Abstract
Objectives
To (1) describe patterns of posthospital care transitions; (2) characterize these patterns as uncomplicated or complicated; (3) identify those at greatest risk for complicated transitions.
Data Sources/Study Setting
The Medicare Current Beneficiary Survey was used to identify beneficiaries aged 65 and older who were discharged from an acute care hospital in 1997–1998.
Study Design
Patterns of posthospital transfers were described over a 30-day time period following initial hospital discharge. Uncomplicated posthospital care patterns were defined as a sequence of transfers from higher-to lower-intensity care environments without recidivism, while complicated posthospital care patterns were defined as the opposite sequence of events. Indices were developed to identify patients at risk for complicated transitions.
Principal Findings
Forty-six distinct types of care patterns were observed during the 30 days following hospital discharge. Among these patterns, 444 episodes (61.2 percent) were limited to a single transfer, 130 episodes (17.9 percent) included two transfers, 62 episodes (8.5 percent) involved three transfers, and 31 episodes (4.3 percent) involved four or more transfers. Fifty-nine episodes (8.1 percent) resulted in death. Between 13.4 percent and 25.0 percent of posthospital care patterns in the 1998 sample were classified as complicated. The area under the receiver operating curve was 0.771 for a predictive index that utilized administrative data and 0.833 for an index that used a combination of administrative and self-reported data.
Conclusions
Posthospital care transitions are common among Medicare beneficiaries and patterns of care vary greatly. A significant number of beneficiaries experienced complicated care transitions—a finding that has important implications for both patient safety and cost-containment efforts. Patients at risk for complicated care patterns can be identified using data available at the time of hospital discharge.
Keywords: Systems of care, care transitions, patient safety, predictive index
Patients with continuous complex care needs frequently require care in multiple settings and are particularly vulnerable to poorly executed transitions (Coleman 2003; Coleman and Boult 2003). The extent to which medical errors, in general, and medication errors, in particular, occur during care transitions is only recently becoming understood (Coleman 2003; Institute of Medicine 2001; Coleman et al. 2002; Forster et al. 2003; Halm et al. 2003; Boockvar et al. 2003; Moore et al. 2003; Beers, Sliwkowski, and Brooks 1992; Meredith et al. 2002; Cook, Render, and Woods 2000; Delgado-Rodriguez et al. 2001; Mitchell, Swift, and Gilbert 1999). Although researchers have examined single care transitions (e.g., returning to the hospital after being discharged or transferring from a nursing home to a hospital), to date there has been a paucity of studies that have explored entire episodes of care—that is, the multiple transitions that these patients often experience (Ashton et al. 1995; Weissman et al. 1999; Barker et al. 1994; Oddone et al. 1996; Jones et al. 1997; Lewis, Cretin, and Kane 1985; Waite et al. 1994; Siu, Manning, and Benjamin 1990; Densen 1991).
The recent Institute of Medicine report, Crossing the Quality Chasm: A New Health System for the Twenty-first Century, calls for greater integration of health care delivery across different settings to improve the quality of care transitions and reduce the threat of medical errors (Institute of Medicine 2001). However, before quality improvement approaches can be initiated, the patterns of posthospital care transitions need to be better understood. In addition, it is important to characterize the frequency and complexity of these transitions. Finally, it is necessary to develop effective targeting strategies that can be used to identify those patients who are at greatest risk for experiencing complicated care transitions and match those patients with evidence-based interventions aimed at improving the quality of their care transitions (Naylor et al. 1999; Rich et al. 1995; Philbin 1999; Townsend et al. 1988; Parry et al. 2003). This investigation aimed to: (1) describe the patterns and prevalence of care transitions among Medicare beneficiaries during a 30-day time period following acute hospitalization; (2) characterize the complexity of these care transitions; and (3) develop and test predictive indices designed to identify Medicare beneficiaries who are at greatest risk for complicated care transitions.
Methods
Setting
This study utilized the 1997 and 1998 Medicare Current Beneficiary Survey (MCBS) Cost and Use files and accompanying Medicare claims data. The MCBS is a continuous, multipurpose survey of a representative sample of Medicare patients that was designed to aid the Centers for Medicare and Medicaid Services (CMS) in administering, monitoring, and evaluating the Medicare program. The results from the survey are combined with information from administrative data files that the CMS maintains. Additional details of the MCBS are described elsewhere (Adler 1994; Centers for Medicare and Medicaid Services 2004). (Permission to use these files and to publish these results was granted under CMS Data Use Agreement number 11941. The Institutional Review Board of the authors' academic institution approved this study, protocol number 02-035.)
Participants
The study sample included Medicare beneficiaries who participated in the MCBS and were discharged from an acute care hospital in 1997 (n=700) or 1998 (n=704). Medicare beneficiaries who were aged 64 years or younger, residing in a long-term care institution, or enrolled in hospice care were excluded.
Unit of Analysis
The unit of analysis for each stage of this investigation was an episode of care, defined as the 30-day time period following discharge from an acute care hospital setting. All transfers that occurred within this time period were considered part of the same episode, including any additional acute hospitalizations. A patient could contribute more than one episode to the analysis. The 1997 and 1998 MCBS Cost and Use files included 726 and 738 discrete care episodes respectively.
To ensure that each episode was unique, acute hospitalizations that occurred within a 30-day time period following another acute hospitalization were included in characterizing the episode of the first hospitalization but were not treated as discrete care episodes. Because a patient's pre-morbid functional status may influence subsequent patterns of care (and is therefore important to adjust for a current assessment in the predictive models), the study sample was restricted to episodes that occurred within four months following the MCBS' annual functional assessment that takes place in September.
Patterns and Prevalence of Posthospital Transfers
In the first stage of this study, distinct patterns of posthospital transfers and their prevalence within the 1997 sample were determined. The following types of transfers were examined: transfers to skilled nursing or rehabilitation facilities, acute care hospitals, emergency departments, and patients' noninstitutional residences. Transfers to the emergency department that resulted in admission to an acute care hospital were considered a single transfer. Episodes that resulted in death within the 30-day time period were included in this stage of the study.
Uncomplicated versus Complicated Care Patterns
Since the existing literature on care transitions provides little insight into the best way to distinguish characterize patterns of care (Coleman 2003; vom Eigen et al. 1999; Naylor, Bowles, and Brooten 2000), the goal of the next stage of this study was to develop a systematic method for classifying the care transfers using administrative data that would be meaningful to consumers (i.e., patients and informal caregivers), clinicians, administrators, and policymakers. For the purposes of this investigation, an uncomplicated posthospital care pattern was operationally defined as one or more transfers from higher-intensity care environments (in which it is presumed that patients have greater functional dependency) to lower-intensity care environments (in which it is presumed that patients have less functional dependency), without recidivism. In contrast, a complicated posthospital care transition was defined as one or more transfers from lower- to higher-intensity care environments.
Patients who died within the 30-day posthospital period (n=59) were not included in this stage of the investigation because the current medical literature does not support a consistent association between the experience of death and the location in which it occurs. While some patients may prefer to die at home, others may consider an institution to be more desirable.
Approximately 80 percent of the episodes that did not result in death readily conformed to this schema. In the remaining 20 percent of episodes, the patients either experienced a transfer between two settings of comparable intensity (i.e., a “lateral” transfer, such as from one acute care hospital to another) or the patients did not return to community living at the end of the 30-day period (i.e., they reached a “plateau”). Because this classification was fundamentally based on determining either an increase or decrease in setting level of intensity, lateral transfers did not lead to the categorization of a patient's episode as complicated. In contrast, episodes characterized by the patient reaching a plateau and not returning to community living were categorized as complicated.
By way of example, an episode in which a patient was transferred from the hospital to a skilled nursing facility and then to home, would be categorized as uncomplicated. An episode that included transfer from a hospital to the patient's residence and then back to the hospital or emergency department without hospital admission within 30 days would be categorized as complicated. An episode that included transfer from a hospital to another hospital and then home would not be initially classifiable using an administrative approach, but would be categorized as uncomplicated using the more inclusive approach. Finally, an episode in which the patient was transferred home and then died would not be classified using either approach.
Predictive Indices for Complicated Transitions
The goal of the third stage of this investigation was to develop two predictive indices that could be used to identify Medicare beneficiaries who are at risk for experiencing complicated care transitions within 30 days of discharge from an acute care hospital. The dependent variable—complicated care patterns—was defined using the classification described in the previous section. The independent variables were derived from two sources: (1) patients' prior utilization data (6 months) and diagnoses abstracted from Medicare administrative files, and (2) patient-reported MCBS survey items. These two sources yielded a wide range of variables, including demographic information, burden of comorbidity calculated using the Charlson index (Charlson 1987), functional status, Medicaid enrollment, and prior utilization history. Pre-morbid Function Score was constructed by averaging the responses (1=No, 2=A little, 3=Some, 4=A lot, and 5=Unable) for various physical functional tasks (lifting, reaching, stooping, and walking a quarter of a mile). Assistance with Activities of Daily Living Score was constructed by averaging the indicators (1=Yes, 0=No) for having difficulty in the individual Activities of Daily Living categories (bathing, dressing, eating, walking, using the toilet, transferring in or out of bed or chairs). The functional responses were averaged to account for the fact that not all survey respondents answered every item (Ware 1997).
Models were constructed using data from the 1997 Medicare sample to develop indices predictive of complicated posthospital care patterns; data from the 1998 Medicare sample were used to validate the indices. Backward elimination modeling techniques were used to select the most parsimonious models. In the first strategy, the goal was to create a relatively simple index that Centers for Medicare and Medicaid Services (CMS) claims representatives without a clinical background can use to determine patients' risk for complicated care transfers and potential eligibility for a care coordination intervention; thus, the independent variables were restricted to those that are routinely available from administrative data maintained by CMS. In the second strategy, a broader array of variables were employed, including those obtained from both administrative and patient (or informal caregiver) self-reported data, with the only constraint being that the variables needed to be routinely available at the time of hospital discharge. The area under the curve of receiver operating curves was used to compare the predictive accuracy of these two strategies.
Results
Participants
Table 1 compares the 1997 and 1998 MCBS samples. There were no significant differences between the two groups in terms of demographic characteristics and medical diagnoses. However, the 1997 sample had significantly higher utilization rates for skilled nursing facilities prior to the study period, as measured by both length of stay and number of admissions. The most prevalent primary discharge diagnoses for the 1997 sample included coronary artery disease (9.7 percent), congestive heart failure (6.3 percent), stroke (4.1 percent), chronic obstructive pulmonary disease (4.0 percent), and hip fracture (3.0 percent). Similarly, the most prevalent primary discharge diagnoses for the 1998 sample included coronary artery disease (10.6 percent), congestive heart failure (5.7 percent), stroke (5.0 percent), chronic obstructive pulmonary disease (4.1 percent), and hip fracture (3.1 percent).
Table 1.
Demographic, Diagnostic, and Prior Utilization Characteristics of the Study Population
| Variables | 1997 Sample (n=700) | 1998 Sample (n=704) | P-Value (2-Tailed) |
|---|---|---|---|
| Administrative Data | |||
| 80 years of age or older (%) | 52.1 | 53.3 | 0.673 |
| Medicaid recipient (%) | 21.9 | 22.7 | 0.695 |
| Male (%) | 41.9 | 40.8 | 0.678 |
| Heart disease (%) | 65.8 | 62.8 | 0.275 |
| Hypertension (%) | 67.7 | 64.6 | 0.256 |
| Prior stroke (%) | 20.3 | 20.7 | 0.866 |
| Prior hip fracture (%) | 9.2 | 8.3 | 0.561 |
| Cancer (%) | 23.3 | 23.0 | 0.899 |
| Diabetes (%) | 21.8 | 22.5 | 0.769 |
| Emphysema (%) | 24.0 | 22.6 | 0.592 |
| Number of prior hospitalizations | 1.37±0.78 | 1.32±0.70 | 0.294 |
| Average length of prior hospitalizations (days) | 7.83±10.00 | 7.72±8.57 | 0.379 |
| Number of prior skilled nursing facility stays | 0.09±0.37 | 0.05±0.24 | 0.010 |
| Average length of prior skilled nursing facility stays (days) | 2.43±11.79 | 1.31±8.79 | 0.007 |
| Charlson comorbidity index (32) | 1.26±2.33 | 1.34±2.51 | 0.972 |
| Self-Reported Data | |||
| Alzheimer's disease (%) | 7.0 | 5.3 | 0.208 |
| Self-rated general health | 0.827 | ||
| 1=Excellent (%) | 7.2 | 6.3 | |
| 2=Very good (%) | 17.0 | 19.1 | |
| 3=Good (%) | 30.2 | 30.4 | |
| 4=Fair (%) | 25.3 | 25.4 | |
| 5=Poor (%) | 20.3 | 18.8 | |
| Visual Impairment | 0.910 | ||
| 1=None (%) | 48.0 | 48.9 | |
| 2=Little (%) | 34.6 | 34.5 | |
| 3=Lot of (%) | 17.5 | 16.6 | |
| Function score (1–5)* | 2.84±1.23 | 2.86±1.22 | 0.769 |
| Assistance with ADLs score (0–1)** | 0.26±0.32 | 0.24±0.31 | 0.447 |
| Unmarried (%) | 56.2 | 57.0 | 0.775 |
Function score was constructed by averaging the responses (1=No, 2=A little, 3=Some, 4=A lot, and 5=Unable) for various physical functional tasks (lifting, reaching, stooping, and walking a quarter of a mile).
Assistance with Activities of Daily Living (ADLs) score was constructed by averaging the indicators (1=Yes, 0=No) for having difficulty in the individual ADLs categories (bathing, dressing, eating walking, using the toilet, transferring in or out of bed or chairs).
Patterns and Prevalence of Posthospital Transfers
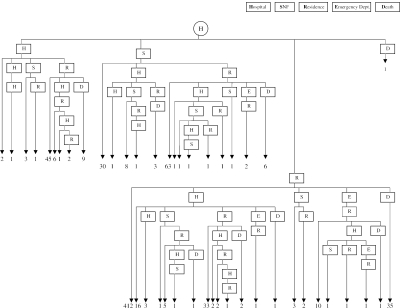
Forty-six distinct care patterns were observed among the Medicare beneficiaries included in the 1997 sample during the 30-day episode of care following discharge from an acute hospital (Figure 1). Immediately following the first acute hospitalization, 535 episodes (73.7 percent) resulted in a transfer to the patient's residence, 120 episodes (16.5 percent) resulted in a transfer to a skilled nursing or rehabilitation facility, 70 episodes (9.6 percent) resulted in a transfer within the existing hospital (i.e., to a transitional care unit) or to a different hospital, and 1 episode (0.1 percent) resulted in death before the initial transfer was complete.
Figure 1.
Health Care Transition Patterns after Discharge from an Acute Care Hospital
Following the initial transfer, a wide variation in patterns of care was observed over the 30-day time period: 444 episodes (61.2 percent) were limited to a single transfer, 130 episodes (17.9 percent) included two transfers, 62 episodes (8.5 percent) involved three transfers, and 31 episodes (4.3 percent) involved four or more transfers. Fifty-nine episodes (8.1 percent) resulted in death during the 30-day posthospitalization time period.
Uncomplicated versus Complicated Care Patterns
Thirty-day care episodes that did not result in death were categorized using two approaches. In the first approach, only those episodes that could be categorized using the classification schema when applied administratively were evaluated. This approach resulted in 11.1 and 13.4 percent of episodes categorized as complicated in the 1997 and 1998 samples respectively. The second approach accounted for all of the episodes that did not result in death, including those that involved transfers between settings of similar care intensity and episodes in which the patient did not return to community living. Using this latter classification schema, 21.9 and 25.0 percent of episodes were categorized as complicated in the 1997 and 1998 samples, respectively.
Predictive Indices for Complicated Care Transitions
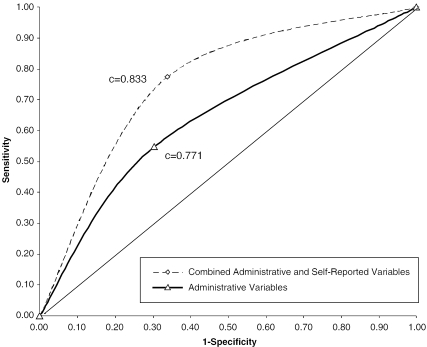
The parameter estimates for the 1997 sample variables included in the two models (i.e., the model using administrative variables only and the one using both administrative and self-reported variables) constructed to predict complicated care transitions are presented in Table 2. Figure 2 illustrates the receiver operating curves for both models using data from the 1998 validation sample. Both models accurately predicted complicated care patterns. The area under the receiver operating curves was 0.771 for the model restricted to administrative data only and 0.833 for the model utilizing a combination of administrative and self-reported data.
Table 2.
Parameter Estimates for the Two Predictive Indices
| Combined Administrative and Self-Reported Variables | |||||
|---|---|---|---|---|---|
| Parameter | DF | Estimate | Standard Error | Wald Chi-Square | P-Value |
| Intercept | 1 | −7.1499 | 1.5927 | 20.1529 | <0.001 |
| 80 yrs. of age or older | 1 | 0.0289 | 0.3919 | 0.0054 | 0.941 |
| Medicaid recipient | 1 | 1.2785 | 0.5175 | 6.1038 | 0.014 |
| Heart disease | 1 | 5.4719 | 1.5586 | 12.3250 | <0.001 |
| Prior stroke | 1 | −6.8802 | 3.1167 | 4.8733 | 0.027 |
| Cancer | 1 | −4.1493 | 2.4993 | 2.7563 | 0.097 |
| Diabetes | 1 | −1.5497 | 0.5448 | 8.0924 | 0.004 |
| No. of prior hospitalizations | 1 | 0.4826 | 0.1737 | 7.7199 | 0.006 |
| Self-rated general health | 1 | −0.1895 | 0.1959 | 0.9361 | 0.333 |
| Visual impairment | 1 | 1.9768 | 0.6168 | 10.2718 | 0.001 |
| Function score | 1 | 0.2408 | 0.2140 | 1.2663 | 0.261 |
| Assistance with ADL score | 1 | −0.9625 | 0.8738 | 1.2131 | 0.271 |
| Charlson comorbidity index | 1 | −0.0721 | 0.3000 | 0.0577 | 0.810 |
| Age*Medicaid | 1 | −2.3025 | 0.9314 | 6.1113 | 0.013 |
| Diabetes*Comorbidity | 1 | 0.8123 | 0.2258 | 12.9367 | <0.001 |
| Function*Comorbidity | 1 | −0.2095 | 0.1050 | 3.9758 | 0.046 |
| ADL*Comorbidity | 1 | 1.4267 | 0.4562 | 9.7819 | 0.002 |
| Stroke*Self-Rated Health | 1 | 1.4977 | 0.6820 | 4.8227 | 0.028 |
| Cancer*Self-Rated Health | 1 | 1.6282 | 0.5626 | 8.3768 | 0.004 |
| Heart Disease*Vision | 1 | −2.2555 | 0.6641 | 11.5359 | 0.001 |
| Heart Disease*Cancer | 1 | −2.7605 | 1.0610 | 6.7702 | 0.009 |
| Administrative Variables | |||||
| Parameter | DF | Estimate | Standard Error | Wald Chi-Square | Pr>ChiSq |
| Intercept | 1 | −4.8864 | 0.6996 | 48.7867 | <0.0001 |
| 80 yrs. of age or older | 1 | 1.2875 | 0.6243 | 4.2534 | 0.039 |
| Medicaid recipient | 1 | 2.0092 | 0.5518 | 13.2575 | <0.001 |
| Male | 1 | 0.6443 | 0.3601 | 3.2003 | 0.074 |
| Heart disease | 1 | 1.3054 | 0.5171 | 6.3737 | 0.012 |
| Cancer | 1 | 1.5582 | 0.6733 | 5.3552 | 0.021 |
| Diabetes | 1 | −1.3212 | 0.5105 | 6.6974 | 0.010 |
| No. of prior hospitalizations | 1 | 1.0779 | 0.2769 | 15.1496 | <0.0001 |
| Charlson comorbidity index | 1 | 0.1644 | 0.2235 | 0.5409 | 0.462 |
| Age*Medicaid | 1 | −1.7618 | 0.8062 | 4.7758 | 0.029 |
| Age*PriorHosp | 1 | −0.7989 | 0.3512 | 5.1755 | 0.023 |
| Age*Male | 1 | −2.6733 | 1.2094 | 4.8861 | 0.027 |
| Diabetes*Comorbidity | 1 | 0.5339 | 0.1751 | 9.2969 | 0.002 |
| PriorHosp*Comorbidity | 1 | −0.2868 | 0.1431 | 4.0195 | 0.045 |
| Heart Disease*Cancer | 1 | −2.1560 | 0.8523 | 6.3994 | 0.011 |
Figure 2.
Receiver Operating Curves (ROC) for Predicting Poor Care Transitions
Optimal sensitivity and specificity for the 1997 development sample were calculated to be 94.6 percent and 39.2 percent, respectively, for the model using administrative variables only and 98.1 percent and 44.7 percent, respectively, for the model using both administrative and self-reported variables. Optimal sensitivity and specificity for the 1998 validation sample were calculated to be 51.6 percent and 38.2 percent, respectively, for the model using administrative variables only and 61.3 percent and 45.0 percent, respectively, for the model using both administrative and self-reported variables.
Discussion
This investigation had three specific aims: (1) to describe the patterns and prevalence of care transitions among a sample of Medicare beneficiaries during a 30-day time period following an acute hospitalization; (2) to characterize the complexity of these care transitions; and (3) to develop and test two predictive indices designed to identify Medicare beneficiaries who are at greatest risk for complicated care transitions. With respect to the first aim, 46 distinct care patterns were observed among the Medicare beneficiaries in the study sample 30 days after hospital discharge. Sixty-one percent of beneficiaries experienced one transfer (among these 93 percent were discharged home), and 31 percent of beneficiaries experienced more than one posthospital transfer during the 30-day posthospitalization time period. With regard to the second aim, approximately one in eight 30-day care episodes in the 1998 sample were classified as complicated when rigidly applying the criteria evaluating transfers from lower- to higher-intensity care environments. When this criteria was broadened to include “lateral” transfers and “plateaus” in care, approximately one in four 30-day care episodes were deemed complicated. Regarding the third goal of the study, both of the indices designed to identify those beneficiaries at greatest risk for complicated care transitions (that is, the index based on administrative data only and the index based on administrative and self-reported data) were found to have acceptable predictive accuracy.
Few prior studies have addressed the three aims of this investigation, whether separately or collectively. In fact, little attention has been paid to the tracking of care transfers over time. Using the National Long Term Care Survey, Murtaugh and Litke (2002) found a prevalence rate of 24 percent for potential transition-related problems over a two-year time period, defined as emergency department visits, hospital admissions, and returns to an institutional setting following discharge to the community. Fairchild and colleagues developed a predictive index designed to identify patients who may require the use of postdischarge medical services; however, the index was constructed using a single study population (i.e., patients hospitalized at an urban teaching hospital) and relied on predictor variables that are not routinely available in the hospital setting (Fairchild et al. 1998). Prior studies have demonstrated that indices that utilize administrative or self-reported data have similar rates of predictive accuracy (Coleman et al. 1998; Roblin et al. 1999; Fethke, Smith, and Johnson 1986; Anderson and Steinberg 1985; Mukamel et al. 1997; Roos et al. 1988).
The findings from this investigation need to be considered within the broader context of improving the quality of care transitions among Medicare beneficiaries. This study provides important insights into the nature of post-acute care episodes and suggests that the needs of Medicare beneficiaries who are discharged after an acute hospitalization are both complex (requiring care from different practitioners in multiple settings) and ongoing (lasting 30 days or more). This understanding may help guide current attempts to modernize the Medicare program through the creation of financial incentives designed to improve posthospital care, such as bundling payments for acute and post-acute care services across episodes of care. At present, there is no uniformly accepted definition of an episode of care for Medicare beneficiaries.
Furthermore, the fact that over 30 percent of patients in this investigation underwent more than one posthospital transfer is significant since the potential for mismanagement or medical errors increases as patients undergo more care transitions (Coleman 2003; Institute of Medicine 2001; Murtaugh and Litke 2002). In addition, the significant number of care patterns in this study characterized as complicated (one in eight, and one in four episodes, depending upon the classification approach utilized) strongly emphasizes the need for both the system-level and patient-level approaches outlined in the Institute of Medicine report, Crossing the Quality Chasm: A New Health System for the Twenty-first Century (Institute of Medicine 2001).
Finally, this study has demonstrated that Medicare beneficiaries who are at risk for complicated care transitions can be identified with reasonable accuracy using either Medicare administrative data alone or a combination of administrative and self-reported data. Given the number of evidence-based interventions that are being tested to improve the quality of transitional care, the indices developed and tested in this study have immediate practical applications (Naylor et al. 1999; Rich et al. 1995; Philbin 1999; Townsend et al. 1988; Parry et al. 2003). Specifically, the instruments can be used to target specialized care coordination programs tested or implemented in health delivery systems.
This study has a number of strengths. First, the investigation utilized a nationally representative sample of Medicare beneficiaries to investigate three areas of posthospital care transitions that have previously received little to no attention. Second, in contrast to most studies reported in the literature, the findings from this study are contemporaneous—that is, the time period examined in this study (1997–1998) coincides with the implementation of the Balanced Budget Act that is believed to have influenced patterns of post-acute care service delivery (Angelelli et al. 2002). Third, the study tracked transfers over a 30-day time period and thereby extended our understanding of posthospital care beyond the initial discharge location. Finally, since hospital discharge planners and utilization managers often develop discharge plans based upon their clinical judgment, the application of an empirically derived instrument may provide a more reliable means for identifying patients in need of additional services and monitoring.
The findings of this study need to be considered in light of a number of limitations. First, this study was not able to evaluate all possible care transitions. The results reported in this study were heavily influenced by return to the hospital or emergency department because data on transfers to assisted living facilities, primary or specialty care, or home health care were not readily available from the MCBS. Second, the patterns of care in this study that resulted in recidivism may not have been due to transition-related problems. Collectively, the patients studied had a high burden of illness and some of the recidivism may have been attributable to the natural progression of moderate-to-advanced chronic illnesses. Third, in order to ensure that the functional status measurements used in the predictive indices were current, the Medicare samples were restricted to those patients with care episodes that occurred within four months of the annual MCBS functional assessment that takes place in September. It is unknown whether a temporal effect may have influenced the results of this study. Prior studies have demonstrated an association between transfers to and from acute care settings and functional status (Covinsky et al. 2003; Gill, Williams, and Tinetti 1999). Fourth, different health conditions have different periods of recovery that a 30-day episode may not fully encompass. Finally, it could be argued that identifying high-risk Medicare beneficiaries at the time of hospital discharge is a relatively “downstream” perspective that is more reactive than proactive. Nevertheless, hospital discharge was targeted in this study because it is unquestionably a time of great patient vulnerability and because there is a growing number of evidence-based interventions that show potential for significantly improving posthospital care transitions (Naylor et al. 1999; Rich et al. 1995; Philbin 1999; Townsend et al. 1988; Parry et al. 2003).
In summary, these findings demonstrate that posthospital transitions are common among Medicare beneficiaries and that the associated patterns of care vary greatly overly a relatively short time. Furthermore, the finding that a significant number of Medicare beneficiaries experience complicated posthospital care transitions has important implications for both patient safety and cost-containment. Finally, this study shows that Medicare beneficiaries who are at risk for experiencing complicated care transitions can be identified using data available at the time of hospital discharge. Thus, the predictive indices developed in this study may have direct application in matching high-risk patients with evidence-based interventions designed to improve posthospital care transitions.
Footnotes
Funding support was provided by the Paul Beeson Faculty Scholars in Aging Research, which is administered by the American Federation for Aging Research. The funding organization had no role in the design, conduct, or interpretation of the study, or the preparation of this manuscript.
References
- Adler G S. “A Profile of the Medicare Current Beneficiary Study.”. Health Care Financing Review. 1994;15(4):153–63. [PMC free article] [PubMed] [Google Scholar]
- Anderson G, Steinberg E. “Predicting Hospital Readmissions in the Medicare Population.”. Inquiry. 1985;22(3):251–8. [PubMed] [Google Scholar]
- Angelelli J, Gifford D, Intrator O, Gozalo P, Laliberte L, Mor V. “Access to Postacute Nursing Home Care before and after the BBA.”. Health Affairs. 2002;21(5):254–64. doi: 10.1377/hlthaff.21.5.254. [DOI] [PubMed] [Google Scholar]
- Ashton C, Kuykendall D, Johnson M, Wray N P, Wu L. “The Association between the Quality of Inpatient Care and Early Readmission.”. Annals of Internal Medicine. 1995;122(6):415–21. doi: 10.7326/0003-4819-122-6-199503150-00003. [DOI] [PubMed] [Google Scholar]
- Barker W H, Zimmer J G, Hall W J, Ruff B C, Freundlich C B, Eggert G M. “Rates, Patterns, Causes, and Costs of Hospitalization of Nursing Home Residents: A Population-Based Study.”. American Journal of Public Health. 1994;84(10):1615–20. doi: 10.2105/ajph.84.10.1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beers M, Sliwkowski J, Brooks J. “Compliance with Medication Orders among the Elderly after Hospital Discharge.”. Hospital Formulary. 1992;27:720–4. [PubMed] [Google Scholar]
- Boockvar K, Halm E, Litke A, Silberzweig S B, McLaughlin M A, Penrod J D, Magaziner J, Koval K, Strauss E, Siu A L. “Hospital Readmissions after Hospital Discharge for Hip Fracture: Surgical and Nonsurgical Causes and Effect on Outcomes.”. Journal of the American Geriatric Society. 2003;51(3):399–403. doi: 10.1046/j.1532-5415.2003.51115.x. [DOI] [PubMed] [Google Scholar]
- Centers for Medicare and Medicaid Services. The Medicare Current Beneficiary Survey. Available at http://www.cms.hhs.gov/mcbs/ [accessed June 17, 2004].
- Charlson M, Pompei P, Ales K, MacKenzie C R. “A New Method of Classifying Prognostic Comorbidity in Longitudinal Studies: Development and Validation.”. Journal of Chronic Disease. 1987;40(5):373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- Coleman E A. “Falling through the Cracks: Challenges and Opportunities for Improving Transitional Care for Persons with Continuous Complex Care Needs.”. Journal of the American Geriatric Society. 2003;51(4):549–55. doi: 10.1046/j.1532-5415.2003.51185.x. [DOI] [PubMed] [Google Scholar]
- Coleman E A, Boult C. “Improving the Quality of Transitional Care for Persons with Complex Care Needs.”. Journal of the American Geriatric Society. 2003;51(4):556–7. doi: 10.1046/j.1532-5415.2003.51186.x. [DOI] [PubMed] [Google Scholar]
- Coleman E A, Smith J D, Frank J, Eilertsen T B, Thiare J N, Kramer A M. “Development and Testing of a Measure Designed to Assess the Quality of Care Transitions.”. International Journal of Integrated Care. 2002;2(June):1–8. doi: 10.5334/ijic.60. Available at: http://www.ijic.org [accessed May 24, 2004] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman E A, Wagner E, Grothaus L, Hecht J A, Savarino J, Buchner D M. “Predicting Hospitalization and Functional Decline in Older Health Plan Enrollees: Are Administrative Data as Accurate as Self-Report?”. Journal of the American Geriatric Society. 1998;46(4):419–25. doi: 10.1111/j.1532-5415.1998.tb02460.x. [DOI] [PubMed] [Google Scholar]
- Cook R, Render M, Woods D. “Gaps in the Continuity of Care and Progress on Patient Safety.”. British Medical Journal. 2000;320(7237):791–4. doi: 10.1136/bmj.320.7237.791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Covinsky K E, Palmer R M, Fortinsky R H, Counsell S R, Stewart A L, Kresevic D, Burant C J, Landefeld C S. “Loss of Independence in Activities of Daily Living in Older Adults Hospitalized with Medical Illnesses: Increased Vulnerability with Age.”. Journal of the American Geriatric Society. 2003;51(4):451–8. doi: 10.1046/j.1532-5415.2003.51152.x. [DOI] [PubMed] [Google Scholar]
- Delgado-Rodriguez M, Gomez-Ortega A, Sillero-Arenas M, Llorca J. “Epidemiology of Surgical-Site Infections Diagnosed after Hospital Discharge: A Prospective Cohort Study.”. Infection Control and Hospital Epidemiology. 2001;22(1):24–30. doi: 10.1086/501820. [DOI] [PubMed] [Google Scholar]
- Densen P. “Tracing the Elderly through the Health Care System: An Update.”. AHCPR Monograph. 1991;91(11):1–36. [Google Scholar]
- Fairchild D, Hickey M, Cook E, McCarthy R M, Rossi L P, Timmons T C, Mangione M, Lee T H. “A Prediction Rule for the Use of Postdischarge Medical Services.”. Journal of General Internal Medicine. 1998;13(2):98–105. doi: 10.1046/j.1525-1497.1998.00025.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fethke C, Smith I, Johnson N. “Risk Factors Affecting Readmission of the Elderly into the Health Care System.”. Medical Care. 1986;24(5):429–37. doi: 10.1097/00005650-198605000-00006. [DOI] [PubMed] [Google Scholar]
- Forster A J, Murff H J, Peterson J F, Gandhi T K, Bates D W. “The Incidence and Severity of Adverse Events Affecting Patients after Discharge from the Hospital.”. Annals of Internal Medicine. 2003;138(161):167. doi: 10.7326/0003-4819-138-3-200302040-00007. [DOI] [PubMed] [Google Scholar]
- Gill T M, Williams C S, Tinetti M E. “The Combined Effects of Baseline Vulnerability and Acute Hospital Events on the Development of Functional Dependence among Community-Living Older Persons.”. Journal of Gerontology. 1999;54(7):M377–83. doi: 10.1093/gerona/54.7.m377. [DOI] [PubMed] [Google Scholar]
- Halm E, Magaziner J, Hannan E, Wang J J, Silberzweig S B, Boockvar K, Orosz G M, McLaughlin M A, Koval K J, Siu A L. “Frequency and Impact of Active Clinical Issues and New Impairments on Hospital Discharge in Patients with Hip Fracture.”. Archives of Internal Medicine. 2003;163(1):107–12. doi: 10.1001/archinte.163.1.107. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Crossing the Quality Chasm: A New Health System of the Twenty-first Century. Washington, DC: National Academy Press; 2001. [Google Scholar]
- Jones J S, Dwyer P R, White L J, Firman R. “Patient Transfer from Nursing Home to Emergency Department: Outcomes and Policy Implications.”. Academy of Emergency Medicine. 1997;4(9):908–15. doi: 10.1111/j.1553-2712.1997.tb03818.x. [DOI] [PubMed] [Google Scholar]
- Lewis M, Cretin S, Kane R. “The Natural History of Nursing Home Patients.”. Gerontologist. 1985;25(4):382–8. doi: 10.1093/geront/25.4.382. [DOI] [PubMed] [Google Scholar]
- Meredith S, Feldman P, Frey D, Giammarco L, Hall K, Arnold K, Brown N J, Ray W A. “Improving Medication Use in Newly Admitted Home Healthcare Patients: A Randomized Controlled Trial.”. Journal of the American Geriatric Society. 2002;50(9):1484–91. doi: 10.1046/j.1532-5415.2002.50402.x. [DOI] [PubMed] [Google Scholar]
- Mitchell D, Swift G, Gilbert G. “Surgical Wound Infection Surveillance: The Importance of Infections That Develop after Hospital Discharge.”. Aust NZ Journal of Surgery. 1999;69(2):117–20. doi: 10.1046/j.1440-1622.1999.01500.x. [DOI] [PubMed] [Google Scholar]
- Moore C, Wisnevesky J, Williams S, McGinn T. “Medical Errors Related to Discontinuity of Care from an Inpatient to an Outpatient Setting.”. Journal of General Internal Medicine. 2003;18(8):646–51. doi: 10.1046/j.1525-1497.2003.20722.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukamel D, Chou C, Zimmer J, Rothenberg B M. “The Effect of Accurate Patient Screening on the Cost-Effectiveness of Case Management Programs.”. Gerontologist. 1997;37(6):777–84. doi: 10.1093/geront/37.6.777. [DOI] [PubMed] [Google Scholar]
- Murtaugh C M, Litke A. “Transitions through Postacute and Long-Term Care Settings: Patterns of Use and Outcomes for a National Cohort of Elders.”. Medical Care. 2002;40:227–36. doi: 10.1097/00005650-200203000-00006. [DOI] [PubMed] [Google Scholar]
- Naylor M, Bowles K, Brooten D. “Patient Problems and Advanced Practice Nurse Interventions during Transitional Care.”. Public Health Nursing. 2000;17(2):94–102. doi: 10.1046/j.1525-1446.2000.00094.x. [DOI] [PubMed] [Google Scholar]
- Naylor M, Brooten D, Campbell R, Jacobsen B S, Mezey M, Pauly M V, Schwartz J S. “Comprehensive Discharge Planning and Home Follow-Up of Hospitalized Elders: A Randomized Clinical Trial.”. Journal of the American Medical Association. 1999;281(7):613–20. doi: 10.1001/jama.281.7.613. [DOI] [PubMed] [Google Scholar]
- Oddone E, Weinberger M, Horner M, Mengel C, Goldstein F, Ginier P, Smith D, Huey J, Farber N J, Asch D A, Loo L, Mack E, Hurder A G, Henderson W, Feussner J R. “Classifying General Medicine Readmissions.”. Journal of General Internal Medicine. 1996;11(10):597–607. doi: 10.1007/BF02599027. [DOI] [PubMed] [Google Scholar]
- Parry C, Coleman E A, Smith J, Frank J, Kramer A M. “The Care Transitions Intervention: A Patient-Centered Approach to Ensuring Effective Transfers between Sites of Geriatric Care.”. Home Health Care Services Quarterly. 2003;22(3):1–18. doi: 10.1300/J027v22n03_01. [DOI] [PubMed] [Google Scholar]
- Philbin E. “Comprehensive Multidisiplinary Programs for the Management of Patients with Congestive Heart Failure.”. Journal of General Internal Medicine. 1999;14:130–5. doi: 10.1046/j.1525-1497.1999.00291.x. [DOI] [PubMed] [Google Scholar]
- Rich M, Beckham V, Wittenberg C, Leven C L, Freedland K E, Carney R M. “A Multidisciplinary Intervention to Prevent the Readmission of Elderly Patients with Congestive Heart Failure.”. New England Journal of Medicine. 1995;333(18):1190–5. doi: 10.1056/NEJM199511023331806. [DOI] [PubMed] [Google Scholar]
- Roblin D, Juhn P, Preston B, Della Penna R, Feitelberg S P, Khoury A, Scott J. “A Low-Cost Approach to Prospective Identification of Impending High Cost Outcomes.”. Medical Care. 1999;37(7):1155–63. doi: 10.1097/00005650-199911000-00007. [DOI] [PubMed] [Google Scholar]
- Roos N, Roos L, Mossey J, Havens B. “Using Administrative Data to Predict Important Health Outcomes: Entry to Hospital, Nursing Home, and Death.”. Medical Care. 1988;26(3):221–39. doi: 10.1097/00005650-198803000-00001. [DOI] [PubMed] [Google Scholar]
- Siu A, Manning W, Benjamin B. “Patient, Provider and Hospital Characteristics Associated with Inappropriate Hospitalization.”. American Journal of Public Health. 1990;80(10):1253–6. doi: 10.2105/ajph.80.10.1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Townsend J, Piper M, Frank A O, Dyer S, North W R, Meade T W. “Reduction in Hospital Readmission Stay of Elderly Patients by a Community Based Hospital Discharge Scheme: A Randomised Controlled Trial.”. British Medical Journal. 1988;297:544–8. doi: 10.1136/bmj.297.6647.544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- vom Eigen K A, Walker J D, Edgman-Levitan S, Cleary P D, Delbanco T L. “Carepartner Experiences with Hospital Care.”. Medical Care. 1999;37(1):33–8. doi: 10.1097/00005650-199901000-00006. [DOI] [PubMed] [Google Scholar]
- Ware J E. SF-36 Health Survey, Manual and Interpretation Guide. Boston: The Health Institute, New England Medical Center; 1997. [Google Scholar]
- Weissman J, Ayanian J, Chasan-Taber S, Sherwood M J, Roth C, Epstein A M. “Hospital Readmissions and Quality of Care.”. Medical Care. 1999;37(5):490–501. doi: 10.1097/00005650-199905000-00008. [DOI] [PubMed] [Google Scholar]
- Waite K, Oddone E, Weinberger M, Samsa G, Foy M, Henderson W. “Lack of Association between Patients' Measured Burden of Disease and Risk for Hospital Readmission.”. Journal of Clinical Epidemiology. 1994;47(11):1229–36. doi: 10.1016/0895-4356(94)90127-9. [DOI] [PubMed] [Google Scholar]