Abstract
Objective
To determine the relationship between hospital membership in systems and the treatments, expenditures, and outcomes of patients.
Data Sources
The Medicare Provider Analysis and Review dataset, for data on Medicare patients admitted to general medical-surgical hospitals between 1985 and 1998 with a diagnosis of acute myocardial infarction (AMI); the American Hospital Association Annual Survey, for data on hospitals.
Study Design
A multivariate regression analysis. An observation is a fee-for-service Medicare AMI patient admitted to a study hospital. Dependent variables include patient transfers, catheterizations, angioplasties or bypass surgeries, 90-day mortality, and Medicare expenditures. Independent variables include system participation, other admission hospital and patient traits, and hospital and year fixed effects. The five-part system definition incorporates the size and location of the index admission hospital and the size and distance of its partners.
Principal Findings
While the effects of multihospital system membership on patients are in general limited, patients initially admitted to small rural system hospitals that have big partners within 100 miles experience lower mortality rates than patients initially admitted to independent hospitals. Regression results show that to the extent system hospital patients experience differences in treatments and outcomes relative to patients of independent hospitals, these differences remain even after controlling for the admission hospital's capacity to provide cardiac services.
Conclusions
Multihospital system participation may affect AMI patient treatment and outcomes through factors other than cardiac service offerings. Additional investigation into the nature of these factors is warranted.
Keywords: Multihospital systems, hospitals, treatments, expenditures, quality
In recent years the proportion of hospitals affiliated with other hospitals has grown. In 1985, for example, 38 percent of nonpublic general medical-surgical hospitals responding to the American Hospital Association (AHA) Annual Survey identified themselves as being members of health care systems; by 1998, this percentage had grown to 66 percent. Bazzoli et al. (2001) report that in 1998, 3,221 hospitals nationwide participated in 365 health systems. Recent articles have examined multihospital systems in detail, developing a taxonomy of hospital networks and systems (Bazzoli et al. 1999), documenting changes in hospital ownership and related policy concerns (Spetz, Mitchell, and Seago 2000), and reporting on the financial performance of system hospitals (Bazzoli et al. 2000).1 Yet much remains to be understood about the nature of multihospital system membership. In particular, little is known about whether the formation of partnerships between hospitals has affected patient care. This study expands the literature on health care organizations by examining the relationship between multihospital system membership and the treatment, expenditures, and health outcomes of Medicare patients with acute myocardial infarction (AMI).
The potential motivations for joining a system are many. They include the consolidation of administrative, information processing, and purchasing functions; increased access to capital, management expertise, and medical services (through increased physician recruiting, for example); improved ability to participate in managed care contracting; expanded referral flows; and enhanced market power with respect to purchasers of hospital services. These potential goals relate to two concerns central to the administration of a hospital, and any other self-financed organization: reducing costs and increasing revenues. Previous studies have examined the influence of system membership on measures of financial performance (Bazzoli et al. 2000; Clement et al. 1997; Menke 1997; Ermann and Gabel 1986).
Hospital affiliations can affect much more than income statements and balance sheets, however. They may also affect the treatment of patients, through at least two channels. The first channel is the impact of system membership on participating hospitals' decisions to offer services, including cardiac services such as catheterizations or angioplasties. While very small hospitals are unlikely to offer these services, and large hospitals are unlikely not to offer these services, other hospitals may be on the decision-making margin. System membership may affect the offerings of these hospitals, but the direction of such an effect is unclear. Affiliations may encourage the proliferation of sophisticated services by providing the management expertise and capital to build new facilities and recruit physicians (see, e.g., Blecher 1998). Systems may also choose to replicate services across their facilities to exploit economies of promotion (Dranove and Shanley 1995). Alternatively, affiliated hospitals may choose to concentrate services in a limited number of locations to exploit economies of scale. A multihospital system might consist of a large urban hospital offering a full range of cardiac services, and several smaller suburban or rural hospitals that would refer patients in need of services to the urban facility.2
If system participation affects cardiac service offerings, it may also affect patient treatment patterns. Service offerings certainly affect the location of patient treatment; if a hospital does not offer catheterizations, for example, then the patient must be transferred to another location to receive one. But decisions about service offerings may also affect whether the patient receives a procedure at all. Previous studies have found that patients admitted to hospitals with onsite cardiac facilities are more likely to receive cardiac services (Every et al. 1993; Blustein 1993). Service proliferation would then lead to higher procedure rates, on average, among patients of system hospitals, while service concentration would lead to lower procedure rates.
By affecting the nature and location of patient treatment, service offerings may also affect patient expenditures and health outcomes. If a hospital offers few services, it would likely experience higher transfer rates, which would tend to raise expenditures, but may also experience lower procedure rates, which would tend to lower expenditures (see discussion in the Data and Methods section). A hospital that offers a full complement of services, on the other hand, would not need to transfer patients, but might tend to treat its patients more intensively. The net effect on expenditures is unclear.
The net effect of service offering decisions on patient health outcomes is also unclear. Outcomes would depend on the clinical appropriateness of the procedures provided and the expertise of the providers. For example, if service proliferation increases procedure rates, and cardiac procedures are underprovided, then service proliferation would improve patient outcomes, all else equal. On the other hand, if proliferation leads to the overprovision of services, then patient outcomes would worsen. Proliferation may also harm patients by dispersing procedure volume across multiple facilities; lower cardiac procedure volumes have been shown to be associated with worse outcomes (Grumbach et al. 1995; Phillips, Luft, and Ritchie 1995).
The second channel though which multihospital systems may affect patient treatment is improved coordination and information transfer between hospitals. In a study of AMI patients admitted to Veterans Affairs hospitals, Wright, Petersen, and Daley (1998) find that between 1988 and 1994, cardiac procedure use grew and patient survival improved most for AMI patients initially admitted to hospitals without onsite invasive cardiac services. The authors speculate that the relative growth in procedure use may be due to “improvements in system protocols for inter-hospital transfer and better inter-hospital integration.” If system hospitals face lower transaction costs in developing and implementing such protocols because of their affiliations, they may be more likely than independent hospitals to consistently use them. Protocols could lead to a greater propensity to transfer patients for treatment unavailable at the admission hospital, as well as enhance the participating hospitals' ability to complete transfers quickly. Recent studies have shown that timely transfer for primary angioplasty improves patient outcomes (Andersen et al. 2003). Protocols may also improve hospitals' ability to identify patients who do not need procedures so that they may remain at their initial admission hospital.
Systems may also increase the sharing of information among medical staffs. Soumerai et al. (1998) show that discussions and consultations with peer “opinion leaders,” combined with performance feedback, accelerated adoption of certain (nonsurgical) AMI treatments. Escarce (1996) discusses the transmission of information about procedures, and suggests that information externalities in hospitals help explain the rapid spread of technologies. If system partnerships lead to greater interaction among the staff of member hospitals, then information about new procedures or medical treatments may spread more rapidly among system partners than among independent hospitals. Systems may also provide information about technological developments more formally; continuing education programs for clinical personnel have been cited as one benefit of system partnerships (McKay 1998). Finally, systems may provide administrative and other support to member hospitals that do not alter service offerings but do change other aspects of hospital operations.
If system participation encourages greater coordination and information transfer, then it may alter decision making about the appropriate candidates for transfers and procedures, and may more generally improve the quality of care. These patient care effects may be reinforced or undermined by the patient care effects arising from systems' impacts on service offerings. Because system affiliations can affect patient treatment in so many ways, the net effect of systems on patients must be assessed empirically.
Few prior studies have examined the relationship between system affiliation and patient treatment or outcomes. Most of those that have are now dated (see, e.g., Gaumer 1986; Shortell and Hughes 1988).3 This study uses information about Medicare patients admitted to for-profit or private not-for-profit acute care hospitals between 1985 and 1998 with a primary diagnosis of acute myocardial infarction to determine the relationship between multihospital system membership and hospital transfer decisions, treatment intensity, expenditures, and health outcomes.
Data and Methods
Hospital Variables
Hospital data for this study come primarily from the American Hospital Association's Annual Survey of Hospitals (the AHA survey) for each year 1985 through 1998. The study includes U.S. hospitals that the survey database identifies as private nonprofit or for-profit general medical-surgical hospitals, that have all relevant data, and that are matched to study patients.4 The survey database indicates whether a hospital is for-profit, religiously affiliated, or contract managed. If a hospital reports having more than 20 full-time residents, it is classified as a teaching hospital. Bed totals include adult general medical and surgical, other acute care, intensive care, and burn care beds, but exclude subacute, neonatal, pediatric, and obstetric beds.5 A hospital was coded as offering catheterization if more than 10 procedures in a given year were reported in the Medicare claims records; it was coded as offering PTCA or CABG services if more than 10 angioplasties or more than 10 open-heart surgeries were reported.6
The hospital system participation variable is based on AHA survey data. Because multihospital systems may differ along so many dimensions, researchers' approaches to system definition have varied. For example, previous authors have separated nonprofit systems from investor-owned chains (Alexander and Morrisey 1988), or focused on local affiliations (Luke, Ozcan, and Olden 1995). To facilitate a broad exploration of the relationship between system affiliation and patient treatment, this study uses a broad definition of multihospital system membership. The AHA defines a multihospital system as two or more hospitals owned, leased, sponsored, or contract managed by a central organization. While the AHA takes steps to validate its system listings, the system data and the AHA survey responses often differ. For example, in the 1998 survey, 24 percent of nongovernmental general medical-surgical hospitals that report being part of a health care system do not have an AHA-assigned system identifier, while 11 percent of hospitals that have a system identifier fail to report being in a system. While some discrepancies may stem from delay in assigning official identifiers to newly formed systems, most likely result from differences in the time-frame considered by the AHA and survey respondents in assessing system status, or differences in perceptions of what constitutes a health care system. In light of these discrepancies, the AHA-assigned system identifier has been supplemented with additional information.
System identifiers were assigned as follows. Hospitals with an AHA-assigned system identifier for a particular year retained that identifier. But system identifiers were also assigned when at least two hospitals reported the same system name, or when hospitals reported participation in systems that were ever listed either in the AHA Guide (between 1985 and 2000) or in system listings prepared annually by Modern Healthcare. A gap-filling algorithm was then applied to ensure that missing data did not result in a hospital suddenly disappearing from, then reappearing in, a hospital system. Finally, to be treated as a system hospital for this study, a hospital must have had at least one nongovernmental, general medical-surgical hospital partner for which size and location could be determined.
Hospitals with system identifiers are further subdivided by type, to allow more complete exploration of the proliferation, concentration, and coordination hypotheses. First, system hospitals are classified based on whether they have more or fewer than 250 beds. Smaller hospitals are unlikely to be able to offer the full range of expertise and services that larger hospitals can support. They are therefore more likely than larger hospitals to be the recipients of information transfer, and to be on the service-offering decision-making margin. As a result, to the extent that systems have any of their hypothesized effects, patients of smaller hospitals are more likely to be affected. This paper will therefore focus on the effects of system membership on hospitals with fewer than 250 beds (“small” hospitals).
Small system hospitals are divided into three groups: urban hospitals with “big” partners (i.e., partners with more than 250 beds) within 25 miles, rural hospitals with big partners within 100 miles, and other system hospitals. Distant partners are distinguished from local partners because for patient transfers to be reasonable, the transferring and receiving hospitals must be nearby. Physical proximity may also facilitate coordination and information transfer. The mile threshold used to define “nearby” for rural hospitals is greater because they are likely to be more distant from potential transfer partners than urban hospitals are. Hospitals without nearby big partners are distinguished from other small system hospitals because they are less likely to be able to take advantage of the service concentration and coordination benefits of systems. They can, however, take advantage of other benefits of system participation, such as improved access to capital.
System hospitals with more than 250 beds are stratified according to whether they have local partners. Big system hospitals with local partners (rural hospitals within 100 miles, or urban hospitals within 25 miles) may serve as the sort of “flagship” hospital contemplated by the service concentration and coordination hypotheses. Big system hospitals without local partners cannot serve this function, but like their smaller counterparts, may take advantage of other benefits of system participation.
Patient Variables
Patients included in this study are non-HMO Medicare beneficiaries between the ages of 65 and 99 who reside within the 50 states or the District of Columbia and who were admitted to a study hospital with an AMI.7 AMI patients are an ideal study population not only because meaningful health outcomes such as mortality are available in administrative records, but also because AMI patients generally are taken to the nearest hospital (Thiemann et al. 1999). This ameliorates concerns about the econometric difficulties that would arise if patients (or others) selected initial admission hospitals on the basis of hospital and patient characteristics. Patient hospital records come from the Health Care Financing Administration's 100 percent sample Medicare Provider Analysis and Review tapes (which contain Medicare Part A claims). Additional demographic information comes from HCFA's HISKEW tapes. Patients who have had an AMI within the previous year are excluded. See Kessler and McClellan (2000) for more information on the creation of the AMI sample.
Patient characteristics available in this data and used as independent variables are sex, race (black or nonblack), and age. Other patient information provides the basis for dependent variables meant to provide insight into treatment patterns, treatment intensity, health outcomes, and medical expenditures. A patient is defined to have been transferred if he or she was admitted to a hospital for an AMI, discharged, and then admitted to a different hospital on the same day or the next day with a diagnosis of AMI, congestive heart failure, or ischemic heart disease. A transfer patient is likely to be one who is stable enough to be transferred, and who would benefit from more intensive treatment than the initial admission hospital is prepared to provide, such as a catheterization, percutaneous transluminal coronary angioplasty (PTCA or angioplasty), or coronary artery bypass graft (CABG or bypass surgery). Treatment intensity is measured by indicator variables for having a catheterization within 90 days of admission, and having an angioplasty or bypass surgery within 90 days of admission. Health outcomes are measured by 90-day mortality.
Medical expenditure is measured by the log of total payments for the Medicare patient's inpatient care (including Medicare hospital reimbursement, deductibles, and copayments) in the 90 days following the patient's index admission, in 1993 dollars.8 Total expenditure is determined by multiple factors. Medicare makes a fixed payment to a hospital based in part on the patient's diagnosis-related group (a function of the patient's diagnosis and surgical procedures), as well as various hospital characteristics, such as case mix, local wage rates, treatment of a disproportionate share of low-income patients, and the provision of medical education. Medicare expenditures may also reflect patient transfers. Buczko (1993) notes that under Medicare's payment system, hospitals that ultimately transfer a patient receive a per diem payment based on the average cost and length of stay for the diagnosis related group (DRG) assigned to the initial stay. Hospitals accepting a transfer receive the full DRG payment for the patient. This means that payments on behalf of transferred patients are likely to exceed those for similar patients who were not transferred. Ultimately, the log 90-day payment variable reflects not only the patient's AMI diagnosis, but also the patient's transfers, treatments, and readmissions.
Methodology
At the core of this study is a simple question: Do patients of hospitals that participate in multihospital systems experience differences in care relative to patients of otherwise similar independent hospitals? Ordinary least squares regressions examining transfer rates, treatment rates, expenditures, and mortality rates are used to answer this question. An observation is a Medicare patient initially admitted to a study hospital between 1985 and 1998 with a primary diagnosis of AMI. The observation contains the characteristics, treatments, and outcomes Yijt of a patient i initially admitted to a hospital j in year t, as well as the characteristics associated with hospital j. Note that the patient need not actually have received all treatment at hospital j. (The research question is not how hospital j treats its patients, but whether the system affiliation of hospital j has any effect on how the patient is treated, wherever the patient is ultimately treated.) The core regression is of the form:
The hospital traits vector includes indicator variables for four hospital-size categories interacted with two time periods (1985–1991 and 1992–1998), which allows for variation in the impact of hospital size over time. It also includes hospital teaching, contract management, religious affiliation, and for-profit status. The patient characteristics (sex, age category, and race) are fully interacted with one another.
The regression also includes fixed effects, which address several methodological problems. Probably due to technological advances, procedure rates have increased greatly over time, while mortality rates have decreased. In a regression without time fixed effects, if a particular system type were formed primarily in later years, it may appear to have had a much more positive effect on outcomes than it had in reality. The inclusion of year fixed effects prevents such a result. Similarly, the inclusion of hospital fixed effects controls for unchanging characteristics associated with a hospital or with a hospital's market area. For example, if systems tend to acquire hospitals operating in areas with a high demand for lucrative hospital procedures, regression results might show a misleading correlation between system membership and high cardiac procedure rates. Hospital fixed effects would pick up the impact of high patient demand, allowing the system variable to pick up the independent impact of system membership. In total, about 44 percent of hospitals joined, left, or switched system types during the study period, contributing to the identification of the effects of system status.
One potential concern about the proper interpretation of this regression is the difficulty of disentangling the effects of joining a system from the effects of changing hospital or hospital market characteristics. Previous studies, including Luke, Ozcan, and Olden (1995) and Alexander and Morrisey (1988), demonstrate that the selection of hospitals into systems is not random.9 If system formation is a function of time-varying hospital characteristics not included in the regression, the regression results will provide biased measures of the effect of systems. More specifically, if the omitted characteristics influencing system affiliation have an independent impact on the dependent variables, the estimates of the effects of system membership will be biased.
Such a bias might be revealed in a regression analysis comparing the treatments, expenditures, and outcomes for patients of independent hospitals about to join systems with the same measures for patients of independent hospitals that do not join systems. To be included in this comparison, a hospital must show one of four patterns in four consecutive years, beginning in any year between 1985 and 1995. It could remain independent for all four years (a nonsystem hospital), be in a particular system type for all four years (a system hospital), remain independent for two years and then join a system for two years (a system joiner), or be in a system for two years and then become independent for two years (a system leaver).10 An observation in the regression is a patient admitted in the first of the four years to a hospital meeting these criteria, and the dependent variables are the patient's outcomes for that admission year. The regression includes the same variables included in the core regression, except that it includes five regressors for system joiners, five for system hospitals, and five for system leavers, each set corresponding to the system types of the core regression. If the effects visible in the core regression are due entirely to system formation, there would be no statistically significant difference between coefficients of independent hospitals soon to join systems and those of independent hospitals that would remain independent. While this analysis cannot alleviate all potential concerns about endogeneity, it can help to assure that statistically significant results in the core regression are not simply due to preexisting differences in the hospitals that join systems.
An extension of the core regression model includes all previously described variables, but also includes indicator variables for catheterization and PTCA/CABG services. The coefficients on the system variables in this regression thus reveal the relationship between system participation and patient treatment, controlling for cardiac service capabilities at the patient's initial admission hospital. If patient care differences at system hospitals arise primarily through the direct impact of a system hospital's decision to offer services, the service offering variables would have statistically significant coefficients, and the importance of the system variables in explaining patient treatments, expenditures, and outcomes would be accordingly reduced. If system effects instead persist, then they have likely arisen through other channels, such as information transfer and care coordination.
Results
Descriptive Analysis
Multihospital system membership increased between 1985 and 1998, but not at a fast pace until the 1990s (see Table 1). System participation grew among both small and big hospitals, but the growth rate was faster among big hospitals. One particularly prominent pattern among big hospitals is the sharp increase in local system membership in the 1990s, in contrast to the decline of nonlocal system membership over the same time period. The percentage of big hospitals participating in local systems increased from 32 percent in 1990 to 64 percent in 1998, while the percentage of big hospitals participating in nonlocal systems dropped from over 16 percent to 10 percent. A significant trend among small hospitals is the increase in prevalence of affiliations with local big partners; the proportion of small hospitals involved in such relationships increased from 7.9 percent in 1990 to 18.5 percent in 1998.
Table 1.
Prevalence of Multihospital System Membership, by Hospital Size
| Bed Size | System Type | 1985 | 1990 | 1994 | 1998 |
|---|---|---|---|---|---|
| Under 250 | Urban w/local big partner | 4.4 | 4.1 | 7.1 | 11.3 |
| Rural w/local big partner | 5.1 | 3.8 | 5.5 | 7.2 | |
| Other system | 38.9 | 42.6 | 39.6 | 43.0 | |
| Total: Any system | 48.3% | 50.4% | 52.1% | 61.5% | |
| Over 250 | Local partner | 28.9 | 32.4 | 41.6 | 63.8 |
| Other system | 16.5 | 16.5 | 13.5 | 9.9 | |
| Total: Any system | 45.4% | 48.8% | 55.1% | 73.6% | |
| All | Any system | 47.8% | 50.2% | 52.5% | 62.8% |
| Urban hospitals <250 beds | 1,703 | 1,717 | 1,690 | 1,568 | |
| Rural hospitals <250 beds | 1,462 | 1,338 | 1,296 | 1,268 | |
| All hospitals <250 beds | 3,165 | 3,055 | 2,986 | 2,836 | |
| All hospitals ≥250 beds | 689 | 559 | 452 | 345 | |
| All hospitals | 3,854 | 3,614 | 3,438 | 3,181 |
Table 2 compares characteristics of system and independent hospitals in selected study years. System hospitals are more likely than independent hospitals either to be for-profit or to have a religious affiliation. System hospitals were on average smaller than independent hospitals in 1985 and 1992, but larger in 1998. Independent hospitals were consistently less likely to offer cardiac services. Relative to independent hospitals, system hospitals are disproportionately located in urban areas, a pattern that becomes more visible later in the study period. System hospitals tend to be located in the South Central, Mountain, and Pacific regions, while independent hospitals dominate the New England, Mid-Atlantic, and North Central regions.
Table 2.
Study Hospital Characteristics in Selected Study Years
| 1985 | 1992 | 1998 | ||||
|---|---|---|---|---|---|---|
| System | Independent | System | Independent | System | Independent | |
| No. of Hospitals | 1,842 | 2,012 | 1,745 | 1,772 | 1,997 | 1,184 |
| Hospital Type | ||||||
| % Nonprofit (NP) | 37.7 | 88.3 | 43.7 | 88.6 | 52.2 | 88.9 |
| % Religious (NP) | 28.9 | 6.0 | 28.3 | 5.2 | 22.3 | 4.7 |
| % For-profit | 33.3 | 5.7 | 28.0 | 6.2 | 25.5 | 6.4 |
| Hospital Size | ||||||
| Mean Beds | 147 | 156 | 138 | 142 | 127 | 104 |
| <250 Beds | 83.0 | 81.3 | 85.3 | 84.7 | 87.3 | 92.3 |
| ≥250 Beds | 17.0 | 18.7 | 14.7 | 15.3 | 12.7 | 7.7 |
| Hospital Services | ||||||
| % Offering Catheterization | ||||||
| <250 beds | 19.4 | 12.5 | 41.3 | 30.9 | 47.3 | 34.8 |
| ≥50 beds | 85.0 | 71.8 | 98.4 | 88.2 | 97.2 | 93.4 |
| % Offering Angioplasty or Bypass Surgery | ||||||
| <250 beds | 6.3 | 3.6 | 15.1 | 9.7 | 22.6 | 12.6 |
| ≥250 beds | 61.7 | 49.5 | 85.2 | 64.0 | 88.2 | 67.0 |
| Metropolitan Statistical Area Size | ||||||
| % Rural | 36.5 | 40.1 | 35.7 | 40.0 | 35.9 | 47.6 |
| % Under 250 k | 11.3 | 10.8 | 11.8 | 10.9 | 10.7 | 11.4 |
| % 250 k–1 m | 20.6 | 19.4 | 21.8 | 19.5 | 22.3 | 18.1 |
| % 1 m+ | 31.5 | 29.8 | 30.7 | 29.6 | 31.1 | 23.0 |
| Region | ||||||
| % New England | 1.9 | 9.1 | 2.3 | 8.7 | 3.2 | 8.2 |
| % Mid-Atlantic | 6.3 | 19.3 | 6.0 | 20.8 | 10.3 | 18.0 |
| % South Atlantic | 14.9 | 13.5 | 16.3 | 13.9 | 16.3 | 14.9 |
| % North Central | 26.0 | 32.9 | 28.0 | 31.2 | 26.8 | 32.9 |
| % South Central | 26.1 | 13.2 | 24.6 | 13.1 | 23.2 | 13.8 |
| % Mountain | 8.1 | 3.5 | 8.4 | 3.6 | 7.0 | 4.5 |
| % Pacific | 16.7 | 8.6 | 14.4 | 8.8 | 13.2 | 7.8 |
Of the patient sample pooled across all years, 50 percent are female and 5 percent are black. Twenty-one percent of sample patients are between the ages of 65 and 69, 24 percent between 70 and 74, 22 percent between 75 and 79, 28 percent between 80 and 89, and 5 percent between 90 and 99. The demographic characteristics of patients vary across admission hospitals by system status. For example, black patients comprise 3.9 percent of patients in small independent hospitals, but 5.5 percent of patients in small hospitals that have partnered with nearby big hospitals. Patients older than age 80 comprise 32.3 percent of patients of big independent hospitals, but only 29.5 percent of patients of big system hospitals without local partners. These demographic differences should not affect the analyses, however, since demographic characteristics will be included as regressors. Table 3 similarly shows considerable variation in means of dependent variables by hospital size and system status, variation that calls for further exploration in regressions controlling for other hospital and patient characteristics.
Table 3.
Means of Dependent Variables by Initial Admission Hospital Characteristics
| Number of Patients | % Trans- ferred | % with Catheter within 90 Days | % with PTCA or CABG within 90 Days | Log 90-Day Payments | % 90-Day Mortality | |
|---|---|---|---|---|---|---|
| 1985 | 186,654 | 4.6 | 13.7 | 7.5 | 9.01 | 31.0 |
| 1990 | 177,239 | 10.8 | 32.8 | 21.1 | 9.13 | 27.4 |
| 1994 | 195,115 | 16.3 | 45.9 | 32.0 | 9.29 | 24.1 |
| 1998 | 173,261 | 15.4 | 50.6 | 37.8 | 9.47 | 24.2 |
| All Years: Under 250 Beds | ||||||
| Urban w/local big partner | 127,517 | 16.8 | 40.0 | 26.9 | 9.34 | 26.5 |
| Rural w/local big partner | 61,370 | 23.9 | 30.9 | 20.2 | 9.04 | 28.7 |
| Other system | 645,261 | 14.5 | 37.0 | 25.3 | 9.20 | 27.6 |
| Independent | 863,806 | 16.3 | 30.7 | 20.3 | 9.16 | 27.4 |
| Over 250 Beds | ||||||
| Local Partner | 343,930 | 3.2 | 47.7 | 33.3 | 9.33 | 25.0 |
| Other system | 126,622 | 3.1 | 43.7 | 28.8 | 9.24 | 25.6 |
| Independent | 416,896 | 6.6 | 36.4 | 24.0 | 9.30 | 25.9 |
Regression Analysis
Table 4 contains the OLS coefficient estimates (in percentage point terms) for five separate regressions, each including the five system variables, as well as the nonsystem independent variables described previously. Dependent variables are listed across the top of the table, and the system independent variables down the side. There are several statistically significant system effects. Among small hospitals, patients of rural system hospitals with big local partners experience approximately one percentage point lower mortality rates than patients of otherwise similar independent hospitals (a result significant at the p =.001 level). Patients of small system hospitals without nearby big partners are less likely to be transferred. Patients of big system hospitals with local partners are less likely to be transferred than patients of similar independent hospitals. Finally, patients of big system hospitals without local partners incur higher expenditures, and may be more likely to receive catheterizations (a result significant at the p <.10 level).
Table 4.
OLS Regressions of AMI Patient Treatments, Payments, and Outcomes on System Status, 1985–1998
| Dependent Variables | ||||||
|---|---|---|---|---|---|---|
| Hospital Size | System Status | Transferred | Catheter within 90 Days | PTCA or CABG within 90 Days | Log 90-Day Payments | 90-Day Mortality |
| <250 Beds | Urban w/local | −.12 | −.39 | −.19 | .23 | .17 |
| big partner | (.62) | (.36) | (.29) | (.87) | (.21) | |
| Rural w/local | .18 | .34 | .19 | 1.26 | −1.09 ** | |
| big partner | (.83) | (.56) | (.48) | (1.27) | (.34) | |
| Other system | −1.09 ** | −.16 | .33 | −.14 | −.05 | |
| (.36) | (.28) | (.23) | (.50) | (.15) | ||
| ≥250 Beds | Local partner | −.75* | .65 | .51 | .88 | .02 |
| (.36) | (.43) | (.36) | (.76) | (.17) | ||
| Other system | .24 | .94 | .66 | 2.44** | −.17 | |
| (.52) | (.54) | (.52) | (.90) | (.24) | ||
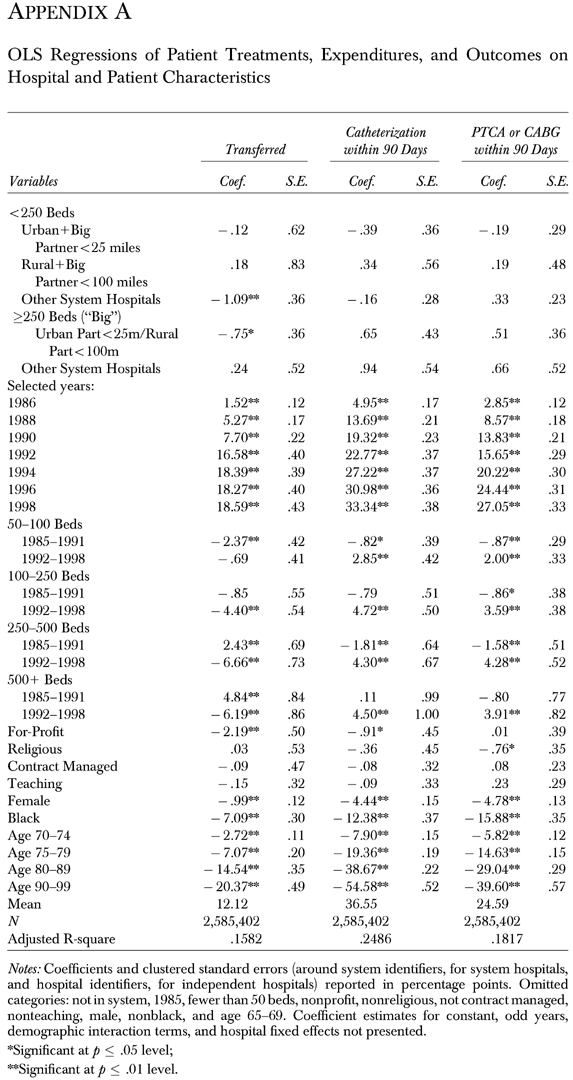
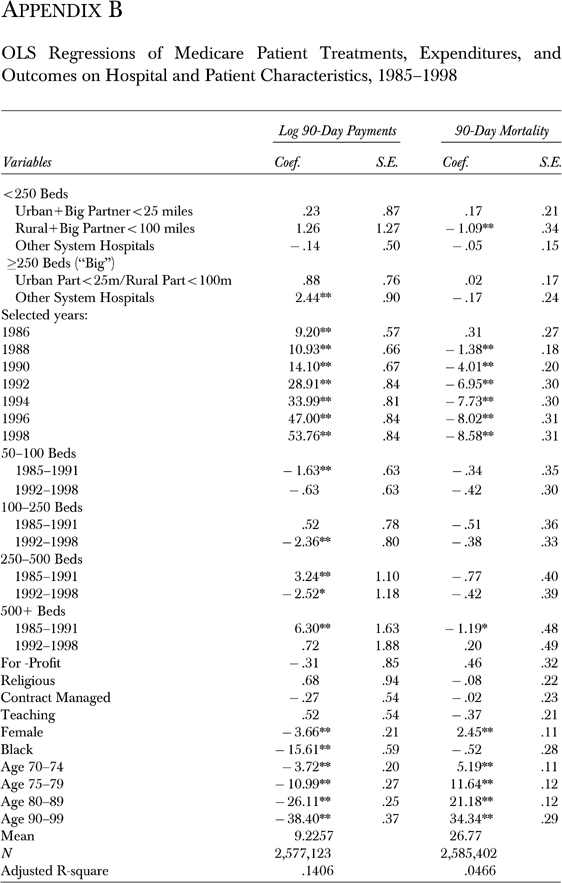
Notes: Coefficients and clustered standard errors (in parentheses) are reported in percentage points.
See Appendix A and Appendix B available online at http://www.blackwell-synergy.com for full regression results.
Significant at p≤.05 level;
Significant at p≤.01 level.
One possible concern is that these results may be sensitive to the precise definition of the system categories. Sensitivity analyses that vary system definitions based on hospital size and distance between hospital partners, however, suggest that the results are robust.11
Table 5 shows a number of statistically significant differences between independent hospitals that will remain independent and those that will join systems, particularly in the small-hospital-with-big-local-partner system categories. Patients of hospitals about to join the small-rural-hospital-with-big-local-partner category, for example, are significantly more likely to be transferred and to receive cardiac procedures than patients of otherwise similar hospitals that were not about to join systems. (It is perhaps not surprising that small hospitals actively transferring patients would make particularly attractive system partner candidates for nearby big hospitals.) Note, however, that these hospitals do not exhibit significantly lower mortality rates before joining systems. More generally, the results of this analysis do not foreshadow the system effects displayed in Table 4.
Table 5.
Association between Future System Participation and Treatments, Payments, and Outcomes, 1985–1995
| Dependent Variables | ||||||||
|---|---|---|---|---|---|---|---|---|
| Currently Independent but Will Be of System Type: | Transferred | Catheter within 90 Days | PTCA or CABG within 90 Days | Log 90-Day Payments | 90-Day Mortality | |||
| <250 Beds | Urban w/local | 2.79* | .19 | −.96 | 1.00 | 1.70** | ||
| big partner | (1.16) | (1.00) | (.68) | (1.73) | (.56) | |||
| Rural w/local | 5.03** | 3.37* | 2.80* | 4.51 | −.03 | |||
| big partner | (1.65) | (1.56) | (1.35) | (2.89) | (1.30) | |||
| Other system | −.79 | −.26 | −.23 | −1.00 | −.31 | |||
| (.67) | (.55) | (.50) | (1.21) | (.41) | ||||
| ≥250 Beds | Local partner | .16 | −.03 | −.50 | 2.35 | .14 | ||
| (.64) | (.68) | (.60) | (1.45) | (.47) | ||||
| Other system | .04 | .05 | .07 | 4.12 | 1.29 | |||
| (2.64) | (2.36) | (1.85) | (6.76) | (1.47) | ||||
Notes: Coefficients and clustered standard errors reported in percentage points. Nonsystem variables noted in Appendix A and Appendix B, available online at http://www.blackwell-synergy.com, are also included, as are indicator variables for hospitals that remain in systems and hospitals that leave systems. N =1,607,596, except for log 90-day payments, where N =1,604,010.
Significant at p≤.05 level;
Significant at p≤.01 level.
The extension of the core regression that includes service offerings suggests that while service offerings are associated with significant differences in patient care, system participation continues to have an independent influence. Offering catheterization is associated with a higher level of transfers, procedures, expenditures, and lower mortality, while offering angioplasty or bypass surgery is associated with a substantially lower level of transfers, a higher level of procedures, and a lower level of mortality. The inclusion of service offering variables in the system regressions produced very little change in the estimates of the system coefficients. Relative to the results in Table 4, for example, the mortality coefficient for rural hospitals with local big partners increased by just .02 percentage points.12
Discussion
By revealing the relationship between system status and a variety of measures of patient treatment, expenditures, and outcomes, Table 4 fulfills the primary objective of the study. It shows a few statistically significant results among big system hospitals, but does not show a substantially greater number of significant effects among the small hospitals for which system membership was hypothesized to have the greatest impact. For example, while a small hospital's membership in a system without big local partners is associated with fewer transfers, a result consistent with the proliferation hypothesis, this lower transfer rate does not appear to be associated with any statistically significant differences in patient treatments, expenditures, or outcomes. And among urban hospitals with local big partners—the fastest growing system category—no statistically significant effects were identified at all.
There was one system effect among small hospitals that was both statistically significant and substantial: patients of small rural hospitals with big local partners experienced lower mortality rates.13 This difference in mortality does not appear to have predated system formation, suggesting that it may in fact be related to system status, rather than preexisting unobservable differences between hospitals that join systems and hospitals that do not.
The mortality result remains even after controlling for cardiac service offerings.14 Thus, although cardiac service offerings are associated with lower mortality rates, the improvement in mortality associated with system membership does not appear to have been achieved through this mechanism.15 Other channels of system influence, such as those suggested by the coordination and information transfer hypothesis, may instead be at work.
Conclusion
Observers of “integrated” delivery systems have commented that many fail to operate in a truly integrated, coordinated way. Shortell (1988) hypothesizes that the effects of systems may be limited because system hospitals often do not behave as system partners. If formal affiliations have no impact on hospital operations, then there is no reason to expect system status to have any effect on patient treatment. This article's findings imply, however, that AMI patients initially admitted to system hospitals may indeed be treated differently from patients admitted to independent hospitals. The differences are not pervasive; patients of many types of system hospitals do not experience any difference in treatments, expenditures, or outcomes. But for some patients, affiliations matter. In particular, patients of rural system hospitals with big local partners experience lower mortality rates. This difference does not appear to be the result of a relationship between system membership and cardiac service offerings. It may instead be a result of other changes associated with system membership; perhaps system hospitals more effectively share information and coordinate care. These factors cannot be fully explored without more detailed information about patient care.
Multihospital system membership has grown and shifted form in recent years. These changes make understanding the effects of system membership on the treatment of patients even more important than it was in the past. The results of this paper suggest that system membership may make a difference, but also that these differences may be limited to just a few system types; future research should distinguish among system types. In addition, while heart attacks are an important subject of study both because of their prevalence and because of their dramatic health effects, heart disease is certainly not the only disease for which system status may affect treatments, expenditures, or outcomes. A thorough evaluation of the net effects of systems on patients will require examination of the effects of systems on patients with a broader, more representative set of diseases. This study serves as an initial step in the assessment of the effects of multihospital system membership on patients.
Acknowledgments
I thank Jason Brown, Kate Bundorf, Jeff Geppert, Dan Kessler, Al Klevorick, Julie Lee, Mark McClellan, John Pencavel, Abigail Tay, Kevin Volpp, Ed Vytlacil, and especially Akila Weerapana for their encouragement, suggestions, assistance in obtaining data, and many helpful discussions. I have also benefited from the insights of the reviewers and seminar participants at Stanford University, the University of Minnesota, and the University of Pennsylvania, as well as the 10th Annual Health Economics Conference.
APPENDIX A
OLS Regressions of Patient Treatments, Expenditures, and Outcomes on Hospital and Patient Characteristics
APPENDIX B
OLS Regressions of Medicare Patient Treatments, Expenditures, and Outcomes onHospital and Patient Characteristics, 1985-1998
Notes
This study does not use the Bazzoli et al. (2000) taxonomy. The taxonomy encompasses both hospital–physician relationships and insurance products, which will not be studied here, and much of the data supporting the taxonomy becomes available only in the mid-1990s.
Using Medicare records from fiscal year 1987, Buczko (1993) found that small and rural hospitals tend to send transfers to large urban hospitals of 200 beds or more, and receive relatively few transfers themselves. The three most common DRGs for transfer admissions were coronary bypass with cardiac catheterization (7.9 percent), percutaneous cardiovascular procedures (6.8 percent), and coronary bypass without cardiac catheterization (5.7 percent).
An exception is Huckman (2000), which examines hospital acquisitions in New York between 1990 and 1997 involving hospitals with disparate levels of cardiac services. The author finds that the acquisitions were associated with increased procedure volumes and, for bypass surgery patients in the market of target hospitals, increased risk-adjusted costs and decreased risk-adjusted mortality.
Local and federal government hospitals were excluded because they may not face the same incentive structures as nongovernment hospitals, and because systems that operate these hospitals may face more constraints on their behavior.
If a bed total was missing, it was assumed to be the average of totals in the nearest nonmissing preceding and subsequent years.
The AHA survey contains data on facilities, but does not document angioplasty services prior to 1989, and has a nonresponse rate that exceeds 10 percent in some years. The coding methodology therefore applies a gap-filling and consistency correction algorithm to Medicare data rather than using AHA data. The correspondence between Medicare-based coding and AHA-based coding (when present) is generally more than 90 percent.
The use of data from elderly Medicare patients raises the question of applicability to the population as a whole. Medicare patients account for a substantial proportion of people who have AMIs, however, and so are an important study population, even if the findings do not apply universally.
A small number of observations with negative or zero dollar amounts were excluded from the payment analysis. Mean expenditure in the sample was about $13,500.
Among other factors, Luke, Ozcan, and Olden (1995) find that the number of competitors is strongly and positively related to local hospital system penetration. Alexander and Morrisey (1988) find that a higher percentage of elderly in the population, teaching hospital status, larger hospital size, a higher occupancy rate, and a smaller revenue-to-expenditure ratio all make multihospital system acquisition less likely.
While this approach excludes 22 percent of observations in the 1985 through 1995 time period, it ensures that the period in which hospitals transition between system statuses does not cloud the coefficient estimates.
The small-rural-with-big-local-partner coefficient on mortality, for example, remains negative and statistically significant at the p≤.05 level if the threshold separating “small” from “big” hospitals is based on 200- or 500-bed capacities, or teaching status; if the urban “local partner” distance threshold is set at 10 miles rather than 25; or if the rural distance threshold is set at 200, rather than 100. The estimate remains negative (−.65), but becomes statistically insignificant, if the rural distance cutoff is decreased to 50 miles.
The transfer coefficient for small other system hospitals increased from −1.09 to −.93; the transfer coefficient for big local system hospitals increased from −.75 to −.65; and the big nonlocal system coefficient on payments increased from 2.44 to 2.54. None of the other system results were statistically significant at the p≤.05 level. Complete results for these regressions are available from the author.
This result contrasts with an older literature finding little effect of system membership on mortality. Ermann and Gabel (1986) and Shortell (1988) note that previous studies found essentially no differences in mortality rates or patient care outcomes in system hospitals relative to independent hospitals. Gaumer (1986), using 1974–1981 data for selected surgical admissions, finds that for investor-owned hospitals, being in a system is weakly associated with higher in-hospital mortality but lower 180-day mortality, and concludes that there is no pattern of large ownership differences for serious patient outcomes. Shortell and Hughes (1988), using 1983 and 1984 Medicare data for 16 clinical conditions, find no statistically significant association between mortality rates among inpatients and affiliation with a multihospital system. Huckman (2000), however, finds that hospital acquisitions are associated with lower mortality.
A regression including system membership and service offering interaction terms as well as service offering variables confirms that differences persist even after taking into account the presence of facilities. Rural local system hospitals that do not offer catheterization or PTCA/CABG services experience mortality rates .76 percentage points lower than independent hospitals without facilities (p =.038), while system hospitals offering only catheterizations experience mortality rates 2.10 percentage points lower than independent hospitals with similar services (p =.001). The coefficient on the system-PTCA/CABG interaction term was positive (1.77), but not statistically significant (p =.206).
A logit regression of service offerings on the five system types (and all of the other hospital variables included in the Appendix regression) confirms this observation. The only result statistically significant at the p <.05 level was that small hospitals without local big partners were more likely to have catheterization facilities. Rural system partnership with big local hospitals had no statistically significant impact on service offerings.
References
- Alexander JA, Morrisey MA. Hospital Selection into Multihospital Systems. Medical Care. 1988;26(2):159–76. doi: 10.1097/00005650-198802000-00007. [DOI] [PubMed] [Google Scholar]
- Andersen HR, Nielsen TT, Rasmussen K, Thuesen L, Kelbaek H, Thayssen P, Abildgaard U, Pedersen F, Madsen JK, Grande P, Villadsen AB, Krusell LR, Haghfelt T, Lomholt P, Husted SE, Vigholt E, Kjaergard HK, Mortensen LS. A Comparison of Coronary Angioplasty with Fibrinolytic Therapy in Acute Myocardial Infarction. New England Journal of Medicine. 2003;349(8):733–42. doi: 10.1056/NEJMoa025142. [DOI] [PubMed] [Google Scholar]
- Bazzoli GJ, Chan B, Shortell SM, D'Aunno T. The Financial Performance of Hospitals Belonging to Health Networks and Systems. Inquiry. 2000;37(3):234–52. [PubMed] [Google Scholar]
- Bazzoli GJ, Shortell SM, Ciliberto F, Kralovec PD, Dubbs NL. Tracking the Changing Provider Landscape Implications for Health Policy and Practice. Health Affairs. 2001;20(6):188–96. doi: 10.1377/hlthaff.20.6.188. [DOI] [PubMed] [Google Scholar]
- Bazzoli GJ, Shortell SM, Dubbs N, Chan C, Kralovec P. A Taxonomy of Health Networks and Systems Bringing Order Out of Chaos. Health Services Research. 1999;33(6):1683–717. [PMC free article] [PubMed] [Google Scholar]
- Blecher MB. Wall Street Smart, Main Street Savvy. Hospitals and Health Networks. 1998;72(17):38–42. [PubMed] [Google Scholar]
- Blustein J. High-Technology Cardiac Procedures. Journal of the American Medical Association. 1993;270(3):344–9. doi: 10.1001/jama.270.3.344. [DOI] [PubMed] [Google Scholar]
- Buczko W. Inpatient Transfer Episodes among Aged Medicare Beneficiaries. Health Care Financing Review. 1993;15(2):71–87. [PMC free article] [PubMed] [Google Scholar]
- Clement JP, McCue MJ, Luke RD, Bramble JD. Strategic Hospital Alliances Impact on Financial Performance. Health Affairs. 1997;16(6):193–203. doi: 10.1377/hlthaff.16.6.193. [DOI] [PubMed] [Google Scholar]
- Dranove D, Shanley M. Cost Reductions or Reputation Enhancement as Motives for Mergers The Logic of Multihospital Systems. Strategic Management Journal. 1995;16(1):55–74. [Google Scholar]
- Ermann D, Gabel J. Investor-Owned Multihospital Systems: A Synthesis of Research Findings. In: Gray BH, editor. For-Profit Enterprise in Health Care. Washington, DC: National Academy Press; 1986. pp. 474–91. [Google Scholar]
- Escarce JJ. Externalities in Hospitals and Physician Adoption of a New Surgical Technology: An Exploratory Analysis. Journal of Health Economics. 1996;15(6):715–34. doi: 10.1016/s0167-6296(96)00501-2. [DOI] [PubMed] [Google Scholar]
- Every NR, Larson EB, Litwin PE, Maynard C, Fihn SD, Eisenberg MS, Hallstrom AP, Martin JS, Weaver WD. The Association between On-Site Cardiac Catheterization Facilities and the Use of Coronary Angiography after Acute Myocardial Infarction. New England Journal of Medicine. 1993;329(8):546–51. doi: 10.1056/NEJM199308193290807. [DOI] [PubMed] [Google Scholar]
- Gaumer G. Medicare Patient Outcomes and Hospital Organizational Mission. In: Gray BH, editor. For-Profit Enterprise in Health Care. Washington, DC: National Academy Press; 1986. [Google Scholar]
- Grumbach K, Anderson GM, Luft HS, Roos LL, Brook R. Regionalization of Cardiac Surgery in the United States and Canada. Journal of the American Medical Association. 1995;274(16):1282–8. [PubMed] [Google Scholar]
- Huckman RS. Hospital Consolidation and the Delivery of Cardiac Care. 2000 Unpublished manuscript, Harvard University. [Google Scholar]
- Kessler DP, McClellan MB. Is Hospital Competition Socially Wasteful? Quarterly Journal of Economics. 2000;115(2):577–615. [Google Scholar]
- Luke RD, Ozcan YA, Olden PC. Local Markets and Systems Hospital Consolidations in Metropolitan Areas. Health Services Research. 1995;30(4):555–75. [PMC free article] [PubMed] [Google Scholar]
- McKay NL. Rural Hospitals Organizational Alignments for Managed Care Contracting. Journal of Healthcare Management. 1998;43(2):169–81. [PubMed] [Google Scholar]
- Menke TJ. The Effect of Chain Membership on Hospital Costs. Health Services Research. 1997;32(2):177–96. [PMC free article] [PubMed] [Google Scholar]
- Phillips KA, Luft HS, Ritchie JL. The Association of Hospital Volumes of Percutaneous Transluminal Coronary Angioplasty with Adverse Outcomes, Length of Stay, and Charges in California. Medical Care. 1995;33(5):502–13. doi: 10.1097/00005650-199505000-00005. [DOI] [PubMed] [Google Scholar]
- Shortell SM. The Evolution of Hospital Systems Unfulfilled Promises and Self-Fulfilling Prophesies. Medical Care Review. 1988;45(2):177–214. doi: 10.1177/107755878804500202. [DOI] [PubMed] [Google Scholar]
- Shortell SM, Hughes EFX. The Effects of Regulation, Competition, and Ownership on Mortality Rates among Hospital Inpatients. New England Journal of Medicine. 1988;318(17):1100–7. doi: 10.1056/NEJM198804283181705. [DOI] [PubMed] [Google Scholar]
- Soumerai SB, McLaughlin TJ, Gurwitz JH, Guadagnoli E, Hauptman PJ, Borbas C, Morris N, McLaughlin B, Gao X, Willison DJ, Asinger R, Gobel F. Effect of Local Medical Opinion Leaders on Quality of Care for Acute Myocardial Infarction. Journal of the American Medical Association. 1998;279(17):1358–63. doi: 10.1001/jama.279.17.1358. [DOI] [PubMed] [Google Scholar]
- Spetz J, Mitchell S, Seago JA. The Growth of Multihospital Firms in California. Health Affairs. 2000;19(6):224–30. doi: 10.1377/hlthaff.19.6.224. [DOI] [PubMed] [Google Scholar]
- Thiemann DR, Coresh J, Oetgen WJ, Powe NR. The Association between Hospital Volume and Survival after Acute Myocardial Infarction in Elderly Patients. New England Journal of Medicine. 1999;340(21):1640–8. doi: 10.1056/NEJM199905273402106. [DOI] [PubMed] [Google Scholar]
- Wright SM, Petersen LA, Daley J. Availability of Cardiac Technology Trends in Procedure Use and Outcomes for Patients with Acute Myocardial Infarction. Medical Care Research and Review. 1998;55(2):239–54. doi: 10.1177/107755879805500205. [DOI] [PubMed] [Google Scholar]


