Abstract
Objective
To determine whether mortality rates for patients with acute myocardial infarction (AMI) changed in New Jersey after implementation of the Health Care Reform Act, which reduced subsidies for hospital care for the uninsured and changed hospital payment to price competition from a rate-setting system based on hospital cost.
Data Sources/Study Setting
Patient discharge data from hospitals in New Jersey and New York from 1990 through 1996 and the Healthcare Cost and Utilization Project (HCUP) Nationwide Inpatient Sample (NIS).
Study Design
A comparison between states over time of unadjusted and risk-adjusted mortality and cardiac procedure rates.
Data Collection
Discharge data were obtained for 286,640 patients with the primary diagnosis of AMI admitted to hospitals in New Jersey or New York from 1990 through 1996. Records of 364,273 NIS patients were used to corroborate time trends.
Principal Findings
There were no significant differences in AMI mortality among insured patients in New Jersey relative to New York or the NIS. However, there was a relative increase in mortality of 41 to 57 percent among uninsured New Jersey patients post-reform, and their rates of expensive cardiac procedures decreased concomitantly.
Conclusions
The introduction of hospital price competition and reductions in subsidies for hospital care of the uninsured were associated with an increased mortality rate among uninsured New Jersey AMI patients. A relative decrease in the use of cardiac procedures in New Jersey may partly explain this finding. Additional studies should be done to identify whether other market reforms have been associated with changes in the quality of care.
Keywords: Quality of health care; health care reform, economics; financing; economics/hospital
Over the past decade and a half, many states have adopted market-based reforms to slow the rate of growth in health care costs (Zwanziger, Melnick, and Bamezai 2000; Dranove, Shanley, and White 1993). Although market-based reforms are becoming more widespread, little is known about how they affect the quality of care (Gaynor and Haas-Wilson 1999; Kessler and McClellan 2000). There is concern that market-based reforms may disproportionately affect the care provided to uninsured (Gruber 1994), low-income (Ware et al. 1986; Ware et al. 1996), or “unprofitable” patients (Chung and Meltzer 2000).
In 1992, New Jersey passed the Health Care Reform Act (HCRA), which replaced a rate-setting system that prevented hospital price competition with a system that encouraged price competition. This change, along with the growth of large-volume buyers such as HMOs, placed new competitive pressures on hospital prices in New Jersey. Under the rate-setting system, rates were based on incurred costs, and hospitals competed for patients by providing more services. Numerous studies in other contexts have shown that this type of competition leads hospitals in more competitive areas to have higher costs and to provide more technologically advanced services and more amenities (Robinson and Luft 1987; 1985; Held and Pauly 1983; Farley 1985). Under price competition, in contrast, buyers negotiate price discounts with hospitals, and each hospital must use a combination of price and quality to compete for patients. As competition intensifies, hospitals are compelled to grant discounts, which may lead to decreased quality of care because discounts force hospitals to cut costs and many of the technical aspects of care are not easily monitored (Arrow 1963; Weisbrod 1989).
The new act also substantially reduced subsidies for hospital care for the uninsured that existed under the rate-setting system. Under the new act the 19 percent surcharge on all hospital bills that was used to pay hospitals for care of the uninsured (Volpp and Siegel 1993) was eliminated. As a result, the funds available in the charity care pool with which New Jersey compensated hospitals for care of the uninsured went from $700 million in 1992 to $500 million in 1993, to $450 million in 1994, to $400 million in 1995, and to $350 million in 1996 (Cantor 1993; Bovbjerg, Cuellar, and Holahan 2000).
To identify changes in the quality of care in New Jersey after the introduction of the new act, this study focused on patients hospitalized with acute myocardial infarction (AMI), a common high-mortality condition whose outcomes are affected by the process of care (Davies et al. 2001). To measure the effect of the change in hospital financing, we measured how mortality rates changed over time in New Jersey relative to New York. Effects on the process of care were measured by looking at changes in the rates of cardiac catheterization and mechanical revascularization in the two states. Since all of 1993 was set aside as a transition year before full implementation of the legislation on January 1, 1994, we focused on how AMI outcomes and cardiac procedure rates changed from the pre-reform time period (1990–1992) to the post-reform time period (1994–1996). Particular attention was paid to the size of the effects among uninsured patients, the group most likely to be vulnerable in the transition to price competition.
Methods
Study Sample and Choice of Control Group
Patients with AMI were chosen for this study because acute myocardial infarctions are common, the treatment objective generally is to ensure survival, and the quality of care affects the likelihood of survival (Pashos, Newhouse, and McNeil 1993; Davies et al. 2001). In addition, all patients with recognized AMI are admitted to the hospital. Therefore, there is little opportunity for selection bias to affect the decision about who gets admitted, and thus less need to adjust results for differences in patient characteristics. Bias could occur if there were significant changes in admission criteria or systematic movement of people with different than average AMI mortality to or from New Jersey in conjunction with the introduction of the new act, but these changes were unlikely. This is particularly true in studies like ours that compare outcomes for all patients within a large geographic area over time. In contrast, it is imperative to adjust for patient characteristics in studies that use cross-sectional analyses or examine hospital-level outcomes over time, even though selection bias can never be completely controlled for (Iezzoni 1994; Greenfield et al. 1988).
Even in the absence of policy changes, improvement in mortality over time would be expected as medical technology advances. Because of this trend it is important to have a suitable control group that suggests how New Jersey mortality rates would evolve in the absence of a change in the law. New York was chosen as the primary control state for heart attack mortality because it has a large population, it is an adjacent state, there were no major changes in New York's hospital financing system from 1990 to 1996, and similar patient discharge data were available. The Healthcare Cost and Utilization Project (HCUP) Nationwide Inpatient Sample (NIS) contains an estimated 20 percent of all patients in the country. Because it does not include patients representative of each geographic area, we used it only to examine national AMI mortality trends.
We used a multiple time series research design because it provides a strong test of whether the change in hospital financing changed the underlying trend in AMI mortality in New Jersey (Campbell and Stanley 1963). Provided that there were no major policy changes in New York after the change in New Jersey's law, the validity of New York as a control for New Jersey in the pre-reform period is testable. If we cannot reject the hypothesis that the pattern of changes in mortality (and procedure rates) was the same in both New Jersey and its control state pre-reform, the control state provides a valid control for New Jersey.
This study primarily assessed patients from New Jersey and New York with a principal diagnosis of acute myocardial infarction during the first episode of care for a newly diagnosed acute myocardial infarction (ICD9-CM codes 410.x1) or if the time of the infarction was unspecified (410.x0) (n=453,712). Because of concerns that patients with this diagnosis code may have included “rule out” AMIs, we excluded patients who were discharged alive with a length of stay of less than three days. We chose this cutoff because it seemed like a reasonable minimum length of stay for a true myocardial infarction during that time period in New Jersey. Shorter length of stay cutoffs have been used in examining California discharge data (three days in 1993, two days in 1996), but length of stay for AMI patients in New Jersey has been much longer than in California (an average of more than 2 days longer from 1990–1996 according to the HCUP Nationwide Inpatient Sample).
We used the following exclusion criteria: (1) Age younger than 18, because the pathophysiology of disease in this age group is likely to be different than for adults (n=192); (2) Age greater than 85, because such patients may be treated less aggressively than younger patients (Greenfield et al. 1988) (n=32,424); (3) Length of stay less than three days when the reason for discharge was something other than death or against medical advice, because these patients probably had some diagnosis other than acute myocardial infarction (Udvarhelyi et al. 1992; Luft and Romano 1996) (n=19,457); (4) Pretransfer hospitalizations, because we could not link information from the discharging and receiving hospitals and thus could not determine whether patients died or received procedures (n=83,863); (5) Length of stay greater than 30 days (n=11,507); (6) Nonresidents of New Jersey treated in New Jersey (n=8,360) or nonresidents of New York treated in New York (n=6,746); (7) The AMI specified to be some time other than the initial hospitalization (410.x2) (n=3,098); and (8) Records missing an essential field such as patient age or discharge status (n=1,425). A total of 286,640 patient records from New Jersey and New York remained for the analysis, and the rates of exclusions for each of the exclusion criteria were similar in New Jersey and New York.
The principal outcome measure was death that occurred during the initial hospitalization, provided length of stay was less than or equal to 30 days. We also recorded the number of cardiac catheterizations (ICD9-CM codes 37.21–37.23 and 88.55–88.57) and the number of mechanical revascularization procedures, which we defined as the sum of coronary artery bypass procedures (36.11–36.19) and coronary angioplasties or stents (36.01, 36.02, 36.05, 36.06) during the first 30 days of the initial hospitalization.
The sources of the data were the hospital discharge data from New Jersey (Uniform Billing-82 and Uniform Billing-92), New York (Statewide Planning and Research Cooperative System Inpatient Output Data Dictionary). Hospitals were required by the states to submit these data and all inpatient discharges were included. At the end of 1996, legislation was passed that dissolved the New York hospital rate-setting system so we do not include data after 1996. In addition to mortality outcome, the data included information on patient age, sex, race, hospital where treated, length of stay, source and type of admission, discharge date, expected principal payer, principal diagnosis, principal procedure, and any secondary diagnoses and procedures (up to 8 in New Jersey and up to 14 in New York).
Statistical Analysis
The impact of HCRA on the quality of care for New Jersey patients was measured using a “differences in differences” measurement approach, comparing New Jersey trends in mortality and procedure use with those of New York.
The differences in differences measurement framework is implemented in the following linear probability model:
| (1) |
In this equation, y=an indicator of mortality or procedure utilization within 30 days of hospital admission, for individual i, Xi=characteristics of the individual (except when we include risk-adjustment variables, this is simply a constant), and the δ terms are dummies for New Jersey (δNJ), for particular years (δt), and New Jersey in particular years (δNJ,t). We measure the effect of the change in the law on New Jersey outcomes of interest by examining the sign, size, and significance of the coefficients αNJ,1994, αNJ,1995, αNJ,1996, as 1993 was a transition year.
In this model, baseline mortality risk is allowed to differ between New Jersey and its control state, and New Jersey and its control state have a common mortality rate time trend until the change in the law, after which time the New Jersey trend is allowed to diverge. We test for differences in the rate of change between New Jersey and its control state pre-HCRA by using a multiple partial F-test to measure whether the coefficients for the interaction terms for New Jersey combined with 1991 and 1992 equal zero.
Although we assumed that patients with AMI had similar severity of illness before and after the new act in New Jersey, changes were possible, for example from secular demographic change such as an aging population. Since New York outcomes were used to control for New Jersey outcomes, these changes matter only if they happened faster or slower in New Jersey than in New York. While these differences would be expected to be small over this period, we estimated models with risk adjustment to control for any such changes. Risk adjustment was particularly important for subgroups of the population such as the uninsured because the type of patient who was uninsured may have changed over time.
Risk Adjustment
An approach to risk adjustment similar to that used in the California Hospital Outcomes Project (Luft and Romano 1996) was taken. Only the following risk factors that were present on admission to the hospital were considered for inclusion in our primary risk-adjustment model: age, sex, location of acute myocardial infarction (anterior, inferior, or subendocardial), prior coronary artery bypass graft (CABG), congestive heart failure, complications of diabetes, high-risk or secondary malignancy, chronic renal failure, nutritional disorders, and prior placement of cardiac pacemaker. Because secondary diagnoses included in risk-adjustment models may be complications of treatment as opposed to comorbidities that were present on admission and this cannot be differentiated with the available data, this risk-adjustment model was constructed only with secondary diagnoses that were likely to be comorbidities. To construct the risk-adjustment model, the entire dataset for patients in New Jersey was randomly divided into equally sized estimation and validation samples. The bivariate association between each clinical risk factor and death was examined using relative risk estimates with 95 percent confidence limits and p-values derived from a continuity-adjusted chi-square distribution. Risk factors not associated with death at a p<0.10 level were eliminated from the analysis. We also eliminated risk factors shown by other investigators to have an increased risk of death that in our sample appeared to lower risk because we thought it likely that there was selective underreporting of secondary diagnoses among patients with adverse outcomes (Jencks et al. 1988; Hannan et al. 1995).
To determine which risk factors should be included in the model, a multivariate logistic regression model was fit using stepwise forward selection with a significance level to enter of p<0.01 and a significance level to stay of p<0.05. Only interactions involving the most important main effects (age and infarct site) were examined. The resulting risk-adjustment model was internally validated by applying the model developed using the estimation sample to the validation sample and testing the equality of the coefficients. The validated risk-adjustment instruments developed on New Jersey data were subsequently used in the predictive models for both New Jersey and New York. While we used logistic regression to construct our risk-adjustment models, for ease of interpretation a linear probability model with a dependent variable of mortality or procedure use for individual patients was employed for the final analyses after checking that the results achieved with these two approaches had qualitatively and quantitatively similar interpretations.
Results
Study Sample
The number of admissions for AMI patients in New Jersey and New York was roughly constant from year to year, deviating from one year to the next by no more than 5.7 percent in New Jersey and 5.5 percent in New York (Table 1). There are no systematic trends in the number of cases in the two states that would lead to differential changes in mortality rates. The relative stability supports our assumption that the number of patients admitted from one year to the next within the same geographic area was roughly constant, mitigating the need for risk adjustment. The percentage of uninsured patients was 5.9 percent in New Jersey in 1992, and it ranged from 5.7 to 6.2 percent from 1994 to 1996, while the percentage of uninsured patients in New York increased slightly from 3.6 percent in 1992 to 4.3–4.7 percent in 1994–1996. The risk characteristics of the uninsured population did not change significantly in the two states, and there were no systematic changes in the frequency of comorbidities that would bias the analysis toward finding worse outcomes in New Jersey post-reform.
Table 1.
Basic Characteristics of the Sample
| 1990 | 1991 | 1992 | 1993 | 1994 | 1995 | 1996 | |
|---|---|---|---|---|---|---|---|
| Admissions | |||||||
| New Jersey (n) | 11,157 | 11,796 | 12,122 | 12,411 | 12,257 | 12,449 | 12,707 |
| New York (n) | 27,694 | 27,600 | 29,217 | 29,088 | 29,471 | 29,759 | 28,913 |
| Proportion uninsured patients | |||||||
| New Jersey (%) | 4.4 | 5.6 | 5.9 | 6.1 | 5.9 | 5.7 | 6.2 |
| New York (%) | 3.3 | 3.4 | 3.6 | 3.8 | 4.5 | 4.3 | 4.7 |
| Average length of stay in days—insured patients | |||||||
| New Jersey | 10.0 | 9.9 | 9.7 | 9.2 | 8.6 | 8.2 | 7.8 |
| New York | 9.8 | 9.7 | 9.5 | 9.3 | 9.2 | 8.9 | 8.4 |
| Length of stay in days—uninsured patients | |||||||
| New Jersey | 9.9 | 8.9 | 9.1 | 8.5 | 8.0 | 7.1 | 7.5 |
| New York | 8.6 | 8.4 | 8.0 | 7.9 | 7.8 | 8.0 | 7.4 |
| Insured mortality rate (%) | |||||||
| New Jersey | 15.9 | 14.6 | 13.8 | 13.0 | 12.9 | 12.8 | 12.6 |
| New York | 14.2 | 13.8 | 12.8 | 12.4 | 11.6 | 11.3 | 11.0 |
| Uninsured mortality rate (%) | |||||||
| New Jersey | 9.7 | 9.8 | 7.8 | 7.5 | 8.4 | 9.7 | 8.3 |
| New York | 13.9 | 11.7 | 12.0 | 10.5 | 7.1 | 8.2 | 8.0 |
| Cardiac catheterization rate (%)—insured | |||||||
| New Jersey | 26.7 | 32.9 | 37.0 | 39.0 | 43.4 | 44.7 | 47.6 |
| New York | 21.9 | 26.4 | 31.5 | 34.9 | 38.9 | 44.3 | 47.3 |
| Cardiac catheterization rate (%)—uninsured | |||||||
| New Jersey | 28.1 | 37.2 | 44.0 | 45.3 | 42.8 | 45.5 | 51.1 |
| New York | 21.4 | 27.0 | 32.5 | 35.3 | 43.1 | 53.6 | 54.8 |
| Mechanical revascularization rate (%)—insured | |||||||
| New Jersey | 11.3 | 18.2 | 22.1 | 25.2 | 29.2 | 31.9 | 36.4 |
| New York | 8.3 | 11.6 | 16.9 | 20.5 | 25.0 | 30.9 | 35.0 |
| Mechanical revascularization rate—insured | |||||||
| New Jersey | 11.3 | 17.1 | 23.6 | 27.5 | 29.2 | 28.7 | 35.0 |
| New York | 6.5 | 10.4 | 16.2 | 19.5 | 26.8 | 36.1 | 39.5 |
Effects on Mortality
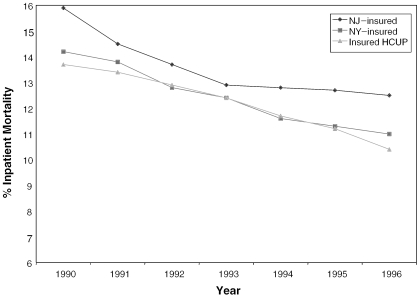
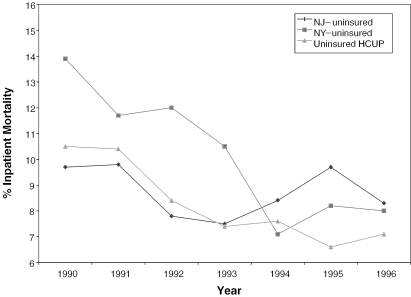
Mortality rates declined steadily from 1990 to 1996 for insured patients in New York (Figure 1a). The rate of decline from 1990 to 1992 was similar in New Jersey and New York (see test of controls, bottom of Table 2). Following the introduction of the new act in New Jersey in 1992, there was a leveling off of mortality rates in New Jersey (Figure 1a). Among the uninsured, mortality rates decreased from the pre-reform period 1990–1992 to the post-reform period 1994–1996 in New York, but increased from the pre-reform period to the post-reform period in New Jersey (Figure 1b). The trends observed in New York were similar to trends observed in the HCUP Nationwide Inpatient Sample.
Figure 1a.
AMI Mortality—New Jersey versus New York and HCUP States—Insured Only
Table 2.
The Effect of the New Jersey Health Care Reform Act on Mortality
| Insured Patients | Uninsured Patients | |||
|---|---|---|---|---|
| Risk Adjustment | Risk Adjustment | |||
| No | Yes | No | Yes | |
| Constant | 0.1436*** | −0.1499*** | 0.1369*** | −0.1287*** |
| New Jersey | 0.0114*** | .0079*** | −0.0341*** | −0.0284*** |
| 1991 | −0.0067** | −0.0025 | −0.0128 | −0.0080 |
| 1992 | −0.0159*** | −0.0092*** | −0.0190 | −0.0104 |
| 1993 | −0.0193*** | −0.0108*** | −0.0313** | −0.0217 |
| 1994 | −0.0276*** | −0.0166*** | −0.0652*** | −0.0517*** |
| 1995 | −0.0308*** | −0.0148*** | −0.0543*** | −0.0369*** |
| 1996 | −0.0337*** | −0.0170*** | −0.0561*** | −0.0450*** |
| Interaction—NJ and 1993 | −0.0054 | −.0034 | 0.0047 | 0.0064 |
| Interaction—NJ and 1994 | 0.0020 | 0.0052 | 0.0469** | 0.0491*** |
| Interaction—NJ and 1995 | 0.0035 | 0.0021 | 0.0490** | 0.0519*** |
| Interaction—NJ and 1996 | 0.0045 | 0.0047 | 0.0367* | 0.0428*** |
| Age | 0.0030*** | 0.0035*** | ||
| Female sex | 0.0340*** | 0.0447*** | ||
| Anterior MI | −0.0791*** | 0.0112 | ||
| Inferior MI | −0.0741*** | −0.0450 | ||
| Other MI | 0.2264*** | 0.2363*** | ||
| Previous CABG | −0.0168*** | 0.0067 | ||
| Congestive heart failure | −0.0022 | −0.0445 | ||
| Complications of diabetes | 0.0175*** | 0.0314 | ||
| Cancer | 0.1308*** | 0.2866*** | ||
| Chronic renal failure | 0.0992*** | 0.0483 | ||
| Nutritional disorders | 0.1279*** | 0.0917 | ||
| Pacemaker | −0.0224*** | −0.0031 | ||
| Number of observations | 273,877 | 273,877 | 12,763 | 12,763 |
| F value | 34.8 | 95.3 | 5.2 | 45.3 |
| Adjusted R2 | .001 | .09 | .004 | .094 |
| Test of controls (p-value) | 1.74 (.17) | 0.83 (.44) | 0.85 (.43) | 1.24 (.29) |
Asterisks indicate the level of significance
<.05
<.01
<.001.
Figure 1b.
AMI Mortality—New Jersey versus New York and HCUP States—Uninsured Only
Table 2 provides information about the statistical significance of the changes described in Figures 1aFigures 1b. The values for the interactions between New Jersey and 1994 through 1996 are the coefficients of greatest interest, because January 1, 1994 was when the reforms that encouraged price competition were fully implemented. The values for insured patients were positive and indicate that the mortality rate in New Jersey increased by 0.20 to 0.52 percentage points relative to New York from 1990–1992 to 1994–1996, but this was too small an increase to be statistically significant. Effects were much larger for the uninsured, whose mortality rate in New Jersey increased 3.7 to 5.2 percentage points from 1990–1992 to 1994–1996 relative to New York. This change represents a relative increase of approximately 41 to 57 percent in mortality relative to the 1990–1992 New Jersey baseline mortality rate of 9.1 percent.
Sensitivity Analyses
To further assess whether differences measured between New Jersey and New York were attributable to the reform in New Jersey and not to changes in New York, we compared the trend in AMI mortality rates in these two states with those in the Nationwide Inpatient Sample constructed by the HCUP. After eliminating patients who met our exclusion criteria, 364,273 AMI patients remained. We used the NIS with and without sample weights and found no qualitative or quantitative differences in interpretation.
We also tested the sensitivity of our results to a length-of-stay cutoff of less than three days for patients who were discharged alive, by rerunning our models using a length-of-stay cutoff of less than two days. There were no significant changes in the size of the relative increase in mortality among the insured or uninsured using this different cutoff.
Effects on Cardiac Procedure Utilization
The mechanism whereby AMI in-hospital mortality in New Jersey worsened relative to New York is unclear, but one contributing factor may have been differences in the rate of utilization of cardiac procedures. From 1990 to 1996, the rate of utilization of cardiac catheterization steadily increased in both states. The rate of increase from 1990 to 1992 was similar in New Jersey and New York (see test of controls, Table 3), but the rate of increase in New Jersey was slower than in New York after 1992. For insured patients, the catheterization rate in New Jersey was 32.2 percent in 1990–1992, and it increased less than the catheterization rate in New York by 1.1 to 5.4 percentage points from 1990–1992 to 1994–1996. For uninsured patients, the catheterization rate in New Jersey was 36.4 percent in 1990–1992, and it increased less than the catheterization rate in New York by 9.4 to 17.3 percentage points from 1990–1992 to 1994–1996.
Table 3.
The Effect of the New Jersey Health Care Reform Act on Cardiac Catheterization Rates
| Insured Patients | Uninsured Patients | |||
|---|---|---|---|---|
| Risk Adjustment | Risk Adjustment | |||
| No | Yes | No | Yes | |
| Constant | 0.2167*** | 0.8524*** | 0.1980*** | 0.4046*** |
| New Jersey | 0.0560*** | 0.0593*** | 0.0916*** | 0.0842*** |
| 1991 | 0.0495*** | 0.0461*** | 0.0766*** | 0.0729*** |
| 1992 | 0.0980*** | 0.0933*** | 0.1364*** | 0.1271*** |
| 1993 | 0.1325*** | 0.1279*** | 0.1548*** | 0.1478*** |
| 1994 | 0.1721*** | 0.1638*** | 0.2334*** | 0.2206*** |
| 1995 | 0.2256*** | 0.2121*** | 0.3379*** | 0.3193*** |
| 1996 | 0.2564*** | 0.2444*** | 0.3502*** | 0.3397*** |
| Interaction—NJ and 1993 | −0.0145* | −0.0185** | −0.0088 | 0.0022 |
| Interaction—NJ and 1994 | −0.0106 | −0.0164** | −0.0948*** | −0.0979*** |
| Interaction—NJ and 1995 | −0.0512*** | −0.0483*** | −0.1729*** | −0.1731*** |
| Interaction—NJ and 1996 | −0.0538*** | −0.0522*** | −0.1289*** | −0.1374*** |
| Number of observations | 273,877 | 273,877 | 12,762 | 12,762 |
| F value | 742.1 | 1285.5 | 52.3 | 36.8 |
| Adjusted R2 | 0.03 | 0.12 | .04 | .08 |
| Test of controls (p-value) | 2.5 (0.8) | 1.8 (.17) | 1.9 (.14) | 1.9 (.16) |
Asterisks indicate the level of significance:
<.05,
<.01,
<.001.
From 1990 to 1996, the rate of utilization of mechanical revascularization also steadily increased in both states. The rate of increase from 1990 to 1992 was similar in New Jersey and New York for the uninsured (see test of controls, Table 4), and the rate of increase in New Jersey was slower than in New York for both the insured and uninsured after 1992. For insured patients, the mechanical revascularization rate in New Jersey was 17.2 percent in 1990–1992, and it increased less than the revascularization rate in New York by 0.3 to 4.0 percentage points from 1990–1992 to 1994–1996. For uninsured patients, the mechanical revascularization rate in New Jersey was 17.3 percent in 1990–1992, and it increased less than the mechanical revascularization rate in New York by 4.0 to 14.1 percentage points from 1990–1992 to 1994–1996.
Table 4.
Effect of the New Jersey Health Care Reform Act on Mechanical Revascularization Rates (Angioplasty or CABG)
| Insured Patients | Uninsured Patients | |||
|---|---|---|---|---|
| Risk Adjustment | Risk Adjustment | |||
| No | Yes | No | Yes | |
| Constant | 0.0772*** | 0.3934*** | 0.0589*** | 0.0513 |
| New Jersey | 0.0501*** | 0.0541*** | 0.0644** | 0.0651*** |
| 1991 | 0.0433*** | 0.0415*** | 0.0460* | 0.0455** |
| 1992 | 0.0925*** | 0.0920*** | 0.1072*** | 0.1049*** |
| 1993 | 0.1281*** | 0.1284*** | 0.1363*** | 0.1349*** |
| 1994 | 0.1726*** | 0.1710*** | 0.2086*** | 0.2031*** |
| 1995 | 0.2314*** | 0.2266*** | 0.3025*** | 0.2954*** |
| 1996 | 0.2729*** | 0.2701*** | 0.3359*** | 0.3319*** |
| Interaction—NJ and 1993 | −0.0035 | −0.0068 | −0.0152 | 0.0132 |
| Interaction—NJ and 1994 | −0.0075 | −0.0135** | −0.0404 | −0.0440 |
| Interaction—NJ and 1995 | −0.0395*** | −0.0399*** | −0.1388*** | −0.1408*** |
| Interaction—NJ and 1996 | −0.0362*** | −0.0374*** | −0.1085*** | −0.1132*** |
| Number of observations | 273,878 | 273,878 | 12,762 | 12,762 |
| F value | 1177 | 1005.8 | 67.8 | 33.0 |
| Adjusted R2 | .05 | .10 | .05 | .07 |
| Test of controls | 15.3 (.00) | 13.6 (.00) | .03 (.70) | .03 (.72) |
Asterisks indicate the level of significance:
<.05,
<.01,
<.001.
Alternative Explanations for Observed Effects
Several other possible explanations for the differential change in mortality rates between New Jersey and New York were explored. One such explanation was that the length of stay decreased more in New York than in New Jersey during this time period. However, average length of stay for both the uninsured and all patients decreased more in New Jersey than in New York from 1992 to 1996 (Table 1).
A second explanation was that more procedures were done in fewer centers over time in New York relative to New Jersey, because higher hospital volume is known to be associated with better procedural outcomes. The number of mechanical revascularizations per provider that performed mechanical revascularization in the two states increased by 62.9 percent in New Jersey from 1992 to 1996 compared with 94.7 percent in New York. However, the number of mechanical revascularizations per provider was consistently higher in New Jersey throughout this time period, so it is unclear what impact these changes may have had.
Another possible explanation for differences in relative mortality rates is the introduction of policy reforms in New York, such as the Cardiac Surgery Reporting System that was introduced in New York in 1989 (Hannan et al. 1994). However, other investigators have shown that this system did not change mortality trends for CABG patients in New York relative to those in Massachusetts and some other states (Ghali et al. 1997). Furthermore, the changes in CABG mortality rates that occurred in New Jersey and New York during the time period of this study cannot explain the differences in mortality rates for AMI that we observed in the two states. During the two years before the change in New Jersey's law, mortality among AMI patients who received CABG decreased 14.6 percent in New Jersey and 27.6 percent in New York; during the four years after the change in New Jersey's law, mortality among AMI patients who received CABG decreased by 15.8 percent in New Jersey but increased 7.1 percent in New York. Therefore, the changes in CABG mortality were in the opposite direction of those needed to explain our results. (New Jersey also implemented a cardiac surgery reporting system, but these data were first released in November 1997.)
Another potential concern is that the HCRA could have led to increased transfer rates in New Jersey. Because we excluded pretransfer hospitalizations from our data, a significant relative increase in the rate of transfers in New Jersey could have led to a relative increase in the measured inpatient mortality rates in New Jersey. Among insured patients, the relative difference in transfer rates between New Jersey and New York narrowed from 5.8 percentage points (1990–1992) to 4.5 percentage points (1994–1996). Among the uninsured, there was a slight relative increase in the difference in transfer rates between New Jersey and New York from 1.4 percentage points to 3.0 percentage points. This relative difference, however, increased the AMI mortality rate only by less than 0.2 percentage points in New Jersey from 1994 to 1996. Since our effect sizes among the uninsured were between 3.7 and 5.2 percentage points, this did not affect the statistical significance of our results.
The decrease in the rate at which AMI patients received mechanical revascularization in New Jersey relative to New York raises the question of whether physicians substituted thrombolytic therapy for mechanical revascularization in these patients. We could not examine thrombolysis rates directly because thrombolysis was not accurately recorded in the discharge data. (There were only about 30 cases per state per year.) Therefore, we examined mechanical revascularization rates among patients for whom thrombolytic therapy was contraindicated, for example, those with acute gastrointestinal bleeding, a history of stroke, or acute peptic ulcer disease (n=19,671). Using risk adjustment, we found a relative reduction in mechanical revascularization rates in New Jersey relative to New York in these patients from 1990–1992 to 1994–1996 of 3.2 percentage points (p=.003). Because relative mechanical revascularization rates decreased in New Jersey patients who were not candidates for thrombolysis, we believe that substitution of thrombolysis did not explain the relative decrease in New Jersey's overall mechanical revascularization rates.
Comment
Our findings indicate that the quality of care for uninsured patients with AMIs in New Jersey declined following implementation of a law that permitted price competition between hospitals and reduced subsidies for hospital care for the uninsured. These results are consistent with the hypothesis that the uninsured were particularly vulnerable in the switch to a market-based system, given the cuts in subsidies for their care.
We are confident that the findings for the overall population were not caused by changes in patient severity over time because we studied patients who nearly always are admitted to the hospital when the diagnosis is suspected, regardless of their severity of illness, and because we found similar coefficients and significance levels with and without risk adjustment. While examination of outcomes among the entire population of AMI patients within the state should not require risk adjustment, the population of uninsured patients may change over time and thus some of the findings observed among the uninsured may be attributable to changes in patient mix not measurable with our administrative data. The fact that the decline in mortality over time observed in New York was similar to that found in the HCUP NIS as well as in other studies (Kessler and McClellan 2000) supports the premise that the observed effects were in fact due to reforms in New Jersey and not changes in New York.
A probable explanation for the increased mortality in New Jersey patients was a change in the way these patients were managed in the hospital. While the number of hospitalized uninsured patients with AMIs did not change greatly over time, suggesting that access to hospital admission was maintained for medical emergencies post-1992, the relative decreases in cardiac catheterization and mechanical revascularization rates in New Jersey (Tables 3 and 4) suggest that patients were treated differently once they were admitted. These differences included less frequent use of cardiac catheterization and mechanical revascularization, which we measured, but it also may have included other changes that we could not measure, for example, less frequent use of aspirin and beta blockers, delays in appropriate diagnosis or treatment, lower nurse-to-patient ratios, the use of ionic versus nonionic contrast dye for cardiac catheterization, or less successful resuscitation of patients who suffered cardiac arrests or other complications of AMI. We also could not examine other potential explanations, such as increased delays among uninsured New Jersey patients in presenting to emergency rooms or increases in transport time to New Jersey hospitals. In assessing these results, other limitations should be kept in mind. Our analysis is limited to only one diagnosis, and thus we do not know whether these results are generalizable to patients with other diagnoses. There was no available information on transaction prices paid by insurance companies to hospitals, making it impossible to directly examine cost-quality tradeoffs, although numerous investigators have shown that this type of reform is likely to cut costs and shrink hospital margins (Zwanziger and Melnick 1988; Dranove, Shanley, and White 1993).
Few other studies have directly examined how process or outcome measures change in response to changes in hospital financial incentives, and it is, therefore, difficult to draw overarching conclusions from the existing literature. In the shift to price competition in California, the amount of uncompensated care, financed out of hospital net revenues, was reduced in more competitive hospital markets relative to less competitive hospital markets (Gruber 1994). Using one year of state-level data, Shortell and colleagues found that expected mortality rates for 16 conditions ranging from total knee replacement to congestive heart failure were higher in states with stringent rate-setting programs and for states with higher HMO penetration (Shortell and Hughes 1988), but this study did not directly assess the effects of competition and the higher mortality rates measured may have been attributable to unmeasured differences in case mix. In a Medicare-only population, Kessler and McClellan (2000) demonstrated that while competition had ambiguous effects on social welfare before 1991 (higher costs and inconsistent effects on quality), after 1990 hospital competition appeared to both lower costs and improve outcomes. Since their study is based on changes in hospital market concentration using a national sample, it measures the effect of hospital exit from markets under a mixture of state-level regulatory regimes, making it difficult to infer from their results what effect a switch to price competition such as that in New Jersey would be expected to have. In addition, by studying only Medicare patients, they measured outcomes of financial incentives different from the ones in New Jersey.
Our results demonstrate that market-based reforms designed to reduce the rate of increase in health care costs may affect the quality of care. The magnitude of the effects found raises concerns about the impact of cost-saving reforms on the quality of care provided to the uninsured. Cost-saving reforms are more likely to affect the quality of care provided to the uninsured because care for the uninsured is funded primarily from revenues in excess of costs, and cost-saving reforms put increased pressure on those hospital margins. Further reform efforts need to take careful stock not only of cost savings, but also of the potential for reductions in the quality of care.
Acknowledgments
We gratefully acknowledge helpful suggestions from seminar participants at the National Bureau of Economic Research Summer Institute, the Association of Public Policy and Management, the American Economic Association, Brigham and Women's Hospital, the University of Pennsylvania, Stanford University, the University of Pittsburgh, and the University of Cincinnati, Dartmouth College. We also thank the several anonymous reviewers of this manuscript.
Footnotes
Support for this research came from the VA Center for Health Equity Research and Promotion, the Agency for Health Care Policy and Research (grant no. RO3 HS09325-01) and National Institutes of Health (NIH) grant no. 5-T32-GM-07170.
References
- Antman EM, Kuntz KM. “The Length of the Hospital Stay after Myocardial Infarction.”. New England Journal of Medicine. 2000;342(11):808–10. doi: 10.1056/NEJM200003163421109. [DOI] [PubMed] [Google Scholar]
- Arrow KJ. “Uncertainty and the Welfare Economics of Medical Care.”. American Economic Review. 1963;53:941–73. [Google Scholar]
- Bovbjerg RR, Cuellar AE, Holahan J. Market Competition and Uncompensated Care Pools. Washington, DC: Urban Institute; 2000. [Google Scholar]
- Campbell DT, Stanley JC. Experimental and Quasi-Experimental Designs for Research. Dallas, TX: Houghton Mifflin; 1963. [Google Scholar]
- Cantor JC. “Health Care Unreform: The New Jersey Approach.”. Journal of the American Medical Association. 1993;270(24):2968–70. [PubMed] [Google Scholar]
- Chung JC, Meltzer D. “Effects of Competition under Prospective Payment on Hospital Costs among High and Low Cost Admissions: Evidence from California, 1983–1993.”. 2000 Paper presented at National Bureau of Economic Research Summer Institute, Cambridge, MA. [Google Scholar]
- Davies SM, Geppert J, McClellan M, McDonald K, Romano P, Shojaniu K. Refinement of the HCUP Quality Indicators. Rockville, MD: Agency for Healthcare Research and Quality; 2000. Technical review no4 (prepared by UCSF–Stanford Evidence-based Practice Center under contract no290-97-0013)AHRQ publication no01-0035. [PubMed] [Google Scholar]
- Dranove D, Shanley M, White W. “Price and Concentration in Hospital Markets: The Switch from Patient-Driven to Payer-Driven Competition.”. Journal of Law and Economics. 1993;36(1):179–203. [Google Scholar]
- Farley DE. 1985. Competition among Hospitals: Market Structure and Its Relation to Utilization, Costs and Financial PositionResearch note 7Rockville, MD: Hospital Studies Program, National Center for Health Services Research.
- Gaynor M, Haas-Wilson D. “Change, Consolidation, and Competition in Health Care Markets.”. Journal of Economic Perspectives. 1999;13(1):141–64. doi: 10.1257/jep.13.1.141. [DOI] [PubMed] [Google Scholar]
- Ghali W, Ash A, Hall R, Moskowitz M. “Statewide Quality Improvement Initiatives and Mortality after Cardiac Surgery.”. Journal of the American Medical Association. 1997;277(5):379–82. [PubMed] [Google Scholar]
- Greenfield S, Aronow HU, Elashoff RM, Watanabe D. “Flaws in Mortality Data: The Hazards of Ignoring Comorbid Disease.”. Journal of the American Medical Association. 1988;260(15):2253–5. [PubMed] [Google Scholar]
- Greenfield S, Bianoco DM, Elashoff RM, Ganz PA. “Patterns of Care Related to Age of Breast Cancer Patients.”. Journal of the American Medical Association. 1987;257(20):2766–70. [PubMed] [Google Scholar]
- Gruber J. “The Effect of Competition Pressures on Charity: Hospital Responses to Price Shopping in California.”. Journal of Health Economics. 1994;13 (2):183–212. doi: 10.1016/0167-6296(94)90023-x. [DOI] [PubMed] [Google Scholar]
- Hannan EL, Siu AL, Kumar D, Kilburn H, Chassin MR. “The Decline in Coronary Artery Bypass Graft Surgery Mortality in New York StateThe Role of Surgeon Volume.”. Journal of the American Medical Association. 1995;273(3):209–13. [PubMed] [Google Scholar]
- Hannan EL, Kilburn H, Jr, Raez M, Shields E, Chassin MR. “Improving the Outcomes of Coronary Artery Bypass Surgery in New York State.”. Journal of the American Medical Association. 1994;271(10):761–6. [PubMed] [Google Scholar]
- Held P, Pauly M. “Competition and Efficiency in the End-Stage Renal Disease Program.”. Journal of Health Economics. 1983;2(2):95–118. doi: 10.1016/0167-6296(83)90001-2. [DOI] [PubMed] [Google Scholar]
- Iezzoni LI, editor. Risk Adjustment for Measuring Health-Care Outcomes. Ann Arbor, MI: Health Administration Press; 1994. [Google Scholar]
- Jencks SF, Daley J, Draper D, Thomas N, Lenhart G, Walker J. “Interpreting Hospital Mortality Data: The Role of Clinical Risk Adjustment.”. Journal of the American Medical Association. 1988;260(24):3611–6. [PubMed] [Google Scholar]
- Kessler DP, McClellan MB. “Is Hospital Competition Socially Wasteful?”. Quarterly Journal of Economics. 2000;115(2):577–615. [Google Scholar]
- Luft HS, Romano PS. 1996. Second Report of the California Hospital Outcomes ProjectAcute Myocardial InfarctionVol2: Technical AppendixSacramento, CA: California Office of Statewide Health Planning and Development.
- Pashos CL, Newhouse JP, McNeil BJ. “Temporal Changes in the Care and Outcomes of Elderly Patients with Acute Myocardial Infarction, 1987 through 1990.”. Journal of the American Medical Association. 1993;270(15):1832–6. [PubMed] [Google Scholar]
- Robinson JC, Luft HS. “Competition and the Cost of Hospital Care: 1972–1982.”. Journal of the American Medical Association. 1987;257(23):3241–5. [PubMed] [Google Scholar]
- Robinson JC, Luft HS. “The Impact of Hospital Market Structure and Patient Volume, Average Length of Stay, and the Cost of Care.”. Journal of Health Economics. 1985;4(4):333–56. doi: 10.1016/0167-6296(85)90012-8. [DOI] [PubMed] [Google Scholar]
- Shortell SM, Hughes E. “The Effects of Regulation, Competition, and Ownership on Mortality Rates among Hospital Inpatients.”. New England Journal of Medicine. 1988;318 (17):1100–7. doi: 10.1056/NEJM198804283181705. [DOI] [PubMed] [Google Scholar]
- Udvarhelyi IS, Gastonis C, Epstein AM, Pashos CL, Newhouse JP, McNeil BJ. “Acute Myocardial Infarction in the Medicare Population: Process of Care and Clinical Outcomes.”. Journal of the American Medical Association. 1992;268(18):2530–6. [PubMed] [Google Scholar]
- Volpp KG, Siegel B. “State Model: New JerseyLong-Term Experience with All-Payer State Rate Setting.”. Health Affairs. 1993;12(2):59–65. doi: 10.1377/hlthaff.12.2.59. [DOI] [PubMed] [Google Scholar]
- Ware JE, Jr, Brook RH, Rogers WH, Keeler EB, Davies AR, Sherbourne CO, Goldberg GA, Camp P, Newhouse JP. “Comparison of Health Outcomes at a Health Maintenance Organization with Those of Fee-for-Service Care.”. Lancet. 1986;1(8488):1017–22. doi: 10.1016/s0140-6736(86)91282-1. [DOI] [PubMed] [Google Scholar]
- Ware JE, Jr, Bayliss MS, Rogers WH, Kosinski M, Tarlov AR. “Differences in 4-year Health Outcomes for Elderly and Poor, Chronically Ill Patients Treated in HMO and Fee-for-Service SystemsResults from the Medical Outcomes Study.”. Journal of the American Medical Association. 1996;276(13):1039–47. [PubMed] [Google Scholar]
- Weisbrod BA. “Rewarding Performance That is Hard to Measure: The Role of Nonprofit Organizations.”. Science. 1989;244(May):541–6. doi: 10.1126/science.244.4904.541. [DOI] [PubMed] [Google Scholar]
- Zwanziger J, Melnick G. “The Effects of Hospital Competition in the Medicare PPS Program on Hospital Cost Behavior in California.”. Journal of Health Economics. 1988;7(4):301–20. doi: 10.1016/0167-6296(88)90018-5. [DOI] [PubMed] [Google Scholar]
- Zwanziger J, Melnick G, Bamezai A. “The Effect of Selective Contracting on Hospital Costs and Revenues.”. Health Services Research. 2000;35(4):849–67. [PMC free article] [PubMed] [Google Scholar]