Abstract
Objective
To determine the economic impact on the hospital of a hospitalist program and to develop insights into the relative economic importance of variables such as reductions in mean length of stay and cost, improvements in throughput (patients discharged per unit time), payer methods of reimbursement, and the cost of the hospitalist program.
Data Sources
The primary data source was Tufts-New England Medical Center in Boston. Patient demographics, utilization, cost, and revenue data were obtained from the hospital's cost accounting system and medical records.
Study Design
The hospitalist admitted and managed all patients during a six-week period on the general medical unit of Tufts-New England Medical Center. Reimbursement, cost, length of stay, and throughput outcomes during this period were contrasted with patients admitted to the unit in the same period in the prior year, in the preceding period, and in the following period.
Principal Findings
The hospitalist group compared with the control group demonstrated: length of stay reduced to 2.19 days from 3.45 days (p<.001); total hospital costs per admission reduced to $1,775 from $2,332 (p<.001); costs per day increased to $811 from $679 (p<.001); no differences for readmission within 30 days of discharge to extended care facilities. The hospital's expected incremental profitability with the hospitalist was−$1.44 per admission excluding incremental throughput effects, and it was most sensitive to changes in the ratio of per diem to case rate reimbursement. Incremental throughput with the hospitalist was estimated at 266 patients annually with an associated incremental profitability of $1.3 million.
Conclusion
Hospital interventions designed to reduce length of stay, such as the hospitalist, should be evaluated in terms of cost, throughput, and reimbursement effects. Excluding throughput effects, the hospitalist program was not economically viable due to the influence of per diem reimbursement. Throughput improvements occasioned by the hospitalist program with high baseline occupancy levels are substantial and tend to favor a hospitalist program.
Keywords: Hospitalist, economic analysis, hospital utilization
The Balanced Budget Act together with increasing managed care penetration contributed to lower hospital profitability in the late 1990s. Thirty-four percent of hospitals experienced operating losses in 1997, and bond ratings of not-for-profit hospitals decreased during this period (Heffler et al. 2001; Cunningham 2001). Simultaneously, national hospital capacity was downsized by 72,000 beds from 1989 through 1999 (American Hospital Association 2001). As a result of this consolidation, remaining hospital emergency departments have recently become a major delivery system stress point in cities such as Boston, as reflected in increasing diversion rates (Velianoff 2002). In consequence of these events, many hospitals are focusing on the dual goals of reducing costs and increasing patient throughput (discharges per unit time). The former presumes that there is still some inefficiency left in hospital operations (Rosko and Chilingerian 1999); and the latter represents a recent emphasis on reducing patient queues in the emergency room, capturing patient referrals for inpatient services, and increasing overall hospital productivity and profitability.
The hospitalist delivery model was developed to reduce average length of stay and improve patient throughput. It is a recent natural outgrowth of an environment where there is increasing pressure for hospital utilization to be tightly managed for both quality and cost reasons (Wachter and Goldman 1996; Wachter 1999; Freese 1999). Hospitalists are physicians who focus all of their clinical efforts on the management of hospital inpatients. The hospitalist model seeks to generate higher quality, more cost-effective patient care while maintaining the satisfaction of the hospital, the primary care physician, consulting physicians, the patients, and the patients' families. The hospitalist relieves primary care physicians of inpatient responsibilities that in turn permit them to spend more time pursuing outpatient services. The hospitalist model has been shown to be effective in decreasing both community and academic hospital lengths of stay and hospital costs; while the hospitalist does not reduce quality as measured by increases in patient mortality, increases in discharges to subacute care facilities, increases in readmission rates, or decreases in patient or physician satisfaction due to lack of continuity between the hospitalist and primary care physicians (Freese 1999; Wachter et al. 1998; Diamond, Goldberg, and Janosky 1998).
One might conclude that the hospitalist inevitably leads to increases in hospital productivity and profitability. However, previous studies have not analyzed the impact of the hospitalist delivery model on hospital economics, taking into consideration the joint effects of the hospitalist on utilization, cost, patient throughput, and the different ways in which hospitals are reimbursed by health care payors.
This study examines the implications of the hospitalist from the hospital's economic point of view. The economic impact was estimated in terms of length of stay reduction, changes in cost per day, additional patient throughput, reimbursement effects, cost of the hospitalist program, and incremental profitability. Although the study was carried out at the general medical unit of Tufts-New England Medical Center, the approaches described here are general. The economic model used to evaluate the hospitalist applies to any hospital investment in an intervention that reduces length of stay. Sensitivity analysis is used to demonstrate relationships between key variables driving overall hospital profitability.
METHODS
Study Design and Patient Population
The study took place on the General Medical Service (GMS) at the Tufts-New England Medical Center in Boston, Massachusetts. The New England Medical Center is the principal teaching hospital for the Tufts University School of Medicine. The hospital is predominantly a tertiary teaching institution that also serves as a primary care site for some inner-city neighborhoods. The GMS occupied 10 routine care beds during the study period, accommodating patients whose primary care physician is a member of one of the adult primary care groups based at, or affiliated with, the hospital. The GMS includes residents and a varying number of medical students. Both primary care physicians from the Division of General Internal Medicine and specialists attend on GMS patients.
The performance of a hospitalist physician was compared with attendings on the GMS in a one-time experiment to assess the effectiveness of a hospitalist. The hospitalist study period was six consecutive weeks in August and September 1998. For comparisons, three control groups were used: the six weeks immediately prior to the study period, the six weeks immediately after the study period, and the same six week period during 1997.
Utilization, Cost, and Revenue Data
Patient demographic, utilization, and discharge disposition data were obtained from the medical record. Discharge disposition recorded the destination of all patients discharged to a skilled nursing facility, a rehabilitation hospital, or community based chronic care facility, the home with services, or the home without services. Patient severity was approximated using the Medicare case-mix index (Medical Payment Advisory Commission 1998). Length of stay, Medicare case-mix index, net revenue, and direct cost per case were obtained from the hospital's cost accounting system.
Direct cost includes all costs associated with the delivery of care to patients (e.g., nursing, drugs, ancillary tests, supplies), and it is used in this analysis as a proxy for incremental hospital cost (Friedman and Pauly 1981). The incremental cost of the hospitalist program was derived from the hospitalist's productivity and salary level adjusted for benefits. For example, if the hospitalist's salary and benefits are $180,000 and the hospitalist can cover 15 patients per day, then the hospitalist cost per patient day is $46=($180,000) /[(15)(5/7)(365)]. The 1998 costs were inflated to 1999 using the Medicare price index for hospitals (Medical Payment Advisory Commission 1999).
Net revenue is defined as charges minus contractual adjustments made to payments by third party payers. Incremental net revenue was expressed in terms of the average payment amount per day for payers reimbursing the hospital on a per diem basis and the average payment amount per case for those payers reimbursing the hospital a prospective payment per case. Indemnity insurers paying charges were treated as per diem rate payers based on their average reimbursement per day. The overall economic effect on the hospital of the hospitalist program was measured by the incremental contribution margin, defined as incremental net revenue less incremental costs.
Patient Flow Model
The effect of the hospitalist on patient throughput was estimated with a queueing model of patient flow (Green and Nguyen 2001). Patient flow through the GMS was modeled using a multiserver queuing model with system capacity capped at 10 patients, the size of the unit. The model's key assumptions are: (1) patients arrive randomly with an average daily arrival rate and exponential distribution of interarrival times; (2) lengths of stay are randomly distributed according to the exponential distribution; (3) lengths of stay do not shorten with increased patient arrivals; and (4) patients seeking admission when the unit is operating at capacity are lost to the system—that is, are admitted to another hospital. The model is estimated from data collected on the mean length of stay with and without the hospitalist and on the average baseline occupancy rate of the GMS. The model yields probabilities for each possible daily census (Giffin 1978).
Since it is impossible to count patients lost when the GMS is operating at capacity, it is impossible to observe the actual arrival rate. By equating the observed average daily census with the expected average daily census calculated from the model, however, it is possible to derive the implicit arrival rate using a numerical search algorithm. Based on the estimated arrival rate and the reduction in average length of stay attributable to the hospitalist, the model generates estimates of the additional number of patients served by the GMS over a one-year period. Applying the incremental contribution margin per patient to the additional number of patients seen on the unit produces an estimate of the incremental contribution margin attributable to the increase in throughput generated by the hospitalist program. Separate analyses of contribution margin were conducted with and without the estimated throughput effect.
Sensitivity Analysis
We performed two-way sensitivity analysis on the joint effects of length-of-stay reduction and payer mix on incremental contribution margin excluding throughput effects. Incremental contribution margin from additional patient throughput was calculated for various reductions in mean length of stay achieved by the hospitalist, and a two-way sensitivity analysis was conducted of the joint effects of mean length-of-stay reduction and the percentage of payment from per diem payers on the incremental contribution margin.
We relaxed assumption 4 above by expanding the size of the medical unit to comprise all two hundred medical beds at the hospital and assuming that the hospitalist effect on average length of stay applies to all medical beds. The queueing model produces estimates of additional throughput conditional on initial occupancy rate and reductions in the mean length of stay.
Statistical Analysis
Demographic, utilization, and cost variables describing the three control groups were analyzed using one-way analysis of variance for continuous variables and chi-square tests for discrete variables. The variance of length of stay and cost per case across the three groups was analyzed using Bartlet's Homogeneity of Variance Test. The control groups were pooled and compared to the experimental group using Student's t-test for continuous variables, chi-square tests for discrete variables, and Mood's Median Test (Netter et al. 1996).
RESULTS
Comparing Intervention and Control Groups
Table 1 presents descriptive statistics for the three control groups. The average age of the controls was 64 years, 50 percent of the patients were female, the mean case-mix index was. 95, average length of stay was 3.5 days, and mean direct hospital cost per case was $2,332. There were no statistically significant differences among the control groups in terms of the impact of the hospitalist on length of stay and direct cost per day for each of the individual control groups, nor was there a difference in terms of the demographic characteristics of the control groups (Table 1). We also compared the Medicare DRG mix across control groups and found no significant differences. Consequently the control groups were pooled for all subsequent analyses.
Table 1.
Comparison of Control Groups
| Statistics | Prestudy Group | Poststudy Group | Prior Year Group | P-value |
|---|---|---|---|---|
| Sample size | 121 | 87 | 101 | |
| Age (Mean) | 62.4 | 64.6 | 64.3 | .603‡ |
| Female | 52% | 48% | 49% | .854† |
| Case-mix index (Mean) | 93% | 95% | 96% | .909‡ |
| (Standard Error) | (0.06) | (0.06) | (0.07) | |
| Length of stay days (Mean) | 3.5 | 3.3 | 3.70 | .708‡ |
| (Standard Error) | (0.27) | (0.32) | (0.33) | |
| Direct cost (Mean)* | $2,510 | $2,279 | $2,163 | .491‡ |
| (Standard Error) | (254) | (267) | (218) |
Hospital costs in 1998 inflated by 1999 Medicare Prospective Payment System market basket inflation index (Medicare Payment Advisory Commission 1998).
P-value for chi-square test.
P-value for one-way analysis of variance.
Table 2 presents the results of univariate statistical tests comparing the experimental group of patients with the pooled control groups. Although there are no significant differences in patient demographics, case-mix index, or payer mix between the two groups, there are significant differences in length of stay, cost per case, and cost per day. The length of stay for the hospitalist was 1.29 days shorter when observation days were included and 1.5 days shorter when observation days were excluded. Although there was a greater percentage of observation days for the hospitalist than the pooled controls, the difference was not statistically significant. Neither readmission rates nor discharge disposition rates differed significantly between the two groups. Direct hospital costs were $540 per case lower for the hospitalist than for the pooled controls, but the cost per day was $155 higher for the hospitalist.
Table 2.
Comparison of Hospitalist Group to the Pooled Control Group
| Measure | Hospitalist | Pooled Controls | P-value |
|---|---|---|---|
| Sample size | 93 | 309 | |
| Mean age | 64 | 63.6 | .85† |
| Proportion female | 58% | 50% | .15‡ |
| Case-mix index (Mean) | 0.886 | 0.946 | .30† |
| Payer Mix: | |||
| HMO | 23% | 18% | .8§ |
| Medicare | 54% | 59% | |
| Medicaid | 10% | 7% | |
| Other | 13% | 16% | |
| Length of stay (Mean) | 2.19 | 3.48 | <.001† |
| Length of stay (Median) | 1 | 3 | <.001M |
| Percent observation days | 30% | 23% | 0.14 |
| Length of stay with observation days (N) excluded | 2.71 | 4.22 | <.001† |
| Mean direct hospital cost per case | $1,775 | $2,332 | .015† |
| Mean direct hospital cost per day | $811 | $670 | <.001† |
| Readmission rate | 14% | 18% | .29‡ |
| Discharge Disposition: | |||
| Home health | 23% | 19% | .62§ |
| Rehabilitation/chronic hospital | 18% | 14% | |
| Skilled nursing facility | 10% | 7% | |
| Home | 40% | 46% | |
| Other | 10% | 14% | |
Notes:P-value for Student's t-test of means.
P-value for normal approximation to binomial test of proportions.
Mood's chi-square test of medians.
Chi-square test for independence of discharge disposition versus presence of the hospitalist.
The annualized incremental cost of the hospitalist was $180,000, and the hospitalist's productivity was 15 patients per day based on the average staffing ratio employed. The hospitalist cost per patient day was $46, and the cost per case was $101.
Incremental Contribution Margin and Throughput Effects
Table 3 presents an analysis of the incremental contribution margin per patient attributable to the hospitalist. The incremental contribution margin of the hospitalist is estimated to be about−$1.44 per patient and−$1,285 annually excluding throughput effects. Contribution margin declines with the hospitalist due to the fewer days of care reimbursed by per diem payers and the increase in cost due to the hospitalist.
Table 3.
Calculation of Incremental Contribution Margin with and without the Hospitalist
| Group | |||||
|---|---|---|---|---|---|
| Payer Category | Payer Mix | Measure | Hospitalist | Control | Variance |
| Per Diem | 25% | Average payment per day | $1,418 | $1,418 | $0 |
| Average direct cost per day | $811 | $670 | $141 | ||
| Average length of stay | 2.19 | 3.48 | −1.29 | ||
| Cost of hospitalist per patient day | $46 | $46 | |||
| Incremental contribution margin per patient | $1,229 | $2,602 | −$1,373 | ||
| Per Case | 75% | Average payment per case | $8,048 | $8,048 | $0 |
| Average direct cost per case | $1,775 | $2,332 | −$557 | ||
| Cost of hospitalist per case | $101 | $101 | |||
| Incremental contribution margin per patient | $6,172 | $5,716 | $456 | ||
| All Payers | 100% | Contribution margin per patient | $4,936 | $4,938 | −$1.44 |
| Admissions to GMS | 892 | 892 | 0 | ||
| Total contribution margin (unadjusted) | $4,403,220 | $4,404,505 | −$1,285 | ||
| Additional admissions with hospitalist | 266 | ||||
| Total contribution margin (adjusted) | $5,715,016 | $4,404,505 | $1,310,510 | ||
Notes: Unadjusted contribution margin does not include additional admissions generated by throughput improvement, while adjusted contribution margin includes the incremental margin from throughput improvement with the hospitalist. The cost of the hospitalist is averaged over the number of patients managed in a week with allowance for weekend coverage requirements, and it is expressed as a cost per patient day. Data on mean payment levels under per diem and per case reimbursement methods are estimated from modeled net revenue by payer produced by New England Medical Center's cost accounting system for the study patient population and cost data are estimated from the same source.
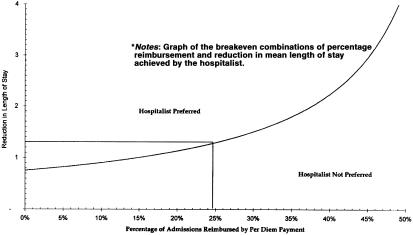
Figure 1 presents a two-way analysis of the sensitivity of contribution margin (excluding throughput effects) to changes in the reduction in average length of stay and the proportion of patients on the GMS reimbursed on a per diem basis. It graphs the break-even combinations of per diem payment mix and length-of-stay reduction achieved by the hospitalist. For example, if the hospitalist achieves a one-day average length-of-stay (ALOS) reduction, the break even per diem mix is about 13 percent. If the ALOS reduction achieved by the hospitalist is greater than one and the percentage per diem reimbursement is 13 percent, then the decision to add a hospitalist to the GMS unit is favored. If, on the other hand, the percentage of per diem patients is greater than 13 percent and reduction in ALOS is one, then the economically favored decision is not to use a hospitalist. The actual GMS per diem reimbursement mix is 25 percent, and the breakeven reduction in ALOS is slightly more than 1.3 days—that is, greater than the 1.29 day reduction achieved by the hospitalist. Consequently the hospitalist is not favored. At about 50 percent per diem reimbursement on the GMS unit, it is impossible to break even by adding a hospitalist since it would require that the ALOS be negative.
Figure 1.
Impact of Length-of-Stay Reduction and Percent per Diem Payment on Hospitalist's Economic Acceptability to the Hospital
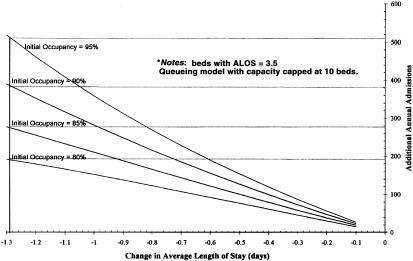
Figure 2 graphs the relationship between incremental patient throughput and length-of-stay reductions for various baseline occupancy rates on the GMS. The increased throughput generated by the hospitalist's 1.29 day reduction in mean length of stay is estimated to be 266 patients per year given a baseline occupancy rate of 85 percent on the GMS. This increase in throughput results in additional contribution margin of about $1,300,000. If the baseline mean occupancy rate for the GMS were to increase to 90 percent, then an estimated 380 additional patients per year could be accommodated on the GMS.
Figure 2.
Increased Throughput from Hospitalist Program Ten-Bed General Medical Unit
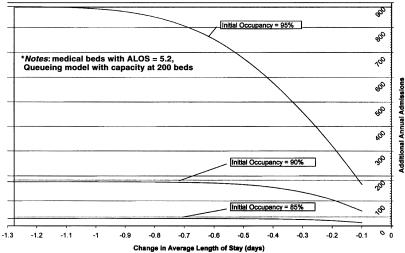
Figure 3 graphs the relationship between incremental annual patient throughput and ALOS reductions for two hundred medical beds at the hospital. Given a baseline occupancy of 85 percent, incremental throughput with the hospitalist is only 32 annual admissions for a reduction in ALOS of 1.29. Incremental throughput due to the hospitalist with two hundred beds increases exponentially with baseline occupancy rates, growing to 177 incremental admissions at 90 percent occupancy.
Figure 3.
Increased Throughput from Hospitalist Program Two Hundred Beds
DISCUSSION
This analysis underscores the importance of modeling the joint effects of a hospital intervention designed to reduce length of stay in terms of cost, reimbursement, mean length of stay, and patient throughput. The hospitalist program demonstrated comparable reductions in mean length of stay and cost as those reported in the literature (Wachter and Goldman 1996; Wachter 1999; Freese 1999). Mean length of stay declined by 37 percent and direct hospital cost per day increased by 24 percent during the hospitalist's presence on service. The disparity between the reduction of total hospital cost per admission and the increase in the unit cost per day supports the concept that the hospitalist delivery model results in more diagnostic and therapeutic modalities being utilized in a shorter period of time. Thus a large part of the savings that accrue to an institution comes from the reduction in costs tied to a hospital day. This observation has been reported by others who have noted that the hospitalist delivery model reduced length of stay but did not decrease laboratory, radiology, consult, or pharmacy costs (Freese 1999). Despite the dramatic impact of the hospitalist on length of stay and cost per case, however, use of the hospitalist was not supported by the economic analysis excluding consideration of potential throughput effects.
Per diem reimbursement methods diminish the economic attractiveness of the hospitalist to the hospital, whereas prospective case-based reimbursement favors the use of a hospitalist. The opportunity cost of employing a hospitalist includes the loss in reimbursement based on per diem. Prospective case-based reimbursement was initially introduced by Medicare in 1982, and it is now widely imitated by managed care organizations (Chen, Kane, and Finch 2001). Moreover, many hospitals today are experiencing high occupancy rates and simultaneously losing money on operations. These conditions should lead to increasing adoption of the hospitalist delivery model.
The hospitalist program improves the ability of a hospital to accommodate more admissions, assuming the demand for additional admissions exists. Increased admissions result in increases in the incremental contribution margin associated with a hospitalist delivery model. The number of additional patients depends on the baseline bed occupancy, the bed capacity, the rate of demand for the unit as reflected in the average arrival rate, the mean length of stay with the hospitalist, and on the timing of patient arrivals relative to the availability of freed beds. It would be misleading to assume that every bed-day freed up as a result of hospitalist-induced reductions in length of stay could be filled with new patients—for example, that the incremental mean daily census generated by the hospitalist would be completely filled with new patients. This approach does not account for the mean rate of demand for beds, the random nature of patient arrivals, the randomness in length of stay, and the problem of matching available beds with patient arrivals. The queuing model used in this analysis does account for these factors (Green and Nguyen 2001).
Limitations in this analysis include daily changes in the patient arrival rate in response to higher occupancy levels and the possibility that patients denied access to the GMS could be accommodated elsewhere in the hospital. Since a certain amount of “leakage” of patients to other hospital units undoubtedly occurs when the GMS is at capacity, our results could be considered an upper bound on the throughput effects. The impact of potential leakage of patients to other hospital wards due to lack of a GMS bed could be significant. The extreme case would be to view all medical beds as substitutes for GMS. In Figure 3, we estimated the impact of the hospitalist program when applied to two hundred adult medical beds at the hospital. At a baseline mean annual occupancy rate of 85 percent, the throughput effect of the hospitalist is only 32 additional admissions; and the differential throughput effect for the ten-bed GMS vis-à-vis two hundred beds is 234 admissions. Thus as capacity increases, the throughput effect of the hospitalist declines holding the occupancy rate constant. Alternatively, the probability that the demand for beds exceeds capacity declines as the number of beds is increased and occupancy rate is held consistent (Green and Nguyen 2001). At higher occupancy rates (e.g., 90 percent to 95 percent), the hospitalist throughput effects on the ten-bed GMS compared to two hundred medical beds converge, and the leakage of patients from GMS to other medical beds accordingly declines. Although more complex conditions could be modeled using a simulation approach, producing different quantitative estimates of the differential throughput effects, the qualitative effects would remain the same.
The case mix of the patients on the GMS is low compared to the total case mix for the hospital as reflected in the higher mean length of stay for all medical patients. Whether a hospitalist program could produce comparable reductions in length of stay for more severely ill patients is not clear.
The decision to implement a hospitalist model is fraught with political implications that may trump the economic effects. For example, the intervention may not be acceptable to medical staff members who derive income from rounding on inpatients. Similarly the entity that employs the hospitalist may influence the use. For example, a hospitalist program may be attractive to a group of physicians who are assuming high levels of global capitation risk.
Finally, the hospitalist program may be more effective in regions where lengths of stay tend to be higher, and it is only one of several approaches to reducing mean length of stay and increasing patient throughput. For example, more aggressive discharge management by attending physicians, unit nurses, and case managers may achieve comparable results at significantly less cost. Thus, hospitalist programs, if widely undertaken, could actually increase both the cost per patient day and total hospital costs.
CONCLUSION
This study supports several conclusions. The use of a hospitalist delivery model on the general medical unit of a tertiary, academic teaching hospital results in length of stay and hospital costs being reduced without increasing the readmission rate or cost shifting to subacute provider facilities. Most of the cost savings result from decreases in the length of stay. The economic contribution of the hospitalist is determined by the reduction in cost, the impact on hospital reimbursement, and improvements in patient throughput. Per diem reimbursement methods diminish the economic attractiveness of the hospitalist, whereas prospective case-based reimbursement favor the use of a hospitalist. Depending on the capacity of the inpatient unit(s) targeted for a hospitalist program, the baseline occupancy rate, and the availability of substitute beds elsewhere in the hospital, the hospitalist program may generate substantial increases in patient throughput with accordant increases in hospital margins. Hospitals may be reluctant to implement any length-of-stay reducing intervention when the levels of per diem or charge-based reimbursement are high, even when the cost reductions are substantial. The approaches described here are general and apply to any hospital intervention designed to reduce mean length of stay.
Acknowledgments
The authors benefited from numerous helpful comments made by the reviewers of this article.
REFERENCES
- American Hospital Association . Hospital Statistics. Chicago: American Hospital Association; 2001. [Google Scholar]
- Chen Q, Kane RL, Finch MD. “The Cost Effectiveness of Post-Acute Care for Elderly Medicare Beneficiaries.”. Inquiry. 2001;37:359–75. [PubMed] [Google Scholar]
- Cunningham R. “Hospital Finance: Signs of ‘Pushback’ Amid Resurgent Cost Pressures.”. Health Affairs. 2001;20(2):234–340. doi: 10.1377/hlthaff.20.2.233. [DOI] [PubMed] [Google Scholar]
- Diamond HS, Goldberg E, Janosky JE. “The Effect of Full-Time Hospitalists on the Efficiency of Care at a Community Teaching Hospital.”. Annals of Internal Medicine. 1998;129:197–203. doi: 10.7326/0003-4819-129-3-199808010-00006. [DOI] [PubMed] [Google Scholar]
- Freese RB. “The Park Nicollet Experience in Establishing a Hospitalist System.”. Annals of Internal Medicine. 1999;130:350–4. doi: 10.7326/0003-4819-130-4-199902161-00004. [DOI] [PubMed] [Google Scholar]
- Friedman B, Pauly MV. “Cost Functions for a Service Firm with Variable Quality and Stochastic Demand.”. Review of Economic Statistics. 1981;63(4):620–74. [Google Scholar]
- Giffin WC. Queueing: Basic Theory and Applications. Columbus, OH: Grid Inc; 1978. [Google Scholar]
- Green LV, Nguyen V. “Strategies for Cutting Hospital Beds: The Impact on Patient Service.”. Health Services Research. 2001;36(2):421–42. [PMC free article] [PubMed] [Google Scholar]
- Heffler S, Levit K, Smith S, Smith C, Cowan C, Lazenby H, Freeland M. “Health Spending Growth Up in 1999: Faster Growth Expected in the Future.”. Health Affairs. 2001;20(2):193–203. doi: 10.1377/hlthaff.20.2.193. [DOI] [PubMed] [Google Scholar]
- Medicare Payment Advisory Commission . Report to the Congress: Selected Medicare Issues. Washington, DC: Medicare Payment Advisory Commission; 1998. [Google Scholar]
- Netter J, Kutner MH, Nachtsheim CJ, Wasserman W. Applied Linear Statistical Models. Chicago: Irwin; 1996. [Google Scholar]
- Rosko MD, Chilingerian JA. “Estimating Hospital Inefficiency: Does Case Mix Matter?”. Journal of Medical Systems. 1999;23(1):57–71. doi: 10.1023/a:1020823612156. [DOI] [PubMed] [Google Scholar]
- Velianoff GD. “Overcrowding and Diversion in the Emergency Department: The Health Care Safety Net Unravels.”. Nursing Clinics of North America. 2002;37(1):59–66. doi: 10.1016/s0029-6465(03)00082-3. [DOI] [PubMed] [Google Scholar]
- Wachter RM. “An Introduction to the Hospitalist Model.”. Annals of Internal Medicine. 1999;130:338–42. doi: 10.7326/0003-4819-130-4-199902161-00002. [DOI] [PubMed] [Google Scholar]
- Wachter RM, Goldman L. “The Emerging Role of Hospitalists in the American Heath Care System.”. New England Journal of Medicine. 1996;335:514–7. doi: 10.1056/NEJM199608153350713. [DOI] [PubMed] [Google Scholar]
- Wachter RM, Katz P, Showstack J, Bindman AB, Goldman L. “Reorganizing an Academic Medical Service.”. Journal of the American Medical Association. 1998;279:1560–5. doi: 10.1001/jama.279.19.1560. [DOI] [PubMed] [Google Scholar]