost data were available for 52 of 68 REMATCH patients randomized to LVAD therapy. We combined the clinical dataset with Medicare data, standard billing forms (UB-92), and line item bills provided directly by clinical centers. Charges were converted to costs by using the Ratio-of-Cost-to-Charges for each major resource category.
Results:
The mean cost for the initial implant-related hospitalization was $210,187 ± 193,295. When implantation hospitalization costs are compared between hospital survivors and nonsurvivors, the mean costs increase from $159,271 ± 106,423 to $315,015 ± 278,713. Sepsis, pump housing infection, and perioperative bleeding are the major drivers of implantation cost, established by regression modeling. In the patients who survived the procedure (n = 35), bypass time, perioperative bleeding, and late bleeding were the drivers of cost. The average annual readmission cost per patient for the overall cohort was $105,326.
Conclusions:
The cost of long-term LVAD implantation is commensurate with other life-saving organ transplantation procedures like liver transplantation. As an evolving technology, there are a number of opportunities for improvement that will likely reduce costs in the future.
This paper addresses the hospital cost for long-term LVAD patients in the REMATCH trial. The mean cost for the initial implant-related hospitalization was $210,187 ± 193,295. When these costs are compared between hospital survivors and nonsurvivors, the mean costs increase from $159,271 ± 106,423 to $315,015 ± 278,713. Sepsis, pump housing infection, and perioperative bleeding are the major drivers of implantation cost. The average annual readmission cost per patient was $105,326. The cost of long-term LVAD implantation is similar to other life-saving procedures like liver transplantation. As an evolving technology, there are a number of opportunities for improvement that may reduce cost.
Since the inception of the National Institutes of Health (NIH) artificial heart program in 1964, significant public and private funds have been invested in the development of left ventricular assist devices (LVAD). In the mid 1990s, these devices received Food and Drug Administration (FDA) approval to support patients awaiting cardiac transplantation. Favorable results in this bridge to transplant population encouraged the design of the multicenter REMATCH (randomized evaluation of mechanical assistance for the treatment of congestive heart failure) trial to evaluate the efficacy and safety of long-term LVAD support in patients with chronic end-stage heart failure (stage D). Compared with optimal medical management (n = 61), LVAD implantation (n = 68) doubled the 1-year survival rate (from 25 to 51%) in this terminally ill population. Moreover, these patients had a significant improvement in quality of life and functional status compared with their medical counterparts.1 The editorial accompanying this publication concluded with the observation: “We now know that ventricular assist devices prolong life; we do not yet know for how long and at what cost.”2
This concern is critically important because congestive heart failure is a highly prevalent and growing disorder. Overall, 4.7 million Americans are affected, and CHF is a contributing factor in over 250,000 deaths per year. With over 900,000 hospitalizations in 2002, the annual cost of this disease is estimated to range from $10 to $40 billion.3 Given the magnitude of the end-stage heart failure population and the life-threatening nature of the disease, the clinical and policy-making communities will now need to confront challenging resource allocation decisions that require insight into detailed economic as well as clinical data. To date, there are no studies exploring the cost of LVAD as destination therapy. Published analyses only review the cost of bridge to transplant patients in single centers.4 This paper examines the cost of hospital resource use, and the predictors of such cost, for the LVAD patients enrolled in the multicenter REMATCH trial.
METHODS
Patient Population and Treatment Modalities
The trial targeted patients with chronic end-stage heart failure, in NYHA class IV for at least 60 of the previous 90 days before enrollment, despite adequate medical therapy. Detailed trial eligibility criteria are documented elsewhere.5
We were able to obtain detailed cost records for 52 out of the 68 patients (77%). The remaining 16 patients were not in the Center for Medicare and Medicaid Services (CMS) database, and the participating hospitals were unable to provide cost data for these patients. All device patients received the HeartMate VE LVAD and associated medical care. A surgical management committee developed guidelines and monitored adherence to them. The LVAD patients were compared with patients on optimal medical management, which included the use of angiotensin-converting enzyme inhibitors (ACEI), diuretics, digoxin, and beta-blockers, if not contraindicated. Guidelines were established, and a medical management committee monitored adherence. The study was approved by the institutional review board, and all patients signed informed consent.
Costing Methodology
To determine hospitalization costs, the REMATCH data set was combined with data from CMS (common working file), standard billing forms (UB-92), and line item bills provided directly by clinical centers. All costs prior to patient randomization were eliminated to provide a uniform starting point for trial-related treatment costs. Merging of these databases enabled an accurate compilation of implantation hospital charges for 52 of the 68 LVAD patients.
Institution-specific cost reports were used to calculate Ratio-of-Cost-to-Charges (RCCs) for each major resource category. The VAD cost was estimated to be $60,000, which was the cost to high-volume institutional users. Fees for professional services were not included in this analysis, in part because many of the physicians in the trial did not bill for their services. Implantation hospitalization costs began at randomization and ended at discharge from the acute care facility. Rehospitalization costs included readmissions to acute care facilities or intermediate care/rehabilitation centers.
Study Design and Statistical Analysis
The REMATCH trial was conducted in 20 centers and supported by a cooperative agreement among the National Heart, Lung, and Blood Institute, Thoratec, Inc., and Columbia University. The clinical data set used for this analysis was closed on June 20, 2002. The primary end point was all-cause mortality, analyzed by intention to treat, using the log-rank statistic. Adverse events were adjudicated by an external morbidity and mortality committee and designated as serious if they caused death, permanent disability, threatened life, or required or prolonged hospitalization. The trial follow-up was every 4 weeks, for a total of 24 visits or 672 days. Survival and costs were truncated at that time. Frequency of occurrence for serious adverse events was analyzed by Poisson regression. Continuous variables were expressed as means ± standard deviation.
Costing data were compared by Student t test after log-transformation and predictors determined by regression. The multiple regression models evaluated baseline factors (eg, age, sex, renal function, and blood pressure), operative factors (eg, reoperative status, peri-operative bleeding, and bypass time), and postoperative events (eg, stroke and device reliability) as independent variables. To assure that our costing population was representative of the overall LVAD cohort, we compared the frequency of critical adverse events (ie, sepsis, bleeding, and device failure) in those with and without cost data. Average annual in-patient costs were calculated by determining the average number of hospitalizations and associated costs per patient-day of LVAD support and annualized to 1 year. A few readmission costs (7.4% of all length of stay [LOS]) were missing from the economic dataset. However, from the clinical dataset we knew the length of stay (ICU and regular floor days), major operative procedures, and whether an LVAD was replaced for each patient. We inferred the costs for these readmissions by using the average cost of a resource category and multiplying it by the units of that resource use.
RESULTS
REMATCH Clinical Data
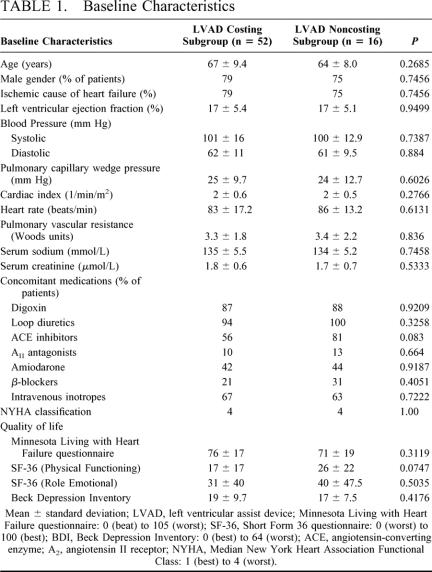
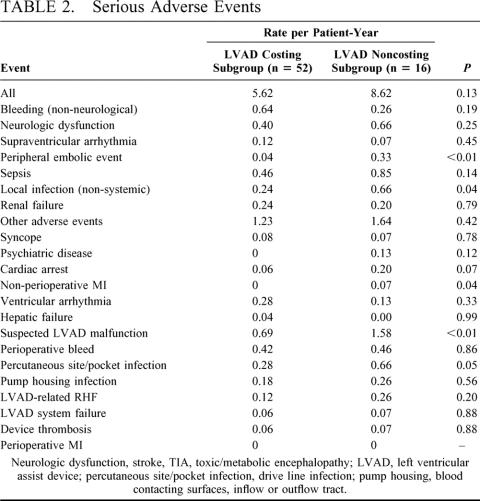
Table 1 depicts the patient demographics and baseline characteristics of the REMATCH LVAD costing subgroup (n = 52) and the balance of the REMATCH LVAD population (n = 16). There was no significant difference between the 2 groups. The one-year survival in the costing subgroup was 52% (95% CI, 38–66%) and 24% (95% CI, 10–38%) at 2 years. The survival for the LVAD patients not in our costing subgroup was not significantly different (P = 0.87). As of closure of the data set in June 2002, there were 16 patients alive in the LVAD cohort. Serious adverse events were similar in frequency for all but 5 event types (peripheral embolic events; nonperioperative myocardial infarction; suspected device malfunction; and percutaneous site/pocket infection). None of these events were significant predictors of cost. Sepsis and bleeding were the events with highest frequencies (Table 2).
TABLE 1. Baseline Characteristics
TABLE 2. Serious Adverse Events
LVAD Implantation Hospitalization Costs
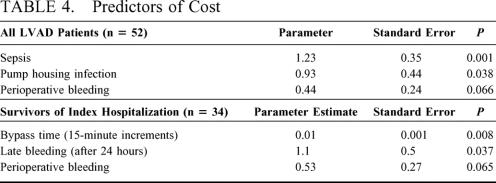
The mean length of stay was 43.5 days, and the median length of stay was 29 days, with 17 in-hospital deaths, in our costing subgroup, which were not significantly different from the subgroup constituting the balance of the LVAD population (mean = 50.9 days and median = 29 days, P = 0.83 and P = 0.85, respectively). The mean cost for the initial implant-related hospitalization was $210,187 ± 193,295. The median cost was $137,717 with a range of $72,583 to $1,123,565 (Table 3). The skewing of the costing data set was in part due to an outlier whose charges were almost 3 standard deviations above the mean for the group. Days spent in the ICU and regular floor (33%), and LVAD (30%) were the leading cost categories.
TABLE 3. Resource Categories for the Index Hospitalization
Of the 52 study patients, 35 survived the initial hospitalization. When implantation hospitalization costs are compared between hospital survivors and nonsurvivors, the mean costs increased from $159,271 ± 106,423 to $315,015 ± 278,713. Median costs increased from $136,700 to $183,805. These differences were partly driven by the increased length of stay from 35 ± 21 days to 66 ± 75 days.
Predictors of Implantation Costs
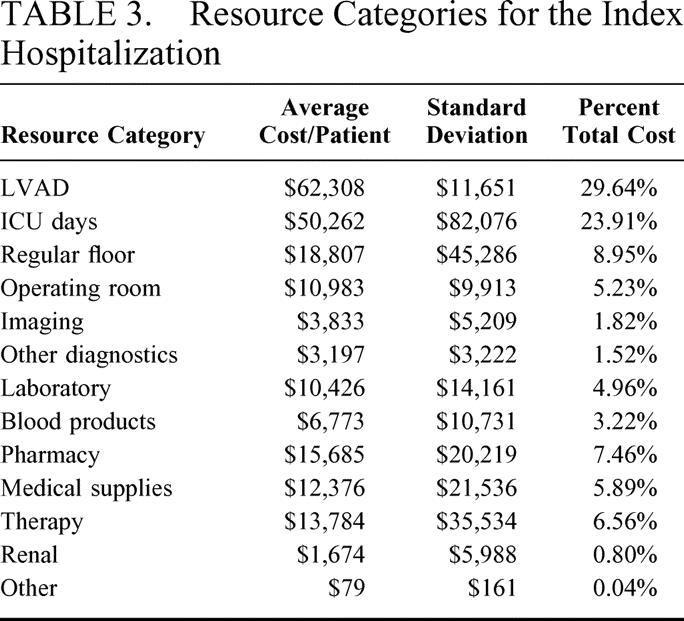
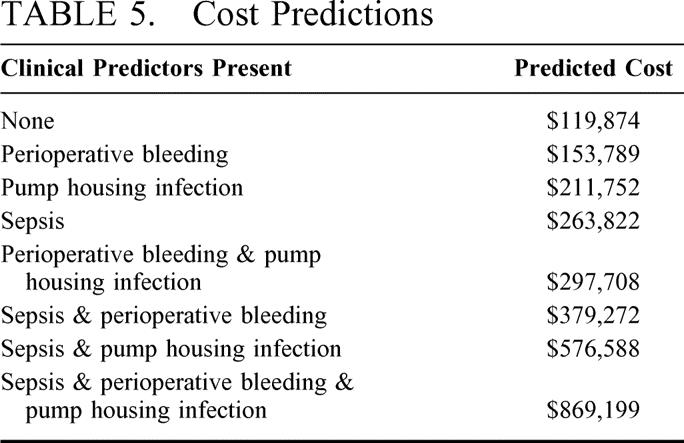
Table 4 depicts the independent predictors of implantation cost based on multiple regression analysis. Sepsis, pump housing infection, and perioperative bleeding are the major drivers of implantation cost (n = 52). In the patients who survived the procedure (n = 35), bypass time, perioperative bleeding, and late bleeding were the drivers of cost. Table 5 uses the model to predict the cost of the index hospitalization for all patients. In the absence of sepsis, pump housing infection, and perioperative bleeding, the predicted cost would be $119,874. If sepsis alone were present, the implantation hospitalization would be expected to increase to $263,822. If all 3 of these adverse events were present, the implantation hospitalization would be expected to reach $869,199.
TABLE 4. Predictors of Cost
TABLE 5. Cost Predictions
Annual Readmission Costs
The costing cohort experienced a total of 18,406 LVAD-supported days, of which 14,510 days were out of the hospital, during the follow-up period. There were a total of 152 readmissions, which involved 34 patients (4.5/patient) and 1634 hospital days. Sixteen patients in the cohort had 17 LVAD replacements during the entire follow-up period. The average readmission cost was $30,627 ± 61,569. The average annual readmission cost per patient for the overall cohort was $105,326, and $99,118 for the 27 patients who survived more than 1 year. When including both the implantation and readmission cost, the average annual cost for these 27 patients was $196,116. This is in contrast to the $309,273 annual cost for the entire costing cohort (n = 52).
DISCUSSION
Congestive heart failure (CHF) is a highly prevalent and life-threatening condition. Randomized trials have shown the mortality in the subset of patients with refractory end-stage disease to exceed 50% at 1 year, and in the REMATCH trial it was even higher (75%).1,6 These rates are higher than those for breast, colon, and even lung cancer. Pharmacological treatment offers limited benefit to these patients, while heart transplantation is seriously constrained by the shortage of donors. The REMATCH trial paved the way for FDA approval of LVADs as destination therapy, and payers must now confront coverage and reimbursement decisions for this indication. Shortly after FDA approval, the BlueCross and BlueShield Association’s Technology Evaluation Center, which provides scientific assessments of selected medical technologies to the Plans, concluded that the use of LVADs for destination therapy in patients with end-stage heart failure met its criteria for coverage. CMS and other private payers will be tackling this decision soon. While cost and cost effectiveness do not explicitly enter into their coverage decisions, these factors will, undoubtedly, shape the conditions of the CMS approval and will expressly enter the decision-making process of many of the private payers.
What is the critical evidence that is required to make these coverage decisions? Although limited in absolute magnitude, this technology offers important survival and quality of life benefits for a population with a dismal prognosis and few therapeutic options. The device improved the median survival by 8.6 months in REMATCH, more than doubling what was seen with optimal medical management, and significantly improving the quality of life of recipients, as measured by the SF-36, Minnesota Living with Heart Failure, and the Beck Depression Inventory scales. This net improvement in health outcome over an established alternative therapy was derived from a randomized trial that was conducted in cardiac transplantation centers around the nation, making the results generalizable to many clinical centers that hold expertise in the treatment of end-stage heart failure and the implantation of mechanical ventricular assist devices. The mean total cost to insert an LVAD in the REMATCH patient population was $210,187, which includes a $60,000 charge for the device. This is comparable to other life-saving organ replacement procedures, such as liver transplant, which has been estimated to cost $203,434 per procedure.7 This procedure has long been accepted by payers, and it is no longer considered experimental. Finally, as LVADs for destination therapy are an emerging procedure, opportunities exist for reducing costs with experience.
The evidence suggests several areas for improvement. First, our analysis revealed that sepsis was the most important predictor of cost. By itself, it more than doubled the cost of the index hospitalization, adding roughly $140,000 to the cost of the stay. Improvements in the design of current devices offer a sizeable opportunity to reduce infections and consequent costs for future patients. The REMATCH device uses a large-bore percutaneous driveline, which is a potential conduit for bacterial and fungal infection. Newer devices have smaller, more flexible drivelines or use a totally implantable design, which eliminates this portal for infection entirely. Moreover, malnutrition, due to the long course of chronic heart failure preceding implantation, and pump-related gastric constriction and a chronic inflammatory state that follows implantation, is a major factor that predisposes this population to bacterial and fungal infections. Malnutrition may be reduced with newer axial flow devices, which do not have an intra-abdominal component, and with newer approaches to both nutritional management and chronic inflammation.
Second, improved surgical proficiency and innovative approaches to management of bleeding would address another important factor that could drive up the cost of device implantation. In particular, efforts to develop antagonists that work at higher levels in the coagulation cascade (eg, on factors 9 and 10a) may offer anticoagulants that will reduce the current rate of postoperative bleeding.8,9 Device-related bleeding has already been reduced with bearing housing modification and strain relief modification to the outflow graft.
Third, improvement in device reliability will be important to minimize the cost of readmissions. Seventeen devices needed replacement in 52 patients. The leading causes of replacement were, in addition to sepsis, mechanical pump failure, and inflow valve incompetence. Reinforcement of the valve housing has already been implemented and may ameliorate part of the problem.
Finally, patient selection offers an opportunity to reduce costs. Survivors of the index hospitalization cost on average $156,000 less to manage than nonsurvivors. Moreover, those surviving more than 1 year had substantially less hospital resource utilization than the rest of the cohort ($196,116 versus $309,273 per annum). Clearly, this makes the case for improving patient selection. However, in our predictive model, there were no significant predictors of cost among the baseline patient characteristics. But, this may be a result of our small sample size. In the bridge-to-transplant population, analyses of “wearable” LVADs have identified preimplant patient characteristics that are independent risk factors for survival.10 This research has led to reliable scoring systems for predicting implantation survival.11 Although additional data would be necessary to develop such scoring systems for destination therapy, such systems could identify patient profiles of high-risk and high-cost patients that would assist in the patient selection process.
In short, should these devices be covered and reimbursed? These decision-making processes are dependent on analysis, as well as value judgments. Some would argue that LVADs offer limited benefits at considerable cost. Costs are, indeed, considerable at this stage of the development of the technology. However, this perception ignores that LVAD therapy is a substantial gain for a group of people with a terminal illness. This degree of benefit for patients with pancreatic cancer would be hailed as a major breakthrough and stimulate further development of what would be perceived to be a promising therapy. The need for such a therapy is unquestionable; of the estimated 60,000 patients who could benefit from cardiac transplantation each year, we conjecture that approximately 20% would be candidates for long-term LVAD therapy at present. Moreover, there is considerable potential for improving the technology in terms of effectiveness and cost. Even in the REMATCH trial, there was a significant improvement in survival in patients enrolled during the second half of the trial as compared with those enrolled during the first half of the trial, which ultimately should result in a decrease in cost. But, such improvements depend upon more widespread use of the technology, which would require adequate reimbursement. Contrary to accepted wisdom, innovation does not predominately occur in the laboratory, but in clinical practice.12 Such “learning by using,” as first identified by the Nobel Laureate Arrow, is a critical phase of the innovation process, particularly for medical devices and surgical procedures, which depend more on incremental modification than do pharmaceuticals.13
These learning-by-using experiences generate different types of knowledge. On one hand, these experiences may generate information about shortcomings or potential new applications of a technology that require further fundamental bench research or engineering/design modifications. This feedback loop was responsible for several important changes to the REMATCH device, including locking screw ring connectors on the inflow and outflow grafts to avert disconnections, and outflow graft bend relief to prevent kinking, which was responsible for the inflow valve incompetence observed in REMATCH. On the other hand, the knowledge generated in clinical practice may lead to changes in patient selection and management that require no design modifications. The recognition of the importance of sepsis, for instance, led to infection management guidelines, which defined the choice of antimicrobial prophylaxis, and the use of abdominal binders to stabilize the driveline exit site.
Coverage and reimbursement of this intervention does not mean that the procedure is ready for indiscriminate use. Certification standards for centers need to be introduced that specify the clinical experience required in the management of end-stage heart failure, in mechanical circulatory support devices, and the knowledge of transplantation selection criteria to assure that those who qualify are selected for this procedure. Ultimately, such centers should be certified on the basis of outcomes. However such determinations will require a data set that is considerably larger than the 68 patients from REMATCH. It argues for the conduct of postmarketing studies to measure the effectiveness and costs associated with destination therapy, providing a dynamic set of benchmarks for centers to meet, which would change with improvements in devices and management. Such a data set could, in turn, facilitate a dynamic clinical and policy-making decision process, which would assure that the use of this technology is tailored to the most appropriate patients at a reasonable cost to society.
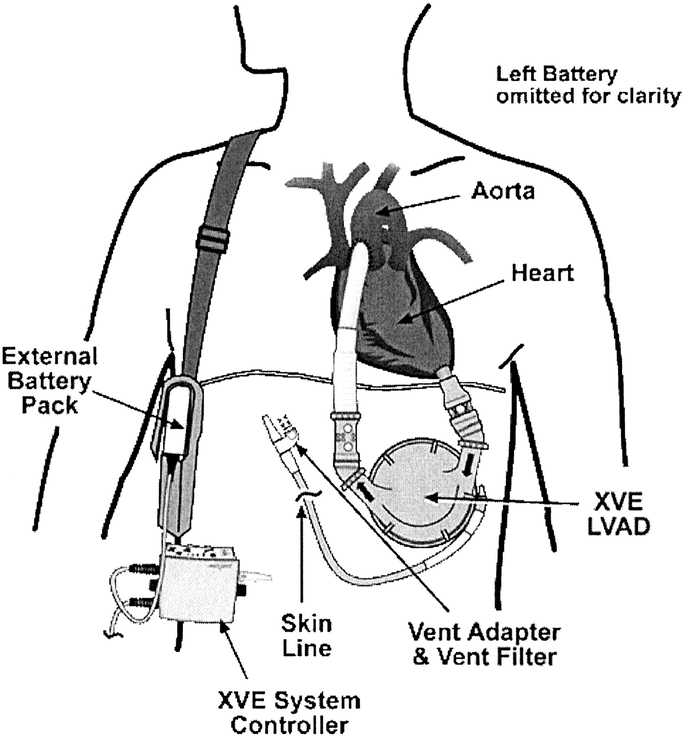
FIGURE 1. A wearable left ventricular assist device (LVAD) and its components. The inflow cannula is inserted into the apex of the left ventricle, and the outflow cannula is anastomosed to the ascending aorta. Blood returns from the lungs to the left side of the heart and exits through the left ventricular apex and across an inflow valve into the prosthetic pumping chamber. Blood is then actively pumped through an outflow valve into the ascending aorta. The pumping chamber is placed within the abdominal wall or peritoneal cavity. One percutaneous line carries the electrical cable and air vent to the battery packs and electronic controls, which are worn on a shoulder holster or belt.
Discussion
Dr. D. Glenn Pennington (Johnson City, Tennessee): Dr. Rose, this is an outstanding report and we are all indebted to you for showing all of us in this field that device support can actually render results better than that we can do medically. As a matter of fact we have been trying to say that for many years, but this is the first real evidence that that is the case. I wanted to ask some questions regarding the more widespread application of these devices.
One of them relates to the question of whether selection criteria might be changed. You indicated that might be 1 way to improve the results. What specific changes would you make in this patient population that you think might still provide evidence that it is superior to medical therapy but perhaps reduce cost?
The other question relates to device costs. You made the point that the device itself accounted for some 30% of the total cost, which all of us think is rather high, of course. But I wondered, with more widespread application will that cost actually go up or will it go down? In other words, was this a special deal for the study? Are the devices going to cost twice as much as we begin to implant them more widely?
I think we all agree that if we could somehow reduce the number of complications in these patients it could certainly impact costs. Along that thought, what will be the impact of a totally implantable system? Since this system still has a tube coming through the chest wall, which creates a possibility for infection, will a totally implantable device make a difference, particularly in costs?
It was an excellent presentation, and I appreciate the opportunity to discuss it.
Dr. Eric A. Rose (New York, New York): Thank you, Dr. Pennington. It is particularly gratifying to have the question coming from such an important pioneer in this field.
We frankly don’t know yet what the selection criteria should be. When we did a multivariate analysis to see if there is a subgroup we could define that had better results with this, no facts emerged. But the REMATCH database only includes 68 patients who received devices, so the database is not large enough to definitively answer the question.
That having been said, I think we have some leads. One that was not initially obvious to us and should have been is the issue of nutrition in these patients. Putting a device in someone who is severely nutritionally depleted is probably especially risky. It is an indication of our state of ignorance that we didn’t even gather prospectively serum albumin data in this trial.
Pulmonary vascular resistance, with regard to cost, shakes out as a predictor. With regard to survival, I don’t think we have enough power to make that judgment. Age may also be a factor, although even in the cohort of patients in this trial that were older than 70 years of age, their one-year survival was double that of the control group.
With regard to cost for the device, in these analyses we imputed a cost that is a reasonable estimate of the market cost of the device. I think it is likely that once a monopoly is broken in this field, and in particular when devices are available that don’t require as much titanium or 2 prosthetic valves as part of the configuration, eg, some of the axial flow pumps and centrifugal pumps that are already in trials, the cost of the device could come down substantially. I think it is not hard to envision a device or at least a manufacturing cost to be in the range of something less than an implantable defibrillator now.
In terms of reducing complications, I think it is certainly arguable that a totally implantable system would reduce these. There is an experience now with a fully implantable VAO, the Arrow Lionheart that has had patients survive as long as 2 years and even more with a fully implantable device. The patient experience is just too small to say that these devices are not going to be complicated by infection. The incidence of infection is so high with the wearable transcutaneous type of device that we have to be able to do better than we are doing now.
Dr. William L. Holman (Birmingham, Alabama): Dr. Rose, that was a very nice presentation. And I couldn’t agree with you more about looking at the cost of these high-tech interventions.
I asked earlier today about cost and accessibility to high-tech care. I think that is an important issue and something we need to keep in mind. Some of my own patients on assist devices have had problems just purchasing the materials that they require following implantation. These include replaceable batteries, air filters, et cetera.
We have seen dramatic improvements in the quality of life for some of these patients. Presumably as you and the InCHOIR group move forward with analysis you will begin to tackle the more complex question of cost and benefit. In that regard, how important do you think device reliability will be in improving cost efficacy? In the REMATCH trial there were a substantial number of device failures out at about 12 to 16 months. Recently Jim Long from LDS Hospital in Salt Lake City presented new data suggesting that the reliability of this particular device has been enhanced by several recent changes. Do you think that improved device reliability will provide a small or large increment to the quality of adjusted life years for these patients?
Dr. Eric A. Rose (New York, New York): I suspect it will be a blend of incremental and hopefully faster change. I am a firm believer that dissemination of this technology is going to allow the rapid development of better, more durable devices.
As a result of this trial, there have been more than 40 modifications made to the device that we initially employed in this trial. That set of changes was approved last week by the FDA.
Our expectation was that this was a two-year device. We did a small preliminary randomized trial before we did REMATCH called PREMATCH in which the two-year survival rate of device patients was zero. That ended in 1998. In a mere 5 years we have gone to almost a 40% two-year survival rate. I am optimistic we will be able to do even better.
Dr. Nancy L. Ascher (San Francisco, California): Dr. Rose, I have an unpopular question. You have told us about the cost of caring for these patients, but you haven’t told us about their contribution to margin. The cost of taking care of these patients is over $4,000 a day. I doubt that you are able to recoup that. Can you talk about that?
Dr. Eric A. Rose (New York, New York): Until the 90th patient enrolled there was no contribution margin. All the costs were borne by the centers that participated in this trial. And I think that is a remarkable act of multi-institutional philanthropy to make this happen.
We actually were the first trial to be approved for reimbursement by Medicare after Clinton announced in his last 6 months in office that Medicare would pay for randomized trials of potentially life-saving therapy. And I must say if that had not happened I am not sure we would have completed it, because there was a good deal of negative feedback from hospitals and their administrators with regard to the costs involved.
That having been said, we have had a very substantial dialogue with Medicare as far as the approval process. I and 3 other coinvestigators have petitioned Medicare to pay for destination therapy. That was the basis for a recent Medicare Coverage Advisory Committee decision.
The Medicare staff tell us that the statute under which they operate says that they have to pay for things that are necessary and reasonable. If they are going to start saying that approaches that make people live longer and feel better are not necessary and reasonable care, they realize this essentially up-ends their entire reimbursement mechanism. So they have been enormously cooperative in moving this ahead.
With regard to how much hospitals will be paid, this is already part of an existing DRG, DRG-525, which right now pays hospitals poorly. But the reason for that many have thought was some diabolical plot to restrict this technology. What Medicare does is go through their caseload, see what the costs are, and then they impute a reasonable payment for it.
This DRG also includes postcardiotomy shock support. Those patients had a 75% inpatient mortality and generally a short length of stay. The devices that are employed for that indication are much cheaper, about $10,000 each. The payment just went up about $20,000 this past year because bridge patients are starting to be blended into that cost.
We did gather the REMATCH data together with the Medicare people, and we are hoping that if they approve destination therapy that they will use that cost data as a point of departure to update the DRG payment as well.
Footnotes
The REMATCH trial was supported, in part, by a cooperative agreement (HL-53986) funded by the National Heart Lung and Blood Institute of the National Institutes of Health (NIH), Bethesda, MD, and Thoratec Corporation, Pleasanton, CA. Additional funding for the routine costs of clinical care associated with the trial was made available by the Center for Medicare and Medicaid Services and by the participating clinical centers.
Reprints: Annetine C. Gelijns, PhD, International Center for Health Outcomes and Innovation Research, 600 West 168th Street (7th Floor), New York, NY 10032. E-mail: acp10@columbia.edu
REFERENCES
- 1.Rose E, Gelijns A, Moskowitz A, et al. Long-term mechanical left ventricular assistance for end-stage heart failure. N Engl J Med. 2001;345:1435–1443. [DOI] [PubMed] [Google Scholar]
- 2.Jessup M. Mechanical cardiac-support devices–dreams and devilish details. N Engl J Med. 2001;345:1490–1493. [DOI] [PubMed] [Google Scholar]
- 3.O’Connell J, Birstow M. Economic impact of heart failure in the United States: time for a different approach. J Heart Lung Trans. 1994;13:S107–S112. [PubMed] [Google Scholar]
- 4.Gelijns AC, Richards AF, Williams DL, et al. Evolving costs of long-term left ventricular assist device implantation. Ann Thoracic Surg. 1997;64:1312–1319. [DOI] [PubMed] [Google Scholar]
- 5.Rose EA, Moskowitz AJ, Packer M, et al. The REMATCH trial: rationale, design, and end points. Randomized Evaluation of Mechanical Assistance for the Treatment of Congestive Heart Failure. Ann Thoracic Surg. 1999;67:723–730. [DOI] [PubMed] [Google Scholar]
- 6.Califf R, Adams K, McKenna W, et al. A randomized controlled trial of epoprostenol therapy for severe congestive heart failure: The Flolan International Randomized Survival Trial (FIRST). Am Heart J. 1997;134:44–54. [DOI] [PubMed] [Google Scholar]
- 7.Showstack J, Katz PP, Lake JR, et al. Resource utilization in liver transplantation: effects of patient characteristics and clinical practice. NIDDK Liver Transplantation Database Group. JAMA. 1999;281:1381–1386. [DOI] [PubMed] [Google Scholar]
- 8.Spanier TB, Oz MC, Madigan JD, et al. Selective anticoagulation with active site blocked factor IXa in synthetic patch vascular repair results in decreased blood loss and operative time. ASAIO J. 1997;43:M526–M530. [PubMed] [Google Scholar]
- 9.Buller HR. Treatment of symptomatic venous thromboembolism: improving outcomes. Semin Thromb Hemost. 2002;28(Suppl 2):41–8. [DOI] [PubMed] [Google Scholar]
- 10.Deng MC, Loebe M, El-Banayosy A, et al. Mechanical circulatory support for advanced heart failure: effect of patient selection on outcome. Circulation. 2001;103:231–237. [DOI] [PubMed] [Google Scholar]
- 11.Oz MC, Goldstein DJ, Pepino P, et al. Screening scale predicts patients successfully receiving long-term implantable left ventricular assist devices. Circulation. 1995;92:II169–II173. [DOI] [PubMed] [Google Scholar]
- 12.Gelijns A, Rosenberg N, Moskowitz A. Capturing the unexpected benefits of medical research. N Engl J Med. 1998;339:693–698. [DOI] [PubMed] [Google Scholar]
- 13.Arrow K. The economic implications of learning by doing. Rev Econ Stud. 1962;29:155–173. [Google Scholar]