Abstract
Background
Physical functional decline is often the determining factor that leads to loss of independence in older persons. Identifying risk factors for physical disability may lead to interventions that may prevent or delay the onset of functional decline. Our study objective was to determine the association between hyperkyphotic posture and physical functional limitations.
Methods
Participants were 1578 older men and women from the Rancho Bernardo Study who had kyphotic posture measured as the distance from the occiput to table (units = 1.7-cm blocks, placed under the participant’s head when lying supine on a radiology table). Self-reported difficulty in bending, walking, and climbing was assessed by standard questionnaires. Physical performance was assessed by measuring grip strength and ability to rise from a chair without the use of the arms.
Results
Men were more likely to be hyperkyphotic than were women (p < .0001). In multiply adjusted comparisons, there was a graded stepwise increase in difficulty in bending, walking and climbing, measured grip strength, and ability to rise from a chair. For example, the odds ratio (OR) of having to use the arms to stand up from a chair increased from 1.6 (95% confidence interval [CI]: 0.9–3.0) for individuals defined as hyperkyphotic by 1 block to 2.9 (95% CI: 1.7–5.1) for individuals defined as hyperkyphotic by 2 blocks to 3.7 (95% CI: 2.1–6.3) for individuals defined as hyperkyphotic by ≥ 3 blocks compared to those who were not hyperkyphotic (p for trend < .0001).
Conclusions
Older persons with hyperkyphotic posture are more likely to have physical functional difficulties.
MAINTAINING physical functional ability is an important prerequisite for preserving independence in later life. Many studies have shown that being physically active is associated with less morbidity and mortality (1–3). In general, a physically active lifestyle should be promoted to maintain good health; however, there may be certain populations that are at particular risk for poor physical function and that could potentially benefit from early intervention. If risk factors for poor physical function can be identified before the onset of disability, targeted interventions for those at risk may potentially prevent or delay the onset of dependence.
Hyperkyphosis, or an increased thoracic curvature, is commonly observed in older persons and may be an important determinant of poor physical function. Of the studies that have investigated the association between hyperkyphosis and physical function, three of four found a strong association between having excess kyphosis and poor physical functioning, by self-reported and objective measures (4–7). However, most of these studies included a small number of participants and only one included men, probably because it is generally assumed that hyperkyphosis is more common in women.
Although most studies on hyperkyphosis have focused on women, men also suffer from postural changes with age (8,9) and little is known about how these postural changes might affect men’s overall health. To gain a better understanding of hyperkyphotic posture and its effects on physical function in a larger general population of older community-dwelling men and women, we assessed the association of hyper-kyphotic posture with self-reported and measured physical performance in 1578 older adults.
Methods
Participants
Between 1988 and 1992, surviving male and female participants aged 55 and over from the Rancho Bernardo Study were invited to participate in a study of osteoporosis. This population-based cohort study was first established in 1972 to study heart disease risk factors, and is comprised of older middle to upper-middle class white residents of Rancho Bernardo, a southern California community. Of those persons invited, 80% agreed to participate and provided informed, written consent. The Institutional Review Board of the University of California, San Diego, approved the study protocol.
Kyphotic Posture Measurement
During the 1988–1991 visit, participants were asked to lie flat on a radiology table, during which time the distance from the occiput to table was measured, similar to the measurement of the occiput to wall that is taken in the standing position (5). Hyperkyphotic individuals are unable to lie flat with their heads in a neutral position on a flat surface. If the participant was unable to lie flat with his or her head in a neutral position, 1.7-cm blocks were placed under the head until a neutral position was achieved (the participant’s head neither hyperextended nor hyperflexed) and with his or her eyes directed toward the ceiling (Figure 1).
Figure 1.
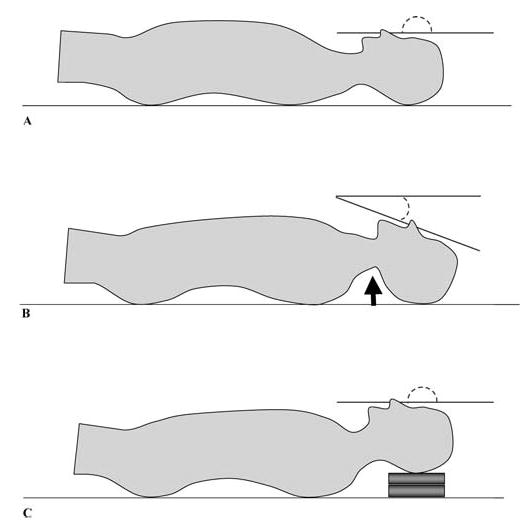
Measure of hyperkyphotic posture. A, Neutral head and neck position; B, hyperextended neck position; C, head on blocks restores neutral head and neck position.
Questionnaire
Study participants provided information on basic characteristics including age, sex, and educational level and gave a self-reported history of medical conditions including stroke, myocardial infarction, diabetes, chronic obstructive pulmonary disease, osteoarthritis, and osteoporotic fractures, of which those of the hip, spine, wrist, and clavicle were confirmed by medical review. Participants answered questions regarding health behaviors including smoking (current versus past or never), alcohol use (more than 12 drinks in the past year), and exercise (self-reported regular physical activity three times or more per week). Self-reported functional status was also assessed by asking the participants whether they had any difficulty bending over to the floor, walking 2–3 blocks on level ground, or climbing a flight of stairs.
Examinations
Between 1988 and 1992, bone mineral density (BMD) of the total hip, femoral neck, and lumbar spine was measured using dual-energy X-ray absorptiometry (QDR 1000; Hologic, Waltham, MA). Total hip BMD was determined by adding the bone mineral content of the femoral neck, intertrochanter, and greater trochanter and then dividing by the composite area of these three sites. Spine BMD was calculated by averaging the BMD of the lumbar vertebrae L1–L4. Using a phantom standard, daily calibration of the DXA scanner yielded measurement precisions of ≤1% for the spine and ≤1.5% for the hip. While the participant was wearing light clothing without shoes, height and weight were measured and body mass index was calculated as kilograms per meter squared. A handheld dynamometer (Therapeutic Instruments Hand Dynamometer; Clifton, NJ) was used to measure grip strength in each hand. Participants were also timed doing a chair stand exercise during which they were asked to stand up and sit down in a chair five times without using their arms. A categorical variable was created to classify participants as never having to use their arms versus those who had to use their arms at least some of the time while doing the chair stand exercise.
Statistical Analysis
The block measure of kyphotic posture had a range of values between 0 and 15. Because there were few individuals who had at least 3 blocks, the variable was categorized either as no blocks, 1 block, 2 blocks, or ≥3 blocks. Separate logistic regression age- and sex-adjusted analyses were performed to evaluate the odds of having self-reported difficulty in bending, walking, or climbing. For the performance-based measures, logistic regression was also used to determine the odds of being in the worst quartile of measured hand grip strength and to determine the odds of having difficulty in performing the chair stand exercise five times without the use of the arms. To test whether sex may modify the association between kyphosis and poor physical function, we checked for an interaction between sex, kyphosis, and each physical function measure.
To test for possible confounders of the association between hyperkyphotic posture and poor physical function, we considered a list of variables thought to be associated with both hyperkyphosis and poor physical function. We used chi-square or Student’s t tests as appropriate to test for significant associations between the candidate variable and either kyphotic posture or poor physical function (p < .10). If the candidate variable met the initial screening criteria of being significantly associated with both hyperkyphotic posture and poor physical function, it was added to a larger multivariable model and backward selection techniques (p < .10) were used to improve model fit. SAS software was used for all analyses (SAS Institute, Cary, NC).
Results
Selected characteristics of the study population are provided in Table 1 and include potential covariates that were associated with poor self-reported and measured physical function. The mean age of the participants was 73 years, and 59% were women. Although there was an average reported height loss of 4 cm, there were very few clinical spine fractures reported (<3%).
Table 1.
Selected Characteristics of Women and Men in the Study Sample
| Women (N = 827–937)* |
Men (N = 628–641)
|
|
|---|---|---|
| Characteristic | Mean (SD) or N (%) | Mean (SD) or N (%) |
| Age, y | 72.5 (9.6) | 73.2 (9.4) |
| Body mass index, kg/m2 | 24.6 (4.0) | 26.1 (3.4) |
| Height, cm | 159.4 (6.1) | 173.7 (6.5) |
| Weight, kg | 62.5 (11.2) | 78.7 (11.9) |
| Alcohol use in past mo., % yes | 681 (73.8) | 524 (82.5) |
| Spine BMD, g/cm2 | 0.90 (0.48) | 1.07 (0.20) |
| Hip BMD, g/cm2 | 0.79 (0.15) | 0.94 (0.16) |
| Clinical spine fracture, % yes | 46 (4.5) | 22 (3.2) |
| Arthritis, % yes | 324 (34.6) | 203 (31.7) |
| Current smoker, % yes | 103 (11.1) | 53 (8.3) |
Notes: Sample sizes vary due to missing values.
BMD = bone mineral density.
Using the block method of measuring kyphotic posture, we found that men were more likely to be hyperkyphotic than were women regardless of the cutoff definition used (Table 2). Our lowest cutoff point was one 1.7-cm block; with this cutoff, 21% of the women and 44% of the men were hyperkyphotic. Eight percent of the women and 14% of the men required one block to achieve a neutral head position, 7% of the women and 11.4% of the men required two blocks, and 6.3% of the women and 18.3% of the men required three or more blocks.
Table 2.
Distribution of Kyphotic Posture, by Sex
| Women (N = 937)
|
Men (N = 641)
|
|
|---|---|---|
| No. of Blocks* | Frequency (%) | Frequency (%) |
| 0 | 739 (78.9) | 360 (56.2) |
| 1 | 74 (7.9) | 91 (14.2) |
| 2 | 65 (6.9) | 73 (11.4) |
| 3 | 25 (2.7) | 57 (8.9) |
| 4 | 12 (1.3) | 27 (4.2) |
| 5 | 10 (1.1) | 14 (2.2) |
| 6 | 9 (0.96) | 10 (1.6) |
| 7 or more | 3 (0.33) | 9 (1.4) |
Note: Occiput-to-table distance was measured in number of 1.7 cm blocks.
In age- and sex-adjusted analyses, greater kyphotic posture was associated with increasing odds of having difficulty in each of the physical functional measures examined (p for trend < .0001) (Figure 2). For example, compared to those who required no blocks, persons who required 2 or more blocks had a 2.1- to 2.7-fold increased odds of reporting difficulty in bending, walking, and/or climbing, whereas those who required 3 or more blocks had a 2.0- to 3.7-fold increased odds of reporting difficulty in these activities. There was no evidence that sex modified the association between kyphotic posture and each physical function measure.
Figure 2.
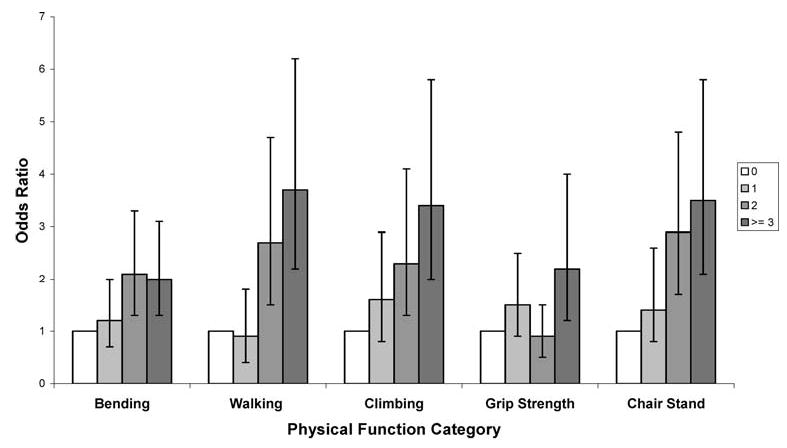
Age and sex adjusted analyses of kyphotic posture and odds of having poor physical functional ability. Reported as odds ratios with 95% confidence intervals. All p for trends < .0001 except for grip strength which had a p for trend = .048.
Examining performance-based measures revealed similar results (Figure 2). For grip strength, the trend was weaker but still statistically significant (p for trend = .048); those persons who required 3 or more blocks had a 2.2-fold increased odds of being in the lowest quartile of grip strength. The results for the chair stand measure were stronger. The odds ratio of having to use the arms during the chair stand exercise increased from 1.4 for those who had hyperkyphotic posture defined as 1 block to 2.9 for those with more hyperkyphotic posture defined as 2 blocks to 3.5 for those who had the most hyperkyphotic posture defined as ≥3 blocks compared to those who required no blocks to achieve a neutral head position.
In multivariable models, the odds of reporting poor physical function in any of the three categories were statistically significantly associated with greater kyphosis. All models were age, sex, and weight adjusted; however, covariate screening and the backward selection procedure resulted in the inclusion of spine BMD, alcohol use, smoking status, or height in individual models (Table 3). After adjusting for age, sex, weight, and spine BMD, the odds of difficulty bending ranged from 1.17 to 1.80 with increasing number of blocks from 1 to ≥3 (p for trend = .003). Likewise, for difficulty in walking, the odds ranged from 0.77 to 3.35 in models adjusted for age, sex, weight, and alcohol use (p for trend = .0001). For difficulty in climbing, the odds ranged from 1.6 to 3.07 in models adjusted for age, sex, weight, and smoking status (p for trend = .0001).
Table 3.
Multivariable Models of Hyperkyphotic Posture and Impaired Physical Function*
| No. of Blocks | Bending‡ | Walking§ | Climbing|| | Grip Strength¶ | Chair Stand# |
|---|---|---|---|---|---|
| 0† | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| 1 | 1.2 (0.7–2.0) | 0.8 (0.4–1.7) | 1.5 (0.8–2.7) | 1.5 (.9–2.6) | 1.6 (0.9–3.0) |
| 2 | 1.9 (1.2–3.1) | 2.5 (1.4–4.4) | 2.1 (1.2–3.7) | 0.8 (0.5–1.5) | 2.9 (1.7–5.1) |
| ≥3 | 1.8 (1.1–2.9) | 3.4 (2.0–5.7) | 3.1 (1.8–5.3) | 2.1 (1.1–3.9) | 3.7 (2.1–6.3) |
| p for trend | .003 | .0001 | .0001 | .10 | .0001 |
Reported as odds ratios and 95% confidence intervals.
Reference group.
Adjusted for age, sex, weight, and spine bone mineral density.
Adjusted for age, sex, weight, and alcohol use.
Adjusted for age, sex, weight, and smoking status.
Adjusted for age, sex, weight, and height. The outcome is being in the bottom quartile of grip strength.
Adjusted for age, sex, weight, height, and hip bone mineral density. The outcome is having any difficulty arising up from a chair five times without the use of the arms.
Greater kyphosis was also related to measured physical performance (Table 3). After adjusting for age, sex, height, and weight, the odds of being in the lowest quartile of hand grip ranged from 1.5 to 2.1 (p for trend = .10). For the chair stand exercise, the results remained strong and significant after adjusting for age, sex, height, weight, and hip BMD, with odds ranging from 1.59 to 3.66 (p for trend = .0001).
Discussion
In this cohort, older men and women with hyperkyphotic posture were more likely to have self-reported difficulty in bending, walking, and/or climbing; worse measured hand grip; and more trouble performing the chair stand exercise five times without using their arms. Furthermore, the odds of having difficulty in each of these measures increased, in a dose-dependent manner, with worsening kyphotic posture. Regardless of the physical function outcome studied, the association between hyperkyphotic posture and poorer function was remarkably consistent and independent of age, sex, body size, BMD, clinical spinal fractures, other comorbidities, and health-related behaviors.
These results are concordant with those of previous studies that reported a cross-sectional association between hyperkyphosis and impaired physical function (4–6). In the sole prior study that found no significant association between kyphosis and self-reported activity level (7), the study sample was small and very high functioning so that there might not have been enough variability to detect significant differences. To date, the Rancho Bernardo Study is the largest cohort study reporting the effects of clinical hyperkyphosis on physical function.
In the present study, older men were approximately twice as likely as women to be classified as having hyperkyphotic posture based on a simple clinical measurement. These findings are in contrast to the commonly held belief that hyperkyphosis is more prevalent in older women than men, and are likely due to differences in the kyphosis measurement method. Whereas the traditional radiologic measurement of kyphosis angle includes only the thoracic spine (approximately T4–T12), clinical measurements such as the measure we used incorporate some of the cervical spine curvature because the measurement begins at the occiput or lower cervical spine (5,6). Men in our study may have been classified as hyperkyphotic more than women because the block measurement includes the cervical lordotic curvature that tends to flatten with age, particularly in males (9).
Hyperkyphosis is thought to result mainly from underlying vertebral fractures, and has not gained much clinical interest other than as a marker for osteoporosis. Previous studies (10,11) have reported that some of those individuals with the most severe hyperkyphosis have no evidence of underlying vertebral fractures. Moreover, those persons with hyperkyphosis and no spinal deformity suffer a similar degree of physical and emotional impairments as do those persons who have hyperkyphosis and underlying vertebral deformities (5). Similarly, women who report height loss of >5 cm or kyphosis, without prior fracture, have significantly more physical difficulty and more adaptations to their lives as a result of physical disability than do women who reported only a prior fracture and no postural changes (12). Likewise, the results of our study reveal that hyperkyphotic posture is associated with poor physical function, independent of spine or hip BMD and clinical spine fractures. Although vertebral fractures can lead to substantial height loss and postural deformities, there are clearly other poorly defined causes.
Why might hyperkyphosis be associated with physical functional limitations? With increased kyphotic posture, the resultant thoracic deformation that occurs is associated with a restrictive ventilatory defect (10), and impaired pulmonary function can limit physical functional ability. It is also hypothesized that hyperkyphosis may lead to changes in balance that presumably could lead to worse physical function, but this remains to be definitively shown (13). An alternative explanation may be that hyperkyphosis is a marker for an increased rate of physiologic aging. Several mouse knockout models have been developed in which the affected mice demonstrate an increased rate of aging and hyperkyphosis (14–17). In humans, accelerated physiologic aging might occur through dysregulated stress responses and/or underlying inflammation, both of which are associated with decline in physical function. A high allostatic load, or cumulative measure of dysregulation across multiple physiologic systems, is an independent predictor of physical functional decline (18). Similarly, high levels of interleukin 6, a marker of inflammation, are associated with the development of disability in older persons (19).
There are some limitations to our study. First, it was cross-sectional, so we are unable to determine the direction of the association. Although it seems intuitive that hyperkyphotic posture may precede difficulties in physical function, this remains to be shown in a prospective study. Second, we used a novel measure of kyphotic posture that required participants to be in a supine position. Because gravity can affect standing posture, the supine measure may underestimate the true degree of hyperkyphosis; even so, we were able to demonstrate strong and consistent associations with poor physical function. Furthermore, this measure has been shown to be associated with other adverse outcomes (20,21), suggesting that it has construct validity.
Our study also possesses some strengths. First, it included both community-dwelling older men and women. Second, it used both self-reported as well as objective measures of physical function. Lastly, it used a measure of clinical hyperkyphosis that is inexpensive and simple to perform, and could potentially be applied in a clinical setting.
As the percentage of older persons increases in the population, more and more emphasis is being placed on healthy aging, and an integral part of aging successfully is maintaining physical functional ability. Our study demonstrates a strong and graded association between worsening hyperkyphotic posture and poor self-reported and measured physical function. We conclude that hyperkyphotic posture affects both older men and women and that it is a marker of poor health. Whether preventing or treating hyperkyphotic posture improves health outcomes remains unknown.
Acknowledgments
Supported by Public Health Service Grants AG007181-15, 1K12AG01004, and 1-RO1 AG024246-01, and by the Claude D. Pepper Older Americans Independent Center (5P60AG10415-11).
This abstract was presented at the annual meeting of the American Geriatrics Society, Washington, D.C., May 10, 2002.
Footnotes
Decision Editor: John E. Morley, MB, BCh
References
- 1.Sandvik L, Erikssen J, Thaulow E, et al. Physical fitness as a predictor of mortality among healthy, middle-aged Norwegian men. N Engl J Med. 1993;328:533–537. doi: 10.1056/NEJM199302253280803. [DOI] [PubMed] [Google Scholar]
- 2.Fried LP, Kronmal RA, Newman AM, et al. Risk factors for 5-year mortality in older adults. JAMA. 1998;279:585–592. doi: 10.1001/jama.279.8.585. [DOI] [PubMed] [Google Scholar]
- 3.Rockhill B, Willett WC, Manson JE, et al. Physical activity and mortality: a prospective study among women. Am J Public Health. 2001;91:578–583. doi: 10.2105/ajph.91.4.578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chow RK, Harrison JE. Relationship of kyphosis to physical fitness and bone mass on post-menopausal women. Am J Phys Med. 1987;66:219–227. [PubMed] [Google Scholar]
- 5.Leidig-Bruckner G, Minne HW, Schlaich C, et al. Clinical grading of spinal osteoporosis: quality of life components and spinal deformity in women with chronic low back pain and women with vertebral osteoporosis. J Bone Miner Res. 1997;12:663–675. doi: 10.1359/jbmr.1997.12.4.663. [DOI] [PubMed] [Google Scholar]
- 6.Ryan SD, Fried LP. The impact of kyphosis on daily functioning. J Am Geriatr Soc. 1997;45:1479–1486. doi: 10.1111/j.1532-5415.1997.tb03199.x. [DOI] [PubMed] [Google Scholar]
- 7.Eagan MSS, Sedlock DA. Kyphosis in active and sedentary post-menopausal women. Med Sci Sports Exerc. 2001;33:688–695. doi: 10.1097/00005768-200105000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Milne JS, Williamson J. A longitudinal study of kyphosis in older people. Age Ageing. 1983;12:224–233. doi: 10.1093/ageing/12.3.225. [DOI] [PubMed] [Google Scholar]
- 9.Boyle JJW, Milne N, Singer KP. Influence of age on cervicothoracic spinal curvature: an ex vivo radiographic survey. Clin Biomechanics. 2002;17:361–367. doi: 10.1016/s0268-0033(02)00030-x. [DOI] [PubMed] [Google Scholar]
- 10.Leech JA, Dulberg C, Kellie S, et al. Relationship of lung function to severity of osteoporosis in women. Am Rev Respir Dis. 1990;141:68–71. doi: 10.1164/ajrccm/141.1.68. [DOI] [PubMed] [Google Scholar]
- 11.Kado DM, Browner WS, Palermo L, et al. Vertebral fractures and mortality in older women. Study of Osteoporotic Fracture Research Group. Arch Intern Med. 1999;159:1215–1220. doi: 10.1001/archinte.159.11.1215. [DOI] [PubMed] [Google Scholar]
- 12.Martin AR, Sornay-Rendu E, Chandler JM, et al. The impact of osteoporosis on quality-of-life: the OFELY Cohort. Bone. 2002;31:32–36. doi: 10.1016/s8756-3282(02)00787-1. [DOI] [PubMed] [Google Scholar]
- 13.O’Brien K, Culham E, Pickles B. Balance and skeletal alignment in a group of elderly female fallers and nonfallers. J Gerontol Med Sci. 1997;52:B221–B226. doi: 10.1093/gerona/52a.4.b221. [DOI] [PubMed] [Google Scholar]
- 14.de Boer J, Andressoo JO, de Wit J, et al. Premature aging in mice deficient in DNA repair and transcription. Science. 2002;296:1276–1279. doi: 10.1126/science.1070174. [DOI] [PubMed] [Google Scholar]
- 15.Tyner SD, Venkatachalam S, Choi J, et al. p53 mutant mice that display early ageing-associated phenotypes. Nature. 2002;415:45–53. doi: 10.1038/415045a. [DOI] [PubMed] [Google Scholar]
- 16.Vogel H, Lim SD, Karsenty G, et al. Deletion of Ku86 causes early onset of senescence in mice. Proc Natl Acad Sci U S A. 1999;96:10770–10775. doi: 10.1073/pnas.96.19.10770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kuro-o M, Matsumura Y, Aizawa H, et al. Mutation of the mouse klotho gene leads to a syndrome resembling aging. Nature. 1997;390:45–51. doi: 10.1038/36285. [DOI] [PubMed] [Google Scholar]
- 18.Karlamangla A, Singer BH, McEwen BS, et al. Allostatic load as a predictor of functional decline. MacArthur Studies of successful aging. J Clin Epidemiol. 2002:696–710. doi: 10.1016/s0895-4356(02)00399-2. [DOI] [PubMed] [Google Scholar]
- 19.Ferrucci L, Harris TB, Guralnik JM, et al. Serum IL-6 and the development of disability in older persons. J Am Geriatr Soc. 1999;47:630–646. doi: 10.1111/j.1532-5415.1999.tb01583.x. [DOI] [PubMed] [Google Scholar]
- 20.Greendale GA, Huang M, Barrett-Connor E. Kyphotic posture and impaired pulmonary function: The Rancho Bernardo Study. J Am Geriatr Soc. 2002;50:S150. [Google Scholar]
- 21.Kado DM, Huang M, Karlamangla A, et al. Hyperkyphotic posture predicts mortality in older community-dwelling men and women in a prospective study. J Am Geriatr Soc. 2004;52:1662–1667. doi: 10.1111/j.1532-5415.2004.52458.x. [DOI] [PubMed] [Google Scholar]


