Abstract
Objective
To compare nursing homes (NHs) that report different staffing statistics on quality of care.
Data Sources
Staffing information generated by California NHs on state cost reports and during onsite interviews. Data independently collected by research staff describing quality of care related to 27 care processes.
Study Design
Two groups of NHs (n=21) that reported significantly different and stable staffing data from all data sources were compared on quality of care measures.
Data Collection
Direct observation, resident and staff interview, and chart abstraction methods.
Principal Findings
Staff in the highest staffed homes (n=6), according to state cost reports, reported significantly lower resident care loads during onsite interviews across day and evening shifts (7.6 residents per nurse aide [NA]) compared to the remaining homes that reported between 9 to 10 residents per NA (n=15). The highest-staffed homes performed significantly better on 13 of 16 care processes implemented by NAs compared to lower-staffed homes.
Conclusion
The highest-staffed NHs reported significantly lower resident care loads on all staffing reports and provided better care than all other homes.
Keywords: Staffing, quality of care
Nursing home (NH) staffing resources necessary to provide care consistent with regulatory guidelines are the subject of national debate due to emerging evidence that existing staffing resources may not be adequate (U.S. Department of Health and Human Services 2000b). One recent study for the Centers for Medicare and Medicaid Services (CMS) reported that 4.1 mean total (nursing aides [NAs] plus licensed nurses) direct care hours per resident per day (hprd) and 1.3 licensed nurse hprd (.75 for registered nurses [RNs] and .55 for licensed vocational nurses [LVNs]) were the minimum staffing levels associated with a lower probability of poor resident outcomes, such as weight loss and pressure ulcers (Kramer and Fish 2001). This study is supported by other correlational data documenting a relationship between staffing (particularly RNs) and a variety of outcomes, including: lower death rates, higher rates of discharges to home, improved functional outcomes, fewer pressure ulcers, fewer urinary tract infections, lower urinary catheter use, and less antibiotic use (Linn, Gurel, and Linn 1977; Nyman 1988; Munroe 1990; Cherry 1991; Spector and Takada 1991; Aaronson, Zinn, and Rosko 1994; Bliesmer et al. 1998; Harrington et al. 2000; U.S. Department of Health and Human Services 2000b). Few studies have specifically examined the relationship between staffing and the implementation of daily care processes, but inadequate staffing has been associated with inadequate feeding assistance during meals, poor skin care, lower activity participation, and less toileting assistance (Spector and Takada 1991; Kayser-Jones 1996, 1997; Kayser-Jones and Schell 1997). The results of these correlational studies led two Institute of Medicine committees to recommend higher nurse staffing in nursing facilities, including 24-hour registered nursing care (Wunderlich, Sloan, and Davis 1996; Wunderlich and Kohler 2001;). An expert panel recommended even higher minimum staffing levels (4.55 hprd including 1.85 licensed nurse hprd) (Harrington et al. 2000). However, neither the correlational studies nor the CMS study directly measured specific care processes that may be better implemented in higher staffed homes and that could explain the effects on resident outcomes.
A second study conducted for CMS focused on this care process implementation issue (Schnelle, Simmons, and Cretin 2001). This study used staff time estimates in computerized simulations to predict the nursing assistant (NA) staffing ratios necessary to provide care recommended in regulatory guidelines. Care processes related to incontinence care, feeding assistance, exercise, and activities of daily living (ADL) independence enhancement (e.g., dressing), all of which are typically implemented by NAs, were included in the simulation. The results of this study showed that 2.8 to 3.2 NA hprd, depending on the acuity level of the NH population, were necessary to consistently provide all of these daily care processes. The NA staffing levels reported in this process-focused study are similar to those recommended by one expert consensus panel who also attempted to identify the labor requirements to implement key care processes, such as feeding assistance (Harrington, Kovner et al. 2000). Unfortunately, 92 percent of the nation's NHs report staffing levels below the staffing minimums identified by the expert panel as well as the two recent CMS studies, and more than 50 percent of NHs would have to double current staffing levels to meet these minimums (U.S. Department of Health and Human Services 2000a).
The fact that so many NHs report staffing levels below this minimum has led to recent efforts to develop staffing indicators so that long-term care consumers can make informed judgements about the adequacy of NH staffing within a facility. However, neither the simulated staffing predictions nor the expert consensus recommendations have been subjected to a field test evaluation. Based on the simulation predictions, one would hypothesize that higher staffed NHs would be better able to provide labor-intense daily care activities, such as feeding assistance, toileting assistance, repositioning, and exercise care. More specifically, it would be predicted that homes that report 2.8 to 3.2 NA hprd would perform significantly better than all other homes in the implementation of these daily care processes. The purpose of this study was to address this issue by describing the relationship between staffing levels in 21 NHs and directly measured processes of care that are both labor intense and recommended in NH regulatory guidelines. The primary question addressed in this study was: Is there a relationship between staffing, as separately reported by NH administrators and NAs, and the implementation of daily care processes that reflect quality of care?
Methods
Subjects and Setting
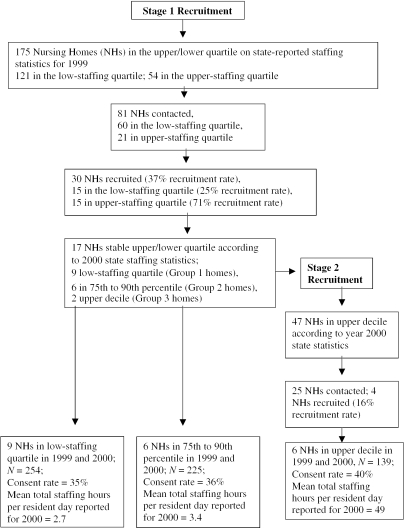
Recruitment of homes was accomplished in two phases (Figure 1). In phase one, 175 homes were identified in the southern California region as being in the upper 75th percentile or lower 25th percentile according to staffing data reported by NH administrators in 1999 to the State of California (California Office of Statewide Health Planning and Development 2002). Mean total direct hprd was used to determine each home's percentile rank. Thirty homes agreed to participate (15 in each of the extreme quartiles). However, only 17 of the 30 homes remained in the same quartile according to state staffing data reported in the year 2000 (9 lower quartile; 8 upper quartile). In addition, six of the eight homes in the upper quartile in both years (stable homes) reported a decrease in staffing in 2000 (4.0 hours to 3.4 hours) with all six homes clustered at 3.4 direct care hprd. The two remaining homes in the upper quartile were more stable and reported 3.7 and 5.1 direct care hprd in 2000. Furthermore, NAs in these two higher staffed homes also reported significantly lower resident care loads on interview in the year 2001 when compared to homes in the remaining upper quartile, as will be reported later. Thus, homes were initially divided into the following three categories for analytical comparisons: nine homes that reported an average of 2.7 hprd in both 1999 and 2000 (Group 1: lower quartile homes), six homes that reported 3.4 hprd in both 1999 and 2000 (Group 2: upper quartile homes), and two homes that reported an average of 4.9 hprd in both 1999 and 2000 (Group 3: upper-decile homes).
Figure 1.
Flow of Participants through Trial
Because of the potential importance of the upper-decile homes, Phase 2 was initiated to recruit additional homes in the 91st to 100th percentile (upper decile) following the completion of data analyses for Phase 1 homes. Research staff was blind to the staffing percentile ranking for each home during the data collection and analyses for Phase 1 but not in Phase 2 (see Figure 1). In Phase 2, 47 homes in the Southern California region were identified as being in the upper decile according to 2000 state staffing data. These homes also had small (<10 percent) Medicare populations because large Medicare populations can inflate staffing levels for the long-term care portion of the NH. Four homes were recruited that reported staffing levels above 3.8 total hprd in the year 2000 (upper decile) for a predominantly long-term care population.
Thus, a total of 21 homes were studied across the two phases. Residents who were long stay (not covered by Medicare) were eligible for participation, and resident recruitment occurred over two weeks within each home. The number of participants and consent rates are illustrated in Figure 1. Onsite data collection both to assess quality of care and to confirm state staffing reports with NH staff interviews occurred over three consecutive days and were conducted from June 2001 to September 2002. State cost report staffing data were not available for the year 2001.
Staff Interviews: Accuracy of State Staffing Reports
To check the accuracy of year 2000 staffing statistics reported by NH administrators to the state and also to update these statistics, research staff conducted interviews with 118 NAs who worked on the 7 a.m. to 3 p.m. and 3 p.m. to 11 p.m. shifts during onsite data collection in 2001–2002. The NAs were asked “How many residents are you responsible for today?” and “Are you working ‘short’?” Administrators were also asked to report the number of NAs, LVNs, and RNs that were usually scheduled during the time period that onsite data collection was being completed. These data were converted into staffing hours per resident day by assuming that a full-time staff member worked 7.5 hours and dividing staffing hours by the number of occupied beds in the facility. Even though these staffing data were not collected according to the same specific definitions used for the state reporting system, it does represent a more current staffing estimate. Independent checks of time cards to validate staffing statistics were not possible because it would have required consent from each NH staff member in the facility. The onsite staffing reports were not regarded as more or less accurate than the state staffing reports, only more timely. The agreement between the different staffing data sources was considered an important estimate of data accuracy.
Measurement Domains
Sixteen care processes typically implemented by NAs were measured by research staff using standardized direct observation and resident interview protocols during three consecutive 12-hour weekdays in each NH. The care process measures relevant to NA job performance can be divided into four major domains: out of bed/social engagement; feeding assistance; incontinence care; exercise and repositioning. Each of these NA care process measures can be defended as representing “good practice” and should be sensitive to differential NA staffing between homes because most of these care processes are also labor intense to implement.
All participants were observed with at least one of three different observational protocols (described below), but subgroups of participants were selected for interview. Participants with an MDS recall score of two or greater were asked questions about the occurrence of specific care processes (e.g., How often do you receive walking or toileting assistance?) because a recent study showed that residents who meet this interview selection criterion are able to accurately describe the care they receive (Simmons and Schnelle 2001). However, all participants were asked more general questions about the quality of assistance (e.g., Do you have to wait too long?) because there is evidence that residents who are capable of completing an interview can provide stable responses to these types of questions. Eleven care process measures related primarily to licensed nurse staff performance (e.g., pressure ulcer risk assessment) were evaluated based primarily on medical record review, with the exception of two resident interview measures, using standardized protocols.
Out of Bed and Engagement: Observations
To assess participants' time spent in bed and social engagement during the day research staff observed participants for one 12-hour day (7 a.m. to 7 p.m.). The time-sampling protocol involved locating each participant every hour between 7 a.m. and 7 p.m. and observing the resident for up to one minute. Engagement was defined as interaction with either a staff member, a resident, or another person; an organized group activity; or with an object (e.g., television, reading, sewing). These two measures (out-of-bed time and engagement) are related to staffing levels, because assisting residents out of bed is labor intense since it occurs during the morning or evening periods when there are numerous competing activities (e.g., breakfast) and the resident must be dressed or groomed at the same time. There is evidence that NH residents spend excessive times in bed (Schnelle et al. 1998). It was also hypothesized that staff in high-staffed homes would have more time either to interact with or encourage residents to participate in activities during the day. Social interaction with and prompting residents to participate in activities are not necessarily labor intensive but are optional care activities that may not occur if staff are rushed to provide more mandatory physical care (e.g., providing feeding assistance to residents).
Feeding Assistance: Observation and Interview Measures
Seven measures related to the quality of feeding assistance care were measured using direct, continuous (not time-sampled) observations during meals in which one staff member observed six to eight participants. All feeding assistance measures were assessed regardless of dining location (dining room versus room), with the exception of social interaction and verbal prompting during meals. The percent of social interaction or verbal prompts during meals was designed to assess the quality of feeding assistance, and interaction was counted if at least one minute of social interaction or verbal prompting occurred between the resident and the NH staff. Social interaction during meals has been related to increased food intake, and even the most cognitively impaired resident should receive some verbal prompts and social interaction during meals as opposed to physical assistance rendered in silence. The development, rationale, and scoring rules for all feeding assistance care process measures have been described elsewhere (Simmons et al. 2002). Brief descriptions of a few measures are provided here. Two measures were related to determining if a resident who is at risk for weight loss due to either low oral food and fluid intake or physical dependency on staff for eating, received at least a minimal amount of staff assistance during meals. Participants were considered to “pass” the first care process measure if they ate less than 50 percent of their meal but still received more than one minute of staff assistance. The logic of this indicator is that residents with intake below 50 percent are at risk for weight loss, and staff should try to provide assistance to these residents. If a resident ate less than 50 percent and received less than one minute of staff attention, it is not possible to separate poor assistance from other explanations for the poor eating. Participants were considered to pass the second care process measure if they were rated as physically dependent on the MDS and received more than five minutes of assistance. A measure relating to the accuracy of NH staff documentation of residents' oral food and fluid intake during meals and, thus, the ability of staff to identify residents with potentially problematic intake was also assessed. A participant passed this care process measure if he or she was observed by research staff to eat less than 50 percent of their meal and NH staff recorded less than 60 percent. Low intake is associated with weight loss and accurately identifying this problem is a logical prerequisite for prevention. Participants who had an MDS recall score of two or greater were also asked one interview question related to the NH food service, “If you don't like the food served at a particular meal, can you get something else?”
It was hypothesized that feeding assistance would be significantly associated with staffing levels because it is labor intense to provide this daily care process for all residents who need it. Both the simulation predictions conducted for the CMS study and one expert consensus panel predicted that a NA staffing ratio of two to five residents per NA is necessary to provide adequate feeding assistance care (Harrington, Kovner et al. 2000; Schnelle, Simmons, and Cretin 2001).
Incontinence Care: Interview Measures
Incontinent participants, according to the most recent MDS assessment, with MDS recall scores of two or greater were asked how often they received toileting assistance, and all incontinent residents who responded to the interview questions were asked the more general question, “Do you have to wait too long for assistance?”
Exercise and Repositioning: Observation and Interview Measures
Observational data relevant to participants' physical movements were obtained from a wireless monitor worn on the thigh that measures horizontal and vertical orientation every four seconds. Preliminary research showed that repositioning movements in bed were characterized by the monitor recording a minimum 40° move in the horizontal position followed by maintenance of at least a 20° change in the horizontal position and at least two 40° vertical changes when repositioning occurred in a chair. The monitor also enabled the detection of physical activities that involved sustained participant movement for at least six minutes and, thus, could possibly reflect an episode of exercise care. Because exercise (e.g., walking assistance) could not be discriminated from care processes that involved movement for other reasons (e.g., incontinence care), all participant movements that were sustained for at least six minutes were characterized as “activity episodes” possibly related to exercise. The thigh monitor was used because preliminary data indicated that any observational schedule feasible for a human observer to implement with more than three residents would underestimate the frequency of care episodes, such as walking and repositioning, that occur less than every two hours and are relatively brief in duration.
Two movement measures were calculated from thigh monitor data. First, the number of repositioning episodes per hour was calculated for participants who were noted in the medical record as being on a two-hour repositioning program and who could not reposition themselves independently according to a performance test conducted by research staff. In this test, participants who were unable to move from side to side unless they received physical assistance were considered dependent on staff for repositioning. Next, the number of activity episodes per hour was calculated for each of the above participants to determine whether there were differences between high- and low-staffed homes in the provision of care processes that could be interpreted as exercise.
Finally, all participants with MDS recall scores of two or greater and who were in need of walking assistance were asked how many walking assists they received per day. The participants' need for walking assistance was determined during a performance test conducted by research staff in which participants were asked to stand and walk and provided graduated levels of assistance to do so. Participants who were unable to stand and bear weight, even if provided full physical assistance by research staff, were excluded from this analysis. It was hypothesized that higher-staffed homes would be more likely to consistently provide exercise, repositioning, and walking assistance to participants because all of these care processes are labor intensive.
Medical Record Review: Licensed Nurse Measures
Descriptive information for all participants was collected from the medical record and the most recent MDS or the annual assessment for some items. A trained physician or geriatric nurse practitioner conducted medical record reviews to assess care processes related to licensed nurse activities. It was hypothesized that licensed nurses in homes with higher staffing would perform better at assessment of conditions typically managed by nurses, as opposed to primary care providers, than licensed nurses in homes with lower staffing.
Eight of the licensed nurse care process measures used in this study are derived from the RAND Assessing the Care of Vulnerable Elderly (ACOVE) project. The quality indicators in the ACOVE project were operationalized with specific scoring rules and data sources identified for rating each indicator. The methodology used to develop the ACOVE indicators and the evidence that supports their validity has been reported elsewhere (Wenger and Shekelle 2001; Shekelle et al. 2001; Saliba and Schnelle 2002). Eight care processes from the set of ACOVE quality indicators most relevant to licensed nurse performance were identified by a geriatric nurse practitioner and clinical nurse specialist who covered three care areas: pressure ulcer, incontinence assessment, and pain. In addition, three care processes that were not specific ACOVE indicators were identified that evaluated how well nurses either assessed pain or provided medications to residents with chronic pain.
The ACOVE indicators are relatively self-explanatory even though it should be noted that liberal scoring rules were used to determine if a participant's medical record documentation met the pass criteria for each indicator. For example, in regard to incontinence Indicator 5, a medical record was considered to have fulfilled the intent of this indicator if documentation was provided for just two of the three conditions (e.g., skin health, genital system examination, fecal impaction assessment). The measures used to assess how well nurses were detecting and treating pain requires more explanation.
Three interview measures were used to evaluate licensed nurse performance relevant to pain. Research staff attempted to interview all participants with MDS recall scores of two or above with a set of six questions about pain. Two questions were related to communication between the licensed nurse and the resident regarding pain, “Do you tell the nurse about your pain?” and “Does the nurse ask you about pain?” We report data on the latter question and hypothesized that licensed nurses in higher-staffed homes would ask participants about pain more frequently than nurses in lower-staffed homes. Directly taking a proactive approach and asking residents about pain was considered better care than the more passive approach of simply reacting when a resident spontaneously complains of pain.
The four remaining pain questions were used to identify participants with chronic pain symptoms. Participants were asked: “Do you have pain every day?”; “Does pain ever keep you from doing things you enjoy (like social activities, walking)?”; “Does pain ever keep you from sleeping at night?”; and “Do you have pain right now?” Participants were judged as endorsing chronic pain if they responded “yes” to the question, “Do you have pain everyday?” or if they responded “yes” to all three remaining pain questions. To assess how well licensed nurses were detecting pain we determined the percent of participants who were judged as having chronic pain according to research staff interview who also had licensed nurse documentation of pain on the most recent MDS assessment. We also assessed licensed nurse performance relevant to management of chronic pain. First, we identified a subgroup of participants who had chronic pain according to research staff interviews. Then we determined the percent of this subgroup of participants who were offered pain medication by the licensed nurse at least 50 percent of the days in the previous month. We believed that licensed nurses in higher staffed homes would both detect chronic pain symptoms and offer as needed pain medication more frequently than licensed nurses in lower staffed homes.
Reliability and Stability
Interrater reliability for time in bed and engagement observational measures was statistically significant for both measures but high only for the in-bed measures (measures 1 and 2, Table 3; kappa values .65 and .29; p<.001). A subset of 272 participants was observed for a second day on these measures to evaluate stability. The Pearson correlation was .79 for in-bed and .47 for engagement (p<.05). Interrater reliability for all observational-based feeding assistance care process measures shown in Table 3 (measures 3 to 10) ranged from .92 to 1.0; n=55 to 199; p<.001. Mealtime observations were repeated on a second day for all participants and correlations between the two days were significant on all variables (range .22 to .75; p<.05) with social interaction and verbal prompting measures showing the lowest but still significant correlations. The low correlation for this social interaction variable was due to the relatively low frequency that this behavior was observed. Correlations for all the other nutritional measures were above .60. Correlation between a resident's reported having received toileting assistance on two separate days (measure 11, Table 3) was .62; p<.01. The interrater agreement for the interpretation of thigh monitor data necessary to calculate exercise care process measures (measures 13, 14, 15) produced kappa statistics of .61 for repositioning movements, .82 for activity episodes while in a chair, and .75 for activity episodes while in bed. The correlation of a participant's report of walking assistance (measure 16) between two days was calculated for 38 residents (day 1 number of assists reported versus day 2 number of assists reported; r=.35, p<.05).
Table 3.
Observation and Interview Measurement Domains
| (1) | (2) | (3) | ||
|---|---|---|---|---|
| Measurement Domains | Low Homes <25th Percentile | High Homes 75–90th Percentile | Highest Homes 91st+Percentile | Significant Comparisons |
| Out of Bed/Engagement | N=227 | N=205 | N=125 | |
| 1. Percent observations of residents in bed 7:00 a.m. to 7:00 p.m. | 41 | 50 | 26 | 1 and 2 vs. 3** |
| 2. Percent observations of residents engaged with nursing home staff, other residents, another person, or an organized group activity, or with an object (e.g., television, reading, sewing) | 47 | 44 | 52 | 1 and 2 vs. 3* |
| Nutrition: Feeding Assistance | N=407 meals | N=350 meals | N=252 meals | |
| 3. Percent of resident meals in dining room | 25 | 39 | 80 | 1 and 2 vs. 3** |
| 4. Average duration of feeding assistance to residents in minutes | 2.5 (5.9) | 4.11 (8.6) | 7.0 (11.7) | 1 and 2 vs. 3** |
| 5. Average resident tray access time in minutes | 26.9 (3.9) | 32.5 (5.3) | 38.2 (14.8) | 1 and 2 vs. 3** |
| Providing assistance to residents with low intake: | ||||
| 6. Percent of residents who eat < 50% and are provided≥1 minute of assistance | 19 (n=106) | 31 (n=96) | 46 (n=95) | 1 and 2 vs. 3** |
| Providing assistance to physically dependent residents: | ||||
| 7. Percent of residents feeding dependent, MDS>1, and who receive≥5 minutes assistance | 66 (n=83) | 48 (n=134) | 80 (n=72) | 1 and 2 vs. 3** |
| Accuracy of food intake documentation: | ||||
| 8. Percent of residents who ate less than 50%; NA recorded≤60% | 24 (n=106) | 50 (n=96) | 52 (n=95) | 1 and 2 vs. 3* |
| 9. Percent of mealtime observations with social interaction and verbal prompting | 18 (n=103) | 28 (n=137) | 25 (n=199) | – |
| 10. Percent residents responding yes to “Do you have food choice during meals?” | 84 (n=99) | 86 (n=104) | 98 (n=55) | 1 and 2 vs. 3* |
| Incontinence | ||||
| 11. Number of toileting assists received; MDS Recall Score≥2 | 1.76 (1.18) | 1.8 (1.25) | 2.8 (1.12) | 1 and 2 vs. 3** |
| (n=48) | (n=64) | (n=31) | ||
| 12. Percent residents responding yes to “Do you have to wait too long for assistance?” All Recall Scores | 49 (n=90) | 39 (n=89) | 31 (n=58) | 1 and 2 vs. 3* |
| Exercise Activities | N=42 | N=46 | N=30 | |
| 13. Number of exercise activities per hour (Day)—Thigh monitor (can't reposition or walk independently) | .20 (.15) | .18 (.13) | .27 (.20) | 1 and 2 vs. 3* |
| 14. Number of repositioning movements per hour (Night)—Thigh monitor (can't reposition independently) | .25 (.17) | .17 (.14) | .23 (.14) | |
| 15. Number of repositioning movements per hour (Day)—Thigh monitor (can't reposition independently) | .26 (.40) | .20 (.14) | .36 (.28) | 1 and 2 vs. 3** |
| 16. Number of walking assists received MDS Recall Score≥2 and can bear weight | .51 (.72) | .76 (.68) | .69 (1.1) | – |
P≤.05;
P≤.001.
Results
Characteristics of Participants in Key Comparison Groups
Table 1 shows the demographic characteristics of the participants in each group of homes. There were significant differences between participants in all three groups (Table 1). In particular, participants in the upper-decile homes were significantly more likely to be female, older, private pay, and Caucasian when compared to participants in all the other homes; while participants in the lower quartile homes were significantly more likely to be minority and MediCal. In terms of participant acuity, participants in the lower quartile homes (Group 1) tended to be more independent for transfer and feeding assistance and had better cognitive functioning (MDS recall scores) when compared to participants in both the 75th to 90th percentile (Group 2) and upper-decile homes (Group 3). There was no difference on five MDS based acuity measures (recall, transfer and eating dependency, incontinence, pressure ulcer RAP triggered) when comparisons were made between residents in the highest-staffed homes (upper decile) and those in the two lower-staffed homes (combined Groups 1 and 2 versus Group 3).
Table 1.
Facility and Demographic Characteristics of Participants in Sample Nursing Homes
| 1 | 2 | 3 | ||
|---|---|---|---|---|
| Low Homes <25th Percentile | High Homes 75–90th Percentile | Highest Homes 91st+Percentile | Significant Comparisons | |
| Demographic Measures | N=228 | N=204 | N=115 | |
| Number of Beds | 118 | 158 | 77 | 12 v 3* |
| Age—Mean Years (SD) | 79 (12) | 82 (10) | 91 (6) | 1 and 2 vs. 3** |
| 1 vs. 2** | ||||
| 2 vs. 3** | ||||
| 1 vs. 3** | ||||
| Length of Residency—Mean Months (SD) | 28 (32.6) | 24.9 (27.7) | 26.9 (24.3) | – |
| Percent Female | 66 | 75 | 89 | 1 and 2 vs. 3** |
| 1 vs. 3** | ||||
| 2 vs. 3* | ||||
| Percent Caucasian | 49 | 72 | 97 | 1 and 2 vs. 3** |
| 1 vs. 2** | ||||
| 2 vs. 3** | ||||
| 1 vs. 3** | ||||
| Percent MediCal | 79 | 66 | 37 | 1 and 2 vs. 3** |
| 2 vs. 3** | ||||
| 1 vs. 3** | ||||
| 1 vs. 2* | ||||
| MDS Transfer Level—Mean (SD)*** | 2.3 (1.4) | 3.02 (1.0) | 2.77 (1.2) | 1 vs. 2** |
| (n=217) | (n=194) | (n=102) | 1 vs. 3* | |
| MDS Recall Score—Mean (SD)*** | 2.35 (1.5) | 2.24 (1.7) | 1.95 (1.6) | 1 vs. 3* |
| (n=218) | (n=200) | (n=102) | ||
| MDS Feeding Assistance Level—Mean (SD)*** | 1.16 (1.5) | 1.62 (1.7) | 1.28 (1.4) | 1 vs. 2* |
| Mean (SD)*** | (n=220) | (n=203) | (n=97) | |
| Percent Urinary Incontinent | 74 | 86 | 84 | |
| Percent Pressure Ulcer RAP Triggered | 81 | 95 | 88 | 1 vs. 2* |
P≤.05;
P≤.001.
All MDS scale scores vary from 0 (independent) to 4 (completely dependent)
To address generalizability issues, efforts were made to determine if differences existed between 9 highest-staffed and 45 lower-staffed homes that declined participation in this project and the 6 highest-staffed and 15 lower-staffed homes that participated. The homes that declined participation and the homes that participated were compared on MDS-derived measures of prevalence of weight loss, physical restraint use, and residents' need for assistance with transfer, eating, and toileting characteristics, all of which are available from a new public reporting system in California (http://www.calnhs.org). In addition, data were available describing homes' profit status, total nursing staff hours, nursing staff turnover, total federal deficiencies cited for 2001–2002, and expenditures for direct resident care per resident day. The only difference between participating lower-staffed homes and nonparticipating lower-staffed homes was on the expenditures per resident per day ($59 versus $68, respectively; t=2.115, p=.04). The only difference between participating and nonparticipating highest-staffed homes was on for-profit status of the home (33 percent versus 100 percent, χ2=8.182, p=.004). These results should be cautiously interpreted but in general suggest that the homes participating in this project comprise a relatively typical sample.
Sample Characteristics: Staffing Data
Table 2 illustrates the staffing data for the three groups of NHs. The first eight rows alternatively illustrate state staffing statistics for the year 2000 and onsite staffing data reported by administrators. There were large differences between high-decile homes and all remaining homes on all staffing variables except RN hours according to 2000 state staffing data. These differences are most dramatic for total staffing hours and aide staffing hours. In regard to total hours, high decile homes reported an average of 4.88 hours compared to lower quartile and 75th to 90th percentile homes that reported 2.7 and 3.4 hrpd, respectively. There were also significant but less dramatic differences between homes in the lower quartile and the 75th to 90th percentile on most staffing variables. However, interview data collected in 2001–2002 while the research team was onsite suggested that there were no longer differences between lower quartile homes and those in the 75th to 90th percentile on any staffing variable. Lower-quartile home administrators reported an increase in total staffing from 2.7 in 2000 to 3.2 in 2001–2002 and the 75th to 90th percentile homes reported a staffing decrease from 3.4 to 3.0. Administrator reports of staffing and NA reports of workload continued to show a significant difference for Group 3 (upper decile) homes compared to the remaining homes. Administrators reported a total of 4.5 hrpd in 2001–2002 in the upper-decile homes. Both administrators and NAs in the upper-decile homes reported a ratio of residents to NAs on the 7 a.m. to 3 p.m. and 3 p.m. to 11 p.m. shifts combined that were very close (7.1 to 7.6 residents to NAs, respectively). These reports were significantly different from the NA workload reports in other homes (e.g., nine to 10 residents per aide, see Table 2, rows 9, 10). These data suggest that there are two distinct groups of homes based on staffing statistics. The difference in staffing between Group 1 and Group 2 homes is not only small and unstable, but also well below those minimums thought to indicate better care according to both expert panels and recent CMS studies. Alternatively, the homes in the upper decile were not only dramatically higher on staffing measures when compared to all other homes but also staffed at those levels thought to be necessary to provide good care (Harrington, Kovner et al. 2000; Schnelle, Simmons, Cretin 2001; Kramer and Fish 2001). For these reasons, the primary comparisons on all care process measures were conducted between homes in the upper decile (Group 3) and the remaining sample (Groups 1+2 combined).
Table 2.
Staffing Characteristics of Sample Nursing Homes
| 1 | 2 | 3 | ||
|---|---|---|---|---|
| Staffing Measures | Low Homes <25th Percentile Mean (SD) Range | High Homes 75–90th Percentile Mean (SD) Range | Highest Homes 90th+Percentile Mean (SD) Range | Significant Comparisons |
| 2000 State Registered Nurse Staffing Data—Hours per resident day | .29 (+/−.006) | .48 (+/−.13) | .57 (+/−.42) | 1 vs. 2* |
| 2001–2002 Registered Nurse Staffing Data according to Administrator Interview—Hours per resident day | .34 (+/−.08) | .38 (+/−.14) | .70 (+/−.55) | 1 and 2 vs. 3* |
| 1 vs. 3* | ||||
| 2000 State Licensed Vocational Nurse Staffing Data—Hours per resident day | .51 (+/−.11) | .58 (+/−.004) | .90 (+/−.18) | 1 and 2 vs. 3** |
| 1 vs. 3** | ||||
| 2 vs. 3* | ||||
| 2001–2002 Licensed Vocational Nurse Staffing Data according to Administrator Interview—Hours per resident day | .62 (+/−.12) | .49 (+/−.19) | .88 (+/−.12) | 1 and 2 vs. 3** |
| 1 vs. 3** | ||||
| 2 vs. 3** | ||||
| 2000 State Aide Staffing Data—Hours per resident day | 1.95 (+/−.10) | 2.32 (+/−.13) | 3.43 (+/−.74) | 1 and 2 vs. 3** |
| 1 vs. 2** | ||||
| 1 vs. 3** | ||||
| 2 vs. 3* | ||||
| 2001–2002 Aide Staffing Data according to Administrator Interview—Hours per resident day | 2.3 (+/−.24) | 2.1 (+/−.16) | 2.99 (+/−.98) | 1 and 2 vs. 3* |
| 1 vs. 3* | ||||
| 2 vs. 3* | ||||
| 2000 State Total Staffing Data (licensed and nonlicensed nursing staff)—Hours per resident day | 2.73 (+/−.009) | 3.40 (+/−.000) | 4.88 (+/−1.13) | 1 and 2 vs. 3** |
| 1 vs. 2** | ||||
| 1 vs.3** | ||||
| 2 vs. 3* | ||||
| 2001–2002 Total Staffing Data according to Administrator Interview—Hours per resident day | 3.26 (+/−.29) | 3.0 (+/−.35) | 4.57 (+/−1.49) | 1 and 2 vs. 3* |
| 1 vs. 3* | ||||
| 2 vs. 3* | ||||
| Nurse Aide Interview Data: How many people are you working with? (7-3 shift and 3-11 shift combined)—Mean residents per aide 2001–2002 | 9.4 (2.5) | 10.4 (2.2) | 7.6 (1.5) | 1 and 2 vs. 3** |
| n=48 | n=27 | n=41 | 1 vs. 3** | |
| 2 vs. 3** | ||||
| Administrator Interview Data 2001–2002: How many aides are usually scheduled from 7a.m. to 11p.m.?—Mean residents per aide | 9.3 (+/−1/6) | 9.7(+/−.73) | 7.0(+/−1.8) | 1 and 2 vs. 3** |
| 1 vs. 3* | ||||
| 2 vs. 3* |
P≤.05;
P≤.001.
NA Care Process Measures: Do Homes That Report the Highest NA Staffing (Group 3 Upper Decile) Provide Different Care Than the Remainder of the Homes (Groups 1 and 2 Combined)
Table 3 illustrates that upper-decile homes (Group 3) were significantly different in the same direction on 13 of 16 different care process measures; and, in eight cases significance levels exceeded p<.001. The probability that 13 out of 16 comparisons would be significant at the .05 level by chance is less than .00001. The pattern of significant differences was consistent across all care areas listed in Table 1, but the care process differences were most compelling for feeding assistance and least compelling for exercise and repositioning. In general, participants in the upper-decile homes spent more time out of bed during the day; were engaged more frequently; received better feeding and toileting assistance; were repositioned more frequently; and showed more physical movement patterns during the day that could reflect exercise. However, even participants in these highest-staffed facilities did not receive repositioning at the rate of once every two hours during the day or night and only received potential exercise activities at the rate of approximately one episode every four hours. In addition, there were no differences between the groups of homes in repositioning frequency at night; walking assistance frequency during the day as reported by the participants; or the amount of social interaction observed between residents and staff during meals.
Social interaction during meals could only be measured in the dining room, and participants in the upper-decile homes were observed significantly more often in the dining room than those in the remaining homes. If one assumes that there are very low or zero levels of social interaction between residents and staff if residents eat in their rooms, which is a reasonable assumption, then there would be significant overall differences in the amount of social interaction that participants in upper-decile homes received during meals as compared to participants in all remaining homes.
There were no differences on five MDS-based acuity measures that could explain why more residents ate in their rooms more often in the lower-staffed homes (Groups 1 and 2 combined versus those in the highest-staffed NHs—see Table 1). The significant higher age of residents in the highest-staffed home would seem predictive of these residents spending more time in bed as opposed to less time as was observed. However, none of the demographic characteristics including age were correlated with in-bed or feeding assistance measures across all homes. A multiple regression analysis using staffing as a categorical variable (upper decile versus all others) and MDS acuity scores that were correlated with in-bed time (transfer and feeding assistance, recall scores, and prevalence of UI and pressure ulcer RAP triggered) revealed that staffing remained the only significant predictor of in-bed time (standardized beta=−.28, standard error=8.8, p<.003).
Licensed Nurse Performance Measures
Table 4 presents the licensed nurse comparisons between the three groups of homes. Unlike the NA care process comparisons, there were no licensed nurse performance measures that favored the upper-decile homes. In fact, licensed nurses in the lower-staffed homes performed better on 2 of the 11 indicators when compared to the upper-decile homes (Group 3). This difference was primarily due to Group 1 homes' nurses scoring significantly better on two pressure ulcer indicators. In addition to the low pass rates for higher-staffed homes on licensed nurse measures, there was also relatively poor performance on some indicators across all homes. Specifically, no group of homes performed well on the indicators assessing licensed nurse management of chronic pain by offering “as needed” pain medication on at least 50 percent of the days in the prior month to those residents with chronic pain symptoms. Less than 10 percent of participants who had chronic pain symptoms and who also had a physician's order for pain medication “as needed” were offered the pain medication on at least 50 percent of the days in the prior month across all homes. Furthermore, licensed nurses failed to identify many residents with chronic pain because less than 50 percent of participants who had chronic pain also had documentation of pain on their most recent MDS assessment. The kappa statistic agreement for residents with chronic pain on two different interviews was .65 (p<.01), indicating high stability. Finally, licensed nurses in all homes also performed poorly on several of the incontinence indicators. Most notably, no incontinent participants had documentation of a three-to-five day toileting assistance trial, which is the most valid method of determining if a resident should receive a scheduled toileting program.
Table 4.
Measures of Licensed Nurse Care Processes
| 1 | 2 | 3 | ||
|---|---|---|---|---|
| Licensed Nurse Care Process Indicators | Low Homes <25th Percentile % (n/total n) | High Homes 75–90th Percentile % (n/total n) | Highest Homes 91st+Percentile % (n/total n) | Significant Comparisons |
| ACOVE Pressure Ulcer Indicators: Medical Record Data | ||||
| 1. Percent of participants admitted with inability or limited ability to reposition him- or herself who have a pressure ulcer risk assessment on admission. | 92 (84/91) | 32 (24/74) | 46 (27/59) | 1 and 2 vs. 3* |
| 2. Percent of participants identified as “at risk” (e.g., Minimum Data Set [MDS] assessment indicates Pressure Ulcer Resident Assessment Protocol initiated) for pressure ulcer development who have documentation of all three: scheduled repositioning every two hours, pressure reduction, and nutritional status assessment for pressure ulcer prevention. | 78 (104/133) | 32 (34/106) | 57 (33/58) | 1 and 2 vs. 3* |
| 3. Percent of participants with a pressure ulcer present or history of a pressure ulcer within the previous 12 months who have four characteristics of the wound documented (e.g., location, stage, size, and presence or absence of necrotic tissue) | 38 (20/53) | 36 (11/31) | 25 (4/16) | – |
| ACOVE Incontinence Indicators: Medical Record Data | ||||
| 4. Percent of participants with assessment of presence or absence of urinary incontinence on admission | 100 (119/119) | 92 (72/78) | 97 (68/70) | |
| 5. Percent of incontinent participants with at least two of three of the following assessed: fecal impaction, skin examination, genital system examination | 35 (13/37) | 13 (3/24) | 20 (8/41) | |
| 6. Percent of incontinent participants with a targeted history that documents at least two or more of the following: mental status, voiding characteristics, ability to get to the toilet, prior incontinence treatment, and importance of incontinence to resident. | 100 (37/37) | 78 (18/23) | 88 (35/40) | |
| 7. Percent of incontinent participants who have documented an evaluation of a 3–5 day toileting assistance trial | 0 (0/37) | 0 (0/23) | 2% (1/42) | – |
| ACOVE Pain Indicator: Medical Record Data | ||||
| 8. Percent of participants noted to have pain on the MDS assessment who have a pain assessment using a standard scale within two weeks of admission | 85 (23/27) | 78 (29/37) | 92 (11/12) | – |
| Pain Measures: Medical Record Data | ||||
| 9. Percent of participants who have chronic pain*** according to interview by research staff with documentation on the MDS assessment of moderate or excruciating pain less than daily or mild, moderate, or excruciating pain daily. | 33 (22/67) | 43 (34/79) | 22 (8/37) | |
| 10. Percent of participants with chronic pain according to interview by research staff who are offered ordered as needed pain medications on at least 50% of the days in the previous month | 8 (3/39) | 3 (1/35) | 6 (1/18) | – |
| Pain Measures: Participant Interview Data | ||||
| 11. Percent of participants with MDS recall score≥2 responding yes to “Does the nurse ask you about pain?” | 47 (66/140) | 45 (53/118) | 41 (22/54) | – |
P≤.05;
P≤.001;
Participants were judged as endorsing chronic pain if they responded yes to the question “Do you have pain every day?”or if they responded yes to three or more of the following interview questions about pain: “Do you have pain every day?”, “Does pain ever keep you from doing things you enjoy (like social activities, walking, going to the dining room for meals, knitting, bingo, going outside)?”, “Does pain ever keep you from sleeping at night?”, “Do you have pain right now?”.
Discussion
Nursing home self-reported staffing statistics do reflect differences in quality between homes that report the highest staffing level (upper decile) and all remaining homes. There were few differences between homes that report staffing levels below the 90th percentile and the staffing levels in these homes were unstable across the different staffing measures. There appears to be a two-tiered staffing system with only the homes reporting the highest level of staffing showing both stability and significantly better care on most measures.
The most dramatic differences between the homes were reported for NA hours and the most dramatic quality improvement occurred for homes that reported a total staffing hrpd average from 4.8 (state data) to 4.5 (onsite interview data). There was also a significant improvement in these upper-decile homes for multiple care processes delivered by NAs even though residents in the upper-decile homes needed as much care according to multiple functional measures as residents in the lower-staffed homes.
There were smaller differences between homes in reported licensed nurse hours and particularly RN hours and there were also fewer differences between homes on licensed nurse performance measures. The differences that did exist favored the lower-staffed homes for two pressure ulcer assessment indicators derived from medical record data. In contrast, observation and resident interview measures related to pressure ulcer care actually received by residents (e.g., toileting assistance, repositioning care) favored the upper-decile homes. This finding highlights an important discrepancy between quality conclusions about NH care process implementation derived from different data sources (medical record versus observation and resident interview).
Despite this discrepancy, it is still surprising that the medical record documentation provided by licensed nurses in higher-staffed facilities was not better since other studies have reported a relationship between licensed nurses' hours and some quality measures (Kramer and Fish 2001). There are two potential explanations for this finding. First, it is possible that none of the homes in this study had adequate licensed nurses, particularly RNs, to improve care quality. Furthermore, RN hours failed to reach the minimum level recommended by a recent CMS study (.75 hours) in all homes, and RN hours were much less in all homes than that recommended by an expert panel (1.15 hours) (Harrington, Kovner et al. 2000). Second, licensed nurses in all facilities simply may be unaware of some care processes that define good quality (e.g., no homes documented a trial of toileting assistance for incontinent residents and all homes did poorly on all pain-related measures). This possibility reinforces arguments that licensed nurses who practice in NHs should receive more specialized training focused on the NH population.
It is also important to note that some care processes were poorly implemented in even the highest-staffed facilities, despite the fact that these facilities had sufficient numbers of NAs to potentially provide 100 percent of care to all residents. One plausible explanation for this finding is that all homes lacked management mechanisms necessary to assure that care was provided on a daily basis, in particular, for care processes that are difficult to measure and manage. For example, the fewest differences occurred between homes on care processes related to repositioning and walking exercise, both of which are difficult to measure when compared to more visible types of care (e.g., resident out of bed). In addition, even though the highest-staffed facilities provided better feeding assistance than other homes, there were still problems that could be traced to measurement issues. For example, even staff in the highest-staffed facilities did not accurately record that 48 percent of the residents were eating less than 50 percent of the food offered and that 54 percent of these low-intake residents were provided less than one minute of feeding assistance during meals. Both of these problems in higher-staffed homes could reflect the absence of a quality assessment technology to accurately measure and monitor these care processes.
We should also note that the differences in the care for the highest-staffing homes (Group 3, upper decile) and all lower-staffed homes were significantly greater than the differences in quality measured for homes that differed on MDS clinical quality indicators. This finding, as reported in other studies, suggests that staffing data may be the best information to give consumers (Bates-Jensen et al. 2003; Simmons et al. 2003; Schnelle, Cadogan et al. 2003; Cadogan et al. 2003; Schnelle et al. 2004).
The conclusions are limited to the relatively small regional sample and our inability to check staffing accuracy with time card records even though time card accuracy checks can also be problematic (Hurd, White, and Feuerberg 2001). Fortunately, the reports by aides of their workloads appears to be a measure that is both associated with other workload reports and discriminative of care quality. This fact suggests that consumers might want to monitor the adequacy of staffing in NHs by asking aides how many people they are working with.
It is also possible that NH characteristics correlated with staffing may have mediated some of the effects reported in this study. For example, higher wages and benefits and lower staff turnover have been linked to better quality and we did not measure these variables. Future studies should expand the number of NH homes (particularly high-staffed homes) and variables studied in an effort to more comprehensively delineate the effects of staffing on quality. The low number of high-staffed homes in this study prevented statistical controls for potentially important facility variables that differentiated these homes, such as size and proportion of Medicaid residents. In addition, we did not measure all resident acuity variables that may have explained why residents in low-staffed homes spent so much time in bed. Direct measures of a resident's sickness severity are particularly important for this purpose.
The standardized measurement technology described in this paper represents a major strength of this study. The measurement protocols are clearly defined, can be replicated, and meet scientific measurement criteria related to reliability and stability. Even though one can argue about the importance of some of the measures for assessing quality, the specificity of the measures allows for this argument to be evidence-based.
Despite the limitations of this study, an excellent case can be made that the highest-staffed homes provided better care. Furthermore, NA staffing levels reported by only the highest-staffed homes exceeded those levels that were identified in two recent CMS reports as associated with higher care quality. This finding provides some verification that NA staffing above 2.8 hours per resident per day is associated with better quality.
Footnotes
Supported by a grant from the California HealthCare Foundation. The views expressed in this paper are those of the authors and may not reflect those of the Foundation. The California HealthCare Foundation, based in Oakland, California, is a nonprofit philanthropic organization whose mission is to expand access to affordable, quality health care for underserved individuals and communities, and to promote fundamental improvements in the health status of the people of California. This research was also supported by grant AG10415 from the National Institute on Aging, UCLA Claude D. Pepper Older Americans Independence Center.
References
- Aaronson W E, Zinn J S, Rosko M D. “Do For-Profit and Not-For-Profit Nursing Facilities Behave Differently?”. Gerontologist. 1994;34(6):775–86. doi: 10.1093/geront/34.6.775. [DOI] [PubMed] [Google Scholar]
- Bates-Jensen B M, Cadogan M, Osterweil D, Levy-Storms L, Jorge J, Al-Samarrai N R, Grbic V, Schnelle J R. “The Minimum Data Set Pressure Ulcer Indicator:Does It Reflect Differences in Care Processes Related to Pressure Ulcer Prevention and Treatment in Nursing Homes?”. Journal of the American Geriatric Society. 2003;51(9):1203–12. doi: 10.1046/j.1532-5415.2003.51403.x. [DOI] [PubMed] [Google Scholar]
- Bliesmer M M, Smayling M, Kane R, Shannon I. “The Relationship between Nursing Staffing Levels and Nursing Home Outcomes”. Journal of Aging and Health. 1998;10(3):351–71. doi: 10.1177/089826439801000305. [DOI] [PubMed] [Google Scholar]
- Cadogan M P, Schnelle J F, Yamamoto-Mitani N, Cabrera G, Simmons S F. “A Minimum Data Set Prevalence of Pain Quality Indicator: Is It Accurate and Does It Reflect Differences in Care Processes?”. Journal of Gerontology: Medical Science. doi: 10.1093/gerona/59.3.m281. (Accepted) [DOI] [PubMed] [Google Scholar]
- California Office of Statewide Health Planning and Development. Annual Long Term Care Facility, Cost Report Files, 1994–2000. Sacramento: California Office of Statewide Health Planning and Development; 2002. “Composite file prepared for this study”. [Google Scholar]
- Cherry R L. “Agents of Nursing Home Quality of Care: Ombudsmen and Staff Ratios Revisited”. Gerontologist. 1991;21(2):302–8. doi: 10.1093/geront/31.3.302. [DOI] [PubMed] [Google Scholar]
- Harrington C, Kovner C, Mezey M, Kayser-Jones J, Burger S, Mohler M, Burke R, Zimmerman D. “Experts Recommend Minimum Nurse Staffing Standards for Nursing Facilities in the United States”. Gerontologist. 2000;40(1):5–16. doi: 10.1093/geront/40.1.5. [DOI] [PubMed] [Google Scholar]
- Harrington C, Zimmerman D, Karon S L, Robinson J, Beutel P. “Nursing Home Staffing and Its Relationship to Deficiencies”. Journal of Gerontology: Social Sciences. 2000;55B(5):S278–87. doi: 10.1093/geronb/55.5.s278. [DOI] [PubMed] [Google Scholar]
- Hurd D, White A, Feuerberg M. Appropriateness of Minimum Nurse Staffing Ratios in Nursing Homes. Washington, DC: U.S. Department of Health and Human Services, Health Care Financing Administration; 2001. “Development of Improved Nurse Staffing Data Collection and Audit Tool”; pp. 1–26. Report to Congress, Phase 2 final, chap. 9. [Google Scholar]
- Kayser-Jones J. “Mealtime in Nursing Homes”. Journal of Gerontological Nursing. 1996;22(3):26–31. doi: 10.3928/0098-9134-19960301-09. [DOI] [PubMed] [Google Scholar]
- Kayser-Jones J. “Inadequate Staffing at Mealtime: Implications for Nursing and Health Policy”. Journal of Gerontological Nursing. 1996;23(8):14–21. doi: 10.3928/0098-9134-19970801-07. [DOI] [PubMed] [Google Scholar]
- Kayser-Jones J, Schell E. “The Effect of Staffing on the Quality of Care at Mealtime”. Nursing Outlook. 1997;45(2):64–71. doi: 10.1016/s0029-6554(97)90081-6. [DOI] [PubMed] [Google Scholar]
- Kramer A M, Fish R. Appropriateness of Minimum Nurse Staffing Ratios in Nursing Homes. Washington, DC: U.S. Department of Health and Human Services, Health Care Financing Administration; 2001. “The Relationship between Nurse Staffing Levels and the Quality of Nursing Home Care”; pp. 1–26. Report to Congress, Phase 2 final, chap. 2. [Google Scholar]
- Linn M, Gurel L, Linn BA. “Patient Outcome as a Measure of Quality of Nursing Home Care”. American Journal of Public Health. 1977;67(4):337–44. doi: 10.2105/ajph.67.4.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munroe D J. “The Influence of Registered Nursing Staffing on the Quality of Nursing Home Care”. Research in Nursing and Health. 1990;13(4):263–70. doi: 10.1002/nur.4770130409. [DOI] [PubMed] [Google Scholar]
- Nyman J A. “Improving the Quality of Nursing Home Outcomes: Are Adequacy-or Incentive-Oriented Policies More Effective?”. Medical Care. 1988;26(12):1158–71. doi: 10.1097/00005650-198812000-00006. [DOI] [PubMed] [Google Scholar]
- Saliba D, Schnelle J F. “Indicators of the Quality of Nursing Home Residential Care”. Journal of the American Geriatric Society. 2002;50(8):1421–30. doi: 10.1046/j.1532-5415.2002.50366.x. [DOI] [PubMed] [Google Scholar]
- Schnelle J F, Bates-Jensen B M, Levy-Storms L, Grbic V, Yoshii J, Cadogan M P, Simmons S F. “The Minimum Data Set Prevalence of Restraint Quality Indicator: Does It Reflect Differences in Care?”. Gerontologist. 2004;44(2) doi: 10.1093/geront/44.2.245. [DOI] [PubMed] [Google Scholar]
- Schnelle J F, Cadogan M P, Yoshii J, Al-Samarrai N R, Osterweil D, Bates-Jensen B M, Simmons SF. “The Minimum Data Set Urinary Incontinence Quality Indicators: Do They Reflect Differences in Care Processes Related to Incontinence?”. Medical Care. 2003;41(8):909–22. doi: 10.1097/00005650-200308000-00005. [DOI] [PubMed] [Google Scholar]
- Schnelle J F, Cruise P A, Alessi C A, Al-Samarrai N R, Ouslander J G. “Sleep Hygiene in Physically Dependent Nursing Home Residents: Behavioral and Environmental Intervention Implications”. Sleep. 1998;21(5):515–23. [PubMed] [Google Scholar]
- Schnelle J F, Simmons S F, Cretin S. In Appropriateness of Minimum Nurse Staffing Ratios in Nursing Homes. Washington, DC: U.S. Department of Health and Human Services, Health Care Financing Administration; 2001. “Minimum Nurse Aide Staffing Required to Implement Best Practice Care in Nursing Facilities”; pp. 1–40. Report to Congress, Phase 2 final, chap. 3. [Google Scholar]
- Simmons S F, Babineau S, Garcia E, Schnelle J F. “Quality Assessment in Nursing Homes by Systematic Direct Observation: Feeding Assistance”. Journal of Gerontology: Medical Sciences. 2002;57A(10):M665–71. doi: 10.1093/gerona/57.10.m665. [DOI] [PubMed] [Google Scholar]
- Simmons S F, Garcia E T, Cadogan M P, Al-Samarrai N R, Levy-Storm L F, Osterweil D, Schnelle J F. “The Minimum Data Set Weight Loss Quality Indicator: Does It Reflect Differences in Care Processes Related to Weight Loss”. Journal of the American Geriatric Society. 2003;51(10):1410–18. doi: 10.1046/j.1532-5415.2003.51459.x. [DOI] [PubMed] [Google Scholar]
- Simmons S F, Schnelle J F. “The Identification of Residents Capable of Accurately Describing Daily Care: Implications for Evaluating Nursing Home Care Quality”. Gerontologist. 2001;41(5):605–11. doi: 10.1093/geront/41.5.605. [DOI] [PubMed] [Google Scholar]
- Shekelle G, MacLean C H, Morton S C, Wenger N. “Assessing Care of Vulnerable Elders: Methods for Developing Quality Indicators”. Annals of Internal Medicine. 2001;135(8, part 2):647–52. doi: 10.7326/0003-4819-135-8_part_2-200110161-00003. [DOI] [PubMed] [Google Scholar]
- Spector W D, Takada H A. “Characteristics of Nursing Facilities That Affect Resident Outcomes”. Journal of Aging and Health. 1991;3(4):427–54. doi: 10.1177/089826439100300401. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services, Health Care Financing Administration (USHCFA) Report to Congress: Appropriateness of Minimum Nurse Staffing Ratios in Nursing Homes. Washington, DC: Health Care Financing Administration; 2000a. Executive Summary. [Google Scholar]
- U.S. Department of Health and Human Services, Health Care Financing Administration (USHCFA) Appropriateness of Minimum Nurse Staffing Ratios in Nursing Facilities. 1,2, and 3. Washington, DC: Health Care Financing Administration; 2000b. Report to Congress. [Google Scholar]
- U.S. Department of Health and Human Services, Health Care Financing Administration (USHCFA) Appropriateness of Minimum Nurse Staffing Ratios in Nursing Homes. Washington, DC: Health Care Financing Administration; 2001. Report to Congress. Executive Summary. [Google Scholar]
- Wenger N S, Shekelle P G. “Assessing Care of Vulnerable Elders: ACOVE Project Overview”. Annals of Internal Medicine. 2001;135(8, part 2):642–6. doi: 10.7326/0003-4819-135-8_part_2-200110161-00002. [DOI] [PubMed] [Google Scholar]
- Wunderlich G S, Kohler P O, editors. Improving the Quality of Long-Term Care. Washington, DC: National Academy of Sciences, National Academy Press; 2001. Report by the Committee on Improving the Quality in Long-Term Care, Division of Health Care Services, Institute of Medicine. [PubMed] [Google Scholar]
- Wunderlich G, Sloan F, Davis C, editors. Nursing Staff in Hospitals and Nursing Homes: Is It Adequate? Washington, DC: National Academy Press; 1996. Report by the Institute of Medicine. [PubMed] [Google Scholar]