Abstract
Salmonella enterica serovar Typhimurium mutants with mutations in the ompS1 and ompS2 genes, which code for quiescent porins, were nevertheless highly attenuated for virulence in a mouse model, indicating a role in pathogenesis. Similarly, a strain with a mutation in the gene coding for LeuO, a positive regulator of ompS2, was also attenuated.
Salmonella enterica serovar Typhimurium pathogenesis is a complex multifactorial process that results from the activities of many bacterial gene products. It has been estimated that at least 4% of its genome is involved in virulence, and both in vitro and in vivo models have been used to better understand the infectious process (5, 17).
The ompC and ompF genes encode the two major porins of Escherichia coli and S. enterica. In S. enterica serovars Typhi and Typhimurium, the ompS1 and ompS2 genes code for two other porins that are expressed at very low levels, relative to the major porins OmpC and OmpF, under standard laboratory conditions. As for OmpC and OmpF, OmpS1 and OmpS2 are regulated by the EnvZ/OmpR two-component signal transduction system. In addition, ompS1 is negatively regulated by the HN-S nucleoid protein, and ompS2 is positively regulated by the LeuO regulator (10, 11, 26, 27).
Porins have been shown to trigger multiple synergistic signal transduction pathways in Salmonella infections, as they induce cellular activation, cytokine release, and the activation of protein tyrosine kinase, protein kinase A, and protein kinase C (14, 16). A role for the S. enterica serovar Typhimurium OmpC protein in initial recognition by macrophages and the distinction of regions of this protein that potentially participate in host cell recognition of bacteria by phagocytic cells have been documented (25). In addition, OmpS1 appears to have a role in the Salmonella life cycle, since mutations causing defects in swarming motility and biofilm formation have been found to map in S. enterica serovar Typhimurium ompS1 (32, 34). Moreover, vaccination of mice with S. enterica serovar Typhi and Typhimurium porins confers protective immunity against live bacteria (18, 21, 24), and specific humoral and cellular immune responses are mounted against S. enterica serovar Typhi outer membrane proteins in typhoid fever patients, which has allowed the design of novel diagnostic assays (1, 6, 33).
It has been reported that porins play a role in virulence. For Shigella flexneri, both ΔompB (ΔompR envZ) and ΔompC mutants were affected in two key steps for pathogenesis, i.e., in spreading from one epithelial cell to another and in host cell killing (2, 3). For S. enterica serovar Typhimurium, mutants lacking the ompR gene and a double ompF ompC mutant showed increased oral 50% lethal doses (LD50), by >1,600- and 300-fold, respectively, relative to the wild type. Interestingly, a single ompF or single ompC mutant did not show attenuation (7, 9). Furthermore, ompR mutants were not cytotoxic to macrophages (23). Moreover, the EnvZ/OmpR two-component system has been shown to regulate Salmonella pathogenicity island 2 (15, 19, 22).
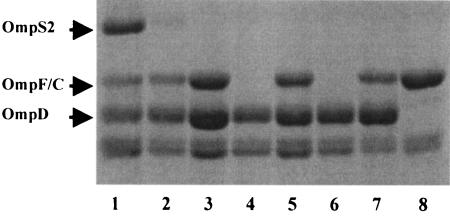
To define the role of the ompS1 and ompS2 genes in serovar Typhimurium regarding virulence, we constructed mutants (Table 1) of Salmonella in which the ompS1 and ompS2 genes were deleted by a one-step nonpolar gene inactivation procedure and replaced with selectable antibiotic resistance gene markers (8). The same procedure was used to obtain deletions of ompR, envZ, and leuO (Table 1). The antibiotic resistance gene was generated by PCR by using primers with 42-nucleotide homology extensions, and different primer sets were used to verify the presence of the antibiotic resistance gene cassette for kanamycin or chloramphenicol (Kmr and Cmr, respectively) and of junctional sequences in the mutant, as described previously (8) (Table 2). The ompS2 mutant was further characterized by the lack of induction of the OmpS2 porin in the presence of the cloned LeuO positive regulator (Fig. 1, lane 2). In contrast, the expression of LeuO from a cloned plasmid rendered OmpS2 expression in the wild-type control, as previously observed for S. enterica serovar Typhi (Fig. 1, lane 1) (10). The ompS1 mutant was not verified in this manner, as there is no known positive regulator that causes its overexpression (11). Furthermore, both the ompR and envZ mutants lacked the presence of the OmpC and OmpF porins, which were restored upon complementation solely with the corresponding ompR and envZ cloned genes, respectively (Fig. 1, lanes 4 to 7). This observation particularly illustrated the nonpolar effects generated by the technique of Datsenko and Wanner (8), as the ompR and envZ genes are in close proximity, forming the ompB operon.
TABLE 1.
S. enterica serovar Typhimurium strains and plasmids used for this study
| Strain or plasmid | Genotype and/or relevant marker(s) | Reference or source |
|---|---|---|
| Strains | ||
| ATCC 14028 | Wild type (Spr) | American Type Culture Collection |
| STMS14 | ATCC 14028 ΔompS1::Km | This study |
| STMS23 | ATCC 14028 ΔompS2::Km | This study |
| STMR | ATCC 14028 ΔompR::Km | This study |
| STMZ | ATCC 14028 ΔenvZ::Cm | This study |
| STMLEUO1 | ATCC 14028 ΔleuO::Km | This study |
| STMS23S15 | STMS23 ΔompS1::Cm | This study |
| STMD | ATCC 14028 ΔompD::Km | This study |
| STMA1 | ATCC 14028 ΔinvA::Cm | This study |
| Plasmids | ||
| pKD46 | oriR101ts, λ Red recombinase system under paraB promoter control; Ampr | 8 |
| pKD4 | pANTSγ derivative containing an FRT-flanked Kmr gene from pCP15 | 8 |
| pKD3 | pANTSγ derivative containing an FRT-flanked Cmr gene from pSC140 | 8 |
| pFMtrc12 | P15A1 lacI trcp Apr | 10 |
| pFMtrcleuO | Vector pFMtrc12-derived plasmid carrying the leuO gene | 10 |
| pFM2001 | Vector pACYC184-derived plasmid carrying the ompR gene | This study |
| pROZ | Vector pMPMA6-derived plasmid carrying the envZ gene | This study |
TABLE 2.
Oligonucleotide primers used for this study
| Primer | Sequence (5′-3′) |
|---|---|
| Primers for mutant constructiona | |
| ompS1-H1P1 | ATAATGAACAGAAAAGTTCTGGCACTGCTTGTCCCGGCGTTATTGTAGGCTGGAGCTGCTTCG |
| ompS1-H2P2 | TTAGAACTGGTAGACCAGACCAACACCTACGATATCATCGGTCATATGAATATCCTCCTTAG |
| ompS2-H1P1 | GATAAAAAAATGAAAAGAAAAGTATTGGCACTTGTCATCCTGTAGGCTGGAGCTGCTTCG |
| ompS2-H2P2 | GAATAATTAGAACTGGTAAACCATACCCAGCGCGACGATATCCATATGAATATCCTCCTTAG |
| envZ-H1P1 | GCCCGCACGCTGTTGCTCATCGTCACCTTGCTGTTCGTCATGTAGGCTGGAGCTGCTTCG |
| envZ-H2P2 | TCCCCTGGACGCGAGCCACAGGAACCGGTAGCCAGGCGCGCATATGAATATCCTCCTTAG |
| ompR-H1P1 | GAGAATTATAAGATTCTGGTGGTTGATGACGATATGCGTCTGTGTAGGCTGGAGCTGCTTCG |
| ompR-H2P2 | GACGTAGCCCAGGCCCCATACGGTCTGAATATAACGCGGCATATGAATATCCTCCTTAG |
| leuO-H1P1 | AAAACCGAAAAGCCGCATCTTTTAGATATGGGCAAACCACTGTAGGCTGGAGCTGCTTCG |
| leuO-H2P2 | TATCGCTTACAAACAGAGACTAATAAATCTTCCATCCATTCATATGAATATCCTCCTTAG |
| ompD-H1P1 | TTGAGGAAACACGCTAAGAAAATTATAAGGATTATTAAAATGTGTAGGCTGGAGCTGCTTCG |
| ompD-H2P2 | CCCTGAAAGGACTGGCTTTGTATTCAGACTACAACAAAATTACATATGAATATCCTCCTTAG |
| invA-H1P1 | CTATAGTGCTGCTTTCTCTACTTAACAGTGCTCGTTTACGACCTGTAGGCTGGAGCTGCTTCG |
| invA-H2P2 | CCTTATATTGTTTTTATAACATTCACTGACTTGCTATCTGCTACATATGAATATCCTCCTTAG |
| Primers for mutant verificationb | |
| k1 | CAGTCATAGCCGAATAGCCT |
| k2 | CGGTGCCCTGAATGAACTGC |
| kt | CGGCCACAGTCGATGAATCC |
| c1 | TTATACGCAAGGCGACAAGG |
| c2 | GATCTTCCGTCACAGGTAGG |
| ompS1-F | CATAATCAAAGCATCAAATAC |
| ompS1-R | CATCCATCATCTATAGTGGCA |
| ompS2-F | ACATAATAACAAATATATTCACCATAAATA |
| ompS2-R | TCTGTGCCCAGGGAACTGTGCGTTCTGTT |
| envZ-F | ATGAGGCGAATGCGCTTCTC |
| envZ-R | GCGCCGGACCGAAGCTGTAA |
| ompR-F | CATAACGTGATCGTCCCGACA |
| ompR-R | TAACTGCGTGCCGTCCTCCAG |
| leuO-F | CATTATGAATCGCAATGGTGTGAC |
| leuO-R | TTACGCCTTGATCGATAAGCGATC |
| ompD-F | CAGTCCCTATTTGAATTAATAC |
| ompD-R | CATAGACATCCAGCATTTCGA |
| invA-F | GATATTGCCTACAAGCATGAAATGG |
| invA-R | AAATGTTGCATAGATCTTTTCCTTA |
FIG. 1.
Sodium dodecyl sulfate-polyacrylamide gel showing outer membrane protein profiles for various S. enterica serovar Typhimurium strains. Lanes: 1, STM14028 (wild type)/pFMtrcleuO (plus 50 μM IPTG [isopropyl-β-d-thiogalactopyranoside]); 2, STMS23 (ΔompS2::Km)/pFMtrcleuO (plus 50 μM IPTG); 3, STM14028 (wild type)/pFMtrc12 (plus 50 μM IPTG); 4, STMR (ΔompR::Km); 5, STMR (ΔompR::Km)/pFM2001 (ompR); 6, STMZ (ΔenvZ::Cm); 7, STMZ (ΔenvZ::Cm)/pROZ (envZ); and 8, STMD (ΔompD::Km).
There were no observable differences between the wild-type strain and the isogenic ompS1 and ompS2 mutants of S. enterica serovar Typhimurium in growth rates in LB or nutrient broth at a low or high osmolarity, in RPMI medium, or in Dulbecco's modified Eagle's medium (data not shown).
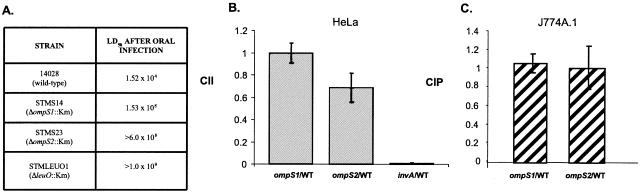
S. enterica serovar Typhimurium ompS1 and ompS2 mutants were compared with the wild-type strain, 14028, in a mouse model of infection. For inoculation, bacteria were grown in LB with shaking to an optical density at 540 nm of 0.6. Groups of six innately Salmonella-susceptible 6- to 8-week-old female BALB/c mice (Harlan Sprague-Dawley Inc., Mexico) were inoculated orally with serial 10-fold dilutions of bacteria, and deaths were recorded over the following 28 days. Thirty minutes prior to oral infection, the gastric pH was neutralized by oral administration of 0.1 ml of 1% sodium bicarbonate. LD50s were calculated by the method of Reed and Muench (28) in three to four repetitions. Mice inoculated with only phosphate-buffered saline (pH 7.4; PBS) were used as controls. S. enterica serovar Typhimurium strains STMS14 (ΔompS1::Km), STMS23 (ΔompS2::Km), and STMLEUO1 (ΔleuO::Km) were highly attenuated for oral infection (Fig. 2A).
FIG. 2.
Phenotypes of S. enterica serovar Typhimurium STMS14 (ΔompS1::Km) and STMS23 (ΔompS2::Km) mutant strains. (A) LD50s of S. enterica serovar Typhimurium strains in BALB/c mice after oral infection. The values are the means of three to four independent experiments. The LD50 of the mutant with a deletion of the gene for LeuO, the positive regulator of ompS2, is also shown. (B) CII of mutants upon mixed infection with the wild-type strain in cultured HeLa cells. The CII was calculated by obtaining the ratio between the two strains in the output (intracellular bacteria recovered 3 h after infection) and dividing it by their ratio in the input (initial mixed inoculum). (C) CIP upon mixed infection of the J774.A1 macrophage line with either the STMS14 or the STMS23 mutant and the wild type. The CIP was calculated by obtaining the ratio between the two strains 24 h after infection and dividing it by their ratio 1 h 5 min after infection. For panels B and C, all values are means ± standard deviations of at least two experiments done in triplicate (P < 0.001 by Student's t test).
To begin to understand the basis of the attenuation, mixed oral and mixed intraperitoneal infections (IPI) of mice were performed to establish a competitive index (CI) between the wild type and each particular mutant (4). Groups of six mice were inoculated either orally or intraperitoneally with 0.3 ml of an equal mixture of the strains, with total inocula of 108 and 105 bacteria, respectively. Mice were euthanized 6 and 3 days after oral and intraperitoneal infections, respectively, and spleens and livers were collected. Organs were homogenized in 5 ml of PBS. Resuspended cells were lysed by the addition of an equal volume of 0.5% sodium deoxycholate in PBS and incubated at room temperature for 15 min. Dilutions of cell lysates were plated on LB agar plates both with Km (40 μg/ml) or Cm (25 μg/ml) for enumeration of the CFU/mg of organ for the mutant strain and without antibiotics for enumeration of the mixture of the mutant and wild-type strains. CIs were calculated as described previously (4).
As shown in Table 3, the CIs in spleens and livers after oral infection for the ompS1 and ompS2 mutants indicated >250-fold reductions in survival, with 4- to 5-fold reductions in both spleens and livers after IPI. Furthermore, attenuation of the double ΔompS1::Cm ΔompS2::Km (STMS23S15) mutant was the predicted combined effect of the single mutations, suggesting that each mutation results in the loss of independent functions (Table 3). In addition, both the ompS1 and ompS2 mutants were impaired in the ability to cause bacteremia at an early time after infection (2 days), with CIs of <1 × 10−4. These results point towards a role of the ompS1 and ompS2 genes mainly in the initial stages of infection, since the virulence of these strains was not as severely compromised during IPI.
TABLE 3.
Competitive indices of mixed oral and mixed intraperitoneal S. enterica serovar Typhimurium infections in BALB/c mice
| Mutant mixed with wild type | Infection routea | CI of infection in indicated organb
|
|
|---|---|---|---|
| Spleen | Liver | ||
| ompS1 | Oral | 3.8 × 10−3 ± 1.0 × 10−3 | 3.8 × 10−3 ± 1.2 × 10−3 |
| i.p. | 0.25 ± 0.11 | 0.28 ± 0.17 | |
| ompS2 | Oral | 3.4 × 10−3 ± 9.0 × 10−4 | 2.6 × 10−3 ± 9.3 × 10−4 |
| i.p. | 0.19 ± 0.11 | 0.26 ± 0.12 | |
| envZ | Oral | 2.3 × 10−5 ± 9.0 × 10−6 | 2.6 × 10−5 ± 1.7 × 10−5 |
| i.p. | 4.8 × 10−4 ± 1.4 × 10−4 | 6.8 × 10−4 ± 3.2 × 10−4 | |
| ompR | Oral | 6.6 × 10−6 ± 5.7 × 10−6 | 8.7 × 10−6 ± 9.0 × 10−6 |
| i.p. | 2.2 × 10−4 ± 4.2 × 10−5 | 4.4 × 10−4 ± 4.0 × 10−4 | |
| leuO | Oral | 2.0 × 10−3 ± 1.3 × 10−3 | 1.0 × 10−3 ± 1.1 × 10−3 |
| i.p. | 0.12 ± 0.051 | 0.11 ± 0.041 | |
| ompS1 ompS2 | Oral | 3.4 × 10−5 ± 1.6 × 10−5 | 2.5 × 10−5 ± 2.4 × 10−5 |
| i.p. | 9.0 × 10−3 ± 3.0 × 10−3 | 1.3 × 10−2 ± 1.0 × 10−2 | |
Organs from oral infections were collected at 6 days postinoculation; organs from IPI infections were collected at 3 days postinoculation.
The CI was calculated as the ratio between the mutant strain and the wild type in the output divided by the ratio of the two strains in the input. All values are means ± standard deviations of at least two independent experiments. Differences between the wild type and each mutant were statistically significant (P < 0.001) by Student's t test.
Bacterial shedding was determined by measuring the proportions of the wild type and the ompS1, ompS2, or ompS1 ompS2 mutant in the feces after mixed oral inoculation as described above. Both the wild type and the mutants were shed in equal numbers at 1, 4, 8, 12, and 24 h postinfection: shedding was maximal at 4 h, at 3 × 104 ± 1 × 104 per mg of feces. The shed Salmonella cells were identified on MacConkey plates by the use of spectinomycin, and the mutants were identified by the use of spectinomycin and kanamycin. The identity of the shed Salmonella was further verified by streaking onto LB plates with the appropriate antibiotics. Groups of four mice were used for each mixed inoculation, and the experiment was done twice. In accordance with the shedding experiments, no particular sensitivity of the ompS1, ompS2, or double ompS1 ompS2 mutant was observed to a battery of stress factors compared to the wild type. The stress factors tested were as follows: lactic acid, 0.1 to 0.5%; pH, 3.5 to 6; bile salts, 3 to 7.5%; polymyxin B, 1 to 3 μg/ml; propionate, butyrate, and acetate, 50 to 200 mM; and deoxycholate or Triton X-100, 0.1 to 0.5%. Thus, attenuation of these mutants does not appear to be due to reduced survival in the gastrointestinal tract.
The CIs for the envZ and ompR mutants showed about 40,000- and 120,000-fold reduced abilities to colonize both the spleen and liver after oral infection, respectively, and about a 3,000-fold reduction after IPI (Table 3). Hence, the ompR mutant behaved as in previous studies, being highly attenuated in accordance with the proposed pleiotropic role for the OmpR regulator (7, 9, 19, 22, 23). Interestingly, the envZ mutant was also highly attenuated, indicating that it is the main phosphorylase for OmpR and that phosphorylation by other regulators or by acetyl-phosphate is not as relevant in vivo, in agreement with studies of the regulation of the ssrAB genes in Salmonella pathogenicity island 2 (19). Complementation in mice of the phenotypes of the ompS1 and ompS2 mutants was not feasible, although it was possible for bacteria grown in laboratory media (Fig. 1), since the vector plasmids were not stable in the host. Thus, future studies are aimed at generating stable constructs that will allow such complementation in the mice, although the technique of Datsenko and Wanner (8) has been designed to avoid polar effects.
Strains 14028 (wild type), STMS14 (ΔompS1::Km), and STMS23 (ΔompS2::Km) were used in mixed infections in vitro to determine the competitive indices of invasion (CII) of the human epithelial HeLa cell line (ATCC CCL-2) and in survival/proliferation (CIP) in the murine phagocytic cell line J774.A1 (ATCC TIB-67) (29). Invasion assays were done with a modified version of a previously described gentamicin protection assay (30), using 5 × 104 cells per well (90% confluent). Bacteria were grown under low-oxygen conditions and collected at the early/mid-logarithmic growth phase (optical density at 590 nm, ∼0.2) as described previously (12, 20). A 1:1 mixture of the mutant and wild-type bacterial strains was applied at a multiplicity of infection of 100. For the survival/proliferation assay, a 1:1 mixture of two bacterial strains was prepared in PBS and added to the macrophages at a multiplicity of infection of 10 (30). As shown in Fig. 2B, no significant differences were observed between the mutants and the wild type regarding epithelial cell invasion compared with the invA mutant (STMA1 strain), which was severely impaired (13). Likewise, no difference was observed regarding survival/proliferation in mouse macrophages (Fig. 2C).
Thus, the attenuated phenotypes in the host were not evident upon assays in vitro. In this respect, the observations presented here are similar to those of other studies, where some S. enterica serovar Typhimurium mutants have been identified as being attenuated intraperitoneally and intragastrically yet show comparable invasion of cultured epithelial cells and survival in macrophages to those of the wild-type strain (5).
In agreement with the role of LeuO as a positive regulator of ompS2 expression, it also appears to play a role in the initial stages of infection (Table 3). The CIs for the leuO mutant indicated 500- to 1,000-fold reduced survival in the spleen and liver, respectively, after oral infection and a <10-fold reduced survival after IPI in both the spleen and liver. However, it remains to be seen if LeuO regulates the expression of other genes required for the initial virulence events during Salmonella infection. This is in accordance with the recent identification of LeuO as a virulence factor in the Caenorhabditis elegans model of Salmonella infection (31).
Acknowledgments
We acknowledge Irma Martínez-Flores for her advice and help during the initial stages of this work, Armando Isibasi and Ismael Secundino for helping us to set up the virulence assays in mice, and Ricardo Oropeza for plasmid pROZ. We are grateful to Elizabeth Mata, Sergio González, and Bárbara Mondragón for assistance with mouse care and housing.
All experimental animal work for this study was carried out under protocols approved by the Guide for the Care and Use of Laboratory Animals, National Institutes of Health, publication no. 93-23.
O.R.-M. was supported by a Ph.D. fellowship (117004) from the Consejo Nacional de Ciencia y Tecnología (CONACyT) and by the Sistema Nacional de Investigadores (SNI) (833). J.L.P. is a Howard Hughes International Research Scholar. This work was supported by grants to J.L.P. and E.C. from the Universidad Nacional Autónoma de México (DGAPA IN230398, IN229001, and IN223603) and from CONACyT (25187-N, 37738-N, and 46115-Q).
Editor: F. C. Fang
REFERENCES
- 1.Aron, L., G. Faundez, C. González, E. Roessler, and C. Cabello. 1993. Lipopolysaccharide-independent radio-immunoprecipitation and identification of structural and in vivo induced immunogenic surface proteins of Salmonella typhi in typhoid fever. Vaccine 11:10-17. [DOI] [PubMed] [Google Scholar]
- 2.Bernardini, M. L., A. Fontaine, and P. J. Sansonetti. 1990. The two-component regulatory system OmpR-EnvZ controls the virulence of Shigella flexneri. J. Bacteriol. 172:6274-6281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bernardini, M. L., M. G. Sanna, A. Fontaine, and P. J. Sansonetti. 1993. OmpC is involved in invasion of epithelial cells by Shigella flexneri. Infect. Immun. 62:3625-3635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beuzón, C. R., and D. W. Holden. 2001. Use of mixed infections with Salmonella strains to study virulence genes and their interactions in vivo. Microbes Infect. 3:1345-1352. [DOI] [PubMed] [Google Scholar]
- 5.Bowe, F., C. J. Lipps, R. M. Tsolis, E. Groisman, F. Heffron, and J. G. Kusters. 1998. At least four percent of the Salmonella typhimurium genome is required for fatal infection of mice. Infect. Immun. 66:3372-3377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Calderón, I., S. R. Lobos, H. A. Rojas, C. Palomino, L. H. Rodríguez, and G. C. Mora. 1986. Antibodies to porin antigens of Salmonella typhi induced during typhoid infection in humans. Infect. Immun. 52:209-212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chatfield, S. N., C. J. Dorman, C. Hayward, and G. Dougan. 1991. Role of ompR-dependent genes in Salmonella typhimurium virulence: mutants deficient in both OmpC and OmpF are attenuated in vivo. Infect. Immun. 59:449-452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Datsenko, K. A., and B. L. Wanner. 2000. One-step inactivation of chromosomal genes in Escherichia coli K-12 using PCR products. Proc. Natl. Acad. Sci. USA 97:6640-6645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dorman, C. J., S. Chatfield, C. F. Higgins, C. Hayward, and G. Dougan. 1989. Characterization of porin and ompR mutants of a virulent strain of Salmonella typhimurium: ompR mutants are attenuated in vivo. Infect. Immun. 57:2136-2140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fernández-Mora, M., J. L. Puente, and E. Calva. 2004. OmpR and LeuO positively regulate the Salmonella enterica serovar Typhi ompS2 porin gene. J. Bacteriol. 186:2909-2920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Flores-Valdez, M., J. L. Puente, and E. Calva. 2003. Negative osmoregulation of the Salmonella ompS1 porin gene independently of OmpR in an hns background. J. Bacteriol. 185:6497-6506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Francis, C. L., M. N. Starnbach, and S. Falkow. 1992. Morphological and cytoskeletal changes in epithelial cells occur immediately upon interaction with Salmonella typhimurium grown under low-oxygen conditions. Mol. Microbiol. 6:3077-3087. [DOI] [PubMed] [Google Scholar]
- 13.Galán, J. E., and R. Curtiss III. 1989. Cloning and molecular characterization of genes whose products allow Salmonella typhimurium to penetrate tissue culture cells. Proc. Natl. Acad. Sci. USA 86:6383-6387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Galdiero, M., M. D'Isanto, M. Vitiello, E. Finamore, L. Peluso, and M. Galdiero. 2003. Monocytic activation of protein tyrosine kinase, protein kinase A and protein kinase C induced by porins isolated from Salmonella enterica serovar Typhimurium. J. Infect. 46:111-119. [DOI] [PubMed] [Google Scholar]
- 15.Garmendia, J., C. R. Beuzón, J. Ruiz-Albert, and D. W. Holden. 2003. The roles of SsrA-SsrB and OmpR-EnvZ in the regulation of genes encoding the Salmonella typhimurium SPI-2 type III secretion system. Microbiology 149:2385-2396. [DOI] [PubMed] [Google Scholar]
- 16.Gupta, S., D. Kumar, H. Vohra, and N. Kumar Ganguly. 1999. Involvement of signal transduction pathways in Salmonella typhimurium porin activated gut macrophages. Mol. Cell Biochem. 194:235-243. [DOI] [PubMed] [Google Scholar]
- 17.Hurley, B. P., and B. A. McCormick. 2003. Translating tissue culture results into animal models: the case of Salmonella typhimurium. Trends Microbiol. 11:562-569. [DOI] [PubMed] [Google Scholar]
- 18.Isibasi, A., V. Ortíz, M. Vargas, J. Paniagua, C. González, J. Moreno, and J. Kumate. 1988. Protection against Salmonella typhi infection in mice after immunization with outer membrane proteins isolated from Salmonella typhi 9, 12, d, Vi. Infect. Immun. 56:2953-2959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim, C. C., and S. Falkow. 2004. Delineation of upstream signaling events in the Salmonella pathogenicity island 2 transcriptional activation pathway. J. Bacteriol. 186:4694-4704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kusters, J. G., G. A. W. M. Mulders-Kremers, C. E. M. van Doornik, and B. A. M. van der Zeijst. 1993. Effects of multiplicity of infection, bacterial protein synthesis, and growth phase on adhesion to and invasion of human cell lines by Salmonella typhimurium. Infect. Immun. 61:5013-5020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kuusi, N., M. Nurminen, H. Saxen, and P. H. Mäkela. 1981. Immunization with major outer membrane protein (porin) preparation in experimental murine salmonellosis: effect of lipopolysaccharide. Infect. Immun. 34:328-332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee, A. K., C. S. Detweiler, and S. Falkow. 2000. OmpR regulates the two-component system SsrA-SsrB in Salmonella pathogenicity island 2. J. Bacteriol. 182:771-781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lindgren, S. W., I. Stojilkovic, and F. Heffron. 1996. Macrophage killing is an essential virulence mechanism of Salmonella typhimurium. Proc. Natl. Acad. Sci. USA 93:4197-4201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Muthukummar, S., and V. R. Muthukkaruppan. 1993. Mechanism of protective immunity induced by porin-lipopolysaccharide against murine salmonellosis. Infect. Immun. 62:3984-3993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Negm, R. S., and T. G. Pistole. 1999. The porin OmpC of Salmonella typhimurium mediates adherence to macrophages. Can. J. Microbiol. 45:658-668. [PubMed] [Google Scholar]
- 26.Oropeza, R., C. L. Sampieri, J. L. Puente, and E. Calva. 1999. Negative and positive regulation of the non-osmoregulated ompS1 porin gene in Salmonella typhi: a novel regulatory mechanism that involves OmpR. Mol. Microbiol. 32:243-252. [DOI] [PubMed] [Google Scholar]
- 27.Puente, J. L., A. Verdugo-Rodríguez, and E. Calva. 1991. Expression of Salmonella typhi and Escherichia coli OmpC is influenced differently by medium osmolarity; dependence on Escherichia coli OmpR. Mol. Microbiol. 5:1205-1210. [DOI] [PubMed] [Google Scholar]
- 28.Reed, L. J., and H. Muench. 1938. A simple method of estimating fifty per cent endpoints. Am. J. Hyg. 27:493-497. [Google Scholar]
- 29.Segura, I., J. Casadesús, and F. Ramos-Morales. 2004. Use of mixed infections to study cell invasion and intracellular proliferation of Salmonella enterica in eukaryotic cell cultures. J. Microbiol. Methods 56:83-91. [DOI] [PubMed] [Google Scholar]
- 30.Tang, P., V. Foubister, M. G. Pucciarelli, and B. B. Finlay. 1993. Methods to study bacterial invasion. J. Microbiol. Methods 18:227-240. [Google Scholar]
- 31.Tenor, J. L., B. A. McCormick, F. M. Ausubel, and A. Aballay. 2004. Caenorhabditis elegans-based screen identifies Salmonella virulence factors required for conserved host-pathogen interactions. Curr. Biol. 14:1018-1024. [DOI] [PubMed] [Google Scholar]
- 32.Toguchi, A., M. Siano, M. Burkait, and R. M. Harshey. 2000. Genetics of swarming motility in Salmonella enterica serovar Typhimurium: critical role for lipopolysaccharide. J. Bacteriol. 182:6308-6321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Verdugo-Rodríguez, A., Y. López-Vidal, J. L. Puente, G. M. Ruíz-Palacios, and E. Calva. 1993. Early diagnosis of typhoid fever by an enzyme immunoassay using Salmonella typhi outer membrane protein preparations. Eur. J. Clin. Microbiol. Infect. Dis. 12:248-254. [DOI] [PubMed] [Google Scholar]
- 34.Wang, Q., J. G. Frye, M. McClelland, and R. M. Harshey. 2004. Gene expression patterns during swarming in Salmonella typhimurium: genes specific to surface growth and putative new motility and pathogenicity genes. Mol. Microbiol. 52:169-187. [DOI] [PubMed] [Google Scholar]