Abstract
Objective
We estimate long-term health care costs of former smokers compared with continuing and never smokers using a retrospective cohort study of HMO enrollees. Previous research on health care costs associated with former smokers has suggested that quitters may incur greater health care costs than continuing smokers, therefore, getting people to quit creates more expensive health care consumers. We studied the trend in cost for former smokers over seven years after they quit to assess how the cessation experience impacts total health care cost.
Data Sources/Study Setting
Group Health Cooperative (GHC), a nonprofit mixed model health maintenance organization in western Washington state.
Study Design
Retrospective cohort study using automated and primary data collected through telephone interviews.
Principal Findings
We find that former smokers' costs are significantly greater (p<.05) in the year immediately following cessation relative to continuing smokers, but former smokers' costs fall in year two. This decrease maintains throughout the six-year follow-up period. Although former smokers cost more than continuing smokers in the year after cessation, this increase appears to be transient. Long-term costs for former smokers are not statistically different from those of continuing smokers and cumulative health care expenses are lower by the seventh year postquit. Our evidence suggests that smoking cessation does not increase long-term heath care costs.
Conclusions
Health care costs among former smokers increase relative to continuing smokers in the year after cessation but fall to a level that is statistically indistinguishable in the second year postquit. Any net increase in costs among former smokers relative to continuing smokers appears compensated for within two years post-quit and is maintained for at least six years after cessation.
Keywords: Cost of smoking, smoking cessation
Various studies demonstrate that smoking results in greater health care costs (Hodgson 1992; Miller et al. 1998; Bartlett et al. 1994; Pronk et al. 1999; Zhang et al. 1999; Miller, Ernst, and Collin 1999) that may account for 6–8 percent of national health care spending in the United States (Warner, Hodgson, and Carroll 1999). There are also clear health benefits that accrue to persons who stop smoking that should translate into long-term cost savings for former smokers and their health care sponsors (Bartecchi, MacKenzie, and Schyle 1994; U.S. Department of Health and Human Services 1990; Ockene et al. 1992; Gritz et al. 1993; Rosal et al. 1998; Halpern et al. 2001). Although smoking increases health care costs, there is also evidence that former smokers cost more than continuing smokers, at least in the immediate post-quit period (Wagner et al. 1995; Pronk et al. 1999). Other research, however, suggests that smoking may not increase net health care costs or that smoking related costs may not be as great as commonly believed (Barendregt, Bonneux, and van der Maas 1997; Leu and Schaub 1983).
The expectation that smoking does not increase net national health care spending, and by extension that savings may not result from smoking cessation, does not consider the context in which this research has been conducted. The result that smokers cost less than nonsmokers is based on a social analytic perspective that derives almost entirely from smokers dying younger and more quickly than never smokers (Leu and Schaub 1983; Barendregt, Bonneux, and van der Maas 1997). Studies conducted on a cross-sectional basis for specific market segments show that smoking does impose an economic burden on the health care system (Miller et al. 1998; Bartlett et al. 1994; Pronk et al. 1999; Zhang et al. 1999). Although former smokers may be more expensive than continuing smokers in the short run, this effect ought to be transient because health care use among former smokers is likely to fall to levels at or below those of continuing smokers within a few years (Wagner et al. 1995). The ultimate source of this post-quit transient cost increase is also relevant. Former smokers may seek medical care that they had delayed while smoking and incur greater short-term costs as unmet health care needs are addressed. There is also evidence that smoking cessation coincides with, or immediately follows, a health event that motivates the effort to quit (Bartecchi, MacKenzie, and Schyle 1994; U.S. Department of Health and Human Services 1990; Ockene et al. 1992; Gritz et al. 1993; Rosal et al. 1998). Quitting does not necessarily create more expensive people, rather, quitting likely occurs in the midst of an already expensive health episode.
Although these issues have been addressed by previous research, this literature has several limitations that contribute to an ongoing debate. First, much of the extant cost research is based on simulations rather than on the actual experience of continuing and former smokers (Leu and Schaub 1983; Barendregt, Bonneux, and van der Maas 1997). Second, research examining the experience of former smokers has not been conducted over a long enough time period to assess whether post-quit cost increases are eventually compensated for by subsequent decreases in utilization and cost. Third, previous studies have not always explored the full range of health care utilization and have often focused on components of health care use, rather than total cost (Vogt and Schweitzer 1985; Wagner et al. 1995). Finally, the focus of earlier studies has often been on either smokers and never smokers or former smokers and continuing smokers (Vogt and Schweitzer 1985; Wagner et al. 1995). Lacking is comprehensive research evaluating the cost experience of former smokers, continuing smokers, and never smokers.
This study extends the literature by examining the health service cost experience for seven years following successful cessation among former smokers relative to continuing smokers and never smokers who receive care from an established managed health care provider. We are not aware of previous research that has used a population-based managed care sample to estimate the change in costs over this long a time period among former smokers with both continuing and never smokers included as a comparison.
Research Setting and Subjects
Setting
This study was conducted at Group Health Cooperative of Puget Sound (GHC), an integrated health service delivery system providing the full range of health services on a population basis to approximately 400,000 individuals in western Washington state. Group Health Cooperative is the nation's largest consumer governed health care organization; its 650 staff physicians provide health services through 28 primary care clinics, two specialty centers, and one hospital. In addition, GHC has contractual relationships with external physicians and other health service professionals and facilities that also provide services to GHC enrollees.
Subjects
Subjects for this study were drawn from past and present GHC enrollees whose smoking status was originally determined through a population-based random telephone survey administered between July 1990 and May 1991. Subjects were aged 18 and older at the time of the 1990–1991 survey and included 8,013 persons enrolled in GHC at that time. This survey was conducted to identify subjects for a population-based, randomized trial evaluating the effects of general and personalized self-help materials and outreach telephone counseling among nonvolunteer smokers (Curry, Grothaus, and Wagner 1995). The project completed 5,364 surveys and identified 3,024 never smokers, 1,137 current smokers, and 1,203 former smokers. Never smokers reported smoking fewer than one hundred cigarettes over their entire life. Former smokers reported smoking at least one hundred cigarettes over their lifetime, but answered “no” when asked if they smoked at the present time. An additional question ascertained the length of time since they last smoked “at least one cigarette a day.” Current smokers reported smoking at least one hundred cigarettes over their lifetime and answered “yes” when asked if they smoked at the present time. Because there was no requirement that self-reported current smokers use cigarettes daily, current smokers included nondaily smokers.
Sampling Strategy
Smoking status may change over time. To estimate long-term health care costs associated with smoking and smoking cessation, we needed to reestablish smoking status before assessing health care costs. In designing the sample frame for a follow-up survey, we were faced with several constraints. Group Health cooperative's information systems report costs only from 1990 forward so there is limited follow-up data on former smokers who quit before that time. There would also be little follow-up cost data for persons who disenrolled from GHC shortly after the baseline survey was administered. Further, contact information for disenrollees is valid only to the point they discontinued their GHC coverage, and addresses and phone numbers among longer-term disenrollees may therefore be less accurate.
After analyzing smoking status and enrollment patterns among subjects identified as smokers and formers smokers at baseline, we sampled all smokers and former smokers who reported quitting within five years of the baseline survey and who were still enrolled in GHC through December 1994. This included 1,005 individuals: 716 current smokers and 289 subjects who reported quitting within five years of baseline. Of these, 261 (26 percent) had disenrolled from GHC after December 31, 1994. We attempted to contact these 1,005 individuals for a 10–15-minute interview via telephone in August 1998.
The current study also includes a random sample of 489 never smokers. These individuals were respondents to the 1990–1991 baseline survey who indicated that they had not smoked one hundred or more cigarettes in their lifetime and who remained enrolled in GHC through December 1994. We did not resurvey these individuals because we assumed that they were unlikely to start smoking as adults.
Health Care Costs
Beginning in January 1990, GHC information systems capture and fully allocate health service costs for all internal services provided directly by GHC as well as for claims for covered services that enrollees receive from contracted providers (Fishman et al. 1997). To allocate costs, a resource intensity weight is assigned to each service, procedure, pharmacy fill, or diagnostic test provided by GHC or its contracted providers. The methodology for computing the resource intensity weight is unique to each cost center in the delivery system. For some service and cost centers, such as pharmacy, assigned costs are unweighted acquisition charges from suppliers. Costs that are not directly related to the delivery of health services, such as insurance administration and marketing, are not allocated to enrollees and are not reported in the analyses presented below. Any plan margin is included in this allocation, but because GHC is organized as a nonprofit consumer-governed cooperative, these revenues are redistributed into the delivery system.
Costs allocated to GHC enrollees for services received from providers outside the GHC group model are GHC's payment to those providers. Although such services will more likely reflect market prices (services bought “on the margin”) than services provided internally, they are the financial liability GHC incurs in delivering health services to its enrollees. These services represent approximately half of inpatient admissions and half of all specialty visits (or 15 percent of all ambulatory encounters) during a typical year. Costs to non-GHC providers represent approximately 25 percent of total delivery system costs in a typical year (Fishman et al. 1997). The cost allocation system allows the identification of costs for specific encounters and services as well as aggregation of costs for individuals over time.
Methods
Each subject is assigned an index date relevant to their smoking status. The index date for never smokers and continuing smokers is the date that they completed the baseline telephone survey conducted during 1990–1991. We chose this date because it is the earliest point at which smoking status was verified. The index date for former smokers is the date they quit, which we determined from the baseline survey conducted in 1990–1991 and verified at the follow-up conducted in 1998, or determined during the 1998 survey for subjects who had stopped smoking between the two surveys.
Cost and utilization for each 12-month period postindex is identified for all subjects from GHC automated information systems from January 1990 through December 1998. Therefore, the first postindex year among former smokers is the first 12-month period following successful cessation. The GHC cost information is reported in nominal dollars and we use the Seattle–Tacoma component of the Medical Care Consumer Price Index (MCPI) to adjust GHC costs for inflation (U.S. Department of Labor, Bureau of Labor Statistics 2001). All costs are reported in 2000 U.S. dollars.
We assume that total health care costs over time are a function of subject age, sex, smoking status, and overall health status. Among former and continuing smokers, costs are also assumed to be a function of the total number of years smoked and whether the subject was a heavy smoker, defined as smoking more than one pack of cigarettes a day on average (Sayette et al. 2001; Brauer et al. 1996).
Empirical estimation of this model requires time series methods that support complex variance structures caused by the intertemporal correlation of health care costs. We also face the challenge of missing data as GHC did not report cost data prior to January 1990, and our data include missing values for subjects who stopped smoking prior to that point. We also have truncated cost data for subjects that disenrolled from GHC after December 1994.
An additional empirical challenge in estimating the model is caused by the skewed distribution of health care costs, which results in nonnormally distributed regression residuals that limit the use of standard linear regression methods for estimating the model. To address this challenge we estimate health care costs over time using a Generalized Linear Model (GLM) multivariate regression (McCullagh and Nelder 1989). Following Blough et al. (Blough, Madden, and Hornbrook 1999), regression residuals are modeled based on the gamma distribution, an approach that has been demonstrated as an appropriate distribution for health care costs. To assess the sensitivity of our results to this choice of empirical specification we also estimated the model using Generalized Estimating Equations (GEE).
We adjust for baseline health status using a modified version of each individual's Chronic Disease Score (CDS) (Clark et al. 1995) for the six-month period prior to their index date. The CDS is a pharmacy-based measure of comorbidity and relative disease severity that classifies adults into one or more of 28 chronic conditions based on prescription drugs dispensed. We are able to calculate a CDS for all study participants because GHC has computerized pharmacy data from 1977 to the present. A score is produced from a regression equation that estimates expected health service cost as a function of age, sex, and the chronic condition classes in which drug fills are observed. Higher CDS values are therefore associated with expected higher future health care costs. Case-mix adjustment is a challenge when modeling the cost of tobacco because of the interaction between smoking and many chronic conditions used to assess case mix. To address this we have created a modified CDS for this study by estimating an Ordinary Least Squares regression model with the unadjusted CDS as a dependent variable and subject age, sex, and smoking status as independent variables. The difference between this predicted value and the unadjusted CDS is included as a covariate in the GLM regression used to estimate health care costs over time.
Partial-year costs for any 12-month-period postindex date in which a subject was not continuously enrolled in GHC were annualized by multiplying observed costs by the actual number of enrolled months, and dividing this product by 12. Chi-square tests of cost differences among smokers, former smokers, and never smokers at each year postindex are based on the gamma distributed regression results.
The GLM regression is estimated using the GENMOD procedure of the SAS software program (SAS Institute 1990). Because of the different eligibility periods present among individuals who are partially enrolled in GHC for any specific year, we provide robust standard error estimates using the Huber/White “sandwich” method (Huber 1981).
Results
Subject Characteristics
A total of 723 (72 percent) of 1,005 subjects completed the survey in August 1998. Ninety-two subjects (9.2 percent) refused the survey and we were unable to locate 181 subjects (15 percent). Seven subjects were too ill and two others did not speak English well enough to complete the telephone survey. Descriptive characteristics for the sample are provided in Table 1. Compared to continuing smokers, former smokers smoked for more years (p<.05), were more likely to be heavy smokers (p<.01), were older (p<.01), and were more likely to be female (p<.01). Never smokers were more likely to be female than either former (p<.05) or continuing smokers (p<.01). Former smokers had significantly higher Chronic Disease Scores (p<.01) than either current or never smokers, suggesting that former smokers are expected to cost more than either never or continuing smokers.
Table 1.
Sample Characteristics
| Smoking Status | |||
|---|---|---|---|
| Never Smokers | Former Smokers | Continuing Smokers | |
| N | 489 | 381 | 342 |
| Mean age at index date (SD) | 43.5 (11.4)* | 47.3 (12.3)@ | 42.4 (10.5) |
| Percent male | 37.1&,$ | 43.0@ | 48.8 |
| Mean years smoked (SD) | N/A | 26.0 (13.9)@@ | 25.3 (10.3) |
| Percent heavy smoker# | N/A | 29.1%@ | 15.5% |
| Mean Chronic Disease Score## (SD) | .89 (.82) | 1.38 (1.3)@ | 1.1 (2.3) |
Difference between Never and Former Smokers significant at p<.01.
Difference between Continuing and Former Smokers significant at p<.01.
Difference between Never and Continuing Smokers significant at p<.01.
Difference between Never and Former Smokers significant at p<.05.
Difference between Continuing and Former Smokers significant at p<.05.
Heavy smoker: Average of one or more packs of cigarettes a day when smoking.
Chronic Disease Score [Clark et al. 1995]: Pharmacy-based comorbidity/health status measure.
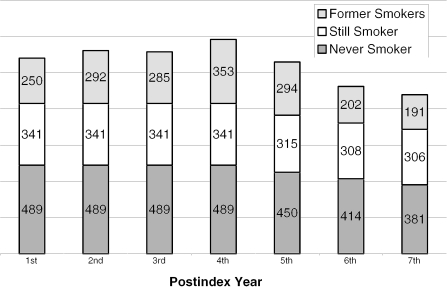
The distribution of subjects by smoking group and postindex follow-up data is presented in Figure 1. Follow-up cost data is available for all never and continuing smokers through postindex year four because we required that all subjects be continuously enrolled in GHC from baseline until December 1994. After that point we observe disenrollment from GHC among these groups at a rate lower than GHC's overall disenrollment rate of approximately 15 percent. This lower disenrollment rate is expected because longer-term enrollees are less likely to change health plans than more recently enrolled persons.
Figure 1.
Follow-up Data Availability by Index Year and Smoking Status
Among former smokers, we have two different patterns of follow-up data. We have missing follow-up cost data for former smokers that disenrolled from GHC after December 1994, and we also have missing follow-up data for former smokers who quit before GHC began collecting cost data in 1990. As we report in Figure 1, at least half of the former smokers we surveyed are represented in each postindex year with the largest number of former smokers in years three, four, and five postindex.
Health Care Costs over Time
Regression results are reported in Table 2. We estimate the model with a unique intercept for each smoking group and, due to collinearity constraints, we exclude the first-period postindex date for each smoking group from the regression. Therefore, the unique intercept for each group is estimated costs for the first period postindex. Regression coefficients for each smoking group for the second through sixth year postindex are expressed in relative terms to first year costs. Age (p<.001) and the smoking-adjusted Chronic Disease Score (p<.001) are associated with significantly greater costs over time. Male gender, years smoked, and whether a subject was a heavy smoker are negatively, but statistically insignificantly, associated with cost over time.
Table 2.
Generalized Linear Model Regression Results#
| Variable | Estimate | Standard Error* | P-value |
|---|---|---|---|
| Age | 0.021141 | 0.0041779 | 0.000 |
| Gender (male=1) | −0.1631995 | 0.1175306 | 0.165 |
| Years smoked | −0.0044493 | 0.0079547 | 0.576 |
| Amount Smoked (1 if more than one pack per day on average during period when smoker) | −0.1081014 | 0.1306493 | 0.408 |
| Smoking status adjusted Chronic Disease Score | 0.0004978 | 0.0000275 | 0.000 |
| Never Smoker Results | |||
| Never Smokers | 6.951912 | 0.1812939 | 0.000 |
| Never Smokers at 2nd year postindex date | −0.4552492 | 0.1449004 | 0.002 |
| Never Smokers at 3rd year postindex date | −0.2698587 | 0.1539378 | 0.080 |
| Never Smokers at 4th year postindex date | −0.267589 | 0.1515546 | 0.077 |
| Never Smokers at 5th year postindex date | −0.2801944 | 0.1348713 | 0.038 |
| Never Smokers at 6th year postindex date | −0.2894081 | 0.1181291 | 0.014 |
| Continuing Smoker Results | |||
| Continuing Smokers | 7.534945 | 0.306946 | 0.000 |
| Continuing Smokers at 2nd year postindex date | −0.473149 | 0.0908107 | 0.000 |
| Continuing Smokers at 3rd year postindex date | −0.4735299 | 0.1328942 | 0.000 |
| Continuing Smokers at 4th year postindex date | −0.2226533 | 0.1615293 | 0.168 |
| Continuing Smokers at 5th year postindex date | −0.174815 | 0.1418589 | 0.218 |
| Continuing Smokers at 6th year postindex date | −0.3593193 | 0.1478066 | 0.015 |
| Former Smoker Results | |||
| Former Smokers | 8.0235 | 0.2863548 | 0.000 |
| Former Smokers at 2nd year postindex date | −0.8872 | 0.1379016 | 0.000 |
| Former Smokers at 3rd year postindex date | −0.4282 | 0.2383935 | 0.072 |
| Former Smokers at 4th year postindex date | −0.4245 | 0.2932646 | 0.148 |
| Former Smokers at 5th year postindex date | −0.5444 | 0.1771111 | 0.002 |
| Former Smokers at 6h year postindex date | −0.25741 | 0.2381042 | 0.280 |
Generalized Linear Model estimated with an independent structure to the correlation matrix.
Standard Errors are based on the Huber/White “sandwich” estimate.
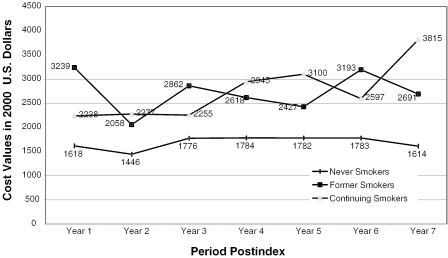
Mean nominal cost values for each smoking group over time are reported in Figure 2. The dollar amounts reported in Figure 2 are the mean values for Σt[exp(Σi xiβj)] where the subscript t represents each smoking group (never, former, and continuing smokers), i represents each individual subject, xi are the values for the independent variables in the model, and βj are the corresponding regression coefficients for those independent variables. These results were robust to empirical specification as we found almost identical costs over time using a GEE model to estimate model parameters.
Figure 2.
Health Care Costs over Time by Smoking Status
We summarize statistical tests of differences for each smoking group at each time period in Table 2. For convenience we report cost differences in dollar values, but the statistical tests are based on the gamma distributed regression results. We find a pattern of cost over time consistent with previous research. Costs among former smokers are significantly (p<.001) higher than continuing smokers in the first year postindex, and costs for former smokers fall significantly from year one to year two. Although there is some fluctuation over time, health care costs of former smokers are less than those of continuing smokers in four of the remaining six years, but the difference is statistically significant (p<.1) only in year seven postindex. These data replicate the first-year cost spike among former smokers demonstrated in previous studies: costs among former and continuing smokers are higher than never smokers in each year.
Cumulative Health Care Costs
This pattern of health care costs raises the issue of whether subsequent cost decreases among former smokers offset initial cost increases in the first year postindex relative to continuing smokers. We calculate the discounted or net present value (NPV) of health care costs for former and continuing smokers given by equations (1).
| (1) |
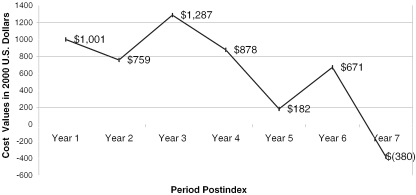
Where i=1 for former smokers and 2 for continuing smokers, t are the number of postindex periods where the first year postindex is defined as year 0, and r is the discount rate. We test the sensitivity of our analysis to alternative discount rates by calculating NPV for discount rates of 3, 5, and 7 percent, and report results for a 3 percent discount rate in Figure 3.
Figure 3.
Discounted Cumulative Cost Difference: Former versus Continuing Smokers
The Net Present Value analysis shows that even with the cost bounce among former smokers in years three and six, the spike in year one is compensated for by the decrease in year two, and this compensation holds throughout the six-year follow-up period. This result is not sensitive to the choice of discount rate. Because the present value of costs among former smokers is not different for former, relative to continuing, smokers, successful smoking cessation did not create more expensive consumers within our sample.
Discussion
We reported estimates of health services costs among former smokers, never smokers, and continuing smokers at Group Health Cooperative, an integrated health care delivery system in western Washington state. We examined the impact of cessation on health services cost for seven years following successful cessation among former smokers and found that health care costs in the first year postindex are higher relative to continuing smokers. However, this initial increase dissipates in subsequent years. We also found that after adjusting for age, sex, and health status, smokers have greater health costs than never smokers, which demonstrates the excess costs that smoking imposes on the health care delivery system.
We calculated the net present value of total health care costs among former smokers relative to continuing smokers and found that, despite significant short-run increases, costs among former smokers are equal to those of continuing smokers by the second year postindex. This result has implications for whether smoking cessation programs are likely to be cost-effective health promotion activities. Health care costs among former smokers do eventually fall below those of continuing smokers. Depending on the cost of the smoking cessation services offered and the relative success rate of these programs, health plans may be in a position to recover their investment in smoking cessation relatively quickly.
We observed a cost spike among former smokers in the year immediately following cessation that dissipated in the second year post-index, but we also observed a couple of rebounds in costs over time. The cost trends we estimated for former smokers suggested that smoking cessation may coincide with or even precede an expensive health event that may motivate a successful quit. The elevated expenses we found in the first year postquit point to intensive health service use consistent with above average medical care needs. Lower than average costs for former smokers, although still higher than never smokers, in the second year postquit suggest a recovery period. The rise to higher steady state levels in subsequent years is consistent with the greater health care expense we might expect from persons who may have neglected health and preventive services for extended periods of time.
The overall trend in costs over the time series is negative for former smokers and positive for continuing smokers, but this pattern may not be obvious based on data reported in Figure 2. Health care costs for these groups fluctuate over time and although the differences are not statistically significant, there are several years in which former smokers have greater health care costs than continuing smokers. Figure 3, which reports the net difference in cost over time between former and continuing smokers, may demonstrate this phenomenon more directly. Figure 3 demonstrates that following the immediate postquit cost spike, costs among former smokes are consistently less than continuing smokers over the seven-year time series we studied.
We should not expect smoking cessation to immediately reverse the need for health care that results from several years, or even decades, of a behavior that is the single largest contributor to preventable morbidity and mortality in the United States. However, we find that smoking cessation does not increase even short-term health care costs when considering consequences two years postquit. Future research may demonstrate that the long-term health benefits from cessation translate into significantly lower health care costs. An informative comparison would be between the health care costs of former smokers and their predicted costs had they not quit. For example, the higher Chronic Disease Scores observed in former smokers would predict that their health care costs would escalate health care costs over time, which was not observed in this study. Former smokers may be less expensive than they would have been had they continued to smoke.
Our study has several limitations. We relied on data from a single managed care organization. Ideally, smoking-related cost analyses should be conducted on a nationally representative sample of individuals receiving care from a diverse set of health delivery systems.
The costs of smoking, and the implications of cessation, may be related to gender and age. Our study did not have adequate power to address economic consequences stratified by these factors. We also did not have the ability to assess costs based on how people quit—whether they used a smoking cessation service or some other formal program.
Our research design excluded subjects who died before the follow-up survey was conducted because we had no opportunity to verify their smoking status. However, because of the potential impact that smoking related mortality has on health care costs, we conducted a secondary analysis that included subjects who met all of the other inclusion criteria and were enrolled in GHC through December 1994, but died after January 1995. Smoking status information was taken from a 12-month follow-up survey conducted as part of the original randomized trial. We estimated the same model as above but included a flag for the two never smokers, 11 former smokers, and 14 continuing smokers who died after January 1995.
Death is a statistically significant (p<.001) predictor of health care costs. The dollar value of costs did change slightly when we included these subjects, but the statistical results changed only for the fourth period postquit. In this period we found that former smokers had significantly lower health care costs than continuing smokers. The small number of subjects hinders this secondary analysis, but it suggests that the impact of smoking-related mortality, even in a shorter-term analysis, may affect estimates of health care cost. The retrospective nature of our study precluded our ability to model the impact of death on short-term smoking-related health care costs, but future research will certainly examine this issue in greater detail.
In the future, automated health care information systems will include more data on enrollee health behaviors. These efforts are motivated by the desire to provide more feedback to providers, consumers, and sponsors of health care on the success of a wide range of preventive services and are driven in part by purchasers demanding better feedback on health plan performance. The new generation of health plan information systems will make it possible to link information on health behaviors with health services use data, and perhaps across health plans. Future research may take advantage of this more comprehensive data to conduct studies with longer postsmoking follow-up and more diverse populations.
Table 3.
Tests of Difference in Cost by Smoking Status and Postindex Date Period
| P-Values for Tests of Difference Based on Generalized Linear Model | ||||||
|---|---|---|---|---|---|---|
| Cost Difference*/P-Value | ||||||
| Former—Continuing Smokers | Former—Never Smokers | Continuing—Never Smokers | ||||
| Period | Cost Difference | P-Value | Cost Difference | P-Value | Cost Difference | P-Value |
| 1st year postindex | 1001 | 0.07 | 1621 | 0.06 | 620 | 0.40 |
| 2nd year postindex | −219 | 0.47 | 612 | 0.25 | 831 | 0.18 |
| 3rd year postindex | 607 | 0.22 | 1085 | 0.14 | 479 | 0.55 |
| 4th year postindex | −328 | 0.61 | 833 | 0.23 | 1161 | 0.27 |
| 5th year postindex | −673 | 0.22 | 646 | 0.29 | 1318 | 0.18 |
| 6th year postindex | 596 | 0.21 | 1411 | 0.07 | 815 | 0.37 |
| 7th year postindex | −1125 | 0.07 | 1077 | 0.09 | 2202 | 0.06 |
Cost values reported in 2000 U.S. dollars.
Acknowledgments
The authors acknowledge statistical advice provided by Carolyn Rutter, Ph.D., and Laura Ichikawa, M.S., as well as advice offered by anonymous reviewers of earlier versions of this research.
Footnotes
Research was funded by Glaxo Wellcome Inc.
References
- Barendregt JJ, Bonneux L, van der Maas PJ. “The Health Care Costs of Smoking.”. New England Journal of Medicine. 1997;337(15):1052–7. doi: 10.1056/NEJM199710093371506. [DOI] [PubMed] [Google Scholar]
- Bartecchi CE, MacKenzie TD, Schyle RV. “The Human Costs of Tobacco Use.”. New England Journal of Medicine. 1994;330(13):907–12. doi: 10.1056/NEJM199403313301307. [DOI] [PubMed] [Google Scholar]
- Bartlett JC, Miller LS, Rice DP, Max WB. “Medical Care Expenditures Attributable to Cigarette Smoking—United States 1993.”. Morbidity and Mortality Weekly Report. 1994;43:469–72. [PubMed] [Google Scholar]
- Blough DK, Madden CW, Hornbrook MC. “Modeling Risk Using Generalized Linear Models.”. Journal of Health Economics. 1999;18(2):153–71. doi: 10.1016/s0167-6296(98)00032-0. [DOI] [PubMed] [Google Scholar]
- Brauer LH, Hatsukami D, Hanson K, Shiffman S. “Smoking Topography in Tobacco Chippers and Dependent Smokers.”. Addictive Behavior. 1996;21(2):233–8. doi: 10.1016/0306-4603(95)00054-2. [DOI] [PubMed] [Google Scholar]
- Clark D, Von Korff M, Saunders K, Baluch W, Simon G. “A Chronic Disease Score with Empirically Derived Weights.”. Medical Care. 1995;33(8):783–95. doi: 10.1097/00005650-199508000-00004. [DOI] [PubMed] [Google Scholar]
- Curry SJ, Grothaus L, Wagner EH. “A Randomized Trial of Self-Help Materials, Personalized Feedback and Telephone Counseling with Nonvolunteer Smokers.”. Journal of Consulting and Clinical Psychology. 1995;63(6):1005–14. doi: 10.1037//0022-006x.63.6.1005. [DOI] [PubMed] [Google Scholar]
- Fishman P, Von Korff M, Lozano P, Hecht J. “Chronic Care Costs in Managed Care.”. Health Affairs. 1997;16(3):239–47. doi: 10.1377/hlthaff.16.3.239. [DOI] [PubMed] [Google Scholar]
- Gritz ER, Carr CR, Rapkin D, Abemayor E, Chang LJ, Wong WK, Belin TR, Calcaterra T, Robbins KT, Chonkich G. “Predictors of Long-term Smoking Cessation in Head and Neck Cancer Patients.”. Cancer Epidemiology Biomarkers and Prevention. 1993;2(3):261–70. [PubMed] [Google Scholar]
- Halpern MT, Shikiar R, Rentz AM, Khan ZM. “Impact of Smoking Status on Workplace Absenteeism and Productivity.”. Tobacco Control. 2001;10(3):233–8. doi: 10.1136/tc.10.3.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halpern MT, Khan ZM, Young TL, Battista C. “Economic Model of Sustained-Release Bupropion Hydrochloride in Health Plan and Work Site Smoking-Cessation Programs.”. American Journal of Health System Pharmacy. 2000;57(15):1421–9. doi: 10.1093/ajhp/57.15.1421. [DOI] [PubMed] [Google Scholar]
- Hodgson TA. “Cigarette Smoking and Lifetime Medical Expenditures.”. Milbank Quarterly. 1992;70(1):81–125. [PubMed] [Google Scholar]
- Huber PJ. Robust Statistics. New York: Wiley; 1981. [Google Scholar]
- Leu RE, Schaub T. “Does Smoking Increase Medical Expenditures?”. Social Science and Medicine. 1983;17(23):1907–14. doi: 10.1016/0277-9536(83)90168-5. [DOI] [PubMed] [Google Scholar]
- McCullagh P, Nelder JA. Monographs on Statistics and Applied Probability. Cambridge, UK: Cambridge University Press; 1989. vol. 37, Generalized Linear Models. [Google Scholar]
- Miller LS, Zhang X, Rice DP, Max W. “State Estimates of Total Medical Expenditures Attributable to Cigarette Smoking, 1993.”. Public Health Reports. 1998;113(5):447–58. [PMC free article] [PubMed] [Google Scholar]
- Miller VP, Ernst C, Collin F. “Smoking-Attributable Medical Care Costs in the USA.”. Social Science and Medicine. 1999;48(3):375–91. doi: 10.1016/s0277-9536(98)00344-x. [DOI] [PubMed] [Google Scholar]
- Ockene J, Kristeller JL, Goldberg R, Ockene I, Merriam P, Barrett S, Pekow P, Hosmer D, Gianelly R. “Smoking Cessation and Severity of Disease: The Coronary Artery Smoking Intervention Study.”. Health Psychology. 1992;11(2):119–26. doi: 10.1037//0278-6133.11.2.119. [DOI] [PubMed] [Google Scholar]
- Pronk NP, Goodman MJ, O'Connor PJ, Martinson BC. “Relationship between Modifiable Health Risks and Short-Term Health Care Charges.”. Journal of the American Medical Association. 1999;282(23):2235–9. doi: 10.1001/jama.282.23.2235. [DOI] [PubMed] [Google Scholar]
- Rosal MC, Ockene JK, Ma Y, Hebert JR, Ockene IS, Merriam P, Hurley TG. “Coronary Artery Smoking Intervention Study (CASIS): 5-Year Follow-up.”. Health Psychology. 1998;17(5):476–8. doi: 10.1037//0278-6133.17.5.476. [DOI] [PubMed] [Google Scholar]
- SAS Institute . SAS Procedures Guide, Version 6. 3d ed. Cary, NC: SAS Institute; 1990. [Google Scholar]
- Sayette MA, Martin CS, Wertz JM, Shiffman S, Perrott MA. “A Multi-dimensional Analysis of Cue-Elicited Craving in Heavy Smokers and Tobacco Chippers.”. Addiction. 2001;96(10):1419–32. doi: 10.1080/09652140120075152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U. S. Department of Health and Human Services . The Health Benefits of Smoking Cessation: A Report of the Surgeon General. Rockville, MD: Department of Health and Human Services; 1990. Publication no. (CDC) 90-8416. [PubMed] [Google Scholar]
- U. S. Department of Labor, Bureau of Labor Statistics Available at http://www.bls.gov/
- Vogt TM, Schweitzer SO. “Medical Costs of Cigarette Smoking in a Health Maintenance Organization.”. American Journal of Epidemiology. 1985;122(6):1060–6. doi: 10.1093/oxfordjournals.aje.a114187. [DOI] [PubMed] [Google Scholar]
- Wagner EH, Curry SJ, Grothaus L, Saunders KW, McBride CM. “The Impact of Smoking and Quitting on Health Care Use.”. Archives of Internal Medicine. 1995;155(16):1789–95. [PubMed] [Google Scholar]
- Warner KE. “The Economics of Tobacco: Myths and Realities.”. Tobacco Control. 2000;9(1):78–89. doi: 10.1136/tc.9.1.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warner KE, Hodgson TA, Carroll CE. “Medical Costs of Smoking in the United States: Estimates, Their Validity, and Their Implications.”. Tobacco Control. 1999;8(3):290–300. doi: 10.1136/tc.8.3.290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright VB. “Will Quitting Smoking Help Medicare Solve Its Financial Problems?”. Inquiry. 1986;23(1):76–82. [PubMed] [Google Scholar]
- Zhang X, Miller LS, Max W, Rice DP. “Cost of Smoking to the Medicare Program in 1993.”. Health Care Financing Review. 1999;20(4):179–96. [PMC free article] [PubMed] [Google Scholar]