The prevalence of perforated sigmoid diverticular disease in developed countries has increased from 2.4/100 000 in 1986 to 3.8/100 000 in 2000.1 Diverticular disease is one of the five most costly gastrointestinal disorders in the United States.2 Thirty years ago, the proportion of people who died from diverticular disease was decreasing.3 During the past 20 years, however, annual age standardised rates of admission and surgical intervention have increased by 16% from 20.1/100 000 to 23.2/100 000, whereas inpatient and population mortality remains unchanged.4
This increasing burden of disease means that clinicians in primary and secondary care will see increasing numbers of patients with diverticular disease and its complications. This review covers recent developments in the management of diverticular disease, including the current trend towards conservative rather than operative management after recovery from the initial episode.5
Sources and selection criteria
We searched Medline and the Cochrane Library to locate English language articles on diverticular disease and diverticulitis, from 1964 until April 2005. We obtained further articles from the references cited in the initial literature review. We prioritised evidence from well designed randomised controlled trials, when available.
Natural history of diverticular disease
The prevalence of diverticulosis (see box 1 for definitions) increases uniformly with age, affecting 50% of people by the fifth decade and 67% by the eighth decade,6 with similar frequency in men and women.7 Approximately three quarters of patients with anatomical diverticulosis remain asymptomatic throughout their lifetime.6 Asymptomatic disease is often an incidental finding during investigation of colonic disorders; these patients need no specific treatment or follow-up. Of the remaining 25% of patients who develop symptoms, approximately three quarters develop diverticulitis (a third of whom have complications; box 1), and a quarter develop diverticular haemorrhage, which is massive in a third of cases.8
Pathophysiology
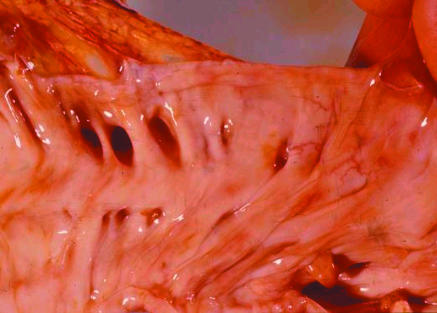
Although diverticular disease is common, the pathogenesis remains incompletely understood. Epidemiological studies have shown an inverse relation between the incidence of diverticular disease and fibre content of the diet.9 Low dietary fibre decreases stool bulk and prolongs transit time, causing increased intraluminal pressure. High intraluminal pressure may cause herniation of colonic mucosa through areas of weakness, produced by penetration of vasa recta that supply the submucosa and mucosa. As a result, diverticula are typically found in parallel rows between the taeniae coli (fig 1).6
Fig 1.
Pathology specimen showing two parallel rows of diverticula between the taeniae coli
Summary points
Diverticular disease is a common disorder, the prevalence of which is increasing as the proportion of elderly people increases
Dietary fibre may prevent development of diverticular disease, but once symptoms develop the benefit from fibre supplementation is unclear
The risk of perforation may be increased by use of non-steroidal anti-inflammatory drugs
Recent advances in diagnosis and treatment have enabled successful medical management of patients who would previously have had surgery
Emergency surgery has evolved from a three stage procedure to a two stage or one stage procedure
Most studies indicate that patients with diverticula have higher resting and postprandial colonic pressures than controls.6,10 However, other studies have found normal intraluminal pressures in patients with symptomatic diverticular disease,11 suggesting an alternative pathogenesis. Muscle wall thickening and contraction of the taeniae coli precedes diverticula formation and may be the primary pathogenic mechanism. Irreversible contraction occurs as a result of increased elastin deposition,12 which together with age related changes in collagen composition may weaken the colonic wall, predisposing to diverticula formation.
The interrelation of high intraluminal pressures and colonic wall weakness remains poorly understood. The sigmoid colon is less compliant than the ascending colon. This may predispose to the classic type of diverticulosis seen in Western countries, characterised by increased intraluminal pressures, infectious complications, and perforation. In contrast, right sided diverticula predominate in Asian countries, typically with normal intraluminal pressures and a tendency to bleeding rather than perforation,13 presumably owing to underlying connective tissue abnormality. Other mechanisms may account for these diverse geographic phenotypes; a recent theory proposes that hypersensitivity of colonic smooth muscle to anti-cholinesterases causes dysmotility in diverticular disease, which may promote diverticula formation.14
Box 1: Terminology
Diverticulosis—the presence of diverticula that are asymptomatic
Diverticular disease—diverticula associated with symptoms
Diverticulitis—evidence of diverticular inflammation (fever, tachycardia) with or without localised symptoms and signs
Complicated diverticulitis—perforation*, abscess, fistula, stricture/obstruction
*As diverticulitis by definition means at least a microperforation in all cases,6 in this review “perforation” means rupture of a peridiverticular abscess into the peritoneal cavity, causing either purulent or faecal peritonitis.
Once diverticula have formed, stool may become inspissated within the neck. In a process similar to appendicitis, the obstructing faecalith promotes secretion of mucus and bacterial overgrowth, which distends and erodes the thin walled diverticulum. Localised ischaemia develops, enabling translocation of mucosal bacteria and eventual perforation.15 Hinchey et al developed a useful system to classify the inflammation following diverticular perforation (box 2).16 Most perforations are small and contained within pericolic fat, causing a small pericolic abscess (stage one disease). Larger abscesses (stage two) may rupture into the peritoneal cavity (stage three). Progression to gross faecal peritonitis (stage four) is determined by whether the faecalith continues to obstruct the diverticulum.
Symptomatic disease
Patients often develop colicky abdominal pain, bloating, or flatulence, which is exacerbated by eating and relieved by passage of flatus or stool. Although these symptoms are largely due to colonic wall tension and raised intraluminal pressure, a recent randomised controlled study found that intravenous hyoscine butylbromide (an antispasmodic agent) was no better than placebo at relieving distension.17 Bleeding from the rectum or a positive faecal occult blood test warrants careful exclusion of other colonic pathology. Examination may reveal tenderness in the left lower quadrant without guarding or systemic signs of inflammation.
Considerable overlap exists between symptoms of diverticular disease and irritable bowel syndrome. As both diagnoses are relatively common, some people may have symptoms attributable to both conditions. However, the temporal relation between these distinct entities remains controversial. Although irritable bowel-like symptoms may follow an episode of diverticulitis,18 evidence of the reverse is lacking, as the natural history of irritable bowel syndrome seems to be independent of the presence or absence of symptomatic diverticular disease.19
Treatment of uncomplicated disease
Large prospective studies have identified a preventive effect of both dietary fibre and physical exercise in the development of diverticular disease.20 Once symptoms have developed, however, evidence of a benefit from fibre is less convincing: of two small randomised controlled trials comparing fibre and placebo, one found no difference in symptoms and the other reported improved symptoms but no change in bowel dysfunction after three months' follow-up.21,22 Another randomised controlled trial found that adding rifaximin, a rifamycin antibiotic, to fibre supplementation decreased symptoms after 12 months of treatment23; 10% of participants were unable to complete the trial, however, and analysis was not by intention to treat. Although some people may benefit from supplementary fibre, more evidence is needed from studies with longer follow-up before fibre supplementation can be widely recommended.
Mesalazine has been shown to significantly reduce symptomatic recurrence at four years compared with placebo,24 but abdominal pain was more common with mesalazine. A more recent randomised controlled trial suggests that mesalazine may be superior to rifaximin in overall control of symptoms.25 A large case-control study found that use of calcium channel blockers, which decrease intracolonic pressure, was associated with a reduction in diverticular perforation.26 Long term use of opioids (which increase intracolonic pressure) seems to increase the risk of diverticular perforation.27 Whether these associations are causal remains unclear, so insufficient evidence exists to make recommendations on use of calcium channel blockers or opioid analgesics in patients with diverticular disease.
Box 2: Hinchey classification of peritoneal contamination in diverticulitis
Stage 1. Pericolic or mesenteric abscess
Stage 2. Walled-off or pelvic abscess
Stage 3. Generalised purulent peritonitis
Stage 4. Generalised faecal peritonitis
Use of non-steroidal anti-inflammatory drugs remains the most consistently identified risk factor for diverticular perforation but accounts for only a fifth of all cases of perforation.28 The hypothesised mechanism is due to the adverse affect of prostaglandin inhibition on mucosal blood flow. When considering non-steroidal anti-inflammatory drugs for patients with diverticular disease, the risk of perforation should be balanced against the therapeutic benefit.
Diverticulitis
Evidence of systemic inflammation (fever, neutrophilia, tachycardia) differentiates diverticulitis from simple diverticular disease. A tender inflammatory mass is occasionally palpable, and an associated change in bowel habit may occur. Initial outpatient treatment should include a clear liquid diet and broad spectrum oral antibiotics with activity against anaerobes and Gram negative rods.1 Symptomatic improvement should be seen within two or three days. The need for admission in uncomplicated cases is determined by response to treatment, ability to tolerate oral intake, and comorbid disease. Conservative treatment of acute uncomplicated diverticulitis results in resolution of symptoms in 70-100% of patients.5 Admitted patients should improve after two to four days of bowel rest and intravenous antibiotics; failure of conservative measures warrants further investigation.
Complicated diverticulitis
The natural history of complicated diverticular disease remains poorly understood, probably because consultant surgeons see only two or three cases a year, and almost a third of patients die from unrelated causes during follow-up.29 Advances in antimicrobial chemotherapy may have contributed to more successful medical management; recent reports have shown recurrence rates of 2% per patient year of follow-up.29
Diagnostic imaging
In acute diverticulitis, the colonic mucosa is grossly and microscopically normal, despite substantial inflammation of the pericolic fat. Consequently, contrast enemas are limited because the disease process is predominantly extraluminal. Computed tomography is a safer, more cost effective alternative,6,7 with therapeutic potential for drainage of percutaneous abscesses.
Box 3: Indications for surgery
Tomographic evidence of diverticulitis includes inflammation of pericolic fat, clonic wall thickening, or peridiverticular abscess (fig 2). Abscesses less than 5 cm in diameter tend to regress after antibiotic treatment,30 and abscesses under 2 cm can be successfully managed on an outpatient basis with oral antibiotics,31 the cost of which is 80% lower than inpatient treatment. Computed tomography guided percutaneous drainage gives rapid control of sepsis and prompt relief of symptoms for Hinchey stage 1-2 lesions, after which patients may remain asymptomatic.31
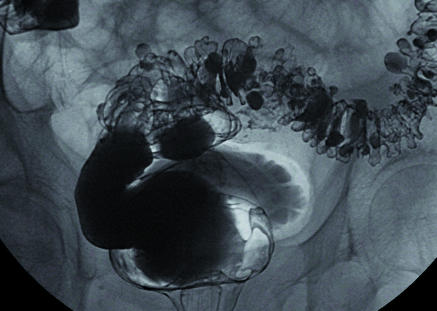
Fig 2.
Computed tomogram of a large sigmoid diverticular abscess, with thickening of the bowel wall and inflammation of the surrounding fat
After recovery from the initial episode, the risk of recurrent symptoms varies from 7% to 45%,5 reflecting a broad spectrum of disease severity and diagnostic criteria in various studies. Most complications occur during the first admission,32 after which the disease seems to run a benign course, with a greater risk of dying from unrelated diseases than from complications related to diverticulitis.29
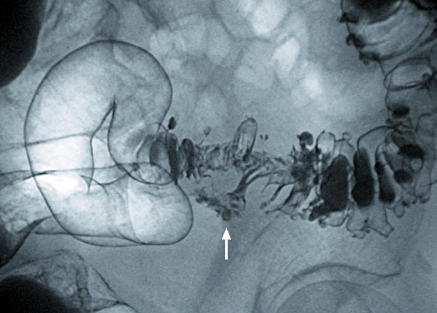
Fig 3.
This elderly man with diverticular disease developed a urinary tract infection and pneumaturia. Double contrast barium enema showed a colovesical fistula. Diverticular disease is the most common cause of this type of fistula
Emergency surgery
Box 3 summarises indications for surgery. Purulent or faecal peritonitis was traditionally managed by three stage procedures. The first operation controlled sepsis by drainage and transverse colostomy formation. After an unspecified time, the disease segment was excised. Eventual colostomy closure and restoration of bowel continuity completed the third stage. A critical literature review published in 1984 found that the operative mortality with a three stage procedure approached 25%.33 Subsequently, a two stage procedure involving formation of an end colostomy with oversewing of the rectal stump (Hartmann procedure) became preferable, and operative mortality was almost halved. A recent multicentre randomised controlled trial found that a one stage procedure (primary anastomosis) significantly reduced rates of postoperative peritonitis and emergency reoperation compared with a two stage procedure,34 without adversely affecting operative mortality. Use of a one stage procedure has been limited by concerns about anastomosis failure due to peritoneal contamination, gut oedema or inflammation, and unprepared bowel. Relatively recently introduced techniques, such as preoperative computed tomography guided drainage of abscesses followed by staged laparotomy and on-table colonic lavage in patients with obstructive diverticular disease may decrease anastomotic failure and facilitate one stage procedures.35
Elective resection to prevent complications of diverticular disease
During the past 20 years, postoperative mortality after emergency procedures has remained unchanged at 12-36%,5 despite advances in surgical techniques, antibiotic treatment, and intensive care. Elective sigmoid resection after two episodes of uncomplicated diverticulitis has been recommended to prevent complications and reduce emergency procedures.6,7 These recommendations were based on historic data of low validity, which suggested that recurrent attacks are less likely to respond to medical treatment and have a higher mortality rate.
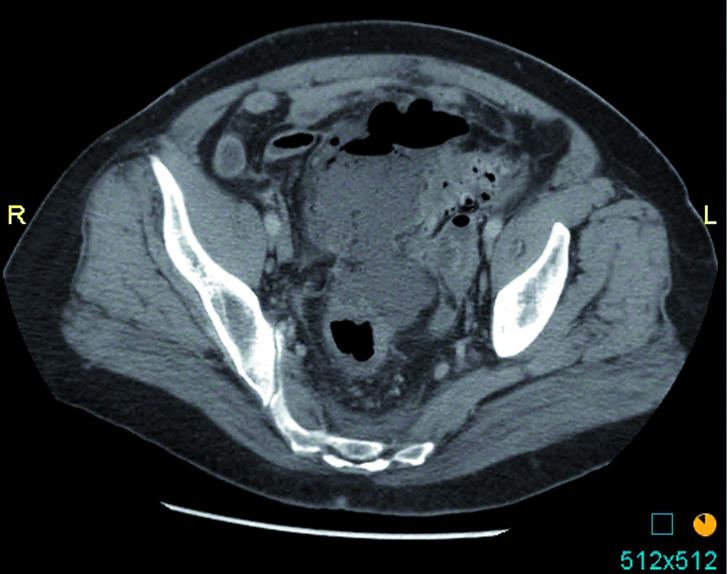
Fig 4.
Double contrast barium enema showing a suspicious stricture (arrow) and multiple diverticula. Pathology confirmed that the stricture was non-malignant
Recent evidence indicates that prophylactic resection would have little impact in preventing subsequent complications,5 as most patients who need urgent surgery have no history of diverticular disease. A large cross sectional population based study estimated the incidence of perforated diverticulitis at 4 cases per 100 000 population per year, with less than a quarter of patients having a history of diverticular disease.36 Other studies show that only 3-33% of patients who need emergency surgery for perforation have documented diverticular disease,37,38 indicating that for most people who develop complications a complication is the first manifestation of disease.
Recommending elective resection needs a careful risk-benefit assessment, in which the morbidity, mortality, and costs of all subsequent attacks (including emergency surgery) are weighed against the morbidity, mortality, and costs when patients have elective resection. A cost effectiveness study found that expectant management rather than elective resection was associated with fewer deaths and 2% fewer colostomies and saved up to $5249 per patient, with most benefit seen in younger patients.39 After elective resection, approximately a quarter of patients have persisting symptoms (probably reflecting coexisting irritable bowel syndrome),7 and up to 10% develop recurrent diverticulitis, of which 0-3.1% need re-resection.40-43 Mortality increases with advancing age from zero to 15%, and around half of patients who have a Hartmann procedure never regain intestinal continuity. Patients should be fully informed about the risks and benefits associated with either conservative management or elective resection when treatment options are being discussed.
Diverticulitis in special circumstances
Symptoms and signs may develop late, and conservative treatment is more likely to fail, in immunocompromised patients, so early surgical intervention may be needed. Approximately 10% of people with diverticular disease are under 40 years of age. Historically, the disease was thought to be more aggressive in younger people, with a male predominance, and resection after one episode of diverticulitis was recommended. Recent prospective data cast doubt on these recommendations.5 The diagnosis is often not considered in younger women, who have a wide range of differential diagnoses. In both sexes, higher rates of emergency surgery are attributable to high rates of misdiagnoses. The risk of complications attributable to young age at diagnosis may simply reflect prolonged exposure to diverticular disease, rather than pathological mechanisms.
Ongoing research
Alternatives in diverticulitis management trial—prospectively evaluating one stage procedures for surgical management of acute complicated diverticulitis. depts.washington.edu/sorce/projects.html (accessed 4 Sept 2005)
Sigmoid diverticular disease: the surgical epidemiology—an ongoing large scale study from the Mayo Clinic, USA. www.mayoclinic.org/diverticulitis/research.html (accessed 4 Sept 2005)
Clinical research questions that remain unanswered
Why diverticula are so common in the colon in Western societies
Whether changes in lifestyle, especially diet, by young people would prevent development of diverticula in later life
Why some people get symptoms from diverticular disease, but most do not
Why some people have an associated abnormality of muscle in the colon
What leads to infection or other complication of a diverticulum
How treatment of symptoms or complications can be improved
Questions from the CORE homepage: www.digestivedisorders.org.uk/Default.aspx?docname=doc_diverticular&sec=Section12 (accessed 4 Sept 2005)
Additional educational resources
Resources for doctors
Simpson J, Spiller R. Colonic diverticular disease. Clin Evid 2004;12: 599-609 (www.clinicalevidence.org/ceweb/conditions/dsd/0405/0405.jsp)—up to date evidence based information on treatment and interventions for diverticular disease
Janes S, Meagher A, Frizelle FA. Elective surgery after acute diverticulitis. Br J Surg 2005;92: 133-4215685694—a comprehensive review of the evidence supporting elective resection
Cleveland clinic website (www.clevelandclinicmeded.com/diseasemanagement/gastro/colonic/colonic.htm)—online educational resource for clinicians
Resources for patients
National Digestive Diseases Information Clearinghouse (digestive.niddk.nih.gov/ddiseases/pubs/diverticulosis/)—information on what diverticular disease is (with pictures) and what causes it, the symptoms, and the complications, as well as medical and surgical treatment options
ASCRS (www.fascrs.org/displaycommon.cfm?an=1&subarticlenbr=10)—similar information to the above site, but more concise
Conclusions
Dietary fibre supplementation, though often recommended for patients with symptomatic diverticular disease, is probably more useful as a preventive rather than a therapeutic intervention. Although non-steroidal anti-inflammatory drugs seem to increase the risk of perforation, further studies are needed to determine the effects of calcium channel blockers and opiates on perforation. Most complications of diverticulitis are associated with the initial attack, after which the disease seems to run a benign course, with more deaths caused by unrelated diseases than by complications of acute diverticulitis. Little evidence exists that elective surgery after two attacks of diverticulitis prevents future complications. Surgery for diverticular disease has a high complication rate, and the outcomes after surgery are often unpredictable. The recent trend towards a one stage procedure may reduce overall mortality for acute resections.
Contributors: SEJJ had the idea for the article and wrote the first draft. AM and FAF critically reviewed and corrected the draft version and provided additional references. FAF is the guarantor.
Competing interests: None declared.
References
- 1.Mäkelä J, Kiviniemi H, Laitinen S. Prevalence of perforated sigmoid diverticulitis is increasing. Dis Colon Rectum 2002;45: 955-61. [DOI] [PubMed] [Google Scholar]
- 2.American Gastroenterological Association. The burden of gastrointestinal diseases. Bethesda, MD: American Gastroenterological Association, 2001.
- 3.Kyle J, Davidson AI. The changing pattern of hospital admissions for diverticular disease of the colon. Br J Surg 1975;62: 537-41. [DOI] [PubMed] [Google Scholar]
- 4.Kang JY, Hoare J, Tinto A, Subramanian S, Ellis C, Majeed A, et al. Diverticular disease of the colon on the rise: a study of hospital admissions in England and Wales between 1989/1990 and 1999/2000. Aliment Pharmacol Ther 2003;17: 1189-95. [DOI] [PubMed] [Google Scholar]
- 5.Janes SEJ, Meagher A, Frizelle FA. Elective surgery after acute diverticulitis. Br J Surg 2005;92: 133-42. [DOI] [PubMed] [Google Scholar]
- 6.Stollman N, Raskin JB. Diverticular disease of the colon. Lancet 2004;363: 631-9. [DOI] [PubMed] [Google Scholar]
- 7.Ferzoco LB, Raptopoulos V, Silen W. Acute diverticulitis. N Engl J Med 1998;338: 1521-6. [DOI] [PubMed] [Google Scholar]
- 8.Young-Fadok TM, Roberts PL, Spencer MP, Wolff BG. Colonic diverticular disease. Curr Probl Surg 2000;37: 457-514. [DOI] [PubMed] [Google Scholar]
- 9.Painter NS, Burkitt DP. Diverticular disease of the colon: a deficiency disease of Western civilisation. BMJ 1971;ii: 450-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arfwidsson S, Knock N, Lehmann L, Winberg T. Pathogenesis of multiple diverticula of the sigmoid colon in diverticular diseases. Acta Chir Scan 1964;342(suppl): 1-68. [PubMed] [Google Scholar]
- 11.Ming SC. Diverticular disease of the colon. In: Ming SC, Goldman H, eds. Pathology of the gastrointestinal tract. Baltimore, Williams and Wilkins, 1998:801- 17. [Google Scholar]
- 12.Whiteway J, Morson BC. Elastosis in diverticular disease of the sigmoid colon. Gut 1985;26: 258-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ryan P. Changing concepts in diverticular disease. Dis Colon Rectum 1983;26: 12-8. [DOI] [PubMed] [Google Scholar]
- 14.Golder M, Burleigh DE, Belai A, Ghali L, Ashby D, Lunniss PJ, et al. Smooth muscle cholinergic denervation hypersensitivity in diverticular disease. Lancet 2003;361: 1945-51. [DOI] [PubMed] [Google Scholar]
- 15.Williams R, Davis I. Diverticular disease of the colon. 5th edn. Philadelphia: Saunders, 1995.
- 16.Hinchey EF, Schaal PG, Richards GK. Treatment of perforated diverticular disease. Adv Surg 1978;12: 85-109. [PubMed] [Google Scholar]
- 17.Bruzzi JF, Moss AC, Brennan DD, MacMathuna P, Fenlon HM. Efficacy of IV Buscopan as a muscle relaxant in CT colonography. Eur Radiol 2003;10: 2264-70. [DOI] [PubMed] [Google Scholar]
- 18.Simpson J, Neal KR, Scholefield JH, Spiller RC. Patterns of pain in diverticular disease and the influence of diverticulitis. Eur J Gastroenterol Hepatol 2003;15: 1005-10. [DOI] [PubMed] [Google Scholar]
- 19.Otte JJ, Larsen L, Anderson JR. Irritable bowel syndrome and symptomatic diverticular disease—different diseases? Am J Gastoenterol 1986;81: 529-31. [PubMed] [Google Scholar]
- 20.Aldoori WH, Giovannucci EL, Rimm EB, Wing AL, Trichopoulos DV, Willett WC. A prospective study of diet and the risk of symptomatic diverticular disease in men. Am J Clin Nutr 1994;60: 757-64. [DOI] [PubMed] [Google Scholar]
- 21.Ornstein MH, Littlewood ER, Baird IM, Fowler J, North WR, Cox AG. Are fibre supplements really necessary in diverticular disease of the colon? A controlled clinical trial. BMJ 1981;282: 1353-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brodribb AJ. Treatment of symptomatic diverticular disease with a high fibre diet. Lancet 1977;1: 644-66. [DOI] [PubMed] [Google Scholar]
- 23.Papi C, Ciaco A, Koch M, Capurso L. Efficacy of rifaximin in the treatment of symptomatic diverticular disease of the colon: a multicentre double-blind placebo-controlled trial. Aliment Pharmacol Ther 1995;9: 33-9. [DOI] [PubMed] [Google Scholar]
- 24.Trespi E, Colla C, Panizza P, Polino MG, Venturini A, Bottani G, et al. Therapeutic and prophylactic role of mesalazine (5-ASA) in symptomatic diverticular disease of the colon: 4-year follow-up results. Minerva Gastroenterol Dietol 1999;45: 245-52. [PubMed] [Google Scholar]
- 25.Di Mario F, Aragona G, Leandro G. Efficacy of mesalazine in the treatment of symptomatic diverticular disease. Dig Dis Sci 2005;50: 581-6. [DOI] [PubMed] [Google Scholar]
- 26.Morris CR, Harvey IM, Stebbings WSL, Speakman CTM, Kennedy HJ, Hart AR. Do calcium channel blockers and antimuscarinics protect against perforated colonic diverticular disease? A case-control study. Gut 2003;52: 1734-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Morris CR, Harvey IM, Stebbings WS, Speakman CT, Kennedy HJ, Hart AR. Anti-inflammatory drugs, analgesics and the risk of perforated colonic diverticular disease. Br J Surg 2003;90: 1267-72. [DOI] [PubMed] [Google Scholar]
- 28.Hart AR, Kennedy HJ, Stebbings WS, Day NE. How frequently do large bowel diverticula perforate? An incidence and cross-sectional study. Eur J Gastroenterol Hepatol 2000;12: 661-5. [DOI] [PubMed] [Google Scholar]
- 29.Sarin S, Boulos PB. Long-term outcome of patients presenting with acute complications of diverticular disease. Ann R Coll Surg Engl 1994;76: 117-20. [PMC free article] [PubMed] [Google Scholar]
- 30.Stabile BE, Puccio E, van Sonnenberg E, Neff CC. Preoperative percutaneous drainage of diverticular abscess. Am J Surg 1990;159: 99-104. [DOI] [PubMed] [Google Scholar]
- 31.Mizuki A, Nagata H, Tatemichi M, Kaneda S, Tsukada N, Ishii H, et al. The out-patient management of patients with acute mild-to-moderate colonic diverticulitis. Aliment Pharmacol Ther 2005;21: 889-97. [DOI] [PubMed] [Google Scholar]
- 32.Haglund U, Hellberg R, Johnson C, Halten L. Complicated diverticular disease of the sigmoid colon: an analysis of long term outcome in 392 patients. Ann Chir Gynaecol 1979;68: 41-6. [PubMed] [Google Scholar]
- 33.Krukowski ZH, Matheson NA. Emergency surgery for diverticular disease complicated by generalized and faecal peritonitis: a review. Br J Surg 1984;71: 921-7. [DOI] [PubMed] [Google Scholar]
- 34.Zeitoun G, Laurent A, Rouffet F, Hay J, Fingerhut A, Paquet J, et al. Multicentre, randomised clinical trial of primary versus secondary sigmoid resection in generalised peritonitis complicating sigmoid diverticulitis. Br J Surg 2000;87: 1366-74. [DOI] [PubMed] [Google Scholar]
- 35.Koruth NM, Krukowski ZH, Youngson GG, Hendry WS, Logie JR, Jones PF, et al. Intra-operative colonic irrigation in the management of left-sided bowel emergencies. Br J Surg 1985;72: 708-11. [DOI] [PubMed] [Google Scholar]
- 36.Hart AR, Kennedy HJ, Stebbings WS, Day NE. How frequently do large bowel diverticula perforate? An incidence and cross-sectional study. Eur J Gastroenterol Hepatol 2000;12: 661-5. [DOI] [PubMed] [Google Scholar]
- 37.Nylamo E. Diverticulitis of the colon: role of surgery in preventing complications. Ann Chir Gynaecol 1990;79: 139-42. [PubMed] [Google Scholar]
- 38.Lorimer JW. Is prophylactic resection valid as an indication for elective surgery in diverticular disease? Can J Surg 1997;40: 445-8. [PMC free article] [PubMed] [Google Scholar]
- 39.Salem L, Veenstra DL, Sullivan SD, Flum DR. The timing of elective colectomy in diverticulitis: a decision analysis. J Am Coll Surg 2004;199: 904-12. [DOI] [PubMed] [Google Scholar]
- 40.Benn PL, Wolff BC, Ilstrup DM. Level of anastomosis and recurrent diverticulitis. Am J Surg 1986;151: 269-71. [DOI] [PubMed] [Google Scholar]
- 41.Bacon HE, Berkley JL. The surgical management of diverticular disease of the colon with particular reference to rehabilitation. Arch Surg 1960;80: 646-9. [DOI] [PubMed] [Google Scholar]
- 42.Leigh JE, Judd ES, Waugh JM. Diverticulitis of the colon: recurrence after apparently adequate segmental resection. Am J Surg 1962;103: 51-4. [DOI] [PubMed] [Google Scholar]
- 43.Marsh J, Liem RKT, Byrd BG, Daniel RA. One hundred consecutive operations for diverticular disease of the colon. South Med J 1975;68: 133-7. [DOI] [PubMed] [Google Scholar]