Abstract
Objective
To quantify the total contribution to generalist care made by nurse practitioners (NPs) and physician assistants (PAs) in Washington State.
Data Sources
State professional licensure renewal survey data from 1998–1999.
Study Design
Cross-sectional. Data on medical specialty, place of practice, and outpatient visits performed were used to estimate productivity of generalist physicians, NPs, and PAs. Provider head counts were adjusted for missing specialty and productivity data and converted into family physician full-time equivalents (FTEs) to facilitate estimation of total contribution to generalist care made by each provider type.
Principal Findings
Nurse practitioners and physician assistants make up 23.4 percent of the generalist provider population and provide 21.0 percent of the generalist outpatient visits in Washington State. The NP/PA contribution to generalist care is higher in rural areas (24.7 percent of total visits compared to 20.1 percent in urban areas). The PAs and NPs provide 50.3 percent of generalist visits provided by women in rural areas, 36.5 percent in urban areas. When productivity data were converted into family physician FTEs, the productivity adjustments were large. A total of 4,189 generalist physicians produced only 2,760 family physician FTEs (1 FTE=105 outpatient visits per week). The NP and PA productivity adjustments were also quite large.
Conclusions
Accurate estimates of available generalist care must take into account the contributions of NPs and PAs. Additionally, simple head counts of licensed providers are likely to result in substantial overestimates of available care. Actual productivity data or empirically derived adjustment factors must be used for accurate estimation of provider shortages.
Keywords: Nurse practitioners, physician assistants, generalist care, provider shortage
Over the past thirty years, nurse practitioners (NPs) and physician assistants (PAs) have become an established presence in the primary health care workforce. Despite the growth of these professions, most estimates of provider shortage have focused on physicians. In this study, we describe the contribution to generalist care made by NPs and PAs in Washington State, with special attention paid to the role of nonphysician clinicians (NPCs) in underserved rural areas.
Specifically, this study of Washington State addresses the following questions:
What is the total contribution to generalist care made by NPCs?
What is the role of NPCs in providing generalist care in rural Health Professional Shortage Areas (HPSAs)?
What proportion of the total generalist care provided by women is provided by women NPCs?
An important issue in health workforce analysis is how to count the contribution to patient care of each provider and each provider type. Simple head counts of providers are unlikely to produce realistic estimates of the actual supply of health care available to a population (Larson, Ballweg, and Hart 2001; Ricketts, Hart, and Pirani 2000). Differences in training, location, specialty, in-patient care activities, experience, scope of practice, and full-time/part-time status create large differences in the number of visits that a given clinician is likely to perform during a week. Data from the American Medical Association (Randolph, Seidman, and Pasko 1997), for example, indicate that an average family physician provides 105 ambulatory patient visits each week, a general pediatrician 95, and a general internist about 65. If estimates of available care are to include NPCs, basing estimates of available care on head counts becomes yet more doubtful because so little is known about the productivity of NPCs and their total contribution to care (Scheffler, Waitzman, and Hillman 1996). In this study, we use state licensing data and self-reports of outpatient visit productivity to count contribution to care by providers in family physician full-time equivalents (FTEs). By measuring productivity in this way, we can correct for individual differences in productivity and directly compare productivity across professions.
Because the analysis is based on individual-level productivity data, we are able to base our analysis on FTEs rather than head counts of providers. While many states and other jurisdictions do not have the data necessary to carry out such an analysis, this work presents some empirically derived “productivity adjustment factors” for different provider types in different settings. If we can determine, for example, that full-time PAs perform 70 percent of the number of visits performed by full-time family physicians, we can, in the absence of actual visit data, use the .7 productivity adjustment to estimate the contribution to care made by a PA in meeting the visit requirements of a population. Productivity adjustments can be used to estimate available care based on provider type, specialty, and location when productivity data are not available.
Methods
Data Source
Washington State health professional licensure information was the main data source used in this study. In addition to basic demographic information collected on the required license renewal form, the state administered a survey with the license renewal that was used to collect information on practice type, medical specialty, practice location, and weekly number of outpatient and inpatient visits performed.
Geographic Units of Analysis
The 124 zip-code-based generalist Health Service Areas (HSAs) that were developed by the Washington State Department of Health are the basic geographic unit of analysis used in this study. Fifty-two of the HSAs are considered to be rural and are based on the normative service areas of the state's rural hospitals and clinics. The remaining 72 HSAs are considered urban. The use of these zip-code-based units avoids the problems of overbounding and underbounding so often associated with the use of county-based definitions such as the metro/nonmetro definition or Urban Influence Codes (Ricketts, Johnson-Webb, and Taylor 1998). The NPC contribution-to-care was measured at the HSA level and at the rural/urban level (all rural HSAs compared to all urban HSAs). To assess the contribution to care of various providers in rural HPSAs, we determined the percentage of the population in each rural HSA that resided in a designated geographic HPSA in 1998. In 4 (7.7 percent) of the 52 rural HSAs, 100 percent of the population lived within a designated HPSA. Twenty-five of the rural HSAs had no one living in a designated HPSA. The HPSA population in the remaining 27 rural HSAs ranged from 2 to 91 percent.
Study Population and Survey Response
The study population consisted of physicians (medical doctors [MDs] and doctors of osteopathy [DOs]), nurse practitioners, and physician assistants who renewed their professional licenses between April of 1998 and May of 1999. Annual license renewal is required by Washington State for MD/DOs and PAs, biannual renewal is required for NPs. Counts of active providers and their full-time/part-time status in certain rural areas of Washington State were verified with the assistance of the Western Washington Area Health Education Center and the Eastern Washington Area Health Education Center (AHECs). This helped to improve the accuracy of our estimates in low population areas where the consequences of miscounting providers would result in serious over- or underestimates of the total available care. After eliminating duplicates, retirees, residents, and providers practicing outside of the state, license data identified 12,296 physicians, 2,277 NPs, and 1,033 PAs licensed and actively practicing medicine in Washington State (15,606 total providers). Response rates to the optional survey instrument varied across profession. Ninety percent of physicians, 81.9 percent of PAs and 61.8 percent of NPs completed the survey. Most providers with survey data were actively practicing medicine (94.7 percent of MD/DOs, 98.1 percent of NPs, and 95.4 percent of PAs).
Data on physicians who did not respond to the state licensure survey were obtained by linking American Medical Association (AMA) Masterfile data to the licensing data, reducing the effective rate of missing specialty data for physicians to only 1.7 percent. Though the AMA data provided specialty information, it did not include data on patient visits.
Estimating the Proportion of Generalists among Unknown Providers
Because of this study's goal of estimating the contribution of each provider type to generalist care, it was not possible to simply exclude cases with missing data. Instead, we examined the proportion of rural and urban providers of the three provider types who were generalists and then applied those proportions as weights to estimate the generalist contribution of each unknown provider. The proportion of generalists is estimated separately for rural and urban providers because generalists make up a much larger proportion of providers in rural areas (for example, generalist PAs are 72.3 percent of the PA population in rural areas but only 40.2 percent in urban areas [Larson, Ballweg, and Hart 2001]). Generalists were defined as providers principally involved in general/family practice, general internal medicine, and general pediatrics. The total rural and urban estimated generalist head counts for a single provider type is calculated (equation (1)):
Where: t=count of known active generalists
g=proportion of active generalists among known providers
s=count of unknown providers
r=rural/urban location
Imputation of missing specialty data in this manner is a conservative measure that guards against undercounting the number of providers of any given type in a population.
Determining the Total Supply of Generalist Visits
The use of head counts of providers to assess the supply of visits available to a population is inherently inaccurate. Head counts, even after careful adjustment in the manner described above, fail to take into account differential levels of productivity within professions, and across professions and individuals (Larson, Ballweg, and Hart 2001). A more realistic approach to ascertaining supply and comparing productivity and contribution-to-care is employed here. Rather than estimating available care from head counts, ambulatory visit data were used to determine the total supply of generalist care in a given area. To assess the contribution to care made by each provider type, the number and proportion of outpatient visits being provided by NPs, PAs, and physicians were counted and compared to the total number of visits being provided by all three types of providers in a given HSA or HPSA. These counts were then converted into family physician FTEs, a more intuitive and convenient unit. To convert them, visit counts were divided by the number of visits performed by an average full-time family physician (105 visits per week).
Counts of number of outpatient visits performed each week from providers who completed the survey were used to estimate the number of generalist visits performed by providers who did not provide specialty and/or productivity information (equation (2)):
Where: B=total visits
V=reported visits
t=provider type (FP, GIM, Ped, PA, NP)
M=median visits from known providers
r=rural or urban
a=proportion of providers actively practicing
p=proportion of provider type in primary care
(this will be 1 for known FPs, GIMs, and Peds who did not have productivity data)
The productivity adjustment factors and median outpatient visits (M and p) applied to all unknown providers are reported below. All were derived from the provider population with complete survey data.
Data Imputation
We performed two general types of imputations during the analyses: (1) imputation of license renewal survey missing items, and (2) imputation for licensed providers who did not return a survey with their license renewal. In both cases, we elected to use cell-specific tailored median and proportion substitution methods rather than regression methods after inspection of regression results and close examination of the data. Besides the low predictive power of imputation regression models, we saw that the regressions were prone to making some imputations, especially at the extreme values and for small subgroups, that were clearly incorrect. The following data made our estimates unusually accurate: (a) licensing renewal data for all providers (license type, age, sex, rural/urban status, but not specialty), (b) high response rates to the license renewal survey (physicians over 90 percent, PAs over 80 percent, and NPs over 60 percent), (c) linked AMA data for physicians, and (d) verification of our data on the relevant providers in all rural communities with 20 or fewer providers by the two Washington State AHECs.
To impute missing items for providers who responded to the survey we systematically worked our way through all the large and small groups of providers over a six-month period. The imputation decisions usually involved either imputing missing productivity data (for clearly identified generalists only) or deciding whether or not to count the visits of particular combinations of provider type and primary and secondary specialties (e.g., family medicine, community medicine, and public health) as generalists. The research team met weekly to discuss the various options and review analyses (including regressions), and used our workforce experience and the data to create consistent decision rules. Many of the analyses involved printing out all members of a small subgroup and examining the data by hand per all the relevant reported items and combinations of items. For example, if a physician listed his or her first specialty type as community health (or as a nonclinical position, public health, etc.) and listed FP as a second specialty and provided information on direct patient care and visits, they were included as generalists. Many other combinations were not included (e.g., a physician who had a nonclinical position and family physician combination, but did not report patient visits was not included as contributing generalist visits). In selected cases where visits were missing but direct patient care hours was present, visits were estimated. Both the AMA Masterfile and AHEC data were integrated into this process.
In the case of providers who did not respond to the survey, we generally assumed that nonrespondents were similar to respondents. As indicated above, regression analysis results were suspect, given the limited license variables and its poor performance in tests. Therefore, we created algorithms that attributed the characteristics of the respondents to the nonrespondents using available data: license data, AMA data for physicians, and AHEC data (e.g., if the AHECs reported that a nonrespondent was practicing full-time as a generalist at a site, we reflected this in the database). We then extrapolated the available information to the nonrespondents. After all steps to identify specialty via license data, AMA data, and AHEC information, we had to impute specialty for only 8 percent of the 15,606 active specialist and generalist providers in the state (Hart and Palazzo [in press]). The use of information from the AHECs reduced the possibility of error in estimating care in the low-population HSAs where the consequences of an error would be the most severe.
In some cases, we chose to exclude providers rather than impute specialty or productivity data. For example, providers who did not provide direct patient hours or visits (either as missing questionnaire items or through survey nonresponse) and who were age 70 or older, were excluded from the analyses. It would have introduced more error into the estimates to impute to all licensed 70 or older providers (there being many), when few would have produced meaningful numbers of visits. Instead we chose to be conservative and only include those who also reported their actual visits. In this case, the assumption was that the nonrespondents were much more likely to not be practicing than the respondents. The rule of thumb was one of reducing the largest source of probable error. An exhaustive description of the imputation and exclusion methods used in this study can be found in Hart and Palazzo (in press).
Measuring Contribution to Care
The proportion of outpatient visits reported by each provider type can be used to address the study questions. However, it is useful to re-express outpatient visits as physician FTEs. This facilitates comparison across professions and allows corrections for individual differences in productivity. Comparing FTE counts is far more convenient and intuitive than a count of total visits provided. The FTE unit is also useful when attempting to address questions of shortage mitigation. If converting to FTEs, an important question is what figure to use for the conversion. We chose to convert visits to FTEs using the AMA's nationally representative 1997 estimate of average full-time family physician productivity, 105 outpatient visits per week (Randolph, Seidman, and Pasco 1997). This estimate remained stable during the 1990s, varying from 111.6 visits per week in 1991 to 102.6 in 1998. The 105 figure was also quite close to the productivity found in a survey of Washington physicians conducted in 1997. That study estimated full-time family practitioner productivity at 103 outpatient visits per week (Hart 1998).
It should be emphasized that the conversion to family physician FTEs is done only for convenience and the facilitation of comparisons. The proportion of care provided by NPs, PAs, and physicians can be calculated directly from the components of equation (2). These proportions remain the same regardless of whether they are converted to family physician FTEs, or to any other provider standard FTE; one could, for example, decide to estimate FTEs based on median generalist productivity. In this study, available primary care FTEs in a given area are calculated (equation(3)):
F=total family physician FTEs available
B=total visits (from equations (2))
t=provider type (FP, GIM, Ped, PA, NP)
For example, if a family physician in a given HSA provides 110 visits each week and an NP and a PA provide 60 and 40 visits (respectively), then the provider supply in the HSA is estimated at 210 visits or two family physician FTEs.
Results
Distribution of Providers
In 1998–1999 the state licensed 12,296 active physicians and osteopaths, 2,277 active NPs and 1,033 active PAs—a total of 15,606 providers. When analysis is restricted to active providers known to be generalists (Table 1), the total number of providers drops substantially to 5,051. The majority of the generalist MD/DOs were family physicians or general practitioners (56.3 percent). General internists and general pediatricians made up 28.2 percent and 15.3 percent of the generalist physician population respectively. It should be borne in mind that the provider counts shown in Table 1 are undercounts of the number of generalist providers; the table data are restricted to known generalists. To estimate accurately the contribution to care of NPCs, the provider counts had to be adjusted for the likely number of generalists in the population of providers who did not provide survey information on specialty or productivity.
Table 1.
Active Generalist Providers in Washington State, 1998–1999
| Generalist MD/DOs | Generalist NPs | Generalist PAs | Total | |
|---|---|---|---|---|
| Count | 4,124 | 442 | 485 | 5,051 |
| (81.6%) | (8.8%) | (9.6%) | (100.0%) | |
| Mean age | 46.7 | 47.1 | 45.4 | 46.6 |
| % female | 28.9 | 92.7 | 38.8 | 35.5 |
| % practicing in rural HSAs | 19.4 | 19.7 | 27.8 | 20.2 |
| % practicing in geographic HPSAs | 0.8 | 3.1 | 2.0 | 1.1 |
| Physician Specialty: | ||||
| % family physician/general practitioner (FP/GP) | 56.3 | — | — | 46.0 |
| % general internal medicine (GIM) | 28.2 | — | — | 23.0 |
| % general pediatrics (Ped) | 15.3 | — | — | 12.6 |
Estimating the Total Generalist Population
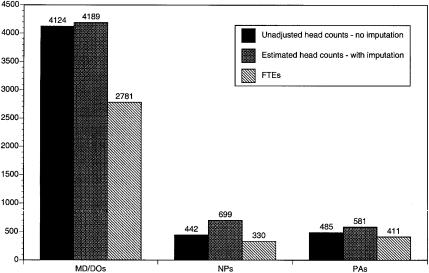
Using the procedure described above (equations (1)), unadjusted head count data were evaluated and a revised, estimated head count for each provider type was calculated. The productivity adjustment factors used for each provider type in each location are found in Table 2. In rural areas, for example, 37.8 percent of the NPs are known to be generalists, in urban areas, 31.1 percent. These proportions were applied as weights to the 38.2 percent of NPs that did not respond to the survey. The same procedure was used to estimate the proportion of generalists among MDs and PAs who did not respond to the survey. Adjusted estimates of the numbers of generalist providers of each type in rural and urban parts of the state are presented in Table 3. The estimate of the total number of physicians increased slightly (from 4,124 to 4,189), reflecting a low rate of missing survey/AMA data. The estimate of the total number of generalist NPs increased substantially from 442 to 699, reflecting a higher rate of missing survey information. The final estimate of the total number of generalist PAs increased from 485 to 581.
Table 2.
Factors Used in Estimating the Productivity of Providers Who Were Missing Productivity Data
| Median Visits (M in Equation (2)) | % in Generalist Specialties (p in Equation (2)) | ||||
|---|---|---|---|---|---|
| Rural | Urban | Rural | Urban | % Active (a in equations (2)) | |
| Family physicians | 80 | 72 | 32.1* | 17.1* | 94.7 |
| General internists | 55 | 60 | 9.7* | 9.7* | 94.7 |
| General pediatricians | 83 | 75 | 5.3* | 5.3* | 94.7 |
| Nurse practitioners | 58 | 45 | 37.8 | 31.1 | 98.1 |
| Physician assistants | 70 | 75 | 71.2 | 54.7 | 95.4 |
For MDs with no known specialty data only. Those MDs with known generalist specialty but no productivity information are assumed to be 100 percent generalists.
Table 3.
Active Identified and Imputed Generalist Providers by Rural/Urban Location in Washington State, 1998–1999
| Generalist MD/DOs Count (%) | Generalist NPs Count (%) | Generalist PAs Count (%) | Total Count (%) | |
|---|---|---|---|---|
| Rural | 811.2 (73.9) | 133.9 (12.2) | 152.7 (13.9) | 1097.8 (100.0) |
| Urban | 3377.8 (77.3) | 565.5 (12.9) | 428.1 (9.8) | 4371.4 (100.0) |
| Total | 4189.0 (76.6) | 699.4 (12.8) | 580.8 (10.6) | 5469.2 (100.0) |
Estimating the Supply of Generalist Ambulatory Visits and FTEs
Following the procedure outlined in equations (2) above, we estimated the total supply of ambulatory visits available from each provider type in rural and urban areas of the state. Total visits were then converted into family physician FTEs using equations (3). In Figure 1, the fairly dramatic effects of converting from unadjusted head counts, to estimated head counts, to physician FTEs can be observed. The licensing/survey data identified 4,124 generalist physicians. We estimated that of the licensed active physicians for whom we did not have productivity or specialty information, an additional 65 physicians were generalists, for an estimated total of 4,189 active generalist physicians. Outpatient visit productivity data indicated that those physicians were providing the visits that could be supplied by 2,781 family physician FTEs. An estimated 699 NPs provided 330 family physician FTEs and 581 PAs provided 411 family physician FTEs. In short, there are an estimated 5,469 generalist providers in Washington (see Table 3) who provide approximately 3,522 family physician FTEs of outpatient visits. Generalist physicians make up 76.6 percent of the generalist providers in Washington State and provide 78.9 percent of the generalist FTEs; NPs provide 9.4 percent and PAs provide the remaining 11.7 percent.
Figure 1.
Generalist Head Counts and FTEs, by Provider Type, Washington State, 1998–1999
There are some differences in the contribution to care made by NPCs in rural versus urban areas of Washington. Overall, NPCs provide 24.7 percent of the total generalist outpatient visits in rural areas (10.3 percent by NPs, 14.4 percent by PAs) compared to 20.1 percent in urban areas (p=.014). In both rural and urban settings, NPs provide about 10 percent of the outpatient visits; the rural/urban difference in NPC contribution is primarily attributable to the larger proportion of total visits provided by rural PAs. The range of NPC contribution to generalist care in rural HSAs is quite wide. In five rural HSAs, NPCs provide less than 10 percent of total generalist visits. In three HSAs, NPCs provide over 75 percent of visits. In the majority of rural HSAs, NPCs provide between 20 and 30 percent of the generalist outpatient visits.
Contribution of NPCs to Care in Rural HPSAs
Rural NPCs contribute more to generalist care than their urban counterparts. To determine whether NPCs were making a relatively larger contribution to care in underserved rural areas, we restricted the analysis to rural providers alone and examined differences in NPC FTEs across the HPSA/non-HPSA dimension. As shown in Table 4, NPCs perform between 25.3 and 32.6 percent of the outpatient visits in HSAs that are at least partially designated as geographic HPSAs. In non-HPSA rural HSAs, they contribute about 22.6 percent of the total visits. Though these findings suggest that NPCs make a larger contribution to care in HPSA-designated HSAs, the observed contribution differences were not statistically significant. The proportions of care contributed separately by NPs and PAs were also compared to physician contribution. The PAs in HSAs where at least 34 percent of the population lives in a designated HPSA made a larger contribution to care than in HSAs with no HPSA population (21.6 percent compared to 12.5 percent, p=.03). No other statistically significant differences across the HPSA/non-HPSA dimension were found (not tabled).
Table 4.
Generalist Provider Supply (in FTEs) in Rural Geographic HPSAs, Washington State, 1989–1999
| Generalist MD/DOs Count (%) | Generalist NPs Count (%) | Generalist PAs Count (%) | Total Count (%) | |
|---|---|---|---|---|
| Rural HSAs with no HPSA population (25 HSAs) | 320.3 (77.4) | 41.6 (10.1) | 51.8 (12.5) | 413.7 (100.0) |
| Rural HSAs 1–33% of population in HPSAs (12 HSAs) | 170.5 (74.6) | 23.8 (10.4) | 34.1 (14.9) | 228.4 (100.0) |
| Rural HSAs 34–100% of population in HPSAs (15 HSAs) | 64.4 (67.4) | 10.5 (11.0) | 20.6 (21.6) | 95.5 (100.0) |
| Total | 555.2 (75.3) | 75.9 (10.3) | 106.5 (14.4) | 737.6 (100.0) |
Female Generalists in Rural HSAs
Stark rural/urban differences in the relative contribution of NPCs compared to physicians were found when we examined the role of NPCs in the ambulatory visits performed by female providers (Table 5). Women generalist physicians provided 49.3 percent of the rural visits performed by women, compared to 63.5 percent among urban female generalist providers (p<.01). Not surprisingly, NPs (a group that is 87 percent female [89 percent in rural areas]) provided 31.9 percent of female provider visits in rural areas and 24.3 percent in urban ones (p<.01 compared to MD/DOs). Female PAs also made a larger contribution to generalist care provided by women in rural areas compared to urban ones, 18.8 percent compared to 12.2 percent (p<.01 compared to MD/DOs). Overall, NPs and PAs provided over half (50.7 percent) of the generalist care provided by women in rural areas.
Table 5.
Percentage of Female Generalist Providers by Provider Type (in FTEs) by Rural/Urban Location, Washington State, 1998–1999
| MD/DOs Count (%) | NPs Count (%) | PAs Count (%) | Total Count (%) | |
|---|---|---|---|---|
| Rural | 98.6 (49.3) | 63.8 (31.9) | 37.8 (18.8) | 200.2 (100.0) |
| Urban | 599.3 (63.5) | 228.8 (24.3) | 115.1 (12.2) | 943.2 (100.0) |
| Total | 697.9 (61.0) | 292.6 (25.6) | 152.9 (13.4) | 1143.4 (100.0) |
Discussion
Summary
The analysis presented above indicates that nonphysician clinicians provide about 21.0 percent of the generalist ambulatory visits performed in Washington State. The contribution of NPCs is slightly higher in rural parts of the state, about 24.7 percent compared to 20.1 percent in urban areas. These estimates are improvements over those based on unadjusted head counts because they are based on actual productivity data (when available, and imputed estimates when not available) and actual differences in specialty distribution. Converting estimated head counts into FTEs also revealed the difficulties with estimating available care from head counts. There were productivity differences both within and across professions that, when applied to head counts and converted to FTEs, result in steep downward productivity adjustments.
The contribution of NPCs to generalist care in rural geographic HPSAs appeared to be slightly higher than in non-HPSAs, but the observed differences were not found to be statistically significant. We had hypothesized that NPCs would make up a larger part of the care system in HPSAs than in non-HPSAs because NPCs generally cost less and are believed to be easier to recruit and retain than physicians. The data presented here do not generally support that hypothesis. The PAs do appear to make a larger contribution in HSAs with large HPSA populations, compared to non–HPSA HSAs.
Though women make up an increasing part of the generalist physician workforce and are the providers of choice of many female patients (Fennema, Meyer, and Owen 1990), rural medicine has been relatively unattractive to women physicians (Doescher, Ellsbury, and Hart 2000). We hypothesized, therefore, that in rural settings, NPCs would provide a larger share of the care provided by women. This hypothesis was sustained. In rural settings female physicians provided less than half (49.3 percent) of the FTEs provided by women. In contrast, women physicians provided 63.5 percent of the generalist care provided by women in urban settings. In both rural and urban settings, NPs provided the majority of female NPC FTEs.
Limitations
Several data limitations should be borne in mind when evaluating the contribution-to-care estimates discussed above. First, the data come from one state, Washington. The extent to which the productivity estimates and adjustments used to assess contribution-to-care of different provider types are generalizable to other states is not known. The methods for estimating contribution-to-care that are outlined above can be used to generate estimates from other states using licensing data. Other state-level studies would definitely enhance our understanding of the contribution of NPCs to generalist care. Caution is also dictated by the cross-sectional study design; significant increases in the supply of NPs and PAs during the 1990s and into the current decade could alter the relative contributions to care in Washington and elsewhere.
Because we wanted to assess the total contribution to generalist care made by physicians, NPs, and PAs, we could not simply exclude cases missing productivity data. It was necessary to develop the imputation method described above for estimating productivity (and sometimes specialty and active/nonactive status) based on the known population of providers. Any productivity estimate is bound to involve some inaccuracy. The degree of error will vary with the proportion of cases being estimated compared to the proportion that is known and the degree to which the respondents were representative of the nonrespondents. This is most problematic for the NP estimates since NPs responded to the survey instrument at a much lower rate than physicians or PAs. For example, if survey nonrespondent NPs were less likely to be actively practicing, their contribution to primary care would be less than estimated.
In interpreting the results of the study the reader is cautioned that observed differences in productivity across professions may reflect either differences in hourly productivity or differences in number of hours worked (or, most likely, both) (Larson, Ballweg, and Hart 2001). Since our purpose here was to assess the overall contribution of NPCs to generalist ambulatory care, we did not adjust our contribution estimates for hours worked. Our estimates are based on reports of total ambulatory visits performed weekly.
Any time physicians are compared to other clinicians the question of substitutability is raised. Washington's less restrictive practice environment for NPs and PAs may allow for a level of substitution not found in other states where prescriptive authority, insurance requirements, and supervisory arrangements may allow considerably less substitution. Caution must also be exercised in employing these findings in discussions of provider shortage mitigation. The NPCs may be providing 25 percent of care in a location and the overall provider population ratio may seem reasonable—but this does not mean, necessarily, that there is no physician shortage in that place. A population with a high disease burden of severe acute or chronic illness, for example, may require a higher number of visits to physicians (as opposed to NPCs) than a population with a lower burden. The health of a local population, patient preferences, facilities, and a host of other factors make up the background that determines the constellation of services and providers that will effectively address the health care needs of a given population. Access to primary care ambulatory visits is important, but hospitals, emergency care systems, and public health systems all play vital roles in addressing those needs as well. Finally, the FTE estimates shown above should be treated with caution. While the proportion-of-care estimates are stable, the FTE estimates shown are based on national (and Washington state) estimates of full-time family physician productivity (105 outpatient visits per week). In some situations, another FTE standard, such as median generalist productivity in a given state, might be deemed more appropriate.
Conclusions
The results of this study point to the need for empirically based estimates of provider counts and provider productivity. For example, proposed changes to HPSA designation rules include a change that would count PAs and NPs as .5 of a primary care physician FTE (Department of Health and Human Services 1998). Under the proposed rules, all primary care physicians are counted as one FTE. No adjustments are made for specialty, part-time status, or any actual known productivity data. The results of this study indicate strongly that simple provider head counts are likely to result in severe overestimates of available care. Recall, for example, that we estimated that a total of 4,145 generalist physicians produce only 2,760 family physician FTEs. The NP and PA counts were also decreased substantially when turned into FTEs.
While head count to FTE adjustments are important, it is also important to consider productivity differences across and within provider groups. Work based on a national sample of PAs (Larson, Ballweg, and Hart 2001), as well as some earlier work (Cyr 1985; Scheffler, Waitzman, and Hillman 1996), for example, suggests that generalist PAs are likely to perform about 75 percent as many outpatient visits as generalist physicians, not the 50 percent suggested in the proposed HPSA designation rules. Nurse practitioners appear more likely to work part-time than other providers. However, their hourly visit productivity appears to be only slightly lower than for PAs. In a case where one is trying to estimate the available care in a given area, it is obviously important to know the part-time/full-time distribution of providers both within and across professions. Taken together, the analyses presented above highlight the inherent and severe weaknesses associated with using provider head count to population ratios as measures of available care. More accurate estimates of provider productivity and contribution-to-care can significantly enhance our ability to assess provider shortage, identify solutions, and plan for the education of future health care providers. Such estimates can be made using the methods outlined above with data that are relatively simple and inexpensive to collect.
This study describes the overall configuration of generalist care in Washington State in 1998–1999 and shows that NPCs provide over 20 percent of the generalist ambulatory visits performed in urban areas and 24 percent in rural areas. Additionally, rural areas of Washington State are particularly dependent on NPCs for women primary care providers. Clearly, NPC contributions must be taken into account whenever one is trying to assess the availability of generalist care. At the same time, care must be taken with the methods used to count providers and estimate productivity. When working from provider head count data, the use of productivity adjustment procedures, such as those described above, are essential for accurate estimates of provider shortages and available care.
Acknowledgments
The authors would like to thank the Eastern Washington Area Health Education Center, the Western Washington Area Health Education Center, the Washington State Department of Health, and Vince Schueler of the Washington State Office of Community and Rural Health for their assistance with data collection.
References
- Cyr KA. “Physician-PA Practice in a Military Clinic: A Statistical Comparison of Productivity/Availability.”. Physician Assistant. 1985:112–24. (April): [PubMed] [Google Scholar]
- Department of Health and Human Services “Designation of Medically Underserved Populations and Health Professional Shortage Areas—Proposed Rules.”. Federal Register. 1998;5(169) [PubMed] [Google Scholar]
- Doescher M, Ellsbury KE, Hart LG. “The Distribution of Rural Female Generalist Physicians in the United States.”. Journal of Rural Health. 2000;16(2):111–8. doi: 10.1111/j.1748-0361.2000.tb00444.x. [DOI] [PubMed] [Google Scholar]
- Fennema K, Meyer DL, Owen N. “Sex of Physician: Patients' Preferences and Stereotypes.”. Journal of Family Practice. 1990;30(4):441–6. [PubMed] [Google Scholar]
- Hart LG. Washington Academy of Family Physicians, 1996–97 Survey of Family Physicians. Woodinville, WA: Washington: Academy of Family Physicians; 1998. [Google Scholar]
- Hart LG, Palazzo L. Off with Their Headcounts! The Consequences of Using FTEs for Generalist Shortage Designation. Seattle, WA: Department of Family Medicine, University of Washington; In press. WWAMI Center for Health Workforce Studies, working paper. [Google Scholar]
- Larson EH, Ballweg R, Hart LG. “National Estimates of Physician Assistant Productivity.”. Journal of Allied Health. 2001;3(3):146–52. [PubMed] [Google Scholar]
- Randolph LB, Seidman B, Pasko T. Physician Characteristics and Distribution in the U.S. Chicago: American Medical Association; 1997. [Google Scholar]
- Ricketts TC, Hart LG, Pirani M. “How Many Rural Doctors Do We Have?”. Journal of Rural Health. 2000;16(3):198–207. doi: 10.1111/j.1748-0361.2000.tb00457.x. [DOI] [PubMed] [Google Scholar]
- Ricketts TC, Johnson-Webb KD, Taylor P. Definitions of Rural: A Handbook for Health Policy Makers and Researchers. Washington, DC: Health Resources and Services Administration, Department of Health and Human Services; 1998. Federal Office of Rural Health Policy technical issues paper. [Google Scholar]
- Scheffler RM, Waitzman NJ, Hillman JM. “The Productivity of Physician Assistants and Nurse Practitioners and Health Work Force Policy in the Era of Managed Care.”. Journal of Allied Health. 1996;25(3):207–17. [PubMed] [Google Scholar]