Abstract
Objective
To examine nationally representative patterns and predictors of delays in contacting a professional after first onset of a mental disorder.
Data Sources
The National Comorbidity Survey, a nationally representative survey of 8,098 respondents aged 15–54.
Study Design
Cross-sectional survey.
Data Collection
Assessed lifetime DSM-III-R mental disorders using a modified version of the Composite International Diagnostic Interview (CIDI). Obtained reports on age at onset of disorders and age of first treatment contact with each of six types of professionals (general medical doctors, psychiatrists, other mental health specialists, religious professionals, human services professionals, and alternative treatment professionals). Used Kaplan–Meier (KM) curves to estimate cumulative lifetime probabilities of treatment contact after first onset of a mental disorder. Used survival analysis to study the predictors of delays in making treatment contact.
Principal Findings
The vast majority (80.1 percent) of people with a lifetime DSM-III-R disorder eventually make treatment contact, although delays average more than a decade. The duration of delay is related to less serious disorders, younger age at onset, and older age at interview. There is no evidence that delay in initial contact with a health care professional is increased by earlier contact with other non–health-care professionals.
Conclusions
Within the limits of recalling lifetime events, it appears that delays in initial treatment contact are an important component of the larger problem of unmet need for mental health care. Interventions are needed to decrease these delays.
Keywords: Epidemiology, health services delivery, mental health
Despite the substantial distress and impairment caused by mental disorders and the availability of effective therapies, unmet need for treatment of mental disorders remains a serious public health problem (Kessler, Olfson, and Berglund 1998; Olfson et al. 1998; Regier et al. 1993; Wang, Berglund, and Kessler 2000; Wang, Demler, and Kessler 2002). To begin addressing this problem, it is essential to understand the patterns and correlates of failing to progress in the help-seeking process (Gallo et al. 1995; Rogler and Cortes 1993). One important initial stage in the help-seeking process is making treatment contact in a timely manner after first onset of a mental disorder. Little is known about patterns and correlates of initial treatment contacts, as help-seeking research has generally focused on recent service use among prevalent cases over relatively short time periods rather than on delays in initial treatment contact among incident cases over longer time periods (Breakey and Kaminsky 1982; Frank and McGuire 1986; Gallo et al. 1995; Goodman, Sewells, and Jampol 1984; Hu et al. 1991; Joseph and Boeckh 1981; Keeler et al. 1986; Leaf, Bruce, and Tischler 1986; Leaf et al. 1988; Padgett et al. 1994; Phillips and Murrell 1994; Sherbourne 1988; Taube and Rupp 1986; Temkin-Greener and Clark 1988; Wells et al. 1988). The few studies that have focused on the latter question have consistently shown that the vast majority of people with mental disorders eventually establish treatment contact (Johnstone et al. 1986; Kessler, Olfson, and Berglund 1998; Lincoln and McGorry 1995; Loebel et al. 1992; Olfson et al. 1998). However, these studies have also shown that long delays are pervasive. For example, an analysis of first treatment contact for depression in a nationally representative sample of people with a lifetime history of depression estimated that more than 80 percent eventually seek treatment, but that the median delay is seven years (Kessler, Olfson, and Berglund 1998).
The present study has three aims. First, we estimate the cumulative lifetime probability and typical delays in making initial treatment contact after first onset of commonly occurring mental disorders in the National Comorbidity Survey (NCS). Based on the previous work cited above, we hypothesized that the cumulative probability of eventual treatment contact would be high and that typical delays would be substantial. Second, we study predictors of delay for which NCS data allowed retrospective dating relative to the age of first seeking treatment and for which there were a priori hypotheses concerning effects on treatment delays. Based on the results of prior studies, we hypothesized that delays would be shorter for those with younger ages at interview (i.e., younger age cohorts) (Wang et al. 2000), women compared to men (Kessler 1986), whites compared to nonwhites (Padgett et al. 1994; Temkin-Greener and Clark 1988), the married compared to the unmarried (Gallo et al. 1995; Leaf et al. 1988), the well educated compared to the poorly educated (Leaf et al. 1988; Wells et al. 1988), residents of urban compared to rural areas (Joseph and Boeckh 1981), and for people with more severe mental disorders (Leaf et al. 1988; Wang, Berglund, and Kessler 2000; Wells, Burnam, and Camp 1995).
Third, we assess the typical length and predictors of delays in contacting each of six specific types of professionals: general medical doctors, psychiatrists, other mental health specialists, religious professionals, human services professionals, and alternative treatment professionals. Prior studies have generally aggregated these different types of professionals, despite the fact that their care is not likely to be equivalent. A growing body of literature (Katon et al. 1996, 1995; Lehman and Steinwachs 1998a; Wells et al. 2000) suggests that treatments must conform to evidence-based guidelines (Agency for Health Care Policy and Research 1993; American Psychiatric Association 1994, 1997, 1998, 2000; Lehman and Steinwachs 1998b) to be effective. Non-health-care professionals may provide effective treatments for some disorders (e.g., substance disorders); however, for many mental disorders, only health care professionals (i.e., general medical doctors, psychiatrists, and other mental health specialists) have the training or authorization to deliver treatments with documented effectiveness. In our analyses disaggregated by provider type, we also explore whether initially contacting non-health care professionals reduces the probability or speed of subsequently contacting health care providers able to deliver effective treatments. Answering this question is of public health importance given the recent proliferation in treatment options available for mental health problems (Eisenberg et al. 1998, 1993; Kessler et al. 2001).
Methods
Sample
The National Comorbidity Survey (NCS) includes 8,098 respondents who were interviewed face-to-face between September 1990 and February 1992. The institutional review board at the University of Michigan approved the study methods used in the National Comorbidity Survey. Respondents were selected using a stratified, multistage area probability sample representative of persons aged 15 to 54 in the 48 coterminous United States. The response rate was 82.4 percent. The diagnostic assessment, which is described in the next subsection, was administered in part 1 of the interview. All respondents classified as having a lifetime DSM-III-R disorder and a probability subsample of other respondents were administered part 2 of the interview. A total of 5,877 respondents participated in the part 2 interview. The treatment questions on which the current report is based were included in the part 2 interview. The analysis reported here was based on weighted part 2 data, with the weights adjusting for differential probabilities of selection and nonresponse as well as for discrepancies between the sample and the population on a range of sociodemographic variables. The NCS sampling and weighting procedures are described in more detail elsewhere (Kessler et al. 1994; Kessler, Little, and Groves 1995).
Diagnostic Assessment
Lifetime psychiatric diagnoses are based on a modified version of the Composite International Diagnostic Interview (CIDI) (World Health Organization 1990). The diagnoses considered are DSM-III-R (American Psychiatric Association 1987) major depressive episode and dysthymia (considered together), panic disorder, generalized anxiety disorder, phobia (either simple, social, or agoraphobia with or without panic), nonaffective psychosis (schizophrenia, schizoaffective disorder, schizophreniform disorder, delusional disorder, brief psychotic disorder, and psychotic disorder not otherwise specified), and substance use disorders (alcohol or drug abuse or dependence). World Health Organization CIDI Field Trials (Wittchen 1994) and NCS CIDI clinical reappraisal studies (Kessler et al. 1998; Wittchen et al. 1995, 1996) have documented acceptable to good concordance between most of these diagnoses and blind clinical reinterviews using the Structured Clinical Interview Diagnostic (SCID) as the validation standard. Exceptions were mania (Kessler et al. 1997) and nonaffective psychosis (Kendler et al. 1996), both of which were overdiagnosed by the CIDI according to clinical reinterviews. We addressed overdiagnosis of mania by confining received CIDI diagnoses to the euphoric-grandiose subtype of mania, which was assessed with good validity in the NCS. Overdiagnosis of nonaffective psychosis was addressed by carrying out clinical reinterviews with all NCS respondents who screened positive for nonaffective psychosis by the CIDI and basing final diagnoses on these clinical assessments rather than on the original CIDI classifications.
Treatment Contact with Specific Types of Professionals
All part 2 NCS respondents were asked a series of lifetime questions about whether and, if so, at what age they first made contact with each of six types of professionals for problems with their emotions, nerves, mental health, or alcohol and substance use: general medical doctors other than psychiatrists (including general practitioners, family physicians, and physician specialists such as cardiologists and gynecologists); psychiatrists; mental health specialists other than psychiatrists (including psychologists, mental health counselors, social workers [other than in a social services agency], and providers in mental health, alcohol, and drug outpatient clinics); religious professionals (including ministers, priests, rabbis, and their counterparts in other religions); human services professionals (including counselors and social workers specifically in a social service agency); and alternative treatment professionals (including spiritualists, herbalists, natural therapists, faith healers, self-help groups, and similar advisors or agencies).
Predictor Variables
Sociodemographic variables used as predictors of delay in treatment contact included age at interview (i.e., born in 1936–1945, 1946–1955, 1956–1965, or 1966–1975), sex, race (non-Hispanic white, non-Hispanic black, Hispanic, other), marital status (never married, married, previously married), educational attainment (less than high school, high school graduate, some college, college graduate), urbanicity (metropolitan area, other urbanized area, rural), and region of the United States (northeast, midwest, south, west). Clinical variables used as predictors included type of mental disorder (depression or dysthymia, panic disorder, generalized anxiety disorder, phobias, nonaffective psychosis, and substance abuse/dependence), number of disorders, and the presence of suicidal thoughts, suicidal plans, and suicide attempts.
Analysis Procedures
Kaplan–Meier curves (Kaplan and Meier 1958) were used to calculate cumulative lifetime probabilities of contacting any professional and each type of professional. Separate curves were plotted for subsamples defined by predictor variables. Discrete-time survival analysis (Efron 1988) restricted to respondents who eventually made treatment contact was then used to study predictors of delay in initial treatment contact after first onset of a disorder. Sex, race, and age at interview were treated as time-invariant predictors, while age at first onset of a mental disorder, education, marital status, urbanicity, and region of the country were treated as time-varying predictors. Reported ages of onset were used to assign time-varying values to the following predictors: type of disorder, number of disorders, the presence of suicidal thoughts, the presence of a suicide plan, and a history of past suicide attempts.
Separate survival equations were then estimated to predict the probability of and delays in making treatment contact with each of the six specific types of professionals. In addition to the variables described above, these equations included time-varying predictors representing prior treatment with each of the other five types of professionals. The Taylor Series Linear Approximation technique implemented in SUDAAN (Research Triangle Institute 2000) was used to adjust for the effects of weighting and clustering of the survey data on significance tests.
Results
Cumulative Lifetime Probability of Treatment Contact
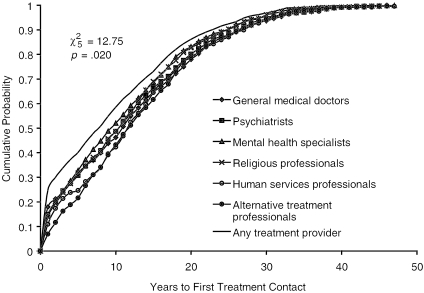
Figure 1 presents Kaplan–Meier curves for the cumulative probabilities of ever contacting any professional and specific types of professionals after first onset of any of the disorders considered here. These curves were estimated in the subsample (46.9 percent) of NCS respondents with a lifetime history of at least one of these disorders. The estimated cumulative lifetime probability of making contact with any professional for any of these disorders is 80.1 percent (Table 1). Probabilities of contacting specific types of professionals differ significantly across the six types (χ25=12.75; p=.020) and range from a high of 51.2 percent for mental health specialists to a low of 19.4 percent for human services providers.
Figure 1.
Cumulative Probabilities of Contacting Specific Professionals after First Onset of Mental Disorders among Respondents with a Lifetime History of Mental Disorders
Note: For more detailed description of each specific type of professional, see the footnotes included on Tables 1 and 3.
Table 1.
Cumulative Lifetime Probabilities and Median Number of Years until First Contacting Professionals for Mental Disorders
| Cumulative Lifetime Probability | Median Years from Onset to Probability | |
|---|---|---|
| % | Years | |
| General medical doctors† | 46.1 | 10 |
| Psychiatrists | 27.3 | 11 |
| Mental health specialists‡ | 51.2 | 9 |
| Religious professionals§ | 34.1 | 11 |
| Human services professionals∥ | 19.4 | 12 |
| Alternative treatment professionals¶ | 41.1 | 12 |
| Any treatment provider (of above 6) | 80.1 | 11 |
General medical doctors refers to doctors other than psychiatrists (including general practitioners, family physicians, and physician specialists such as cardiologists and gynecologists).
Mental health specialists refers to specialists other than psychiatrists (including psychologists, mental health counselors, social workers [other than in a social services agency], and providers in mental health, alcohol, and drug outpatient clinics).
Religious professionals refers to ministers, priests, rabbis, and their counterparts in other religions.
Human services professionals refers to counselors and social workers, specifically in a social service agency.
Alternative treatment professionals refers to spiritualists, herbalists, natural therapists, faith healers, self-help groups, and similar advisors or agencies.
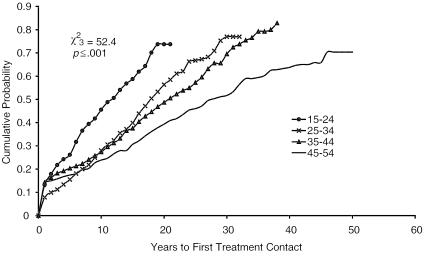
Figure 2 presents the Kaplan–Meier curve of contacting any professional disaggregated by age at interview. The curves are significantly different across age cohorts (χ23=52.4; p<.001), with the probability of treatment contact increasing among those with younger ages at interview. These curves suggest that the vast majority of people in younger age cohorts with mental disorders will eventually make treatment contact and that the contemporary problem is not failure to seek treatment but rather pervasive delay in seeking treatment.
Figure 2.
Cumulative Probabilities of Contacting Any Professional after First Onset of Mental Disorders, Shown for Specific Age Cohorts
Delay in Treatment Contact
The extent of delay can be seen in Table 1, which shows that the median number of years between the onset of the first mental disorder and first treatment contact is 11 years in the subsample of NCS respondents who eventually seek treatment. There is no significant difference in the median time of delay depending on type of professional eventually contacted (χ25=9.3; p=.097).
Predictors of Delay in Treatment Contact
The net effects of sociodemographic and clinical variables in predicting duration of delay among people who eventually seek treatment are presented in Table 2. Significant predictors of longer delays include older age cohorts, early age at onset, absence of severity indicators (suicidal thoughts, plans, or attempts, depressive disorders, panic disorders, and substance disorders), and not being married. (Note, alcohol and drug disorders did not affect delay in treatment contact differently when placed separately into the model shown in Table 2; therefore, alcohol and drug disorders were combined in all subsequent analyses as “substance disorders”). Contrary to our a priori hypotheses, there are no significant associations between delay and gender, race/ethnicity, education, or urbanicity.
Table 2.
Predictors of Speed in Making Treatment Contact with Any Professional for Mental Disorders, among Those That Received Treatment
| Characteristics | OR† | (95% CI) | χ2 | d.f. |
|---|---|---|---|---|
| Age at interview | 741.8* | 3 | ||
| 15–24 | 24.0* | (18.6, 31.0) | ||
| 25–34 | 4.9* | (3.7, 6.5) | ||
| 35–44 | 1.2* | (1.7, 2.7) | ||
| 45–54 | 1.0 | — | ||
| Gender | 0.3 | 1 | ||
| Female | 1.1 | (0.9, 1.3) | ||
| Male | 1.0 | — | ||
| Marital status | 13.1* | 2 | ||
| Married | 1.0 | — | ||
| Never married | 1.3* | (1.1, 1.5) | ||
| Separated/widowed/divorced | 1.4* | (1.1, 1.8) | ||
| Age at first onset | 50.0* | 3 | ||
| 1–12 | 1.0 | — | ||
| 13–19 | 1.0 | (0.9, 1.2) | ||
| 20–29 | 1.2 | (0.9, 1.5) | ||
| 30–54 | 1.7 | (1.0, 2.9) | ||
| Type of disorder | 112.3* | 6 | ||
| Depression/dysthymia | 2.6* | (2.2, 3.2) | ||
| Panic disorder | 2.8* | (1.6, 4.8) | ||
| GAD‡ | 1.6 | (1.0, 2.5) | ||
| PTSD§ | 1.3 | (1.0, 1.6) | ||
| Psychotic disorder | 1.3 | (0.8, 2.2) | ||
| Substances∥ | 1.7* | (1.3, 2.0) | ||
| Phobias | 1.0 | — | ||
| Suicide | 81.5* | 2 | ||
| Thought | 4.5* | (2.8, 7.4) | ||
| Plan | 6.7* | (2.4, 18.3) | ||
| Attempt | 3.8* | (2.3, 6.1) | ||
| None | 1.0 | — |
Significant at the .05 level, two-sided test.
Odds ratio (95% CI) of the speed in making initial contact with any professional. The model was run on the subsample with disorders who sought treatment from any professional. Non-significant predictor variables are not shown, but results for them are available upon request.
GAD refers to generalized anxiety disorder.
PTSD refers to posttraumatic stress disorder.
Substances refers to either alcohol or drug disorders.
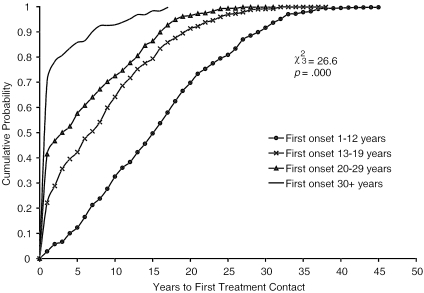
The effect of early age at onset is of considerable importance, as patients whose first onsets occurred when they were children or adolescents have significantly longer delays (χ23=26.6; p<.001) than patients whose first onsets occurred in adulthood. Survival curves (Figure 3) show that patients with early-onset disorders typically do not make their first treatment contacts until early adulthood.
Figure 3.
Cumulative Probabilities of Contacting Any Professional for Mental Disorder among Those Making Any Treatment Contact, Shown Separately for Groups Defined by the Age of Disorder Onset
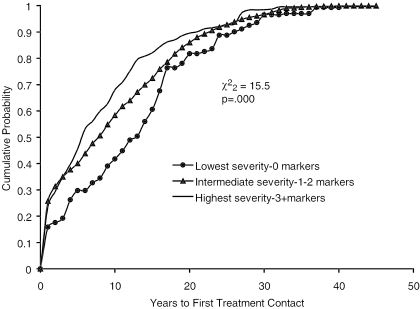
To examine the effect of global severity rather than separate indicators, we created a severity score by assigning respondents one point for each of the significant severity indicators in Table 2 (e.g., suicidal thoughts, plans, or attempts, depressive disorders, panic disorders, and substance disorders). A three-category classification was then created in which the lowest level was defined as none of the severity markers, the intermediate level 1–2 severity markers, and the highest level as having three or more severity markers. The Kaplan–Meier curves for these three subsamples are shown in Figure 4. Despite significant subsample differences in median time of delay based on this severity gradient (χ22=15.5; p<.001), median delay remains substantial (approximately five years) even in the subsample classified as having the highest severity.
Figure 4.
Cumulative Probabilities of Contacting Any Professional for Mental Disorder among Those Making Any Treatment Contact, Shown Separately for Groups Defined by the Number of Markers of Disorder
Predictors of Provider-Specific Delay
Parallel survival equations were estimated to study the predictors of contacting each of the six types of professionals (in the total sample) and the predictors of delay in contacting each of these six types of professionals (in the subsamples of respondents who eventually sought treatment with that type of professional). The only difference from the equation in Table 2 was that these provider-specific equations included as additional predictors variables representing prior treatment contact with other types of professionals. In general, the significant predictors of delay in making any treatment contact shown in Table 2 were also found to consistently predict delays in provider-specific analyses (results of full models available on request).
Several results across the six provider types are worth highlighting. First, while younger age cohorts have the shortest delays in contacting all six types of professionals, the largest age cohort effects are for contacting mental health specialists and alternative treatment professionals. Second, while early age of disorder onset is associated with longer delays in contacting all six types of professionals, it is especially true for contacting human services professionals and least true for contacting psychiatrists. Markers of illness severity (suicidal thoughts, plans, or attempts; depressive disorders; panic disorders; and substance disorders) were generally associated with shorter delays in contacting all types of professionals. However, there were shorter delays for suicidal patients in contacting non–health-care professionals.
The provider-specific equations also showed that, contrary to our initial hypothesis, earlier treatment-seeking with another type of professional is consistently associated both with elevated odds of subsequently seeking treatment with each of the other types of professionals (in the total sample) and with shorter delays (in the subsamples who sought treatment from one of the various types of professionals). (See Table 3.) Importantly, this pattern also held between initial contacts with non–health-care professionals (i.e., religious professionals, human services professionals, and alternative treatment professionals) and greater or faster subsequent contacts with health care providers (i.e., general medical doctors, psychiatrists, and other mental health specialists), with all of the coefficients in Table 3 for these associations being statistically significant.
Table 3.
The Effects of Prior Contacts on the Probability and Speed of Contacting Specific Professionals for Mental Disorders
| Cumulative Lifetime Probability of Contacting Specific Professionals | Speed of Contacting Specific Professionals | |||||||
|---|---|---|---|---|---|---|---|---|
| Effect of Any Prior Contact | Effect of a Single Visit Increase in the Number of Prior Contacts | Effect of Any Prior Contact | Effect of a Single Visit Increase in the Number of Prior Contacts | |||||
| Specific Professional Subsequently Contacted | OR† | (95% CI) | OR‡ | (95% CI) | OR† | (95% CI) | OR‡ | (95% CI) |
| General medical doctors§ | 5.0* | (3.9, 6.3) | 2.2* | (1.9, 2.5) | 2.9* | (2.3, 3.5) | 1.7* | (1.5, 1.9) |
| Psychiatrists | 12.3* | (9.0, 16.8) | 2.7* | (2.2, 3.2) | 7.4* | (5.5, 9.8) | 2.2* | (1.9, 2.6) |
| Mental health specialists∥ | 5.4* | (4.3, 6.9) | 2.3* | (2.1, 2.7) | 2.8* | (2.3, 3.5) | 1.7* | (1.5, 1.9) |
| Religious professionals¶ | 11.8* | (9.4, 14.8) | 2.5* | (2.1, 2.9) | 6.1* | (4.9, 7.7) | 2.0* | (1.7, 2.3) |
| Human services professionals†† | 23.7* | (17.9, 31.3) | 2.5* | (2.1, 2.9) | 14.8* | (10.8, 20.2) | 2.3* | (1.9, 2.6) |
| Alternative treatment professionals‡‡ | 9.2* | (7.9, 10.7) | 2.2* | (2.0, 2.4) | 4.8* | (4.1, 5.7) | 1.8* | (1.7, 2.0) |
Significant at the .05 level, two-sided test.
Odds ratios (OR) with 95% Confidence Interval (95% CI) of making subsequent treatment contact with specific professional identified in each row. In addition to the variable representing any prior contacts with any professionals, models also contained all predictor variables described on page 5 in text. All models were run in the total sample of respondents with mental disorders.
Odds ratios (OR) with 95% Confidence Interval (95% CI) of the speed of making subsequent treatment contact with specific professional identified in each row. In addition to the variable representing number of prior contacts, models also contained all predictor variables described on page 393 in text. All models were run in the subsample of respondents with mental disorders who sought treatment from the professional identified in each row.
General medical doctors refers to doctors other than psychiatrists (including general practitioners, family physicians, and physician specialists such as cardiologists and gynecologists).
Mental health specialists refers to specialists other than psychiatrists (including psychologists, mental health counselors, social workers [other than in a social services agency], and providers in mental health, alcohol, and drug outpatient clinics).
Religious professionals refers to ministers, priests, rabbis, and their counterparts in other religions.
Human services professionals refers to counselors and social workers, specifically in a social service agency.
Alternative treatment professionals refers to spiritualists, herbalists, natural therapists, faith healers, self-help groups, and similar advisors or agencies.
Discussion
Results of the current study should be interpreted with three sets of limitations in mind. First, respondents were asked to retrospectively recall and date the first onset of disorders and seeking treatment in their lifetime. In the absence of confirmatory records, we cannot quantify the extent to which there was recall failure (Kessler et al. 1998). Recall bias could also have occurred if respondents who did not receive treatment in the past were more likely to forget or “normalize” their symptoms when interviewed than respondents who had received treatments. Such biased recall, to the extent it occurred, would have caused us to overestimate the proportion eventually making treatment contact. To address these issues, the CIDI used three-part question series that began with “prequests” asking “Can you remember the EXACT age the VERY FIRST TIME you had…” Positive responses were associated in pilot work with characteristics enhancing the accuracy of recall (e.g., more recent events, smaller total numbers of events, and events with distinctive contexts), so these were then followed by questions about the age of onset. On the other hand, negative responses were followed by questions asking explicitly for estimates (e.g., “ABOUT how old were you the first time you had…”); ranges of responses were accepted without probing. Additional questions placed upper bounds on the uncertainty of age-of-onsets (e.g., “What is the earliest age you can CLEARLY REMEMBER having….”). How these measures affected recall accuracy of lifetime events is uncertain, but fewer implausible age-of-onsets have been found in the NCS than in earlier surveys (Knauper et al. 1999).
Second, the potential predictors we examined were necessarily limited to a small number of patient demographic and clinical variables included in the NCS that could be retrospectively dated in relation to the age of first seeking treatment and for which a priori hypotheses concerning effects on treatment delays had been raised in prior studies. We were also limited in the number of characteristics we examined to avoid finding spurious relationships from multiple comparisons. Finally, the data were collected in the early 1990s. Many changes have occurred both in treatments for mental disorders (e.g., introduction of new medications with potentially greater tolerability) and in mental health care delivery systems (e.g., greater proportions receiving mental health treatment under managed care) since that time. A National Comorbidity Survey Replication (NCS-R) is currently being carried out to document the effects of these changes on patterns of help-seeking for mental disorders (Kessler, Olfson, and Berglund 1998; Wang, Berglund, and Kessler 2000).
Within the context of these potential limitations, the results highlight the importance of moving beyond the traditional focus of mental health services research on low rates of recent treatment among prevalent cases (Breakey and Kaminsky 1982; Frank and McGuire 1986; Gallo et al. 1995; Goodman, Sewells, and Jampol 1984; Hu et al. 1991; Joseph and Boeckh 1981; Keeler et al. 1986; Leaf, Bruce, and Tischler 1986; Leaf et al. 1988; Padgett et al. 1994; Phillips and Murrell 1994; Sherbourne 1988; Taube and Rupp 1986; Temkin-Greener and Clark 1988; Wells et al. 1988). The vast majority of people with a lifetime mental disorder eventually make treatment contact. In the youngest age cohorts, eventual contact is likely to be nearly universal. These findings clearly suggest that the focus should be on the more than decade-long delay in treatment contact that typically separates disorder onset from first treatment contact.
The finding that delays in initial treatment contact are shorter in the youngest age cohorts could reflect public education programs focused on mental disorders, liberalization of public attitudes toward mental illness, advances in treatments, and expansion of insurance programs (Bhugra 1989; Regier et al. 1988; Ridgely and Goldman 1989; Ross 1993). However, the fact that this cohort effect is at least as strong in predicting contacts with non–health-care professionals as with health care professionals is a source of concern. This finding confirms the results of other studies, which have shown that acceptance of alternative, self-help, and nontraditional forms of health care has been growing rapidly in recent years (Eisenberg et al. 1993; 1998; Kessler et al. 2001).
The longer delays for early-onset versus later-onset disorders could be due to the fact that minors rely on parents or other adults (e.g., teachers) to get them into treatment. Parental attitudes and perceptions are important determinants of children's health care use (Janicke, Finney, and Riley 2001) including mental health care (Morrissey-Kane and Prinz 1999). Only children with the most serious disorders or vigilant parents may receive timely care. In addition, children with early-onset mental disorders may develop coping strategies that ultimately interfere with treatment seeking later in life (e.g., developing extreme social withdrawal for social phobia or substance abuse to self-medicate depression).
The finding that severity is associated with shorter delays is not surprising, given previous research on the predictors of current treatment among prevalent cases (Leaf et al. 1988; Wang, Berglund, and Kessler 2000; Wells et al. 1995). Suicidal thoughts and behaviors may shorten delays because suicidal patients are mandated to receive emergent evaluations in most jurisdictions. Shorter delays for depressive disorders may be the result of mass screenings in the general public as well as improved recognition and treatment in primary care (Hirschfeld et al. 1997; Jacobs 1995). The prominent somatic symptoms that are often part of panic disorder have been suggested to lead to earlier evaluation (Katerndahl and Realini 1995; Katon, Von Korff, and Lin 1992). Difficulties forming or maintaining relationships, to the extent that they are captured by marital status, may have led those not married to more rapidly seek out the social support of mental health treatment following disorder onset. Alternatively, greater dysfunction from psychiatric disorders may be responsible for both difficulty in relationships and shorter delays (Gallo et al. 1995; Leaf et al. 1988).
An important question raised by these findings is whether the delays found here are of public health importance. Long delays might be found only for disorders that are of low severity, self-limiting, or free of long-term disabilities (Narrow et al. 2002). However, as shown in Figure 4, this does not appear to be the case. Delays between onset and first treatment contact average five years even for cases classified in the highest of the three severity categories considered here.
Furthermore, even delays for less severe disorders may be of concern. Preclinical studies suggest that untreated psychiatric disorders can progress in frequency, severity, and spontaneity due to neural “kindling” and that interventions effective in earlier phases of kindling may become ineffective during later full-blown syndromes (Post and Weiss 1998); however the relevance of such preclinical findings for human populations requires additional study. Epidemiological data have also been suggestive in showing that many negative outcomes such as school failure, teenage child-bearing, failure to establish a stable employment history, early marriage, marital violence, and marital instability are significantly related to early-onset mental disorders and typically occur before first treatment contacts (Forthofer et al. 1996; Kessler et al. 1997, 1995; Kessler, Walters, and Forthofer 1998). Studies of the natural history of mental disorders also show that the majority of people with one mental disorder subsequently develop comorbid disorders and such comorbidity is associated with a more persistent and severe course of illness (Kessler 1997; Kessler and Price 1993; Kessler et al. 1997). Psychological autopsy studies reveal that a considerable proportion of individuals who complete suicide are not in active mental health treatment at the time of their deaths (Houston, Hawton, and Shepperd 2001; Isometsa et al. 1994). However, some studies have failed to find a relationship between the duration of untreated mental illness and long-term outcomes such as likelihood of relapse (Norman and Malla 2001).
Clearly, definitively answering whether reducing treatment delays can actually prevent such negative outcomes from occurring will require data from experimental trials evaluating the long-term effects of aggressive outreach and treatment of cases with recent onsets. While rare, such long-term early intervention trials are beginning to be carried out. For example, the Multimodel Treatment Study (MTA) of children with Attention-Deficit/Hyperactivity Disorder (ADHD) (MTA Cooperative Group 1999) is a decade-long randomized effectiveness trial of medication management strategies and intensive behavioral treatment of ADHD children who are now being followed into adulthood. Another intervention trial is examining the effects of school-based screening plus early cognitive-behavioral therapy for children with social phobia, with the goal being to identify long-term effects by following youngsters into early adulthood (Dierker et al. 2000). Another long-term follow-up of a randomized intervention trial of social phobia treatment is also being carried out (Beidel, Turner, and Morris 2000). Even if such trials ultimately show benefits, it is important to keep in mind that earlier treatment might also have negative consequences such as unnecessary treatment of those who would not have developed serious disorders as well as the occurrence of more adverse effects from treatment. Formal cost-effectiveness analyses would then be needed to balance these and identify the net benefits of early intervention.
It is important to consider what could ultimately be done to reduce the pervasive delays observed here. National screening days and large-scale public education programs, such as the National Institute of Mental Health (NIMH) Depression, Awareness, Recognition, and Treatment (DART) program, hold promise for hastening the awareness, detection, and treatment of mental disorders (Morrissey-Kane and Prinz 1999; Regier et al. 1988). Demand management strategies developed by health educators may also reduce critical time-delays in treatment contacts as well as prevent premature dropout from treatments (Carleton et al. 1996; Velicer et al. 1995). Additional efforts may be needed to train non–health-care professionals to recognize individuals with mental disorders, especially severe disorders in need of emergent care, and encourage timely referrals to appropriate health care professionals (Kessler et al. 2001; Weaver 1995). The availability of brief parent- and teacher-administered scales to assess common childhood disorders (Connors 1994) increases the feasibility of school-based screening to detect early-onset disorders. It is likely that a combination of such interventions will be required to make meaningful progress in shortening the high-risk period of untreated mental disorders.
References
- Agency for Health Care Policy and Research. Depression in Primary Care, 2: Treatment of Major Depression. Clinical Practice Guideline Number 5. Rockville, MD: Agency for Health Care Policy and Research, U.S. Dept of Health and Human Services; 1993. AHCPR publication 93-0551. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. (3d ed., rev.) Washington, DC: American Psychiatric Association; 1987. DSM-III-R. [Google Scholar]
- American Psychiatric Association. Practice Guideline for the Treatment of Patients with Bipolar Disorder. Washington, DC: American Psychiatric Association; 1994. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Practice Guideline for the Treatment of Patients with Schizophrenia. Washington, DC: American Psychiatric Association; 1997. [Google Scholar]
- American Psychiatric Association. Practice Guideline for the Treatment of Patients with Panic Disorder. Washington, DC: American Psychiatric Association; 1998. [PubMed] [Google Scholar]
- American Psychiatric Association. Practice Guideline for the Treatment of Patients with Major Depressive Disorder. 2d ed. Washington, DC: American Psychiatric Association; 2000. [PubMed] [Google Scholar]
- Beidel D C, Turner S M, Morris T L. “Behavioral Treatment of Childhood Social Phobia.”. Journal of Consulting and Clinical Psychology. 2000;68(6):1072–80. [PubMed] [Google Scholar]
- Bhugra D. “Attitudes towards Mental Illness: A Review of the Literature.”. Acta Psychiatrica Scandinavica. 1989;80(1):1–12. doi: 10.1111/j.1600-0447.1989.tb01293.x. [DOI] [PubMed] [Google Scholar]
- Breakey W R, Kaminsky M J. “An Assessment of Jarvis Law in an Urban Catchment Area.”. Hospital and Community Psychiatry. 1982;33(8):661–3. doi: 10.1176/ps.33.8.661. [DOI] [PubMed] [Google Scholar]
- Carleton R A, Bazzarre T, Drake J, Dunn A, Fisher E B, Jr., Grundy S M, Hayman L, Hill M N, Maibach E W, Prochaska J, Schmid T, Smith S C, Jr., Susser M W, Worden J W. “Report of the Expert Panel on Awareness and Behavior Change to the Board of Directors, American Heart Association.”. Circulation. 1996;93(9):1768–72. doi: 10.1161/01.cir.93.9.1768. [DOI] [PubMed] [Google Scholar]
- Dierker L D, Albano A M, Clarke G, Heimberg R G, Kendall P C, Merikangas K R, Lewinsohn P, Offord D, Kessler R C, Kupfer D. “Screening for Anxiety and Depression in Early Adolescence.”. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;40(8):929–36. doi: 10.1097/00004583-200108000-00015. [DOI] [PubMed] [Google Scholar]
- Efron B. “Logistic Regression, Survival Analysis, and the Kaplan–Meier Curve.”. Journal of the American Statistical Association. 1988;83(402):415–25. [Google Scholar]
- Eisenberg D M, Davis R B, Ettner S L, Appel S, Wilkey S A, Van Rompay M I, Kessler R C. “Trends in Alternative Medicine Use in the United States, 1990–1997: Results of a Follow-Up National Survey.”. Journal of the American Medical Association. 1998;280(18):1569–75. doi: 10.1001/jama.280.18.1569. [DOI] [PubMed] [Google Scholar]
- Eisenberg D M, Kessler R C, Foster C L, Norlock F E, Calkins D R, Delbanco T L. “Unconventional Medicine in the United States: Prevalence, Costs, and Patterns of Use.”. New England Journal of Medicine. 1993;328(4):246–52. doi: 10.1056/NEJM199301283280406. [DOI] [PubMed] [Google Scholar]
- Forthofer M S, Kessler R C, Story A L, Gotlib I H. “The Effects of Psychiatric Disorders on the Probability and Timing of First Marriage.”. Journal of Health and Social Behavior. 1996;37(2):121–32. [PubMed] [Google Scholar]
- Frank R G, McGuire T G. “A Review of Studies of the Impact of Insurance on the Demand and Utilization of Specialty Mental Health Services.”. Health Services Research. 1986;21(2, part 2):241–65. [PMC free article] [PubMed] [Google Scholar]
- Gallo J J, Marino S, Ford D, Anthony J C. “Filters on the Pathway to Mental Health Care: II. Sociodemographic Factors.”. Psychological Medicine. 1995;25(6):1149–60. doi: 10.1017/s0033291700033122. [DOI] [PubMed] [Google Scholar]
- Goodman S H, Sewells D S, Jampol R C. “On Going to the Counselor: Contributions of Life Stress and Social Supports to the Decision to Seek Psychological Counseling.”. Journal of Counseling Psychology. 1984;31(3):306–13. [Google Scholar]
- Hirschfeld R M A, Keller M B, Panico S, Arons B S, Barlow D, Davidoff F, Endicott J, Froom J, Goldstein M, Gorman J M, Marek R G, Maurer T A, Meyer R, Phillips K, Ross J, Schwenk T L, Sharfstein S S, Thase M E, Wyatt R J. “The National Depressive and Manic-Depressive Association Consensus Statement on the Undertreatment of Depression.”. Journal of the American Medical Association. 1997;277(4):333–40. [PubMed] [Google Scholar]
- Houston K, Hawton K, Shepperd R. “Suicide in Young People Aged 15–24: A Psychological Autopsy Study.”. Journal of Affective Disorders. 2001;63(1–3):159–70. doi: 10.1016/s0165-0327(00)00175-0. [DOI] [PubMed] [Google Scholar]
- Hu T W, Snowden L R, Jerrell J M, Nguyen T D. “Ethnic Populations in Public Mental Health: Services Choice and Level of Use.”. American Journal ofPsychiatry. 1991;81(11):1429–34. doi: 10.2105/ajph.81.11.1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isometsa E T, Henriksson M M, Aro H M, Heikkinen M E, Kuoppasalmi K I, Lonnqvist J K. “Suicide in Major Depression.”. American Journal ofPsychiatry. 1994;151(4):530–6. doi: 10.1176/ajp.151.4.530. [DOI] [PubMed] [Google Scholar]
- Jacobs D G. “National Depression Screening Day: Educating the Public, Reaching Those in Need of Treatment, and Broadening Professional Understanding.”. Harvard Review of Psychiatry. 1995;3:156–9. doi: 10.3109/10673229509017181. [DOI] [PubMed] [Google Scholar]
- Janicke D M, Finney J W, Riley A W. “Children's Health Care Use: A Prospective Investigation of Factors Related to Care-Seeking.”. Medical Care. 2001;39(9):990–1001. doi: 10.1097/00005650-200109000-00009. [DOI] [PubMed] [Google Scholar]
- Johnstone E C, Crow T J, Johnson A L, MacMillan J F. “The Northwick Park Study of First Episodes of Schizophrenia: I Presentation of the Illness and Problems Relating to Admission.”. British Journal of Psychiatry. 1986;148(2):115–20. doi: 10.1192/bjp.148.2.115. [DOI] [PubMed] [Google Scholar]
- Joseph A E, Boeckh J L. “Locational Variation in Mental Health Care Utilization Dependent upon Diagnosis: A Canadian Example.”. Social Science and Medicine. 1981;15(3):395–440. doi: 10.1016/0160-8002(81)90058-7. [DOI] [PubMed] [Google Scholar]
- Kaplan E L, Meier P. “Nonparametric Estimation from Incomplete Observations.”. Journal of the American Statistical Association. 1958;53(282):281–4. [Google Scholar]
- Katerndahl D A, Realini J P. “Where Do Panic Attack Sufferers Seek Care?”. Journal of Family Practice. 1995;40(3):237–43. [PubMed] [Google Scholar]
- Katon W J, Robinson P, Von Korff M, Lin E, Bush T, Ludman E, Simon G E, Walker E. “A Multifaceted Intervention to Improve Treatment of Depression in Primary Care.”. Archives of General Psychiatry. 1996;53(10):924–32. doi: 10.1001/archpsyc.1996.01830100072009. [DOI] [PubMed] [Google Scholar]
- Katon W J, Von Korff M, Lin E. “Panic Disorder: Relationship to High Medical Utilization.”. American Journal of Medicine. 1992;92(1A, Supplement):7–11S. doi: 10.1016/0002-9343(92)90130-4. [DOI] [PubMed] [Google Scholar]
- Katon W J, Von Korff M, Lin E, Walker E, Simon G E, Bush T, Robinson P, Russo J. “Collaborative Management to Achieve Treatment Guidelines: Impact on Depression in Primary Care.”. Journal of the American Medical Association. 1995;273(13):1026–31. [PubMed] [Google Scholar]
- Keeler E B, Wells K B, Manning W G, Rumpel J D, Hanley J M. The Demand for Episodes of Mental Health Services. Santa Monica, CA: Rand Corporation; 1986. Rand Documents publication no. R-3432-NIMH. [Google Scholar]
- Kendler K S, Gallagher T J, Abelson J M, Kessler R C. “Lifetime Prevalence, Demographic Risk Factors, and Diagnostic Validity of Nonaffective Psychosis as Assessed in a U.S. Community Sample.”. Archives of General Psychiatry. 1996;53(11):1022–31. doi: 10.1001/archpsyc.1996.01830110060007. [DOI] [PubMed] [Google Scholar]
- Kessler R C. “Sex Differences in the Use of Health Services.”. In: McHugh S, Vallis T M, editors. Illness Behavior: A Multidisciplinary Model. New York: Plenum; 1986. pp. 135–48. [Google Scholar]
- Kessler R C. “The Prevalence of Psychiatric Comorbidity.”. In: Wetzler S, Sanderson W C, editors. Treatment Strategies for Patients with Psychiatric Comorbidity. New York: Wiley; 1997. pp. 23–48. [Google Scholar]
- Kessler R C, Berglund P A, Foster C L, Saunders W B, Stang P E, Walters E E. “Social Consequences of Psychiatric Disorders, II: Teenage Parenthood.”. American Journal of Psychiatry. 1997;154(10):1405–11. doi: 10.1176/ajp.154.10.1405. [DOI] [PubMed] [Google Scholar]
- Kessler R C, Foster C L, Saunders W B, Stang P E. “Social Consequences of Psychiatric Disorders, I: Educational Attainment.”. American Journal of Psychiatry. 1995;152(7):1026–32. doi: 10.1176/ajp.152.7.1026. [DOI] [PubMed] [Google Scholar]
- Kessler R C, Little R J A, Groves R M. “Advances in Strategies for Minimizing and Adjusting for Survey Nonresponse.”. Epidemiologic Reviews. 1995;17(1):192–204. doi: 10.1093/oxfordjournals.epirev.a036176. [DOI] [PubMed] [Google Scholar]
- Kessler R C, McGonagle K A, Zhao S, Nelson C B, Hughes M, Eshleman S, Wittchen H-U, Kendler K S. “Lifetime and 12-Month Prevalence of DSM-III-R Psychiatric Disorders in the United States: Results from the National Comorbidity Survey.”. Archives of General Psychiatry. 1994;51(1):8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Kessler R C, Olfson M, Berglund P A. “Patterns and Predictors of Treatment Contact after First Onset of Psychiatric Disorders.”. American Journal of Psychiatry. 1998;155(1):62–9. doi: 10.1176/ajp.155.1.62. [DOI] [PubMed] [Google Scholar]
- Kessler R C, Price R H. “Primary Prevention of Secondary Disorders: A Proposal and Agenda.”. American Journal of Community Psychology. 1993;21(5):607–34. doi: 10.1007/BF00942174. [DOI] [PubMed] [Google Scholar]
- Kessler R C, Rubinow D R, Holmes C, Abelson J M, Zhao S. “The Epidemiology of DSM-III-R Bipolar I Disorder in a General Population Survey.”. Psychological Medicine. 1997;27(5):1079–89. doi: 10.1017/s0033291797005333. [DOI] [PubMed] [Google Scholar]
- Kessler R C, Soukup J, Davis R B, Foster D F, Wilkey S A, Van Rompay M I, Eisenberg D M. “The Use of Complementary and Alternative Therapies to Treat Anxiety and Depression in the United States.”. American Journal of Psychiatry. 2001;158(2):289–94. doi: 10.1176/appi.ajp.158.2.289. [DOI] [PubMed] [Google Scholar]
- Kessler R C, Walters E E, Forthofer M S. “The Social Consequences of Psychiatric Disorders, III: Probability of Marital Stability.”. American Journal of Psychiatry. 1998;155(8):1092–6. doi: 10.1176/ajp.155.8.1092. [DOI] [PubMed] [Google Scholar]
- Kessler R C, Wittchen H-U, Abelson J M, McGonagle K A, Schwarz N, Kendler K S, Knäuper B, Zhao S. “Methodological Studies of the Composite International Diagnostic Interview (CIDI) in the U.S. National Comorbidity Survey.”. International Journal of Methods in Psychiatric Research. 1998;7(1):33–55. [Google Scholar]
- Kessler R C, Wittchen H-U, Abelson J, Zhao S. “Methodological Issues in Assessing Psychiatric Disorders with Self-Reports.”. In: Stone A A, Turkkan J S, Bachrach C A, Jobe J B, Kurtzman H S, Cain V S, editors. The Science of Self-Report. Mahwah, NJ: Erlbaum; 2000. [Google Scholar]
- Knauper B, Cannell C F, Schwarz N, Bruce M L, Kessler R C. “Improving Accuracy of Major Depression Age of Onset Reports in the U.S. National Comorbidity Survey.”. International Journal of Methods in Psychiatric Research. 1999;8(1):39–48. [Google Scholar]
- Leaf P J, Bruce M L, Tischler G L. “The Differential Effect of Attitudes on the Use of Mental Health Services.”. Social Psychiatry. 1986;21(4):187–92. doi: 10.1007/BF00583999. [DOI] [PubMed] [Google Scholar]
- Leaf P J, Bruce M L, Tischler G L, Freeman D H, Jr., Weissman M M, Myers J K. “Factors Affecting the Utilization of Specialty and General Medical Mental Health Services.”. Medical Care. 1988;26(1):9–26. doi: 10.1097/00005650-198801000-00002. [DOI] [PubMed] [Google Scholar]
- Lehman A F, Steinwachs D M. “Patterns of Usual Care for Schizophrenia: Initial Results from the Schizophrenia Patient Outcomes Research Team (PORT) Client Survey.”. Schizophrenia Bulletin. 1998a;24(1):11–20. doi: 10.1093/oxfordjournals.schbul.a033303. [DOI] [PubMed] [Google Scholar]
- Lehman A F, Steinwachs D M. “Translating Research into Practice: The Schizophrenia Patient Outcomes Research Team (PORT) Treatment Recommendations.”. Schizophrenia Bulletin. 1998b;24(1):1–10. doi: 10.1093/oxfordjournals.schbul.a033302. [DOI] [PubMed] [Google Scholar]
- Lincoln C V, McGorry P. “Who Cares?”. Psychiatric Services. 1995;46(11):1166–71. doi: 10.1176/ps.46.11.1166. [DOI] [PubMed] [Google Scholar]
- Loebel A D, Lieberman J A, Alvir J M J, Mayerhoff D I, Geisler S H, Szymanski S R. “Duration of Psychosis and Outcome in First-Episode Schizophrenia.”. American Journal of Psychiatry. 1992;149(9):1183–8. doi: 10.1176/ajp.149.9.1183. [DOI] [PubMed] [Google Scholar]
- Maruish M, editor. Use of Psychological Testing for Treatment Planning and Outcome Assessment. Hillsdale, NJ: Erlbaum; 1994. [Google Scholar]
- Morrissey-Kane E, Prinz R J. “Engaged in Child and Adolescent Treatment: The Role of Parental Cognitions and Attributions.”. Clinical Child and Family Psychology Review. 1999;2(3):183–98. doi: 10.1023/a:1021807106455. [DOI] [PubMed] [Google Scholar]
- MTA Cooperative Group. “A 14-Month Randomized Clinical Trial of Treatment Strategies for Attention-Deficit/Hyperactivity Disorder. The Multimodal Treatment Study of Children with ADHD.”. Archives of General Psychiatry. 1999;56(12):1073–86. doi: 10.1001/archpsyc.56.12.1073. [DOI] [PubMed] [Google Scholar]
- Narrow W E, Rae D S, Robins L N, Regier D A. “Revised Prevalence of Mental Disorders in the United States Using a Clinical Significance Criterion to Reconcile 2 Surveys' Estimates.”. Archives of General Psychiatry. 2002;59(3):115–23. doi: 10.1001/archpsyc.59.2.115. [DOI] [PubMed] [Google Scholar]
- Norman R M G, Malla A K. “Duration of Untreated Psychosis: A Critical Examination of the Concept and Its Importance.”. Psychological Medicine. 2001;31(3):381–400. doi: 10.1017/s0033291701003488. [DOI] [PubMed] [Google Scholar]
- Olfson M, Kessler R C, Berglund P A, Lin E. “Psychiatric Disorder Onset and First Treatment Contact in the United States and Ontario.”. American Journal of Psychiatry. 1998;155(10):1415–22. doi: 10.1176/ajp.155.10.1415. [DOI] [PubMed] [Google Scholar]
- Padgett D K, Patrick C, Burns B J, Schlesinger H J. “Ethnicity and Use of Outpatient Mental Health Services in a National Insured Population.”. American Journal of Public Health. 1994;84(2):222–6. doi: 10.2105/ajph.84.2.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips M A, Murrell S A. “Impact of Psychological and Physical Health, Stressful Events, and Social Support on Subsequent Mental Health Help Seeking among Older Adults.”. Journal of Consulting and Clinical Psychology. 1994;62(2):270–5. doi: 10.1037//0022-006x.62.2.270. [DOI] [PubMed] [Google Scholar]
- Post R M, Weiss S R. “Sensitization and Kindling Phenomena in Mood, Anxiety, and Obsessive-Compulsive Disorders: The Role of Serotonergic Mechanisms in Illness Progression.”. Biological Psychiatry. 1998;44(3):193–206. doi: 10.1016/s0006-3223(98)00144-9. [DOI] [PubMed] [Google Scholar]
- Regier D A, Hirschfeld R M A, Goodwin F K, Burke J D, Jr., Lazar J B, Judd L L. “The NIMH Depression Awareness, Recognition, and Treatment Program: Structure, Aims, and Scientific Basis.”. American Journal of Psychiatry. 1988;145(11):1351–7. doi: 10.1176/ajp.145.11.1351. [DOI] [PubMed] [Google Scholar]
- Regier D A, Narrow W E, Rae D S, Manderscheid R W, Locke B Z, Goodwin F K. “The De Facto U.S. Mental Health and Addictive Disorders Service System: Epidemiologic Catchment Area Prospective One-Year Prevalence Rates of Disorders and Services.”. Archives of General Psychiatry. 1993;50(2):85–94. doi: 10.1001/archpsyc.1993.01820140007001. [DOI] [PubMed] [Google Scholar]
- Research Triangle Institute. Cary, NC: Research Triangle Institute; 2000. SUDAAN statistical software (release 7.5.6) [Google Scholar]
- Ridgely M S, Goldman H H. “Mental Health Insurance.”. In: Rochefort D A, editor. Handbook on Mental Health Policy in the United States. Westport, CT: Greenwood; 1989. [Google Scholar]
- Rogler L H, Cortes D E. “Help-Seeking Pathways: A Unifying Concept in Mental Health Care.”. American Journal of Psychiatry. 1993;150(4):554–61. doi: 10.1176/ajp.150.4.554. [DOI] [PubMed] [Google Scholar]
- Ross J. “Social Phobia: The Consumer's Perspective.”. Journal of Clinical Psychiatry. 1993;54:5–9. [PubMed] [Google Scholar]
- Sherbourne C D. “The Role of Social Support and Life Stress Events in Use of Mental Health Services.”. Social Science and Medicine. 1988;27(12):1373–7. doi: 10.1016/0277-9536(88)90205-5. [DOI] [PubMed] [Google Scholar]
- Taube C A, Rupp A. “The Effect of Medicaid on Access to Ambulatory Mental Health Care for the Poor and Near-Poor under 65.”. Medical Care. 1986;24(8):677–86. doi: 10.1097/00005650-198608000-00003. [DOI] [PubMed] [Google Scholar]
- Temkin-Greener H, Clark K T. “Ethnicity, Gender, and Utilization of Mental Health Services in a Medicaid Population.”. Social Science and Medicine. 1988;26(10):989–96. doi: 10.1016/0277-9536(88)90216-x. [DOI] [PubMed] [Google Scholar]
- Velicer W F, Hughes S L, Fava J L, Prochaska J O, DiClemente C C. “An Empirical Typology of Subjects within Stage of Change.”. Addictive Behaviors. 1995;20(3):299–320. doi: 10.1016/0306-4603(94)00069-b. [DOI] [PubMed] [Google Scholar]
- Wang P S, Berglund P A, Kessler R C. “Recent Care of Common Mental Disorders in the U.S. Population: Prevalence and Conformance with Evidence-Based Recommendations.”. Journal of General Internal Medicine: Official Journal of the Society for Research and Education in Primary Care Internal Medicine. 2000;15(5):284–92. doi: 10.1046/j.1525-1497.2000.9908044.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang P S, Demler O V, Kessler R C. “The Adequacy of Treatment for Serious Mental Illness in the United States.”. American Journal of Public Health. 2002;92(1):92–8. doi: 10.2105/ajph.92.1.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weaver A J. “Has There Been a Failure to Prepare and Support Parish-Based Clergy in Their Role as Frontline Community Mental Health Workers? A Review.”. Journal of Pastoral Care. 1995;49(2):129–47. doi: 10.1177/002234099504900203. [DOI] [PubMed] [Google Scholar]
- Wells K B, Burnam M A, Camp P. “Severity of Depression and Fee-for-Service General Medical and Mental Health Specialty Practices.”. Medical Care. 1995;33(4):350–64. doi: 10.1097/00005650-199504000-00003. [DOI] [PubMed] [Google Scholar]
- Wells K B, Golding J M, Hough R L, Burnham A, Karno M. “Factors Affecting the Probability of Use of General and Medical Health and Social/Community Services for Mexican Americans and Non-Hispanic Whites.”. Medical Care. 1988;26(5):441–52. doi: 10.1097/00005650-198805000-00001. [DOI] [PubMed] [Google Scholar]
- Wells K B, Sherbourne C D, Schoenbaum M, Duan N, Meredith L, Unutzer J, Miranda J, Carney M F, Rubenstein L U. “Impact of Disseminating Quality Improvement Programs for Depression in Managed Primary Care: A Randomized Controlled Trial.”. Journal of the American Medical Association. 2000;283(2):212–20. doi: 10.1001/jama.283.2.212. [DOI] [PubMed] [Google Scholar]
- Wittchen H-U. “Reliability and Validity Studies of the WHO-Composite International Diagnostic Interview (CIDI): A Critical Review.”. Journal of Psychiatric Research. 1994;28(1):57–84. doi: 10.1016/0022-3956(94)90036-1. [DOI] [PubMed] [Google Scholar]
- Wittchen H-U, Kessler R C, Zhao S, Abelson J. “Reliability and Clinical Validity of UM-CIDI DSM-III-R Generalized Anxiety Disorder.”. Journal of Psychiatric Research. 1995;29(2):95–110. doi: 10.1016/0022-3956(94)00044-r. [DOI] [PubMed] [Google Scholar]
- Wittchen H-U, Zhao S, Abelson J M, Abelson J L, Kessler R C. “Reliability and Procedural Validity of UM-CIDI DSM-III-R Phobic Disorders.”. Psychological Medicine. 1996;26(6):1169–77. doi: 10.1017/s0033291700035893. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Composite International Diagnostic Interview (CIDI), Version 1.0. Geneva, Switzerland: World Health Organization; 1990. Version 1.0. [Google Scholar]