Abstract
Objective:
Although quality assessment is gaining increasing attention, there is still no consensus on how to define and grade postoperative complications. This shortcoming hampers comparison of outcome data among different centers and therapies and over time.
Patients and Methods:
A classification of complications published by one of the authors in 1992 was critically re-evaluated and modified to increase its accuracy and its acceptability in the surgical community. Modifications mainly focused on the manner of reporting life-threatening and permanently disabling complications. The new grading system still mostly relies on the therapy used to treat the complication. The classification was tested in a cohort of 6336 patients who underwent elective general surgery at our institution. The reproducibility and personal judgment of the classification were evaluated through an international survey with 2 questionnaires sent to 10 surgical centers worldwide.
Results:
The new ranking system significantly correlated with complexity of surgery (P < 0.0001) as well as with the length of the hospital stay (P < 0.0001). A total of 144 surgeons from 10 different centers around the world and at different levels of training returned the survey. Ninety percent of the case presentations were correctly graded. The classification was considered to be simple (92% of the respondents), reproducible (91%), logical (92%), useful (90%), and comprehensive (89%). The answers of both questionnaires were not dependent on the origin of the reply and the level of training of the surgeons.
Conclusions:
The new complication classification appears reliable and may represent a compelling tool for quality assessment in surgery in all parts of the world.
The lack of a uniform way of reporting complications hampers interpretation of surgical outcome data and quality assessment. The authors revisited a previously reported classification of complications and propose a new grading system. The new classification was tested in a cohort of 6336 patients undergoing general surgery and through an international survey.
Growing demand for health care, rising costs, constrained resources, and evidence of variations in clinical practice have triggered interest in measuring and improving the quality of health care delivery. For a valuable quality assessment, relevant data on outcome must be obtained in a standardized and reproducible manner to allow comparison among different centers, between different therapies and within a center over time.1–3 Objective and reliable outcome data are increasingly requested by patients and payers (government or private insurance) to assess quality and costs of health care. Moreover, health policy makers point out that the availability of comparative data on individual hospital's and physician's performance represents a powerful market force, which may contribute to limit the costs of health care while improving quality.4
Conclusive assessments of surgical procedures remain limited by the lack of consensus on how to define complications and to stratify them by severity.1,5–8 In 1992, we proposed general principles to classify complications of surgery based on a therapy-oriented, 4-level severity grading.1 Subsequently, the severity grading was refined and applied to compare the results of laparoscopic versus open cholecystectomy9 and liver transplantation.10 This classification has also been used by others11–13 and was recently suggested to serve as the basis to assess the outcome of living related liver transplantation in the United States (J. Trotter, personal communication). However, the classification system has not yet been widely used in the surgical literature.
The strength of the previous classification relied on the principle of grading complications based on the therapy used to treat the complication. This approach allows identification of most complications and prevents down-rating of major negative outcomes. This is particularly important in retrospective analyses. However, we felt that modifications were necessary, particularly in grading life-threatening complications and long-term disability due to a complication. We also felt that the duration of the hospital stay can no longer be used as a criterion to grade complications. Although definitions of negative outcomes rely to a large extend on subjective “value” appraisals, the grading system must be tested in a large cohort of patients. Finally, a classification is useful only if widely accepted and applied throughout different countries and surgical cultures. Such a validation was not done with the previous classification.
Therefore, the aim of the current study was 3-fold: first, to propose an improved classification of surgical complications based on our experience gained with the previous classification1; second, to test this classification in a large cohort of patients who underwent general surgery; and third, to assess the reproducibility and acceptability of the classification through an international survey.
METHODS AND DEFINITIONS OF COMPLICATIONS
Definition of Negative Outcome
As in the previous publication of 1992, we kept the 3 definitions of negative outcomes by differentiating complications, failure to cure, and sequelae.1 Complications were defined as any deviation from the normal postoperative course. This definition also takes into account asymptomatic complications such as arrhythmia and atelectases. A sequela is an “after-effect” of surgery that is inherent to the procedure (eg, inability to walk after a amputation of the leg). Finally, surgery may be well executed without any complications but still fail. If the original purpose of surgery has not been achieved, this is not a complication but a “failure to cure” (eg, residual tumor after surgery). Sequelae and failure to cure should not be included in the new classification of complications.
Classification of Surgical Complications
The previous classification consisted of 4 severity grades.1,9,10 Grade 1 included minor risk events not requiring therapy (with exceptions of analgesic, antipyretic, antiemetic, and antidiarrheal drugs or drugs required for lower urinary tract infection). Grade 2 complications were defined as potentially life-threatening complications with the need of intervention or a hospital stay longer than twice the median hospitalization for the same procedure. Grade 2 was divided into 2 subgroups based on the invasiveness of the therapy selected to treat the complication; grade 2a complications required medications only and grade 2b an invasive procedure. Grade 3 complications were defined as complications leading to lasting disability or organ resection, and finally, a Grade 4 complication indicated death of a patient due to a complication.
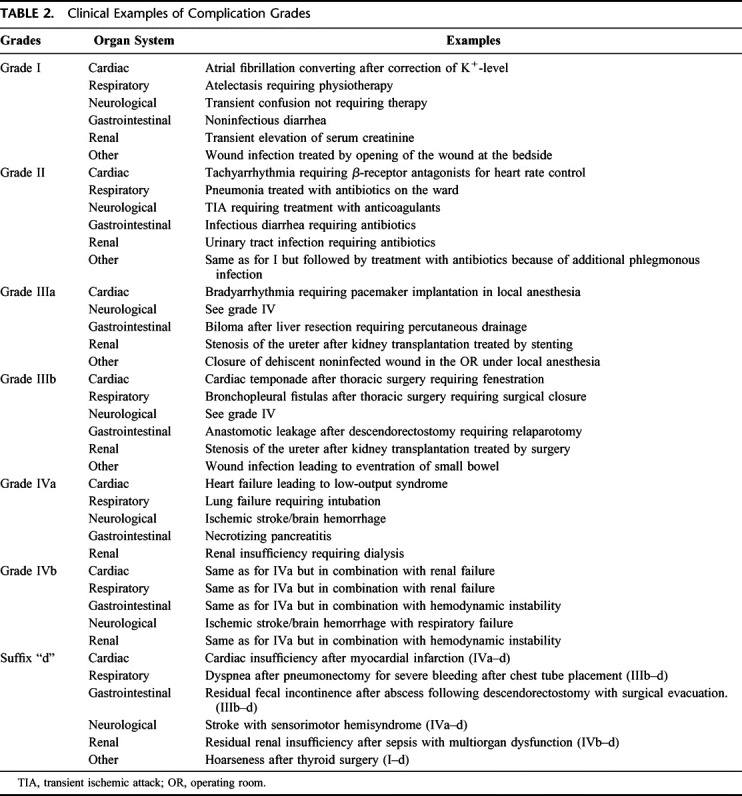
The modified classification is presented in Table 1 with clinical examples in Table 2. The therapy used to correct a specific complication remains the cornerstone to rank a complication. We made significant modifications compared with the previous classification and increased the number of grades from 5 to 7, including 2 subgroups for grades 3 and 4. The rationale to divide some grades into 2 subgroups is that these types of complication are likely to be often pooled due to small numbers. Grades I and IIa complications in the initial classification correspond to grades I and II complications in the modified version. Grade IIb events (need for invasive procedures) in the former classification are now listed as a separate entity (grade III complications), further subdivided into grades IIIa and IIIb depending on the need for general anesthesia. The length of hospital stay as a criterion to rank grade 2 complications was eliminated. Life-threatening complications such as an acute respiratory distress syndrome (ARDS) with the need for mechanical ventilation, listed as grade IIb complications in the initial classification, are now recognized as a higher grade (grade IV complications). Finally, disability, as defined as any impairment of a body function (such as neurologic deficits of an extremity due to positioning of the patient during surgery or hoarseness after thyroid surgery), is no longer a grade on its own (grade III in the previous version), but is now highlighted by the suffix “d” (for “disability”). Thus, any grade of complication may be supplemented with this information.
TABLE 1. Classification of Surgical Complications
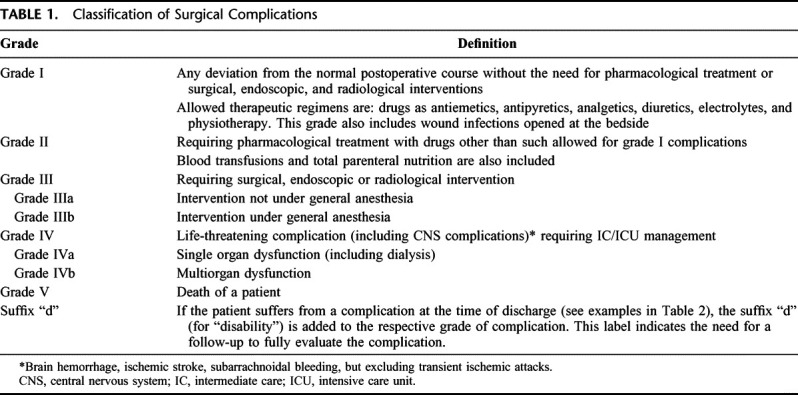
TABLE 2. Clinical Examples of Complication Grades
Validation of the Modified Classification in a Cohort of 6336 Patients
Data of 6336 patients undergoing elective surgery in our institution between 1988 and 1997 were prospectively collected. This database has been used in another study assessing the effects of obesity on the outcome of surgery.14 Here, we evaluated possible correlations between the various grades of complications and complexity of surgery as well as the length of hospital stay in this large cohort of patients. For the latter analysis, the most severe complication was registered for patients with more than 1 complication.
The complexity of surgery was estimated according to a modification of a previously published graduation.15 Briefly, operation type A includes surgical procedures without opening of the abdominal cavity (eg, type A: hernia repair, soft tissue surgery, thyroid surgery, excision of lymph nodes). Operation type B includes abdominal procedures except liver surgery and major surgery in the retroperitoneum (eg, type B: stomach, small bowel and colon surgery, splenectomy, and cholecystectomy). Operation type C includes liver surgery, operations on the esophagus, pancreas, rectum, and retroperitoneum.
International Survey to Assess Acceptability and Reproducibility of the Classification
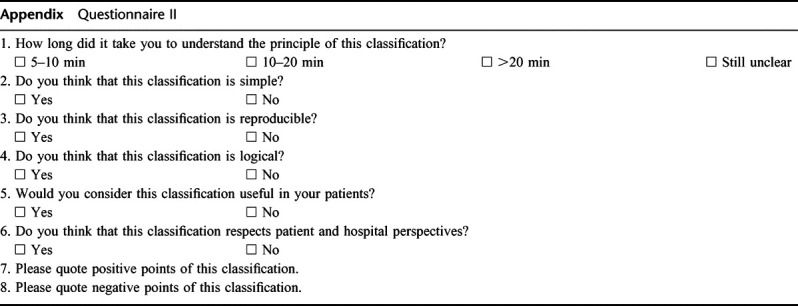
To assess the acceptability and reproducibility of the modified classification, 2 questionnaires were mailed to heads or senior surgeons of surgical departments in 10 centers around the world (Argentina, Australia, Japan, Korea, Switzerland, and United States). The first questionnaire presented 14 clinical cases including postoperative complications to be ranked according to the new classification. The second questionnaire focused on personal judgments about the classification (see Appendix). The corresponding surgeons were asked to obtain at least 5 replies from surgeons at various levels of training, respectively, at the junior level (intern to second year), at the senior resident level, and from experienced surgeons. Replies were kept anonymous.
Statistical Analyses
In the cohort of patients, the correlations between the complication grades and the complexity of surgery as well as length of hospital stay were analyzed using the bivariate Spearman rank correlation test. Values are expressed as median (range). For the first questionnaire of the international survey, an arcsine transformation of the percentages of correct answers of physicians was performed to obtain an approximately normal distribution. Differences between countries and levels of training were analyzed using 2-way analysis of variance (ANOVA). In the second questionnaire, multiple logistic regression was used to evaluate differences between countries (provenance of reply) and level of training. For all analyses, P < 0.05 was considered significant. Statistic analyses were made by a statistician of the Department of Biostatistics of the University of Zurich. Statistical Package for the Social Sciences (SPSS, version 10.0, Chicago, IL) was used for all analyses.
RESULTS
Validation of the Modified Classification in a Cohort of 6336 Patients
One or more complications occurred in 16.4% of the patients in the cohort. Grade I complications were recorded in 7.4%, grade II in 4.2%, grade IIIa in 0.8%, grade IIIb in 4.0%, grade IVa complications in 1.6%, and grade IVb in 0.7% of patients. The mortality rate (grade V complications) was 1.2%. Until 2000, there was no policy for early discharge in our hospital, and therefore the length of stay was possibly still a good marker of outcome. We therefore correlated the new grading system with the length of stay in this cohort of patients. The classification of complications (grades I–IV) significantly correlated with the duration of the hospital stay (P < 0.0001, Spearman rank correlation test). Median length of hospitalization in patients without complication was 7 days (range 1–28). Hospital stay in patients with complications was, respectively, 14 days (range 1–44 days) when patients developed grade I complications only, 17 days (range 1–68 days) in those with grade II, 20 days (range 5–59 days) in presence of grade IIIa, 23 days (range 4–137 days) in grade IIIb, 26 days (2–74 days) in grade IVa, and finally, 53 days (14–175 days) in grade IVb complications (Fig. 1). Length of hospitalization of patients who died due to a complication (grade V) was 18 days (1–81 days). A strong correlation was also found between the complexity of surgery (and assumed higher complication rates) and outcome of surgery as assessed by the new classification (P < 0.0001, Spearman rank correlation test; Fig. 2).
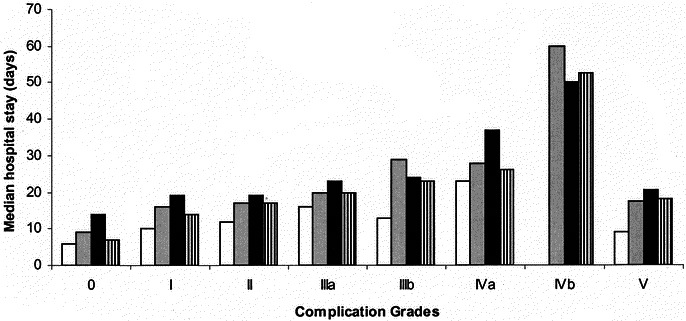
FIGURE 1. Length of hospital stay related to the types of complications. A statistically significant correlation was noted between the respective grades of complications and the length of hospital stay (P < 0.0001; Spearman rank correlation test). When more than 1 complication occurred in a patient, only the most severe was taken into account in this analysis. Grade 0 means no complication; grade V means death of a patient due to a complication. (□), Operation Type A; ( ), Operation Type B; (▪), Operation Type C; (▥), overall.
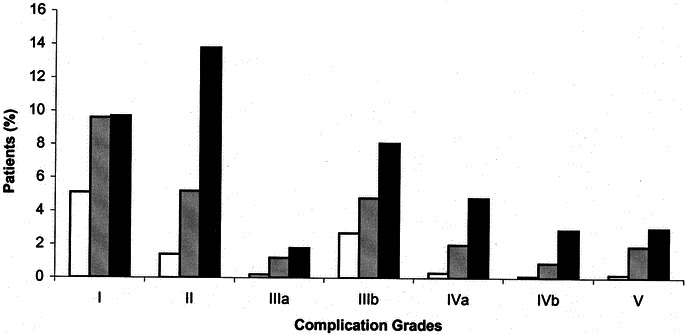
FIGURE 2. Percent of patients presenting a complication for each grade of complications. A significant correlation was observed between the number of patients presenting the respective complication and the types of surgery (P < 0.0001; Spearman rank correlation test). In other words, in each complication grade, complications occurred more frequently in complex surgical procedures. Operation Type A (□) < Operation Type B ( ) < Operation Type C (▪).
International Survey to Assess Acceptability and Reproducibility of the Classification
All 10 centers contacted answered the survey. The survey was completed by 144 surgeons, of whom 21 were from Argentina, 31 from Asia, 9 from Australia, 30 from the United States, and 51 from Switzerland. The surveyed surgeons were at different levels of training: 44 interns/junior residents, 55 senior residents, and 31 were board certified usually with at least 10 years of experience. Disclosure of level of training was not available in 14 surveys.
Most complications were graded correctly in the first questionnaire. The rates of accurate answers was 93% for surgeons from Argentina (273/294 [number of questions × number of surgeons]), 87% (402/462) for Asian surgeons, 93% (117/126) for surgeons from Australia, 89% (374/420) for American, and 91% (650/714) for Swiss surgeons (Table 3). The rates of correct answers did not depend on the level of training (intern, resident, board surgeon; 2-way ANOVA; P = 0.6) or the origin of the reply (2-way ANOVA; P = 0.08).
TABLE 3. Results From the Survey
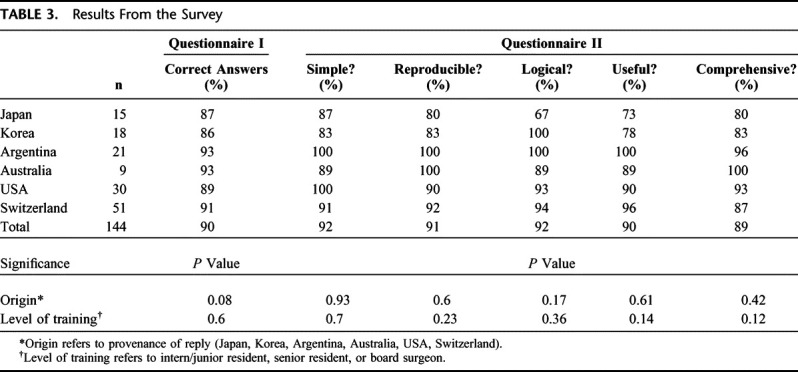
On the second questionnaire, 133 of the 144 surgeons judged the classification to be simple (92%), 131 to be reproducible (91%), and 133 surgeons found the classification logical (92%). A total of 130 surgeons (90%) replied that they would support the introduction of the classification in their clinical practice, and 128 (89%) surgeons stated that this classification covers both the patient's as well as the medical perspective. Similar to the first questionnaire, the answers appeared not to depend on the level of training and the origin of surgeons (multiple logistic regression; Table 3).
DISCUSSION
The absence of consensus within the surgical community on the best way to report surgical complications has hampered proper evaluation of the surgeon's work and possibly progress in the surgical field.16 In 1992, Clavien et al proposed a classification of complications,1 which has subsequently been used by us9,10 and others11–13 for outcome assessment. In the present study, we propose significant revisions of this classification by increasing the number of grades and the weight for life-threatening complications requiring intensive care management. The length of hospital stay was also eliminated as a criterion to rank complications. We also gave more emphasis to the patient perspective by introducing the notion of presumed long-lasting disability, which can be added to each type of complication. An attempt was made to validate the new proposal by correlating the various grades of complications with presumed parameters of severity of morbidity in a cohort of 6336 patients. Finally, the acceptance and reproducibility of the classification was shown through an international survey completed by surgeons at various levels of training.
As with the previous classification,1 the present classification focuses mainly on the therapeutic consequences of a complication. However, based on our experience, we made 4 important modifications to increase its reliability and potential use in the surgical literature. First, life-threatening complications requiring an intermediate or intensive care management (IC/ICU) were differentiated from complications treated on the ward. Such complications are associated with a high mortality, stress for the patients, and substantial resource consumption.17 Secondly, complications involving the central nervous system (eg, ischemic stroke, brain hemorrhage, subarachnoidal bleeding) are also considered in the same category (grade IV complications). The high mortality rate associated with central nervous system injuries and recent evidence that such complications must be managed in an ICU setting18 justify this ranking. Third, the length of hospital stay is no longer considered in the ranking of complications. In the previous classification, any complication resulting in “hospital stay greater than twice the median stay for the procedure” was considered at least a grade II complication, but information about median stay may not be available for all procedures and greatly varies among centers. Moreover, length of hospital stay is highly influenced by the medical system of a given center. Fourth, the presumed long-term consequences of a complication are considered in the present classification. Complications that have the potential for long-lasting disability after patient's discharge (eg, paralysis of a voice cord after thyroid surgery) are highlighted in the present classification by a suffix (“d” for disability). This suffix indicates that a follow-up is required to comprehensively evaluate the outcome and related long-term quality of life. This is an important amelioration of the former classification, where disabilities were only charted when considered to be permanent and recorded as complication of high severity (eg, stroke).
The ranking of complications by severity depends on the perspective considered. A classification integrating medical, payer, and patient perspectives is not feasible, as correlation between these different perspectives is poor.19 The new classification mainly focuses on the medical perspective, with a major emphasis on the risk and invasiveness of the therapy used to correct a complication. This perspective tends to minimize subjective interpretation and any tendency to down-rate complications because it is based on hard facts.1 This approach is particularly important in retrospective studies where postoperative problems are often poorly reported, whereas the therapy to treat a complication is well documented in both physician and nursing reports. As a limitation, it could be argued that policies in the management of a given surgical complication vary among different physicians and centers or countries. For example, an intra-abdominal abscess after bowel resection may be treated either by antibiotics, percutaneous drainage or relaparotomy, often depending on personal and somewhat subjective appraisals. Such variation is mostly due to the lack of accepted paradigm for the “best practice,” but may also depend on local factors such as the availability of medical resources (eg, interventional radiologist).
Despite these variations, we believe that the use of therapeutic consequences as the basis to rank complications remains the best approach: First, this is the most readily available and objective information regarding the postoperative course. Second, a therapy may induce stress to a patient and further morbidity (eg, antibiotics, full anticoagulation, anesthesia, etc), which justifies inclusion in the ranking system. Third, medical resources are limited and have to be used with reluctance. The least invasive or expensive treatment that is effective should be chosen to treat a complication. A recent study reviewing the definition of anastomotic leakage after gastrointestinal surgery would support this concept.20 The authors identified 56 different definitions of anastomotic leaks in 97 publications, making comparison among the studies impossible. To address these inconsistencies, they recommended using the therapeutic consequences of the anastomotic leakage to assess the severity of the complication.
The rising cost of health care is given increasingly importance worldwide. A major factor affecting hospital cost is complications following surgery,21–25 and it could be argued that cost should be included in the ranking of complications. However, cost evaluation is not a valid tool for comparison among centers because detailed systems that permit comparative, uniform cost accounting for complications are not yet fully developed. Furthermore, death is the worst complication for a physician and a patient, but may be associated with low cost, thus decreasing the impact of cost analyses for outcome research. For these reasons, the payer's perspective cannot be included in such classification system, and we would argue that it should be computed and presented separately.
In addition to the medical and payer's perspectives, the patient′s perspective (ie, quality of life, pain, psychologic strain) may also be taken into account to estimate the severity of a complication. Although this perspective is obviously crucial, the perception of patients varies greatly depending on the patient's character, the management and the information policy of the physician as well as the physical condition of the patient before and after surgery. For example, patients with dramatic improvement of their clinical condition after liver transplantation may tolerate complications much better than those after low morbidity procedures (eg, hernia repair).19 Additionally, quality of life assessments are complex typically targeting on many aspects of life (eg, the SF-3626 survey measures 8 dimensions of health). Thus, simplicity and attractiveness of a classification focusing on morbidity and mortality would be lost if an attempt was made to comprehensively include parameters of quality of life. However, some patient insight was newly taken into account in the classification by enabling the recording of potential permanent disability associated to any type of complications.
Subjectivity remains a potential limitation in the use of a classification of complications. Different surgical approaches and cultural discrepancies may induce a large variability in the evaluation of a specific complication around the world. To explore this potential limitation, the classification was tested in a large cohort of 6336 patients. Complexity of surgery and length of hospital stay significantly correlated with the various grades of complications, providing some evidence of objectivity in the grading system. Others have also showed strong correlation between the complexity of surgery and postoperative complications.27 The duration of hospital stay, although unreliable as criterion of outcome among centers, is a useful parameter of the severity of a complication within a single center, particularly when there is a defined discharge policy. Such correlation between complications and postoperative stay was shown in several single-center studies.25,28 The survey conducted in centers from each continent and including surgeons at different levels of training revealed high reproducibility and acceptability. Taken together, these data suggest that the proposed classification might gain wide acceptance in the surgical community around the world.
We conclude that the proposed morbidity scale based on the therapeutic consequences of complications constitutes a simple, objective, and reproducible approach for comprehensive surgical outcome assessment. This classification seems to be applicable in most parts of the world and may even be used by surgeons who are less experienced. The broad implementation of this classification into surgical literature may facilitate the evaluation and comparison of surgical outcomes among different surgeons, centers, and therapies.
ACKNOWLEDGMENTS
We are grateful to Burkhardt Seifert from the Department of Biostatistics, University of Zurich, Switzerland, for the help with the statistical analyses. We are also indebted to Abe Fingerhut, MD, for his constructive comments. We also gratefully thank the following surgeons and centers for their interest and help in the validation of our complication classification: Koo-Jeong Kang, MD (Department of Surgery, Keimyung University Dongsan Medical Center, Taegu, Korea), Morito Monden, MD (Department of Surgery and Oncology, University of Osaka, Japan), Juan Pekolj, MD (Department of Surgery, Hospital Italiano, Buenos Aires, Argentina), Rob Padbury, MD (Department of Surgery, Flinders Medical Center, Adelaide, Australia), Steven Strasberg, MD (Section of Hepatobiliary, Pancreatic & Gastrointestinal Surgery, Washington University School of Medicine, St. Louis, MO), Jean Nicolas Vauthey, MD (Department of Surgical Oncology, The University of Texas M. D. Anderson Cancer Center, Houston, TX), Ravi Chari, MD (Department of Surgery, Vanderbilt University Medical Center, Nashville, TN), Urban Laffer, MD (Hospital Center Biel, Biel, Switzerland), and Lukas Eisner, MD (Department of Surgery, Cantonal Hospital Olten, Olten, Switzerland), and the staff and residents of the Division of Visceral and Transplantation Surgery, University Hospital of Zurich, Switzerland.
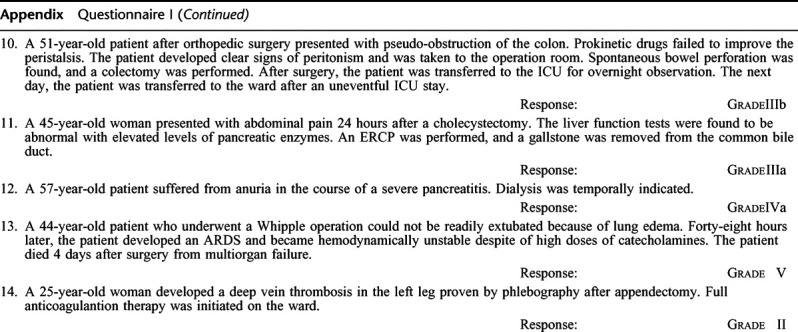
Appendix Questionnaire I
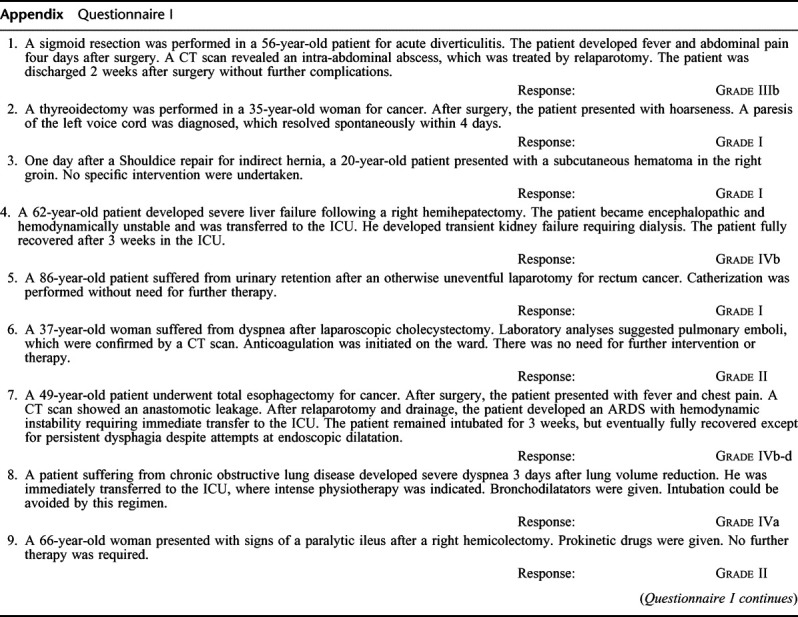
Appendix Questionnaire I (Continued)
Appendix Questionnaire II
REFERENCES
- 1.Clavien P, Sanabria J, Strasberg S. Proposed classification of complication of surgery with examples of utility in cholecystectomy. Surgery. 1992;111:518–526. [PubMed] [Google Scholar]
- 2.Khuri SF, Daley J, Henderson W. et al. The Department of Veterans Affairs’ NSQIP: the first national, validated, outcome-based, risk-adjusted, and peer-controlled program for the measurement and enhancement of the quality of surgical care. National VA Surgical Quality Improvement Program. Ann Surg. 1998;228:491–507. doi: 10.1097/00000658-199810000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nashef SA, Roques F, Michel P. et al. European system for cardiac operative risk evaluation (EuroSCORE). Eur J Cardiothorac Surg. 1999;16:9–13. doi: 10.1016/s1010-7940(99)00134-7. [DOI] [PubMed] [Google Scholar]
- 4.Daley J, Henderson W, Khuri S. Risk-adjusted surgical outcomes. Annu Rev Med. 2001;52:275–287. doi: 10.1146/annurev.med.52.1.275. [DOI] [PubMed] [Google Scholar]
- 5.Pomposelli J, Gupta S, Zacharoulis D. et al. Surgical complication outcome (SCOUT) score: a new method to evaluate quality of care in vascular surgery. J Vasc Surg. 1997;25:1007–1015. doi: 10.1016/s0741-5214(97)70124-1. [DOI] [PubMed] [Google Scholar]
- 6.Gawande A, Thomas E, Zinner M, Brennan T. The incidence and nature of surgical adverse events in Colorado and Utah in 1992. Surgery. 1999;126:66–75. doi: 10.1067/msy.1999.98664. [DOI] [PubMed] [Google Scholar]
- 7.Veen M, Lardenoye J, Kastelein G. et al. Recording and classification of complications in a surgical practice. Eur J Surg. 1999;165:421–424. doi: 10.1080/110241599750006622. [DOI] [PubMed] [Google Scholar]
- 8.Pillai S, van Rij A, Williams S. et al. Complexity- and risk-adjusted model for measuring surgical outcome. Br J Surg. 1999;86:1567–1572. doi: 10.1046/j.1365-2168.1999.01286.x. [DOI] [PubMed] [Google Scholar]
- 9.Clavien P, Sanabria J, Mentha G. et al. Recent results of elective open cholecystectomy in a North American and a European center. Ann Surg. 1992;216:618–626. doi: 10.1097/00000658-199212000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Clavien P, Camargo C, Croxford R. et al. Definition and classification of negative outcomes in solid organ transplantation. Ann Surg. 1994;220:109–120. doi: 10.1097/00000658-199408000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Feldman L, Barkun J, Barkun A, et al. Measuring postoperative complications in general surgery patients using an outcomes-based strategy: comparison with complications presented at morbidity and mortality rounds. Surgery. 1997;122:711–719; discussion 719–720. [DOI] [PubMed]
- 12.Targarona EM, Espert JJ, Bombuy E. et al. Complications of laparoscopic splenectomy. Arch Surg. 2000;135:1137–1140. doi: 10.1001/archsurg.135.10.1137. [DOI] [PubMed] [Google Scholar]
- 13.Ghobrial RM, Saab S, Lassman C. et al. Donor and recipient outcomes in right lobe adult living donor liver transplantation. Liver Transpl. 2002;8:901–909. doi: 10.1053/jlts.2002.35548. [DOI] [PubMed] [Google Scholar]
- 14.Dindo D, Muller MK, Weber M, Clavien PA. Obesity in general elective surgery. Lancet. 2003;361:2032–2035. doi: 10.1016/S0140-6736(03)13640-9. [DOI] [PubMed] [Google Scholar]
- 15.Klotz H, Candinas D, Platz A. et al. Preoperative risk assessment in elective general surgery. Br J Surg. 1996;83:1788–1799. doi: 10.1002/bjs.1800831240. [DOI] [PubMed] [Google Scholar]
- 16.Martin RC, Brennan MF, Jaques DP. Quality of complication reporting in the surgical literature. Ann Surg. 2002;235:803–813. doi: 10.1097/00000658-200206000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chung DA, Sharples LD, Nashef SA. A case-control analysis of readmissions to the cardiac surgical intensive care unit. Eur J Cardiothorac Surg. 2002;22:282–286. doi: 10.1016/s1010-7940(02)00303-2. [DOI] [PubMed] [Google Scholar]
- 18.Ronning OM, Guldvog B. Stroke units versus general medical wards, I: twelve- and eighteen-month survival: a randomized, controlled trial. Stroke. 1998;29:58–62. doi: 10.1161/01.str.29.1.58. [DOI] [PubMed] [Google Scholar]
- 19.Hunt CM, Camargo CA, Dominitz JA. et al. Effect of postoperative complications on health and employment following liver transplantation. Clin Transplant. 1998;12:99–103. [PubMed] [Google Scholar]
- 20.Bruce J, Krukowski ZH, Al-Khairy G. et al. Systematic review of the definition and measurement of anastomotic leak after gastrointestinal surgery. Br J Surg. 2001;88:1157–1168. doi: 10.1046/j.0007-1323.2001.01829.x. [DOI] [PubMed] [Google Scholar]
- 21.Pronovost P, Garrett E, Dorman T. et al. Variations of complication rates and opportunities for improvement in quality of care for patients having abdominal aortic surgery. Arch Surg. 2001;386:249–256. doi: 10.1007/s004230100216. [DOI] [PubMed] [Google Scholar]
- 22.Lang M, Niskanen M, Miettinen P. et al. Outcome and resource utilization in gastrointestinal surgery. Br J Surg. 2001;88:1006–1014. doi: 10.1046/j.0007-1323.2001.01812.x. [DOI] [PubMed] [Google Scholar]
- 23.Ferguson TJ, Ferguson C, Crites K. et al. The additional hospital costs generated in the management of complications of pacemaker and defibrillator implantations. J Thorac Cardiovasc Surg. 1996;111:742–751. doi: 10.1016/s0022-5223(96)70334-3. [DOI] [PubMed] [Google Scholar]
- 24.Mason L, Garcia A. Hospital costs of surgical complications. Arch Surg. 1984;119:1065–1066. doi: 10.1001/archsurg.1984.01390210061013. [DOI] [PubMed] [Google Scholar]
- 25.Ferraris V, Ferraris S, Singh A. Operative outcome and hospital costs. J Thorac Cardiovasc Surg. 1998;115:593–603. doi: 10.1016/S0022-5223(98)70324-1. [DOI] [PubMed] [Google Scholar]
- 26.Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 27.McAleese P, Odling-Smee W. The effect of complications on length of stay. Ann Surg. 1994;220:740–744. doi: 10.1097/00000658-199412000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Collins T, Daley J, Henderson W. et al. Risk factors for prolonged length of stay after major elective surgery. Ann Surg. 1999;230:251–259. doi: 10.1097/00000658-199908000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]


