Abstract
Objective
To analyze the blend of retrospective (fee-for-service, productivity-based salary) and prospective (capitation, nonproductivity-based salary) methods for compensating individual physicians within medical groups and independent practice associations (IPAs) and the influence of managed care on the compensation blend used by these physician organizations.
Data Sources
Of the 1,587 medical groups and IPAs with 20 or more physicians in the United States, 1,104 responded to a one-hour telephone survey, with 627 providing detailed information on physician payment methods.
Study Design
We calculated the distribution of compensation methods for primary care and specialty physicians, separately, in both medical groups and IPAs. Multivariate regression methods were used to analyze the influence of market and organizational factors on the payment method developed by physician organizations for individual physicians.
Principal Findings
Within physician organizations, approximately one-quarter of physicians are paid on a purely retrospective (fee-for-service) basis, approximately one-quarter are paid on a purely prospective (capitation, nonproductivity-based salary) basis, and approximately one-half on blends of retrospective and prospective methods. Medical groups and IPAs in heavily penetrated managed care markets are significantly less likely to pay their individual physicians based on fee-for-service than are organizations in less heavily penetrated markets.
Conclusions
Physician organizations rely on a wide range of prospective, retrospective, and blended payment methods and seek to align the incentives faced by individual physicians with the market incentives faced by the physician organization.
Keywords: Payment incentives, capitation, fee-for-service, medical group, independent practice association
Physician organizations such as medical groups and independent practice associations (IPAs) function as financial intermediaries between the insurer and the individual physician (Robinson 1999b; Penner 1997; Gold et al. 2002). In “three-tier” organizational settings, the insurance firm pays the physician organization on a prospective, retrospective, or blended basis and then the physician organization pays the individual physician, sometimes on a different basis (Conrad et al. 1998; 2002; Kralewski et al. 2000). Prior to the advent of managed care, insurers paid medical groups mostly on the same fee-for-service basis with which they paid physicians working in solo practice, and the medical groups paid their individual physicians on a compatible productivity-based salary schedule (i.e., fee-for-service). This compensation mechanism aligned the incentives of the individual physician with that of the physician organization, both of which profited by increasing the number and complexity of services performed. With the advent of managed care, many health maintenance organizations (HMOs) began to reimburse medical groups on a prospective, capitated basis. Continued payment of individual physicians on a fee-for-service basis created incentive misalignment between the individual physician and the physician organization.
This article analyzes the association between market penetration by managed care and the methods developed by physician organizations to pay their individual physician members. In the increasingly cost-conscious health care environment, medical groups are forced to balance the need to maintain individual physician productivity, for which fee-for-service is an effective incentive, with the need to limit the cost of the clinical services provided, for which capitation is an effective incentive. We hypothesize that physician organizations respond to these conflicting imperatives by developing payment methods that blend elements of fee-for-service with elements of capitation, with the relative weights assigned to each depending on the extent of cost-control pressure they face in their local market environment. This focus on blended payment methods for physicians extends the empirical literature on blended payments for hospitals (where Medicare's diagnosis related group [DRG] system includes both prospective and retrospective elements) and the theoretical literature on optimal payments in multi-task principal-agent relationships.
We use 2001 data collected as part of the National Study of Physician Organizations, which surveyed medical groups and IPAs with 20 or more physician members. The article presents the distribution of pure prospective, pure retrospective, and blended payment methods for both primary care and specialist physicians, for integrated medical groups and IPAs separately. Variation in payment methods among physician organizations is analyzed in terms of the penetration of the local market by HMOs and in terms of organizational factors such as scale, scope of services, and ownership of the physician entities. The article concludes with a brief discussion of the implications of the analysis for contemporary policy initiatives to improve the quality of care by changing methods of payment for physician organizations and individual physicians.
Blending and Aligning Incentives
In the era before the advent of managed care, insurers paid providers on a fee-for-service basis, knowing that this encouraged the provision of visits, tests, and procedures. Medical groups developed analogous productivity-based payment methods for their individual physician members. While employed physicians formally were paid a salary, their financial incentives were aligned with those of their medical group because the salary for each physician was keyed to the numbers of visits and procedures performed, the dollar amount of claims billed, the dollar amount of claims actually paid, or some other measure of individual productivity. As health care costs accelerated during the 1970s and 1980s, policymakers and purchasers sought to moderate the growth in utilization and expenditures. Purchasers increasingly contracted with HMOs, which then often contracted on a prospective, capitated basis with physician organizations (Robinson and Casalino 1995; 1996; Penner 1997). Where integrated medical groups were not available, physicians in solo and small group practice often formed independent practice associations (IPAs) for the purpose of contracting on a capitated basis with HMOs (Robinson 1999b; Grumbach et al. 1999).
Continued payment of individual physicians on a retrospective, fee-for-service basis when the medical group or IPA was paid on a prospective, capitated basis misaligned incentives between the individual and the organization. While cost-conscious practice styles among individual physicians could be fostered through nonfinancial mechanisms such as utilization review, the internal tensions thereby created would place ever-greater burden on the governance and leadership of the physician organizations. Medical groups and IPAs began to shift from pure fee-for-service to pure capitation or to blends of prospective and retrospective methods for their physician members. The limited available studies have reported that IPAs often combine individual capitation with fee-for-service for selected procedures or, alternatively, combine fee-for-service with a prospectively determined bonus (Robinson 1999a; Rosenthal et al. 2002). Integrated medical groups pay physicians on a salaried basis, with salaries keyed to productivity, panel size, and other factors. The actual mix of prospective and retrospective elements, in terms of the percentage of the compensation received by individual physicians from capitation and fee-for-service, has not been quantified, nor have the determinants of variation among physician organization in payment methods.
The blending of retrospective and prospective payment methods under the imperative to balance conflicting incentives falls within the scope of the economic literature on principal–agent relationships and, in particular, the literature on optimal contracts in the context of multitask agency relationships. The canonical analysis of payment mechanisms focuses on the balancing of risk aversion with moral hazard (Pratt and Zeckhauser 1985; Eisenhardt 1989; Sappington 1991). Retrospective payment methods such as fee-for-service shift the risk-bearing function from the agent (in this case, the physician) back to the principal (in this case, the insurer). This allocation of risk is efficient because insurers are better able than are individual physicians to bear the financial consequences of attracting particularly sick patients and having unexpected, costly developments during the course of treatment. Fee-for-service functions as a natural risk-adjuster, as physicians who attract particularly sick patients in need of costly interventions are correspondingly paid more (Newhouse 1996). However, to the extent retrospective payments are set at rates exceeding the marginal cost to the physician of providing additional services to the patient, they create financial incentives for the provision of more care than would be provided in an incentive-neutral context. In practice, retrospective payment levels are always set above marginal costs due to the need to cover the overhead costs of the physician practice. The static inefficiency of overtreatment for any particular standard of care is compounded by the dynamic inefficiencies created by retrospective payment methods, which encourage the diffusion of new clinical products and procedures even if they would fail a cost-benefit analysis.
Prospective physician payment mechanisms such as capitation (fixed payment per patient per month) create an analogous combination of desirable and undesirable incentives. Capitation creates financial incentives for cost-conscious practice patterns, because physicians retain any savings generated by reductions in utilization, complexity, or unit prices. The broader the scope of clinical services brought under the umbrella of capitation payment, the greater the opportunity for physicians to change practice patterns in ways that reduce costs (Berwick 1996). However, capitation shifts to the physician the financial risk of attracting patients whose need for care exceeds the average upon which the payment rate is based, and hence rewards avoidance of the sick and attraction of the healthy. The cost-decreasing incentives inherent in prospective payment also reward practice patterns that deliver an inadequate level of service to the patient. The static inefficiency of under-treatment is compounded by the dynamic inefficiencies of inadequate reward for new products and procedures that would pass a cost-benefit analysis (Cutler and McClellan 2001).
Despite the theoretical virtues of blended payment methods, it is important to highlight the offsetting virtues of unblended methods such as pure fee-for-service or pure capitation. A major limitation on blended payment methods is the difficulty in administering complex incentives and the difficulty in explaining them to those whose behavior they are intended to influence (Baker, Jensen, and Murphy 1988; Robinson 2001). The continuing prevalence of pure fee-for-service and pure capitation, despite their theoretical limitations, is due, at least in part, to their ease of administration and interpretation.
The agency framework on optimal payment incentives has been applied to the health care context by Newhouse (1996) and Ellis and McGuire (1986; 1988; 1993). The extant literature has centered on hospital payment methods and, in particular, the transition from Medicare's retrospective, cost-based method to the partially prospective DRG method. McClellan (1997) estimates that only 12 percent of the variance in payments made under the “prospective payment system” in fact are based on prospective (principal diagnosis and comorbidities) factors, with the majority based on retrospective factors such as procedures performed (29 percent) and outlier payments (46 percent). The literature on blended payment methods has not been applied to the physician context of managed care, which in many markets generated a “three-tier” structure in which the HMO pays the physician organization and then the physician organization pays the individual physician. Rosenthal et al. (2002) argue that physician organizations buffer the individual physician from the full force of the prospective payment incentives generated by the HMOs, in that medical groups paid on a capitated basis typically subcapitate individual physicians only for the services they provide individually (and not for the full range of services used by their patients). In the subsequent analysis, we quantify the effect of managed care on payment incentives by measuring the association between HMO market penetration and the percentage of individual physician compensation received through fee-for-service, with the expectation being that higher rates of managed care penetration are associated with less reliance on fee-for-service as a method of payment.
Economic theory yields conflicting predictions concerning the influence of organizational scale and scope on the structure of individual compensation methods and, in particular, on the weight assigned to individual productivity (fee-for-service). The monitoring of individual contributions becomes more difficult as organizations become larger and more diverse. Free-riding will be a greater concern in larger medical groups, those with both primary care and specialty physicians, and those owned by large nonphysician entities such as hospitals and staff model HMOs, compared to small, single-specialty, and independent groups (Gaynor and Pauly 1990). This suggests that payment methods will be more heavily weighted towards fee-for-service in large and diverse groups than in small, single-specialty groups. On the other hand, large and diverse organizations must be concerned about the pursuit by each individual and business unit of subgoals that interfere with the larger organization's overall performance. For example, piece rate payment has been abandoned in much of the nonhealth sector, despite its spur to individual productivity, due to the potential for wastage of material and inability to adequately reward effort devoted to projects where cooperation is key (Alchian and Demsetz 1972; Baker, Jensen, and Murphy 1988; Lazear 1989; Prendergast 1999). Joint production activities tend to be characterized by low-powered payment mechanisms such as straight salary rather than piece rates or commissions, in order to encourage cooperation and discourage unproductive “influence” activities (Milgrom and Roberts 1988). Low-powered, nonproductivity-based salaries also will be prevalent in large medical groups if the physicians who affiliate with those entities are more adverse to business risk than the entrepreneurial physicians attracted to small groups (Gaynor and Gertler 1995). There may be differences between integrated medical groups and IPAs in the association between scale and compensation method, as large medical groups with employed physicians can rely on peer monitoring and pressure to sustain productivity whereas IPAs must rely principally on payment methods as incentives for their dispersed membership.
Data and Methods
Data for this analysis were derived from the National Study of Physician Organizations and the Management of Chronic Illness (NSPO), which has been described in detail elsewhere (Gillies et al. 2003; Casalino et al. 2003). The NSPO is a survey of all medical groups and IPAs in the United States, derived from the five principal lists of physician organizations, after elimination of duplicative entries, those with fewer than 20 physicians, and those composed solely of hospital-based physicians or opthamologists. Of the 1,587 organizations fitting the study criteria, 1,104 (70 percent) responded to the one-hour telephone survey (which included a written component for financial questions). Specially trained interviewers at the National Opinion Research Center conducted the surveys with the president, CEO, or medical director of each physician organization. Responding organizations did not differ from nonrespondents by size or state, but response rates were higher for IPAs (79 percent) than for medical groups (66 percent). The surveys were conducted between September 2000 and September 2001.
The most important distinction among physician organizations, for purposes of understanding the methods by which they compensate individual clinicians, is between integrated medical groups and IPAs. The integrated medical group employs individual physicians (who may also be partners and owners of the organization) and therefore pays them a salary rather than directly on a fee-for-service or capitated basis. Physician salaries can be based on individual productivity, as measured by patient visits, procedures, relative value units, or percentage of charges. Despite having the legal structure of a salary, these productivity-based salary mechanisms have the economic structure of fee-for-service. Alternatively, the salary of the medical group physician can be divorced from direct productivity and be based on seniority or specialty. An intermediate basis for the salaries of employed physicians is panel size, the number of patients assigned to the particular physician. The IPA is a network form of organization that contracts with, rather than employs, the individual physician (Robinson and Casalino 1996; Grumbach et al. 1999). The individual physicians may belong to multiple IPAs and, in addition, receive some of their patients and revenue without the intermediary of any IPA. The IPA cannot pay a salary to the physician, as it is not the employer. Rather, the IPA compensates its physician members contractually on a fee-for-service, capitated, or blended payment mechanism. Capitation payment from the IPA to the physician is analogous to partial salary from a medical group to the physician. For example, a capitated solo practitioner who belonged to only one IPA and received all patients through the IPA would effectively be salaried, with the “salary” based on panel size.
The NSPO respondents were asked to describe the compensation method used for primary care and specialty physicians, respectively, in terms of the percentage of annual income derived from each of several indicated sources. For IPAs, the categories included fee-for-service and capitation, which are clearly retrospective and prospective payment methods, respectively, plus quality of care, organizational service, and other. Medical groups pay their members on a salaried basis, so responding organizations were asked to categorize the basis of the salaries in terms of individual productivity (patient visits, procedures, etc.), panel size, or straight salary (e.g., specialty, seniority), plus quality, organizational service, and other. In the subsequent analysis of medical group compensation methods, we combine straight salary and salary based on panel size into one category, to contrast them with salary based on number of visits and procedures, the equivalent of fee-for-service (only 2 percent of medical groups base salaries on panel size). Only 6 percent of compensation within medical groups and 1 percent of compensation within IPAs was based on quality, organizational service, or other.
This study used as its measure of physician compensation method the percentage of annual income for primary care and specialty physicians that derives from productivity-based salary (medical groups) and fee-for-service (IPAs). For purposes of analyzing compensation blends, the entire distribution rather than just the mean of these measures across physician organizations is important. We present histograms of these variables for primary care and specialty physicians in medical groups and IPAs, separately. The variation in payment blends among physician organizations was analyzed using multivariate linear regression methods. As the dependent variable is constrained to lie between zero and 100, we experimented with both the logarithmic transformation and the log-odds transformation (Y=log[X/{100−X}]).
The measure of managed care penetration and the consequent incentive for each physician organization to adopt prospective payment methods for individual physicians is the percentage of the nonelderly insured population enrolled in HMOs, using the Metropolitan Statistical Area as the definition of the local market. This variable is based on the annual Interstudy survey of HMOs and obtained from Professor Douglas Wholey at the University of Minnesota. To capture nonlinearities in the relationship between managed care penetration and physician payment method, we transform the market share variable into four dichotomous variables representing the four quartiles of HMO penetration. The scale and scope of the physician organizations were measured in terms of total number of physician members and whether the organization included primary care only, specialty care only, or both primary and specialty physicians (which we refer to as “multispecialty”). We also included measures of whether the physician organization was owned by a hospital system or HMO and the number of years since the founding of the group. To the extent that organizations are imprinted by the principles and procedures prevalent when they were founded and find it difficult to change even in the face of changes in the environment, as argued by sociological theories of organizational ecology (Hannan and Freeman 1977), older medical groups will be more likely to rely on fee-for-service and less likely to rely on prospective payment methods than more recently established organizations.
Results
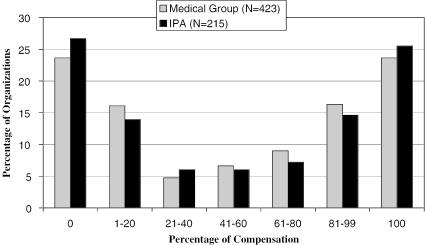
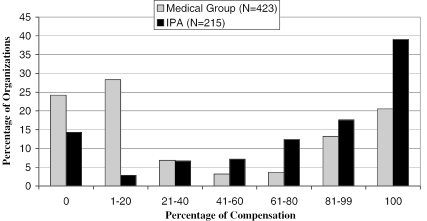
Figure 1 presents the distribution of medical groups and IPAs, respectively, in terms of the percentage of primary care compensation based on fee-for-service. Approximately one quarter of medical groups and IPAs pay primary care physicians purely on individual productivity. Approximately the same percentage base none of compensation on productivity, and the remaining half pay primary care physicians using a blend of retrospective and prospective mechanisms. Analogous findings are presented in Figure 2 for physician specialists. The reliance on pure fee-for-service within IPAs for specialists (40 percent) is higher than for primary care physicians (25 percent). Integrated medical groups rely on fee-for-service for specialists much less than do IPAs, with approximately one quarter of medical groups basing none of specialist compensation on fee-for-service (compared to 14 percent in IPAs) and another quarter basing less than one-fifth of specialist compensation on fee-for-service (compared to 3 percent in IPAs). Medical groups utilize very similar payment blends for primary care and specialty physicians (correlation coefficient 0.87), whereas IPAs tend to compensate primary care and specialty physician members somewhat differently (correlation coefficient 0.54). Nevertheless, the data on specialist payment shows the same relatively even split between blended and unblended mechanisms as for primary care physicians in both medical groups and IPAs.
Figure 1.
Percentage of Primary Care Compensation Based on Productivity (Fee-for-Service) in Physician Organizations
Figure 2.
Percentage of Specialist Compensation Based on Productivity (Fee-for-Service) in Physician Organizations
Table 1 presents descriptive statistics for the payment, market, and organizational variables for medical groups and IPAs, respectively. In addition to the differences in payment mechanisms highlighted in the figures, medical groups and IPAs differ in managed care market penetration, organizational scale, age, primary care and specialty mix, and ownership by a hospital or HMO. Independent practice associations tend to be located in markets with high HMO penetration, with almost a third being in markets where HMOs enroll more than 45 percent of the insured population, whereas only 22 percent of medical groups are in the most heavily penetrated markets. Independent practice associations include significantly more physicians than do medical groups; this reflects the fact that individual physicians within IPAs often belong to multiple organizations and, in addition, receive many patients without any organizational intermediary. Approximately 70 percent of medical groups and almost 90 percent of IPAs include both primary care and specialist physicians (“multispecialty”). Two-fifths of medical groups and one-fifth of IPAs are owned by a larger hospital or HMO system. Medical groups tend to be older that IPAs, with an average of 22 years since establishment compared to an average of 8 years for IPAs.
Table 1.
Descriptive Statistics on Medical Groups and IPAs: Compensation Methods, HMO Market Penetration, and Organizational Characteristics
| Medical Groups | IPAs | |
|---|---|---|
| Primary care payment based on productivity (%) | 51.8 (42.4) | 41.6 (43.0) |
| Specialist payment based on productivity (%) | 51.0 (43.1) | 71.2 (36.6) |
| HMO market penetration, 0–20% | 0.26 (0.44) | 0.18 (0.38) |
| HMO market penetration, 21–30% | 0.24 (0.43) | 0.27 (0.45) |
| HMO market penetration, 31–45% | 0.29 (0.45) | 0.24 (0.43) |
| HMO market penetration, more than 45% | 0.22 (0.41) | 0.32 (0.47) |
| Number of physicians | 128.8 (289.3) | 406.2 (521.3) |
| Multispecialty physician membership | 0.70 (0.21) | 0.88 (0.11) |
| Owned by hospital or HMO | 0.44 (0.50) | 0.18 (0.39) |
| Age of organization (years) | 22.3 (22.7) | 8.26 (6.11) |
| N | 423 | 215 |
Note: Standard deviations in parentheses.
Table 2 presents parameter estimates for the influence of market and organizational factors on the choice of physician compensation mechanism by medical groups and IPAs, respectively. The reliance on fee-for-service and productivity-based salary declines sharply as the penetration of the market by HMOs grows, for both forms of physician organization and for both primary care and specialty physicians. Compared to medical groups in markets with less than 20 percent managed care, medical groups in markets with greater HMO penetration base salaries an average of 12 to 17 percentage points less on productivity for primary care physicians and 12 to 21 percentage points less for specialists. Compared to IPAs in markets with less than 20 percent managed care, IPAs in heavily penetrated markets base primary care compensation 23 to 41 percentage points less on fee-for-service, and specialist compensation 8 to 26 percent percentage points less. There is a monotonic relationship between market penetration and physician payment method for specialists but not for primary care physicians. The principal difference is between organizations in markets with the least penetration and organizations in all other market contexts, rather than there being differences within the subset of more penetrated markets. While all the market penetration coefficients are different from zero at conventional levels of statistical significance, they are not significantly different from one another.
Table 2.
Determinants of the Percentage of Physician Earnings Based on Individual Productivity: Productivity-based Salary (Medical Groups) and Fee-for-Service (IPAs)
| Medical Groups | IPAs | |||
|---|---|---|---|---|
| Primary Care | Specialty Care | Primary Care | Specialty Care | |
| HMO Market Penetration, 21–30% | −13.21** | −12.97** | −39.36*** | −8.27 |
| (5.59) | (5.25) | (8.52) | (7.67) | |
| HMO Market Penetration, 31–45% | −17.00*** | −16.90*** | −23.06*** | −18.80** |
| (5.33) | (5.10) | (8.77) | (7.86) | |
| HMO Market Penetration, Greater Than 45% | −12.37** | −21.10*** | −41.66*** | −26.08*** |
| (5.80) | (5.50) | (8.23) | (7.43) | |
| Number of Physicians | −0.017** | −0.016** | 0.010* | 0.013*** |
| (0.007) | (0.006) | (0.005) | (0.005) | |
| Multispecialty | 2.01 | 29.11*** | 2.77 | 34.93*** |
| (5.54) | (4.95) | (10.64) | (11.45) | |
| Owned by Hospital or HMO | −19.54*** | −23.75*** | 3.99 | 2.12 |
| (4.22) | (4.15) | (7.09) | (6.21) | |
| Age of Organization | 0.233*** | 0.212*** | 0.405 | −0.190 |
| (0.087) | (0.082) | (0.468) | (0.400) | |
| Intercept | 67.27 | 46.86 | 59.29 | 48.39 |
| (6.48) | (5.59) | (11.58) | (13.14) | |
| Adjusted R2 | 0.14 | 0.22 | 0.11 | 0.12 |
| N | 412 | 423 | 215 | 206 |
Note: Standard errors in parentheses. Sample sizes differ because organizations without primary care physicians are not included in regressions for primary care payment method, and analogously for the specialist payment regressions.
=p<.10;
=p<.05;
=p<.01.
We tested the robustness of the association between managed care penetration and physician payment method in several ways. The NSPO, which was mainly a telephonic survey, included a supplemental written component on financial specifics that queried medical groups and IPAs concerning the percentage of their annual revenue derived from capitation. Unfortunately, only approximately half the respondents to the telephone survey completed this financial supplement. Nevertheless, for those who did complete the financial component, we were able to derive a measure of the financial incentive facing the organization to control costs (in addition to our measure of HMO market penetration). Substitution of this measure for the HMO market penetration variable generated an analogous negative association between the financial incentive facing the physician organization to limit costs and the percentage of compensation for individual physicians paid through fee-for-service. We also experimented with transformations of the dependent variable (logarithmic and log-odds) in order to attenuate the effect of the constrained range (from zero to 100 percent); results were very similar to those reported in Table 2 for the untransformed dependent variable.
Significant differences are observed between medical groups and IPAs in the association between organizational scale (number of physicians) and payment mechanism. Larger medical groups are less likely than smaller groups to base salaries on individual productivity, whereas larger IPAs are more likely than smaller IPAs to pay their member physicians on a fee-for-service basis (significant for specialists only). Older medical groups are more likely to pay on a fee-for-service basis than are those established more recently, whereas there is no association between organizational age and physician payment method for IPAs. Medical groups owned by hospitals and HMOs base salaries significantly less on productivity than do physician-owned medical groups; no effect of ownership on payment method is observed in IPAs. The effect of diversity in physician training and practice is quite large, with multispecialty medical groups basing compensation 29 percentage points more on productivity than primary care and specialty-only groups, while multispecialty IPAs base compensation 34 percentage points more on fee-for-service than primary care and specialty-only IPAs. Taken together, the available organizational and environmental variables account for only a modest percentage of the variance in physician payment mechanisms, with adjusted R-squares ranging from 0.14 for primary care to 0.22 for specialty physician payment within medical groups and from 0.11 to 0.12 within IPAs.
Discussion
Half the medical groups and IPAs in the nation pay individual physicians, including both primary care and specialty practitioners, on a blended basis that combines elements of prospective and retrospective incentives. This is consistent with the conceptual framework that physician organizations need to balance incentives for individual productivity and acceptance of severely ill patients (fee-for-service) with incentives for team cooperation and cost control (capitation). It echoes the blending of retrospective and prospective payment incentives found in Medicare's hospital payment system. However, almost half of IPAs pay their physicians either pure fee-for-service or pure capitation and half of medical groups pay their physicians' salaries based purely on productivity or not at all based on productivity. Among physician organizations that pay on one of these unblended bases, there is an almost even split between those that pay purely on a retrospective basis and those that pay purely on a prospective basis. If we define “mostly” as comprising groups that base 80–100 percent of physician compensation on fee-for-service, 45 percent of physicians in medical groups are paid mostly fee-for-service and approximately 35 percent are paid mostly nonproductivity salary. The distribution of payment blends also is bimodal within IPAs, though there is a greater reliance on fee-for-service for specialists than for primary care physicians. Almost 60 percent of IPA specialists are paid mostly fee-for-service, compared to 35 percent of their primary care colleagues. The continuing presence of pure prospective and retrospective payments highlights the virtues of administrative simplicity and ease of interpretation for unblended methods.
High market penetration by HMOs, with their emphasis on capitation as a payment method for physician organizations, is associated with greater reliance on capitation and lesser reliance on fee-for-service for individual physicians. Compared to medical groups and IPAs in markets with less than 20 percent HMO penetration, physician organizations in the most heavily penetrated (more than 45 percent) markets are only half as likely to rely on fee-for-service payment for their individual practitioners. For example, physician organizations in the most highly penetrated markets base an average of 40 percent of primary care compensation on productivity (given the sample average of 48 percent and controlling for the organizational covariates in Table 2), while organizations in the least penetrated markets base an average of 67 percent on productivity. For specialists, physician organizations in the least penetrated markets base 73 percent of compensation of productivity while those in the most penetrated markets base 48 percent on productivity (given the sample average of 57 percent and after adjusting for the organizational covariates).
Large medical groups are less likely than small groups to pay their physicians on a productivity basis, while large IPAs are more likely to rely on fee-for-service and less likely to rely on capitation than small IPAs. This difference in productivity incentives highlights the difference between the range of incentive instruments available to integrated organizations with employed physicians, on the one hand, and those available to loosely structured network organizations, on the other hand. Medical groups are better able to supplement financial incentives with nonfinancial measures such as peer pressure, production quotas, and threat of termination. For specialist payment, medical groups and IPAs that include both specialists and primary care physicians are substantially more likely to rely on fee-for-service than are primary care or specialty-only organizations. Medical groups owned by hospitals and HMOs are substantially less likely to rely on fee-for-service than are physician-owned groups and IPAs. This finding is consistent with the hypothesis that large and diverse organizations favor low-powered incentives such as straight salary rather than piece rates and also may help explain the weak financial performance of many “integrated delivery systems” in recent years (Burns and Pauly 2002). Journalistic accounts frequently report that patient visits and procedures declined after physicians sold their practices to hospitals, leading to a drop in revenue and profitability, and that hospital-based systems now are seeking to reintroduce productivity incentives by basing a higher percentage of total compensation on visits, procedures, or relative value units.
Policy Implications
Large numbers of physician organizations use each of the physician compensation methods examined in this study: unblended fee-for-service, unblended capitation, straight salary, and blended methods. Policies designed to use physician payment methods to influence the quantity or quality of care provided by physician organizations will have to take account of this diversity. Policy initiatives specific to each type of payment method must be developed, implemented, and evaluated. Fee-for-service rewards the provision of more services and capitation rewards the provision of fewer services, but the implications of service volume on patient outcome varies across contexts. In its survey of the research literature on quality of care, the Institute of Medicine (2001) highlighted the simultaneous underuse of appropriate services, for which fee-for-service might be the preferred corrective incentive, and of overuse of inappropriate services, for which capitation might improve quality. In the context of quality deficiencies, interest is growing in linking physician compensation more explicitly to quality improvement. To date there is little evidence to guide policy in this area. As reviewed by Miller and Luft (1997), the extensive literature on managed care and quality finds no consistent influence, either positive or negative, of payment incentives on quality.
Innovative ideas about how to adapt fee-for-service, capitation, and blended physician payment methods to improve the quality of care are emerging (Institute of Medicine 2001). For example, fee-for-service payment could be adapted to provide incentives for quality improvement by establishing reimbursement for care coordination activities and for services outside of the traditional office visit, including phone consults with patients, coordination of care provided to complex cases, use of electronic media to communicate with patients, and follow-up with patients on lab tests. These activities could be compensated through a monthly payment based on panel size, as a supplement to the fee-for-service payment for office visits, as an alternative to seeking to develop fee codes for each new non-office service. For physicians paid on a capitated basis within IPAs, the administration of vaccinations, preventive screenings, and other quality-enhancing procedures increasingly is rewarded by fee-for-service supplements to the monthly capitation payment. Pay-for-performance initiatives in California, which link capitation payments to medical groups and IPAs to quality performance, is leading those physician organizations to link individual physician compensation to the same set of quality metrics. In the context of noncapitated PPO networks, individual physicians can be paid quality-based bonuses as a supplement to annual fee-for-service claims, as pioneered by the Blue Cross/Blue Shield plan in Hawaii and recently adopted by Blue Cross of California.
Compensation methods for physician services often include both prospective and retrospective elements and vary substantially among organizations according to managed care market penetration, number of physicians, specialty mix, and ownership. Policy and purchaser efforts to improve quality of care through financial incentives must take this complexity into account and adopt a pragmatic approach that accommodates diversity and fosters experimentation. Payment methods in a complex task environment are correspondingly complex, and efforts to promote a particular goal (e.g., promotion of preventive services, care coordination for chronic conditions, error reduction in medications) need to base themselves on an understanding of the multiplicity of tasks and incentives that are already in place, if the new initiatives are to prove effective and sustainable.
Footnotes
This study was funded by the Robert Wood Johnson Foundation.
References
- Alchian A A, Demsetz H. “Production, Information Costs, and Economic Organization.”. American Economic Review. 1972;62(5):777–95. [Google Scholar]
- Baker G P, Jensen M C, Murphy K J. “Compensation and Incentives: Practice vs. Theory.”. Journal of Finance. 1988;43(3):593–616. [Google Scholar]
- Berwick D M. “Payment by Capitation and the Quality of Care.”. New England Journal of Medicine. 1996;335(16):1227–31. doi: 10.1056/NEJM199610173351611. [DOI] [PubMed] [Google Scholar]
- Burns L R, Pauly M V. “Integrated Delivery Networks: A Detour on the Road to Integrated Health Care?.”. Health Affairs. 2002;21(4):128–43. doi: 10.1377/hlthaff.21.4.128. [DOI] [PubMed] [Google Scholar]
- Casalino L P, Gillies R R, Shortell S M, Schmittdiel J, Bodenheimer T, Robinson J, Rundall T, Oswald N, Schauffler H, Wang M. “External Incentives, Information Technology, and Organized Processes to Improve Health Care Quality for Patients with Chronic Diseases.”. Journal of the American Medical Association. 2003;289(4):434–41. doi: 10.1001/jama.289.4.434. [DOI] [PubMed] [Google Scholar]
- Conrad D A, Maynard C, Cheadle A, Ramsey S, Marchs-Smith M, Kirz H, Madden C A, Martin D, Perrin E B, Wickizer T, Zierler B, Ross Z, Noren J, Liang S Y. “Primary Care Physician Compensation Method in Medical Groups.”. Journal of the American Medical Association. 1998;279(11):853–8. doi: 10.1001/jama.279.11.853. [DOI] [PubMed] [Google Scholar]
- Conrad D A, Sales A, Liang S, Chaudhuri C, Maynard C, Pieper L, Weinstein L, Gans D, Piland N. “The Impact of Financial Incentives on Physician Productivity in Medical Groups.”. Health Services Research. 2002;37(4):885–905. doi: 10.1034/j.1600-0560.2002.57.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutler D M, McClellan M. “Is Technological Change in Medicine Worth It?.”. Health Affairs. 2001;20(5):11–29. doi: 10.1377/hlthaff.20.5.11. [DOI] [PubMed] [Google Scholar]
- Eisenhardt K M. “Agency Theory: An Assessment and Review.”. Academy of Management Review. 1989;14(4):57–74. [Google Scholar]
- Ellis R P, McGuire T G. “Provider Behavior under Prospective Reimbursement: Cost Sharing and Supply.”. Journal of Health Economics. 1986;5(2):129–51. doi: 10.1016/0167-6296(86)90002-0. [DOI] [PubMed] [Google Scholar]
- Ellis R P, McGuire T G. “Insurance Principles and the Design of Prospective Payment Systems.”. Journal of Health Economics. 1988;7(2):215–37. doi: 10.1016/0167-6296(88)90026-4. [DOI] [PubMed] [Google Scholar]
- Ellis R P, McGuire T G. “Supply-Side and Demand-Side Cost Sharing in Health Care.”. Journal of Economic Perspectives. 1993;7(3):135–51. doi: 10.1257/jep.7.4.135. [DOI] [PubMed] [Google Scholar]
- Gaynor M, Gertler P. “Moral Hazard and Risk Spreading in Partnerships.”. Rand Journal of Economics. 1995;26(4):591–613. [Google Scholar]
- Gaynor M, Pauly M V. “Compensation and Productive Efficiency in Partnerships: Evidence from Medical Group Practice.”. Journal of Political Economy. 1990;98(31):544–73. [Google Scholar]
- Gillies R R, Shortell S M, Casalino L P, Wang M C, Schmittdiel J, Pswald N, Robinson J, Bodenheimer T, Rundall T, Schauffler H. “The National Study of Physician Organizations: Database Development, Comparisons, and Implications.”. 2003. Unpublished manuscript. Berkeley: University of California.
- Gold R M, Lake T, Hurley R, Sinclair M. “Financial Risk Sharing with Providers in Health Maintenance Organizations, 1999.”. Inquiry. 2003;39(1):34–44. doi: 10.5034/inquiryjrnl_39.1.34. [DOI] [PubMed] [Google Scholar]
- Grumbach K, Coffman J, Vranizan K, Blick N, O'Neil E. “Independent Practice Association Medical Groups in California.”. Health Affairs. 1999;17(3):227–37. doi: 10.1377/hlthaff.17.3.227. [DOI] [PubMed] [Google Scholar]
- Hannan M T, Freeman J H. “The Population Ecology of Organizations.”. American Journal of Sociology. 1977;82(5):929–64. [Google Scholar]
- Institute of Medicine. Crossing the Quality Chasm: A New Health System for the Twenty-first Century. Washington DC: National Academy Press; 2001. [Google Scholar]
- Kralewski J E, Rich E C, Feldman R, Dowd B, Bernhardt T, Johnson C, Gold W. “The Effects of Medical Group Practice and Physician Payment Methods on Costs of Care.”. Health Services Research. 2000;35(3):591–613. [PMC free article] [PubMed] [Google Scholar]
- Lazear E P. “Pay Equality and Industrial Politics.”. Journal of Political Economy. 1989;97(3):561–80. [Google Scholar]
- McClellan M. “Hospital Reimbursement Incentives: An Empirical Analysis.”. Journal of Economics and Management Strategy. 1997;6(1):91–128. [Google Scholar]
- Milgrom P, Roberts J. “An Economic Approach to Influence Activities in Organizations.”. American Journal of Sociology. 1988;94(Supplement):154–79. [Google Scholar]
- Miller R H, Luft H S. “Does Managed Care Lead to Better or Worse Quality of Care?.”. Health Affairs. 1997;16(5):7–25. doi: 10.1377/hlthaff.16.5.7. [DOI] [PubMed] [Google Scholar]
- Newhouse J P. “Reimbursing Health Plans and Health Providers: Efficiency in Production versus Selection.”. Journal of Economic Literature. 1996;34(3):1236–63. [Google Scholar]
- Penner M J. Capitation in California: A Study of Physician Organizations Managing Risk. Chicago: Health Administration Press; 1997. [Google Scholar]
- Pratt J W, Zeckhauser R J. Principals and Agents: The Structure of Business. Cambridge, MA: Harvard University Press; 1985. [Google Scholar]
- Prendergast C. “The Provision of Incentives in Firms.”. Journal of Economic Literature. 1999;37(1):7–63. [Google Scholar]
- Robinson J C. “Blended Payment Methods in Physician Organizations under Managed Care.”. Journal of the American Medical Association. 1999a;282(13):1258–63. doi: 10.1001/jama.282.13.1258. [DOI] [PubMed] [Google Scholar]
- Robinson J C. The Corporate Practice of Medicine: Competition and Innovation in Health Care. Berkeley: University of California Press; 1999b. [Google Scholar]
- Robinson J C. “Theory and Practice in the Design of Physician Payment Incentives.”. Milbank Quarterly. 2001;79(2):149–77. doi: 10.1111/1468-0009.00202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson J C, Casalino L P. “The Growth of Medical Groups Paid through Capitation in California.”. New England Journal of Medicine. 1995;333(25):1684–7. doi: 10.1056/NEJM199512213332506. [DOI] [PubMed] [Google Scholar]
- Robinson J C, Casalino L P. “Vertical Integration and Organizational Networks in Health Care.”. Health Affairs. 1996;15(1):7–22. doi: 10.1377/hlthaff.15.1.7. [DOI] [PubMed] [Google Scholar]
- Rosenthal M B, Frank R G, Buchanan J L, Epstein A M. “Transmission of Financial Incentives to Physicians by Intermediary Organizations in California.”. Health Affairs. 2002;21(4):197–205. doi: 10.1377/hlthaff.21.4.197. [DOI] [PubMed] [Google Scholar]
- Sappington D E M. “Incentives in Principal–Agent Relationships.”. Journal of Economic Perspectives. 1991;5(2):45–66. [Google Scholar]