Abstract
Objective
To estimate the magnitude and age distribution of lifetime health care expenditures.
Data Sources
Claims data on 3.75 million Blue Cross Blue Shield of Michigan members, and data from the Medicare Current Beneficiary Survey, the Medical Expenditure Panel Survey, the Michigan Mortality Database, and Michigan nursing home patient counts.
Data Collection
Data were aggregated and summarized in year 2000 dollars by service, age, and gender.
Study Design
We use life table models to simulate a typical lifetime's distribution of expenditures, employing cross-sectional data on age- and sex-specific health care costs and the mortality experience of the population. We determine remaining lifetime expenditures at each age for all initial members of a birth cohort. Separately, we calculate remaining expenditures for survivors at all ages. Using cross-sectional data, the analysis holds disease incidence, medical technology, and health care prices constant, thus permitting an exclusive focus on the role of age in health care costs.
Principal Findings
Per capita lifetime expenditure is $316,600, a third higher for females ($361,200) than males ($268,700). Two-fifths of this difference owes to women's longer life expectancy. Nearly one-third of lifetime expenditures is incurred during middle age, and nearly half during the senior years. For survivors to age 85, more than one-third of their lifetime expenditures will accrue in their remaining years.
Conclusions
Given the essential demographic phenomenon of our time, the rapid aging of the population, our findings lend increased urgency to understanding and addressing the interaction between aging and health care spending.
Keywords: Health care costs, lifetime expenditure, survivors' expenditures, decedents' expenditures
The distribution of health care costs is strongly age dependent, a phenomenon that takes on increasing relevance as the baby boom generation ages. After the first year of life, health care costs are lowest for children, rise slowly throughout adult life, and increase exponentially after age 50 (Meerding et al. 1998). Bradford and Max (1996) determined that annual costs for the elderly are approximately four to five times those of people in their early teens. Personal health expenditure also rises sharply with age within the Medicare population. The oldest group (85+) consumes three times as much health care per person as those 65–74, and twice as much as those 75–84 (Fuchs 1998). Nursing home and short-stay hospital use also increases with age, especially for older adults (Liang et al. 1996).
While the general implications of aging for health care costs are widely appreciated, most of our knowledge of the subject derives from cross-sectional investigation of age-specific expenditures (Waldo et al. 1989; Mustard et al. 1998) or longitudinal studies that follow a cohort as its members age (Lubitz and Riley 1993; Lubitz, Beebe, and Baker 1995; Spillman and Lubitz 2000). The cross-sectional studies do not reflect single individuals' life expectancies, as these studies mix the birth cohorts that comprise the current population. The longitudinal studies risk confounding the effects of age with changes over time in health care prices, medical techniques and technology, and even the incidence of disease and effectiveness of treatment. The present study approaches the issue of the age-specific distribution of health care expenditures from a different perspective, one that considers the distribution of expenditures over the major phases of a single person's lifetime while holding everything other than age constant. To achieve this, we construct a hypothetical individual, one whose probability of being alive at each age comes from a current life table, while his or her age-specific medical expenditures derive from cross-sectional data on age-specific spending in a single year. That is, we assign a single year's age-specific costs to our hypothetical individual at each age, multiplying each age's cost by the probability that the individual will be alive at that age. This permits us to characterize a typical lifetime of medical expenditures in a constant health care environment (i.e., a fixed price of health care services, a fixed armamentarium of medical technology and practices, and a given incidence and natural history of disease). By so doing, this method allows us to compare, for example, how much is spent on our hypothetical individual during childhood, when annual health care expenditures are low but survival probability is high, with how much is spent during the individual's elderly years, when annual costs are high but survival probability substantially diminished.
In addition to the inherent interest of this exercise, we hope that it will enrich the thus far modest literature on the subject of the distribution of health care costs over a typical lifetime, and better inform societal planning for dealing with an aging population. In the process of performing the analysis, as explained below, we evaluate the age-specific impact of differences in expenditures on decedents and survivors. We also examine how much of women's greater lifetime expenditures are attributable to their longer life expectancy.
Methods
To estimate lifetime health care costs, we employ a method based on a current life table, also known as a period life table model (Namboodiri and Schindran 1987; Shryock et al. 1971). We use a single year's per capita health care expenditure data and the mortality experience of a population, differentiated by age and sex, to generate profiles of health care expenditure from birth to death. By determining average expenditures at each age, for each sex, and for decedents and survivors, we create an estimated lifetime distribution of health care expenditures, conceptually converting these cross-sectional expenditures into a longitudinal pattern of expenditure for a contemporary birth cohort. This steady-state perspective is tantamount to assuming that technology, price, and the prevalence, incidence, and natural history of diseases does not vary over the lifetime of an individual born today. Holding these variables constant avoids confounding age differences in expenditures with system changes over time.
A period life table starts out with the “birth” of 100,000 hypothetical persons to whom current age-specific death rates are applied. The life table thus shows the mortality experience of a hypothetical group of infants born at the same time and subject throughout their lifetime to the age-specific mortality rates observed in the current period. We use Michigan vital statistics and population databases to determine 1997 age- and sex-specific mortality rates and population estimates to create the life table (Alemayehu 2001).
Per Capita Health Care Expenditure
We calculate total medical care expenditures using data on direct costs paid by private third-party payers, Medicare, patients themselves, through copays and deductibles, and Medicaid for its contributions to nursing home expenditures. We divide the population into age and sex subgroups and calculate the average expenditure for each. Expenditure categories include facility services (hospital and nursing home), professional services, prescription drugs, dental care, vision care, and hearing services.
We rely primarily on two sources for data on health care expenditures: Blue Cross Blue Shield of Michigan (BCBSM) 1997 claims and membership databases and the 1995 Medicare Current Beneficiary Survey (MCBS) database (Health Care Financing Administration 2001). (See Table 1 for a description of sources of data for all expenditure categories.) We match the Michigan Mortality Database with the BCBSM claims database to estimate decedents' expenditures, to compare them with those of each age's survivors. In all cases, we convert earlier years' expenditure estimates to year 2000 dollars using the medical care component of the Consumer Price Index (CPI) (U.S. Office of Management and Budget 2002). For nursing home expenditure, we employ Medical Expenditure Panel Survey (MEPS) data, adjusted to avoid double counting of the partial coverage of nursing home expenditures by BCBSM and Medicare (Rhodes and Sommers 2000). As a proxy for out-of-pocket payments, we use BCBSM members' copays and deductibles from the BCBSM database. (This is described in more detail later.)
Table 1.
Types of Expenditure and Sources of Data
| Type of Expenditure | Source* |
|---|---|
| Facility services (excluding nursing home)** | |
| Age<65 | BCBSM |
| Age≥65 | BCBSM, MCBS |
| Nursing home care** | |
| Age<65 | MEPS and Michigan nursing home data on age-sex distribution |
| Age≥65 | MEPS |
| Professional services | |
| Age<65 | BCBSM |
| Age≥65 | BCBSM, MCBS |
| Drug, dental, vision and hearing services | BCBSM for members with coverage (Same values assumed for members without coverage) |
| Out-of-pocket | BCBSM (co-pay and deductible) |
BCBSM = Blue Cross Blue Shield of Michigan; MCBS = Medicare Current Beneficiary Survey; MEPS = Medical Expenditure Panel Survey.
To differentiate decedents' and survivors' expenditures for facility services, we matched data from the BCBSM claims database and the Michigan Mortality Database for persons<65 years old. For persons ≥ 65, we used the decedent/survivor ratios from Lubitz and Riley (1993).
Almost all BCBSM members have facility coverage, and almost all of these have professional services covered as well. For covered BCBSM members under the age of 65, we aggregate their BCBSM payments for each of facility and professional services for each age and sex group. To this we add members' copays and deductible payments. We then divide each age-and-sex total expenditure by the number of members in the age and sex group to estimate their per capita facility and professional services expenditures.
For facility and professional services for members with Medicare complementary coverage, we estimate Medicare payments by taking age- and sex-specific per capita data on national Medicare expenditures from the MCBS database and multiplying it by the number of BCBSM members with Medicare complementary coverage. To this we add these members' BCBSM facilities and professional services expenditures and their copay and deductible payments. Again, we divide by age- and sex-specificmembershipnumbers to derive estimates of per capita spending on facilities and professional services.
Of BCBSM members with facility and professional service coverage, 71 percent have drug coverage but only a minority is covered for vision (14 percent), hearing (37 percent), and dental (15 percent) services. Members lacking these coverages through BCBSM may be covered through other carriers or pay for the services out-of-pocket. Lacking data on other coverage, we must estimate their expenditures in each of these expenditure categories. To do so, we determine aggregate expenditures on each of drugs, dental, vision, and hearing by age and sex from the BCBSM claims database. To these totals we add copays and deductibles. These aggregate quantities are then divided by the age- and sex-specific membership count in their respective service categories to determine the annual per capita expenditure of BCBSM members. We treat these estimates as applying to all individuals, whether or not they have BCBSM coverage. Implicitly, this approach assumes that BCBSM members who do not have BCBSM drug, dental, vision, or hearing coverage will pay the same amount for these services, through other carriers or out-of-pocket, as do BCBSM members who do have the coverage. This could overestimate total and per capita expenditures, since less-well-insured individuals might be expected to spend less on these areas of health care service. However, this has little potential impact on our aggregate estimates. Further, as discussed below, our analysis produced overall per capita expenditure estimates very close to estimates of national per capita expenditures produced by the Health Care Financing Administration (HCFA).
To break down the facility services into hospital and nursing home expenditures, we follow two distinct procedures for patients younger than 65 and those 65 and older. For the latter, we use the MEPS age- and sex-specific per capita nursing home expenditure data (Rhodes and Sommers 2000). We then apply MEPS data on the source of payment, by age and sex, to the aggregate figures to estimate the per capita amount paid by Medicare and private insurance. This amount is already included in our facility expenditure estimates, as described above. Thus, we remove this amount—the nursing home share—from the facility estimate to generate our estimate of hospital expenditures (the residual amount). (Our facility estimates include hospital costs and nursing home expenditures covered by BCBSM and Medicare only. The procedure described here permits us to isolate the nursing home share and thus distinguish the hospital-only component of facility expenditures.)
According to the MEPS report, nursing home patients younger than 65 constitute 9 percent of the nursing home population and 0.1 percent of the total population under age 65. The MEPS estimates the aggregate number of nursing home residents under age 65 and their average expenditure by sex. We assume that these expenditure estimates apply to all ages under 65. To determine the number of nursing home patients in our BCBSM membership, we apply the 2000 Michigan nursing home resident age and sex distribution for persons under age 65 (provided by Brant Fries of the University of Michigan's Institute of Gerontology, June 2001) to the BCBSM age-specific populations. As with the data on seniors, we use the MEPS data on proportions of nursing home expenditures paid by Medicare and private insurance to isolate the component of our facility expenditure estimates that should be attributed to nursing home care. For both younger patients and seniors, we convert earlier years' expenditure estimates into year 2000 dollars by employing the medical care component of the CPI, as noted above.
Per Capita Lifetime Expenditure for the Average Life Table Person
The per capita lifetime expenditure at a given age a, projected from birth b (LEb,a), estimates the lifetime expenditure remaining after age a for the average “life table person” at birth. Implicit in this conception is the fact that some members of the original cohort of 100,000 people will have died before this age a, but they are still counted in the denominator (hence the projection from birth). We calculate LEb,a by dividing the aggregate lifetime expenditure of the remaining cohort at age a by the size of the original birth cohort (100,000). Using standard demographic notation,
where
Lx=the person years lived by the cohort in the age interval (x, x+1)
Cx=per capita expenditure at age x (x=0,1,2,3,…..,95+).
Relative lifetime spending at age a, RLEb,a, is the proportion of total lifetime expenditure, calculated from birth, incurred by the average life table person after age a. RLEb,a equals LEb,a divided by LEb,0, the latter representing total lifetime expenditures for the average member of the birth cohort. RLEb,a is interpreted as follows: If RLEb,65=50 percent, half of the average cohort member's total lifetime expenditures will result from health care utilized during or after age 65. This is equivalent to saying that half of the entire cohort's lifetime expenditures will result from health care utilized during or after age 65.
Per Capita Lifetime Expenditure for Survivors
The per capita lifetime expenditure for survivors (s) at a given age a (LEs,a) estimates the remaining lifetime expenditure of an individual who has survived to age a. For LEs,a, the denominator is the number of cohort members alive at age a, rather than the total size of the birth cohort used in calculating LEb,a. By definition, therefore, LEs,a is always greater than LEb,a, by virtue of measuring the same total annual expenditures in the numerator but having a smaller denominator (except at birth).
where
Lx and Cx are defined as above and
la=the number alive at the beginning of the age interval (a, a+1)
The relative lifetime spending of survivors at any age a, RLEs,a is the proportion or fraction of total lifetime expenditure, calculated from birth, incurred after age a by the average life table person surviving to age a. It is calculated by dividing LEs,a by LEas,0, the latter representing total lifetime expenditures for the average member of the birth cohort still alive at age a, measured from birth. If RLEs,65=60 percent, for example, this means that three-fifths of the total lifetime expenditures of the average cohort member who has survived to age 65 will result from health care utilized after that age.
To calculate LEas,0 we must adjust annual per capita expenditures to reflect differences between survivors' and decedents' expenses to age a. In the year of their deaths, decedents have a much higher expenditure than survivors. To accomplish this adjustment, we employ a decedent–survivor ratio of medical expenditures, wi, calculated from BCBSM data comparing survivors' and decedents' expenditures from birth through age 64 (Alemayehu 2001) and from data presented by Lubitz and Riley (1993) concerning the Medicare population. We derive the lifetime expenditure of survivors at each age from the fact that, at each age i, decedent per capita expenditure =wi×survivor per capita expenditure. Application of this ratio reduces survivors' age- and sex-specific expenditures by an amount reflecting the extra expenditures associated with death care. That decedents' expenditures considerably exceed those of survivors is seen in the values of the wi ratios, which are huge for young children (56.1 for 1–10 year olds) and decline with age. (Representative values are 19.2 for 40–49 year olds, 10.6 for the youngest senior citizens, ages 65–69, and 3.9 for the oldest seniors, ages ≥ 90.)
RLEs,a necessarily exceeds RLEb,a, reflecting the exclusion of decedents' higher medical costs from the surviving cohort's expenditures to age a. By virtue of having survived to age a, and the fact that expenditures grow with age, a larger proportion of this group's lifetime expenditures lies ahead of them (including, of course, their own terminal illness care).
Results
Per Capita Lifetime Expenditure for the Average Life Table Person
The average member of the birth cohort will spend $316,579 in 2000 dollars over the course of his or her life. Of this total, 45.1 percent will be devoted to facility services (hospitalization, 32.8 percent, and nursing home stays, 12.3 percent), followed by professional (26.6 percent), drug (16.3 percent), dental (9.9 percent), and vision/hearing (2.1 percent) services. Total lifetime expenditure is 34 percent higher for females ($361,192) than males ($268,679) (Table 2).
Table 2.
Lifetime Per Capita Expenditure at Birth, Adjusted and Unadjusted Male–Female Differences by Type of Service (Year 2000 Dollars)
| (1) Types of Services | (2) Total | (3) Female | (4) Male | (5) Male Adjusted for Female's Life Expectancy | (6) Differences Explained by Female's Longer Life Expectancy (5-4)/(3-4) |
|---|---|---|---|---|---|
| Total | $316,579 | $361,192 | $268,679 | $305,281 | 39.6% |
| Facility (Cross+Nursing Home) | $142,777 | $166,045 | $117,116 | $139,318 | 45.4% |
| Hospital (Facility less Nursing Home) | $103,562 | $114,065 | $92,735 | $104,561 | 55.4% |
| Nursing Home | $39,215 | $51,980 | $24,381 | $34,757 | 37.6% |
| Professional (Shield) | $84,192 | $95,945 | $71,897 | $79,929 | 33.4% |
| Prescription Drug | $51,703 | $58,858 | $44,304 | $48,931 | 31.8% |
| Dental | $31,250 | $33,141 | $29,307 | $31,930 | 68.4% |
| Vision/Hearing | $6,648 | $7,203 | $6,055 | $6,826 | 67.1% |
One obvious reason for females' greater expenditures is their 8 percent longer life expectancy than that of men, 79.4 versus 73.6 years in 2000 (Michigan Department of Community Health 2002). To determine how much of the expenditure excess is attributable to women's longer lives, we recalculate males' lifetime per capita expenditure by applying females' survival experience to the male cohort age-specific expenditures. If men lived as long as women, male lifetime expenditure would rise by $36,600 (14 percent) to $305,281 (Table 2). Thus, 40 percent of the overall difference between female and male expected lifetime expenditure is attributable to female's longer life expectancy. As seen in column 6 of Table 2, close to half (45 percent) of the difference in facility services expenditures owes to women's greater longevity, with life expectancy more important in explaining differences in hospital costs (55 percent of the difference attributable to life expectancy) than nursing home expenditures (38 percent). Fully two-thirds of women's greater lifetime expenditures on dental care and vision/hearing services reflect their longer lives, while only one-third of professional service and prescription drug differences is so explained.
Note that these percentages would vary somewhat had we asked how much of the male–female lifetime expenditure difference would be explained if women lived only as long as men do today (i.e., recalculating females' lifetime per capita expenditure by applying males' shorter survival experience to the female cohort age-specific expenditures). If women's life expectancy fell to that of men, women's total per capita lifetime expenditure would drop from $361,192 to $317,296. With this alternative formulation of the question, 47.4 percent of the total difference in male–female lifetime expenditures would be explained by women's greater longevity.
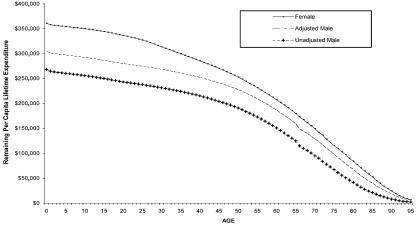
Figure 1 demonstrates the anticipated pattern of the gender difference in overall expenditures, showing female expenditures and male expenditures both unadjusted (i.e., reflecting their shorter life expectancy) and adjusted (as if they lived as long as women do). The difference is greatest through the childbearing years and then diminishes continuously thereafter. From early middle age onward, women's greater longevity explains more than half of their greater total expenditures, with the dominance of that explanation increasing as the cohort ages.
Figure 1.
Remaining Lifetime Per Capita Expenditure by Age, Male versus Female, with/without Adjustment for Female's Longer Life Expectancy (Year 2000 Dollars)
Tables 3 and 4 present per capita lifetime health care expenditure (Table 3) and relative lifetime expenditure (Table 4), at various ages, for both the average life table person and for survivors. For the average life table member, only a fifth of all lifetime expenditures occurs during the first half of life (79.6 percent of expenditures remaining after age 40), while nearly half (48.6 percent) accrues after age 65 (Table 3, column 4). By subtracting the percentage of remaining expenditures at a given age from those remaining at an earlier age, one can assess the proportion of lifetime expenditures incurred in that age range. Thus, 7.8 percent of a cohort's expenditures occurs during the first quarter of life, through childhood (to age 20); an eighth (12.5 percent) is realized during young adulthood, ages 20–39; nearly a third (31 percent) accrues during middle-age (40–64); and nearly half (48.6 percent) is expended during the post-65 years. Three-quarters of those senior citizen expenditures, or 36.5 percent of the lifetime total, accrue during the first two decades. Expenditures on behalf of the nation's oldest citizens, ages ≥85, account for an eighth (12.1 percent) of all lifetime expenditures (Table 4, column 2).
Table 3.
Age-Specific Annual and Lifetime Per Capita Expenditure, Life Table Cohort, and Survivors (Year 2000 Dollars)
| Life Table Cohort | Survivors | |||||
|---|---|---|---|---|---|---|
| (1) Age | (2) Annual Per Capita Expenditure | (3) Lifetime Per Capita Expenditure (LEba) | (4) Relative Lifetime Expenditure (RLEba) | (5) Annual Per Capita Expenditure | (6) Lifetime Per Capita Expenditure (LEsa) | (7)Relative Lifetime Expenditure (RLEsa) |
| 0 | $3,432 | $316,579 | 100.0% | $2,920 | $316,579 | 100.0% |
| 20 | $1,448 | $291,745 | 92.2% | $1,255 | $296,363 | 93.6% |
| 40 | $2,601 | $252,082 | 79.6% | $1,929 | $262,124 | 82.8% |
| 65 | $10,245 | $153,944 | 48.6% | $7,702 | $188,658 | 59.6% |
| 85 | $17,071 | $38,400 | 12.1% | $7,688 | $113,685 | 35.9% |
Table 4.
Relative Lifetime Per Capita Expenditure at Different Age Intervals, Life Table Cohort, and Survivors (Year 2000 Dollars)
| (1) Relative Lifetime Expenditure During | (2) Life Table Cohort | (3) Survivors |
|---|---|---|
| Childhood (0–19) | 7.8% | 6.4% |
| Young adult (20–39) | 12.5% | 10.8% |
| Middle-aged adult (40–64) | 31.0% | 23.2% |
| Senior years (65–84) | 36.5% | 23.7% |
| Old senior years (85+) | 12.1% | 35.9% |
Per Capita Lifetime Expenditure for Survivors
For survivors' expenditures, adjustments for decedents' higher expenditures make little difference during the first half of life (through age 40), given that so little mortality occurs during the first four decades. For example, 40-year-old survivors have experienced just under a fifth of their lifetime expenditures, with 82.8 percent of their expenditures lying in the future (Table 3, column 7). At age 40, the average life table person (including both survivors and decedents) has consumed just over a fifth, with 79.6 percent of expenditures awaiting the future (column 4).
From ages 40 to 65, however, survivors expend under a quarter (23.2 percent) of their lifetime total (Table 4, column 3), compared with 31.0 percent for the cohort as a whole (column 2). From ages 65 to 85, survivors utilize 23.7 percent of their lifetime medical expenditures, while the average life table person consumes 36.5 percent. For those who survive to age 85, more than a third (35.9 percent) of their lifetime expenditures lies in the future. For the cohort as a whole, having lost the majority of its members before age 85, only an eighth of lifetime expenditures (12.1 percent) remains during later years. That the differences rise with age, becoming quite dramatic for the oldest ages, simply reflects the diminishing probabilities of reaching each of these older ages.
Discussion
The findings of this study reinforce and extend knowledge of age-specific health care costs. The basic distribution of expenditures reported here—high during infancy, low during childhood, and rising thereafter, especially during the senior years—is familiar both from previous research and from common understanding of age-specific health care utilization patterns. Our method of deriving this distribution, however, is novel and offers refined insight into age-specific costs by virtue of its life table analysis of cross-sectional data, used to construct a hypothetical “lifetime.” Unlike most previous research, which has employed longitudinal data, this study's reliance on cross-sectional data permits exclusive focus on the effects of age on health care costs; in this analysis, health care technology and price, and the incidence, severity, and outcomes of disease are held constant. An implication concerning the aging of the population is considered later. As well, the survivor expenditure analysis lends new insight into the implications of aging, highlighting the remarkable concentration of survivors' lifetime costs in their senior years, also noted further later.
By relying on data from Michigan, we cannot claim that our findings are truly representative of the experience of Americans as a whole. We believe that they are an excellent approximation of the national health care cost experience, however. We used BCBSM rather than the nationally representative MEPS data for several reasons, including the unavailability of MEPS at the time this project began. Moreover, when MEPS data became available, we ascertained that the expenditures it covers considerably underestimated national personal health expenditures as estimated by HCFA. Further, the Michigan data permitted us to match mortality data to health care cost data. Note that our resulting estimates of personal health care expenditures closely approximate national estimates produced by HCFA ($4,003 and $4,034, respectively, in 2000 dollars—Health Care Financing Administration 2002). As well, as we indicate below, our estimate of the lifetime expenditures of senior citizens is virtually identical to that of Spillman and Lubitz (2000). Thus, for the purposes of this study, we are confident that any differences between the average American's health care cost experience and that of the average resident of Michigan are not qualitatively important.
Although we were able to estimate the role of females' longevity on their greater lifetime expenditures, our age-specific expenditure data did not come with diagnostic codes. Thus, the data did not permit us to assess the other obvious source of male–female difference: pregnancy and the childbirth process. Presumably, much of the male–female difference in expenditures during the reproductive years is attributable to pregnancy and childbirth. Using different methods, Mustard et al. (1998) concluded that differences in mortality-related expenditures combined with women's sex-specific health care conditions account for nearly all of the male–female difference.
Further research should investigate the role of serious illness and death in the age distribution of medical expenditures, as well as how these costs play out over the lifetime: are the much larger costs of decedents manifested primarily in acute or chronic care, in hospitalization or nursing home care? Do the answers to these questions vary systematically by age? The nature of these relationships is less clear than is the distribution of health care costs itself. Scitovsky (1988) argued that both the elderly and persons who die consume a disproportionate share of medical resources. Roos (1987) found that people dying at older ages have more expensive deaths than people dying at earlier ages, attributing much of the excess to heavy nursing home use by the very elderly. Spillman and Lubitz (2000) estimated that total expenditures from the age of 65 years until death increase substantially with longevity, from $36,000 for persons who die at the age of 65 to more than $230,000 for those who die at the age of 90, in part because of steep increases in nursing home expenditures for very old persons. (We have inflated Spillman and Lubitz's published estimates, given in 1996 dollars, to year 2000 dollars, using the medical care component of the CPI.)
Nursing home expenditures clearly play an important role in total expenditures on the elderly, as is seen in a study that omitted them. Based on a sample of patients in a medical center, Temkin-Greener et al. (1992) concluded that decedents' medical care expenditures, excluding nursing home, declined with an increasing age at death. In another study restricted to geriatric patients, Dunlop et al. (1993) and Chelluri et al. (1993) demonstrated that severity of illness was more important than age in predicting use of medical resources. Clearly, the complex relationship among care for decedents, age, and overall medical expenditure needs to be better elucidated.
Our finding that the typical American spends more than $300,000 over a lifetime lends perspective on the enormity of our investment in medical services. The lifecycle timing of the bulk of those expenditures gives special pause, in light of the essential demographic phenomenon of our time: the aging of the population. We find that almost 60 percent—$188,658—of the total lifetime cost of survivors is spent after age 65, a figure identical to Spillman and Lubitz's (2000) post-65 estimate of $188,903 (again inflating their figure to year 2000 dollars). Especially striking is our finding that well over one-third of the average 85-year-old's expenditures lies in that person's future.
Given the disproportionate share of medical resources supporting the elderly, analysis of growth in spending by age is crucial in forecasting medical costs as society ages (Lubitz, Beebe, and Baker 1995). Clearly, it is essential in planning the future of government programs like Medicare and Medicaid. The number of people 65 and older is projected to grow from 13 percent of the population today to 20 percent by the year 2030 (U. S. Census Bureau 2000). The population of the “old-old” (85+) will quadruple over the next few decades as the large baby boomer cohort reaches these advanced ages (Waite 1996). Old-age health care costs thus will impose increasingly severe pressure on private finances and government coffers. Indeed, applying our age-specific estimates to the age distribution anticipated for the year 2030, we find that if nothing is done to alter current patterns of health care, per capita health care expenditures will rise by one-fifth due to population aging alone (calculations not shown; available from authors upon request).
A series of social and public policy changes must begin soon to meet this challenge (Knickman and Snell 2002). Hardly a novel conclusion; the extent of the challenge and the need to plan for it are thrown into stark relief by the findings reported here.
References
- Alemayehu B. Doctoral dissertation. Ann Arbor: University of Michigan; 2001. “The Lifetime Distribution of Healthcare Costs.”. [Google Scholar]
- Bradford D F, Max D A. Cambridge, MA: National Bureau of Economic Research; 1996. “Implicit Budget Deficits: The Case of a Mandated Shift to Community-Rated Health Insurance.”. NBER working paper no. 5514. [Google Scholar]
- Chelluri L, Pinsky M R, Donahoe M P, Grenvik A. “Long-term Outcome of Critically Ill Elderly Patients Requiring Intensive Care.”. Journal of the American Medical Association. 1993;269(24):3119–23. [PubMed] [Google Scholar]
- Dunlop W E, Rosenblood L, Lawrason L, Birdsall L, Rusnak C H. “Effects of Age and Severity of Illness on Outcome and Length of Stay in Geriatric Surgical Patients.”. American Journal of Surgery. 1993;165(5):577–80. doi: 10.1016/s0002-9610(05)80438-6. [DOI] [PubMed] [Google Scholar]
- Fuchs V. Cambridge, MA: National Bureau of Economic Research; 1998. “Provide, Provide: The Economics of Aging.”. NBER working paper no. 6642. [Google Scholar]
- Health Care Financing Administration. “MCBS overview”. [accessed on October 10, 2001]. Available at http://www.hcfa.gov/surveys/mcbs/DFDesc.htm. [Google Scholar]
- Health Care Financing Administration. “National Health Expenditure Tables”. [accessed on July 7, 2002]. Personal Healthcare Expenditures Aggregate and Per Capita Amounts and Percent Distribution, by Source of Funds: Selected Calendar Years 1980-2000. (Table 4.) Available at http://www.hcfa.gov/stats/nhe-oact/tables/t4.htm. [Google Scholar]
- Knickman J R, Snell E K. “The 2030 Problem: Caring for Aging Baby Boomers.”. Health Services Research. 2002;37(4):849–84. doi: 10.1034/j.1600-0560.2002.56.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang J, Liu X, Tu E, Whitelaw N. “Probabilities and Lifetime Durations of Short-Stay Hospital and Nursing Home Use in the United States, 1985.”. Medical Care. 1996;34(10):1018–36. doi: 10.1097/00005650-199610000-00004. [DOI] [PubMed] [Google Scholar]
- Lubitz J, Beebe J, Baker C. “Longevity and Medicare Expenditures.”. New England Journal of Medicine. 1995;332(15):999–1003. doi: 10.1056/NEJM199504133321506. [DOI] [PubMed] [Google Scholar]
- Lubitz J D, Riley G F. “Trends in Medicare Payments in the Last Year of Life.”. New England Journal of Medicine. 1993;328(15):1092–6. doi: 10.1056/NEJM199304153281506. [DOI] [PubMed] [Google Scholar]
- Meerding W J, Bonneux L, Polder J J, Koopmanschap M A, van der Maas P J. “Demographic and Epidemiological Determinants of Healthcare Costs in Netherlands: Cost of Illness Study.”. British Medical Journal. 1998;317(7151):111–5. doi: 10.1136/bmj.317.7151.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michigan Department of Community Health. “Life-Expectancy: Michigan and United Sates”. [accessed on July 7, 2002]. Available at http://www.mdch.state.mi.us/pha/osr/deaths/lifeUSMI.asp. [Google Scholar]
- Mustard C A, Kaufert P, Kozyrskyj A, Mayer T. “Sex Differences in the Use of Healthcare Services.”. New England Journal of Medicine. 1998;338(23):1678–83. doi: 10.1056/NEJM199806043382307. [DOI] [PubMed] [Google Scholar]
- Namboodiri K, Schindran C. Life Table Techniques and Their Applications. New York: Academy Press; 1987. [Google Scholar]
- Rhodes J, Sommers J. Expenses and Sources of Payment for Nursing Home Residents, 1996. Rockville, MD: Association for Healthcare Research and Quality; 2000. MEPS Research Findings no.13. AHRQ publication no. 01-0010. [Google Scholar]
- Roos N P, Montgomery P, Roos L L. “Healthcare Utilization in the Years prior to Death.”. Milbank Quarterly. 1987;65(2):231–54. [PubMed] [Google Scholar]
- Scitovsky A A. “Medical Care in the Last Twelve Months of Life: The Relation between Age, Functional Status, and Medical Care Expenditures.”. Milbank Quarterly. 1988;66(4):640–60. [PubMed] [Google Scholar]
- Shryock H S, Siegel J S, Larmon E A. The Methods and Materials of Demography. vol. 2. Washington, DC: U.S. Bureau of the Census; 1971. [Google Scholar]
- Spillman B C, Lubitz J. “The Effect of Longevity on Spending for Acute and Long-term Care.”. New England Journal of Medicine. 2000;342(19):1409–15. doi: 10.1056/NEJM200005113421906. [DOI] [PubMed] [Google Scholar]
- Temkin-Greener H, Meiners M R, Petty E A, Szydlowski J S. “The Use and Cost of Health Services Prior to Death: A Comparison of the Medicare-Only and the Medicare–Medicaid Elderly Population.”. Milbank Quarterly. 1992;70(4):679–701. [PubMed] [Google Scholar]
- U.S. Census Bureau. Projections of the Total Resident Population by Five-Year Age Groups and Sex with Special Age Categories (NP-T3-A) Washington, DC: Population Projections Program, Population Division, U.S. Census Bureau; 2000. [Google Scholar]
- U.S. Office of Management and Budget. “Consumer Price Index for Major Expenditure Classes, 1958–2000 (Table B-60)”. [accessed on July 7, 2002]. Available at http://w3.access.gpo.gov/usbudget/fy2002/erp.html. [Google Scholar]
- Waldo D R, Sonnefeld S T, McKusick D R, Arnett R H. “Health Expenditures by Age Group, 1977 and 1987.”. Health Care Financing Review. 1989;10(4):111–20. [PMC free article] [PubMed] [Google Scholar]
- Waite L. “The Demographic Face of America's Elderly.”. Inquiry. 1996;33(3):220–4. [PubMed] [Google Scholar]