Abstract
Objective
To characterize and describe variability in processes of asthma care and services tailored for low–income populations in practice sites participating in Medicaid managed care (MMC).
Study Setting
Eighty-five practice sites affiliated with five not-for-profit organizations participating in managed Medicaid (three group-model health maintenance organizations [HMOs] and two Medicaid managed care organizations [MCOs]).
Study Design/Data Collection
We conducted a mail survey of managed care practice site informants using a conceptual model that included chronic illness care and services targeting low-income populations. The survey asked how frequently a number of processes related to asthma care occurred at the practice sites (on a scale from “never” to “always”). We report mean and standard deviations of item scores and rankings relative to other items. We used within-MCO intraclass correlations to assess how consistent responses were among practice sites in the same MCO.
Principal Findings
Processes of care related to asthma varied greatly in how often practice sites reported doing them, with information systems and self-management support services ranking lowest. There was also significant variation in the availability of services targeting low-income populations, specifically relating to cultural diversity, communication, and enrollee empowerment. Very little of the site-to-site variation was attributable to the MCO.
Conclusions
Our conceptual framework provides a means of assessing the provision of chronic illness care for vulnerable populations. There is room for improvement in provision of chronic asthma care for children in managed Medicaid, particularly in the areas of self-management support and information systems. The lack of consistency within MCOs on many processes of care suggests that care may be driven more at the practice site level than the MCO level, which has implications for quality improvement efforts.
Keywords: Chronic illness care, low-income populations, Medicaid managed care
Medicaid managed care (MMC) has the potential to ensure quality of care for poor children by increasing access to care (Gadomski, Jenkins, and Nichols 1998). However, the rapid infusion of large numbers of Medicaid-enrolled children into varied managed care arrangements warrants close scrutiny (Finkelstein et al. 2000; Apter et al. 2001; Porell 2001). In addition to concerns about the delivery of high-quality chronic illness care (Landon and Epstein 1999), MMC faces the challenge of tailoring policies and services to the needs of low-income, culturally diverse, and non-English-speaking populations (Deal and Shiono 1998; Landon and Epstein 1999; Stevens and Shi 2002). Few evaluations of quality of care within MMC have attempted to ascertain the processes of care at the level of the primary care practice (Hurley, Freund, and Paul 1993; Gadomski, Jenkins, and Nichols 1998; Landon and Epstein 1999; Cooper and Kuhlthau 2001; Porell 2001) nor have they addressed the heterogeneity of health plans and clinics that participate in managed Medicaid (Shields et al. 2002).
In 1998, we began the Asthma Care Quality Assessment (ACQA) Study, which followed Medicaid-insured children with asthma in 85 practice sites in five health plans across three states. ACQA focused on two areas in particular: (1) quality of clinical services and (2) the provision of care that is tailored to the needs of low-income, culturally diverse populations. We chose to examine asthma care as an indicator of the quality of clinical services because of the existence of evidence-based guidelines for this common condition as well as a number of clinical tools and strategies for implementing the guidelines (National Asthma Education and Prevention Program 1997; Lozano and Lieu 1999). The current study was designed to describe processes of asthma care and services tailored for low-income populations in the 85 practice sites affiliated with these five managed care organizations (MCOs), as reported by clinic leadership, and to evaluate the extent of variability in these processes both within and between MCOs.
Methods
Design
The Asthma Care Quality Assessment (ACQA) Project is a multipart observational study aimed at identifying factors influencing quality of care for Medicaid-insured children with asthma. This article reports on a cross-sectional survey of leaders in 85 primary care practice sites affiliated with five MCOs participating in Medicaid in three states. Practice site was defined as a group of clinicians working in the same location to provide primary care, including both multispecialty practices and primary care clinics.
Study Settings
We studied practice sites in five large not-for-profit MCOs: the Harvard Vanguard Medical Associates population of Harvard Pilgrim Health Care (HVMA/HPHC) and Neighborhood Health Plan (NHP) in Massachusetts, Kaiser Permanente (KP) in Northern California, Partnership Healthplan of California (PHC), and Group Health Cooperative (GHC) in Washington State. The HVMA/HPHC, KP, and GHC are group-model health maintenance organizations (HMOs) in which a large provider group contracts exclusively or almost exclusively with the health insurance plan. Medicaid members are in the minority in these HMO populations, where most members receive health benefits through their employer. In contrast, NHP and PHC are mixed-model Medicaid MCOs that contract with a variety of provider groups, including multispecialty and pediatric physician groups and community health centers. The NHP and PHC serve primarily low-income, publicly insured or uninsured populations. In all five participating MCOs, primary care services are capitated for most members, while payment mechanisms for specialty and hospital services vary among plans.
The populations served by these practice sites are described elsewhere (Lieu et al. 2002). The self-reported race/ethnicity of parents of Medicaid-insured children with asthma surveyed for the ACQA study was, among group model sites: 38 percent black, 30 percent white, 21 percent mixed race, 7 percent Latino, and 4 percent other; and among Medicaid MCO sites: 34 percent Latino, 28 percent black, 20 percent white, 15 percent mixed race, and 3 percent other.
Practice Site Data Collection
Study staff asked the medical director or clinic manager in each practice site to identify an individual who could be authoritative on the process of care in that site. Study staff made introductory contact with the designated informant by phone or e-mail prior to mailing the practice site survey. If the informant indicated that another clinic member would be a more appropriate respondent, we sent the survey to that individual. After two weeks, study staff contacted nonrespondents and offered to mail a second copy of the survey or to conduct the survey by phone. The main informant was encouraged to obtain information from colleagues if he or she did not feel qualified to answer particular items.
Survey instrument
The 45-item process-of-care survey was developed empirically for this study to assess asthma care and care for low-income populations. Selection of relevant domains in these two areas was guided by the Chronic Care Model (Wagner, Austin, and Von Korff 1996a; Wagner, Austin, and Von Korff 1996b; Wagner et al. 1999; Wagner et al. 2001) (Figure 1) and informed by Starfield's Primary Care Model (Starfield 1992). Because we were interested in aspects of care that address the specific needs of poor populations, we conducted three focus groups of clinicians and staff at three urban primary care clinics in Seattle (not affiliated with the five MCOs participating in the survey). Participants were asked to list processes of care that were important in providing care to disadvantaged populations. Participants grouped structures and processes into several domains. One of the authors (PL) compared the nominated domains to the Chronic Care Model and identified overlapping concepts as well as domains specific to low-income populations. Selected focus group participants reviewed drafts of the framework and provided feedback. The resulting framework included six domains of asthma care and three domains of care for low-income populations. The Appendix shows all nine domains, their definitions, and the corresponding survey items.
Figure 1.
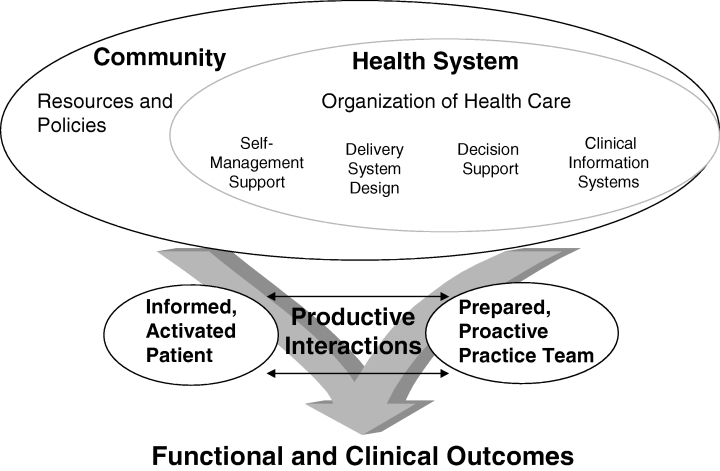
The Chronic Care Model
All items began with the root, “How routinely does your practice site…?” Response categories for all 45 items were never, occasionally, usually, and always. The 26 asthma items represent six domains: self-management support, delivery system design, information systems, decision support, community linkages, and health system (Lozano and Lieu 1999). Items were adapted from the Assessment of Chronic Illness Care (Bonomi et al. 2002), a tool for assessing processes of chronic illness care that is based on the Chronic Care Model (Figure 1) and is responsive to quality improvement efforts. The asthma items represent care processes that have been shown to be associated with high-quality asthma care or, in a generic sense, high-quality chronic illness care (Wagner, Austin, and Von Korff 1996a; Wagner, Austin, and Von Korff 1996b; Wagner et al. 1999; Wagner et al. 2001). Many of these items are cited as components of quality care in the National Asthma Education and Prevention Program's Expert Panel Report (National Asthma Education and Prevention Program 1997). The 12 items pertaining to low-income populations represent three domains: cultural competency, communication, and empowerment. Items were derived from the content of the focus groups. An additional seven items asked about practice site characteristics. Survey items are shown in Tables 2 and 3, as well as in the Appendix, where supporting citations from the literature are listed for each item.
Table 2.
Practice Site Reports of Asthma Processes of Care Sorted by Rating within Each Type of Process
| Processes of Asthma Care | Percent Usually/Always | Mean | SD | Rank | Intraclass Correlation Coefficient within MCO |
|---|---|---|---|---|---|
| Self-Management Support | |||||
| Teach spacer technique | 88 | 3.42 | 1.12 | 1 | .04 |
| Peak flow meters available, low cost | 83 | 3.29 | 1.99 | 2 | .18 |
| Spacers available, low cost | 83 | 3.26 | 0.99 | 3* | .16 |
| Nebulizers available, low cost | 74 | 2.99 | 1.14 | 12 | .16 |
| Make written care plan accessible to primary care, urgent care | 54 | 2.46 | 1.13 | 16 | <.01 |
| Prepare individualized written care plans | 44 | 2.42 | 0.90 | 17 | −.02 |
| Provide self-management support by referral to designated asthma nurse or educator | 50 | 2.40 | 1.04 | 18 | .08 |
| Promote self-management support using problem- solving, empowerment methodologies | 49 | 2.26 | 0.97 | 20 | .01 |
| Assess self-management needs | 10 | 1.49 | 0.82 | 25 | −.03 |
| Mean ICC for all self- management support items | .08 | ||||
| Delivery System Design | |||||
| Ensure primary care provider assignment | 86 | 3.18 | 0.99 | 8 | −.02 |
| Systematically promote continuity in appointments | 92 | 3.19 | 0.78 | 7 | .05 |
| Primary care provider for same-day appointments | 88 | 3.20 | 0.76 | 6 | .10 |
| Ensure primary care follow- up after urgent care visit | 90 | 3.22 | 0.61 | 5 | .26* |
| Promote preventive asthma management visits | 75 | 3.04 | 0.81 | 11 | .16 |
| Use asthma nurses, other case managers | 42 | 2.32 | 1.14 | 19 | .37* |
| Mean ICC for all delivery system design items | .16 | ||||
| Information Systems | |||||
| Reminders about guidelines at individual encounters | 33 | 2.03 | 1.07 | 21 | .09 |
| Feedback reports to providers to improve asthma care | 30 | 1.94 | 0.96 | 22 | .24* |
| Provide registries to clinicians | 14 | 1.66 | 0.88 | 23* | .54* |
| Use registries to prompt clinicians regarding guidelines | 21 | 1.66 | 1.06 | 23* | .34* |
| Mean ICC for all information systems items | .30 | ||||
| Decision Support | |||||
| Promote two-way communication between specialist and primary care | 88 | 3.26 | 1.17 | 3* | −.05 |
| Facilitate specialist referral for difficult cases | 84 | 3.07 | 1.02 | 10 | −.01 |
| Promote guidelines | 83 | 3.12 | 0.97 | 9 | .07 |
| Involve specialists involved in primary care for asthma | 53 | 2.55 | 0.90 | 15 | .01 |
| Asthma education for primary care providers, nurses | 51 | 2.59 | 0.94 | 14 | .09 |
| Mean ICC for all decision support items | .03 | ||||
| Community Linkages | |||||
| Coordinate with community resources, e.g. school nurse | 56 | 2.60 | 0.74 | 13 | .05 |
| Mean ICC for community linkages item | .05 | ||||
| Health System | |||||
| Contractual incentives | 1 | 1.04 | 0.48 | 26 | −.03 |
| Mean ICC for health system item | −.03 | ||||
Mean score: 1=never, 2=occasionally, 3=usually, 4=always. Rank is based on mean score.
ICC=intraclass correlation coefficient=Var(MCO)/[Var(PS)+Var (MCO)]. ICCs were not truncated at zero.
The strength of correlation between each individual process of care and MCO was defined as weak: (ICC<.1 or p>.05), moderate (p<.05 and ICC between .1 and .299) or strong (p<.05 and ICC .300 or greater). Asterisk denotes moderate or strong correlation, and, by definition, p<.05. Mean ICC for each domain represents the mean of the ICCs for each item in the domain. Strength of correlation was not rated for mean ICCs.
Human Subjects
Respondents provided informed consent. The study protocol was approved by the Institutional Review Boards of the participating sites.
Analysis
For each item, we computed the mean and standard deviation on a four-point scale (1=never, 2=occasionally, 3=usually, 4=always) as well as the percent of sites reporting “usually” or “always.” We ranked items by mean. We computed an intraclass correlation coefficient for each item to assess the extent to which practice sites within an MCO gave consistent reports. The strength of within-MCO correlation was rated weak (ICC<.1 or p>.05), moderate (p<.05 and ICC between .1 and .299), or strong (p<.05 and ICC .300 or greater).
Results
Representatives from 73 of 85 sites completed the survey, for an 86 percent overall response rate. Thirty-four belonged to one of three group-model HMOs and 39 were members of one of two Medicaid MCOs (Table 1). The latter included 20 community health centers, 10 single specialty or solo practices, 4 multispecialty group practices, and 4 academic health centers. Other characteristics are shown in Table 1. Practice site survey respondents included clinic administrators (28 percent), physicians (37 percent), and nurses (22 percent). Distribution of respondent types was similar between group model HMOs and Medicaid MCOs.
Table 1.
Practice Site Characteristics
| Site Affiliated with: | ||
|---|---|---|
| Practice Site Characteristic | Group-Model HMOs | Medicaid MCOs |
| Number of sites responding (response rate) | 34 (89%) | 39 (83%) |
| Practice site type, n (%) | ||
| Multispecialty group practice or HMO | 33 (97) | 4 (10) |
| Single specialty group or solo practice | 1 (3) | 10 (26) |
| Community health center | 0 (0) | 20 (51) |
| Academic health center | 0 (0) | 4 (10) |
| Other or missing | 0 (0) | 1 (2) |
| Number of pediatric primary care providers* at site, median (IQR†) | ||
| Physicians | 6 (4–10) | 4 (3–8) |
| Nurse practitioners or physician assistants | 2 (1–5) | 2 (1–3) |
| Estimated proportion (%) of site's patient population insured by Medicaid, median (IQR†) | 14 (9–20) | 45 (33–65) |
Pediatric primary care providers include physicians and midlevel providers who practice either pediatrics or family practice.
IQR=interquartile range.
Asthma Care
Mean scores, rankings, and percent of usually/always for the 27 processes of asthma care are shown in Table 2. Practice site respondents' ratings of asthma processes of care ranged widely from 1 to 92 percent of clinics responding usually/always (Table 2).
As a group, the information system items ranked lowest, comprising four of the six lowest ranked items in the asthma portion of the survey. The frequency with which practice sites responded “usually” or “always” ranged from 14 percent (provide registries) to 33 percent (provide reminders about guidelines at individual encounters).
Items in the self-management support category relate to assisting patients and families in taking a central role in asthma care. Processes in this category varied widely. Most highly rated were device-related items: teaching spacer technique (88 percent usually/always), and making peak flow meters (83 percent) and spacers (83 percent) available at low cost. Less frequently endorsed were several types of self-management support strategies that have been proven effective across chronic conditions (Clark and Gong 2000). Only 10 percent of sites reported that they usually/always assessed self-management needs, almost the lowest-ranking item in the survey. Several processes yielded usually/always responses from about half the sites: preparing written care plans (44 percent), providing self-management support by referral to a designated asthma nurse or educator (50 percent), and promoting self-management support using problem-solving or empowerment methodologies (49 percent).
Decision-support items relate to various mechanisms of assisting primary care providers in clinical decision-making, including expert advice, guidelines, and provider education.
Three of five items were rated usually/always in 83 percent or more of practice sites: promoting two-way communication between specialist and primary care (88 percent), facilitating specialist referral for difficult cases (84 percent), and promoting guidelines (83 percent). About half (51 percent) reported asthma education for primary care providers and nurses.
Delivery system design items relate to designated roles and structures for proactive care. In this area, the four items relating to continuity of care (primary care provider assignment, promoting continuity in appointments, scheduling primary care provider for same-day appointments, ensuring primary care follow-up after urgent care) were uniformly ranked highly with 86 to 92 percent of practice sites responding usually/always. The least highly ranked item in this category was the use of asthma nurses and other case managers (37 percent usually/always).
Care for Low-Income Populations
Responses for questions about services targeting low-income populations were more narrowly distributed than asthma care items, with 10 of 12 items rated as usually/always from 38 percent to 72 percent of clinics (Table 3). Within the area of cultural competency (addressing ethnic and cultural barriers to care), two thirds of clinics (70 percent) reported they usually/always recruit ethnically diverse nurses and providers. Only 14 percent reported usually/always evaluating cultural competency, the lowest-ranked item in the section on services for low-income populations. Almost half (49 percent) of sites reported minimizing cultural barriers through the use of written materials and posters and more than a third (38 percent) offered training in cross-cultural health or diversity.
Table 3.
Practice Site Reports of Processes of Care Targeting Low-Income Populations Sorted by Rating within Each Type of Process
| Processes of Care Targeting Low-Income Populations | Percent Usually/Always | Mean | SD | Rank | Intraclass Correlation Coefficient within MCO |
|---|---|---|---|---|---|
| Cultural Competency | |||||
| Recruit ethnically diverse nurses, providers | 70 | 2.93 | 0.95 | 2 | .21* |
| Minimize cultural barriers by written material, posters | 49 | 2.56 | 0.91 | 6 | .29* |
| Offer cross-cultural health, diversity training to staff | 38 | 2.18 | 1.04 | 10 | .48* |
| Evaluate cultural competency among staff | 14 | 1.79 | 12 | .26* | |
| Mean ICC for all cultural competency items | .31 | ||||
| Communication | |||||
| Access to skilled medical interpreters | 72 | 3.14 | 1.06 | 1 | .02 |
| Non-English telephone support | 63 | 2.89 | 1.44 | 3 | .14 |
| Recruit bilingual nurses, providers | 58 | 2.67 | 1.03 | 4 | .52* |
| Low-literacy health education materials | 59 | 2.58 | 0.96 | 5 | .12 |
| Communication skills training for staff | 24 | 2.04 | 1.01 | 11 | .24* |
| Mean ICC for all communication items | .21 | ||||
| Empowerment | |||||
| Promote enrollee understanding of managed care | 54 | 2.41 | 1.19 | 7 | .09 |
| Proactively orient new enrollees | 48 | 2.34 | 1.12 | 8 | .16 |
| Designate staff to assist patients in navigating system | 42 | 2.29 | 1.11 | 9 | .39* |
| Mean ICC for all empowerment items | .21 | ||||
Mean score: 1=never, 2=occasionally, 3=usually, 4=always. Rank is based on mean score.
ICC=intraclass correlation coefficient=Var(MCO)/[Var(PS)+Var (MCO)]. ICCs were not truncated at zero.
The strength of correlation between each individual process of care and MCO was defined as weak: (ICC<.1 or p>.05), moderate (p<.05 and ICC between .1 and .299) or strong (p<.05 and ICC .300 or greater). Asterisk denotes moderate or strong correlation, and, by definition, p<.05. Mean ICC for each domain represents the mean of the ICCs for each item in the domain. Strength of correlation was not rated for mean ICCs.
Communication items relate to enhancing communication with low-literacy enrollees and non-English-speakers. In this domain, access to medical interpreters and non-English telephone support were ranked most highly (72 percent and 63 percent of clinics reporting usually/always). Least commonly endorsed was communication skills training (24 percent of practices). Slightly more than half the sites reported they usually/always recruit bilingual nurses or providers (58 percent) and use low-literacy health education materials (59 percent).
Empowerment items relate to providing patients with tools to access care effectively. Among the services aimed at empowering low-income clients, none of the three items was endorsed by more than 54 percent of clinics (promoting understanding of managed care). Forty-eight percent of sites report pro-actively orienting new enrollees and 42 percent report that they designate staff to assist enrollees in navigating the managed care system.
Variability between and within MCOs
To determine the extent to which processes of care tended to vary across practice sites as opposed to varying between MCOs, we computed intraclass correlation coefficients (Tables 2 and 3). Intraclass correlation coefficients for the processes of care tended to be low, with a few exceptions. For most asthma processes of care, most of the variation occurred at the level of the practice site. Only six processes (all items related to delivery system design and information systems) had moderate or strong correlations with the MCO (Table 2). In contrast, greater consistency within MCO was noted among the services targeting low-income populations, where seven of twelve items were moderately or strongly associated with the MCO (Table 3).
Discussion
This study represents one of the first attempts to characterize the services provided by practice sites that participate in managed Medicaid and included a variety of types of practices sites in five highly regarded managed care organizations. Given the participating MCOs' reputations for engagement in quality improvement activities and their interest in assessing their services for managed Medicaid enrollees (as evidenced by participation in the ACQA study), our findings may represent optimistic estimates of care processes in other organizations. Reports of how often asthma care services occur varied widely across items and many processes associated with asthma care quality were often not available. Respondents reported limited use of information systems and of state-of-the-art self-management support services (assessment, written care plans, problem-solving techniques). Some of the most highly ranked items included concepts that may be easy to endorse, but difficult to quantify (for example, promoting continuity or ensuring primary care provider assignment).
Services targeting low-income populations varied less widely across items than asthma care processes. Although no benchmarks exist for these services, our findings highlight some areas for further exploration. Support for diversity training and evaluation of cultural competency of the organization was limited. Practice sites appear to be variably involved in assisting patients in overcoming the barriers posed by the complex regulations of managed care. Our findings suggest possible areas for self-assessment and improvement for practice sites now attempting to confront the challenges of meeting the complex needs of Medicaid populations.
Our findings suggest that the MCOs in this study may not have been exerting a major influence on some elements of asthma care in their participating practice sites. Among the processes with strongest correlations within MCO were the use of registries and reports and case management by asthma nurses or other personnel. Because these processes require resources that are difficult for smaller practices to afford, the MCO has the potential to play an important role in facilitating those asthma care processes. Managed care organization affiliation accounted for a larger proportion of variation in processes of care for low-income populations across practice sites (compared to that for asthma care processes). This may be a reflection of the fact that primary care sites that have traditionally served poor or ethnically diverse populations continue to do so, and have developed the services and programs that facilitate their mission. The role of MCO policies in the availability of these services is not known.
Limitations
The major limitation of this study is its reliance on respondents' perceptions of the provision of care in the clinic as a whole. This choice was dictated by our aim to characterize care at the practice site level (not the care provided by individual physicians or the policies of the MCO). Social desirability bias may have inflated the prevalence of the processes of care reported here. Conversely, there may have been underreporting of processes of care that did not originate from or flow through practice site structures (e.g., feedback reports provided by the health plan directly to physicians). We recognize that our measurement strategy resulted in a lack of information about within-site variation. Confirmation of reported processes of care for all practice sites by direct observation would have been infeasible in this study. However, respondents were chosen for their knowledge of the practice site's operations. We purposefully allowed heterogeneity of respondents (leaders with clinical and nonclinical roles) in order to allow the selection of the most appropriate respondent for each site. We also note that measurement error would reduce the power to detect differences among sites
The method used to generate the conceptual domains and survey items for processes relating to low-income populations relied on focus groups. We acknowledge that the group dynamic of focus groups can inhibit the airing of divergent opinions. Further refinement of this instrument should involve critique by individual informants.
Another limitation is the lack of benchmarks. The processes of care for asthma we examine here are supported by varying degrees of evidence (see Appendix: http://www.blackwell publishing.com/products/journals/suppmat/HESR/HESR02200/HESR02200sm.htm). While each individual item may not be required for high-quality asthma care, these process are consistent with the NAEPP Expert Panel Report (National Asthma Education and Prevention Program 1997) and, taken together, the 26 items represent a set of services that can improve quality of asthma care. Although there is no comparable evidence-based guideline addressing needs specific to low-income populations, there is ample evidence that the domains of cultural competency, communication, and empowerment as defined here influence the health care experience for poor and culturally or linguistically diverse families. Other reports from the ACQA Study are examining quality of care as defined by health outcomes at the patient level.
And finally, the five not-for-profit MCOs that participated in this study cannot be considered to be representative of Medicaid managed care nationally. We cannot generalize our findings to for-profit MCOs or to Medicaid managed care in other regions of the United States. (In fact, we believe our findings may represent optimistic estimates of care processes in other organizations.) However, the participating MCOs do represent two different major models of managed Medicaid and consist of a large number practice sites.
Implications
The great variation in reports of asthma care likely reflects true variability in processes of care and suggests that there are opportunities for improvement in services for children with asthma in managed Medicaid, specifically information systems and self-management support services. Significant variation also exists in the availability of services relating to cultural diversity, communication, and enrollee empowerment. Further research is needed to define services associated with quality of care for multicultural and disadvantaged populations. Organizations participating in managed Medicaid could play a larger role in improving asthma care processes in practice sites.
Our conceptual framework, which combines the Chronic Care Model with additional domains to address the needs of low-income patients, provides a means of assessing the provision of chronic illness care for vulnerable populations. The process-of-care survey developed for the ACQA study represents an early attempt to operationalize this model in the form of a practice site self-assessment tool. The considerable between-practice site variation we observed suggests that assessment at the MCO level alone would provide an incomplete evaluation of care processes delivered by the individual sites participating in the MCO. Further studies using such tools for evaluation and quality improvement are needed.
Acknowledgments
We gratefully acknowledge Nancy Jensvold, M.P.H., Cynthia Sisk, M.A., and Kachen Streiff, M.A., for coordinating the surveys; Angela Capra, M.A., and Felicia Chi, M.P.H., for preparing the analytic databases, and Amy Bonomi, M.P.H. and Ed Wagner, M.D., M.P.H., for fruitful discussions of this work at various stages. We thank our senior advisors at the health plans in this study, including Chris Cammisa, M.D. (PHC), Robert Master, M.D. (NHP), James Glauber, M.D. (NHP), Edward Wagner, M.D. (GHC), and Richard Platt, M.D. (HPHC). The ACQA study is indebted to the numerous primary care site leaders and administrators who participated in our survey.
Appendix
Asthma Care Processes and Services for Low-Income Populations: Domains, Domain Definitions, Items, and Supporting References.
| Processes of Asthma Care domains, definitions, and items* | References |
|---|---|
| Self-Management Support: assisting patients in taking a central role in their self-care | |
| 1. Ensure that patients are taught proper technique when spacers are dispensed | NAEPP 1997 |
| 2. Make peak flow meters available at low cost to enrollees | NAEPP 1997 |
| 3. Make spacers available at low cost to enrollees | NAEPP 1997 |
| 4. Make nebulizers available for rent or purchase at low cost to enrollees | NAEPP 1997 |
| 5. Make asthma care plans readily accessible to primary and acute care providers | NAEPP 1997 |
| 6. Prepare individualized written asthma care plans | NAEPP 1997; NAEPP 1995; Lieu, Quesenberry, Capra et al. 1997 |
| 7. Provide self-management support through referral to a designated asthma nurse or educator | NAEPP 1997; NAEPP 1995; Gallefoss and Bakke 1999 |
| 8. Promote self-management using problem-solving and patient empowerment methodologies | Clark and Gong 2000 |
| 9. Assess self-management needs of asthma patients by questionnaire or computer | NAEPP 1997; NAEPP 1995; Clark and Gong 2000 |
| Delivery System Design: designated roles and structures for proactive care | |
| 1. Ensure assignment of all patients to primary care provider | Sox et al. 1998; Christakis, Mell, Koepsell et al. 2001 |
| 2. Systematically promote continuity of care in appointment-making | Sox et al. 1998; Christakis, Mell, Koepsell et al. 2001 |
| 3. Make an effort to have the primary care provider see patients who make same-day appointments | Sox et al. 1998; Christakis, Mell, Koepsell et al. 2001 |
| 4. Ensure follow-up in primary care clinic after an acute visit in an urgent care setting | NAEPP 1997, Sin et al. 2002 |
| 5. Promote appointments for preventive chronic asthma management visits | NAEPP 1997; Stout, White, Rogers et al. 1998; Greineder, Loane and Parks 1999; Fardy 2001 |
| 6. Use asthma nurses, educators, or lay outreach workers to provide asthma case management | NAEPP 1997; Wissow et al. 1988; Stout, White, Rogers et al. 1998 |
| Information Systems: tracking and reminder systems | |
| 1. Provide reminders to providers about asthma guideline adherence for individual patient encounters | Feder, Griffiths and Highton 1995; Bordley 2001 |
| 2. Give feedback reports to providers to improve performance in asthma care | Palmer 1985; Heinrich and Homer 1999 |
| 3. Provide clinician lists of asthma patients in their panels (registries) | Newacheck, Stein, Walker et al. 1996 |
| 4. Use asthma registries that prompt clinicians about appropriate medications or services | Feder, Griffiths, Highton et al. 1995 |
| Decision Support: assisting providers with treatment decisions | |
| 1. Promote two-way communication between specialist and primary care provider | Newacheck et al. 1994; Newacheck, Stein, Walker et al. 1996 |
| 2. Facilitate allergy or pulmonology consultation for difficult asthma cases | Cooper and Kuhlthau 2001 |
| 3. Promote the use of evidence-based asthma guidelines | NAEPP 1997; Ting 2002 |
| 4. Involve allergists or pulmonologists in improving primary care for children with asthma | NAEPP 1997 |
| 5. Offer asthma education to primary care providers and nurses | NAEPP 1997; NAEPP 1995 |
| Community Linkages: partnerships between the practice site and community resources | |
| Coordinate asthma care with appropriate community resources, such as school nurses | NAEPP 1997 |
| Health system: measures taken by the organization to facilitate chronic illness care | |
| Use contractual incentives to motivate providers to improve asthma care | NAEPP 1997 |
| Processes of Care Targeting Low-Income Populations: Domains and Items | |
| Cultural Competency: addressing ethnic and cultural barriers | |
| 1. Recruit ethnically diverse nurses and providers | Cooper-Patrick, Gallo, Gonzales et al. 1999; Saha et al. 2000; Centers for Medicare & Medicaid Services 2003b. |
| 2. Attempt to minimize cultural barriers to care through use of printed materials or waiting room posters depicting different ethnic or cultural groups | NAEPP 1995; Centers for Medicare & Medicaid Services 2003b. |
| 3. Offer cross-cultural health inservices or diversity training to staff and providers | Van Ryn and Burke 2000; AAP Committee on Pediatric Workforce 1999 |
| 4. Evaluate the level of cultural competency among staff and providers | Landon and Epstein 1999; Elixhauser 2002; Schneider, Zaslavsky and Epstein 2002 |
| Communication: enhancing health communication with low literacy populations and non-English speakers | |
| 1. Have ready access to a defined pool of skilled medical interpreters | Baker, Parker, Williams et al. 1996; Hornberger, Gibson, Wood et al. 1996; Morales, Cunningham, Brown et al. 1999; Centers for Medicare & Medicaid Services 2003a. |
| 2. Provide telephone support in patients native language for non-English speakers | Baker, Parker, Williams et al. 1996; Hornberger, Gibson, Wood et al. 1996; Morales, Cunningham, Brown et al. 1999 |
| 3. Recruit bilingual nurses and providers | Cooper and Kuhlthau 2001; Centers for Medicare & Medicaid Services 2003a. |
| 4. Provide health education materials oriented to patients/parents with low literacy skills | NAEPP 1995; Weiss and Coyne 1997; Ad hoc committee on literacy 1999; Williams et al. 2002 |
| 5. Offer training to staff and clinicians to develop communication skills such as working with non-English speakers (through interpreters) or patients with poor literacy skills | Weiss and Coyne 1997; Ad Hoc Committee on Literacy for the Council of Scientific Affairs 1999; Weinick and Krauss 2000; Williams et al. 2002 |
| Empowerment Definition: providing patients with tools to access care effectively | |
| 1. Promote an understanding of health services and managed care policies through written material aimed at Medicaid or low-income enrollees, including posted statements of patient rights and responsibilities | Newacheck et al. 1994; Newacheck, Stein, Walker et al. 1996; Gerteis, Harrison, James et al. 2000 |
| 2. Pro-actively orient new enrollees | Newacheck et al. 1994; Newacheck, Stein, Walker et al. 1996; Gerteis, Harrison, James et al. 2000 |
| 3. Designate a staff member(s) to assist low-income patients in navigating the system and to advocate for them | Gerteis, Harrison, James et al. 2000 |
All items were asked with the root: “How routinely does your practice site…?”
Footnotes
Supported by the Agency for Healthcare Research and Quality grant no. HS09935, the American Associations of Health Plans Foundation, and the Maternal and Child Health Bureau.
References
- Apter AJ, Van Hoof TJ, Sherwin TE, Casey BA, Petrillo MK, Meehan TP. “Assessing the Quality of Asthma Care Provided to Medicaid Patients Enrolled in Managed Care Organizations in Connecticut.”. Annals of Allergy Asthma and Immunology. 2001;86(2):211–8. doi: 10.1016/S1081-1206(10)62693-2. [DOI] [PubMed] [Google Scholar]
- Bonomi AE, Wagner EH, Glasgow R, Von Korff M. “Assessment of Chronic Illness Care: A Practical Tool for Quality Improvement.”. Health Services Research Journal. 2002;37(3):791–820. doi: 10.1111/1475-6773.00049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark NM, Gong M. “Management of Chronic Disease by Practitioners and Patients: Are We Teaching the Wrong Things?”. British Medical Journal. 2000;320(7234):572–5. doi: 10.1136/bmj.320.7234.572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper WO, Kuhlthav K. “Evaluating Medicaid Managed Care Programs for Children.”. Ambulatory Pediatrics. 2001;1(2):112–6. doi: 10.1367/1539-4409(2001)001<0112:emmcpf>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Deal LW, Shiono PH. “Medicaid Managed Care and Children: An Overview.”. The Future of Children. 1998;8(2):93–104. [PubMed] [Google Scholar]
- Finkelstein JA, Barton MB, Donahue JG, Algatt-Bergstrom P, Markson LE, Platt R. “Comparing Asthma Care for Medicaid and Non-Medicaid Children in a Health Maintenance Organization.”. Archives of Pediatrics and Adolescent Medicine. 2000;154(6):563–8. doi: 10.1001/archpedi.154.6.563. [DOI] [PubMed] [Google Scholar]
- Gadomski A, Jenkins P, Nichols M. “Impact of a Medicaid Primary Care Provider and Preventive Care on Pediatric Hospitalization.”. Pediatrics. 1998;101(3):E1. doi: 10.1542/peds.101.3.e1. [DOI] [PubMed] [Google Scholar]
- Hurley RE, Freund DA, Paul JE. Managed Care in Medicaid. Ann Arbor, MI: Health Administration Press; 1993. [Google Scholar]
- Kaiser Commission . “Medicaid and Managed Care.”. Washington, DC: Henry J. Kaiser Family Foundation; 2001. [Google Scholar]
- Landon BE, Epstein AM. “Quality Management Practices in Medicaid Managed Care: A National Survey of Medicaid and Commercial Health Plans Participating in the Medicaid Program.”. Journal of the American Medical Association. 1999;282(18):1769–75. doi: 10.1001/jama.282.18.1769. [DOI] [PubMed] [Google Scholar]
- Lieu TA, Lozano P, Finkelstein JA, Chi FW, Jensvold NG, Capra AM, Quesenberry CP, Selby JV, Farber HJ. “Racial/Ethnic Variation in Asthma Status and Management Practices among Children in Managed Medicaid.”. Pediatrics. 2002;109(5):857–65. doi: 10.1542/peds.109.5.857. [DOI] [PubMed] [Google Scholar]
- Lozano P, Lieu TA. “Asthma in Managed Care.”. Pediatric Annals. 1999;28(1):74–80. doi: 10.3928/0090-4481-19990101-13. [DOI] [PubMed] [Google Scholar]
- National Asthma Education and Prevention Program—Expert Panel. Expert Panel Report 2: Guidelines for the Diagnosis and Management of Asthma. Bethesda, MD: U.S. Department of Health and Human Services; 1997. NIH publication no. 97-4051. [Google Scholar]
- Porell FW. “A Comparison of Ambulatory Care-Sensitive Hospital Discharge Rates for Medicaid HMO Enrollees and Nonenrollees.”. Medical Care Research and Review. 2001;58(4):404–24. doi: 10.1177/107755870105800402. [DOI] [PubMed] [Google Scholar]
- Shields AE, Finkelstein JA, Comstock C, Weiss KB. “Process of Care for Medicaid-Enrolled Children with Asthma Served by Community Health Centers and Other Providers.”. Medical Care. 2002;40(4):303–14. doi: 10.1097/00005650-200204000-00006. [DOI] [PubMed] [Google Scholar]
- Starfield B. Primary Care: Concept, Evaluation, and Policy. New York: Oxford University Press; 1992. [Google Scholar]
- Stevens GD, Shi L. “Effect of Managed Care on Children's Relationships with Their Primary Care Physicians: Differences by Race.”. Archives of Pediatrics and Adolescent Medicine. 2002;156(4):369–77. doi: 10.1001/archpedi.156.4.369. [DOI] [PubMed] [Google Scholar]
- Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A. “Improving Chronic Illness Care: Translating Evidence into Action.”. Health Affairs (Millwood) 2001;20(6):64–78. doi: 10.1377/hlthaff.20.6.64. [DOI] [PubMed] [Google Scholar]
- Wagner EH, Austin BT, Von Korff M. “Improving Outcomes in Chronic Illness.”. Managed Care Quarterly. 1996a;4(2):1–14. [PubMed] [Google Scholar]
- Wagner EH, Austin BT, Von Korff M. “Organizing Care for Patients with Chronic Illness.”. Milbank Quarterly. 1996b;74(4):511–44. [PubMed] [Google Scholar]
- Wagner EH, Davis C, Schaefer J, Von Korff M, Austin B. “A Survey of Leading Chronic Disease Management Programs: Are They Consistent with the Literature?”. Managed Care Quarterly. 1999;7(3):56–66. [PubMed] [Google Scholar]


