Abstract
Objective
To determine whether caregiving grandparents are at an increased risk for depressive symptoms.
Data Source
National sample (n=10,293) of grandparents aged 53–63 years in 1994, and their spouse/partners, who took part in the Health and Retirement Study (HRS).
Study Design
Grandparents were surveyed in 1994 and resurveyed every two years thereafter, through 2000. Over that period, 977 had a grandchild move in or out of their home. These grandparents served as their own controls to assess the impact of having a grandchild in the home.
Data Extraction
Depressive symptoms were measured using an abbreviated form of the Center for Epidemiologic Studies—Depression (CES-D) scale, scored 1–8, with a score ≥4 associated with depression “caseness.”
Principal Findings
At the time of the 1994 interview, 8.2 percent of grandparents had a grandchild in their home. However, there was substantial variation across demographic groups (e.g., 29.4 percent of single nonwhite grandmothers, but only 2.0 percent of single white grandfathers had a grandchild in residence). The impact of having a grandchild in the home varied by grandparent demographic group, with single grandparents and those without coresident adult children experiencing the greatest probability of elevation in depressive symptoms when a grandchild was in residence. For example, single nonwhite grandmothers experienced an 8 percentage point increase in the probability of having a CES-D score ≥4 when a grandchild was in their home, compared to when a grandchild was not in their home, controlling for changes in health care, income, and household composition over time (95 percent CI=0.1 to 15.0 percentage points).
Conclusions
Grandparents have a greater probability of elevated depressive symptoms when a grandchild is in their home, versus when a grandchild is not in their home. Single women of color bear a disproportionate burden of the depression associated with caring for grandchildren. Since an increasing number of grandparents function as a de facto safety net keeping their grandchildren out of formal foster care, identifying strategies to support the health and well-being of caregiving grandparents is an emerging priority.
Keywords: Depression, women's health, minority groups, socioeconomic factors, caregivers
A striking feature of the American demographic landscape is the growth in grandparent-headed households. In 1997, 3.9 million U.S. children lived in a grandparent's home, a 76 percent increase from 1970 (Caspar and Bryson 1998). Grandparent-headed households are found disproportionately in communities of color, and caregiving grandparents are at high risk for poverty (Caspar and Bryson 1998). In approximately two-thirds of grandparent-headed households, at least one of the grandchild's parents is also in residence (“three generation” households); in the remainder, the parents are absent (“split generation” households) (Caspar and Bryson 1998). Grandparent-headed households form under various circumstances, which may include parental divorce, drug-addiction, mental illness, incarceration, or death (Minkler 1999).
While grandparents may derive pleasure and positive challenge from having a grandchild in residence, studies have consistently documented social isolation and financial, physical, and emotional hardship among caregiving grandparents, as well as limited time and energy for self-care (Minkler 1999; 1993; Burton 1992). Numerous studies have linked grandparent caregiving to increased depressive symptoms (Minkler 1999; 1993; Burton 1992; Minkler et al. 1997; Szinovacz, DeViney, and Atkinson 1999; Strawbridge et al. 1997) and poor health (Minkler and Fuller-Thomson 1999; Solomon and Marx 1999). However, much of this work has been based upon convenience samples, and more importantly, much of it has been cross-sectional or based upon limited observation of individuals over time. Because of the correlation between becoming a caregiver and race/ethnicity/socioeconomic status, these studies cannot assess whether caregiving causes increased depressive symptoms. In the present study, this limitation is overcome by repeatedly observing a large nationally representative sample of grandparents over an eight-year period. Grandchildren move in and out of their grandparent's homes with some frequency, allowing us to test the hypothesis that having a grandchild in the home is associated with elevated depressive symptoms.
Methods
Data Source
The Health and Retirement Study (HRS), is a nationally representative longitudinal survey of middle-aged and older individuals that has been described in detail elsewhere (University of Michigan, Health and Retirement Study, accessed Jan. 1, 2000). Subjects were first interviewed in person in 1992. In subsequent, two-year intervals respondents were reinterviewed, generally by telephone. Interviews were in English or Spanish. The work reported here is based upon interviews conducted during four waves (1994, 1996, 1998, and 2000); the 1992 data is not used because the depression variable of interest was not consistently collected in the 1992 interview.
Sample
Subjects were included in these analyses if (1) they and/or their spouse/partner had at least one grandchild; and (2) they or their spouse/partner were householders (i.e., were named on the mortgage or rental lease for their home). The latter criterion was used because it seems likely that grandparents who had moved into their children's home would be less apt to be responsible for a grandchild's care. Numbers of subjects in the sample panel varied across waves; for example, 8,409 grandparents met eligibility criteria in the 1994 wave. Those who were not grandparents in 1994 but subsequently became grandparents entered the panel, as did new spouse/partners of grandparents already in the panel (a total of new 1,884 entrants after 1994). Of the 8,409 respondents to the 1994 wave, 6,419 (77 percent) were still responding in 2000. Discontinuation of response was more common among males, those in poor health, and those with depression scores >0 in 1994. Discontinuation of response was not related to having a grandchild in the home in 1994 (p=0.34) or any other year.
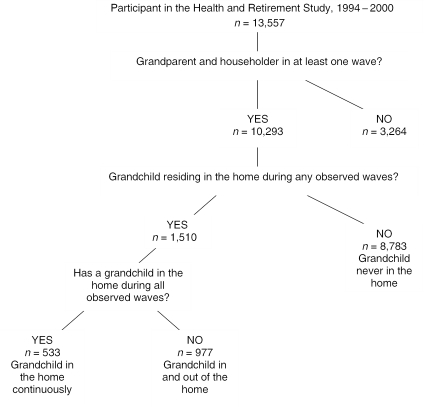
As shown in Figure 1, over the four waves, 10,293 of the 13,557 HRS respondents (75.9 percent) met the eligibility criteria for at least one wave. Of the eligible grandparents, 1,510 (16.7 percent) had a grandchild residing in their home during at least one wave. For the majority of these (977 of 1,510) the grandchild was not in the household during every wave, and so it was possible to observe these subjects both with and without the grandchild in residence. These 977 subjects (hereinafter “switchers”) are key in identifying the impact of having a grandchild in the home.
Figure 1.
Subsets of Participants in the Health and Retirement Study, 1994–2000
Note: Numbers are unweighted.
Measures
Household Composition
During each interview, subjects were asked to enumerate all people in their household, and to provide the ages and their relationships to each of those people. It was therefore possible to ascertain whether there were grandchildren (or great-grandchildren) in residence, and whether the respondent had a spouse/partner or any adult children in residence. However, because household composition was elicited with respect to relationship to the respondent, it was not possible to determine whether resident adult children were parents of a grandchild in residence. For example, a household headed by a respondent co-residing with an adult female child and grandchild could either be composed of a grandchild and that grandchild's mother, or a grandchild and that grandchild's aunt.
Depressive Symptoms
A count of depressive symptoms was derived from an eight-item abbreviated form of the Center for Epidemiologic Studies—Depression (CES-D) instrument. This abbreviated version uses fewer items than the full CES-D, and elicits yes/no responses, rather than responses on a Likert scale of frequency. It was used in the HRS because pilot work showed that some respondents had difficulty responding over the telephone to the full CES-D. In the abbreviated version, subjects were asked to “think about the past week and the feelings you have experienced. Please tell me if each of the following was true for you much of the time this past week. (Would you say yes or no?) (1) Much of the time during the past week, you felt depressed; (2) Much of the time, you felt that everything you did was an effort; (3) Much of the time, your sleep was restless; (4) Much of the time, ‘you could not get going’; (5) Much of the time, you felt lonely; (6) Much of the time you enjoyed life; (7) Much of the time during the past week, you felt sad; and (8) Much of the time, you were happy.” Responses were scored on a scale of 0 to 8 points, with one point allocated to each dysphoric response. The questions were not asked of proxy respondents. Prior research has shown that the abbreviated scale has acceptable internal consistency (Cronbach's alpha, r=0.81) and a factor structure and distribution that are similar to the full 20-item version (Turvey, Wallace, and Herzog 1999). Research suggests that the appropriate cut point for depression “caseness” is ≥4 dysphoric responses, corresponding to a score of ≥16 on the full CES-D (HRS Health Working Group 2002).
Other Covariates
Gender, race/ethnicity, and educational attainment were ascertained, as was household income over the prior year. Also collected were general health, number of doctors visits and hospitalizations in the recent past, health insurance status, and the number of chronic diseases, out of a possible four (hypertension, lung disease such as chronic bronchitis or emphysema, heart disease, and diabetes).
Model, Analytic Approach, and Estimation Strategies
We hypothesized that having a grandchild in the household would directly increase depressive symptoms. Based upon the literature cited above, we also hypothesized that this direct effect can be mitigated by the presence of a partner or adult child who may reduce isolation, provide assistance and support with child care, and free up time and resources for self-care.
Our analyses began by profiling the 1994 cross-section and then exploring the extent to which having a grandchild in the home influenced CES-D score in various gender, partnered/single, and race strata across time. The frequency of CES-D score was tabulated as household composition varied, pooling all of the person-waves for switchers in each stratum. Finally, multivariate estimates of the impact of having a grandchild in the home were developed, using fixed-effects panel data analytic approaches from the field of econometrics (Wooldridge 2002). These techniques are suited to instances in which individuals are repeatedly observed with respect to an outcome of interest over time, while their status with respect to an independent variable of interest changes. The methods allow for “unbalanced panels”—that is, for the entry and exit of individuals from the sample over time, as occurred in the HRS. Models are of the form:
in which i individuals are followed for t waves, with their household composition varying across waves (grandchild, adult child, and/or partner in the home). Characteristics X6 thru n may vary within subjects across waves (for instance, household income, recent receipt of medical care); fixed individual characteristics αi are constant within subjects across waves (for instance, gender); and γt captures cross-wave variation in the mean of CES-D. We hypothesize that b1 is greater than zero. We also hypothesize that the sum b1+b3 is not greater than zero, and the sum b1+b5 is not greater than zero. Hereinafter, we refer to these latter two hypotheses as the “mitigating hypotheses”; they reflect our expectation that there is no adverse effect of having a grandchild in the home, if an adult child or partner is also present.
Multivariate models were estimated with various functional forms and specifications. We examined models that treated the CES-D as a continuous interval measure with values 0–8, as an ordered measure with nine values, and as a dichotomous measure (≥4 or not); both linear and logistic forms were examined. While all approaches yielded similar patterns of findings in terms of signs and significance of coefficients, the results that were most intuitively interpretable—and most consistent with the bivariate findings—came from linear probability models. These are ordinary least squares models run with dichotomous dependent variables, with the interpretation of coefficients in terms of the percentage point change in the probability of the dichotomous outcome occurring (Wooldridge 2003). This is an absolute (i.e., difference) measure of impact. In contrast, epidemiologists generally use logistic regression models with dichotomous dependent variables, with odds ratios approximating risk ratios. These are of course relative (i.e., ratio) measures of impact. But odds ratios have the disadvantage of overstating the apparent effect for common outcomes. Since CES-D scores ≥4 were quite common in the switcher sample, logistic models gave grossly inflated apparent measures of impact. We therefore present findings from the linear probability analyses here.
In specifying models, we were mindful that depressive symptomatology and other factors such as overall health may be causally related. They may be codetermined (factors that increase depressive symptoms may also be associated with a decline in health), or they may be directly causally related, in either direction (poor health causes depression, or vice-versa). Because of the possibility of codetermination, the models of current depressive symptoms shown here do not include current health as a covariate (although they do include number of recent medical encounters and underlying chronic diseases; moreover, auxiliary models that included general health did not substantially yield different estimates). Due to data limitations, our models do not include factors outside the home such as social supports or other measures of social capital, nor do they include the characteristics of the child or children in residence. Because prior work has suggested differential effects of caregiving grandparenthood on men and women (Szinovacz, DeViney, and Atkinson 1999), we estimate models separately by gender. Additionally, because some work has suggested differential effects of caregiving on white and black grandparents (Pruchno 1999; Pruchno and McKenney 2002), we examine subgroups by race, with “white” denoting non-Hispanic whites, and “nonwhite” denoting blacks, Asians, Hispanics, and those designated “other.”
Weights, Sample Design, and Missing Data
The descriptive statistics presented here are weighted and standard errors are adjusted to reflect the HRS sampling design. Multivariate statistics are unweighted and uncorrected. The rationale for this choice and details regarding the handling of missing data appear in the online-only appendix available at http://www.blackwell-synergy.com.
Findings
At the time of the 1994 interview, 8.2 percent of grandparents had a grandchild in their home, but this varied substantially across demographic groups. For example, 9.4 percent of all women, 6.7 percent of all men, 5.9 percent of white women, 23.7 percent of nonwhite women, 4.8 percent of white men, and 15.4 percent of nonwhite men had a grandchild in residence. A demographic group for which having a grandchild in the home was particularly common was nonwhite single women (29.4 percent); one for which it was particularly uncommon was white single men (2.0 percent).
Table 1 gives more information about the 1994 cross-section. It takes advantage of our knowledge of grandparent caregiving patterns over the subsequent eight-year period, comparing the characteristics of those who ultimately fell into the three groups shown in Figure 1. The three groups differed substantially, with those in groups 1 (grandchild in the home continuously) and 2 (grandchild in and out of the home; the “switchers”) consistently more disadvantaged than those in group 3 (grandchild never in the home) in terms of socioeconomic status and health.
Table 1.
Characteristics of Grandparents According to Their Caregiving Status across Waves, 1994*
| Caregiving Status across Waves | |||
|---|---|---|---|
| (1) | (2) | (3) | |
| Grandchild in the Home Continuously* | Grandchild in and out of the Home* | Grandchild Never in the Home* | |
| Sociodemographic | |||
| Female (%) | 66 | 59 | 55† |
| Post-high school education (%) | 18 | 28 | 33.†,‡ |
| Race (%) | |||
| White | 46 | 60 | 85†,‡ |
| Black | 35 | 22 | 8 |
| Latino, non-black | 18 | 15 | 5 |
| Other | 1 | 3 | 2 |
| Age (mean) | 57.7 | 57.1 | 57.6§ |
| Household income (median) | $22,372 | $29,040 | $37,200∥,¶ |
| Health, health care, insurance | |||
| Number of chronic conditions (%) | |||
| None | 33 | 40 | 44†,‡ |
| One | 38 | 34 | 35 |
| Two or more | 29 | 26 | 21 |
| General health status (%) | |||
| Excellent | 11 | 15 | 19†,‡ |
| Very good | 24 | 25 | 31 |
| Good | 32 | 29 | 29 |
| Fair | 20 | 19 | 14 |
| Poor | 14 | 11 | 7 |
| Hospitalized in prior 2 yrs (%) | 21 | 20 | 17†,‡ |
| # MD visits in prior 2 yrs (median) | 4 | 3 | 4¶ |
| Health insurance (%) | |||
| Private | 62 | 72 | 83†,‡ |
| Public | 18 | 11 | 8 |
| None | 20 | 17 | 10 |
| Household Composition | |||
| Partner in household (%) | 68 | 72 | 81†,‡ |
| Adult child in household (%) | 68 | 52 | 23†,‡ |
Notes:
Weighted statistics based upon the cross section of grandparents who were in the sample in 1994 (n=8,409). Unweighted sample size for first column=440; second column=882; third column=7,087.
p<.05 for chi2 test (Column 1 vs. column 3);
p<.05 for chi2 test (Column 2 vs. column 3);
p<.05 for t-test of difference of means (Column 2 vs. column 3);
p<.05 for Mann Whitney U test of difference of medians (Column 1 vs. column 3);
p<.05 for Mann Whitney U test of difference of medians (Column 2 vs. column 3).
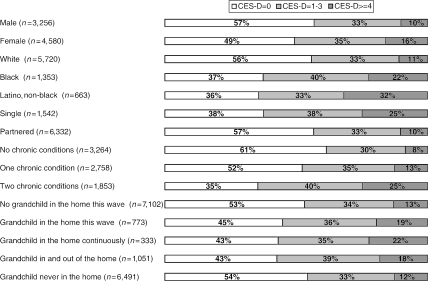
Figure 2 illustrates the association between the outcome of interest (CES-D score) and selected characteristics and household compositions, again in the 1994 cross-section. Those who were female, nonwhite, nonpartnered, or who had more chronic conditions were more likely to have a high number of depressive symptoms. The last several bars of the figure begin to suggest an association between grandparent caregiving status and CES-D. Higher depressive symptoms scores were found among those with grandchildren in their home (CES-D score ≥4 for 13 percent of those without a grandchild in the home, versus 19 percent for those with a grandchild in the home, a 6 percentage point difference, p≤.001 for the test of the difference of proportions). Those who never had a grandchild in the home had a relatively lower percentage with a CES-D score ≥4 (12 percent), as compared with “switchers” (18 percent) and those who had a grandchild in the home continuously (22 percent); p<.01 for the difference in proportions between all groups.
Figure 2.
Distribution of Abbreviated CES-D Scores for All HRS Grandparents, by Selected Characteristics, 1994
Note: Figure reflects the characteristics of HRS grandparents who were in the sample in 1994 and had valid CES-D data (n=7,875). The n's in parenthesis indicate the unweighted number of 1994 HRS grandparents with each characteristic. The n's for some exhaustive characteristics do not total 7,875 due to missing data.
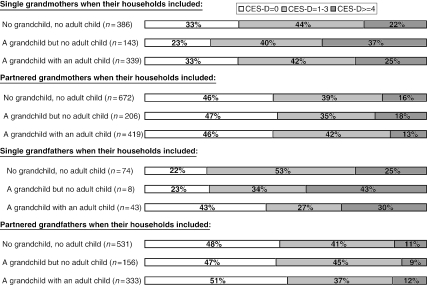
Figure 3 depicts findings over time, as grandchildren moved in and out of their grandparents' homes. Data from these figures were drawn from switchers only, and the unit of observation was the “person-wave.” For example, a switcher grandmother who was in the HRS sample for all four waves contributed four person-waves (observations) to Figure 3. If she lived alone for two waves, then she contributed two observations to the first bar of that figure; if she had a grandchild but no adult child in her home for the other two waves, then she contributed two observations to the second bar. For simplicity, the figure shows selected household configurations only. Some of the bars are based on a relatively small number of observations, and no statistical tests are performed.
Figure 3.
Distribution of Abbreviated CES-D Scores for All “Switcher” HRS Grandparents as Their Household Composition Varied, 1994–2000
Note: Descriptive data drawn from grandparents who had a grandchild move in or out of their home at least once during four waves of observation. Each person-wave counted once (see text for discussion). The n's in parentheses denote the number of person waves contributing to each descriptive bar is shown in parentheses. Only selected household configurations are shown.
The pattern in Figure 3 is consistent with our hypothesis that having a grandchild in the home elevates the probability of having a CES-D score ≥4. For example, the first bar of the figure shows the distribution of CES-D scores for the 386 person waves in which single switcher grandparents' households included neither a grandchild nor a child. For 22 percent of those observations, the grandmother had a CES-D score of ≥4. In contrast, the second bar of Figure 3 shows the distribution of scores for the 143 person waves in which single switcher grandmothers had a grandchild in the home, but no adult child. For 37 percent of those observations, the CES-D score was ≥4. The probability of having a CES-D score ≥4 is elevated by 15 percentage points (37 percent–22 percent).
The pattern of findings in the figure is consistent with the two “mitigation” hypotheses. Compared to partnered grandparents, single grandparents appear to experience a greater increase in the probability of having a score ≥4 when a grandchild moves in (compare Figure 3, bars 1 and 2 for single grandmothers to bars 1 and 2 for partnered grandmothers). Also as predicted, having a co-resident adult child in the home appears to mitigate the adverse effect of having a grandchild in the home (compare Figure 3, bars 1 and 2 for single grandmothers with bars 1 and 3 for the same group).
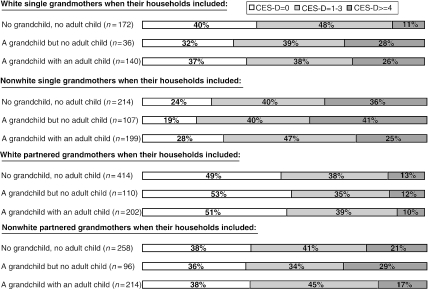
Figure 4 focuses just on grandmothers (the majority of caregiving grandparents), depicting white and nonwhite grandmothers separately. It highlights the extent to which nonwhite grandmothers face a higher baseline likelihood of having CES-D scores ≥4. For single grandmothers—both white and nonwhite—having a grandchild in residence appears to be associated with an increased risk of depressive symptoms (Figure 4, the first two sets of bars). For partnered grandmothers, the effect differs by race/ethnic group. White partnered grandmothers apparently do not experience an elevation in depressive symptoms when a grandchild is in the household (Figure 4, third set of bars). In contrast, nonwhite partnered grandmothers experience an elevation in depressive symptoms when the grandchild is in the household, despite the partner's presence (Figure 4, fourth set of bars).
Figure 4.
Distribution of CES-D Scores for White and Nonwhite “Switcher” HRS Grandmothers as Their Household Composition Varied, 1994–2000
Note: Descriptive data drawn from grandmothers who had a grandchild move in or out of their home during at least one of the four waves of observation. Each person-wave counted once (for example, those present in 4 waves contribute 4 data points). The n's in parentheses denotes the number of person waves contributing to each descriptive bar. Only selected household configurations are shown.
Table 2 provides fixed effects multivariate estimates of the impacts suggested by Figures 3 and 4, as well as formal statistical tests of our hypotheses. The table presents only those coefficients about which we had hypotheses (for full sets of coefficients see the online-only appendix, Table 1). The first coefficient in the first column implies that, compared with when a grandchild is not in their home, grandmothers who have neither a partner nor an adult child co-residing have an 8 percentage-point increase in the probability of having a CES-D score ≥4 when a grandchild is in their home, adjusting for changes in the covariates (95 percent CI 2.9 to 13.2 percentage points). The corresponding increase for white grandmothers is 8.9 percentage points, and 8 percentage points for nonwhite grandmothers (small sample sizes precluded our getting separate estimates for blacks and Latinas, the largest nonwhite subgroups). Impacts for grandfathers were considerably higher (a 14.5 percentage-point increase for all men; the adverse effect is not statistically significant for white grandfathers, but is 22.7 percentage points for nonwhite grandfathers). In sum, for nearly all subgroups, the findings support our hypothesis that having a grandchild in the home increases depressive symptoms.
Table 2.
Key Coefficients* from Fixed Effects Linear Probability Models of the Likelihood of Having an Abbreviated CES-D Score ≥4, HRS Grandparents, 1994–2000 (by Gender, by Race/Ethnicity Subgroups within Gender)
| All Women | White Women | Nonwhite Women | All Men | White Men | Nonwhite Men | |
|---|---|---|---|---|---|---|
| Grandchild in home [b1] | 0.080‡ | 0.089† | 0.080‡ | 0.145† | 0.062 | 0.227† |
| (0.029–0.132) | (0.016–0.162) | (0.009–0.150) | (0.028–0.263) | (−0.110–0.234) | (0.065–0.388) | |
| Grandchild * adult child [b3] | −0.070‡ | −0.054 | −0.075‡ | −0.029 | −0.017 | −0.040 |
| (−0.119–−0.021) | (−0.120–0.011) | (−0.147–−0.003) | (−0.082–0.024) | (−0.078–0.045) | (−0.132–0.052) | |
| Grandchild * partner [b5] | −0.039 | −0.091† | 0.003 | −0.164‡ | −0.088 | −0.237‡ |
| (−0.089–0.012) | (−0.161–−0.022) | (−0.069–0.076) | (−0.277–−0.050) | (−0.254–0.078) | (−0.394–−0.080) | |
| # of persons | 5435 | 3854 | 1576 | 4206 | 3133 | 1064 |
| # of person-waves (observations) | 17298 | 12541 | 4740 | 12332 | 9460 | 2851 |
| R-squared (includes fixed effects) | 0.594 | 0.568 | 0.610 | 0.612 | 0.590 | 0.638 |
| Net impact of grandchild in home§ | ||||||
| With adult child co-residing [b1+b3] | 0.010 | 0.034 | 0.004 | 0.116 | 0.045 | 0.186† |
| (−0.041–0.061) | (−0.037–0.106) | (−0.069–0.078) | (−0.014–0.248) | (−0.142–0.232) | (0.001–0.373) | |
| With partner co-residing [b1+b5] | 0.041 | −0.002 | 0.082† | −0.018 | −0.025 | −0.010 |
| (−0.014–0.096) | (−0.076–0.072) | (0.001–0.165) | (−0.067–0.031) | (−0.802–0.029) | (−0.102–0.081) | |
Coefficients derived from fixed effects linear probability models in which time-varying variables were: adult child in home, partner in home, number of chronic diseases, any hospitalizations in the prior 2 years indicator, number of doctor visits in the prior 2 years, health insurance type (indicator variables: public, private), age, household income, and wave indicators. 95% confidence intervals appear below the coefficients, and are derived with Huber-White robust standard errors.
Coefficient significantly different from zero at p<.05;
Coefficient significantly different from zero at p<.01;
Linear combination of the indicated coefficients, reflecting the change in the probability that the grandparent will have a CES-D score ≥4 when a grandchild is in the home, compared with when a grandchild is not in the home, given that an adult child co-resides (penultimate row) or a partner co-resides (final row).
However, the findings also generally support the mitigation hypotheses, meaning that this increase does not occur if either an adult child or partner co-resides. The negative signs on the interaction coefficients suggest this. Formal statistical tests appear in the penultimate lines of Table 2, with point estimates and 95 percent confidence intervals for impact having a grandchild in the home along with an adult child (the penultimate row) or along with a partner (the final row). For most subgroups these interval estimates pass through zero, meaning that there is no increased risk of depression with a grandchild in the home, provided an adult child or partner co-resides. There are two notable exceptions. First, nonwhite women experience an adverse effect of having a grandchild in their home despite the presence of a partner (probability of CES-D score ≥4 increases by 8.2 percentage points when the grandchild is in the home); conversely, nonwhite men experience an adverse effect of having a grandchild in the home despite the presence of an adult child (probability of CES-D score ≥4 increases by 18.6 percentage points when a grandchild is in the home).
We examined many alternative specifications to the model shown in Table 2. In one set, we explored the temporal impact of having a grandchild in the home. That is, we looked at (1) whether the elevation in depressive symptoms precedes the grandchild's arrival, and (2) whether it is sustained after the grandchild leaves. To address (1) we tested whether current wave depression is predicted by next wave grandchild-in-home status. We found no evidence that that it was (online-only appendix, Table 2). To address (2) we tested whether having a grandchild in the home in the prior wave has an impact on current wave CES-D score. Again, we found no evidence that it does, for men or women (online-only appendix, Table 3). These findings are consistent with the elevation in depressive symptoms reflecting the stress of having the grandchild in residence, rather than simply reflecting global family dysfunction.
We also explored models in which the sample included only “switcher” grandparents. The magnitude of the effects and the pattern of statistical significance were essentially unchanged. The same was true of analyses in which current wave general health and employment status were covariates. Models that included number of grandchildren and ages of grandchildren as interaction terms were not informative, due to relatively large standard errors on those terms.
Discussion
This study provides evidence of a causal link between grandparent caregiving and depression, using a large nationally representative sample, with a relatively strong design that is rarely employed by health services researchers in the analysis of individual-level data. Following the same individual across time, taking a grandchild into the home is associated with an increased probability of having a CES-D score ≥4, controlling for other factors that may have changed over time. The impact varies across demographic subgroups. In the subgroup of grandparents with the highest prevalence of caregiving—single nonwhite women—there is an 8 percentage-point increase in the probability of having a CES-D score ≥4 when a grandchild is in the home, compared with when the grandchild is not in the home. To interpret this absolute impact, it is useful to recall that 36 percent of single nonwhite grandmothers living alone have a CES-D score of ≥4 (Figure 4, second set of bars, bar 1). When a grandchild moves in, the accompanying adjusted 8 percentage-point increase (Table 2, Column 3) translates into 44 percent having a CES-D score ≥4.
Gender, race/ethnicity, and household supports have important connections with the relationship between grandparent caregiving and depressive symptoms. One connection is well known and previously documented: grandparent caregiving is more prevalent among women, nonwhites, and those who are single (Caspar and Bryson 1998). The second connection is not widely appreciated, and it emerged in our analyses: while grandparent caregiving itself increases depressive symptoms, this adverse impact is not felt (is mitigated) for those with a partner or adult child in their home along with the grandchild, in some demographic subgroups.
These findings have important implications for the population distribution of the burden of caregiving-associated depressive symptoms. With respect to gender, men arguably experience relatively less burden than women. For men, having a partner mitigates the adverse impact of having a grandchild in the home, and so the large adverse impact of having a grandchild in the home reported here applies only to single men. As we have shown, it is relatively rare for a single grandfather to have a grandchild in his home. With respect to race/ethnicity, a heavier burden arguably falls on nonwhites, particularly nonwhite women, who experience a negative impact of having a grandchild in their homes whether they are single or partnered (Figure 4; also Table 2). And as previously shown, the point prevalence of caregiving grandmotherhood is high among nonwhite women, both single (29.4 percent) and partnered (19.1 percent).
How does the impact of caregiving grandparenthood compare to that of other life events that may increase depressive symptoms? Because the abbreviated CES-D is relatively new, there is no published work to shed definitive light on this issue. Nonetheless, we present a rough estimate in the online-only appendix to this paper. Referencing published impacts of stressful life events using the full CES-D (Glass, Kasl, and Berkman 1997), we find that having a grandchild move in to one's home over the past two years is roughly comparable to that of being a victim of a crime, or having one's spouse have a serious injury, illness, or hospitalization, in terms of its impact on CES-D score.
There are many limitations to this study. While the panel design overcomes many of the selection problems that limit cross-sectional studies, there are still caveats with respect to causal inference. Perhaps the most important of these has to do with the causal entity: Is it having a grandchild in the home per se that elevates depressive symptoms, or is it family dysfunction that makes the grandchild need care, and the grandparent more prone to depressive symptoms? While we cannot answer this within our data definitively, the fixed-effects approach implicitly holds constant prior history. Moreover, we found no anticipatory effect of having a grandchild in the home next wave. This is consistent with a depressive effect of co-residence per se. In a related vein, “caregiving” and “co-residence” are different causal entities. To what extent do our findings support caregiving as an explanation for the findings? Perhaps the strongest evidence comes from our finding that the adverse effect of co-residence is largely concentrated among grandparents without another adult in the home. Surely these single grandparents bear a substantial portion of the burden of caring for co-resident grandchildren: if they are not the caregivers, then who is?
The generalizability of the study is limited by several factors. While the sample was nationally representative, it drew from a limited age range. The median age of grandparents in the first wave of the study was 57.6 years; this is close to the median age of U.S. grandparents who have ever had primary responsibility of caring for a grandchild (59.4 years) (Fuller-Thomson, Minkler, and Driver 1997). The exclusion of younger grandparents may have meant that those who were parents at a young age were underrepresented. To the extent that these younger grandparents experienced hardships that left them more vulnerable to depression, the study may underestimate the impact of caregiving grandparenthood on depression. A more subtle issue with respect to generalizability is that the impacts on depression reported here are derived from “switchers.” Their response to having a resident grandchild may differ from the response that would occur in other groups of grandparents, were those other groups to have a grandchild move in.
An important issue that is beyond the scope of this study—and one that naturally follows from its findings—is that of the dynamics underlying the findings. When and why is grandparent caregiving associated with dysphoria? As has been noted previously (Minkler et al. 1997), the circumstances leading up to caregiving grandparenthood often leave grandparents feeling ashamed or humiliated at their perceived failure as parents. Isolation may be compounded when pressing demands of caregiving compel grandparents to put their lives “on hold.” These events may give rise to feelings of loss, humiliation, and entrapment—all of which are important underlying vulnerabilities to depression (Brown, Harris, and Hepworth 1995). However, our data cannot shed light on how and why particular grandparent–grandchild configurations lead to depression in grandparents, or what kinds of out-of-home supports might minimize grandparent symptomatology.
For clinicians, this report underscores the importance of the “social history.” In addition to treating clinical depression as appropriate, clinicians should be aware of the resources that are available to caregiving grandparents.1 Support groups are among the most popular, and in qualitative studies have been shown to reduce stress and ease isolation for those raising grandchildren without another adult in their home (American Association of Retired Persons 2003). Data demonstrating that such groups relieve depression, however, are lacking.
Policymakers should be aware that caregiving grandparents are the safety net keeping a growing number of American children out of the dysfunctional and expensive foster care system: nearly twice as many children live in the informal sole care of their grandparents as are in the entire formal foster care system (Caspar and Bryson 1998; Generations United, accessed August 23; 2003). Much evidence suggests that these grandparents make this vital social contribution despite limited personal resources, and at considerable personal cost. If these grandparents can be better cared for, their lives and those of their vulnerable grandchildren may be improved.
Acknowledgments
This project was supported by grant number R03 HS11747 from the Agency for Health Care Research and Quality.
Note
An electronic database of local support groups, along with links to information about public benefits, legal options, and other resources appears on the American Association of Retired Persons (AARP) website (at http://www.aarp.org/grandparents/#raise). Another accessible and useful compendium appears on the Generations United website (at http://www.gu.org).
References
- American Association of Retired Persons. “Lean on Me: Support and Minority Outreach for Grandparents Raising Grandchildren”. 2003 [accessed June 2003]. Washington, DC: AARP. Available at http://research.aarp.org/general/gp_2003.html. [Google Scholar]
- Brown G W, Harris T O, Hepworth C. “Loss, Humiliation and Entrapment among Women Developing Depression: A Patient and Non-Patient Comparison.”. Psychological Medicine. 1995;25(1):7–22. doi: 10.1017/s003329170002804x. [DOI] [PubMed] [Google Scholar]
- Burton L. “Black Grandparents Rearing Children of Drug Addicted Parents: Stressors, Outcomes and Social Needs.”. Gerontologist. 1992;32(6):744–51. doi: 10.1093/geront/32.6.744. [DOI] [PubMed] [Google Scholar]
- Caspar L M, Bryson K R. Co-Resident Grandparents and Their Grandchildren: Grandparent Maintained Families. Washington DC: U.S. Census Bureau; 1998. U.S. Census Bureau Population Division. Working paper no. 26. [Google Scholar]
- Fuller-Thomson E, Minkler D, Driver D. “A Profile of Grandparents Raising Grandchildren in the U.S.”. Gerontologist. 1997;37(3):406–11. doi: 10.1093/geront/37.3.406. [DOI] [PubMed] [Google Scholar]
- Generations United n.d. “Introduction to the Issue of Grandparents and Other Relatives Raising Their Grandchildren”. [accessed on August 22, 2003]. Available at http://www.gu.org/projg&ointro.htm. [Google Scholar]
- Glass T A, Kasl S V, Berkman L F. “Stressful Life Events and Depressive Symptoms among the Elderly: Evidence from a Prospective Community Study.”. Journal of Aging and Health. 1997;9(1):70–89. doi: 10.1177/089826439700900104. [DOI] [PubMed] [Google Scholar]
- HRS Health Working Group. Documentation of the Affective Functioning Measures in the Health and Retirement Study. Ann Arbor, MI: Survey Research Center, University of Michigan; 2002. Report no. DR-005. [Google Scholar]
- Minkler M. Grandparents as Caregivers: Raising Children in the Crack Cocaine Epidemic. Newbury Park, CA: Sage; 1993. [Google Scholar]
- Minkler M. “Intergenerational Households Headed by Grandparents: Contexts, Realities, and Implications for Policy.”. Journal of Aging Studies. 1999;13(2):199–218. [Google Scholar]
- Minkler M, Fuller-Thomson E. “The Health of Grandparents Raising Grandchildren: Results of a National Survey.”. American Journal of Public Health. 1999;89(9):1384–9. doi: 10.2105/ajph.89.9.1384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minkler M, Fuller-Thomson E, Miller D, Driver D. “Depression in Grandparents Raising Grandchildren: Results of a National Longitudinal Study.”. Archives of Family Medicine. 1997;6(5):445–52. doi: 10.1001/archfami.6.5.445. [DOI] [PubMed] [Google Scholar]
- Pruchno R. “Raising Grandchildren: The Experiences of Black and White Grandmothers.”. Gerontologist. 1999;39(2):209–21. doi: 10.1093/geront/39.2.209. [DOI] [PubMed] [Google Scholar]
- Pruchno R A, McKenney D. “Psychological Well-Being of Black and White Grandmothers Raising Grandchildren: Examination of a Two-Factor Model.”. Journal of Gerontology (Psychological Sciences) 2002;57B(5):444–54. doi: 10.1093/geronb/57.5.p444. [DOI] [PubMed] [Google Scholar]
- Solomon J C, Marx J. “Who Cares? Grandparent/Grandchild Households.”. Journal of Women and Aging. 1999;11(1):3–25. doi: 10.1300/J074v11n01_02. [DOI] [PubMed] [Google Scholar]
- Strawbridge W J, Wallhagen M I, Shema S J, Kaplan G A. “New Burdens or More of the Same? Comparing Grandparent, Spouse and Adult-Child Caregivers.”. Gerontologist. 1997;37(4):505–10. doi: 10.1093/geront/37.4.505. [DOI] [PubMed] [Google Scholar]
- Szinovacz M E, DeViney S, Atkinson M P. “Effects of Surrogate Parenting on Grandparents' Well-Being.”. Journal of Gerontology (Social Sciences) 1999;54B(6):S376–88. doi: 10.1093/geronb/54b.6.s376. [DOI] [PubMed] [Google Scholar]
- Turvey C L, Wallace R B, Herzog R. “A Revised CES-D Measure of Depressive Symptoms and a DSM-Based Measure of Major Depressive Episodes in the Elderly.”. International Psychogeriatrics. 1999;11(2):139–48. doi: 10.1017/s1041610299005694. [DOI] [PubMed] [Google Scholar]
- University of Michigan, Health and Retirement Study. n.d. The Health and Retirement Study Introduction and Guide [accessed on January 1, 2001]. Available at http://www.hrsonline.isr.umich.edu/intro. [Google Scholar]
- Wooldridge J M. Econometric Analyses of Cross Section and Panel Data. Cambridge, MA: MIT Press; 2002. [Google Scholar]
- Wooldridge J M. Introductory Econometrics. New York: Thomson Learning; 2003. [Google Scholar]